Editor’s Note: This text course is an edited transcript of an Otometrics webinar on AudiologyOnline. Download supplemental course materials.
Learner Outcomes
Today we will be talking about vestibular evoked myogenic potentials. I will provide a basic overview of the anatomy and physiology, some tips and tricks for running the test, diagnosis and interpretation, and discuss some Food and Drug (FDA) considerations.
At the end of this course, you will be able to describe the vestibular system and structures associated with the VEMP test, describe why EMG monitoring is essential for accurate cVEMP testing, and identify the structures involved in the cVEMP and oVEMP testing.
I hope you will come to understand that VEMP is easy to perform and much easier to record than a traditional ABR. The VEMP provides other information about the vestibular system that the other tests in our current battery do not provide. The VEMP also provides ear-specific information.
We are all aware that the VNG has its limitations, but how does the VEMP help assess the vestibular system? Remember that clinical data is always emerging. While it is an older test, it is new to us, we have to continue to research the literature so that we can provide the best information to our patients based on our test results. The number of publications has gradually increased, especially as the head impulse test (HIT) has emerged into clinical practice.
Review
I would like to begin with a vocabulary review so that we are on the same page.
The VEMP investigates otolith and vestibular nerve function. Dysfunction is characterized by feeling similar to being on a boat or an elevator. It may be a spinning sensation when people say that they are dizzy.
The VEMP is a short-latency electromyographic (EMG) potential and it is evoked in response to high-level acoustic stimuli. The responses are mediated by the vestibular system. It provides ear-specific information about otolith and nerve function.
Clinical Applications
Clinical applications go beyond dizziness. Patients with complaints of sound-evoked vestibular symptoms such as Tullio phenomenon or superior canal dehiscence (SCD). We can assess the saccule and the inferior portion of the vestibular nerve for different vestibular pathologies like Ménière’s or vestibular neuritis. We can also assess the utricle and the superior portion of the vestibular nerves. We are going beyond the semicircular canals in this case.
We also can do an assessment of young children and infants before cochlear implantation. We want to know if the system is intact before the implant array is placed. If there are any balance issues in recovery, we have a baseline for how things were working before as a comparison.
Other emerging data for clinical applications is auditory neuropathy. These children in many cases has abnormal VEMPs. The same is true for concussions. Interestingly, there are some studies coming out about diabetes and VEMP. It is a really important test in these other situations.
The Vestibulo-Ocular System
To continue with this basic review, think about the system. We receive an input, the brain processes it, and then we get the output. In this case of balance, we have ears, vision and somatosensory systems that are taking in information. When the brain receives information, it has to process who or what it needs to respond. It sends that message out to the reflex. This is the process that keeps us balanced, upright, and able to walk and multitask.
The saccule is responsible for acceleration in the vertical plane. When the saccule is intact, you are comfortable going up and down in an elevator. The utricle is responsible for acceleration in the horizontal plane, such as driving in a car. Once the otolith senses the motion, the brain sends the message to the reflex. The vestibulo-ocular reflex (VOR) is going to maintain visual acuity. The vestibule-spinal reflex (VSR) maintains posture and gait. The vestibulo-colic reflex (VCR) maintains head stability. When the brain receives all this information, it is able to determine what piece the body needs to keep it upright.
What are the Differences Between cVEMP and oVEMP?
We have to understand the difference between the cervical VEMP (cVEMP) and the ocular VEMP (oVEMP). The cVEMP tests saccule and inferior nerve. It is recorded from the sternocleidomastoid muscle (SCM). It is an inhibitory potential and an ipsilateral response. When a muscle is flexed, there is a split second within that flex where it releases. That provides the waveform or the response from the sound.
The oVEMP is primarily a utricle and superior nerve response. A little part of this oVEMP response comes from the saccule. This is an excitatory response that we record from the extraocular muscles. What generates that waveform is the person looking up; this a contralateral response. When we stimulate the right, we record the left and vice versa.
Setup for cVEMP
With regard to the patient’s setup for cVEMP, you need to locate the SCM and find the middle third of the muscle. It is important that you place the electrodes symmetrically and in the middle third of the muscle body. If the electrode is too high or too low, you’re not going to get good results. You’ll get smaller amplitudes and the uneven results left and right so you don’t want to have one higher than the other. Also notice that on the clavicular joint, that is where we are going to put the reference there.
You can either use a jumper and put it in the center, or you can use two separate leads and electrodes and put them on the left and right clavicular muscles and junction there. That is where the muscle joins into the collar bone. Remember, that muscle is quite large. You can travel that muscle down with your fingers and feel it all the way to where it inserts into the clavicular junction. I think it is easier to make channel one and channel two references with the jumper in the middle.
Obviously, all tests cannot be performed on everyone. We need to be aware of this for patient safety and for accuracy of results. With the cVEMP, any sort of conductive hearing loss, even as small as 5dB, can make that result disappear. It is important to perform the cVEMP after audiometry, immittance and acoustic reflex testing have been assessed.
Next, check with the patient about any cervical spine problems. Make sure that they can contract the SCM comfortably. Individuals who have had neck surgery or pain may not be able to contract that muscle enough in both directions. The same goes for those with tinnitus or sound sensitivity. As the stimulus used for VEMP is loud, be considerate about putting that stimulus into their ear.
Another challenge is obesity. Sometimes it is difficult to locate the SCM, although there are some strategies to try in order to make the muscle stand out. We will talk about those shortly.
Otometrics offers a differential electrode with two snaps (Figure 1). It provides you the symmetry of the two electrodes being equidistant from each other. We want to make sure that we snap the leads on before we place the electrodes. To get that muscle to “pop out” in some people, I tell them to turn the head to the side. In some people there is a decent contraction, but in others you may have to try to different technique. You may ask them to turn their head and point their chin down to the shoulder; that can increase that contraction. Another way is to have the patient lie supine and lift their head.
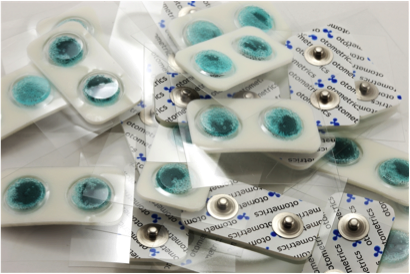
Figure 1. Otometrics differential electrode.
I mentioned putting the leads on the electrodes before placing them. I have seen where audiologists will scrub and stick the electrodes on. Then they have to try and snap that lead onto an electrode that sits atop a wobbly muscle. It becomes very difficult to do so and uncomfortable for the patient.
We want to instruct the patient of how to use the EMG monitor (Figure 2), which includes a visual cue. The green light means the setting is ideal. The red means the contraction is too high, and the blue means the contraction is not enough. This becomes a good coaching tool to help the patient get the correct contraction. Before starting the test, ask the patient to turn their neck so that they are able to see the monitor in action and get an idea of how this works.

Figure 2. EMG monitor.
Setup for oVEMP
The oVEMP patient set up does not require the use of the third channel or EMG monitor. The electrodes are placed just below the eyelids, so the active is the upper and the reference is the lower (Figure 3). Some studies that show that the chin should be used as a reference, and there is supporting information for both. It is your decision which to use.
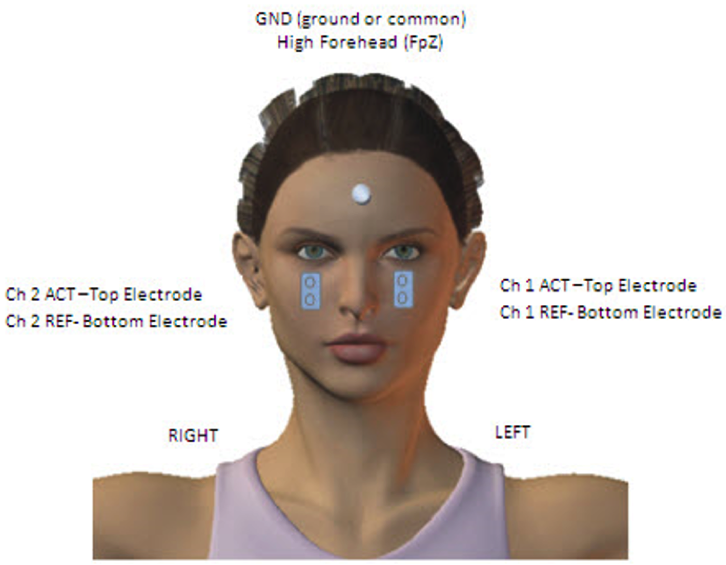
Figure 3. Electrode placement for oVEMP.
You can see how the differential electrodes with the two snaps can be useful in getting the electrodes lined up properly and equally below the eye. Tell the patient to look up so you do not get the eyelashes in the electrodes, and make sure you have enough room to place them properly. The same challenges that we account for with oVEMP are the same with cVEMP (conductive hearing loss, cervical spine problems, tinnitus and obesity), with the addition of checking for absence or damage to the eyes. If this is the case, we cannot make asymmetry comparisons.
Recording the cVEMP
The SCM is activated through a contraction, so turning the head or lifting the head up off the table will activate the contraction. The loud sound from the insert earphone stimulates the saccule, which in turn activates the inferior vestibular nerves. So how do we record this?
We use a high-level acoustic stimulus, at a rate five clicks per second. The saccular afferents have thresholds of 90 to 95dB SPL, so you will get better responses at higher intensities, but be cognizant of patient comfort. The response can be elicited by clicks or tone bursts; most research supports 500 Hz (Akin, Murnane & Proffitt, 2003; Janky & Shepard, 2009). Also pay attention to patient age because there is documentation that VEMP amplitudes decrease as we increase age. If it is absent in an older patient, consider using 1000Hz instead. The surface EMG is averaged to make sure we get an accurate reporting.
Figure 4 shows the Otometrics EP 200 parameter screen. The parameters are relatively universal. The red circled areas are where I would like you to take note. The amplifier gain is set to 5k. Compare that to the ABR, which is set up to 100k. Since we are recording a response from a muscle, it is much larger and easier to record. It does not require as much amplification.
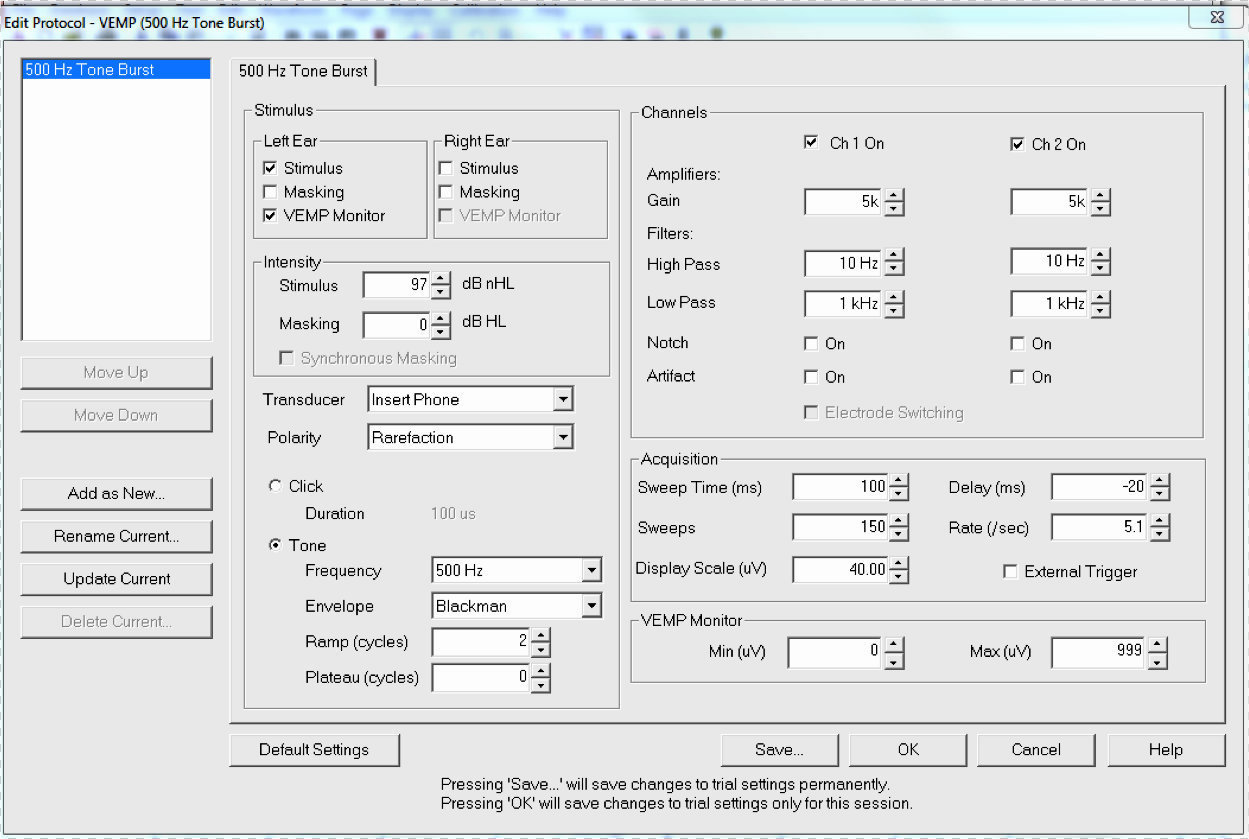
Figure 4. Otometrics EP200 parameters screen.
With regard to acquisition, this response comes very quickly. While we have the sweep number set to 150, you can stop sooner than that. You may see something clearly in 20 sweeps. The sweep time will vary somewhat. We have it set to 100ms with a 20ms pre-stimulus, so there is a bit of a delay so that you can see the onset if you prefer.
The display scale is in microvolts, and you can adjust that as you go. The VEMP monitor is on, and we leave the VEMP monitor wide open so that it will record everything. Initially we leave that monitor at 0 to 999, but there are instances where that might be changed, which we will discuss.
Figure 5 is a test screen where we are recording a left VEMP. Our subject has her head turned and we are actively stimulating. The patient is holding the EMG monitor to make sure the contraction of the muscle is ideal. The purple response is the VEMP, and in the measurement bar, you can see that 45 sweeps were accepted.
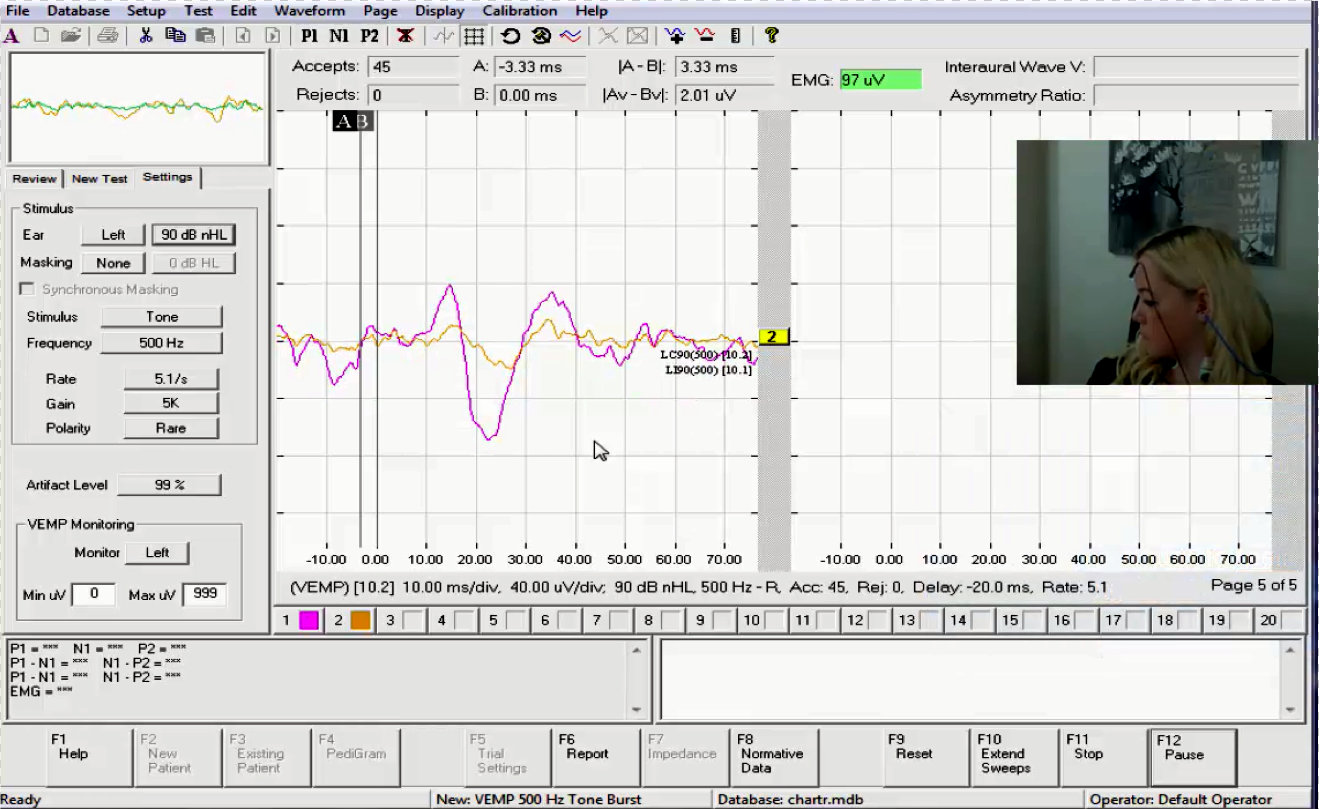
Figure 5. VEMP recording in the Otometrics EP 200. The purple response is the VEMP.
Once we have recorded the cVEMP with wide open settings, we are going to make some changes. We can always turn on the EMG monitor earlier and let the patient practice. In this case, blue means the contraction is under 50 microvolts (Figure 6). That value will be set based on the average of the first recording. We look at that number, and then we will change and go 20 or 25 above and below. We insert that number into the minimum and maximum fields.
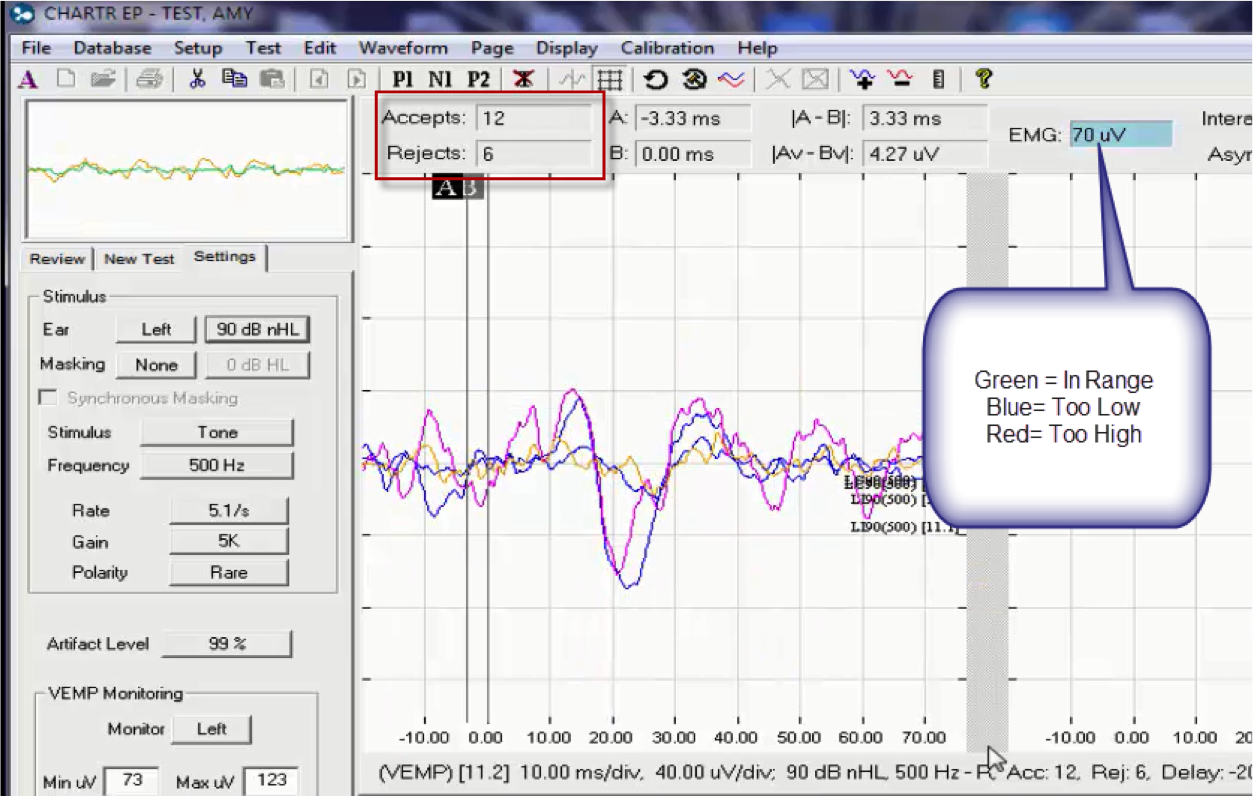
Figure 6. The VEMP recording screen, with emphasis on the EMG monitor.
If the response falls below the contraction setting (the blue indicator), the sweep gets rejected. If it is green, the acceptance will increase. This means that the subject’s contraction needs to be between 73 and 123 in this case, because her previous measurement average was 98.
There is a nice repeatability of two waveforms (Figure 6), so then we can proceed to the other side. You will use the same minimum and maximum settings for both sides; you do not have to re-measure the EMG with the settings wide open. The patient has been adequately instructed in how to make the contraction, and we have seen that they are successful in getting the EMG to the level they need.
Marking and Interpretation of the cVEMP
Once you have recorded on both sides, you will mark the P1 and N1. You may also choose to add the two runs from each side and use the one summed waveform to make the comparison; that is fine. The peak-and-trough is also known as P13 and N23, which is based on the milliseconds at which those responses typically occur. Use normative data to make your markings and interpretation.
Next, you will highlight a left and a right recording and select asymmetry ratio icon on the toolbar (Figure 7). There are two ratio. One takes into account the EMG and one does not. The asymmetry ratio says N23.50. That means this example has a 23% asymmetry ratio. This took into account the EMG contraction.
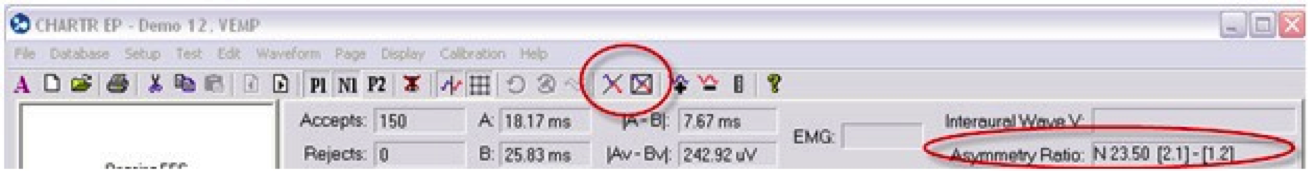
Figure 7. CHARTR EP toolbar, indicating the asymmetry icon (top) and the asymmetry ratio.
The practice of monitoring is of the utmost importance in this test. VEMPs are an amplitude measure. If we do not take into account the contraction by EMG, we cannot accurately analyze any asymmetry. If we do not correct for the EMG, we end up with a 51% asymmetry. In that case, we would tell the physician that this was abnormal and undergo further testing. However, because we used the EMG monitor and we took into account the EMG contraction, the asymmetry was only 14%. If you did not monitor of if you did it incorrectly, there is the likely chance that you would make your patient have further testing, which would be unnecessary.
Recording the oVEMP
To elicit the oVEMP, we record from the inferior oblique, activated through contraction by looking up. You may have your patient sitting or you can do it in the supine position. If sitting, you will ask them to stare straight ahead and then look up as high as they can, 25 or 30 degrees. Sometimes we mark a spot on the wall for easier visual targeting. Then we stimulate at the high intensity for five stimuli per second also. Again, this is predominantly a response from the utricle, superior nerve, with has some saccular fibers contributing.
We do not do EMG averaging with the oVEMP because both eyes should move symmetrically when they are asked to look up. In nearly all cases, the contraction will be the same.
The recording parameters for the oVEMP are shown in Figure 8. Notice that the VEMP monitor is turned off by unchecking the box. We have also increased the gain up to 100k because this is a tiny muscle compared to the SCM. We also lessened the sweep time to a 50 ms window. Keep in mind that you are in control of the parameters. If you only want a delay of 10 ms, you can modify that.
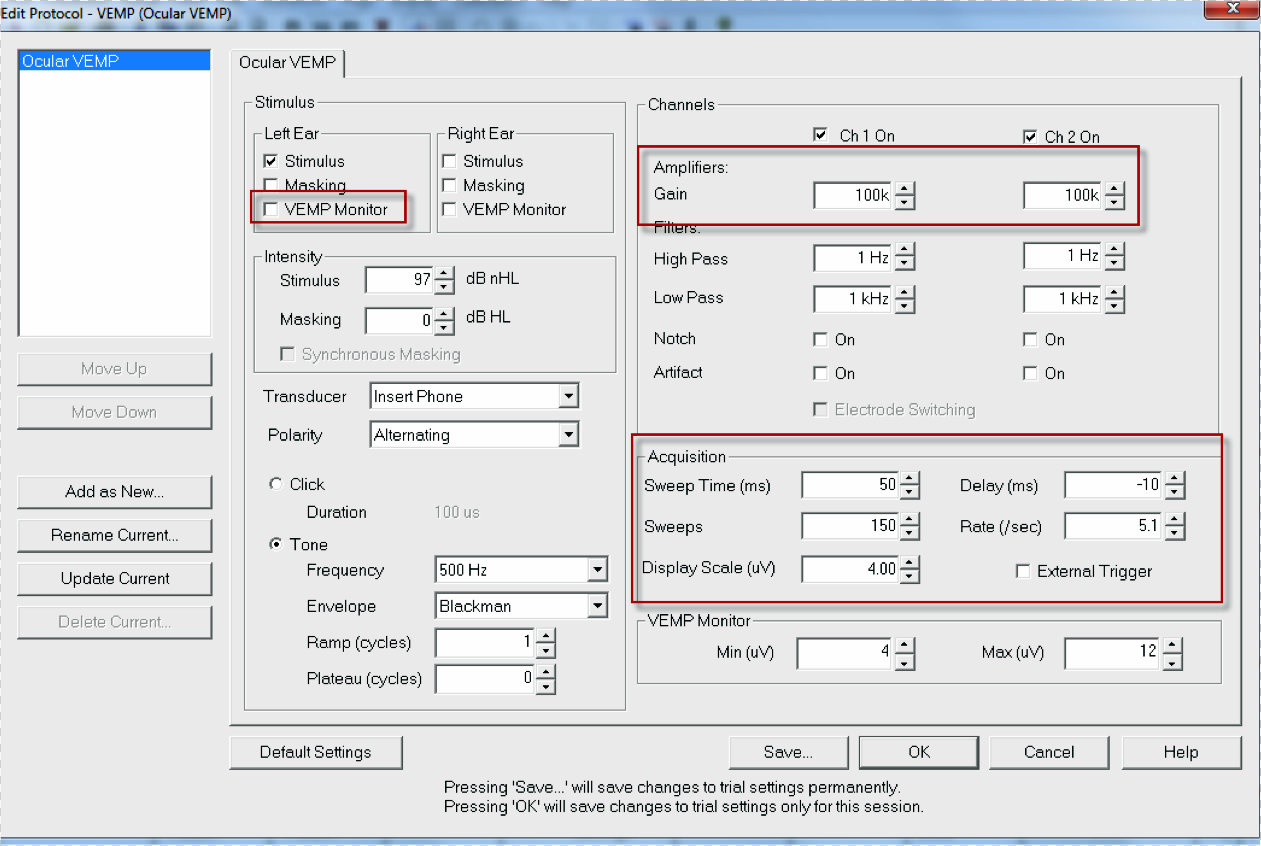
Figure 8. oVEMP testing parameters.
Marking and Interpretation of the oVEMP
When you record the oVEMP, it is a contralateral response. On the waveforms, you will see “LC” next to the run, indicating left contra (Figure 9). The N1 or N10 response should be seen around 10 ms. These responses are clear and repeatable; if you noticed, there were 200 sweeps accepted, which is quite high. You should be able to see this response in very few sweeps.
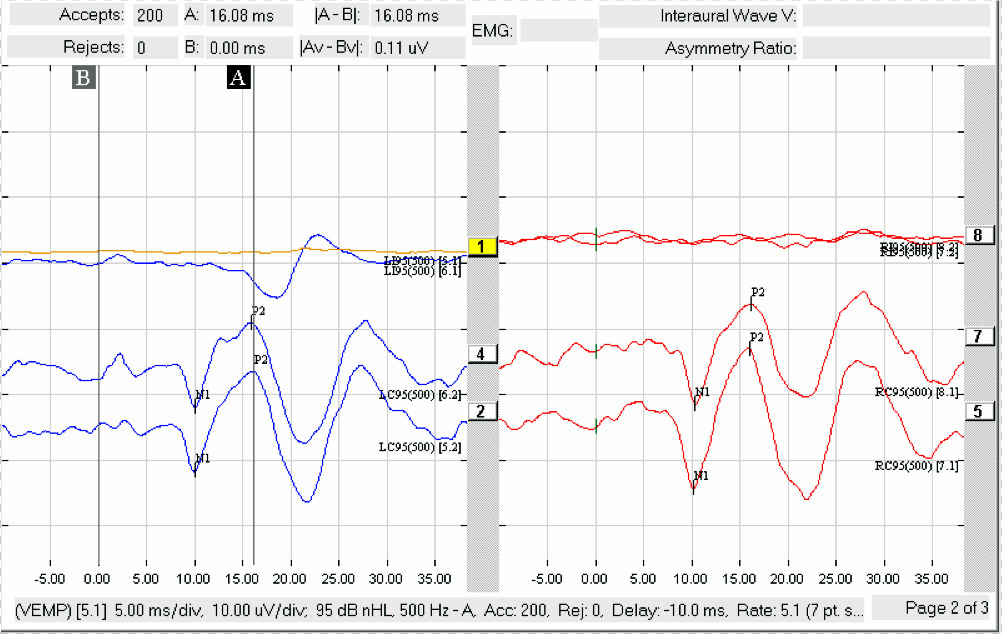
Figure 9. oVEMP recording showing left contralateral and right contralateral responses.
Quick Tips
Many normative papers exist with regard to American recordings if that is your preference. Kristen Janky et al. (2009), Erin Piker et al. (2011), and Owen Murnane et al. (2011) have all published normative data. Some of it is age-matched, and there is always more emerging. We are starting to see pediatric data coming out as well.
Testing guidelines have been published by the British Society of Audiology for audiologists in the United Kingdom, but they are put together step-by-step - you can access them here. International guidelines are also available online here, but unless you have access to the Clinical Neurophysiology Journal, you will likely only have access to the abstract.
Another quick tip is to know that the asymmetry ratio proposed in most papers proposes to be clinically significant is 35% to 40%. Many people run their own norms in their office, and I have seen this up to 45%, which was unique to their facility. I would say you need to be able to run some normal subjects comfortably before you can even think about running an patient with a disorder. That is important.
Latency delays are indicative of a central pathology, and a high asymmetry ratio and low thresholds are indicative of peripheral pathology. Those two points are good know by memory when seeing patient. cVEMPs decrease with age and are affected by the stimulus and frequency levels. If you are 20-years old and use 500 Hz at 90 dB to obtain a VEMP response, you likely will not get the same results with those parameters in someone who is 75 years old.
If the response of the cVEMP is not there, change the stimulus frequency. For cVEMP in children, consider that you will have shorter latencies and larger amplitudes. That should anatomically make sense to you.
Bone-Conducted VEMP
Another challenging discussion is bone-conducted VEMPs. You may read articles about the B&K Mini-Shaker, which is what is used in this setting. The mini-shaker is connected to an amplifier. The problem is that many systems do not have enough output to generate this response. We have to use an external device which will allow us to trigger the response, what can be connected to the CHARTR EP 200.
There is emerging data about the use of a triggered tendon hammer. The problem is that we have to make specific cables for this to work. The B&K mini-shaker is probably the more commonly used piece, but it is expensive. All we do is attach a small cap or use an acrylic post. So there are two ways, and neither is correct or incorrect. They will still generate a stimulus, which is presented at Fz on the head.
Diagnosis/Interpretation
In a healthy subject, we would expect all clinical tests to be normal. In a unilateral vestibular loss, all tests, including head turn and head impulse tests, will be abnormal. If a patient has superior vestibular neuritis, the oVEMP is abnormal and cVEMP would be normal. For patients with inferior vestibular neuritis patients, they should show abnormal results to cVEMP and head impulse test for the ipsilateral posterior canal.
When you add in head impulse testing, you are testing the whole balance system. Figure 10 is a quick guide that comes in handy when you are trying to discern the disorder based on your findings.
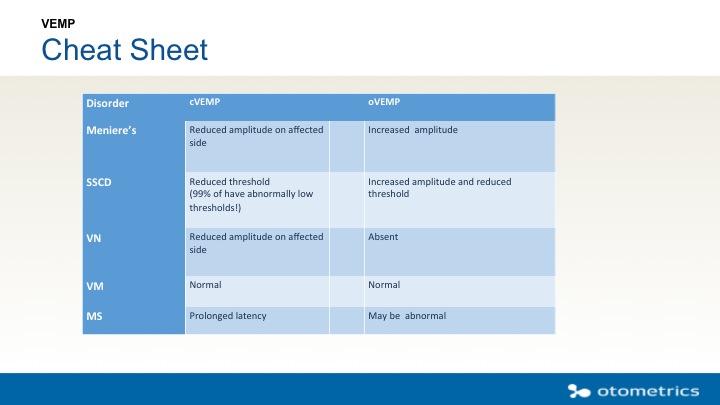
Figure 10. Quick guide for cVEMP and oVEMP findings, based on disorder.
The cVEMP will have reduced amplitude on the affected side of a Ménière’s patient and an increased amplitude in an oVEMP. For superior semicircular canal dehiscence (SSCD), we are going to do a threshold test. When you run a VEMP at the higher intensity, follow that run down to 70 dB. For vestibular neuritis, cVEMP will show reduced amplitude on the affected side, and the oVEMPs will be absent. For a vestibular migraine, results are likely normal for both cVEMP and oVEMP. Multiple sclerosis (MS) is a central disorder, so we will see prolonged latencies on the cVEMP, and the oVEMP may also be abnormal.
Limitations to Traditional Vestibular Testing
The video nystagmography (VNG) and rotational tests only assess the horizontal plane and the VOR. Adding in the VEMP gives us more information. In isolation, if the VNG is normal, there is no more information to give, which is disheartening to the patient because they have endured a terrible test with no answers.
Adding the VEMP assess the saccule, utricle, inferior and superior vestibular nerve; no other test assesses this. Adding the video head impulse test (vHIT) then gives us a complete test of the entire system.
We now have to learn what it means to re-rehabilitate the part of the system that is broken. Now that we have the ability to do VEMP in the United States, we have so much to offer our patients for a diagnosis. We have FDA approval both for the test and the EP 200 device, which means that you will get customer support and training from the manufacturer. This results in better patient care. The good thing about FDA approval is that, while there is currently no procedural code for VEMP specifically, we are eligible for one.
More Information
There are many other course on AudiologyOnline that you can search that relate to VEMP. I encourage you to peruse the literature often for new research on this topic. Google is a good mechanism for finding information that has been published. This continues to be an emerging technology for the end user. We can only make it better with the more research. Now with FDA approval, we expect to see those number grow because we do not have to obtain Institutional Review Board approval s to do these studies.
Questions and Answers
Why is the cVEMP response bigger than an ABR response?
The cVEMP is a recording from a large muscle as opposed to a tiny neural response inside the skull. It has to do with the size of this contraction in the muscles.
Is it true that bone-conduction is a more reliable stimulus transducer for oVEMP than cVEMP?
Yes, there is research to support that.
Is the nonspecific otolaryngology code being used, and is it getting reimbursed?
This varies by state, from what I understand. Each state and insurance companies have different acceptance requirements in their own policies. If you bill that nonspecific code, you can write a letter explaining why you did it and what you expected it to provide. I believe Otometrics has a template of a letter for you. One of the important things you can include in the letter is that that this an FDA-approved test. Prior to the acceptance of the VEMP, some states were billing the ABR code and receiving reimbursement. I cannot give you an absolute answer on that, but hopefully, we will be able to build a code specifically for VEMP.
Are there age-matched normative data in the system?
No, it is not in the system yet. There are only one or two papers published that are true age-matched norms. You want to have those on hand so that you can refer to them for your testing. At this point with data continuing to emerge, we want to see the consensus of normative data. We have not implemented VEMP normative data as we do not know whose to put in there yet, quite honestly.
We are about to start oVEMP in our clinic. Do you have any practical tips on how to set up the reference point for the patient to focus on?
There are two common ways to do that. If you are going to have your patient sitting, use a mark or sticker ahead on the wall at eye-level, and then you can measure up 30 degrees. You could probably do it with a laser measure, but lot of clinicians have them look up to where the ceiling and the wall meet and put another mark up there.
Then the other way is to lay down and put a mark on the ceiling where your eyes look comfortably. Then you (or a friend) will look back almost as far as you can and put another mark up there. When you hit collect, you will ask the patient to look back or up, depending on position. You will see the response appear fairly quickly.
I am confused about sweep time and sweeps. Can you clarify?
Sweeps is the number of pictures or snapshots that you will take of the recording. For the VEMP, this is maxed at a 150. It means that the recording will stop automatically when you have 150 accepted sweeps.
Sweep time is the time window. In an ABR, you may use at 10 or 15 or 20 ms window. In VEMP, we can use 50 ms. Again, you can modify that setting for how you like to see things.
A 50 ms window may be a 35 ms recording with a pre-stimulus of 15 ms. Sometimes people will run the VMEP with an 80 ms window. That is a bit excessive because the cVEMP response occurs back at around 10 ms. Use a window that makes sense for you and allows you to see the entire response.
References
Akin, F. W., Murnane, O. D., & Proffitt, T. M. (2003). The effects of click and tone-burst stimulus parameters on the vestibular evoked myogenic potential (VEMP). Journal of the American Academy of Audiology, 14(9), 500-509.
Janky, K. L., & Shepard, N. (2009) Vestibular-Evoked Myogenic Potential Testing: Normative Threshold Response Curves and Effects of Age. Journal of the American Academy of Audiology, (20)8, 514-522.
Murnane, O. D., Akin, F. W., Kelly, K. J., & Byrd, S. (2011). Effects of stimulus and recording parameters on the air conduction ocular vestibular evoked myogenic potential. Journal of the American Academy of Audiology, 22(7), 469-480. doi: 10.3766/jaaa.22.7.7.
Piker, E. G., Jacobson, G. P., McCaslin, D. L., & Hood, L. J. (2011). Normal characteristics of the ocular vestibular evoked myogenic potential. Journal of the American Academy of Audiology, 22(4), 222-230.
Citation
Craig, J. (2016, March). Vestibular Evoked Myogenic Potentials (VEMP): How do I get started? AudiologyOnline, Article 16713. Retrieved from https://www.audiologyonline.com

