Learning Objectives
After this course, participants will be able to:
- Describe the components of a tinnitus evaluation and management process.
- List the various options available in hearing aids aside from traditional amplification.
- List at least three other resources other than hearing aids for patients with tinnitus.
Introduction
Today's presentation will be focused mainly on the clinical aspects of evaluating and treating tinnitus. However, I will be showing a screenshot or two from our Astera² Tinnitus Module. For the purposes of today's course, we will briefly give an overview of the broad, high-level tinnitus evaluation components: the hearing assessment, questionnaires, and the tinnitus evaluation itself. This presentation is intended to be a jumping off point if you're not quite sure where to get started with tinnitus assessment, or a quick review of the components that you're currently using. If you want more detailed information on tinnitus evaluation, Otometrics does offer another AudiologyOnline course on tinnitus. I also have many resources listed at the end of this presentation for you to dig deeper if you are interested. For the second half of the presentation, we will be focusing on the "meat and potatoes" of tinnitus evaluation and management: the tinnitus toolbox.
Why Do Tinnitus Assessment?
Why should we conduct tinnitus assessments for our patients? There are several reasons. First of all, tinnitus assessment allows for improved communication with your patient. As audiologists and hearing aid dispensers, it's our responsibility to manage hearing disorders to the best of our ability. By improving that communication, and establishing trust and rapport with your patient, they will open up to us a little bit better. It gives us a framework for what that patient is dealing with. Every single tinnitus patient is different and has unique needs. Having a frame of reference for where they are experiencing is absolutely vital. Along those lines, conducting a tinnitus assessment is an affirmation of their tinnitus, and reassures the patient that we acknowledge that their tinnitus is real to them, further building on the trust they have in us.
An assessment allows us to categorize the tinnitus. You can have two people with the same quality of tinnitus, but maybe one has maskability and one doesn't. Perhaps one person's tinnitus sounds like crickets chirping, and another person describes theirs as the sound of bacon frying. Being able to categorize that tinnitus helps gets us on the same page as the patient. Furthermore, assessment is needed to establish a baseline for tinnitus treatment and subsequent assessments, as well as helping us to select the most appropriate treatment for our patients. Finally, the tinnitus assessment is a critical part of our documentation, which is required for legal reasons, HIPAA, billing, worker compensation, and best practices.
The Tinnitus Evaluation
The complete tinnitus evaluation is comprised of the following components:
- Hearing assessment
- Questionnaires
- Tinnitus evaluation
Hearing Assessment
The hearing assessment is a multi-step process. First, we start with a case history/tinnitus intake interview. We obtain medical referrals as needed. As an audiologist, you are within your scope of practice to see patients without a medical referral. However, 10 to 15% of the population currently has some sort of tinnitus, and about 0.4% are significantly bothered by it. Subjective tinnitus is where patients hear ringing in their ears, with no identifiable sound source. It may be caused by hearing loss, or perhaps not. For those patients, we have to rule out any vascular, muscular, skeletal, or respiratory structure-function issues. That's where medical referrals may be necessary.
We must also conduct an audiometric evaluation, which is important to test high frequencies, in particular at higher resolutions around where the tinnitus is suspected. Rather than the interoctaves that are commonly done at 2000, 3000, 4000 Hz, it is helpful to break down those frequencies into something a little bit smaller, like 4010 Hz, 4020 Hz, 4030 Hz. In addition, a total MCL and UCL can be beneficial during that evaluation process. Another part of the hearing assessment involves immittance measures and otoacoustic emissions. OAEs are a sensitive indicator of cochlear damage beyond what is seen on the behavioral audiogram. Often, we see OAEs affected before we see it on an audiogram.
Questionnaires
Some commonly used tinnitus questionnaires include:
- Tinnitus Functional Index
- Tinnitus Handicap Inventory
- Tinnitus & Hearing Survey
- Beck Depression Inventory
- Spuelberger State-Trait Anxiety Inventory
- Primary Care PTSD Screen
The first three questionnaires are commonly used: the Tinnitus Functional Index (TFI), the Tinnitus Handicap Inventory (THI), and the Tinnitus and Hearing Screening (THS). The last three inventories (Beck Depression Inventory, the State-Trait Anxiety Inventory, and the Primary Care PTSD Screen) are listed because approximately 35% of our patients with tinnitus have anxiety, between 13 to 28% of tinnitus patients have depression, and 33% approximately have insomnia. About 25% of our patients have some sort of comorbid psychiatric disorder, and about 33% of our patients with tinnitus have some sort of PTSD or Post Traumatic Stress Disorder. These inventories are a great way to help screen these patients. They might be coming to you because of the ringing in their ears, and they might not associate that with their insomnia or their anxiety. As hearing care practitioners, we can help make that connection and start that conversation with them.
Two other inventories that might be useful: the Six Item Cognitive Impairment Test (6CIT) and the General Practitioner Assessment of Cognition (GPCOG). These questionnaires are geared more at cognition and memory issues. It does fall within the scope of practice for an audiologist to administer these inventories. However, if you're not comfortable doing that, by all means, defer it to another professional. Bring it up with the patient's general physician. If you're working in conjunction with an otolaryngologist, mention it to them and they can introduce these topics. That being said, these additional inventories are nice to have in your back pocket, especially when you suspect something else is going on.
The Tinnitus Functional Index (TFI) is one of the newer questionnaires that has come out. It consists of 25 questions covering eight sub-scales. It includes sleep disturbance, relaxation, and quality of life. Similarly, the Tinnitus Handicap Inventory (THI) is also a 25-question inventory used to assess the patient's self-reported perception of how much their tinnitus influences their life. Both of those are good questionnaires to administer because they don't take terribly long. In addition, they've also been heavily researched and peer-reviewed. The Tinnitus Hearing Survey (THS) consists of 10 questions. It's helpful as a supplemental inventory, but it's not validated as a primary outcome measure. I would strongly caution you against using that as your only source of a tinnitus questionnaire.
We have three tinnitus questionnaires built into our system that can be accessed through Noah: the TFI, the THI, and the THS. Figure 1 shows an example of the TFI. This is a screenshot from our Astera² Tinnitus Module. You can print this out and have the patient complete it on paper, or they can answer these questions on a touchscreen. If they complete it online, the system will score it for you and break down the patient's answers into separate categories.
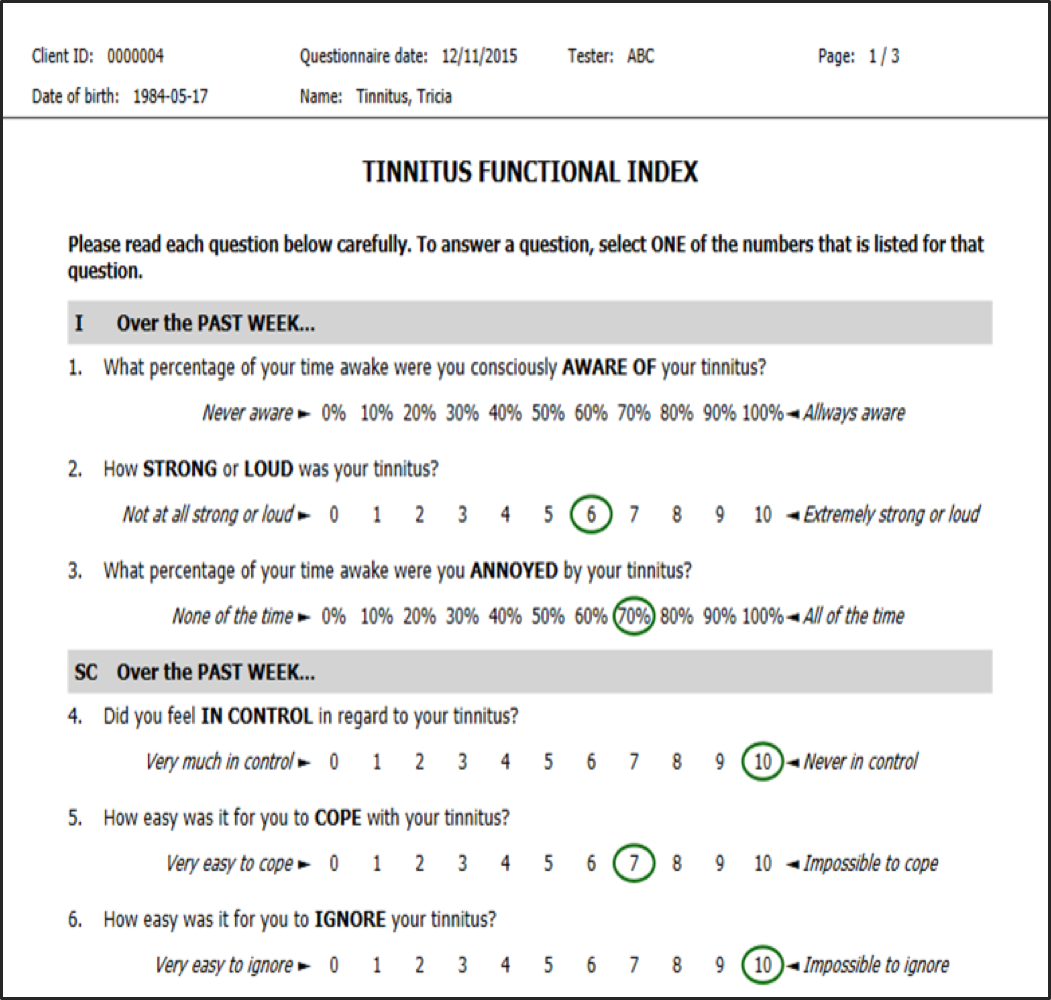
Figure 1. Tinnitus Functional Index (TFI).
Tinnitus Assessment
To reiterate, the following components are traditionally included in the overall tinnitus evaluation:
- Hearing Assessment
- Case History/Tinnitus Intake Interview (Questionnaires)
- Medical Referrals
- Otoscopic Examination
- Audiometric Evaluation
- High Frequencies
- High Resolution around Tinnitus
- Interoctaves
- MCL & UCL
- Immittance
- Otoacoustic Emissions
- Questionnaires
- Tinnitus Evaluation
When we're talking about the actual tinnitus assessment, the four key indicators are pitch matching, loudness matching, minimum masking level and residual inhibition. These indicators are important to keep in mind whenever we're billing for tinnitus. The CPT code to use for tinnitus assessment (which includes pitch, loudness, matching, and masking) is 92625. If you're only doing one ear, you will need to use the 52 modifier with that. Again, after today's general overview, if you want more detail on how to perform each of these indicators, I would strongly encourage you to check out the white papers that we've attached to this presentation, as well as the resources at the end.
Figure 2 shows another screenshot from our Astera² Tinnitus Module. This module was launched in 2013. In the center, you can see the patient's audiogram, with MCLs and UCLs. At the bottom, you can see a list of all the questionnaires that you can administer. It's a nice way to keep everything all organized in one screen.
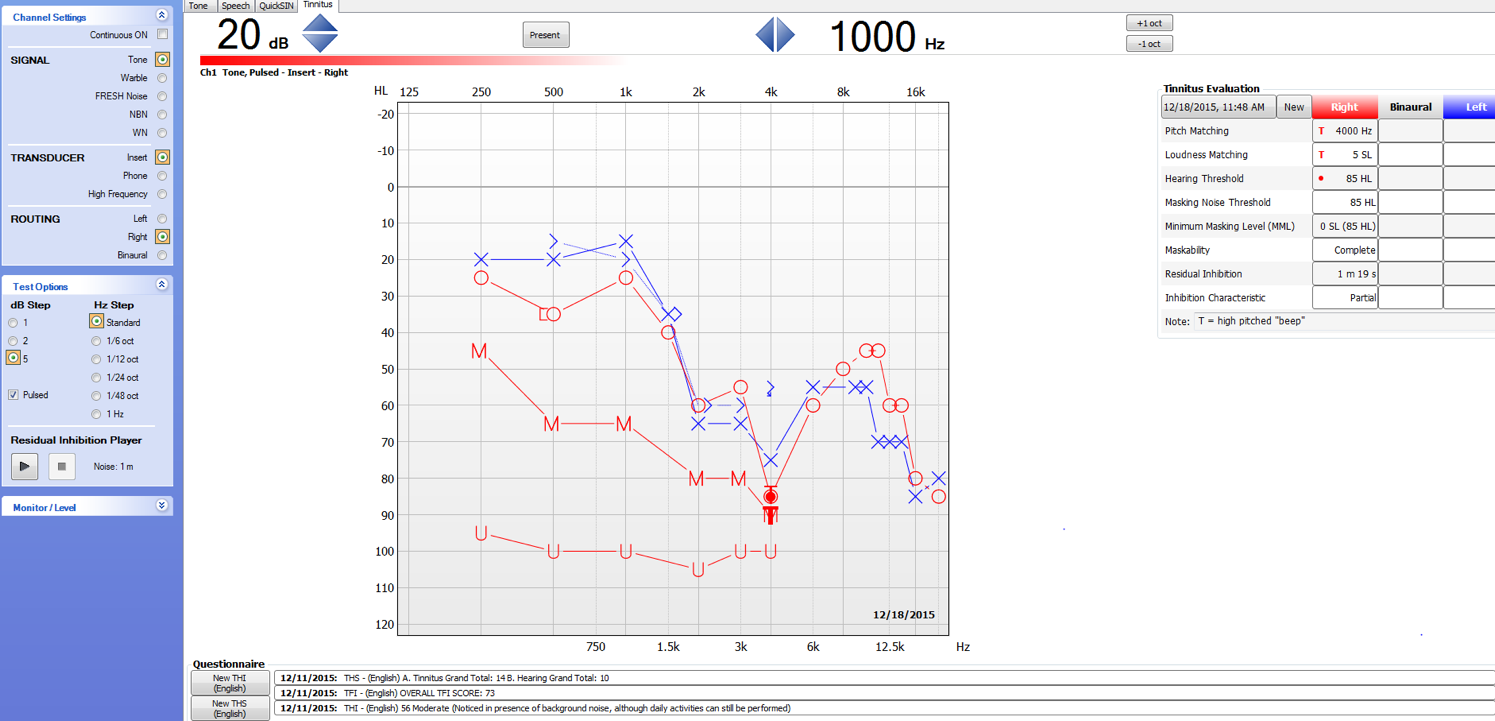
Figure 2. Screenshot from Astera² Tinnitus Module.
In Figure 3, we can see an enlarged image of everything that is needed for billing for a tinnitus evaluation (code 92625). If you fill out everything in this chart, you're going to hit everything included in that code. If you're doing just one ear, remember to use that 52 modifier. If you're doing both the right and left ear for all of these, you won't miss anything. Also, note that you can change the date of service (upper left-hand corner) to access tinnitus evaluations that were conducted on different dates.
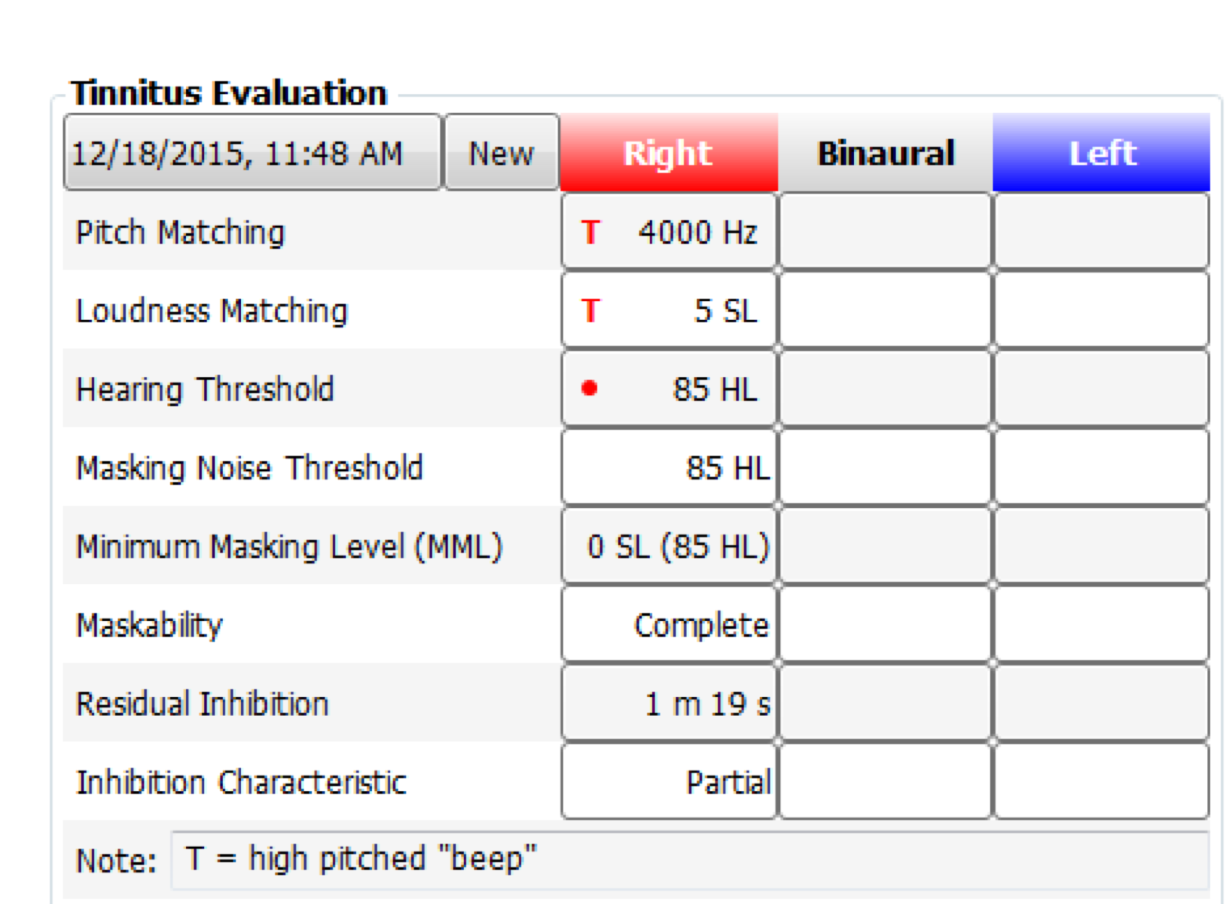
Figure 3. Tinnitus evaluation: billing information.
Hyperacusis Considerations
When tinnitus patients have hyperacusis, that adds another level of complexity. As defined by ASHA, "Hyperacusis is a rare hearing disorder that causes sounds which would otherwise seem normal to most people to sound unbearably loud. People who suffer from hyperacusis may even find normal environmental sounds (e.g., car engines, dishes clanking) to be too loud."
With regard to hyperacusis, there are three different components to be aware of:
- Hyperacusis is the physical condition of discomfort or pain caused by sound.
- Misophonia is a dislike of sound, which is often a learned, behavioral response.
- Phonophobia is a subcategory of misophonia and is defined as a fear response caused by sound.
Patients can have each of these three conditions individually, or a combination thereof. None of these conditions should be confused with loudness recruitment, which is something completely different. Also, for patients with hyperacusis, you might want to consider leaving out acoustic reflexes or UCLs. Tinnitus patients are often already anxious; we don't want to add to their anxiety by doing a UCL.
The Tinnitus Toolbox: Management Options
Some of the different management options (Sweetow & Sabes, 2010) that we have available in our tinnitus toolbox include:
- Amplification
- Tinnitus Retraining Therapy (TRT)
- Acoustic Desensitization (Neuromonics)
- Other Sound Therapies (Sound Cure, Apps)
- Cognitive Behavioral Therapy (CBT)
- Other Management Options
- Holistic
- Medical
The Big Six
Figure 4 is a helpful chart which summarizes all the different hearing aid manufacturers and their tinnitus features. Widex was the first company to have a tinnitus feature. Only within the last year or two have all six of the major HA manufacturers been able to offer an option for tinnitus. As hearing aid companies began to realize the broad impact of tinnitus, they started to see the value of including integrated maskers and soundscapes within their devices and offering more tinnitus treatment options.
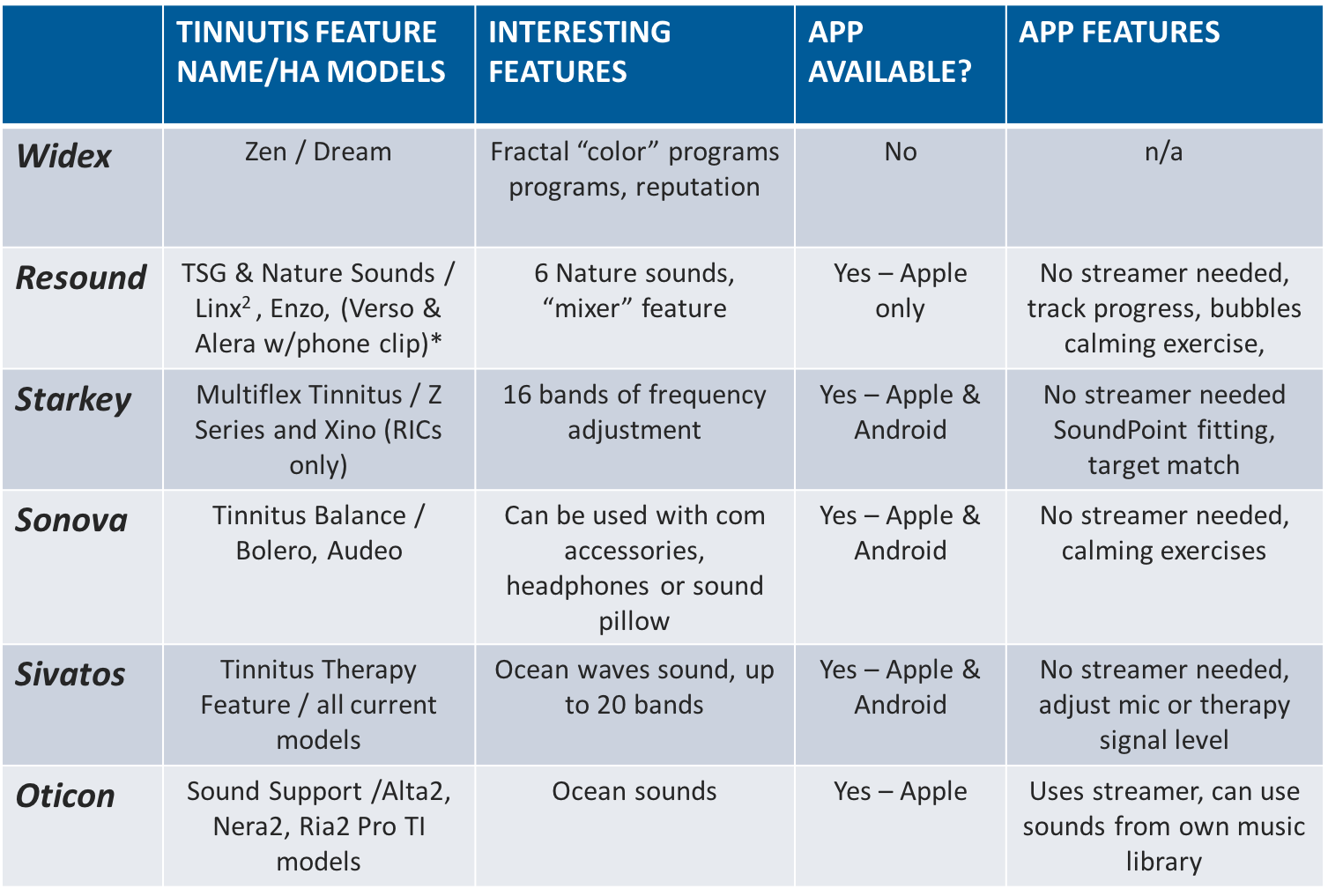
Figure 4. The "Big Six" major hearing aid manufacturers.
Widex. Widex offers Zen fractal sounds that are different "colors", such as aqua, coral, lavender, green and sand. Each "color" is a soundscape that has a different pitch, tonality, dynamic range and tempo. It sounds like ambient music. According to their research, aqua is the most popular of the Widex Zen fractal sounds. If you are thinking about using Widex Zen, aqua is a good place to start. Interestingly, the fractal sounds are programmed from a mathematical equation. It's a sequence of tones; there are no lyrics. It sounds very new-age in nature. There are similar patterns, but they're not predictable, always ebbing and flowing. With the fractal tones at a low level in the background, the patient can start to habituate to their tinnitus. The sounds can be shaped by adjusting the characteristics, such as tonality (major or minor chords) and tempo (slow, medium or fast). You could change the dynamic range of the sounds, choosing a broad and full sound, or narrowing it to be more restricted in the area of the patient's tinnitus. Widex also has a vast, searchable library that includes tinnitus surveys, as well as downloadable white papers. They also have a nice flip book.
Resound. While fractal sounds are unique to Widex, Resound integrates nature sounds into their hearing aids. With the Resound mixer, you can blend up to five different sounds. You can modify them by low, mid, or high cut. Many of their sounds are water-related, such as ocean waves, calmest storm, blue waves and cold Hawaii. They also have city sounds, such as crowd buzzing and restaurant ambiance. The sounds can be controlled with an Apple watch or iPhone. On their app, Resound has calming exercises, such as popping bubbles on a screen. Currently, their app is available for Apple products only. However, it is compatible with the Apple watch. Recently, I was listening to a story on National Public Radio, and they said that over 50% of smartwatches sold in 2015 were of the Apple variety. As such, if you have a patient with a smartwatch, there's a good chance they have an Apple device. Another nice feature about Resound is that a streamer around the neck is not needed. They have their own proprietary Bluetooth 2.4 GHz signal that they developed. It streams directly from your phone to the hearing aid.
Starkey. Starkey has something called a SoundPoint app. It can be used on an iPad and also Android devices as well. You can also use it on a touchscreen in a booth, or you can have the patient control it on your computer with a mouse instead of using a finger. Essentially, you can use it through any medium. It's a way to best fit the tinnitus algorithm. The patient listens through the computer speakers to different kinds of tinnitus-sounding noises (high pitch, low pitch, some with embedded noise, some without). Then they draw a graph on the screen (either by dragging their finger on a touchscreen or using a mouse) to represent what their tinnitus sounds like. It's a great way to give the tinnitus patient some control over their diagnosis, and some control over that evaluation appointment. Many times, patients come in anxious and scared. Being able to give them some degree of control back in their hands is a nice first step for them.
Starkey, along with most manufacturers, also has an extensive library. They include the ICD-9 and ICD-10 tinnitus codes in their brochure so you can see exactly how these two codes correlate, now that we live in an ICD-10 world. Starkey also does not require the use of a streamer. In their high-end hearing aids, the patient has 16 bands to adjust. If you have patients who are sensitive to different pitches and frequencies, Starkey does provide quite a bit of flexibility for them. At the time of this presentation, Starkey's tinnitus product is in the Xino in the Z series.
Sonova. Sonova is otherwise known as Phonak. They have an app that can be used with headphones or a sound pillow, and you don't even need to wear hearing aids. You can incorporate the streamer if you need to. Their tinnitus program is called Tinnitus Balance. It is currently available in the Bolero and Audeo hearing aid lines. It is available in both Apple and Android products. I believe they're currently the only company where the app is compatible with the headphone or the sound pillow specifically. If someone is afraid of or intimidated by hearing aids, or even if they have normal hearing, this is a nice feature to be able to offer them. They have many sounds to choose from, and their library is easily searchable.
Sivantos. Sivantos is formerly known as Siemens. With Sivantos, their tinnitus therapy feature is available in a wide variety of hearing aid styles (ITEs, RICs, slim tubes, BTEs). They are able to offer the flexibility to fit all different kinds of hearing aids, and not be limited to only RIC hearing instruments. Sivantos also has a high tone noise available as a signal option, although I'm not sure how often you would use that because most of our tinnitus patients are annoyed by that high tone noise. However, you may have patients who want more of a maskability option, and that high tone might be their preference. Siemens has 20 bands available for fine tuning of their instruments. The app is also compatible with Apple and Android products, and no streamer is needed.
Oticon. Oticon has a fantastic professional website, as well as an easy-to-navigate consumer website. They also have a wonderful breakdown of the tinnitus therapy, in particular, how to handle follow-up visits. We'll talk a little bit more about tinnitus retraining therapy and cognitive behavioral therapy in a few minutes, but a lot of these manufacturers are pushing a combination of the two. If you read the research, having this combined approach has been shown to be most beneficial to the majority of patients. Oticon does a nice job of synthesizing all that. One thing that I like about Oticon is that they have a chart to help you determine what the goal of tinnitus treatment will be for each patient. They offer different ways to program everything and different ways to treat the patient in an easy-to-read breakdown. That way, if you are new to treating tinnitus, you can get a better idea of how to handle different types of patients.
Currently, Oticon's tinnitus feature is called Sound Support. It's available in the Alta2, Nera2, Ria2 Pro TI models. Similar to Resound, Oticon also focuses on water sounds, such as ocean, beach, stream, waterfall. You do need a streamer for Oticon, which at this point is only Apple compatible. The Oticon streamer is easy to hook up and looks nice.
Tinnitus Retraining Therapy (TRT)
Tinnitus retraining therapy (TRT) focuses on an educational counseling aspect of working with the patient to retrain their brain (Jastreboff & Hazell, 2004; 2011). Jastreboff and Hazell's studies have shown that the plasticity of the brain can habituate once all the negative connotations associated with the tinnitus are gone. This can be achieved through talk therapy, but more particularly, sound therapy (a low-level broadband sound). TRT is administered over a timeline of 18 to 24 months. Eventually, the goal is to wean the patients off of that low-level broadband sound. It's almost like listening to a masker, or a static-like sound. They also encourage, particularly for our hyperacusis patients, to not protect the ears. I've had hyperacusis patients come to my clinic wearing earmuffs or earplugs because sounds are just too loud. Jastreboff and Hazell are definitely proponents of taking those off and eliminating those negative connotations. One of the difficulties with TRT, although it has been proven to be effective, is the timeline. More specifically, billing can be a challenge. Audiologists typically have a tough time getting reimbursed for these types of procedures.
Considerations for hyperacusis. Many of our hyperacusis patients tend to do quite well with variations of TRT. Just like with our traditional tinnitus patients, a desensitization protocol is extremely important with a gradual increase in sound exposure. We want to avoid the earmuffs or noise-canceling headphones and actively listen to interesting sounds, as opposed to focusing and fixating on the tinnitus. In general, these patients tend to do well with noise generators or a combination device. Take care to protect patients from uncomfortably loud sounds as sometimes that can exacerbate the hyperacusis.
One thing you might want to try is using a hearing instrument with compression. Open fit hearing aids tend to be preferred by patients with hyperacusis because we're getting into those low-level ambient sounds from your environment. The fact that 80% of hearing aids fit today are open instruments is to our advantage in these cases. For patients with hyperacusis, an open fit is something that you would want to consider if the audiogram allows it. If you have a lot of patients with hyperacusis, I have included some hyperacusis management resources at the end of your handout that I would encourage you to explore.
Neuromonics
Neuromonics is another option for patients with tinnitus. Traditional Neuromonics treatment can take some time, but the benefits have been proven. There are four Neuromonics options: Oasis, Haven, Sanctuary, and Refuge (Figure 5).
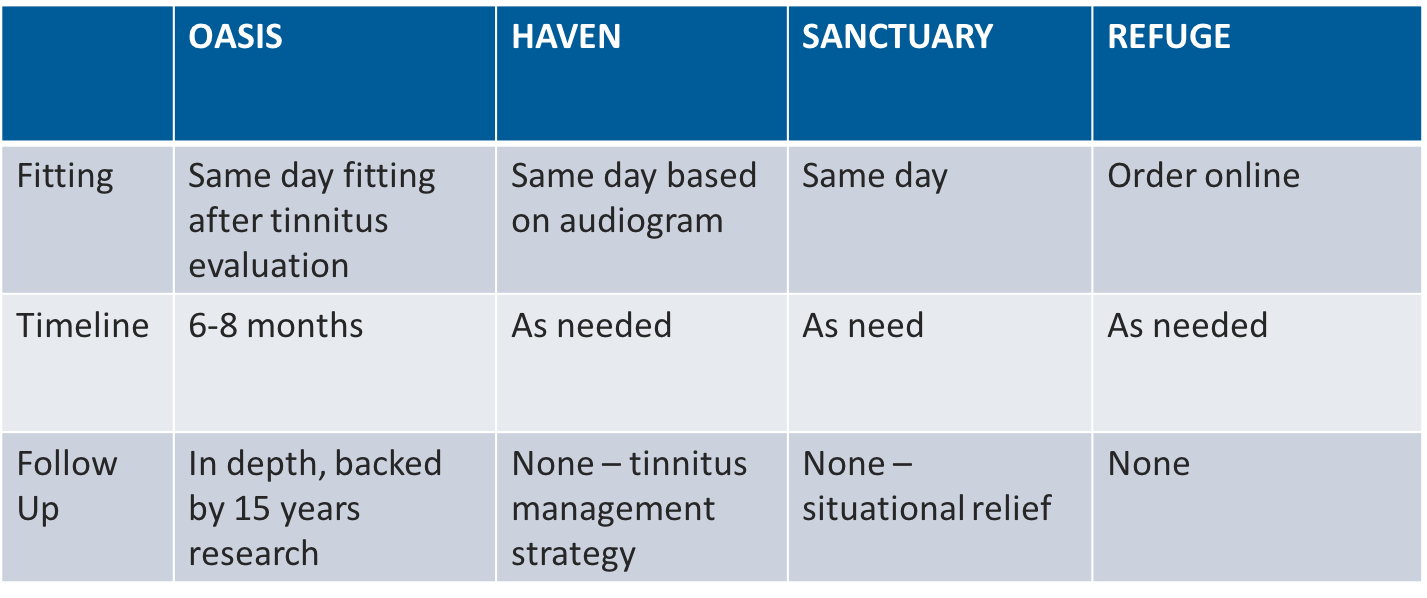
Figure 5. Neuromonics options.
Neuromonics Oasis is the more traditional approach to treating tinnitus. It is a medical device that resembles a Walkman headset. The treatment timeline is six to eight months. Historically, the standard fitting procedure was to do a hearing evaluation and send that information into Neuromonics. They would program the device specifically for the patient by embedding a narrow band noise into four different track options: two that sound like classical music, and two that sound like ambient noise music. Then that would get sent back to the patient. The patient would go through a six- to an eight-month procedure of acoustic desensitization. Every day, they would listen to this device for two hours. Over a couple of weeks, they would reduce the time from two hours to one hour. Then after a couple more months, they would move to an as-needed basis. Today, the Oasis can be fit same-day, but the six- to eight-month timeframe is still recommended. The Oasis device has approximately 15 years of research behind it to support its success. The Neuromonics Oasis device is independent of a hearing aid. If a patient needs amplification, this device is used above-and-beyond the hearing aids. The cost averages anywhere from $1500 to $3000, depending on where you are in the United States. As such, although this method has proven to be a useful and valuable treatment, it has been cost prohibitive for some patients.
In addition to Oasis, Neuromonics has implemented some newer models of tinnitus management devices: Haven, Sanctuary, and Refuge. Specifically, the Refuge can be ordered online without being required to go through an audiologist or a physician. It's supposed to be used on an as-needed basis. At this point, there is not a lot of research behind the Refuge, and when I was putting this presentation together, I couldn't find much information on it. At $300, the Refuge is definitely more cost-effective than the Oasis. The device uses one of three basic audiometric configurations and they embed the signal in there. It resembles a little desktop speaker. It also comes with a pair of headphones. The Refuge could be a cost-effective way of managing a patient's tinnitus.
Sound Cure
Another management option that's similar to Neuromonics is Sound Cure. Sound Cure is newer to the market within the last eight to 10 years. It was developed at UC Irvine, based off of one case study on a cochlear implant patient who had high-pitched tinnitus that was affecting his quality of life. The patient, who had a profound hearing loss, was implanted on one side to help alleviate his tinnitus. Initially, the implant caused his tinnitus to become worse. Doctors went back in to see what was the problem. By accident, they tried what they called an "S" tone: a low rate stimulus that almost sounds like clicking. During the first minute and a half of playing this tone, nothing happened. The patient was still hearing their tinnitus. At about the 180 second mark, all of a sudden, the patient's tinnitus went away. For the first time in two years, he could not hear any of the high-pitched tinnitus. All he heard was a calming, pleasant tone produced by the low-rate stimulus. Sound Cure's research is based on that first case study, and they've had several studies since that time. Sound Cure is a little bit more cost-effective than Neuromonics. For people who don't prefer the music sounds of Neuromonics, Sound Cure is a good alternative. The Sound Cure device looks somewhat like a Walkman. It comes with a pair of headphones as well.
Sound Apps
Sound apps are another cost-effective option for your patients. These can be found in iTunes/App Store or in the Google Play store, often for free or at very low cost. There are lots of different apps to choose from. From my experience, I have found the following two apps to be great as far as their flexibility, ease of use, and design.
Relax Melodies: Sleep Sounds. With this app, you can select a wide variety of sounds and melodies that you like, combine them and adjust the volume of each sound to create a mix. One use is to help you relax and enjoy falling asleep, however, it can be used in other situations, such as relaxing at the spa, during yoga or other exercises, or while getting a massage. These sounds can also help your baby fall asleep. You can use a timer with it so it turns off automatically.
White Noise Baby. These sounds are specifically intended to help your baby go to sleep. They have ambient noise choices such as air conditioner, car ride, and train ride. They also have nature sounds, like crickets and waterfalls. You have the option to set a timer. An added benefit of White Noise Baby is if you have a young child, they have a rattle option, so if you shake the phone, it will make a noise like a rattle.
Cognitive Behavioral Therapy (CBT)
Another fantastic option for tinnitus patients is cognitive behavioral therapy (CBT). This is traditionally done by a licensed psychologist or a psychiatrist. It assists the patient in becoming more aware of their negative thoughts. It allows for more of a positive thinking and owning of the situation (Cima, Andersson, Schmidt, & Henry, 2014). This option does require some research on your end to find the right provider that you can refer to. In my experience, it was a bit of a challenge to locate someone who could relate cognitive behavioral therapy to the tinnitus patient. A lot of times, tinnitus patients are similar to patients that have chronic pain. I live in the Chicago area, and I looked up providers on the Cognitive Behavioral Therapy Association website. I went down the list and I looked to see who had experience with pain management, who had experience with tinnitus, and I started calling people. Most of my tinnitus patients ended up being quite successful with a combination of in-office CBT, TRT and using what the hearing aid manufacturers have, in addition to their hearing instrumentation. However, patients who have comorbid psychiatric issues, such as anxiety or depression, may require a little bit more help than others. Having that option to refer to a mental health professional can prove highly beneficial for those individuals.
Mindfulness-Based Tinnitus Relief
For people who live in more rural areas, those who work full time and are constantly on the go, and even people who have a hard time getting off work to make in-person appointments, mindfulness-based tinnitus relief is a wonderful option. Dr. Jennifer Gans is a doctor of psychology in California. She offers an eight-week online course that's done as a group. When you register for part one of her introductory course, you receive a book (Full Catastrophe Living by Jon Kabat-Zinn, Ph.D.), a yoga mat and, of all things, a handful of raisins. What she does is very much like group counseling. You check in once a week with the group and she walks you through some exercises that are based on CBT and TRT philosophies. You also discuss the book. There are small group sessions that also occur throughout this process.
Other Management Options
If you type the words "tinnitus treatment" into a search engine, you will see a wide variety of results, including many over the counter pills, prescription medicines, ear drops and masking devices. There are also holistic and minimally invasive approaches to manage tinnitus.
OTC Pills. The majority of these OTC approaches (e.g., T-Gone, Ginkgo biloba, zinc) are not FDA approved or monitored. Additionally, there are no peer-reviewed publications to back up these claims. I would strongly recommend that you proceed with caution when using OTC pills. In 2014, Flomer and team published an article in the Journal of the American Academy of Audiology that addresses experimental, controversial and futuristic treatments for chronic tinnitus (Folmer, Theodoroff, Martin, & Shi, 2014). Of the studies that have been done, they've been shown to be nothing more than a placebo effect. The correlations are very loose. I do know that some physicians will recommend something like a T-Gone to provide peace of mind for the patient. Again, that's for the physician to decide. As an audiologist, I tended to not recommend these to my patients.
Medicinal approaches. There are medical approaches that do have some peer-reviewed studies behind them, including:
- Cyclandelate (Cyclospasmol) and Eperisone have been shown to slightly reduce tinnitus match levels in a single study.
- Alprazolam (an anti-anxiety drug) may also slightly reduce tinnitus loudness, although these findings were also from a single study, and the drug can cause dependence.
- Studies using Serotonin Reuptake Inhibitors (SSRIs) have shown mixed results in relieving tinnitus. As SSRIs are normally used to treat depression, anxiety and OCD, tinnitus patients with comorbid psychiatric disorders can derive benefit from these drugs by altering their perception of how their tinnitus affects them.
- Nortriptyline: For patients with insomnia
Holistic approaches. Holistic approaches to tinnitus include such things as acupuncture, massage therapy, meditation and wearable magnets. There are also ultrasonic tinnitus treatment devices that act as a bone conductor. You set the device at a low-level hum and hold it up to your forehead or on your mastoid. The two that I'm aware of are the Inhibitor and the Aurex-3 device. However, most patients found the vibrating in those devices to be a turnoff. If you're using a bone conductor, when you get to a certain degree of hearing loss, that's not going to be very effective. Some practitioners in Europe (particularly France and Germany) have been looking at Ginkgo Biloba as a tinnitus treatment. Again, the results point to essentially a placebo effect. (Dobie, 2004; Folmer, Theodoroff, Martin, & Shi, 2014).
With regard to holistic approaches, my philosophy is that if it's not going to be harmful to the patient, go ahead and try it. I had patients that would swear up and down that massage therapy was curing their tinnitus when it was more likely helping them to relax, which in turn would help them sleep a little bit better. They would wake up feeling more rested. Their tinnitus would not be exacerbated by the stress of their sleepless night, so they would get another good night sleep. It's all about breaking that vicious cycle. If any of these can be beneficial to a patient, and they are not harmful to them, it's worth a shot.
Minimally invasive approaches. Some promising up-and-coming minimally invasive approaches to managing tinnitus include:
- Soft Laser Approach: In this approach, a low-powered laser shot into the patient's ear canal. The original study showed some promise of lowering the impact of tinnitus on the patient, but it failed to have a control group and could not be replicated.
- Transcranial Magnetic Stimulation (TMS): With TMS, a low-frequency electromagnetic pulse is sent through the skull. This study was based on some fMRI studies that have shown people with tinnitus have more activity in their auditory cortex. The study had a small number of participants that did show improvement, but not enough to start recommending this to patients.
- Transcranial Direct Current Stimulation (tDCS): With this approach, there are electrodes applied to the skull which stimulate the left temporal parietal area. With their study, they were able to show a significant immediate decrease in tinnitus perception, however, the results have not yet been replicated.
I have included many additional resources in the handout that accompanies this course. I have listed some direct links to the Beck Depression Inventory, the PTSD screening, and the Spuelberger State-Trait Anxiety Inventory. I have also listed some hyperacusis resources if you would like to learn more about that topic, as well as links to each of the six hearing aid companies, the sound therapy companies, Neuromonics and SoundCure.
Conclusion
In conclusion, there are different ways to manage tinnitus. Not every tinnitus patient is the same. The best course of action is to keep revisiting and adding to the tinnitus toolbox. Perhaps some of the fMRI studies will show that the transcranial electricity methods are working. Maybe we can find an effective cure for tinnitus in a pill form. The best we can do right now is to try to stay on top of that research and always be open to adding (or removing items from our Tinnitus Toolbox.
References
Cima, R. F., Andersson, G., Schmidt, C. J., & Henry, J. A. (2014). Cognitive-behavioral treatments for tinnitus: a review of the literature. Journal of the American Academy of Audiology, 25(1), 29-61.
Dobie, R. A. (2004). Clinical trials and drug therapy for tinnitus. In J.B. Snow (Ed.), Tinnitus theory and management (pp 266-277). Lewiston, NY: BC Decker.
Folmer, R. L., Theodoroff, S. M., Martin, W. H., & Shi, Y. (2014). Experimental, controversial, and futuristic treatments for chronic tinnitus. Journal of the American Academy of Audiology, 25(1), 106-125.
Henry, J. A., Zaugg, T. L., & Schechter, M. A. (2005). Clinical guide for audiologic tinnitus management I: Assessment. American Journal of Audiology, 14(1), 21-48.
Henry, J. A., Roberts, L. E., Caspary, D. M., Theodoroff, S. M., & Salvi, R. J. (2014). Underlying mechanisms of tinnitus: review and clinical implications. Journal of the American Academy of Audiology, 25(1), 5-22.
Jastreboff, P. J., & Hazell, J. W. (2004). Tinnitus retraining therapy: Implementing the neurophysical model. Cambridge University Press.
Jastreboff, P. J. (2011). Tinnitus retraining therapy. In Textbook of tinnitus (pp. 575-596). Springer, New York, NY.
McCombe, A., Baguley, D., Coles, R., McKenna, L., McKinney, C., & Windle‐Taylor, P. (2001). Guidelines for the grading of tinnitus severity: the results of a working group commissioned by the British Association of Otolaryngologists, Head and Neck Surgeons, 1999. Clinical Otolaryngology & Allied Sciences, 26(5), 388-393.
Newman, C. W., Jacobson, G. P., & Spitzer, J. B. (1996). Development of the tinnitus handicap inventory. Archives of Otolaryngology–Head & Neck Surgery, 122(2), 143-148.
Sanchez, C. & Switalski, W (2015). Tinnitus Assessment: the key to successful tinnitus patient management. White paper. Otometrics.
Sanchez, C. & Switalski, W (2015). Tinnitus patient management for today’s audiologists. Audiology Today, 27(2), 14-21.
Shi, Y., Robb, M. J., & Michaelides, E. M. (2014). Medical management of tinnitus: role of the physician. Journal of the American Academy of Audiology, 25(1), 23-28.
Sweetow, R. W., & Sabes, J. H. (2010). An overview of common procedures for the management of tinnitus patients. The Hearing Journal, 63(11), 11-12.
Tyler et al (2009). Tinnitus and Hyperacusis. In Katz, Medwetsky, Burkard & Hood (Eds.), Handbook of Clinical Audiology(pp. 726-742). Philadelphia: Wolters Kluwer Health.
Citation
Young, B. (2018). Tinnitus toolbox. AudiologyOnline, Article 23587. Retrieved from https://www.audiologyonline.com


