Editor’s Note: This text course is an edited transcript of a live webinar. Download supplemental course materials.
In this course today, I’ll talk about what tinnitus is, what causes it, how it impacts patients, the difference between tinnitus treatment and tinnitus management, and what you can do to start offering tinnitus services.
What is Tinnitus?
Tinnitus is from the Latin word tinnire, which means to ring or chime. Tinnitus presents as ringing, hissing, humming, buzzing, roaring, crackling, sizzling, wooshing, howling, and/or grinding. In fact, we once did an informal survey and received over 120 different reported perceptions of tinnitus. It is not ringing only, although that is probably the most common perception. The perception of the sound occurs for the patient only, often in the absence of some kind of external stimulus.
Objective tinnitus has a mechanical source, and this can be due to a constriction of blood flow or spasms of the middle ear muscle, or patent Eustachian tubes. These etiologies tend to be rare, but they are classified as tinnitus. The more common experience is subjective tinnitus, where the sound comes from a physiological but non-mechanical source. Our best guess is that it is neural signals interpreted by the brain as sound, not unlike phantom limb pain, where a person loses a limb and the brain receives signals from the damaged nerve endings and creates a perception of touch or pain.
Epidemiology
One study (Shargorodsky, 2010) looking at the National Health and Nutrition Examination Surveys (NHANES) between 1999 and 2004 found that a little over 25% of people, slightly more men than women, report that they have tinnitus. That equates to over 80 million people in the United States. Those that reported frequent tinnitus were more men than women, but the total came to about 8%, or approximately 24 million people in the United States. Those numbers suggest a horribly underserved population. Factors that increased the likelihood of having frequent tinnitus were if you are white, over 40, a smoker, hypertensive, diabetic, overweight, have cholesterol, noise exposure, a major depressive disorder, a generalized anxiety disorder, and/or existing hearing loss.
We also know that noise is a precipitating factor (Meikle, Creedon, Griest, 2004; Mrena, Paakkonen, Back, Pirvola, & Ylikoski, 2004; Griest & Bishop, 1998). In adults, we find that sudden noise exposures, bursts, transient sounds, explosions, gun shots, even back-firing of cars or prolonged sounds or being around sounds for a long periods of time are the most commonly reported factors related from the patient’s view of the onset of tinnitus. I found it interesting that people report tinnitus in 90% of acoustic trauma events. A 15-year longitudinal study by Griest and Bishop (1998) found that the early indicator of impending permanent noise-induced hearing loss was the presence or the onset of tinnitus. Noise and tinnitus are highly related. The nice thing is that we can prevent almost 100% of noise-induced hearing loss, and therefore, we are in the position to delay or lessen the onset of tinnitus.
Studies also show that tinnitus is present in children. Holgers (2003) found that about 12% of seven-year-olds have tinnitus. Although this is a difficult age group to study, children do experience it, and 2.5% said it was after a loud sound. Coelho et al. (2007) found in their 5 to 12-year-old group that 37.5% experienced a tinnitus sensation, and almost 20% reported that they suffered from it. Noise exposure was a significant factor in that study as well. A study we conducted (Martin el at., 2011) looked at almost 2,000 9 to 11-year-olds. We asked them if they ever experienced ringing or other noises in their ears or head. Forty-seven percent of them said between sometimes and always. Children may think it is normal, so they do not report it.
What Causes Tinnitus?
There are usually two phases that produce tinnitus. One is the induction or trigger that starts the tinnitus. This is usually some kind of pathology or damage in the peripheral system that results in an imbalance in activity in the central nervous system. It triggers abnormal spontaneous neural activity and produces the tinnitus perception. The second phase is maintenance, which is the long-term central auditory process that keep the tinnitus going and makes it problematic over time. We find that well over 90% of sudden-onset incidences of tinnitus resolve spontaneously during the first year. For the ones that do not resolve, they persist for long periods of time and are very problematic.
Peripheral Triggers
Peripheral triggers include cochlear damage at the top of the list; this can be from noise or anything else that happens to the ear. Another is head and neck injury. When we were in Portland, we saw over 1,000 patients whose history pointed to head and neck injury as the trigger for tinnitus. TMJ (temporomandibular joint) problems seem to be implicated as a possible trigger, and there are probably many other things that have not yet been proven as well.
Central Triggers
Central triggers are things that occur in the higher centers of the body like metabolic issues, neural disease, and stress. Most of the time when the stress goes away, the tinnitus does as well. Another central triggers is brain injury. Again, there are likely dozens of central triggers that can cause it. It is a very complex, multifactorial disorder that makes it more difficult to identify treatments and cures.
Long-term Effects
Once there is deafferentation from a hearing loss, the brain creates imbalances, or thalamocortical disrhythmias. Cytotoxicity is another long-term consequence of noise exposure. The delicate balance between excitatory and inhibitory neural activity is disrupted; once that is triggered, treatment-resistant neurologic disorders begin to surface, and one of those is likely tinnitus. Cortical reorganization is another long-term effect.
In What Ways does Tinnitus Impact the Patient’s Life?
Tinnitus impacts the patient’s life in many varied ways. These were the reported difficulties from a patient group that we saw in Portland, and that represented the worst of the worst cases in the United States (Figure 1; Martin et al., 2002). We ended up seeing many patients from all over when other practitioners came to a dead-end in treatment. As you can see in Figure 1, some of the troubles include poor concentration, difficulty in relaxation, irritability, discomfort in quiet, sleep problems, feelings of depression, interference with work or social activities, and more. Over two-thirds of our patients came in with multiple problems in these areas. Keep in mind that these patients are devastated psychologically, emotionally, and often socially. They are in bad shape when they show up at the clinic.
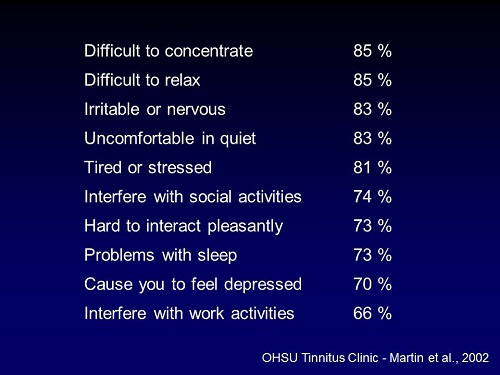
Figure 1. Various impacts of tinnitus on patients’ lives (Martin, et al., 2002).
Why does Tinnitus Become a Problem?
In 1990, Jastreboff explained the neurophysiological model of tinnitus. Typically, external sounds stimulate the cochlea, travel along the auditory nerve, and then the subcortical areas of the brainstem detect those sounds. The information is passed on to the cortex, where it perceives, evaluates, differentiates, discriminates, and performs associated higher tasks. But it does not stop there. Sounds can trigger emotional associations in the limbic system. We can have both positive and negative reactions to sound, as well as ones that evoke historical memories. We might hear a song and it reminds us of our first boyfriend or girlfriend. Screeching brakes may remind us of a terrible car accident.
One of the emotional associations we can experience can be annoyance, such as a barking dog next door. This triggers our sympathetic nervous system, and we get physiological responses. These sounds create feedback loops within our system. When we are annoyed and the sympathetic system is activated, the emotional associations and reactions are stronger. This is what makes us able to detect these sounds in background noise and other contexts. The feedback loop becomes self-perpetuating and creates a problem that is very difficult to address. Many times it is new and frightening.
Our sensory gating, or the hierarchical processing of sensory information, seems to go awry, and the tinnitus is always at the forefront of our perception. It is the only thing we can hear, so it is the only thing we can think about. We reinforce the sound by listening to it, talking about it, monitoring it, measuring it, writing about and charting it. Negative counseling from physicians who say there is nothing that can be done about it or that it might be something like a brain tumor feed back into the problematic aspects of tinnitus and make it more difficult to deal with.
Tinnitus Treatment
People want to know if tinnitus be cured. The premise of medical treatment is to medically or surgically resolve any active disease processes. If there is an active disease process that causes the tinnitus and we can eliminate it, then yes, we have cured the tinnitus. There are issues that can be treated medically or surgically that will make it go away. Whenever possible, active disease processes should be identified and treated prior to tinnitus management.
The flow of tinnitus patients often follow a similar pattern. Most individuals begin their journey with bothersome tinnitus that prompts them go to an Ear, Nose & Throat (ENT) or family doctor. That doctor’s job is to decide whether or not there is an active disease process, and if there is, if can it be treated medically or surgically.
Active Diseases Process
If there is an active disease process, we must consider if there is objective tinnitus, which can be the result of a host of treatable problems (Figure 2). Some of them are mechanical disorders, while others are vascular disorders.
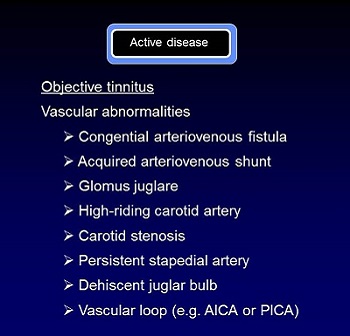
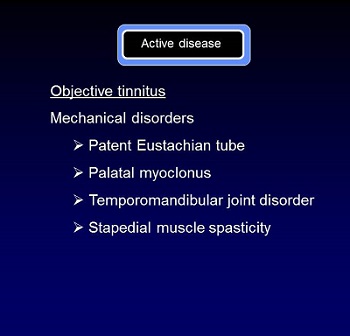
Figure 2. Vascular and mechanical disorders that can cause objective tinnitus.
Subjective tinnitus also results from different types of active disease processes (Figure 3), many of which can be treated medically or surgically. In some cases, genetic predisposition cannot be treated. Ototoxicity cannot be treated. Vascular hypertension sometimes can be treated. Head and neck disorders that cause tinnitus are less likely to be treatable.
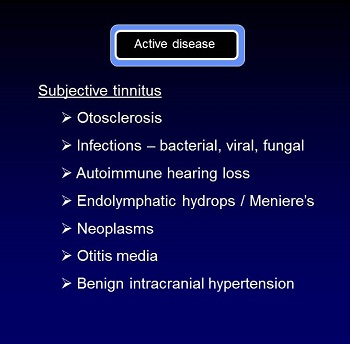
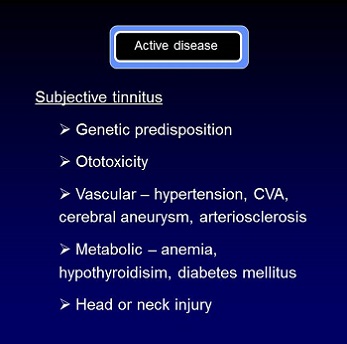
Figure 3. Common causes of subjective tinnitus.
No Active Disease Process
If treatment resolves the tinnitus completely, we are done. If there is no active disease process, but the symptoms persist, there is a problem. Tinnitus in these cases manifests much like the phantom limb pain. Figure 4 summarizes some of the disorders associated with subjective tinnitus in the absence of an active disease process. The physician will say that there is nothing he can do for the patient. That really means that the physician has no treatment for the static medical condition the patient has.
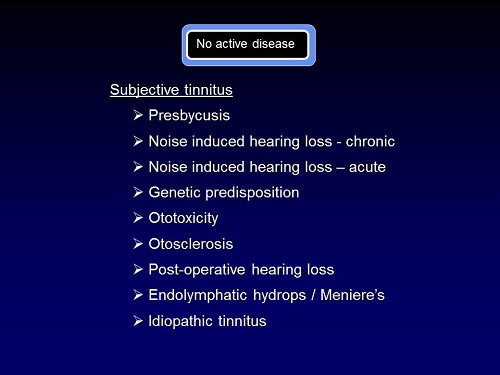
Figure 4. Disorders associated with subjective tinnitus in the absence of an active disease process
Tinnitus Management: Where to Start?
If treatment fails or if there is no active disease process, then we move from a treatment model into a tinnitus management model. A simple paper (Folmer, Martin, & Shi, 2004) published in The Journal of Family Practice can help physicians understand their role in the tinnitus treatment process. This can be distributed to physicians you know in your area. Their role is very important in identifying and treating those processes, but the article also explains tinnitus management in a way that will help them understand that they can still pass the patient on to someone else after their course of evaluation and diagnosis is complete. Hopefully, that professional would be you.
The treatment of chronic tinnitus can be better described in terms of management rather than a cure. The goal of the management program is to reduce the perception of and the reaction to tinnitus until it is no longer a controlling factor in the person’s life. If we cannot make it go away, we have to at least be creative in giving the individual long-term relief and control over their life again.
When you are starting out on a sailing journey, you need several things. You need a captain, a ship, a map, a sextant to navigate, supplies, a crew, and funding. We are going to talk about all those things.
Tinnitus Specialist: The Captain
The captain of the tinnitus team has to be the tinnitus specialist. I use that term specifically, because it is not just an audiologist. It often exceeds the realm of traditional audiology in order to produce effective management results. Figure 5 outlines the roles of the tinnitus specialist.
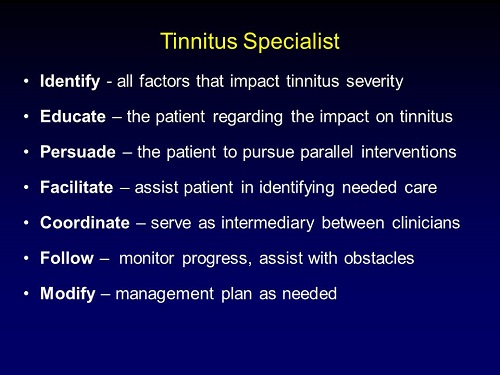
Figure 5. Roles of the tinnitus specialist.
First, the tinnitus specialist uses case histories, tinnitus severity indices and test results to identify all of the factors that impact the severity of the tinnitus. It is more than loudness. The second issue is to educate. One of the important jobs is to educate the patient and family as to the impact of these factors on tinnitus, otherwise they are not going to be willing to deal with them. You take an educational role in helping them understand how the brain works, how the limbic system ties into making the sound bigger than life, and how tinnitus problematic and distracting to the point where they feel they have lost control of their lives.
Next, the tinnitus specialist must persuade the patient to pursue parallel interventions, which may include things that they never wanted to do in their life, but will be necessary to get relief from their tinnitus. For example, you may have people that come in, not because they have a hearing problem, but because their ears are ringing, although they do have hearing loss. They do not want anything to do with hearing aids. However, when they try them for a demonstration in the office, they find that they get better hearing and some immediate relief from their tinnitus.
Some individuals become so depressed that they become self-destructive. You may have to persuade them to see a psychiatrist or psychologist. A lot of our patients are very reluctant to do these types of additional interventions. Your role is to help them understand how those will lessen the load of the tinnitus and make the acoustic interventions much more effective.
The tinnitus specialist is a facilitator. Part of what you are going to do is help the patient identify the needed care. You may have to line them up with other professional caregivers, or if they are from a different area, you may need to refer them to an audiologist who is capable of being creative with devices to help them in a way that they need. You may have to help them with their job situation. We have had to be intermediaries with people’s managers at work and help advocate for them to change their job structure in such a way that the environment would not exacerbate the person’s tinnitus every day.
You will coordinate patient care and serve as the intermediary between the ENT specialist, endocrinologist, neurologist, psychiatrist and psychologist. There is no one else designated in the health care system to do that.
The tinnitus specialist does follow-up. Patients often will voluntarily follow up and contact you, but sometimes you are going to have to initiate that. No news is not always good news. It could mean that they are doing fine on their own, but it can also mean that they have been frustrated, run into obstacles that they cannot overcome, or they have given up.
Finally, the specialist is going to be the modifier. You are going to look at the whole management plan and continually evaluate whether or not the things that you are trying are working. We often start with the simplest, least expensive interventions possible, and then get more expensive and more aggressive as time goes on.
The Clinic Environment: The Ship
Your clinic is your ship. To start, you do not need a lot. You need a test booth and a place to do counseling and education. It is nice if that space is large enough to accommodate family members and close friends, as they play an important role in the evaluation and management of that patient. A medical exam room would be a good addition for later if you will have a physician involved in the practice. As you start to deal with more complex patients, the role of the physician as part of the tinnitus team becomes much more critical.
For equipment, you will need standard audiometric test equipment. You are going to need hearing aid fitting and verification equipment. Devices for acoustic therapy are very important. Later on, it would be beneficial to have a specialized tinnitus matching system, but you can use your standard audiometer to get ballpark figures of the estimated pitch and loudness of the tinnitus.
Charting a Tinnitus Protocol: The Map
Choosing a course for your tinnitus management protocol can be varied, as there are many strategies available such as Neuromonics, Tinnitus Retraining Therapy (TRT), or cognitive behavioral therapy? I recommend that you start simple. Jim Henry, Tara Zaugg, Paula Myers and Caroline Kendall developed the Progressive Tinnitus Management (PTM) program for the Veteran’s Affairs department, comprised of three books. One is a clinical handbook for audiologists, one is a step-by-step workbook, which is good for determining the starting point, and one is a counseling guide. It is a system that starts with simple steps and takes you through a progression of treatment. The PDF files of all their material can be downloaded for free (https://www.ncrar.research.va.gov/education/documents/tinnitusdocuments/index.asp). It is a simple way to start before getting into the other different permutations of behavioral therapy and habituation therapy. It breaks down the program into five levels of tinnitus management.
Five Levels of Tinnitus Management
The first differentiation is between bothersome and non-bothersome tinnitus. About three-quarters of people with tinnitus are not bothered by it. If they are in a quiet room or going to sleep, they hear it, but they do not pay much attention to it. The rest of the population with tinnitus is bothered by it. It prevents them from sleeping. It creates anxiety, insomnia, and depression. Ironically, those very factors exacerbate the tinnitus.
Once a person has bothersome tinnitus, you triage them. Secondly, you do an audiometric evaluation if they are complaining of hearing loss. In fact, if a person reports faint to noticeable tinnitus but no trouble sleeping and no anxiety or depression issues and you diagnose them with hearing loss, a simple thing you can do is to treat the hearing loss with binaural amplification, and a lot of times you will get lucky and the symptoms go away. Start simple.
If they are struggling, group education can be beneficial as the third stage of management. This is different than a support group. We find that support groups vary tremendously in the degree of helpfulness and hurtfulness. If you have a group leader who is good at facilitating communication and information on resources and access to help, that is a good support group. Groups that get together only to rehash how much they are suffering by comparing stories are disaster zones for your patients. Group education explains the neurophysiological model and talks about simple things they can do to improve their quality of life, such as how to avoid complete silence or introduce background stimulation; it gives tips without any other formal intervention.
The fourth stage is interdisciplinary evaluation. If the person has TMJ disorders, a neck injury, or any kind of psychological issues, then you want to bring in the others members of your team to evaluate them.
The fifth level is individualized support. The people who have chronic and multi-faceted problems need intensive, individualized support. This is the highest level of management, where you are custom-applying the sound therapy, psychological therapy, and whatever else they need in an intensive, long-term manner.
How do I know if the Patient is on Course?: The Sextant
When you are out sailing, you need to know whether or not you are headed in the right direction. In the realm of tinnitus, we have questionnaires for that. There are several different types of questionnaires that give you an idea of the impact of the tinnitus on an individual’s life. They can also let you know whether the things you are doing are helpful or not. The four questionnaires I have included are routine tinnitus, hearing, and medical histories, the Modified Beck Depression Inventory, the Anxiety Index, and tinnitus severity indicies.
The Beck Depression Inventory can be obtained online (https://www.beckinstitute.org/beck-inventory-and-scales/). It is a simple scoring tool that lets you know whether or not you need to bring in early psychological and psychiatric help. A score of eight on this inventory indicates moderate depression. We need to pay attention to that.
The State-Trait Anxiety Inventory for Adults is another form you can order online (https://www.mindgarden.com/products/staisad.htm). We find that many of our patients with severe tinnitus have anxiety issues. It is unknown which came first – the anxiety or the tinnitus. It could be that the tinnitus triggered the anxiety, or that a high-strung anxious personality triggered the tinnitus. You will see both.
Tinnitus severity indices are questionnaires that give you a good idea of the impact of tinnitus directly on their lives. The Tinnitus Functional Index (TFI) is probably the new gold standard. It can be download it for free. The Tinnitus Handicap Inventory (THI) is a 25-item questionnaire that can be downloaded for free also. The Tinnitus Handicap Questionnaire (THQ) can be found here, and the Tinnitus Reaction Questionnaire (TRQ) can be obtained here.
I recommend that you use these free resources. The TFI is valuable is because it is not only designed to measure the current tinnitus severity of the patient, but it is also very sensitive to improvements. It is the only questionnaire that has been validated for both the present status and incremental change.
You can also use rated severity indicators to get an estimate of severity (Figure 6). A visual analog scale is a straight line with two ending dots. The patient marks somewhere along the line where they are in severity, which could also be loudness. Visual numerical scales can cover whatever number range you choose, but the same concept applies.
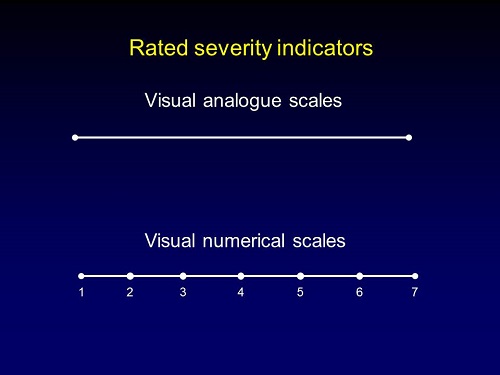
Figure 6. Two examples of severity indicators: visual analog scale (top) and visual numerical scale (bottom).
The rated loudness does not correlate with the matched loudness in decibels. The rated loudness, which is what the patient hears, is going to have a higher correlation with the severity and impact on their lives. We typically use a 0 to 10 scale, and we find that anything over a 6 is often associated with sleep problems and anxiety issues, which puts them in category 5 on the progressive tinnitus management hierarchy.
Tinnitus Management Tools: Supplies
What kind of tinnitus management tools do you need? There are many options to consider, and sometimes your toolbox will depend on your location. As I said before, sometimes amplification is effective. There is a paper by Grant Searchfield et al. (2010) on ways to modify digital amplification programs to be more useful for tinnitus. Amplification is designed as a prosthetic device. We are taught to use hearing aids as devices to replace inferior cochlear function. Tinnitus becomes the secondary purpose of amplification. We use it as a therapeutic device to deliver sounds to the ear that provide relief and can facilitate habituation. Many of the rules for programming hearing aids for someone with tinnitus will be different than if you are using it as a prosthetic device.
Sound Generators
Ear-level sound generators are available. They are small devices, little behind-the-ear hearing aids, which make a gentle background sound that competes with the tinnitus and can provide relief. Combination units combine both amplification and different types of sound generators. If you cannot get a sound that seems to be effective, try a Bluetooth streamer. You can use the patients’ phones, iPods, or MP3 players to bring any kind of sound that proves to be therapeutic through the hearing aids.
Table-top sound generators or a waterfall are used as something to fill the space in the room, especially at night when sleeping. A fan is another item that can be used. Sound pillows have speakers in them that plug into any device to play music, broadband noise, waterfalls or whatever will help them sleep.
Phone Apps
Phone apps are the greatest gift to us as clinicians because there are so many that are inexpensive or free for all the phone platforms. They come under the names of relaxation or meditation apps or nature sounds. You can compile a list of them and have your patients try them out. If they are useful in your acoustic therapy, take advantage of them.
Assembling your Tinnitus Team: The Crew
Recognizing Various Factors for Professionals to Address
There are many different factors that have been shown to either trigger or exacerbate tinnitus, and a team is more effective at addressing varying areas of concern. These areas can include blood pressure, sleep (lack of), anxiety disorders, depression, hearing loss, which may progress over time, stress, continual exposure to excessive noise in work or recreation, and diet. Eating poorly feeds into systemic stress, which will exacerbate tinnitus. Conflicting medications is another one. A person may be taking five different medications that can be either constructive or destructive to tinnitus. You need to have someone involved who can help with the medications.
Inactivity is another factor. Many times, these individuals withdraw and sit alone or research on the computer all day. That is the worst thing possible. You have to get them engaged and back out in life. If they are not communicating as a result of a hearing problem, that adds stress, which is a factor. People with hearing loss are working two to three times harder than anyone else in the room just to follow the sentences. That feeds into this and should be addressed.
Grief is another factor and probably one of the most underestimated problems in tinnitus. I did not realize this until I was snowboarding with my oldest daughter. We were out on a Friday afternoon in the middle of nowhere and we crashed. It was dead silent. We were lying there in the snow, exhausted, and it was completely silent. At 10 years old she looked at me and said, “Your patients never have this anymore, do they?” I said, “No, they don’t.” She said, “That must be terrible.” That was the first time I came to the recognition that it is not the presence of the tinnitus alone that they grieve. It is the absence of peace and quiet. They will often need grief counseling to deal with the reality that they have lost a loved one - their peace and quiet, their ability to read a book in quiet, or to lie out in the sun and relax only hearing the birds or water.
Litigation may be another factor, if applicable, that adds a level of stress because it tends to recycle all of the problems and the events that triggered the tinnitus. TMJ problems and neck issues are factors as well. If you see a diagnosis of degenerative cervical disease or TMJ, encourage them to get those resolved.
All of these factors not only impact the tinnitus, but they exacerbate each other. When you are putting together your team, think of people who can help address these issues as you identify them in the medical history.
The Team
First, you need a clinic administrator. This is someone who has to be sensitive with patients, yet not get walked on and trapped on the phone for hours with someone. This person will know what questions they can answer and how to tactfully and sensitively put the patient in a position where they can wait for your expertise.
You need the tinnitus specialist. This is the commander and captain of the ship. This is the person who is behind the scenes running everything.
A tinnitus physician is very helpful, but I will qualify this. Most otolaryngologists will rule out an acoustic neuroma, look in the ear and rule out an ear infection, and then they are done. They are not looking for other medical factors. They are not looking for depression, thyroid problems, or chronic stress. They are not sensitive to those issues, and you need someone who is willing to work with you, not just spend 5 or 10 minutes looking in the ear only to recommend an MRI to rule out a brain tumor. You need a sympathetic, enlightened physician. We were very lucky in Portland to have a physician that had started as an otolaryngologist. But in his 16 years of working only with tinnitus patients, also took on endocrinology, rheumatology, infectious disease, neurology, and psychiatry in addition to his otolaryngology. He ended up with a total of seven subspecialties, with internal medicine being the seventh one. That kind of physician is a blessing.
Next is a psychiatrist. The role of the psychiatrist is to manage medications. These medications include the sleep, anxiety and depression medications. You need one person reviewing all of the medications that the patient is taking to make sure there are no conflicts.
The psychologist will provide the ongoing psychological support for anxiety and depression. Many times our patients will have post-traumatic stress and other types of anxiety disorders. The psychologist will be doing the heavy lifting in those areas. You will to do some counseling and education, but the rest of it will be done by that teammate.
These team members may not physically be in your office, but as you start to identify community professionals who are willing to work with these patients in a team-like fashion, you will be able to help the patient in significant ways.
Getting Paid
If you want to get rich, do not go into tinnitus. The insurance reimbursement for the things that you can submit are meager and not worth the time. Many clinics set up fee-for-service billing. If you work at a hospital that has insurance contracts, you may have to set up a separate limited liability corporation that shields you from the insurance obligations of the hospital. Set up a fee-for-service and build in charges for your time, based on what you need hourly to survive in the practice. Very few insurance companies will bill for your tinnitus management component. That includes evaluating the instruments, doing the education, and putting in the time that it takes to be responsive to these patients when they have needs on a regular basis. You will have to build that into your costs.
I am a mixed advocate for getting insurance on board, because I find that insurance companies tend to reimburse at the average rate for most procedures. As you get more known for your expertise in tinnitus, you are not going to get average patients. You will start get the ones that have tried everything else before you; they require more time than you can possibly imagine. It is wise to build in a lump sum for services. In Portland, they paid a lump sum which covered our time with them for the first six months of their care, for whatever they needed. We would base that sum on a phone screening that we performed at the beginning. We would do a phone screening to get an idea of the severity and the complexity of their case, and then base our charge on that. Other patients pay on an hourly basis. This is something you will have to figure out.
Importantly, most insurance companies do not cover any devices having to do with tinnitus. Things like sound generators can sometimes be billed as miscellaneous durable medical equipment. If you submit the insurance claim as miscellaneous durable medical equipment either for a combination unit or a sound generator, you may get reimbursement for that. It is difficult to get hearing aids reimbursed, even if you are using them therapeutically under that term.
The Payoff
It is a challenge, yet it is incredibly rewarding. My wife, Jennifer, is co-faculty and she saw three tinnitus patients today. Sometimes they are frustrating. A lot of our patients from the US have tracked us down in Singapore. We still follow with them and encourage them. It is the most intimate form of medicine that I know. It will stretch you and strain you in every possible way, but I encourage you to dedicate at least part of your practice to this if you can, because the need is certainly great.
Questions and Answers
Related to sensory gating in the neurophysiologic model, our brains are built to habituate to unnecessary inputs. For instance, all of you do not know that the chair that you are sitting on is actually pushing up again your rear end. It is, and now all of a sudden you all think about it because it was brought to your attention. The sensory gate is wide open for people with chronic tinnitus. Can you speak as to why that is?
This is fascinating. You said that the brain is designed to habituate. Even more, the brain is designed to ignore. Probably 99.9% of the sensations that are flooding your body right now are being completely suppressed or inhibited by your nervous system. We have this tiny window of sensation that allows us to connect to the world around us and to function without being overwhelmed. In fact, one of the models for autism is that people with autism are overwhelmed with so much sensory information that they cannot function. They resort to self-stimulation, even if it is painful, just to have a reference point.
Imagine something going wrong with the system and allowing this one tinnitus signal to rise to the top of the pile continually. It is like there is a breakdown. I have heard of Ruldolpho Llinas, a well-known neuroscientist, who has indicated there is evidence of things called low threshold calcium spike bursts. Those are based on EEG activity and signal-unit recorders deep in the thalamus. This is evidence of abnormal firing in the thalamus that corresponds to essential tremor and movement disorders, as well as other types of treatment-resistant neurologic problems, likely including depression and tinnitus. When we disrupt that delicate balance between excitatory and inhibitory systems, we set up abnormal firing patterns that seem to take certain symptoms and make them self-perpetuating. Even if we cut the auditory nerve and the patient wakes up deaf, in 70% of those cases, the patient still hears the ringing. Even if it started as a cochlear problem, it becomes a central issue. That is my guess as to how this system gets out of whack, but it is based on theories and models. We do not really have any hard evidence that that proves it yet.
How long does it take for the doctors to rule out the active diseases processes?
It depends on the doctors. Every ENT should have the list of active diseases processes from medical school. The paper that I referred to has an outline (Folmer, et al., 2004). For TMJ, you are going to ask them if they have any problems with their jaw or popping. If they say yes, then have them get checked out. In their history, ask if they have had any head or neck injuries. If they say yes, ask if they have had neck pain or neck problems. If they again say yes, then part of your job as the tinnitus specialist is to send them to a place where they can get these things evaluated.
If they have a neck disorder, it may require cervical decompression. It may require surgery, and therefore, you have a long-term course. For other people, it may be nonsteroidal anti-inflammatories that relieve the pain and that can reduce the some of the tinnitus loudness. Your role is to realize that these things can exacerbate the tinnitus; make sure that they get followed.
When they come in, they do not realize that when they fell off the swing set in college and landed on their head that it could associate with their tinnitus. However, it may be one of the contributing factors. One of the issues is making sure that you encourage the patients to pursue the other things that you have identified that may be related to the tinnitus, that no one else has tied together before.
Are the phone apps good for all kinds of tinnitus and severities?
I would love to do a whole session on acoustic therapy alone. There are three simple guidelines to find sounds that are helpful in facilitating habituation. If we want to move toward a habituation model, use sounds that compete with the tinnitus to bring about a natural process of pushing the tinnitus back into the background where it belongs. There is no magic sound that works for everyone. It is very subjective.
Number one, the sound needs to be tolerable. It needs to be something they can listen to for six or maybe eight hours a day. You may have a sound that is very effective at masking; a chainsaw would be effective at masking the tinnitus completely, but it is not tolerable.
Secondly, you want a sound that is subjectively tolerable and not intrusive to the individual. It should not disrupt their concentration. It is there in the background, but you do not notice it.
The third characteristic is that it has to provide some kind of a space between them and their tinnitus. It does not have to mask it completely, but it has to create some kind of an interference or separation from the tinnitus that gives them some form of relief. As you create this picture for your patient, you will find they will be able to identify the sounds that work. They will test the sound apps and find the three factors that work for them.
We find music works for a lot of people, except musicians because it is too engaging. Musicians get so caught up in the musical part of the sound. Even though they get complete tinnitus relief, they cannot concentrate because they are critiquing or singing to the music. It is very individualized. When you are looking at apps, you want to give your patients the guidelines to use. Likewise, as you are picking sounds available through the sound generators or the combination units, follow these guidelines to find sounds that will facilitate the habituation.
Have you published any other books or articles that you have not already referenced?
Most of my papers are things like spectral analysis of auditory nerve fibers in cats to identify changes in animals with induced tinnitus. Aage Møller edited a book recently on tinnitus that has some amazing contributing authors (Møller, Langguth, DeRidder, Kleinjung, 2010). It is probably the best comprehensive book one that I can think of right now. I co-authored a chapter on tinnitus prevention, but I get no money from it so there is no conflict of interest.
If someone presents with hyperacusis and tinnitus, which do you tackle first?
We let the patients rank the problems in order of perceived severity, and that usually gives us an indication of where to start. Many times, the sound sensitivity or sound tolerance issue is the easiest thing to deal with, especially in comparison to the tinnitus. A lot of times it is a reaction to the onset of tinnitus. Most of the time, we would start with the sound tolerance issue and then do the tinnitus treatment.
References
Coelho, C. B., Sanchez, T. G., Tyler, R. S. (2007). Tinnitus in children and associated risk factors. Progress in Brain Research, 166, 179-191.
Folmer, R. L., Martin, W. H., & Shi, Y. B. (2004). Tinnitus: Questions to reveal the cause, answers to provide relief. Journal of Family Practice 53(7), 532-540.
Griest, S. E., & Bishop, P. M. (1998). Tinnitus as an early indicator of permanent hearing loss: A 15 year longitudinal study of noise exposed workers. Official Journal of the American Association of Occupational Health Nurses, 46(7), 325-329.
Jastreboff, P. J. (1990). Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neuroscience Research, 8(4), 221-254.
Holgers, K. M. (2003). Tinnitus in 7-year-old children. European Journal of Pediatrics, 162(4), 276-278.
Martin, W.H., Griest, S.E., Sobel, J.L. & Howarth, L. (2011). Noise induced hearing loss and tinnitus prevention in Tribal children. Presented to the Confederated Tribes of Umatilla Indian Reservation, Tribal Health Council, Yellowhawk Tribal Health Center, Pendleton, OR.
Martin, W.H. (2002, March). Current tinnitus research. Presented at the American Tinnitus Association Symposium, Dallas, TX.
Meikle, M. B., Creedon, T. A., & Griest, S. E. (2004). Tinnitus archive, second edition. Retrieved from https://www.tinnitusarchive.org
Møller, A. R., Langguth, B., DeRidder, D., & Kleinjung, T. (2010). Textbook of tinnitus. New York, NY: Springer.
Mrena, R., Paakkonen, R., Back, L., Pirvola, U., & Ylikoski, J. (2004). Otologic consequences of blast exposure: a Finnish case study of a shopping mall bomb explosion. Acta Otolaryngologica, 124, 946–952.
Searchfield, G. D., Kaur, M., & Martin, W. H. (2010). Hearing aids as an adjunct to counseling: tinnitus patients who choose amplification do better than those that don't. International Journal of Audiology, 49(8), 574-579. doi: 10.3109/14992021003777267
Shargorodsky, J., Curhan, S. G., Curhan, G. C., & Eavey, R. (2010). Change in prevalence of hearing loss in US adolescents. Journal of the American Medical Association, 304(7), 772-778. doi: 10.1001/jama.2010.1124
Cite this content as:
Martin, W.H. (2014, November). Tinnitus care: what should I know when starting to provide tinnitus care?. AudiologyOnline, Article 13109. Retrieved from: https://www.audiologyonline.com

