Editor's note: This text-based course is an edited transcript of a live webinar.
Learning Outcomes
As a result of this Continuing Education Activity, participants will be able to:
- Describe concepts underlying chirp stimuli.
- Define the role of click versus tone burst stimulation in infant ABR measurement.
- Identify 3 advantages of chirp stimuli in infant ABR measurement.
Introduction
Dr. James Hall: This course is part two of a two part series on auditory evoked responses. The first course provided an overall review of a protocol for ABR. Today we are going to focus on the stimulus parameters, and chirps in particular, because of their importance to pediatric hearing assessment.
Evidence-Based Practice
When I first heard about chirps many years ago, none of the clinical ABR systems had chirps as stimuli. As time went on, some of the manufacturers began to introduce chirps. As with any other new development, they were heavily promoted. However, I was not going to start using a new type of stimulus when the existing stimuli - traditional tone bursts and clicks - worked just fine. I kept an open mind, but I looked for evidence. Today, there is plenty of evidence for the use of chirps. There are dozens and dozens of peer-reviewed journal articles, which provide unequivocal evidence in support of chirps. I will review the literature in this course.
Let me quickly define what we mean by evidence-based. Evidence-based practice is best practice. One definition is that evidence-based practice is “the integration of best research evidence with clinical expertise and patient values” (Sackett et al., 2000, page 1). Best practice means you are providing standard of care, whether you are performing screenings, diagnostic assessments, or implementing management based on research findings. It is not a substitute for clinical expertise, rather, it combines clinical expertise and experience with the latest research findings to provide the very best clinical services.
There are different levels or grades evidence. According to the US Preventative Services Task Force, these include:
Level I: Randomized control trial
Level II: Non-randomized control trial
Level III: Cohort or case-control study
Level IV: Ecological or descriptive studies
Level V: Opinions of respected authorities based on:
Clinical experience
Descriptive studies or
Reports of expert committees
When a clinical guideline is developed by a taskforce, for example, the taskforce always reviews evidence taking into account that some evidence is better than others. You can also evaluate evidence yourself when you read a journal articles, or when you seek out evidence to support a clinical process or clinical decision. In terms of levels of evidence, Level V at the bottom of the list (i.e. weakest evidence) is opinions of respected authorities. This may be a group of experts agreeing that something should be done a certain way, clinical case reports or just one person’s clinical experience.
The strongest evidence, Level I, is a randomized control study where there is a control group and an experimental group. We know that when findings are reported in a peer reviewed journal than it is strong evidence. We can be quite sure our clinical services will be effective when they are based on strong evidence.
Evidence-Based, Frequency-Specific ABR Test Protocol
Stimulus Parameters
Figure 1 provides a brief overview of stimulus parameters to set the stage for today’s course. This topic was covered in depth in part one, so please refer to part one for more details.
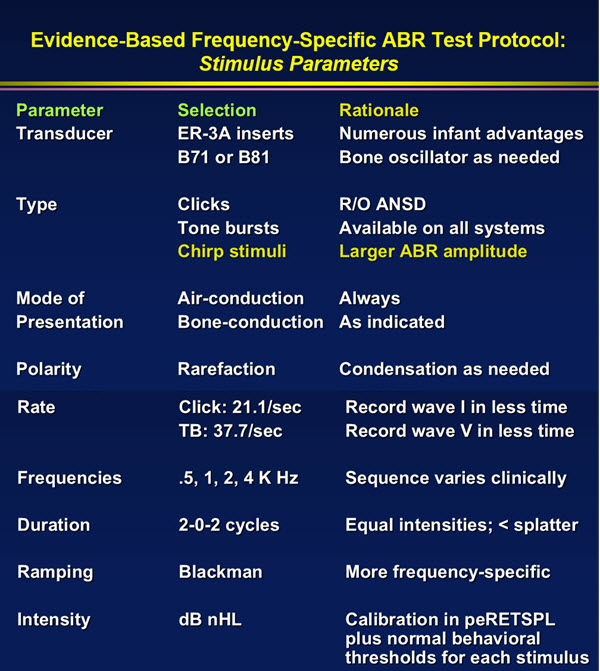
Figure 1. Stimulus parameters for evidence-based, frequency-specific ABR test protocol.
As you can see in Figure 1, ER-3A insert earphones have numerous advantages for infant ABR assessment. While clicks, tone bursts and chirp stimuli are all options for the type of stimulus to use, today’s course will discuss the advantages of chirp stimuli for infant hearing assessment. Air-conduction is always selected as the mode of presentation, with bone-conduction testing performed as indicated. Rarefaction is the polarity used for infant ABR testing, and it is important to consider changing polarity if the response you are trying to record is not optimal. Use the fastest rate possible without deteriorating the response you are recording to save time. Refer to Figure 1 for selection of other parameters such as frequencies, duration, ramping and intensity. Keep in mind that the chirp stimulus is now within the evidence-based ABR test protocol. Use of the chirp stimulus is not mandatory. If you are not using chirps, it doesn’t mean you are providing substandard care; however, there are some compelling advantages to chirps.
Role of Click and Tone Burst Stimulation in Infant ABR Measurement
Even though you can record an ABR in an infant without the use of chirp stimuli, you can record it much quicker and sometimes perhaps more accurately when you use chirps. There are chirp versions of clicks and chirp versions of tone bursts. In my opinion, both of these types of stimuli play an important role in infant ABR measurement. Some experts will say there is no longer a need to use clicks, as tone bursts provide you with all the information you need. I disagree; I do not spend a lot of time recording ABRs with clicks, but in a matter of a couple of minutes per ear, the click-evoked ABR can provide very valuable information.
I have a lot of clinical experience to support this statement: starting off your infant ABR assessment with a click, will provide a lot of information on what type of problem you are dealing with, and will save you time later on in that evaluation. In some cases, a child sleeping naturally might never fully go into a deep sleep, or they may wake up prematurely before you have finished testing. The click ABR can very often give you the information you need to manage that child effectively.
Let me just develop the rationale for why we need to use a click at the beginning and then why we also need to always go on to use tone bursts.
Joint Committee on Infant Hearing Position Statement
One reason for using the click is that it is clearly stated or recommended in the Joint Committee on Infant Hearing Position Statement. Currently, the most recent position statement is 2007, but sometime in 2016 a newer position statement will be available. For those of you who are interested in reading it when it is available, just periodically check the website https://www.jcih.org/posstatemts.htm or do a Google search on “Joint Committee on Infant Hearing”, and look for a guideline that is more recent than 2007.
This position statement is a clinical guideline for how to identify, diagnose, and manage hearing loss in infants. The protocol in the guideline that I've summarized here, is for infants and toddlers from birth to six months. There is another set of guidelines within the same document for ages six months to two years.
The guidelines clearly state that an ABR assessment should include a click evoked ABR with both rarefaction and condensation polarity stimulation if there are risk factors for auditory neuropathy. At the very least, in those patients you should use clicks.
Strengths and Weaknesses of Click-Evoked ABR
Now here is my approach. When it comes to performing ABRs, I am both conservative in terms of not missing anything and I am also quite aggressive because I don’t want to make mistakes. With the child’s whole future at stake based on these test results, I don’t want to make a mistake and miss auditory neuropathy. For a child who has never been evaluated, I begin every ABR assessment with the assumption that the child has auditory neuropathy until I prove otherwise. Now granted, the likelihood of auditory neuropathy being present is less than the likelihood it is not present.
Most children do not have auditory neuropathy, but up to 5% of children with hearing loss have auditory neuropathy. It is pretty high percentage. I am going to do everything I can to rule out auditory neuropathy at the very beginning of the ABR, and in most cases that will happen. After I rule out auditory neuropathy, I can then go on assuming that we are dealing with either a conductive, sensorineural or mixed loss, or normal hearing. That is a good reason for starting off every ABR with a click stimulus. With the click stimulus, within minutes, we can very often differentiate between the major sites of dysfunction within the auditory system.
A minute or two after I've started an ABR using a click stimulus, I have a rough idea of what may be happening. I may suspect normal hearing, or a conductive component, or a neurological problem. Keep in mind that the area around 3000 Hz is the area that is the most activated when you are recording a click ABR; in other words, that part of the cochlea is generating most of the ABR with a click. Of course that depends on the stimulus intensity and some other factors, but certainly the click ABR is giving you information primarily between the 2000 Hz and 4000 Hz region of the audiogram. That means if you have a patient with a low frequency hearing loss, you'll miss the loss altogether if you only use a click ABR. The click ABR will suggest that the hearing sensitivity is normal.
Likewise, if there is a very high frequency loss that might impact speech perception and language acquisition, that too will be missed if hearing in the 2000 or 3000 Hz range is adequate to produce the ABR. For a patient with a severe to profound very high frequency loss, you might actually still record an ABR for a click, but it will be quite a bit delayed. This is because the click stimulus will not produce the ABR up in the higher frequency region. The traveling wave will have to reach 1000 Hz or the lower frequency region to produce the ABR, and therefore you will see a delayed latency.
So while the click-evoked ABR is diagnostically useful, it is not adequate to provide frequency specific measurement. Audiologists around the world routinely contact me with clinical questions. Recently, an audiologist said, “In my country, hearing aids are fit with click ABRs. How would you recommend doing that?” I responded that every piece of ABR equipment you are going to buy these days has tone bursts. It is totally inadequate and impossible to fit a hearing aid based only on click ABR information. That would be like having an adult come in your clinic with a hearing loss, and instead of performing a complete audiologic assessment including loudness discomfort levels and speech audiometry, you simply measured hearing at one frequency. It is like measuring the threshold at 3000 Hz and fitting a hearing aid on this one piece of data. It would be impossible; the same is true for fitting a hearing aid with a click ABR only.
Click-Evoked ABR: Differentiation Among Types of Auditory Dysfunction
Why do we use a click ABR? First of all, it gives us a general idea of what hearing is like up in this critical high frequency region. There are many studies showing the relationship of hearing loss to click ABRs. Gorga and colleagues (2006) at Boystown National Research Hospital looked at ABR threshold for the click ABR, as compared to pure tone thresholds in 2000 to 4000 Hz region. They found the correlation to be very high, well over 0.9. For the most part, there is good agreement between the click ABR and pure tone thresholds in the 2 – 4 kHz region.
At the very least, after a minute or two, the click ABR threshold will reflect hearing sensitivity up in this region. Perhaps more importantly, the click ABR gives you diagnostic information on the type of hearing loss as you can see in Figure 2.
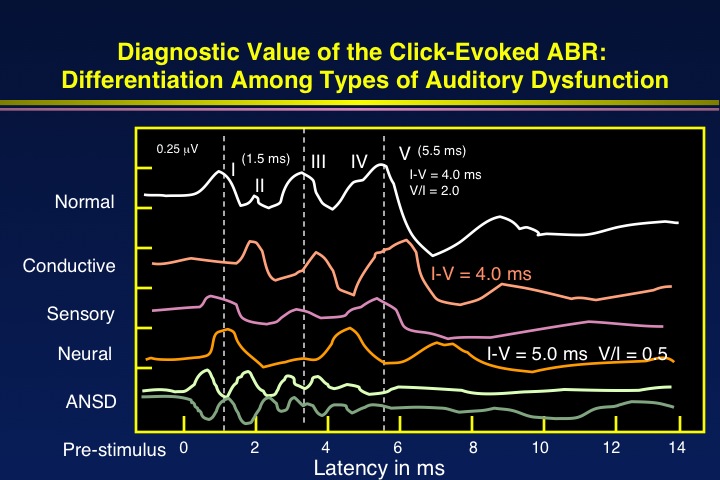
Figure 2. Examples of click-evoked ABRs with various types of auditory dysfunction.
Again, I do not spend much time doing a click-evoked ABR because you can get the information you need in a very short time. For example, in just one or two minutes, if you get a perfectly normal looking ABR with click stimuli at an intensity level of 85-90 dB (like the top “normal” line in Figure 2), you know there is hearing somewhere. You can analyze the latency for wave I, wave III, wave V. You can look at the interwave latencies. In this example, you can immediately tell that there is no conductive loss because wave I has perfectly normal latency.
A conductive loss would shift all the latencies little further out, like the second tracing from top in Figure 2 labeled “conductive”. The interwave latencies are normal, but all the absolute latencies are delayed in a conductive loss. Notice that with a conductive loss, wave I looks like the wave I in a normal ABR. Why? Because once you overcome the air-bone gap with a higher intensity, you are stimulating a perfectly normal cochlea. There is synchronous firing of neurons.
In the top “normal” example, a normal wave I that is normal in latency tells me it is not a conductive issue. The interwave latency is normal in this case; of course, what is considered normal interwave latency depends on the child’s age and other factors including anesthetic agent, and body temperature. In this case, the interwave latency is normal for the child’s age, so there can’t be a neurological problem.
You might ask, what about auditory neuropathy? If you first record with rarefaction stimuli and then condensation stimuli, and you get the same wave with both, then it is a real ABR. If you use rarefaction and then condensation, and the result is a totally opposite polarity response, then that is not an ABR. You can see an example of this on the bottom of Figure 2 for the waves labeled ANSD. That is purely a cochlear microphonic. Everyone has a cochlear microphonic if they have good hearing in the cochlea.
You could get a cochlear microphonic followed by the typical ABR waves, and this would not be ANSD. But, if you only record a cochlear microphonic, then that's an ANSD pattern. That's why I always use rarefaction and condensation polarity clicks to start off the ABR.
The tracing labeled “sensory” in Figure 2 shows a poorly formed response. In these cases they may be no wave I or it is barely there. Then we know there is hearing loss somewhere and it is sensory. There is no delay in the wave I to wave V latency. It is a sensory loss, and now the question is identifying the degree of loss at different frequencies.
In some cases you may find a very delayed wave III and wave V, and a normal wave I, as in the “Neural” example in Figure 2. In this case, you first have to rule out premature age, under the age of 18 months.
You need to rule out body temperature being low such as hypothermia, and you need to rule out the anesthetic effect. If you rule those out, perhaps this is a neurological problem.
In summary, here are the reasons why I feel it is very important to begin with a click-evoked ABR for infant hearing assessment:
- Only requires a few minutes of test time
- Analysis permits differentiation among types of hearing loss
- Waveform analysis indicates test ear (presence of wave I)
- Identification of auditory neuropathy spectrum disorder
- Findings help to determine next steps in the assessment, e.g.,
- Bone conduction ABR
- Tympanometry
- ASSR
- Recommended by the:
- 2007 Joint Committee on Infant Hearing (USA)
- International clinical guidelines (e.g., UK, Canada, Australia)
Estimation of Frequency-Specific Auditory Thresholds with Tone Burst ABRs
Ultimately, the goal that we have in performing an ABR in an infant is to come up with a very first estimation of hearing sensitivity.
If hearing sensitivity is within normal limits for low frequencies (e.g., 500 Hz region), and for mid frequencies around 1000 Hz, and for higher frequencies, then of course there may be no audiologic management necessary.
If we collect data points with our ABR testing for the low, mid and high frequencies and they indicate there is hearing loss, then we know audiological management is in order.
Our goal is to amplify sounds so that even the weakest of the speech sounds - which are always the high frequency consonants - are audible. The only way we can know how to amplify the speech spectrum for a child is to have some reference for that child’s thresholds in the low, mid, and high frequencies. The only consistent way to get that information is with ABR. OAEs don’t give us that information. The admittance measurements are very valuable but they do not give us that information. There is no other technique. The faster we can get this information in a child, and the more complete the information we can obtain about thresholds, then the more accurately and effectively we can manage the child with either hearing aids or perhaps cochlear implants.
The research relating hearing loss to ABR thresholds goes back to the 1990s. There are dozens and dozens of papers, one example of which is Stapells and Oates (1997). In this study, highly experienced pediatric audiologists like Judy Gravel tested children using behavioral methods. The children were obviously not infants because we cannot test infants using behavioral techniques. Then, they’d record ABRs using tone bursts. The bottom line is that there is good correlation between behavioral thresholds and tone burst ABR thresholds at 500 Hz, 1000 Hz, 2000 Hz and 4000 Hz.
This has been proven over and over again. More recent studies, including Gorga and colleagues (2006) and McCreery and colleagues (2014), also show the same thing. Across the range of hearing loss, there's pretty good agreement for different stimuli. If we were to compose a list of all the published references on using tone bursts to estimate frequency specific ABR thresholds, it would be a very long list. I’ve included selected references on this in your handout, and I have also reviewed all of the literature in my book (Hall, 2015).
I encourage you read some of these articles yourself to review the evidence for using tone burst ABR to estimate hearing thresholds.
David Stapells (2000) performed a meta-analysis by reviewing the peer reviewed literature on this topic. He found that there is very little difference between the air conduction tone burst ABR thresholds and pure tone thresholds in children with hearing loss across studies. Tone burst ABR is not perfectly accurate down to the dB, but it is certainly a very good early reference for hearing. Tone burst ABR allows us to fit hearing aids or make valid decisions about cochlear implant candidacy.
Definition of Chirp Stimuli
Anyone who has heard a bird chirping, has heard a chirp. It is a quick sweep through frequencies, either low to high or high to low frequency.
There are more than one type of chirp, or chirp equations, available.
CE-Chirp. The CE-Chirp is a trademarked name for a chirp that was developed by Danish scientist Claus Elberling; CE are his initials. There are at least three manufacturers that offer CE-Chirps – Interacoustics on the Eclipse device; Maico on the MB 11 which is a screening device; and GSI on the Audera. Other manufacturers offer chirps but they are not the same as the CE-Chirp.
Most of the literature that you'll come across and most of literature that I am citing in this article will be based on the CE-Chirp. While the original CE-Chirps were developed by Elberling, he worked with other researchers including Manny Don. Manuel Don was for many years at House Research Institute in Los Angeles and he just retired.
The first articles describing the current generation of chirps include Elberling & Don (2008), Elberling (2010), and Elberling, Callo, & Don (2010). You can go back to the 1980s and find even earlier articles on chirps, but not the chirps that we are talking about.
Click v. Narrow Band Stimuli: Cochlear Excitation Patterns
With a click stimulus, the entire cochlea is activated almost instantly.
The duration of the stimulus is 0.1 millisecond, or 100 microseconds. It is almost instantaneous. A very transient brief stimulus like the click produces a wide range of frequencies in the spectrum. With a click, the ears are stimulated by a wide range of frequencies almost instantly. When the resulting travelling wave reaches the 3000 Hz region, or somewhere between 4000 and 2000 Hz, the hair cells are activated, the neurons fire and the ABR occurs. This all happens within 5.5 milliseconds at a high intensity. Meanwhile, the travelling wave continues up the cochlea to the apical region, but it doesn’t contribute to the ABR response because the response has already occurred.
That is true even for a tone burst or tonal stimulus. A tone burst is usually about an octave range of frequencies; it is not a single frequency. The higher frequency region of that octave produces the ABR and the rest of the tone burst region does not contribute to the ABR because the ABR has already occurred.
How do we get the entire cochlea to contribute to the click ABR or how do we get the entire octave range for a tone burst to contribute to the ABR? That's the goal. The rationale is that if we can get the entire click cochlea producing an ABR rather than just one little region near the base, the response should be much bigger. The same is true for the tone burst.
If you look at a chirp temporal waveform, or the chirp waveform over presented over time, you will see that the lower frequencies are presented first. In fact, the lower frequencies around 500 Hz are presented about 5 milliseconds before the highest frequencies.
These lower frequencies head off towards the apex of the cochlea and get a head start. They are well on their way toward the apex before some of the other frequencies are presented. Then the highest frequencies around 4000 Hz to 5000 Hz, are presented at the very end of this process. Theoretically, each of these frequency regions reaches their destination on the cochlea at the same time, and you have synchronous firing of neurons that represent all the different frequencies. If that is the case, then the low frequency part of the chirp, which starts out earlier will tend to pull in the wave 5 so it is going to occur at the same time as the mid frequency, which is presented a little bit earlier. The same time even as the high frequencies, which are presented almost at the normal time.
You end up with a wave V that is lined up for the low, mid, and high frequencies. This is the concept. It is called temporal compensation. Low frequencies are presented a little earlier in the chirp than the high frequencies, and we end up theoretically with a much bigger response.
There are two questions that I immediately asked when I heard about chirps. First, if you calibrate a chirp and present it to the patient, is the intensity level equivalent to the traditional tone burst and traditional click stimuli? If the intensity were actually higher for the chirp type stimuli, then you wouldn’t be able to accurately estimate threshold.
Studies were done that showed that the peak equivalent reference equivalent threshold SPLs (peRETSPLs) for CE-chirps octave bands and regular tone bursts are exactly the same (e.g., Gotsche-Rasumussen, Poulsen, & Elberling, 2012). If we find that the ABR is occurring at 30 dB for a tone burst, or 30 db for a chirp, it's the same threshold.
The other question I asked is, are chirps representing the same frequencies technically as tone bursts? In other words, is the spectrum of a chirp octave band the same as the spectrum for traditional tone bursts? Plenty of research shows yes. Tone bursts aren't single frequencies. When we are using a 500 Hz tone burst for ABR, it is not exactly 500 Hz; it is an octave band around 500. That is all we need. For the audiogram, we don’t really need to have information for each single frequency. This is because when we fit a hearing aid on an infant, we are fitting amplification with bands of frequency, not a single frequency. This amount of frequency specificity for the chirp tone burst and the traditional tone burst is more than adequate, and it is the same.
If you want to see what these waveforms look like, there is an example in Kristensen & Elberling (2012). They show electrical waveforms for the traditional click and for different chirps at different levels, including the CE-chirp and the LS-chirp. LS-chirp stands for level specific chirp. It is a slightly different looking chirp depending on the intensity level, because the higher the intensity, the more the travelling wave in cochlear mechanics will shift. You are not going to see the same thing happening in a cochlea at lower intensities and high intensities, so you have to have slightly different chirps depending on the intensity.
ABR Latency Values: CE-Chirp Octave Bands
Because the low frequencies in the chirp are being presented early, wave V latencies for low frequency octave bands (e.g. 500 Hz) appear earlier than the high frequency octave bands (e.g. 1000 Hz, 2000 Hz, or 4000 Hz). Typically at 500 Hz, we would expect the ABR to occur at a longer latency. It takes about 5 milliseconds for the travelling wave to get from the 4000 Hz region up to the 500 Hz region in the cochlea. There is a traveling wave delay, but of course that's being compensated for in the chirps as 500 Hz is presented a little earlier. So ironically, using low frequency chirps, the ABR is not delayed in latency. It is not coming in around 10 milliseconds like we would expect it, but it comes in earlier.
This is strictly an issue of how you want to plot the latency. Theoretically, a manufacturer could plot all the latencies based on where the click ABR occurs rather than moving everything earlier. Regardless, you need to know where to look for wave V when you are analyzing the response.
Advantages of Chirp Stimuli in Infant ABR Assessment
What are the advantages of chirp stimuli? First of all, when you are using a chirp stimulus, you are activating the entire cochlea. This is in contrast to a click stimulus that will activate only the 3000-4000 Hz region, or approximately 2000-4000 Hz.
As you get down to lower intensities for your stimuli, the amplitude of the chirp response will be much greater than that of the click response. There is a very small difference at high intensities but as we get near lower intensities, the amplitude is quite a bit different and the chirp wave V amplitude is much greater. If you look at wave V for a 20 dB click stimulus versus a chirp stimulus, you will see the chirp wave V is crisper, cleaner, more obvious and bigger. There are studies from all around the world where you can see this, many of which are included in your handout, such as Rodrigues and Lewis (2013) and Kristensen and Elberling (2012).
Conventional Click versus CE Chirp Evoked ABR
Figure 3 shows waveforms from one of my patients using chirps and clicks.
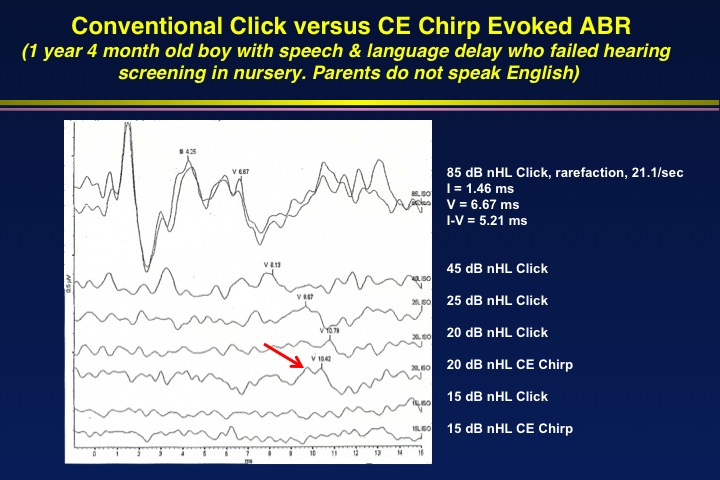
Figure 3. Click versus CE-Chirp Evoked ABR comparison for child age 1 year, 4 months.
When CE-Chirps were first installed on my ABR system, I kept relying on clicks and traditional tone bursts for my assessments, while I did some experimenting with chirps. Much of the literature that I mentioned today wasn’t available at that time. You can see in the figure that the uppermost response to a click at 85 dB nHL is a clear response. I started decreasing the intensity using the traditional click stimulus. You can see the click wave V at 45 dB and 25 dB; the latency is shifting out as the intensity decreases, as you would expect. At 20 dB nHL the click wave V is probably present, but it is really small.
Then, I wanted to see what kind of a response I would get using a chirp stimuli at 20 dB nHL. You can see where the red arrow is on the figure, indicating wave V from this 20 dB nHL chirp. It is as least twice as big as that from the click of the same intensity. The chirp wave V latency is a little shorter than the click wave V, as expected.
At 15 dB nHL, there was no response for either the traditional click or the chirp. This is an example of confirming the threshold was 20 dB for the ABR.
If a CE-Chirp evoked ABR response is twice as big, I should be able to get an ABR in half the amount of time as a click-evoked ABR. When you record an ABR, you are detecting a signal as the ABR in the presence of background noise. Background noise is everything except the ABR, including muscle artifact, electrical artifact, ongoing EEG, etc.
If the ABR response is twice as big, we should reach our criteria of an adequate signal-to-noise ratio or ABR-to-noise ratio of 3:1 more quickly. We should get there quicker with this big a response.
So I ran a chirp-evoked ABR at 4000 Hz. You can see the results in Figure 3. You can see the wave V at 80 dB nHL, 40 dB nHL, 20 dB nHL and 15 dB nHL. In fact, I stopped the averaging early just to make a point. I came up with a total test time of just over 1 minute (69.5 seconds) to find the threshold for 4000 Hz in one ear.
I found the same thing at 2000 Hz. In fact, the response to 20 dB nHL at 2000 Hz was very big. This child turned out to have normal hearing. However, going in to the testing we did not know hearing status and there was a serious concern about hearing loss. The child was 1 year, 4 months of age and was not speaking; both speech and language were very delayed.
The bottom line is by using chirp stimuli, you can radically cut down the test time when you are performing ABRs in infants.
Another advantage of the chirp is that it can give you a more accurate measurement of ABR threshold. Let me give you an example (Figure 4).
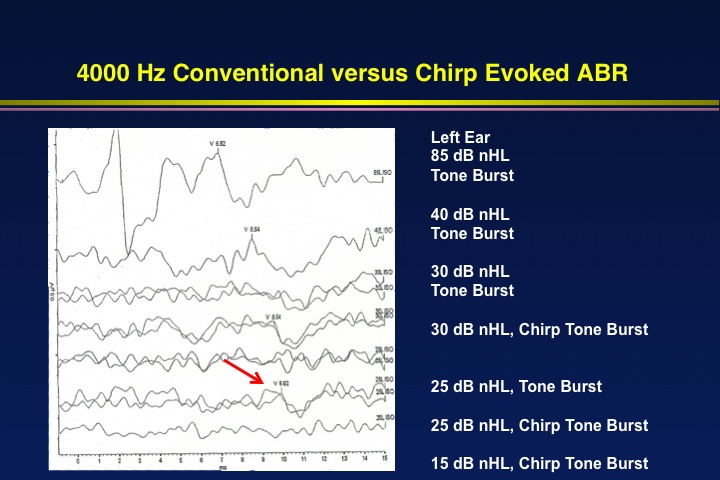
Figure 4. 4000 Hz conventional versus chirp evoked ABR on a 1 year, 4 months old child.
In Figure 4, I was using a 4000 Hz tone burst stimulus and I was able to track down the response at 85 dB nHL and 40 dB nHL. At 30 dB nHL it had disappeared. So I decided to use a chirp stimulus to see if I could detect a response at 30 dB nHL. Sure enough, I got a very repeatable response using the chirp. Then, I went down to 25 dB nHL with a chirp and got a response (see red arrow on Figure 4), even though there was no response from the tone burst stimuli at that same level. Finally, to complete the testing I went down to 15 dB nHL and there was no response to the chirp.
As this example illustrates, I am finding that the chirp stimulus is giving me a more accurate measurement of ABR threshold. In this case, I would have overestimated the ABR threshold based on the tone burst stimulus; the chirp stimulus gave a more accurate ABR threshold. With the chirp results, I can take my ABR thresholds, plot them on an audiogram type form, estimate my behavioral thresholds from there and do it all very quickly.
Advantages of Chirp Stimuli
The advantages of chirp stimuli are as follows:
- ABR amplitude is up to two times larger for chirp stimulation
- Larger amplitude contributes to:
- More confident identification of wave V
- Shorter test time is needed to identify wave V
- Larger amplitude contributes to:
- Reduced test time for each stimulus frequency permits
- More complete estimation of auditory threshold in speech frequency region
- Possibility of infant ABR assessment in natural sleep without the need for sedation or anesthesia
- More accurate thresholds are sometimes possible with chirp stimulation
The research supports the fact that the amplitude for the ABR is usually up to two times larger for chirp stimuli than for traditional stimuli. That means you can identify wave V with more confidence, which leads to reduced test time. Overall, you can save 30 minutes or more by using chirp stimuli, which means you can sometimes get an ABR on a child sleeping naturally in a matter of 15-20 minutes, where you wouldn’t be able to do that with traditional stimuli. Most importantly perhaps, the thresholds that you do get are often more accurate with chirp stimuli.
Review of Selected Literature on Chirps
When I reviewed the literature on chirps for today’s course, I went to the National Library of Medicine and did a PubMed search. Obviously, there were a far more articles than I can summarize here, but I am selecting a few to highlight (Figure 5).
Kristensen & Elberling (2012), as I mentioned earlier, is a good overall review. If you are just getting started, you read their data on level-specific chirps. This article is published in the Journal of the American Academy of Audiology, which AAA members can access online.
While Kristensen & Elberling (2012) used adult subjects in their study, Rodrigues, Ramos & Lewis (2012) used infant subjects. Rodrigues & Lewis (2014) was a follow-up article also showing ASSR with chirps as well as ABR. I am not really emphasizing the ASSR in today’s course, but all the advantages of a bigger ABR with chirps also apply to ASSR. The ASSR is quicker and the ASSR thresholds might be more accurate using chirp stimuli, as compared to traditional stimuli.
Some studies have looked at latency and amplitude. Cebulla, Lurz, & Shehata-Dieler (2014) are researchers from Germany who looked at the waveform, latency and amplitude values of the chirp ABR in newborns. We know the latencies and amplitudes from chirp ABR are going to be different as compared to click or toneburst evoked ABR. We have to have different normative data for latency and amplitude when we are using chirps.
Xu, Cheng & Yao (2014) are researchers from China who looked at chirps. Andrew Stewart at East Carolina University has done a quite a bit of work in this area. His work has shown that you don’t need as many sweeps when using chirps to see the response (Stuart & Cobbs, 2014). There is a lot of research confirming that chirps are an evidence-based strategy for estimating thresholds in infants (e.g., Vanail et al., 2015; Zim et al., 2014; Di Scipio & Mastronardi, 2015; Maloff & Hood, 2014). Di Scipio and Mastronardi (2015) focuses on chirps for intraoperative monitoring. Because they evoke a larger response, we find more clinical applications such as this. Using the chirp intraoperatively, you can get a response more quickly, and provide feedback to the surgeon more quickly.
Roland Muhler has done work in this area (e.g., Muhler et al., 20014). He has shown that you can record ASSRs in a matter of 10 seconds - not the entire ASSR, but you can detect a response for one frequency in little as 10 seconds. At that speed, you can see that an entire ABR or ASSR could be performed in just 10 to 15 minutes - and you might not need sedation for an assessment of that duration. Although I have selected only a few key articles to highlight here (e.g. Ferm & Lightfoot, 2015; Bargen, 2015; Zhou et al., 2015; Wilson et al., 2016), there are many, many other articles on the topic that provide an evidence-based rationale for using chirps clinically.
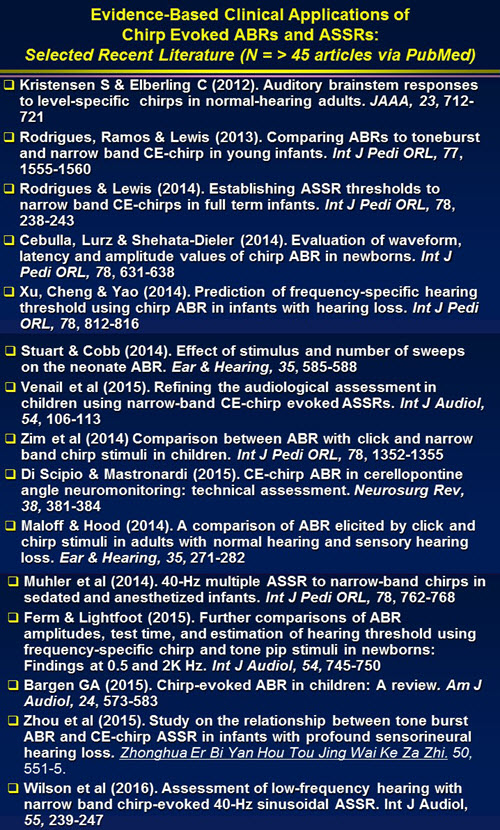
Figure 5. Evidence-based clinical applications of chirp evoked ABRs and ASSRs: Selected recent literature (n = > 45 articles via PubMed).
Evidence-Based Clinical Applications
Enhanced Diagnostic Assessment with ABRs elicited with CE-Chirp Stimuli
The use of chirps in estimating thresholds in infants is certainly the most widely used application. I would not want to do an ABR without a chirp because I know that using chirps will decrease my test time and give me more confidence in my recordings. There is a larger amplitude of wave III and wave V, as well as a larger amplitude of wave I.
Faster Estimation of Frequency-Specific Air-Conduction ABR and ASSR Thresholds
Any device that has chirps for ABR could conceivably have them for ASSR. The ASSR research is catching up with the ABR research. There is up to a 50% reduction in overall test time with chirps. Detection of an ASSR The time savings is enormous. Whether you use ABR, ASSR, or both, you are still saving time with chirps.
Better Detection of ABR and ASSR with Low Frequency Stimuli
When using chirps, there is better detection of ABR and ASSR with low frequency stimuli.
Bone Conduction ABR
The use of chirp stimuli will also enable you to be more confident with the detection of bone conduction ABR. The bone conduction ABR including detection of wave I is always a little challenging because the maximum intensity for bone conduction is only about 45 to 40 dB nHL.
The bone oscillators can’t produce high intensities for transient stimuli. However, with chirps, the ABR is much bigger so even though the intensity is not that high, you can often still easily detect wave I and wave V.
Intraoperative Monitoring
As I mentioned, there are now articles describing intraoperative monitoring using chirps.
These points are summarized in Figure 6.
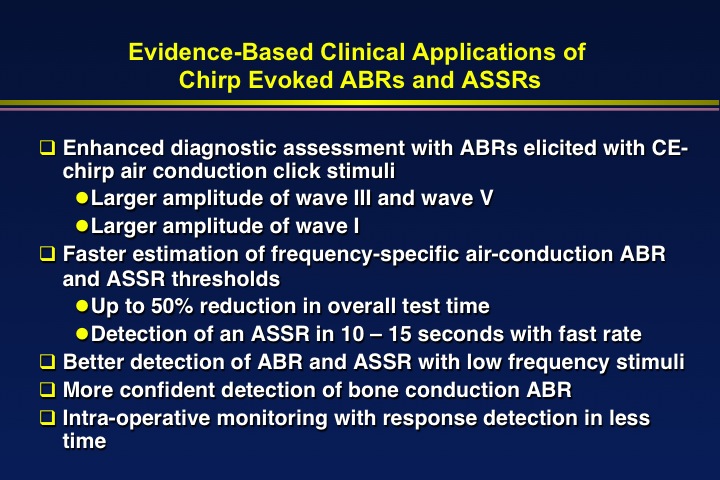
Figure 6. Summary of evidence-based clinical applications of chirp-evoked ABRs and ASSRs.
Summary and Conclusions
I hope I have convinced you in this brief lecture today that chirps stimuli offer a big advantage in infant ABR assessment. While we can get by without chirp stimuli, we can perform ABR assessments quicker and we can estimate thresholds with more confidence when we use them. With children, speed is an important factor in performing ABRs because they must be very quiet during the assessment. Most children aren't going to be quiet for long unless we use sedation or anesthesia, and there are some risks involved with that. Even if we are using anesthesia, the quicker we can perform the ABR, the safer it is for the child. A quicker test time may also allow us to see more patients in the operating room in a given amount of time.
Resources
I have provided you with select articles to review throughout this course, which will serve as great resources for more information. In addition, the new e-handbook of Auditory Evoked Responses covers all of the topics we reviewed today in greater detail, as well as procedures and protocols for many other assessments.
Questions and Answers
Do you always test both ears with ABR testing, or is there a protocol for estimating the opposite ears in certain cases?
Well that's a good question. I always evaluate both ears. Let’s say a child failed a hearing screening in one ear, and comes back to the clinic for a diagnostic assessment. A unilateral failure in the nursery means the other ear that passed the screening is at risk for hearing loss, and there is a lot of research to support that fact. We do not want to assume that just because the screening result was normal in one ear, that a diagnostic assessment of that ear is not in order.
In addition, sometimes you have a unilateral anomaly – such as unilateral atresia or unilateral microtia. Some audiologists would recommend performing ABR only on the ear with the anomaly. That makes no sense to me. If you perform ABR only on the ear with the anomaly, you are assuming that because one of the child’s ears is typical in appearance that there is normal hearing in that ear. If that were the case, we wouldn’t ever have to do hearing tests because we could assume everyone with a typical-looking pinna had normal hearing. Of course we know as audiologists, that you can have a profound hearing loss (or any degree of hearing loss) with a typical-looking outer ear.
In addition, when you have a concern about a conductive loss, whether it is based on an ear anomaly like microtia, based on a delayed wave 1 in the ABR, or based on an abnormal tympanometry result, always do air and bone on both sides. You may think that if there is aural atresia, you only need to do bone conduction to prove that the cochlea is normal. That's not a good idea. You can’t estimate the degree of conductive loss based on looking at somebody’s ear. I've evaluated hundreds of patients with aural atresia and you never know what to expect in terms of hearing. I've had cases with aural atresia in one ear, a perfectly normal looking other ear, but they had otitis media in that ear, which resulted in a bilateral conductive loss.
I would always test both ears, but not always test bone conduction unless there are some risk factors for conductive loss. Always test both ears and try to always use clicks and tone bursts unless you have some other compelling evidence that hearing sensitivity is normal, such as normal OAEs plus the ABR.
Do you have normative data for chirp as well as for clicks and tone bursts, or where can you recommend that audiologists get normative data?
Another good question. First of all, the thresholds that you estimate with chirps are usually the same as the thresholds you estimate with traditional stimuli - clicks or tone bursts. The intensity level is the same, as is the frequency and the specificity. You don’t have to have separate norms in terms of thresholds. For latencies, you definitely have to adjust your expectations because the chirp stimuli almost always produce an ABR with a shorter wave 5. I would strongly recommend that you ask your equipment manufacturer for normative data and ask them also to direct you to the peer-reviewed articles that have been published on their chirps.
If there are no peer-reviewed articles on their chirps, then you have to either find some research or do it yourself. Even if you have published normative data available for your stimuli, test a few normal subjects. Test people with perfectly normal hearing sensitivity that has been proven by an audiogram, normal OAEs etc. – maybe this is you and a few colleagues. Collect some ABR data from these normal hearing people and make sure that the average values fall within the middle of your normative data. This will prove that the normative data you are using is appropriate for your particular protocol and the setting where you are performing your ABRs.
Which protocol do you recommend for diagnostic testing in infants? ABR or ASSR utilizing the chirp?
I would never substitute ASSR entirely for ABR. Even if you wanted to use ASSR to estimate hearing threshold, you’ve got to begin with an ABR at least with a click because ASSR is not going to give you diagnostic information on the site of dysfunction. You are not going to be able to identify auditory neuropathy with ASSR, and if you are using bone conduction for ASSR, you are not going to be looking at a waveform as you can with ABR.
My bias based on my experience is to always use ABR clicks and ABR tone bursts. I use ASSR when there is no ABR to a particular frequency or maybe at any other frequencies, and I use it to supplement the ABR. I think ASSR is really valuable as a supplement for ABR but I don’t rely on it exclusively. With the right equipment, chirps can be used for both ASSR or ABR.
Is screening equipment available with a chirp stimulus?
Yes. The Maico MB 11 uses a chirp stimulus, which is one of the reasons it is so fast. Anyone utilizing ABR for screening can use chirps for screening if the equipment has chirps. I've never heard a really compelling reason not to do that. It is going to result in quicker results and you are not losing anything in that process.
There also has been talk about using multiple frequency ASSRs - more than one frequency at a time or even one with chirps - as a screening technique in automated mode. I would recommend investigating different screening devices as many more may start utilizing chirps in the future.
References
Elberling, C, (2010). A direct approach for the design of chirp stimuli used for the recording of auditory brainstem responses. JASA, 128, 2955-2964.
Elberling, C, Callø, J., & Don, M. (2010). Evaluating auditory brainstem responses to different chirp stimuli and three levels of stimulation. JASA, 128, 215-223.
Elberling, C. & Don, M. (2008). Auditory brainstem responses to a chirp stimulus designed from derived-band latencies in normal-hearing subjects. Journal of the Acoustical Society of America, 124, 3022-3037.
Gorga, M.P., Johnson, T.A., Kaminski, J.K., Beauchaine, K.L., Garner, C.A. & Neely, S.T. (2006). Using a combination of click- and toneburst evoked auditory brainstem response methods to estimate pure-tone thresholds. Ear and Hearing, 27(1), 60-74.
Gotsche-Rasmussen, K., Poulsen, T., & Elberling, C. (2012). Reference hearing threshold levels for chirp signals delivered by an ER-3A insert earphone. International Journal of Audiology, 51(11), 794-9. doi: 10.3109/14992027.2012.705901.
Hall, J.W.III. (2015). eHandbook of auditory evoked responses: Principles, procedures & protocols. Available from https://www.amazon.com/eHandbook-Auditory-Evoked-Responses-Principles-ebook/dp/B0145G2FFM
2007 Joint Committee on Infant Hearing
Kristensen, S. & Elberling, C. (2012). Auditory brainstem responses to level-specific chirps in normal-hearing adults. JAAA, 23, 712-721.
McCreery, R.W., Kaminski, J., Beauchaine, K., Lenzen, N., Simms, K., & Gorga, M.P. (2015). The impact of degree of hearing loss on auditory brainstem response predictions of behavioral thresholds. Ear & Hearing 36(3), 309-19. doi: 10.1097/AUD.0000000000000120.
Rodrigues, G.R., Ramos, N., & Lewis, D.R. (2013). Comparing ABRs to toneburst and narrow band CE-chirp in young infants. Int J Pedi ORL, 77(9), 1555-1560.
Sackett, D.L., Straus, S.E., Richardson, W.S., Rosenberg, W., & Haynes, R.B. (2000). Evidence-Based Medicine: How to practice and teach EBM. London: Churchill Livingstone.
Stapells, D.R. (2000). Threshold estimation by the tone-evoked auditory brainstem response: A literature meta-analysis. J Speech-Language Pathology & Audiology, 24, 74-83.
Stapells, D.R., & Oates, P. (1997). Estimation of the pure-tone audiogram by the auditory brainstem response: a review. Audiology & Neuro-otology, 2(5), 257-280.
Further references are located in the handout for this course.
Citation
Hall, J.W.III. (2016, June). Update on auditory evoked responses: Value of chirp stimuli in ABR/ASSR measurement. AudiologyOnline, Article 17434. Retrieved from www.audiologyonline.com


