Learning Outcomes
After this course learners will be able to:
- Identify the need for telepractice in their clinic to provide better patient care.
- Explain the skills needed to set up a successful teleaudiology practice.
- Explain how the implementation of teleaudiology can change the patient care model in an audiology clinic.
Introduction
Our profession is heading towards a new dimension of patient care and practice management. Throughout this course, I want to show you the complexity and multiplicity of the uses of telecommunication technology. This technology can be utilized in many healthcare arenas, with Audiology being our focus. This course is geared mainly towards private practitioners. We will begin with a basic introduction of telecare (i.e., telepractice, telemedicine). Then, we will discuss the need for telecare in audiology. Lastly, I hope to share insight on what it takes to run a practice with this new dimension of care. Hopefully, this will address some of the issues that are involved in managing a practice, including the financial aspects. We will dive into the specifics of how we can to build a wonderful telepractice. There are many terms used in telepractice, and I would like to begin with a review of each.
Telepractice Terminology
- Telemedicine is the use of telecommunication and information technology to provide clinical health care from a distance. It has been used to overcome distance barriers and to improve access to medical services that would often not be consistently available in distant rural communities. This is a product of the 21st-century advancement in telecommunication and information technology.
- eHealth (i.e., e-health) is a relatively recent healthcare practice supported by electronic processes and communication, dating back to at least 1999. It can also include health applications and links on mobile phones, referred to as mHealth (i.e., m-Health). This application links mobile phones and has resulted in specialized research developments for safer eHealth solutions that can withstand some of the issues related to cybersecurity. There is a continued effort to improve this practice.
- Connected health is a socio-technical model for healthcare management and delivery by using technology to provide healthcare services remotely. Connected health, also known as technology-enabled care (TEC) aims to maximize healthcare resources and provide increased, flexible opportunities for consumers to engage with clinicians and better self-manage their care.
Telerehabilitation (i.e., e-rehabilitation) is the delivery of rehabilitation services over telecommunication networks and the internet. Most types of services fall into two categories: clinical assessment (the patient's functional abilities in his or her environment), and clinical therapy. Some professionals that have used telerehabilitation include neuropsychology, speech-language pathology, audiology, occupational therapy, and physical therapy.
Telecare is the term for offering remote care of elderly and physically less able people, providing the care and reassurance needed to allow them to remain living in their own homes. The use of sensors may be part of a package which can provide support for people with illnesses such as dementia, or people at risk of falling.
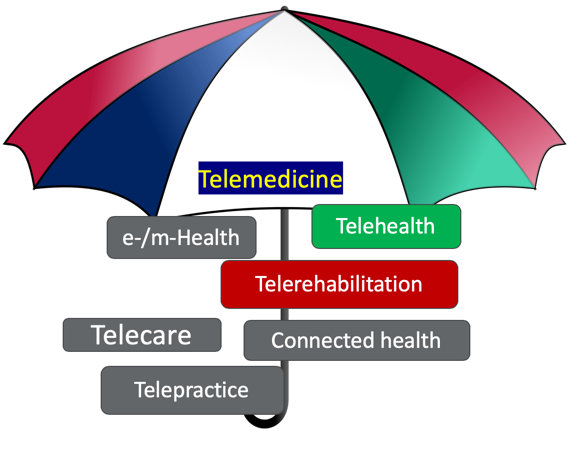
Figure 1. Telepractice Terminology.
Commercial Monitoring and Sensors. Sensors and wearables allow continuous physiological monitoring with reduced manual intervention and at a low cost. Sensors and wearables can be integrated into various accessories such as garments, hats, wrist bands, socks, shoes, eyeglasses and other devices such as wristwatches, headphones, and smartphones. Sensors may allow us a way to connect and understand the environment in which a patient lives and how we can use that kind of information to help build personalized care. Smartwatches and similar gadgets monitor many physiological conditions. Globally, the trend is shifting towards the use of monitors, especially in North America, Europe, and the Asia Pacific. Monitors can track a variety of activities based on the location.
![]()
Figure 2. Examples of sensor tracking.
Telepractice in Audiology
Goals of Teleaudiology
How does teleaudiology change the landscape of clinical services? What are the goals of teleaudiology? We can help patients live the life they want. We can design and personalized hearing care plan to help patients achieve their stated goals. We can find the tools and technologies that are most effective and integrate those in the most efficient, accessible and familiar way.
Teleaudiology Services
- Video otoscopy
- Hearing screening
- Diagnostic testing
- Fitting and programming hearing aids, aural rehabilitation
- Balance and tinnitus evaluation and management
- Need for Teleaudiology
There is a shortage of excellent hearing care professionals in the US and around the world. Teleaudiology has been proven to be very successful in several health care practices. This method of care is quite useful and is not a new dimension. Use of teleaudiology will address the serious shortage of audiologists by utilizing technicians and assistants. Most state laws support telepractice. Each state has a definition of what telepractice means. They are very supportive as there is a need for specific contacts and licensing issues. There is a trend towards the future of hearing care in a commercial setting.
Ian Windmill and Barry Freeman have explained the urgency and need to understand the current audiology practice setting. Each year the current supply of audiologists shifts, as new graduates are added to the pool and other professionals are retiring and exiting the profession. There is going to be a gap between the demand, so we need to start thinking of how we can manage this gap without compromising the quality of care.
ROI and Teleaudiology Implementation
A key component when considering telepractice is looking at the cost of doing business and how telepractice can help. Figure 3. shows how teleaudiology can be implemented and ROI. In this example, we have a full-time employee. Full time usually equates to 40 hours per week for 52 weeks (40x52), which is 2080 total available hours.
Non-billable hours. These hours include if an employee has taken a vacation, sick leave, unrecorded, personal holidays, staff meetings and CEUs, etc. Also, we need to consider other factors such as teaching, patient seminars and snow days. All those are considered non-billable hours because they will not add to your numbers and they do not generate profit.
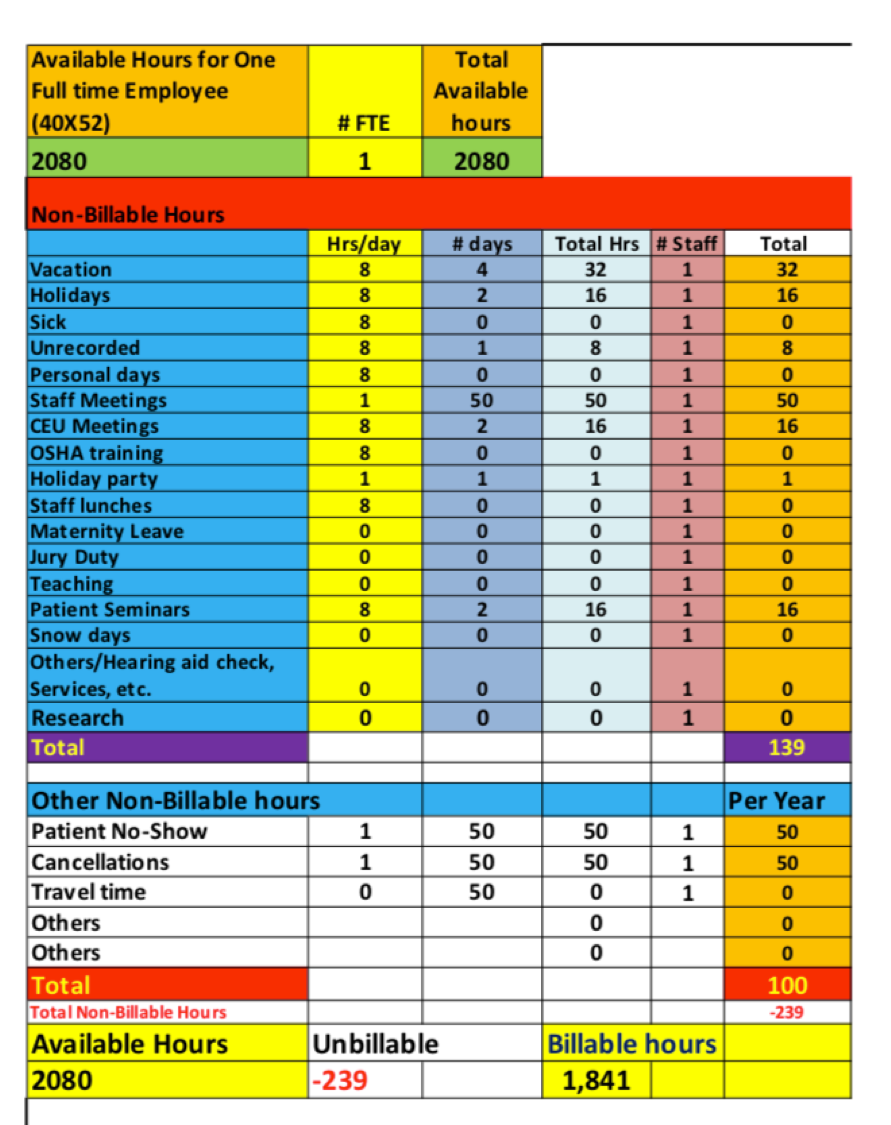
Figure 3. Example of ROI implementation.
Other non-billable hours. Many of us will experience circumstances that result in non-billable hours over 50 weeks. Patient no-shows, cancellations and travel time not previously factored in are the most common that add up non-billable hours. For this example, the billable hours will be 1841 hours, which is very generous. You are welcome to utilize this example to create your template to play around with the numbers. I hope this gives you an idea of what it takes to run a clinic and how much income should be generated as you go. I have included a video clip as an example:
Telehealth Modalities
- Live Video (synchronous): Live, two-way interaction between a person (i.e., patient, caregiver, provider) and a provider using audiovisual telecommunications technology.
- Store-and-forward (asynchronous):
- Video otoscopy and automated testing for later interpretation.
- Audiometry, immittance, OAE, ABR and newborn hearing screening.
- Any other materials that can be stored and evaluated by a specialist
- Real Time (synchronous): Audiological evaluation, hearing aid fittings, real-ear measures, hearing aid counseling, tinnitus management, and aural rehabilitation.
- Remote patient monitoring (RPM): Personal health and medical data collection from an individual in one location via electronic communication technologies, which is transmitted to a provider (sometimes via a data processing service) in a different location for use in care and related support. This type of service allows a provider to continue to track healthcare data for a patient once released to home or a care facility, reducing readmission rates.
- Mobile health (mHealth): Health care and public health practice and education supported by mobile communication devices such as cell phones, tablet computers, and PDAs. Applications can range from targeted text messages that promote healthy behavior to wide-scale alerts about disease outbreaks, to name a few examples.
Implementing Teleaudiology
Steps to Be Successful
To launch telecare in your practice successfully, you will need to have the right foundation. Figure 4 depicts the various aspects required to determine whether telecare is right for your practice. Questions to consider before diving in: do you have a team of people who are qualified or trained? Do you have the right equipment? How will the integration of all the processes that you have work? Do you have a protocol that is established to manage the practice? What kind of regulations do you have?
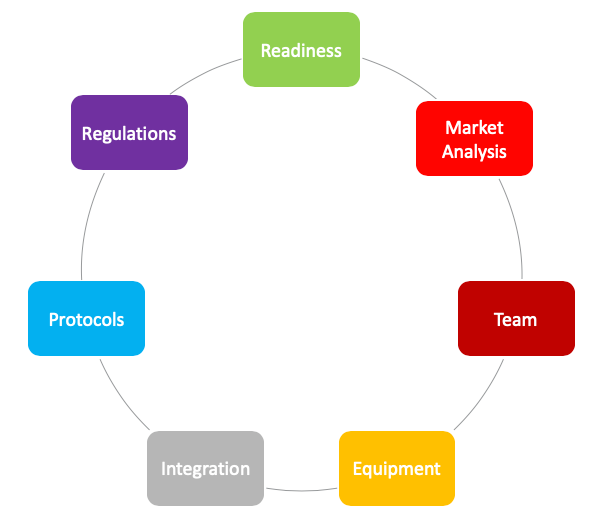
Figure 4. Aspects of Telecare.
Here are ten steps to help your practice be successful with a teleaudiology program:
- Assess and confirm your readiness to start a teleaudiology program. Do you have the intent to extend your practice to different locations? This may be due to distance, time, penetration into different regions. Is it within the mission and vision of your practice?
- Perform a market analysis and write a business plan. I recommend creating a detailed programmatic and technical implementation plan. The most successful teleaudiology programs are the result of careful, comprehensive planning and the deployment of well-considered integrated and streamlined technologies.
- Building your team. Identify and recruit the right people to support your mission and vision. Identify a coordinator to oversee all daily operational activities of the program. This might include scheduling, billing, technical operations, and other aspects of the business. Look for staff who are technically savvy and knowledgeable about the teleaudiology program and applications. Develop and implement a formal, comprehensive and standardized training regimen for all staff.
- Purchase the right equipment. Have appropriate specifications for the devices from trustworthy and knowledgeable sources. Also, be mindful that technology advances so you need to be prepared for changes that will take place in telecare. These are also things that you need to keep in mind when you purchase equipment. I would recommend a system that is compatible with your computer and has access to the internet.
- Create an effective and professional environment that can emulate a traditional face-to-face encounter. Do not compromise because the patient will not see you. They still need to have a professional impression of your practice.
- Plan for the seamless integration of teleaudiology between sites. Think of the teleaudiology technology as just another tool for the delivery of services. The only difference being that the patient is not in the same room as the provider. Keep it simple so that you do not complicate the process. Yes, technology can be challenging and frustrating, so we need to plan.
- Plan for the availability of IT support at all participating locations, applications and network needs. It is very critical because there are occasions when a connection between the primary and satellite clinic can be disrupted. You need to understand how to get back up and running efficiently.
- IT support. You need to establish protocols, policies, and procedures as well as short and long-term performance goals. Create protocols that are as close as possible to face-to-face interaction. Follow standard, recognizable protocols which lead to consistent clinical results. Establish long-term goals that consider the clinical business, and financial outcomes several years into the future and movement towards programmatic self-sustainability.
- Develop an evaluation, monitoring, and quality-improvement plan. This plan needs to be monitored and evaluated as critical elements of the program on a regular and ongoing basis.
- Understand the laws and regulations. HIPAA, credentialing and licensing are equally important.
TeleAudiology Levels and Equipment
Level 1: Hearing aid troubleshooting. Here is a list of equipment for both your primary and satellite clinic to perform hearing aid programming and troubleshooting.
|
Level 2: Diagnostic testing, and hearing aid recommendation-fitting. Here is a list of equipment for both your primary and satellite clinic to perform diagnostic testing and hearing aid counseling and fittings.
|
Equipment Configurations
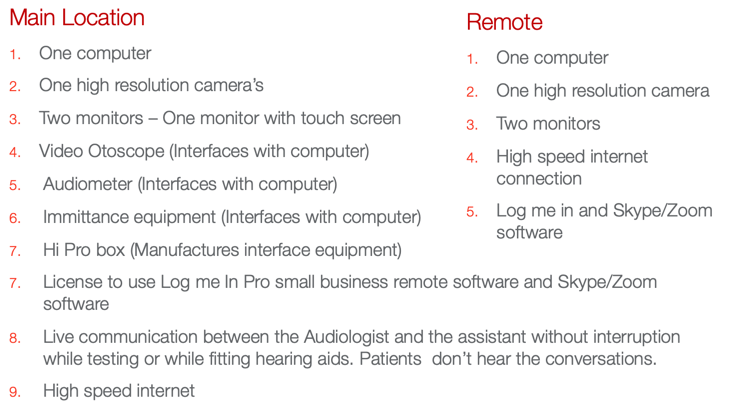
This is the equipment set up I have. I hope this gives you an idea of where to begin in terms of which equipment you will need at each location.
Workflow. In terms of workflow, you could structure this how you would like your practice to function. Hopefully, the patient would arrive 30 minutes before the appointment and the assistant will prepare the exam room. They will also fax the completed history and consent form through a secure line. Once the patient and the audiologist are in the room, the assistant remains in the room to assist with the equipment as necessary. For my practice, this is the flow:
- Turn the computer and monitors on
- Check connectivity
- Check camera location and usage
- Check the case history
- Consultation
- Testing
- Consultation
- Report – Print audiogram at the remote site – Report and chart notes
I have a video demonstration of a teleaudiology practice here that I would like to share. I have used the system when I had my clinical practice, and the video clip demonstrates the technology well.
Codes
The Medicare Telehealth Parity Act of 2017 was introduced by Representative Mike Thompson of California but has not been passed. If approved, audiologists could then see Medicare patients and help with the tests.
Modifiers
Those related to telepractice are available through both the CPT coding system and the Health Care Common Procedure Coding System (HCPCS)—are appended to CPT codes to indicate mode of service delivery. Audiologists should check with each payer to verify appropriate use of modifiers to reflect telepractice services.
HCPCS
GQ. Telehealth service rendered via an asynchronous telecommunications system.
GT. Telehealth service rendered via interactive audio and video telecommunications system.
CPT
95. Synchronous telemedicine service rendered via a real-time interactive audio and video telecommunications system. Modifier 95 was created through the CPT system for 2017 and can be appended to CPT codes to reflect services that were provided via real-time telecommunication systems. This code does not replace the existing GQ and GT modifiers that were created through the HCPCS by the Centers for Medicare & Medicaid Services (CMS). Clinicians should check with individual payers regarding the implementation and use of telepractice-related modifiers on the claim form. I strongly recommend contacting your local carriers, the insurance providers of your patients and see what they need and how you want to address the reimbursement and payment options.
Place of Service Codes
Place of service codes are used on claims to indicate the specific type of location where services were provided. Clinicians should verify with individual payers regarding implementation and use of the POS code for telepractice, listed below. More information on POS codes is available on the CMS website.
02. The location where health services and health-related services are provided or received through a telecommunication system.
Challenges and Opportunities
Let's take a look at a few challenges one might face when setting up a telepractice service. First, you will need to have reliable connectivity. Second is acceptance by the staff and patients. The third is technology and equipment. You have to be savvy and need to understand how it works. The next one is a dedicated staff. You have to have people who understand the process and procedure. Reimbursement or payment, this is another aspect that you need to know. How do you take care of your hours for billable issues? How can do you deal with your insurance carriers. Then there are licensing issues, as each state is different.
TeleAudiology Challenges
- Connectivity
- Acceptance
- Technology/Equipment
- Dedicated staff
- Reimbursement
- Licensing issues
What are the opportunities that a practice can gain? With an extended reach, you can see more patients. How do you imagine this integrated into your system? We all have to have an exit plan at some point in time. If you have established a well-functioning telepractice, then you may be able to help the practice transition smoothly. Less travel time means you do not have to pay providers to go to other locations, which is an expense that you can minimize.
TeleAudiology Opportunities
- Increased income
- Improved patient care
- Improved patient satisfaction
- Extended Reach
- Better exit plan
- Reduced travel time
Conclusion
Citation
Ballachanda, B. (2019). Telepractice in audiology. AudiologyOnline, Article 24859. Retrieved from https://www.audiologyonline.com