Learning Outcomes
- Participants will be able to identify their personal fitting philosophy.
- Participants will be able to develop fitting concepts and script messages that reflect their fitting philosophy.
- Participants will be able to implement these techniques within their clinical practice.
Introduction
Professional organizations such as the American Academy of Audiology, the Independent Hearing Aid Fitting Forum and others have provided hearing care practitioners with protocols to standardize the hearing aid fitting and rehabilitative experience. These protocols provide fitting professionals with a necessary starting point and technical guidelines for hearing aid fittings. However, a significant gray area exists between the technical requirements for a successful fitting (such as the use of pre-fitting objective tests, hearing inventories, and probe microphone measures), their routine implementation, and the verbal descriptions or “positioning” of these items within the fitting process. In the current environment, clinicians have tremendous freedom to experiment with a narrative that matches their professional philosophy and personality. However, the lack of any standardization of – or even contemplation about - these clinical messages limits the ability of the profession to measure the impact that counseling strategies have on the fitting. Furthermore, the lack of standardization also limits the possibility for any scientific examination and refinement beyond anecdotal report.
To help clarify this gray area, a review of our professional fitting protocols is necessary to establish a baseline for a good technical fitting. Next, there is a need to develop a common professional fitting philosophy to understand how the technical steps reinforce the patient journey toward better hearing and in turn how the fitter’s philosophy can reinforce the technical aspects of a fitting. Finally, a method to test our narratives and evaluate how we can improve our fittings is needed to answer the important question of ‘what’s in a fitting’ so that we can, as a final step, determine how to enhance our fittings. This paper will not support or refute any particular technique, approach or specific verbiage to fill the space between the technical requirements. Rather, the possibilities are offered to inspire the reader to reflect upon what is in your fitting and how your strategy can be refined to enhance your patients’ experiences.
A Brief Review of Fitting Protocols
A cursory Internet search using the terms “hearing aid fitting procedures” or “hearing aid fitting protocols” will reveal a wealth of information for both the hearing care professional and the consumer. For professionals, organizations including, but not limited to the International Society of Audiology, International Collegium of Rehabilitative Audiology, the American Academy of Audiology (AAA), and the American Speech-Language-Hearing Association (ASHA), all have clinical guidelines available for review. Likewise, organizations such as the National Acoustics Laboratories in Sydney Australia and the University of Western Ontario have published fitting protocols intended to optimize a fitting using their prescriptive gain targets.
Perhaps it is an over-generalization, but a common characteristic of these protocols and procedures is the focus on technical steps to optimize the fitting for each patient. Protocols of this nature provide the opportunity to approach each fitting from a scientific perspective to reduce the inter-patient variability that inevitably arises. For example, AAA, the Department of Veterans Affairs (VA), and ASHA established a joint hearing aid fitting protocol in 1997 (American Academy of Audiology, 2000). These groups designed this protocol for use as a “practice algorithm” providing the clinician with a visual method to facilitate decision making during the hearing aid assessment and fitting. Included in this algorithm are decision points to evaluate the patient’s acceptance of the hearing aid during the process as well as corrections to the process to be applied when needed. Clinical statements are interspersed throughout the protocol to highlight which assessment tools are appropriate for the scientific evaluation of the fitting for optimal rehabilitative care.
As another example, the Independent Hearing Aid Fitting Forum (IHAFF) developed a protocol that, at its core, uses a method for normalizing loudness growth for the hearing-impaired patient through amplification (Valente & Van Vliet, 1997). This protocol relies heavily on specialized tests for assessing the loudness preferences of the patient. Interestingly, both the joint AAA/ASHA/VA and the IHAFF protocols utilize some form of loudness growth assessment such as Most Comfortable Level (MCL) and Uncomfortable Level (UCL). The inclusion of these measurements in each protocol suggests a high level of importance on these metrics for patient acceptance criteria such as sound quality and speech intelligibility. Tools to evaluate the impact of the hearing loss as well as post fitting benefit outcome measures are also included in these two protocols. These examples of clinical protocols both provide sound technical guidance for the process of hearing care. However, a shared feature of these examples is the absence of a narrative to establish a patient-centered context for the technical steps and a pathway for long-term rehabilitative care.
Many of the protocols available today highlight probe microphone verification as an integral component of the fitting process. In addition to the importance placed on probe microphone measures from professional organizations, Consumer Reports (2015) has specifically identified this procedure as something consumers should inquire about when looking to purchase hearing instruments. Different protocols provide varied levels of information regarding which probe microphone tests to complete, the technical characteristics of the test setup, and potential test outcomes. However, there is little information provided to help the clinician develop a dialog based on the information gained from testing, or how the clinician should proceed based upon varied outcomes. As an example, clinicians who are resistant to using probe microphone measures often ask, “What do I do when I have matched target and the patient does not accept the sound of the instrument?" This objection can be a significant barrier preventing the widespread use of real ear measurement. Clinicians using probe microphone measures with regularity have undoubtedly created their own methods to work around this problem and to incorporate patient feedback as part of their fitting session. However, for the novice and the expert alike, there is little documented guidance for applying real ear measures in a patient-centered context. For example, the clinician can communicate to the patient that the verified settings represent the potential for “best audibility” based upon average levels derived from end user acceptance and performance in laboratory intelligibility tests. If the patient decides the sound of the target-matched settings are not acceptable, they are not lost or denied better hearing through amplification simply because their sound quality preference does not match an average prescribed by the target. An alternative could be to describe the patient’s preferred levels as falling within one, two, or more standard deviations from the prescribed target. Using that narrative, the “average target values” can serve as either a goal for adaptation, a metric for addressing problems that arise in day-to day use, or an upper end limit for a volume control or other patient-controlled adjustment.
As described above, when evaluating what is included in a fitting, the protocols describe the process as a series of lock-step procedures that create a predictable outcome. However, is fitting just a series of button presses, or is there something to a fitting that goes beyond these steps? The example above provides an instance where thoughtful dialog can provide the bridge between best practice application and real-world patient care. Could this positioning also affect patient outcomes? If the answer to that question is yes, is there a common philosophy that can help guide the fitting process above and beyond the protocols?
Developing a Patient-Centered Hearing Care Model
Patient-centered care is a hot topic throughout the medical community. The Institute of Medicine (2001) defines patient-centered care as care that is respectful of and responsive to individual patient preferences, needs, and values, and ensures that patient values guide all clinical decisions. A significant and increasing body of correlated literature is now available in the hearing care industry that describes how a model of shared decision-making between patient and clinician improves outcomes, lowers costs, and leads to greater satisfaction when applied during the patient journey. For example, Laplant-Levèsque and colleagues (2014) conducted research that examined baseline clinician preferences for a patient-centered style of clinical practice. Interestingly, the preference for applying patient-centered techniques varied substantially both by years of practice as well as clinical setting. Could this variation be a component of the fractured landscape within hearing healthcare? Grenness and colleagues (2015) expanded on this baseline research suggesting that clinicians did not regularly address the psychosocial aspects of hearing loss in a sample of clinical exchanges, and, as a result, these factors were not included in remediation plans. Poost-Foroosh, Jennings and Cheesman (2015) compared the views of both clinicians and patients on patient-centered practice characteristics. This research suggests that differences exist in the perceived importance of patient-centered practice between clinicians and patients. It provides further evidence that areas beyond the technical aspects of a fitting can have a profound impact on outcomes. Naylor, Öberg, Wänström & Lunner (2015) conducted an experiment where the settings of the instruments remained unchanged while the accompanying clinical narrative was adapted. In this experiment, the narrative had a measureable impact on patient outcomes. The impact was positive when it supported the stage of the patient (i.e. new user), and negative when there were no patient attributes included in the narrative. These articles only scratch the surface of an area that is in need of further research. However, they indicate that there is growing interest in this aspect of clinical practice to uncover what additional approaches should be encompassed in a fitting. Perhaps institutions of higher learning and professional associations can apply concepts, techniques and actual narratives from the research to help guide clinical dialogue that can enhance hearing healthcare. Alternately, could practicing clinicians themselves already have this narrative mapped out, and can we learn from each other?
The Role of a Fitting Philosophy
During the summer and spring of 2014, the authors of this article created a lecture series called “FittingNOW 2014.” FittingNOW 2014 was a manufacturer-sponsored workshop discussing non-manufacturer specific topics to enhance patient care. A component of the workshop was a presentation titled “How Does This Sound? Using Sound Quality to Guide Fittings.” In this section of the workshop, the questions, “What is your fitting philosophy?” and “How do you implement your philosophy?” were presented to the audience. Attendees wrote down responses to questions about their personal fitting philosophy and verbally shared their responses with the group. Forty-one written responses were collected across four different locations within the US and collated into a spreadsheet. The authors reviewed these responses to identify common themes and create an “average” philosophy and implementation. This information is shared within this article to provide some attention and direction towards the goal of a unified professional philosophy of clinicians providing hearing care services.
The “Average” Philosophies
Two primary trends emerged from the responses. The first trend is described here as the “subjective philosophy.” These philosophical statements focused on the comfort of sounds and the needs of the patient based on their lifestyle. Forty-five percent of responses were included within this group. The second primary trend is best described as an objective philosophy. This philosophy focused heavily on objective measures such as REM and first-fit targets as the starting point to set the hearing aids. Fifty-five percent of responses were judged to be objective in nature. Examples of statements that were judged as subjective or objective are displayed in Figure 1.
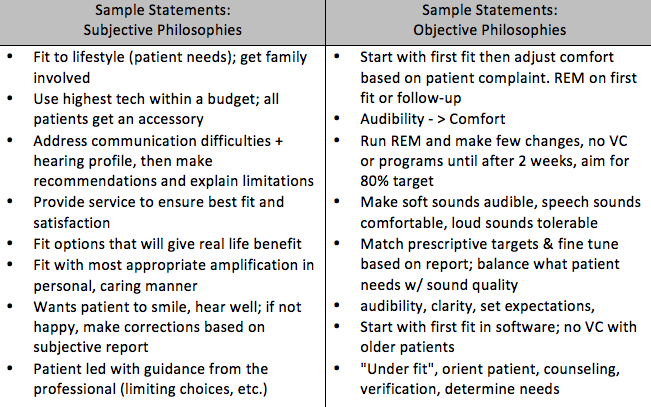
Figure 1. Examples of statements reflecting subjective and objective philosophies.
The second question, “How do you implement your philosophy?” yielded interesting results from the attendees. Of the respondents whose philosophies were judged to be subjective in nature, 35% included some mention of objective measures. The remaining 65% further defined messages and/or counseling strategies including phrases such as “communicate, build relationships, involve the family, review listening strategies, probe with specific questions regarding difficult listening situations." Of the respondents whose philosophies were judged to be objective in nature, 41% described or reinforced their probe microphone techniques. The remaining 59% added counseling, listening strategies and service offerings to add a more subjective implementation to their objective philosophy. Example statements supporting the various philosophy and implementation combinations are shown in Figure 2.
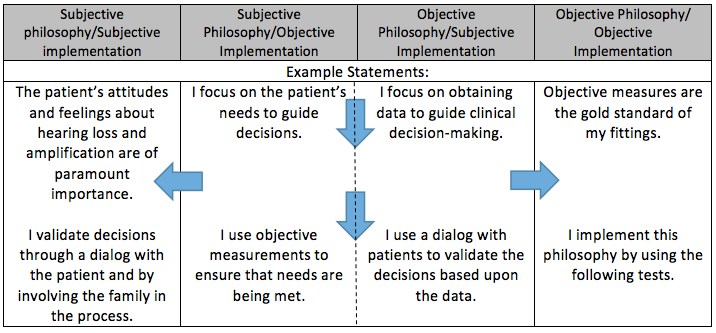
Figure 2. Examples of statements supporting the philosophy-implementation combinations.
A majority of the respondents in the two groups tended to meet in the middle when describing their philosophy and implementation; for example, an objective philosophy coupled with a subjective implementation, and vice versa. The few remaining individuals drifted further towards the periphery by reinforcing their subjective or objective philosophical slant. An additional area of common ground included frequent comments from both groups that indicated the importance of keeping the first fitting very simple by not introducing additional devices and feature options (VC, program button). Finally, it was not surprising that respondents reported a common focus on achieving a fit that the user would wear and be able to acclimatize to over time. Figure 3 illustrates the different combinations of responses obtained from the audiences.
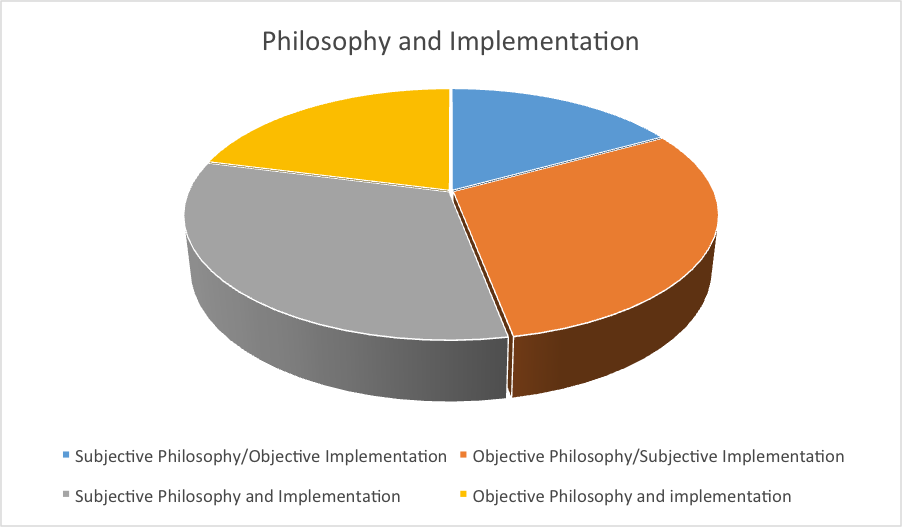
Figure 3: Combinations of responses to the question, "How do you implement your fitting philosophy?" Most attendees either stated a subjective philosophy that was supported objectively and/or vice versa. A smaller subset stated an either subjective or objective philosophy and then supported it with a corresponding subjective or objective implementation.
From Philosophy to Practice: Implications for Programming Hearing Instruments
It stands to reason that if clinicians consistently apply the philosophical statements previously described to every fitting, certain hallmark changes to hearing aid default settings should be visible in the fitting software. For example, many of the attendees explicitly stated a desire for “simplicity” for their patients. One potential fitting action that could enhance the “simplicity” philosophy and create an easy to use system, is to reduce the number of programs and to use automated features. This can have a positive influence on end users who lack the understanding of how and when to make manual changes to the hearing aids. As a second example, many attendees stated they strive to create a fitting that an end user “can accept and become accustomed to at the initial fitting that they will then acclimatize to over time.” The clinical action to accompany this philosophy should include a starting point with lower gain settings, and/or the use of automated acclimatization features. Finally, consistent use of real ear verification should lead to at least minor deviations from the initial gain prescribed in the fitting software based upon adjustments to compensate for individual ear canal differences. One novel way to examine the correlation between philosophy and programming of hearing aid parameters is to evaluate the settings in devices that are returned for credit to the manufacturer. A follow-up article will describe the findings of such a study.
Summary and Discussion: What is in a Fitting?
Trends in the industry including downward pressures on pricing are having an impact on the need of fitters to increase their clinical efficiency. This has the potential to move the profession to adopt more automated fitting procedures. However, this assumes that a fitting consists solely of technical settings that can be mass-produced and accepted by end users on a wide scale. To date, truly automated methods as such have been largely unsuccessful. It is the opinion of the authors that the fitting extends far beyond the technical aspects of the settings programmed into the hearing aid. The success of a fitting relies heavily on a practitioner-patient interaction that reinforces the concept of the patient journey. The interaction should include shared decision-making and co-ownership to help transition the patient from awareness that the hearing loss is problematic toward satisfactory remediation. Other key components beyond the technical settings include a philosophical underpinning that should not only guide decisions but also inspire patients to use the prescribed technology. Clinicians should base both settings and processes upon patient-specific data that supports the philosophical direction of the fitting, and use structured follow-up to reinforce and build upon the initial settings. Fittings should be goal-oriented where the initial session creates a listening experience that provides verified benefit and allows the user to feel confident with the amplification outside of the fitting suite. Clinicians can use verification techniques to meet these goals and to establish a baseline frame of reference. However, the messaging that accompanies these tests is of equal value. Too frequently, clinicians ask the question to their patient, “How does it sound?” However, typical answers such as "It sounds tinny" are immediately viewed as problematic and adjusted away. A potential alternative option to this question is to assess if the newness of the sound falls within a range that includes “different and new, but acceptable” as a first step on the path to better hearing. This can include statements such as “The hearing aids are now set for your hearing loss. Based on my experience and our goals for the fitting, the settings are an ideal starting point.”
In summary, best practice guidelines are a valuable tool to help clinicians ensure a technically good foundation for a first fit. However, it is equally important to first define your philosophy, find and resolve the areas where it deviates from your actual fitting process, and develop narratives to use with patients along the way. In other words, practice not only the procedures that ensure a good fitting, but also the dialogue that supports them. Only when we systematically evaluate and implement all of these factors and parameters can the profession begin to appropriately answer the question, “What is in a fitting?”
References
American Academy of Audiology. (2000). Audiology clinical practice and guideline statements. Audiology Today, Special Issue 2000, 32-49. Retrieved from: https://audiology-web.s3.amazonaws.com/migrated/ClinicalPracticeAlgorithms.pdf_53994878207278.74980219.pdf
Consumer Reports. (2015, September). Hearing aid buying guide. Retrieved from https://www.consumerreports.org
Grenness, C., Hickson, L., Laplant-Levèsque, A., Meyer, C., & Davidson, B. (2015). The nature of communication throughout diagnosis and management planning in initial audiologic rehabilitation consultations. Journal of the American Academy of Audiology, 26,36–50.
Institute of Medicine (2001). Crossing the quality chasm: A new health system for the 21st century. Available from: https://iom.nationalacademies.org/
Laplant-Levèsque, A., Hickson, L., & Grenness, C. (2014). An Australian survey of audiologists’ preferences for patient-centredness. International Journal of Audiology, 53, S76–S82.
Naylor, G., Öberg, M., Wänström G., & Lunner, T. (2015). Exploring the effects of the narrative embodied in the hearing aid fitting process on treatment outcomes. Ear & Hearing, 36(5),517-526.
Poost-Foroosh, L., Jennings, M.B., & Cheesman, M.F. (2015). Comparisons of client and clinician views of the importance of factors in client-clinician interaction in hearing aid purchase decisions. Journal of the American Academy of Audiology, 26(3), 247–259.
Valente, M., & Van Vliet, D. (1997). The Independent Hearing Aid Fitting Forum(IHAFF) protocol. Trends in Amplification (2)1, 6-35.
Citation
Hallenbeck, S.A., & Switalski, W. (2016, March). What's in a fitting? An examination of real world fitting protocols. AudiologyOnline, Article 16507. Retrieved from www.audiologyonline.com



