Editor's note: This text-based course is an edited transcript of the webinar, Supervision: Developing Person-Centered Communication, presented by Karen Munoz, EdD, CCC-A.
Learning Outcomes
After this course learners will be able to:
- Describe supervision objectives and the supervisory relationship.
- Describe skill development areas to provide person-centered care.
- Describe strategies for promoting student growth in person-centered care.
Introduction
As supervisors, I think you all know that this role is multi-layered and has a lot of aspects to it. I worked as a clinical supervisor at a university for many years, so I am in tune with what that involves.
Supervision
Not only are you teaching, but you are also evaluating students, mentoring for skill development, advising students, and modeling behaviors. It is a complex role to have.
Supervisory Relationship
The supervisory relationship is the key to success in this role. This aspect allows you to help students challenge what they know and understand. You are there to help and motivate them, as well as immerse yourself in whatever they are learning. The supervisory relationship and how you connect with students can influence their behavior change. Learning something new requires some behavior change. We need to act on doing something differently based on new information we have learned. The supervisor relationship has a more influential role than you may realize.
Providing Feedback
Here are some crucial points to remember about providing feedback:
- A fundamental aspect of supervision.
- Students often feel particularly vulnerable when receiving feedback about how they communicate.
Providing feedback is common when you are teaching and mentoring. Person-centered care revolves around how we communicate and engage with others. As you are teaching students to provide person-centered care, you are often talking about how they communicate. That can feel vulnerable, especially when it is difficult feedback to get. Considering how you approach it, giving feedback can make a difference in their ability to act. Does that open them up to say, "I see that now, and I'm going to try this," or does it shut them down and make them defensive?
When Providing Feedback
Here are some things to consider when you are providing feedback:
- Create safety
- Who might hear this? Ask permission first (I'd like to talk about how it went today, would that be okay?)
- Be positive
- When addressing both strengths and areas to improve.
- Be specific
- I saw you did [skill] well and noticed you struggled with [skill].
- Be immediate
- Routinely engage while it is fresh on their mind (and yours).
- Be objective
- Be honest, but not mean and make sure it is not emotion-based.
It is easier to hear difficult news when we feel safe in a relationship. It is important to consider if anyone else is able to hear the conversation. Think about whether or not you are giving advice that may be hard to hear in front of others. Also, consider if the conversation is occurring in a place where you can be overheard. Those factors may make it hard for the student to focus on what you are telling them.
Make sure to ask permission first. When we respect the autonomy of the other person, it can help the conversation go in a more positive direction. You must signal where you are headed in a conversation so they can acknowledge that they are okay going there. Getting permission can open up the other person to hear your constructive feedback. Even if this is fine with them, this changes the tone and receptivity of the feedback.
It is essential to be positive. We are addressing both strengths and areas to improve, and how we frame that conversation can make a difference in how receptive that person is. Think about phrasing and be specific. When talking about communication, it is easy to be vague and keep the conversation from being meaningful. If a student is working on asking open-ended questions, you can say, "I saw you ask some good questions today. Did you notice that when you did that, they told you about X, Y, and Z? Something that we wouldn't have thought to ask ended up being so important." Connect the dots with them.
Immediate feedback is also essential. This is because it is fresh in everyone's minds. Different schedules and routines can make this difficult. If there is an opportunity to debrief right after, that may be best. However, make sure you are thinking about the timing of debriefing and how quick it is. Be objective and try to keep emotions out of it. This does not mean you do not have difficult things to say, but this is not a judgment on them. You are looking at their behaviors, the skills that they are learning, and how you can help them do better.
Purposeful Dialogue
When we talk about having purposeful dialogue around learning with our students, it is crucial to help them have realistic expectations. I am sure you have experienced students not realizing how long it takes to learn and develop different skills. Students go to school for four years because we cannot expect them to become experts by the end of their first semester. It is common for students to want to please their supervisor, and that can impact their willingness to ask for help or admit that they do not know something. How do we help them set expectations that make sense for the learning process?
Help them identify and address their learning gaps. This may be obvious from a supervisor's perspective but not for that student. Getting explicit and specific as you look at gaps and how to go about addressing that can help move them along.
Helping them develop specific learning goals can be useful as well. I like to have students write learning goals at the beginning of each semester. It is necessary to talk about those goals and break them down because they may be bigger than students could achieve in a semester. Teach them to ask themselves, "What is an achievable goal? What is the timeframe to do that? How am I going to get there?" Merely asking them to think about their goals does not mean that they can immediately go through the process themselves. For example, a client may be experiencing a barrier while learning a new skill. Let's say they have hearing aids and are having trouble learning how to use them. It is not helpful to say, "It's important that you wear your hearing aids every day." This is because some people cannot break down those goals as easily by themselves. Guiding them in the right direction is an essential and needed conversation.
When looking at engaging in reflective practice, we tend to think about what worked and what did not work. Bringing in that element as part of the dialogue can help students improve their reflection. The self-awareness that they gain in this process is vital in their behavior change. Monitoring progress over time is helpful as well to help them see where they are going.
Reflect on Your Supervision Practices
- Invite students to express their thoughts/feelings.
- Address their questions and concerns.
- Help students develop concrete goals.
- Teach them to embrace their role in learning.
- Monitor your actions and reactions.
- Model dealing with challenges.
- Teach them to provide person-centered care.
Reflecting on your supervision practices and considering how you take action is a helpful step as well. Ask yourself about what you do that is helpful and what you want to adjust. Think about how you invite students to express their thoughts and how you make them feel safe. Do they feel okay about making themselves vulnerable? How do you go about addressing their questions and concerns? This can connect to their feeling of safety.
How do you help them develop concrete goals? What is your role in their process? How do you teach them to embrace their role in learning? It is a dynamic process. How has their role developed throughout their education? That can hinge on how they were taught before? It is a process that takes some talking through.
Monitor your actions and reactions. Are you staying objective, or are your emotions getting in the way? Are your emotions influencing how safe a person feels? Model how you deal with challenges. You are facing challenging situations all the time, and they are going to see how you handle it. Talk through how and why you approached a situation. Also, how do you go about teaching person-centered care? What are you already doing to support a student's learning? What are your opportunities to look at expanding what you do?
Why is it Important to Teach PCC?
If we compare person-centered care with a medical model and take note of the differences, the benefits of that start to show up a bit more, with a medical model, the expert who knows how to fix the problem will tell the patient what to do. That will then set you up with a person who knows the answers. When it comes to learning how to implement new habits, we are not experts on their behavior change. While that assumption can feel safe because we have gone to school, the client is the expert. While you can tell them what to do, it is missing the critical component of what they can do themselves.
How does this come together for our services to be beneficial for them? How is person-centered care different from a medical model? Person-centered care promotes a shared process because it empowers the person to recognize their role in behavior change, as well as be an active part of the process. Person-centered care guides people as well. When you provide person-centered care, the mindset to have is that you are a guide. You are helping them decide where they want to go, why they want to go there, and the best way to get there. It is a strategic approach because your goal for them is to be able to voice what they can do. The actual action of voicing their abilities is essential for behavior change.
On the other hand, if they are passive and you are telling them what to do, the natural reaction for them is to ask themselves why they cannot do something. Instead of voicing why they can, they are now voicing that they cannot. That does not go well with behavior change. Person-centered care is purposeful because it helps people act on what they value. Assisting students to understand the connection of how they interact makes a difference in outcomes is a necessary mindset to talk through.
Person-Centered Care Influence
This is what person-centered care influences within our patients:
- Acceptance
- Understanding
- Adjustment
- Self-management
- Self-advocacy
When we provide person-centered care, it helps patients accept their situation and understand where they are and where they need to go. These aspects help them to provide self-management and advocate for themselves. If we are successful in assisting people in bettering their routines, they are going to have a better quality of life. They are going to feel better, more satisfied, and have better outcomes. It is not going to be as effective if you simply tell someone their overall goal. Picture yourself speaking with a parent of a child with hearing loss, and you say, "The goal is that your child should be wearing their hearing aids for ten or more hours a day. They're going to have better language development." A parent needs to understand these things, but a reminder of that goal is not what is going to help them get there. They are not going to feel confident in how they are helping their child. It is a reminder that that goal is often not what is needed to achieve those goals.
There has been some work in the medical community regarding communication. A meta-analysis done by Zolnierek and DiMatteo (2019) found that the communication provided by physicians was correlated with better patient adherence. That was adherence to whatever was recommended in care, whether it is taking medication or following through on other aspects of medical care. Through this meta-analysis, they found that it was worthwhile to devote some time and resources to learn how to communicate more effectively.
Evidence-based Communication Strategies Help Patients Commit
Patients do not follow treatment recommendations unless they:
- Know what to do.
- Are committed to doing it.
- Have the resources to be able to adhere.
Using evidence-based communication strategies will help your patients commit. Commitment is key with behavior change. People are not going to be able to follow through on treatment recommendations unless they know what to do, are committed to doing it, and have the resources to do it. A lot of what we do is education and teaching, so that information aspect is there. We do need to think about how we deliver the information for that to be effective.
When we think about the resources, it is not just external resources, such as money to buy a hearing aid. There are also mental and emotional resources. When people are having trouble adhering, what are the barriers that can get in the way? It is often that those barriers are internal. It may be concerning how they feel, being self-conscious, or worrying about what other people think. Many things can get in the way. Those are part of their resources. Do they have the mindset and the strategies to overcome those things? That is where we can help them.
Mentoring Person-Centered Care
Mentoring students to practice in a patient-centered way begins with their attitudes and practices. Be aware of how you model and what you want the students to learn. Are you an expert in the room? There has been variability with audiology training, so the skills that we use to provide patient-centered care are aligned with counseling skills. It is what we need in order to practice in a person-centered way.
While many universities have a counseling course, there is no standardization for what these courses should include. Having a clear understanding of what it means to have excellent counseling skills is not as clear as it could be and hopefully will be down the road. Given that variability, what did you learn? How confident are you as a supervisor? You may feel vulnerable, trying to teach these students if you are not as comfortable with your skills. I am asking you to observe your practices and be reflective. What we find is that students may be learning some of these things while we are learning them as well, and that is okay. It can be a mental hurdle to get through that.
Students Model What They See
How you communicate with your patients is going to influence your teaching. There has been a lot of research observing how audiologists communicate and what that looks like in practice. There was a study done in Australia that looked at audiologists who were providing technically-focused responses to client concerns. This means that when clients were raising concerns, the audiologists gave a technical response instead of providing space for acknowledgment. It is reflective of how a lot of people are not comfortable with emotions. I often hear people say, "What if they tell me how they feel? I do not know what to do with that." We need to remember that we do not need to have the answers to everything. Being able to listen and acknowledge that person is powerful in and of itself.
Other things that show up in these studies are audiologists dominating the conversation. This means that the audiologists are doing much more of the talking than the patients. That can interfere with empowering the patient and having a shared process. What does it mean when you are doing most of the talking, and what is the impact?
Another behavior is frequent multitasking during conversations. We are constantly on computers and working with devices. This can take away from listening and hearing what someone has to say. I teach a counseling class where the students watch videotapes of themselves and reflect on that. One student said, "I didn't look at that person the whole time they were talking." Considering how we set up our space versus trying to do more than one thing at a time, there is a trade-off.
These situations set up space for either not using skills or missed opportunities. Providing a technical response to an emotional comment brought up by a patient is a missed opportunity to help that person feel heard. Let's say the person is feeling frustrated, and you are not acknowledging what they are feeling. That frustration gets bigger, and it gets in the way. The act of listening and empathizing reduces that frustration. When the power of that emotion is brought down, the person can move forward-thinking about how you deal with these situations, influences what students see, and try to emulate from observing you.
Reflect On Your Strategies
Take a moment and think about the person-centered strategies that you use in clinical encounters. When you think about that, focus on your approach to understanding patient issues. How do you ask patients about what they value or what their priorities are?
Another element of communication that is not as common as it should be is to find out what patients' priorities are that day. What do they value? It is driven by the agendas that audiologists have in looking at the goal of the appointment that day. Make space for understanding what else is on their mind and whatever is important to them to talk about. There is always room for something that you may not anticipate or know about.
How do you respond to patients' emotions that come up? How do you engage patients in shared planning? What does that look like? How do you approach sharing information? Are you providing the things that you know are important to them? Are you finding out what they already know and what they want to know more about? Are you checking in with them along the way? Those are some questions to consider for your routines.
Teaching Person-Centered Care
When you are teaching person-centered care, you are addressing attitudes, knowledge, and skills. Helping students understand and identify what to work on themselves is important. You want to engage them in the conversation and guide them in a strategic, purposeful way rather than tell them exactly what to do. It will be a more impactful experience for them.
Support Person-Centered Care Skill Development
We did a brief study of different techniques that supervisors use to support the counseling skills of audiology students on their final year placement. Some aspects of the survey were finding out how they were getting feedback from their supervisors and how often. Some events happened for participants more than half of the time.
Forty-eight percent of the students said that they would discuss their performance about counseling after appointments with their supervisor more than half of the time. It was happening more than anything else, but still reasonably infrequent. Approximately a third of the participants discussed counseling skills before the appointment. About a quarter of students said that a rubric was used to evaluate their competencies for specific counseling skills. A little less than that said, they received written feedback about their skill performance. Ten percent had a performance feedback form that was specific for counseling skill development. Similar to any skill that a student is learning, they need frequent and specific feedback to learn how to improve. We are seeing that receiving feedback is not happening as frequently as it could be. This is also one study conducted later in the program.
Person-Centered Care Begins with Attitudes
When we say that person-centered care begins with attitudes, what kinds of attitudes are we talking about? They are probably attitudes that you all have and demonstrate to your students. It is worth talking about why a certain attitude matters.
For example, it is good to be present, caring, and compassionate. Being curious and entering a situation with an open mind is important. It can be easy to get frustrated with clients that are having trouble following through or are not doing the things that we have talked about. We may let judgment creep in, and that can get in the way. Valuing patient engagement is important as well. Are we valuing that they are engaged, or are we thinking, "I don't have time for that, so I am not going to bother"? I have heard concern from people that counseling takes too much time. However, there is not a lot of data to support this. You may meet their goals quicker by taking time.
Show a genuine interest in patients and show concern. Have a desire to help them overcome their barriers. Do you see these things as part of your job? Do you understand that what you teach students about their barriers is part of your job, or is that something that they should work out on their own? If not you, then who?
Our services and support for their success do not end when the appointment is over. It extends to their home, and it may require a different kind of support education to be successful. Be willing to engage in self-evaluation. How is it going? What is going well? What can I do differently?
Identify Skills to Improve
Here is a list of skills that we can consider approving:
- Question-asking
- Active listening
- Shared planning
- Responding to emotions
- Identifying/addressing barriers
- Non-verbal communication
I have discovered that many people think they ask open-ended questions, but they ask closed-ended questions. This matters because asking closed-ended questions often lead to a yes or no answer. It does not invite exploration or understanding. That does not mean you cannot ask closed questions because they can help when you want to understand something specific. However, open-ended questions bring that engagement with the person you are talking to. It is interesting to see the feedback it takes to help students get into asking open-ended questions.
Active listening is another example, as well as shared planning. In an appointment, shared planning can refer to understanding priorities or addressing a barrier that the person is having. However, I am seeing that we are broadly saying what somebody should do rather than help them get there. I have seen shared planning as an area in need of growth.
Responding to emotions is critical, as well. I often see that people fly right past that and do not respond to emotions. Once that self-awareness of this becomes automatic, it will become part of interaction with others. However, getting to that point is what takes work and feedback. Consider how you identify and address barriers. A lot of people are familiar with non-verbal communication.
Identify Knowledge Gaps
Here are some knowledge gaps that correlate with the student's understanding of why they learn skills:
- Psycho-social and functional impacts
- Factors that influence behavior change
- How barriers can impact intervention
- Stereotypes and stigmas and surrounding disorder
- Sociocultural diversity and cultural sensitivity
Different kinds of knowledge come into play, such as what the patient is going through, what factors influence behavior change, how those barriers impact intervention, and why they would talk about it.
Connect the Dots
You want to connect the dots between communication and how it influences behavior change. It is taking an aspect of our work and bringing it into the running conversation we have as we teach students.
Tip 1: The first tip is to use counseling terminology. Use specific words during the conversation that can help them connect the dots between the skill they are trying to develop and why they are trying to develop it. Using common terminology among supervisors will support that development.
- Active listening
- Attending behavior
- Closed questions
- Empathy
- Encouragers
- Open questions
- Reflection
- Validation
Tip 2: Talk about communication ahead of time. Ask them about why they are concerned. Talk through hesitations they may be having about talking with their patients. Help them prepare open-ended questions. You can also roleplay a skill that they are concerned about. Doing this will increase their confidence. It is important to keep taking chances to practice. As a supervisor, you are there to step in and help when you need to. You are going to be stepping into a modeling role. This can work because you are helping the student by modeling when they need extra support.
- Ask students about their concerns
- Prepare open-ended questions to ask
- Roleplay skills
Tip 3: Provide frequent performance feedback. Debrief as soon as possible after a session in order to give them comments to walk away with. If sessions are recorded, reviewing those recordings together is one of the most effective strategies for behavior change around communication. Work together to make a plan for the next session. What are they going to work on? You want them to feel good about what they are doing so they have the confidence to try it. It is also important to accept when they are not there yet, and there are things to work on, so an honest conversation is encouraging.
- Debrief soon after the session
- Provide written comments
- Review recorded sessions together
- Together, make a plan for the next session
Student Counseling Influenced by Performance Feedback
Finai et al., 2018 did a study that looked at the impact of providing counseling performance feedback to students. The study comprised of five AuD students with minutes of counseling, baseline, and after individual instruction. Then performance feedback after was completed after each encounter. Performance feedback provided between encounters increased student counseling behaviors.
The study was a single-subject design with five students. We looked at how many minutes they spent in counseling behaviors and asking open-ended questions, responding, and so on. They received individualized instruction on where their skills were to help them learn what to do. They then had a feedback session after each encounter in the clinic, and we saw their performance increase. The students were responsive to this type of feedback and learning. Audio-recorded clinic sessions that they were having in their practicum allowed them to improve. A couple of students did not respond as well as others and had not yet had the counseling class. I wonder if having an understanding of the "why" makes a difference in how well they are going to act on what they are learning.
Tip 4: Another tip is acknowledging what went well in a specific way. It is easy to say, "That went great today. I love how you talked with them." That does not pick out what they did well. For example, you could say, "Great job validating her frustrations. She seemed to appreciate that you understood her concerns. Did you notice how she then engaged in problem-solving?" Notice how that specific comment connects those dots. Thinking about how you provide feedback is not technical. When we are talking about person-centered care, it is all about communication.
Tip 5: Facilitate their learning to reflect on their practice and raise their self-awareness. Increasing self-awareness is an important piece of changing behavior. Asking key questions can help them do that. Ask them about their barriers or how you can help. Talking about their goals and helping them see their growth can be powerful, too. They do not always see what we see.
- Ask about their barriers
- Ask how you can help
- Talk about their goals
- Help them see their growth
Tip 6: Monitor their development and make sure they have opportunities to practice. Expect growth and evaluate their competencies.
Tip 7: Be aware of your own counseling skills, your strengths, and where you want to go. Be open to expanding that and asking for help as needed. You can see that it was a process to learn how to integrate teaching counseling and person-centered care in our program. It is something that we are still working on because it is a process for the long haul. There are different elements in practice that can support this.
Suggestions and Opportunities
There are some suggestions and opportunities that we found helpful that you might find helpful as well.
Add PCC Questions at the Beginning of Intake Forms
We taught our students to use a case history form, for example, and an intake form. All of our open-ended questions were at the end of the form. No matter how much we talked about understanding the patient's priorities and getting information from their perspective, in their learning, they wanted to follow this intake form. We restructured it to put person-centered care questions at the beginning because that went with their habit and comfort. We then created an intake form for every appointment rather than just a diagnostic. We had an intake form for how they were doing on that day, what was happening and so on:
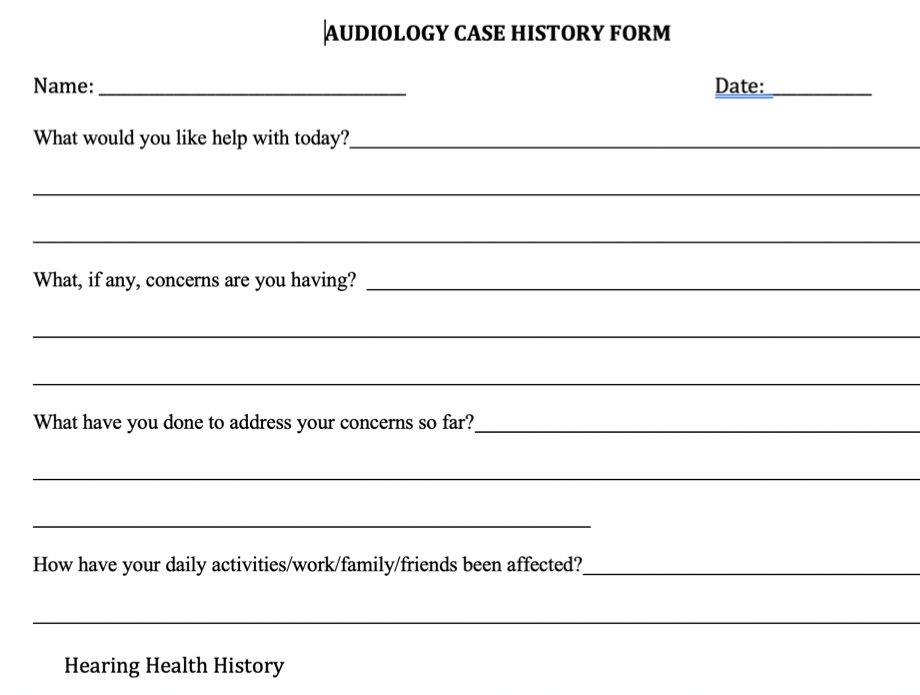
Figure 1. Example of intake form.
Looking at Figure 1, questions that they could use were whether they were coming in for a hearing aid follow-up or something else that did not have the standard hearing evaluation intake form. That step has been helpful.
Add PCC Questions to Patient Feedback Forms
We also like to get feedback on our services and understand how patients are viewing our person-centered care work. We have added a few questions to our patient evaluation form that can help us look at our work from a different perspective.
Track Skill Performance
Figure 2 shows a performance feedback form that provides key communication areas with a brief description:
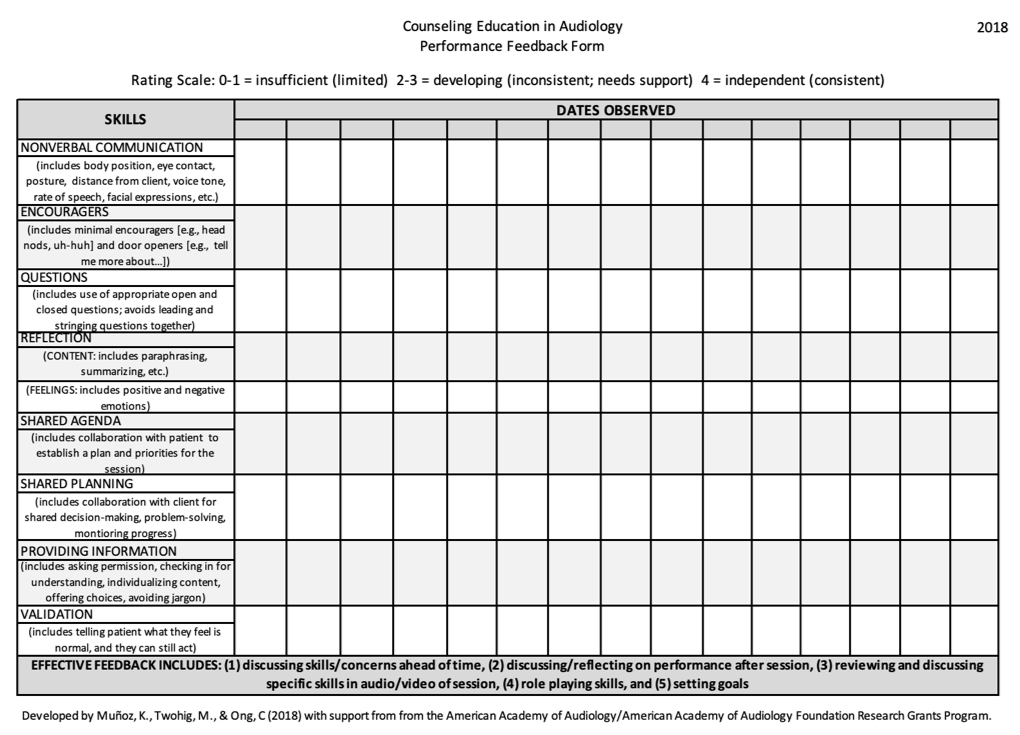
Figure 2. Example of performance feedback form.
Some supervisors use this in written format, and others use it in electronic format. We provided a simple rating scale: a zero to one was insufficient or really limited, two to three is somewhat inconsistent, and four is independent and consistent. You can then see how often they are doing certain skills by whether or not you are rating it. For example, if there is no rating, and they are not asking open-ended questions, this form allows you to see gaps in communication.
Supplement Teaching with Counseling Resources
I received a grant from AAA a few years ago, and we created some counseling videos and materials that you can get for free on the website called www.heartolearn.org. This website is focused on materials for parents and professionals working with young kids from birth to six years old that are learning spoken language.
I added a clinical skills section on our tutorial page. We have some videos that we use early on in our student training to help introduce them to thinking about counseling from the beginning. This is because they are shaping their approach to how they communicate with people from the start, and it is going to develop over time. Those are accessible to anyone.
IDA Institute Resources
The IDA Institute is another place to get great resources. They have done a lot of work with person-centered care and have a strong initiative. I am part of a working group that looks at how we help teach person-centered care in audiology programs. They have more resources coming out, as well.
In light of this work, we have overhauled how we infuse person-centered in order for it to bridge well from coursework to our clinic supervision. Students can then have a person-centered care pathway for their learning as they go through the program. They can see the connections of how that will develop over time, the skills we are expecting them to gain over time, and what we are doing to teach them that.
Vital Talk Resources
VitalTalk has several videos. A number of things that they developed are completely applicable to audiology. I found it useful to get some information to share with students. If you are interested in reading more about it, motivational interviewing is a foundational aspect of a lot of what I am talking about.
Additionally, Motivational interviewing in health care: Helping patients change behavior is a textbook that is easy to get through. It is a great way to think about purposeful and strategic aspects of communication that I have been talking about, which are derived from motivational interviewing.
Citation
Munoz, K. (2020). Supervision: developing person-centered communication. AudiologyOnline, Article 27026. Retrieved from https://www.audiologyonline.com