This is an edited transcript of a live webinar. Download supplemental course materials: Astera2 quick guide; course handout.
Learning Objectives
- After this course learners will be able to demonstrate the components of a tinnitus evaluation.
- After this course learners will be able to describe the Tinnitus Evaluation Tools within the Madsen Astera2.
- After this course learners will be able to explain how tinnitus evaluation can be effectively and efficiently implemented in their clinic.
Introduction
Dr. Wendy Switalski: Today’s focus is on tinnitus evaluation components and the implementation within the Madsen Astera2 audiometer. Then we will drill down into the tinnitus module. There is a bit of overlap between tinnitus evaluation and what can be done in the audiometer modules. I would like to also give you a look at our Loudness Scaling Module, which can be helpful for tinnitus assessment.
Why Evaluate Tinnitus?
While there are many tinnitus services that can be provided without the formal evaluation, performing the evaluation allows us to quantify the characteristics of the patient’s tinnitus. It can help us identify patients who need mental health or other forms of support beyond audiological services, set a baseline for future improvements or fluctuation, and help acknowledge the realness of tinnitus, which can be a distressing issue that is sometimes unacknowledged by hearing care or medical professionals. It can begin the dialogue necessary for treatment. While it does not necessarily give you all of the pieces you need for working with tinnitus patients, it is a great place to start.
Why are these evaluations not used more commonly? I think the time involved, the perceived complexity, and the unfamiliarity with some of these options have been barriers. Furthermore, we had limited treatment options for so long; it was difficult to evaluate a condition for which professionals had few resources at their disposal for treatment. With an abundance of treatment options and technology in the form of sound generators currently available, we see a renewed interest in tinnitus evaluation.
In 2013, Otometrics recognized the need to optimize this clinical process and launched the Tinnitus Module within the Astera and the Astera2. This integrated module provides all the tools necessary to add tinnitus evaluation to your clinical test procedures without making significant changes to your work flow. The module includes psychoacoustic tests, questionnaires, and a dedicated tinnitus report. If you currently have an Astera system, this is available as a no-charge software upgrade. Contact your representative or Audiology Systems directly to get this upgrade in your clinic. The tinnitus module removes some of the barriers we discussed to make evaluations easy and efficient to implement.
OTOSuite Overview
I want to give a brief overview of the OTOsuite software platform, which serves as the foundation for all of our diagnostic and fitting products. The software package operates as a module under NOAH. It allows you to connect and synchronize your test results across devices. It improves your work flow by reducing data entry, and it ensures that your hardware investments stay relevant by using software updates which are often provided at no charge. The Tinnitus Module is one of those; the QuickSIN test is another. The product routinely has software upgrades that allow you to enhance your workflow without replacing your equipment. It also offers you electronic data storage via NOAH or our OTObase EMR (electronic medical record) system.
Audiological Components
The components of the audiological evaluation are standard audiometry, loudness discomfort levels, high-frequency audiometry and otoacoustic emissions. While we will not go into detail on the evaluation for the loudness discomfort levels, know that it is a precursory component to the tinnitus evaluation. Likewise, we will not discuss otoacoustic emissions today, but they add additional information to the intake for tinnitus patients, especially those with normal hearing levels.
We will talk about tinnitus surveys and questionnaires, the psychoacoustic tinnitus evaluation component, as well as loudness scaling.
Audiometric Evaluation: Audiometer
Let’s start with the audiometer, as those technological components are important to the tinnitus evaluation. The Astera2 audiometer is a two-channel, PC-based audiometer that can be controlled by the keyboard, the mouse, touch-screen monitor or audiometer control panel. It can allow you to integrate all of your audiometry and immittance data within NOAH.
The Astera2 also includes a full range of testing capabilities, including integrated speech files, high-frequency testing out to 20000Hz, loudness scaling, and a pediatric module with integrated visual reinforcement audiometry (VRA). All of this operates as a module underneath NOAH. You can open sessions just like you would open hearing aid programming sessions.
The options of tone testing, speech testing, QuickSIN, LipRead, Tinnitus, transducer choices and ear selection are all easily accessible. The information is easy to look at and can be compared to previous sessions. If you have patients with progressive hearing loss as well as tinnitus, you can easily show them changes over time as treatments are successfully implemented for their tinnitus and hyperacusis.
High-Frequency Audiometry
High-frequency audiometry encompasses any frequencies above 8000 Hz. These thresholds can provide sensitive information about cochlear damage, especially if thresholds are within normal limits for tinnitus patients. Due to output limitations, you may want to test only through 16000 Hz. It is quite important to recognize that the outputs in sound pressure level (SPL) can be very high, even at soft levels. You will want to be cautious with all patients, but especially with tinnitus patients because of their sensitivity to loud sounds at times.
Occasionally, you may need to use high-frequency thresholds for pitch-matching, although most pitch-matching for tinnitus takes places in the 3000 to 4000 Hz range. In the software, you can look at the high frequencies alone, all frequencies together, or the standard frequencies alone.
Tinnitus Evaluation
Surveys and Questionnaires
For many, the surveys, questionnaires, case histories, and interviews are important when working with tinnitus patients. In general, the surveys and questionnaires can be used to both assess the impact of tinnitus on the patient’s life at that point in time and to monitor changes or progress over time. They can also be used to provide guidance on what the next step should be. When looking at implementing or enhancing tinnitus services, surveys and questionnaires can help you determine which patients need further tinnitus evaluation, further medical evaluation, or standard hearing aid services.
The Astera2 includes three widely-used surveys and questionnaires: the Tinnitus Handicap Inventory (THI; Newman, Jacobson, & Spitzer, 1996), the Tinnitus Functional Index (TFI; Meikle, Henry, Griest, Stewart, Abrams, McArdle, et al., 2012), and the Tinnitus and Hearing Survey (THS; Henry, Griest, Zaugg, Thielman, Kaelin, Galvez, et al., 2014). The questionnaires are located in the lower left-hand corner of the Tinnitus Module screen. It is easy to load a new questionnaire or look at previous questionnaires within the NOAH file. These questionnaires are not lengthy and are relatively easy to administer.
Tinnitus Handicap Inventory. The THI uses a 25-question inventory to assess the patient’s self-reported handicap. The score that they receive is categorized into a level of handicap from slight/none to severe. That score can help determine the next step for the patient.
Some of the questions are, “Do you feel as though you cannot escape from your tinnitus? Does your tinnitus make you upset?” The patient answers yes, sometimes, or no. Once complete, the patient gets a score based on how many yes, sometimes, and no answers they provide. This score can be converted into a grade class.
A patient with a score from 0 to 36 is considered Grade 1 & 2. For that patient, it is recommended to proceed with a standard hearing instrument evaluation. Patients who fall into Grade 3 are in the moderate category of tinnitus impact, and you can proceed with a tinnitus evaluation and possibly sound treatment. The patients who report a more severe impact, such as those with scores of 58 to 100, may require a referral for a complete medical evaluation or possibly psychological services. Having this rating process can help decide what to do with patients. Many of our patients will report tinnitus during the office visit, but whether it is bothersome or needs to be pursued is not always addressed or evaluated.
Tinnitus Functional Index. The TFI is another 25-question list, but it covers eight different subscales. It looks at what is happening in various aspects of the patient’s life, such as sleep disturbance. You can scale both the severity as well as the negative impact. Like the THI, this also can be used for intake, monitoring over time, and for clinical and research applications.
The scoring is based on a 10-point continuum. For example, “Over the past week, did you feel in control in regards to your tinnitus?” The patient would choose a response based on the 10-point scale, rather than yes, no, or sometimes.
Tinnitus and Hearing Survey. The THS has a slightly different approach, at only 10 questions covering tinnitus and loudness. Many of our patients have hearing loss that accompanies tinnitus. They are not always clear about which is the greater challenge, and this questionnaire can help delineate that. The THS is not validated as a primary outcome measure. If you are looking for an outcome measure to track progress and treatment, it is better to use this as a supplemental measure.
The patient answers questions about how often the tinnitus kept them from sleeping in the last week, but also specifically about hearing and how well they were able to understand in various situations.
While many people many prefer to have their patients complete the questionnaires before their visit, it still may be beneficial to consider them in the software. These can be printed as formal reports for an outside referral source or for the referring physician. It can be provided to the patient, although you may not want them fixating on the scores. You may not always have the patients fill them out within the software, but I think it is beneficial to have that data so we can track it sequentially.
Psychoacoustic Evaluation
Once the questionnaires are complete, we can move into the psychoacoustic evaluation. This is what we normally think of as the tinnitus evaluation.
Pitch Matching
We are going to start with pitch matching. We perform a pitch-matching test by matching the frequency of the patient’s predominant tinnitus tone or tones. It is often found in the 3000 to 4000 Hz range. You can sometimes apply these results for certain sound therapies if you are looking to mask a specific region. We generally measure this ipsilaterally using a forced-choice paradigm. Instead of using tones, you can also use narrowband or FRESH noise, which is a skinny band of noise available in the system.
Pitch matching can be challenging and it can vary from session to session. It can be confused with loudness, and sometimes a patient may match their tinnitus to the octave below their frequency point. We have built in an octave test that you can use as a cross check.
Loudness Matching
Once we have determined the frequency of the tone(s), our next step is to match the perceived volume of the patient’s tinnitus. It is often only a few decibels above their hearing thresholds. This can be enlightening for a patient because even if they perceive their tinnitus to be quite severe, sometimes seeing that it is not that far above their threshold may provide them with a different viewpoint. We perform this by using the pitch-matched tone and an ascending technique in increments of 1 to 2 dB. You will use multiple trials to obtain a final match, just as you would when determining hearing threshold.
Minimum Masking Level
Once we have looked at pitch and loudness, we need to determine if the patient’s tinnitus can be masked. If it can, we need to determine the minimum intensity we can use to effectively mask the tinnitus. This can provide information about whether masking may be a useful treatment option. Occasionally, it may point out that a patient has a negative response to the presentation of noise. The minimum masking level can be measured by presenting the pitch-matched frequency under a narrow band of noise or white noise. You may often reach a plateau before full masking is achieved. Make a decision as to what you are looking for. Are you looking for complete masking or just the point where masking starts to occur? It is important to use caution with masking, as we need to keep in mind the patient’s comfort or discomfort levels.
Residual Inhibition
Next, we look at residual inhibition. This measures the change in perception, if any, after a 60-second presentation of masking noise. We record the time that that effect took place. This can alert clinicians to patients who have a rebound effect - where tinnitus worsens following the application of masking noise. Those patients would not good candidates for masking sound therapy.
To do the test, we present a broadband noise at the minimum masking level for 60 seconds. The patient is asked to report on when their tinnitus returns to normal, as well as what the quality or impact the noise had on their tinnitus. In the system, they press the response button or tell the tester when then tinnitus has returned. When the button is pressed, the response time is automatically recorded in the system and populated into the report. Sometimes the introduction of this noise may completely mask the tinnitus and other times it may only partially mask it or lessen the volume of the tinnitus.
Astera2 Tinnitus Module
Now that we have laid out those components, I would like to describe how to access them in the Astera2 control panel. As in in the audiometer control panel, we have some choices about what stimuli and transducers we would like to use and which ear to test. We also have some special test options.
When you are performing tinnitus evaluations, 5 dB increments are often not satisfactory; we need the option of 1 or 2 dB increments. The same is true with frequency resolution. Standard frequency resolution will not get us as close as we want to get. This module lets you take frequency down to as small as a 1 Hz resolution. While many of us would not have the clinical time to do that, it is available. We also have a built-in residual inhibition player that allows you to present noise for a guaranteed 60 seconds and record the patient’s response when the inhibition ends.
The tinnitus table is always shown on the right-hand side of the Tinnitus Module screen. It is a step-by-step work flow for you to follow during your tinnitus evaluation. If a patient has previous tinnitus evaluations, you can compare their pitch and loudness matching over time.
We also have the octave button as I mentioned during pitch matching. Most of us can calculate above or below one octave without any problem for standard octave testing, but once we start to break it down into 1/6 and 1/12 octaves, it can be more challenging
The components in the data table meet and support the requirements for tinnitus evaluation, CPT code 92625. For further information on billing, I recommend that you refer to your billing department or to our professional organizations.
Once the evaluation is complete, you can generate a tinnitus report, which can serve a few purposes. First of all, it shows the audiogram with tinnitus measures included. It also serves as documentation for billing purposes. You can easily send this out to a referring source, and it presents a comprehensive and professional view of the services that you are providing. You can also attach any questionnaires that the patient completed.
As a note, our tinnitus evaluation module is accessed through the Tinnitus tab. We do not always perform tinnitus evaluations on the same day as the audiometric evaluation. If this is the case, the thresholds would carry over into your new session, and the date would indicate when the thresholds were measured.
Loudness Scaling
Generally speaking, loudness scaling has been cumbersome and time consuming relative to the information obtained. Implementing this with an easy method helps put this at the hands of the clinician. The Loudness Scaling Module (Figure 1) displays the audiogram in a different view. The patient’s thresholds, while they are not shown, are indicated by the top line where the white meets the gray, and the patient’s uncomfortable loudness levels (UCLs) are indicated by bottom line where the white meets the gray. The white area indicates the patient’s dynamic range.
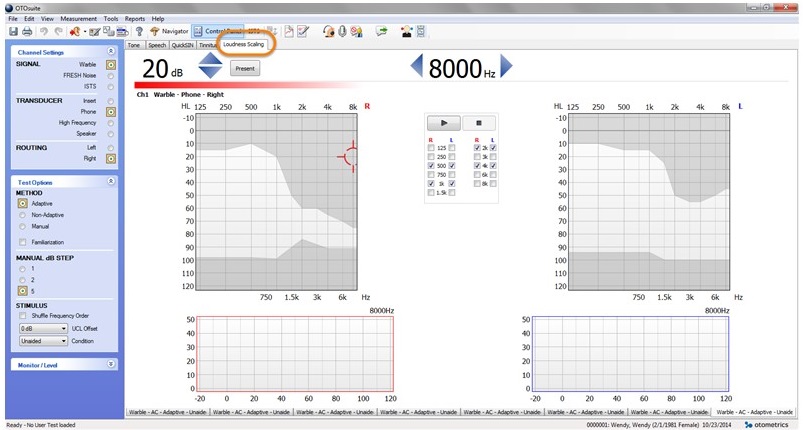
Figure 1. Loudness Scaling Module home screen.
We have the same test options as the tinnitus and audiological modules, although some areas are slightly modified. First, choose what kind of tone or noise you want to use, how you want to route the signal, and what method you want to use. An adaptive method allows you to let the audiometry decide what the next step is based on the patient’s results.
It is also very important to have the UCL offset option. Many patients with a reduced dynamic range may be uncomfortable or even fearful of loud sounds. You can determine the UCL offset so the system will never loudness scale above the UCL offset. You can set it to be equal to the UCL or up to as much as -30 dB. For patients who have tolerance issues, you can give them some reassurance that these noises that they will hear will not rise anywhere close to a point where they are uncomfortable.
You also make a determination in the system of what categorization you want the patient to use when responding for their loudness scaling. There are both 7-point and 11 category choices. The patient can respond on a separate touch-screen inside your booth, or you can give them a laminated card with the choices and they can verbally tell you. You will also pick the frequencies on which you want to focus and the ear or ears you will test.
Once you complete the loudness scaling, the system will generate a loudness growth curve that can be compared to sample data or your clinic norms. Again, you can also print a report, and the data is also stored in their NOAH chart.
Conclusion
The Astera2 provide a simplified, streamlined module to help you continue or begin to conduct tinnitus evaluations in your clinic. Each test will be included in a professional report that can be sent to referring physicians or other specialists involved in the patient’s care. Please let us know if you would like more information or training on the Astera Tinnitus Module or the Loudness Scaling Module.
Questions and Answers
Can you chart on the report?
You have the capability to free-text in a paragraph box that can serve as your report. It will print at the top of the tinnitus, audiometric, or loudness scaling evaluations.
Will the residual inhibition turn off on its own?
The 60-second player does turn off on its own. Once you press play, it generates noise for 60 seconds and then stops on its own. It will wait for a response from the patient’s button or for you to press stop to indicate that the inhibition has stopped. That does require the patient’s input.
Can you use a stimulus other than a pure tone for pitch matching or masking?
The choices you have for matching and for masking are not just tone and warble, but also white noise, narrowband noise, and then what we call FRESH noise, which is a skinny, narrowband noise. It is sort of a blend of tone and noise together. You can use other stimuli and compare one stimulus to another. Those are all built-in options in the system.
What languages are available for the THI?
The TFI and the THS are available in English. The THI is available in English, Cantonese, Mandarin, Spanish, French, Italian, and Swedish.
What two data points do you need to get the T on the tinnitus audiogram?
The tinnitus audiogram needs both the pitch and the loudness match levels in order to plot the T. The tinnitus match is not just available in HL, but also in SL.
If you have other equipment, can you make reports similar to the tinnitus tab? What choices do you have for audiological evaluations?
Within the OTOsuite software, you have reports for every component and piece of equipment that you use through OTOsuite. You have a variety of choices for audiological evaluation as well as real-ear and immittance. You can do combined reporting between audiometry and your immittance as well.
If you already have the module, can you get additional training on residual inhibition?
Absolutely. The quick guide attached to this presentation does walk through each component of the system and can provide you additional training as well as additional resources. Our audiology team or your field team that can help you with that training as well.
Is there a paper manual?
Yes. The quick guide supplements the paper manual, but is probably a better guide because it walks you through the process. There is a manual for the module as well.
Why is loudness scaling important?
Putting loudness scaling in people’s hands can present you the opportunity to look at this more routinely for patients who may not necessarily give you much information otherwise to suggest that they are sound sensitive. Loudness scaling may help you find some of those patients with sound tolerance issues. Even if you are not doing a formal tinnitus assessment, doing a quick loudness scaling test on a hearing aid patient at a couple of points on the audiogram could help you discover sound sensitivities that you would not have otherwise predicted.
What is the binaural section in the tinnitus tab? There was right, left, and binaural.
If you wanted to look at the effect of binaural masking or matching, that is an option. I have also used that selection as another comparison. If I wanted to look at matching with a tone versus matching with a narrow band noise, then can use that as an extra data bank as well.
What is under the CPT code 92625?
That is the code for tinnitus evaluation. It encompasses pitch matching, loudness matching, maskability, and residual inhibition. Questionnaires are not part of that CPT code.
Can you bill tinnitus and audiometric evaluations on the same day?
I am not sure. I would suggest that you check with your billing department. To my knowledge, there is no indication that you cannot. However, I would not want to answer that question without having it confirmed.
I want to start a tinnitus clinic. What organizations are there for tinnitus?
The American Tinnitus Association is a great organization for patients, but there are also tinnitus organizations for professionals. If you Google search or look on AudiologyOnline, you will find numerous training programs for people who want to start adding this to their clinic. I think it is an important way to add services and differentiate yourself as well. With all the treatment options available, it is a good time to do this.
What is the rebound effect?
The rebound effect is something that can happen following the presentation of masking where patients perceive their tinnitus becomes louder for a short period of time. It is somewhat rare, but it is important to be able to determine if a patient has that.
What about testing people with reduced dynamic range?
Any time you test patients with reduced dynamic range, use an ascending technique and be very careful to not exceed their uncomfortable loudness levels. You can reduce the step size by 1 or 2 dB increments.
References
Henry, J. A., Griest, S. A., Zaugg, T. L., Thielman, E., Kaelin, C., Galvez, G., et al. (2014). Tinnitus and Hearing Survey: A screening tool to differentiate bothersome tinnitus from hearing difficulties. American Journal of Audiology, Epub ahead of print. doi: 10.1044/2014_AJA-14-0042.
Newman, C.W., Jacobson, G.P., & Spitzer, J.B. (1996). Development of the Tinnitus Handicap Inventory. Archives of Otolaryngology, 122, 143-148.
Meikle, M. B., Henry, J. A., Griest, S. A., Stewart, B. J., Abrams, H. B., McArdle, R., et al. (2012). The tinnitus functional index: development of a new clinical measure for chronic, intrusive tinnitus. Ear and Hearing, 33(2), 153-176. doi: 10.1097/AUD.0b013e31822f67c0.
Cite this Content as:
Switalski, W. (2015, March). Tinnitus evaluation outside the tinnitus specialty clinic: using the Astera2 Tinnitus Module. AudiologyOnline, Article 13567. Retrieved from https://www.audiologyonline.com.