Learning Outcomes
After this course, participants will be able to:
- After this course learners will be able to list the most common causes of bilateral vestibular system impairment.
- After this course learners will be able to explain the epidemiological aspects of bilateral peripheral vestibular system impairment.
- After this course learners will be able to describe the differential effect of mild cognitive impairment and Alzheimer's disease on semicircular canal and otolith end organ function.
- After this course learners will be able to explain the effect of profound peripheral vestibular system impairment on the hippocampus.
Gary Jacobson: In today’s journal club, we will review articles on the topic of bilateral vestibular hypofunction and failure. The agenda will be as follows: I’ll begin with some opening comments, Dr. Hatton will bring us up to date on epidemiology, I'll cover some recent information about the relationship between bilateral loss, dementia, and vestibular testing, and finally, Dr. McCaslin will review of a landmark paper from 2005 on the effect of bilateral vestibular impairment on cognitive function.
Introduction: Bilateral Vestibular Hypofunction & Failure
Bilateral vestibular hypofunction (BVH), which is a significant bilateral reduction in peripheral vestibular system function, or bilateral vestibular failure (BVF), which represents a bilateral complete loss of peripheral vestibular function, occurs in roughly 7% of outpatients seen in a dizziness clinic. The bilateral damage can affect either the end organs, the nerves, or both.
van de Berg and colleagues (2015) have described four characteristic presentations of these patients. One cohort complains of recurring vertigo spells occurring over years, and this eventually becomes bilateral hypofunction. A second group experiences a slow-progressing bilateral loss, and these patients often don't experience spells of vertigo. A third cohort experiences a rapidly-progressing bilateral loss, and these are the patients who sustain bilateral loss due to ototoxicity or autoimmune causes. The fourth group shows bilateral impairment in conjunction with neurological deficits like cerebellar ataxia.
Symptoms
According to van de Berg and colleagues (2015), common symptoms experienced by patients with bilateral hypofunction and bilateral failure include:
- oscillopsia
- imbalance
- visual vertigo
- cognitive impairments
- psychological or psychiatric impairments
- neurological impairments
- autonomic system impairments
The most common of these symptoms is oscillopsia. Oscillopsia is the symptom that indicates that the vestibulo-ocular reflex is severely or profoundly impaired. Patients complain of “bobbling” of images in front of them as they're walking toward them. If there isn't any peripheral input to the vestibulo-ocular reflex, then the eyes fail to move out of phase with the head, and during ambulation, this makes the outside world jiggle as though it was filmed through a handheld movie camera.
Postural unsteadiness is a second complaint, and this occurs when there is no electrical output from the end organs to the central vestibular pathways that control the vestibulo-spinal tracts. As a result, the brain can't generate motor commands to keep patients steady when they're standing still or walking. When the vestibular system is profoundly impaired, the brain automatically recognizes this, and reorders the hierarchy of the senses that it uses for orientation. The somatic senses, as we know, predominate for standing balance. However, in the presence of bilateral vestibular failure, during ambulation, the brain prioritizes vision as its primary source of orientation information. This means that if the scene in front of the patient is moving, since orientation is being supplied by the visual sense, the patient will feel like they're moving as well. This phenomenon is referred to as visual vertigo.
Bilateral vestibular failure can produce cognitive deficits, and Dr. McCaslin will be addressing those symptoms later in the presentation.
Patients with bilateral peripheral vestibular system impairment may complain of chronic anxiety and depression.
As I mentioned before, patients with bilateral vestibular failure may have concomitant central nervous system disease, including spinocerebellar ataxia, or a new clinical entity that is referred to as CANVAS. CANVAS is an acronym for: cerebellar ataxia neuropathy, vestibular areflexia syndrome. The proportion of patients with bilateral vestibular impairment and CNS disease can be as high as 39%.
Lastly, patients with bilateral peripheral vestibular failure may also have a failure of the vestibulo-sympathetic reflex, and this is a symptom that makes it possible for your brain to automatically adjust your blood pressure when you change position. Bilateral vestibular failure can produce orthostatic hypotension.
Self-report Dizziness Handicap in Patients with BVF
A number of years ago, our group at Henry Ford Hospital examined the impact of bilateral vestibular impairment on self-reported dizziness handicap (Jacobson & Calder, 2000). We measured self-reported dizziness handicap using the Dizziness Handicap Inventory (DHI; Jacobson & Newman, 1990). van de Berg and colleagues (2015) found that approximately 43% of patients experience a moderate self-report dizziness handicap and 41% of patients experience severe self-report dizziness handicap on the DHI. Our experience was that regardless of whether patients had bilateral peripheral vestibular impairment or failure, they reported severe self-reported dizziness handicap. However, the magnitude of the severe handicap was greater for patients with bilateral failure. Patients with bilateral impairment showed an average DHI total score of 50 points out of 100. Those patients with bilateral failure showed an average total DHI score of 71 points out of 100.
Quantitative Assessment of Patients with Bilateral Failure: Tools, Frequency Spectrum, Results
The studies examining bilateral vestibular impairment and failure have employed a number of test techniques. These measures were era dependent. That is, in the 1960's, patients with absent ice-water caloric responses would have been diagnosed with bilateral profound end organ damage, even though we realized that the caloric stimulus emulates the end organ at its lowest and non-physiological frequency as 0.003 Hz. In the 1970's, rotary chairs became commercially available which enable us to measure the function of the vestibular system for frequencies from .01 Hz out to about .64 Hz. VEMPs (vestibular evoked myogenic potentials) were discovered in the 1990's and early 2000's, which made it possible to measure the function of the otolith end organs. Most recently, with the addition of video head impulse testing (vHIT), it's possible for clinicians to measure the function of the vestibular system over its entire frequency spectrum, from .003 Hz to 6 Hz. This is useful because we now know that a patient with absent caloric responses, which again, mimics a low-frequency stimulus, may actually produce normal responses at higher frequencies in the rotational test. The auditory analogy would be the patient who has a precipitous high-frequency hearing loss with normal residual hearing in the low frequencies.
Figure 1 shows expected responses to various vestibular tests for a patient with bilateral failure.
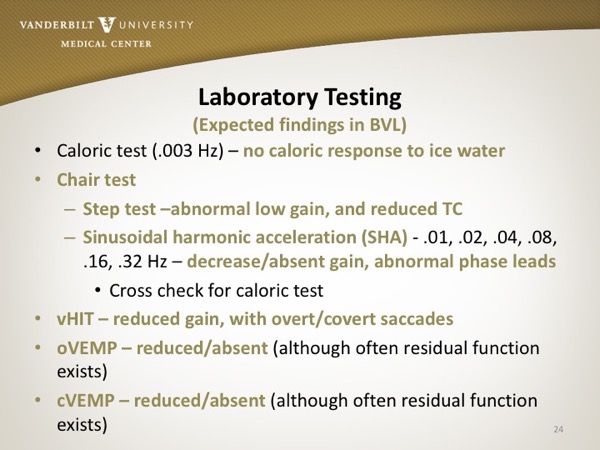
Figure 1. Laboratory testing - expected findings in bilateral vestibular failure.
These are the most common causes of bilateral peripheral vestibular system impairment and failure:
- Ototoxicity
- Idiopathic (including autoimmune, and genetic)
- Meniere’s Syndrome (bilateral)
- Meningitis
- Infectious labyrinthitis (bacterial, viral, fungal)
- NF2
- Bilateral vascular occlusion
- Cogan syndrome: (autoimmune d.) rare rheumatic disorder characterized by recurrent inflammation of the cornea and fever, fatigue, weight loss, episodes of dizziness and hearing loss
- Tumors of the temporal bone
- Otosclerosis
- Head injury
- Radiation therapy
- Aging
The top two most frequent causes are ototoxicity and idiopathic origins.
Kelsey Hatton: Lucieer and colleagues (2016) looked at potential etiologies for bilateral vestibular hypofunction, which is nice transition to discuss prevalence. The found approximately 94% of bilateral hypofunction in the general population comes from idiopathic causes, metabolic or ototoxic causes, infectious diseases, autoimmune disorders, and Meniere's disease. Although Meniere’s disease is on the list of suspected etiologies, it is not as common of a contributing factor in the general population. In a specialty clinic, you might see more Meniere’s disease.
Prevalence and Incidence of BVH
Because the etiologies are varied and the cause of bilateral vestibular hypofunction are not always clear, defining the prevalence and incidence in the population is difficult. In the literature, there is some type of functional testing done in a clinic or a laboratory that identifies the impairment; generally the reference is just to the status of the lateral semicircular canals and associated nerve segments. Most studies in the past, as Dr. Jacobson pointed out, have used VNG. While we've added other components to the vestibular exam, there's not a big body of literature looking at bilateral hypofunction of all the end organs versus just the semicircular canals. So keep in mind that much of the literature is sticking to the definition of BVH in terms of the lateral semicircular canals.
As Dr. Jacobson discussed, BVH leads to deficits in vestibulo-ocular or vestibulo-spinal reflexes, altering the ability to maintain stable gaze and posture. The classic symptoms are oscillopsia, chronic disequilibrium and postural instability.
The problem with some of these symptoms is that the names and terminology are not familiar to most patients. If you interview a patient or conduct a case history, people can describe their symptoms but they will not typically use the specific names or terminology.
To estimate how many people are affected by a certain disorder in a large population, a survey is an effective way to do that.
But how do you put questions together for the symptoms of BVH for the general population, where balance experts will not be conducting the interviews?
Estimates gathered through specialty balance clinics may not provide a fair representation of bilateral vestibular hypofunction among the general population due to economic and health barriers. In other words, If we look at the prevalence of BVH in a dizziness clinic, we are biasing the prevalence numbers and cannot generalize those numbers to the general population.
Prevalence in the General Population - Survey
Ward and colleagues (2013) looked at the prevalence of BVH in the general population. They established the validity of questions that they might use in a survey to identify bilateral vestibular hypofunction.
They utilized data from a large national health survey to identify patients with BVH, and added their validated question regarding BVH.
They had the benefit of joining a survey that had many other variables that they could look at for correlations with BVH. The goal of this paper was to estimate the prevalence of BVH in the American population.
How do you get at vestibular hypofunction from a pen-and-paper standpoint? They started with patients that had clinical examinations that had established BVH, and had them fill out their questionnaire.
There were 12 patients that had gone through testing and had documented bilateral vestibular hypofunction as determined by ice calorics testing where responses were less than 5 degrees per second in total response from right and left ear. Five of the 12 patients had ototoxic causes, one had Meniere's disease, one had head and neck trauma, and five had unknown causes for their bilateral vestibular hypofunction.
They also created a group of 12 patients that had unilateral vestibular hypofunction (UVH), but they required this group to have more tightly defined causes and to have had UVH for more than one year. They wanted to make sure that these patients didn’t have some type of fluctuating disorder. For the UVH group, the ice caloric had to be less than 5 degrees on the impaired side. Everyone in this group had unilateral Meniere's disease and had already undergone intra-tympanic gentamicin injections.
They compared the results from these two groups to a group of 13 survey respondents with no inner ear pathology or reported dizziness.
The questions at the beginning of the questionnaire were more general. They included questions asking if the respondent had “dizziness or balance problems”, or reported feeling off balance or unsteady. Then, the questions became more specific, asking if the respondent had difficulty walking in the dark or on an uneven surface, experienced blurry or fuzzy vision with head movements, or drifted to the side when trying to walk straight. Finally, it asked whether the problem would be defined as at least a “big problem”, and if the duration of symptoms was at least 1 year.
The general questions at the top of the survey don’t really separate out the bilateral versus unilateral vestibular hypofunction respondents. Whether the respondent would define the problem being defined as a “big” problem differentiated the people with BVH from those with UVH. Also, a long duration of symptoms also seemed to separate out the bilateral group.
Both groups with hypofunction oftentimes reported unsteadiness, difficulty walking in the dark, and drifting side to side. Of the 24 people with vestibular hypofunction (12 people with BVH and 12 with UVH), 92% reported “feeling off balance or unsteady”; 67% reported “having difficulty walking in the dark”; 58% reported “drifting side to side when trying to walk straight”, and 42% reported “difficulty walking on uneven ground” and “blurred vision during head movements”. These questions, while they're very good at getting at symptoms of unsteadiness and dizziness, they're not as specific to a bilateral failure.
The 12 people with documented BVH were significantly more likely to rate problems as “big” or “very big” as compared to those with UVH or the controls.
NHIS Survey with Dizziness and Balance Supplement
The investigators then took the questions that they had used in the survey, and created a supplement that would be sent along with the National Health Interview Survey (NHIS). The NHIS is given annually by the U.S. Census Bureau and in 2008, the dizziness and balance supplement was included with it. A total of 74,236 respondents completed the NHIS in 2008, and 21,781 completed the supplement about dizziness and balance.
It’s important to note that there is no follow-up or contact with subjects after they've responded to the survey. The questions have to be as specific as possible as you only get one chance to ask them.
Out of the 21,781 people that completed the dizziness and balance supplement, 3,400 reported at least one of the dizziness questions being positive. They wanted to separate out those with BVH so they required positive answers for the following: blurring of vision with head movement, off-balance or unsteady, drift when trying to walk straight, difficulty walking in the dark, or difficulty walking on uneven ground/surfaces.
Dizziness also had to be rated as at least a “big” problem, with duration of dizziness more than 1 year.
They also wanted to try an exclude anyone who may have a sudden-onset impairment that is not bilateral vestibular hypofunction. They were aiming more for the slow-progressive group that Dr. Jacobson outlined earlier, so they only included those who responded negatively for: spinal injury, stroke, movement disorders, muscular dystrophy, multiple sclerosis, age-related eye diseases, and diabetic retinopathy.
Functional limitations. They also included questions about functional limitations. If a respondent indicated that it was very difficult or they could not perform an activity, then that activity would be counted as one functional limitation. There were nine activities of daily living questions.
Social limitations. They included three questions about social limitations using the same qualifications. The limitation only was counted as positive if the respondent reported that it was “very difficult” or that they “could not perform” the activities listed.
Equipment needs. The survey looked at equipment needs with the following question: Do you have any health problem that requires you to use special equipment such as a cane/wheelchair/special bed/special telephone?
Falls. We know that people that have vestibular hypofunction are at higher risk for falling. They asked if respondents had had any falls, whether the fall was within one to five years, and whether there were any injuries sustained secondary to the fall.
Additional queries. Other queries were included to obtain more detail about the symptoms and what was happening with their medications and the other comorbidities, and any problems in their work or education attendance. These queries included: Dizziness characterization, severity, duration, frequency, mitigating/provoking factors, associated symptoms of dizziness, use of balance aids, physical problems, psychological problems, health care, pharmacological management, other diagnoses, treatments offered, treatment outcomes, and absenteeism.
Related Variables for NHIS BVH
Of the 21,781 respondents that filled out the dizziness supplement, 12 of them fulfilled all the criteria to be considered bilateral vestibular hypofunction patients. These people reported a “big” impact with symptoms of blurring of vision, unsteadiness, drifting when walking, walking difficulties in the dark or on uneven surfaces for more than 12 months, and these symptoms were unrelated to other CNS, vision, or muscular issues.
Sex, Ethnicity, Age, Diagnoses. Females were more likely to have bilateral vestibular hypofunction. In terms of race/ethnicity, those of Hispanic ethnicity were more likely to have BVH. Older respondents as well as those with diabetes or depression more often fulfilled the requirements for this survey of bilateral vestibular hypofunction.
Impairments. People with BVH were more likely to experience functional, social, and physical impairments. More than half of them (58%) were limited in 4 or more of the 9 activities of daily living. They are having difficulty doing what they need to do to get around. Thirty-nine percent limited some of their social activities because of their symptoms. In terms of physical impairments, many of these patients fall; 67% reported a fall within the last year, with one out of four of them sustaining an injury from the fall. When we see patients for a VNG or full battery of testing, it’s important to discuss falls, prevention of falls, and safety in regard to falls. BVH respondents have a 9.9-fold increase of falling compared to those just reporting dizziness, and a 31-fold increase in nationwide average falls risk.
In addition, BVH patients had motion intolerance, or limited/changed driving habits; 55% missed work or school and 75% were unemployed. If you can't tolerate being in the vehicle that gets you to work, it's hard to go to work.
Treatments. Of the 12 BVH survey respondents, 9 had sought and completed some form of treatment. Fifty-six percent had completed physical therapy; 33% altered their diet; and 22% had either tried head rolling maneuvers, massage therapy, or herbal remedies. Eleven percent had undergone head/neck surgery, chiropractic remedy, or tried wearable magnets. Of those who had completed treatment, 75% saw no change or had a worsening of symptoms.
It's very difficult to complete vestibular rehabilitative therapy when you aren't really functioning with much vestibular information. You have to work on substitution exercises and other things to allow you to get around. The patients reported seeing five or more health care professionals on average, and they really didn't feel that health care professionals addressed their dizziness very well.
Goal: Prevalence Estimation
With all of the information from the survey, the goal was to try to estimate the prevalence of BVH in the U.S. population. The finding was that of American civilian adults in 2008, 14% were dizzy over a 12-month period.
There were 12 of the total respondents with BVH based on their history; if you extrapolate that to the general population, it is an estimate of 28 for every 100,000 US adults. Based on 2008 population numbers, this would represent 64,046 US adults with BVH, and 1.8 million adults worldwide.
While these numbers may already seem high, the authors indicated that they used very restrictive qualifications. They stated that if they expanded the qualifications, the prevalence number could be higher. With more lax qualifications, they estimated the prevalence to be 85 out of 100,000 US adults, or 193,369 US adults in total.
It’s interesting to review the process they used in getting to the prevalence of BVH using a pen and paper format, and we hope to see them gather more data using the NHIS at some point in the future.
Vestibular Impairment in Dementia (Harun, Oh, Bigelow, Studenski, & Agrawal, 2016)
Gary Jacobson: The authors of this article represent both Johns Hopkins School of Medicine and the National Institutes of Health (NIH).
In this article, the investigators begin by discussing the most common form of dementia, which is Alzheimer's disease. It was estimated that there would be about 5.1 million cases of Alzheimer's in 2015. Further, there have been studies conducted showing that bilateral loss of peripheral vestibular system function is associated with cognitive impairment for both animals and humans. The greatest impairments involve visuo-spatial skills, including spatial memory and spatial navigation. These are individuals who, on one end of the spectrum, have difficulty finding their car in a large mall parking lot, which is something that happens to all of us from time to time. At the other end of the spectrum, these individuals get lost even in their home environment. The investigators further comment that wandering off is a common symptom of Alzheimer's Disease.
The investigators then turn their attention to mild cognitive impairment, or MCI. The prevalence of MCI increases with age, and patients with MCI have difficulty with some cognitive tasks, although their day-to-day function is intact. Adding a vestibular impairment, though, can complicate dementia by reducing a patient's awareness of their surroundings, which of course places them at risk for falling. We know from previous investigations that patients with Alzheimer's have poorer postural control compared to normal elderly. Additionally, cVEMP abnormalities have been reported to occur significantly more often in patients with cognitive impairments.
It was the investigators' objective to thoroughly assess vestibular function in well-diagnosed patients with both Alzheimer's and MCI. It was the investigators' hypothesis that patients with cognitive impairment would have poorer vestibular function compared to age-matched controls. Further, subjects with more severe cognitive impairment would demonstrate a larger amount of vestibular impairment.
Methods
Subjects were drawn from the Johns Hopkins Memory and Alzheimer's Treatment Center; there were 15 patients with MCI, and 32 patients with Alzheimer's. They were 55 years and older, with an MMSE (Mini–Mental State Examination) of at least 11 points, as 11 points was felt to be the threshold to be able to complete tasks required to generate VEMP and vHIT data.
It’s noteworthy that the mean age of our clinical dizziness population (patients that we see for routine balance function testing), is 57 years and the mean age of patients in our falls clinic, is 76 years of age, which is close to the mean age for this study's subjects.
Subjects were not enrolled if they had a history of dizziness or vertigo, if they were unable to carry out simple commands, if they were blind, or if they had poor neck range of motion or cervical spine instability. Control data was drawn from the Baltimore Longitudinal Study on Aging.
The cVEMP was recorded in response to 500 Hz tone bursts using conventional stimulating and recording techniques. The cVEMP was normalized as a function of the magnitude of the tonic EMG activity from which the response was extracted, and data recorded from the better ear was used for the analysis.
The oVEMP was recorded in response to mechanical stimulation, with the patient supine, and with the head elevated 30 degrees. The active electrodes were placed on the cheek 3mm below the eye; the reference electrode was placed 2cm inferior to the first electrode; and the ground electrode was placed on the manubrium of the sternum. The subjects averted their eyes 20 degrees during data collection, and head taps were delivered from a reflex hammer at midline at the hairline (approximately at Fpz). The oVEMP amplitude for the better ear was used for the analysis.
The vHIT was conducted in the plane of the left and right horizontal semicircular canals. To accomplish this, patient's head was pitched downward 30 degrees to place the canals in the plane of stimulation. Subjects gazed at a target that was placed 1.5 meters at central gaze. The head was moved, 5-15 degrees unpredictably at velocities between 150 and 250 degrees per second. Ten samples were collected in each direction, and abnormal function was a VOR gain that was 80% or less.
Results
The study sample was a sample of 47 patients and 94 controls. Not surprisingly, the Mini-Mental Status Examination score was 28.6 points for controls, but was 25.7 points for patients with MCI, and 19.7 points for patients with Alzheimer's disease.
The primary findings showed that 50% of patients with Alzheimer's and 25% of controls showed bilaterally absent cVEMPS. They also showed smaller cVEMP and oVEMP amplitudes compared to controls. There were no significant differences between the MCI group and controls on any of the vestibular function tests.
Fifty-percent of the patients with Alzheimer's disease show bilaterally absent cVEMPs compared to 25% of controls with absent cVEMPs. Further, the patients with Alzheimer's disease showed significantly smaller cVEMP and oVEMP amplitudes compared to controls. These differences did not occur for the patients with MCI.
Subjects with bilaterally absent cVEMPs had a 3-fold increased odds of having Alzheimer's disease. Subjects with larger oVEMP amplitudes had a 1-fold decreased odds of having Alzheimer's disease. So, the bigger the amplitude of the oVEMP, the less likely patients were to have that diagnosis. For vHIT testing, vestibulo-ocular reflex (VOR) gain did not significantly differ by cognitive impairment category, including Alzheimer's. Interestingly, the gain of the VOR did not help differentiate the two patient groups. The VOR was measured with a vHIT test. This means that measures that differed between the patient groups were only those that quantified the function of the otolith end organs.
Discussion
In their discussion, the authors reiterated that there were a significantly higher proportion of demented patients who demonstrated impairments affecting the saccule and the utricle, compared to normal controls and patients with MCI. It is known that the vestibular system sends projections to cortical areas that are involved with memory and spatial orientation. These areas include the hippocampus. Stimulation of the vestibular system in animals results in increased firing of hippocampal neurons. Also, animals with vestibular lesions perform poorly on spatial navigation tasks. Atrophy of the hippocampus is a hallmark of Alzheimer's. Damage to the peripheral vestibular system and a loss of connections between the vestibular system and the hippocampus may explain the connection between bilateral vestibular impairment and dementia.
Previously, Leandri and colleagues (2009) reported a progressive increase in anterior-posterior sway for normal controls, in patients with MCI, and patients with Alzheimer's. There was a decrement moving from normal to the most abnormal patients. Birdane and colleagues (2012) reported that patients with any degree of cognitive impairment showed lower mean cVEMP amplitudes.
Again, the investigators failed to observe an association between measures of the VOR through the vHIT and cognitive function. The authors reported that neurons in the vestibular nucleus involved with the VOR, unlike other neurons, do not ascend to the thalamus and cortex.
Further, activation of the saccule produces activation of the posterior insular cortex, inferior parietal cortex, intraparietal sulcus, and the temporoparietal junction. All of these areas are involved with cognitive processing. Disruption of the peripheral vestibular projections to the cortex may underlie the association between cognition and otolith function.
The summary statement from the authors is as follows:
“Our work confirms and extends emerging evidence of an association between vestibular loss and cognitive decline. Further investigation is needed to determine the causal direction for the link between peripheral vestibular loss and cognitive impairment. Identification of a possible modifiable risk factor such as vestibular loss for cognitive impairment could lead to interventions to help slow the progression of dementia and reduce the risks of postural instability and falls in this already vulnerable population.”
Vestibular Loss Causes Hippocampal Atrophy and Impaired Spatial Memory in Humans (Brandt et al., 2005)
Devin McCaslin: I’m going to discuss an article that follows from the previous articles. We know how many people have bilateral weakness, we know what causes vestibular weakness, and we know the common symptoms; this article discusses more subtle effects of bilateral vestibular weakness. These include effects on spatial processing and even into some degree, memory.
Background
There's no question that the hippocampus is key in memory processing - encoding memories, consolidating, and retrieving memories. What's been a hot topic recently and since this seminal that we're discussing today is its effect on spatial memory. The groups that believe that the hippocampus is key in spatial navigation also believe that input from the vestibular system is important. They feel the hippocampus plays a key role in spatial navigation. Early animal work has shown that if you disconnect or disable the vestibular system, you effectively change the firing of specific cells in the hippocampus. Electrophysiological studies from the 1990s (O’Mara, Rolls, Berthoz, & Kesner, 1994; Gavrilov, Weiner, & Berthoz, 1995) showed that vestibular stimulation could modulate the activity of ‘place cells’ in the hippocampus.
The word hippocampus comes from the word 'seahorse' as it is similarly shaped. The hippocampus is an elegant system set up to do all sorts of spatial processing. Hippocampal and parahippocampal cortices create cognitive maps, or neural representations of the environment. Construction of these maps are based on different types of cells such as place cells, border cells, head direction cells and grid cells that are found in the hippocampal formation and parahippocampus.
Reports have suggested that spatial learning deficits in animals (such as poor navigation) after vestibular lesions are linked to changes in neural wiring critical for navigation and place learning. Stackman and Herbert (2002) showed that location-related firing of ‘place cells’ in the hippocampus was abolished in rats after bilateral labyrinthectomy.
Purpose
This investigation sought to answer two questions: Can MRI volumetry show morphological changes in the hippocampus of bilateral vestibular loss (BVL) patients?, and, Are the BVL-related deficits in spatial memory and navigation selective or associated with general memory deficits?
In other words, could they tie the MRI data to actual behavior in people? While this has been shown in animals, I think this is one of the first reports showing it in humans.
Methods
The subjects consisted of 10 people - four women and six men - all with bilateral vestibular lesions. They were age-matched with controls who had no known neurological history.
All experimental patients had undergone a bilateral vestibular nerve section 5–10 years before the test and subsequently had a complete BVL. That is a very specific subset of patients, to truly confirm that the experimental subjects did not have any peripheral input.
T2-weighted images were obtained in the oblique coronal orientation perpendicular to the long axis of the hippocampus.
With the correlating MRI data, they assessed intelligence, memory and attentional concentration, as well as spatial learning and spatial memory. Spatial memory is responsible for recording information about one’s environment and its spatial orientation. It is required to navigate around a familiar city, just as a rat’s spatial memory is needed to learn the location of food at the end of a maze. Spatial memory can be short-term or long-term.
Assessing spatial memory. How do we assess spatial memory? The Morris water navigation task is a classic test used for studying spatial learning and spatial memory in rats. In this test, there is a big, round pool of water with spatial cues along the walls so that the animal can know where it is within the big round tub. The rat is placed on a platform in the pool. In some trials the platform is above the water, and in other trials the platform is below the water so that it is not visible. The rat is then dropped into the pool. To avoid drowning, the rat must find its way back to the platform using spatial cues; when the platform is below the water the animal can’t use its vision to find it. What we find on this task is that control animals take a direct path back to the platform, while those with bilateral vestibular dysfunction search in many different directions.
Obviously, you can’t perform this task on humans so we have to devise other means to study spatial learning and spatial memory.
One way to study these issues in humans is with a dark room with small LEDs on the walls. The subject has to find a target on the end of a stick by using the LED cues.
Virtual methods of the virtual Morris water maze test (vMWT) have been developed to study spatial learning and spatial memory in humans. This vMWT is done in a virtual environment on a screen, with the subject using a joystick to move an avatar around the screen. This allows us to study humans and simulate, with some degree of accuracy, the Morris water task that's used in animals.
In the vMWT, the subject looks at a TV screen at watches their avatar go into the water. There are spatial cues on the walls onscreen. Then, they sink the platform, and the subject has to drive the avatar around to find the platform.
This video provides a good explanation of the Morris task and the vMWT.
These investigators used the vMWT and their study consisted of three phases:
Phase I. Participants completed five hidden platform training blocks, each consisting of four trials.
Phase II consisted of a single 45 second probe trial during which the platform was removed from the environment.
Phase III. This condition provided a control task that did not require spatial processing and would be intact in individuals with spatial navigation impairment.
MRI Volumetry Results
MRI volumetry revealed a 16.91% decrease in the total hippocampus volume in the BVL patients relative to the controls.
While there was a statistical difference between the patients and the controls, there was not a significant difference in men versus women for hippocampal measures with whole brain volume. This is sort of a pilot study with a small number of subjects (i.e., only four female patients), and the data indicates that BVL may have had a larger impact on hippocampal volume in female experimental patients. So, if you did a power analysis to find out how many more you had to run, and tested a larger number of subjects, you may end up finding significance there.
Spatial Memory Results
This study found that BVL patients took more time and longer paths to navigate to the platform as compared to controls.
Discussion
This study supports the concept that acquired chronic loss of vestibular function can result in hippocampal atrophy. You have to use caution when generalizing the results as this study used a small number of subjects, but I think we will see this when studies are done with larger numbers of subjects and as imaging technology continues to get better.
The pattern of means for the probe trial measures in the virtual Morris water test closely matched the pattern of hippocampal volume observed in the patient and control groups. So, the smaller the hippocampus volume, the poorer the subjects did.
This study further suggests that vestibular and visual cues are critical for spatial navigation. A continuous accurate updating of the location and motion of the individual within a 3-dimensional environment requires input from both senses for navigation. You may have normal vision, but you also need input from the vestibular system in order to help find that target, at least according to this study.
This study, showing a link between bilateral vestibular loss in patients with bilateral hippocampal atrophy, suggests that the hippocampus plays a key role in spatial aspects of memory processing for navigation. I mentioned earlier that there is still some debate about the role of the hippocampus in spatial navigation.
This study also demonstrated for the first time in humans that spatial navigation is dependent on preserved vestibular function, even when subjects are stationary.
In closing, I’ll leave you with a few things to consider based on these findings. We know there is vestibular compensation. Therefore, if you lose both end organs, you will have a large drop in the vestibular nuclei spontaneous activity, and it will eventually return. There seems to be something key about head movement, or modulating the activity at the vestibular nuclei coming from the peripheral system, that has a key role in keeping the hippocampus from atrophying. We don't know if it is due to changes in neurocellular architecture, or related to cell death; we don’t know why it's shrinking when you have a bilateral vestibular loss. We’ll get more clarity in the future as imaging continues to improve, as more animal studies are conducted, and as more studies with humans are done using larger numbers of subjects.
Questions and Answers
Does bilateral vestibular hypofunction interfere with visuo-spatial orientation even with the eyes open?
Jacobson: Yes. It’s clear that the vestibular system in some way provides additional information about the location of things in the environment. Vision and the vestibular system work together to create “maps” of where things are located in your environment. That is the concept of these place cells; if you damage or destroy the peripheral vestibular system, then you basically ruin the map that the person has created through experience that tells that person where things are located in the environment. Devin, do you want to add anything?
McCaslin: Exactly. What they’re arguing is that it’s a coordination between visual components, vestibular components, and I would bet there are some somatosensory components that play a role as well. They are saying that if you lose one of the sensory systems, it disrupts the input.
Jacobson: This data is interesting, and this article has been frequently referenced by others looking at the effect of bilateral loss of vestibular function and its cognitive impact. It has never been replicated. It leads to all sorts of questions like what you would find in children or babies born with non-functioning vestibular systems, or in people who have lost function. What happens if you implant a vestibular prosthesis? Does that change the hippocampus, or the size of the hippocampus?
Have you, have any of you worked with patients who have had a vestibular implant, and if so, what are your thoughts?
Jacobson: We not doing vestibular implants at our clinic so I do not have experience with them.
McCaslin: There are very few people in the US who have actually had a vestibular implant and I have not had experience with them either. In the next five years or so I expect the number of vestibular implants will increase quite a bit.
References
Birdane, L., Incesulu, A., Gurbuz, M.K., & Ozbabalik, D. (2012). Sacculocollic reflex in patients with dementia: is it possible to use it for early diagnosis? Neurol Sci, 33(1), 17-21.
Brandt, T., Schautzer, F., Hamilton, D.A., Brüning, R., Markowitsch, H.J., Kalla, R., Darlington, C., Smith, P., & Strupp, M. (2005). Vestibular loss causes hippocampal atrophy and impaired spatial memory in humans. Brain, 128(Pt 11), 2732-41.
Gavrilov, V.V., Wiener, S.I., & Berthoz, A. (1995). Enhanced hippocampal theta EEG during whole body rotations in awake restrained rats. Neurosci Lett, 197, 239 –241.
Harun, A., Oh, E.S., Bigelow, R.T., Studenski, S., & Agrawal, Y. (2016). Vestibular impairment in dementia. Otology & Neurotology, 37(8), 1137-42.
Jacobson, G.P., & Newman, C.W. (1990). The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg, 116(4), 424-7.
Jacobson, G.P., & Calder, J.H. (2000). Self-perceived balance disability/handicap in the presence of bilateral peripheral vestibular system impairment. JAAA, 11(2), 76-83.
Leandri, M., Cammisuli, S., Cammarata, S., Baratto, L., Campbell, J., Simonini, M., & Tabaton M. (2009). Balance features in Alzheimer’s disease and amnestic mild cognitive impairment. J Alzheimers Dis, 16(1),113–20.
Lucieer, F., Vonk, P., Guinand, N., Stokroos, R., Kingma, H., & van de Berg, R. (2016). Bilateral Vestibular Hypofunction: insights into etiologies, clinical subtypes, and diagnostics. Front Neurol, 7, 26.
O’Mara, S.M., Rolls, E.T., Berthoz, A., & Kesner, R.P. (1994). Neurons responding to whole-body motion in the primate hippocampus. J Neurosci, 14, 6511-23.
Stackman, R.W., & Herbert, A.M. (2002). Rats with vestibular lesions require a visual landmark for spatial navigation. Behav Brain Res, 128, 27– 40.
van de Berg, R., van Tilburg, M., & Kingma, H. (2015). Bilateral vestibular hypofunction: Challenges in establishing the diagnosis in adults. ORL; J Otorhinolaryngol Relat Spec, 77(4), 197-218.
Ward, B.K., Agrawal, Y., Hoffman, H.J., Carey, J.P., & Della Santina, C.C. (2013). Prevalence and impact of bilateral vestibular hypofunction results from the 2008 US National Health Interview Survey. JAMA Otolaryngol Head Neck Surg 139(8), 803-810.
Citation
Jacobson, G., McCaslin, D., & Hatton, K. (2017, June). Vanderbilt Audiology Journal Club - bilateral peripheral vestibular system impairment. AudiologyOnline, Article 20413. Retrieved from https://www.audiologyonline.com




