Editor’s Note: This text course is an edited transcript of a live seminar. Download supplemental course materials here.
How Trainable Hearing Aids Work
Many of you recall when data logging was introduced in hearing aid technology 15 years ago or so. This feature allowed the hearing aid to store information concerning hearing aid use, which included changes in gain by the user. As technology advanced, it was recognized that this stored information could be used in different ways to alter the hearing aid fitting, which leads us to what we now call trainable hearing aids. In fairly simple terms, the hearing aid can “remember” what user adjustments are made, or in use at a given time, by using the data logging feature. Of course, the key to the effectiveness of this process is that the user has to make an adjustment in order for the hearing aid to collect useful information regarding desired changes to the original fitting. Some products will collect data that allows for the training of gain, the frequency response - particularly the high frequencies, and some products also allow you to train the strength of the noise reduction or other special features. In conjunction with the signal classification system, these training-related data sets can be categorized as a function of the listening environment. That is, totally independent training can be conducted for speech in quiet vs. speech in background noise vs. music. This type of logging can either be time-based or event-based, depending on the company or products that you are using.
Time-based means that the hearing aid records the situation, the input level, and the gain setting at periodic intervals, perhaps once every minute. For example, if the patient adjusted their hearing aids to a comfortable setting, and sat for an hour listening to music, the hearing aid would be continuously recording. If the patient did not make any adjustments to the hearing aid during this time, it would keep recording the same values. Although I know of no research to directly support this, it seems that this might be best for a patient who spends a considerable amount of time in a limited number of situations. The downside of time-based training algorithms, depending on how often they record, is that if a person is going in and out of different situations, and making several changes, the timing of the logging might miss a change. Likewise, if a person prefers to change the hearing aid a lot within a given situation, it might not always pick up on this.
A different method of training is what is called event-based training. This means that every time the patient makes a change to gain or the frequency response, the hearing aid records what is happening; the hearing aid only records when the user does something. That means the user has to do something to make this happen, otherwise, no data helpful for training is available. I would predict that the event-based strategy would be better for a person who is in many different situations and is good at making changes to the hearing aid. Whether the training is time-based or event-based, there are three critical pieces of information that the hearing aid is recording which potentially can be used to alter the original hearing aid settings:
- The listening environment. Was the patient listening to speech in quiet? In background noise? Was the signal simply noise with no speech present? Some models of hearing aids conduct independent training for four or more different listening environments.
- The intensity of the input signal. It is important for today’s products to train independently for different input signals, sometimes referred to as compression training, rather than just train overall gain. We consider this desirable, as it’s very possible that many patients will want to alter gain for soft inputs differently than gain for loud inputs.
- The action of the hearing aid user. Was gain turned up or down? How much? Was the frequency response altered?
As more and more samples are gathered, the hearing aid develops a preference profile for the listener. It evaluates all of the adjustments over time and predicts what setting the listener prefers, on average. The training is based on cumulative use over several weeks, as we would expect that the same listener may not pick the exact same setting every time. Ideally, the more information that is collected, for more inputs and listening situations, the better the average prediction would be. This could be for average speech, loud speech, speech in background noise, etc., depending on level of sophistication of the product that the patient is using. An example of this is shown in Table 1 for a fellow whose wife listened to music in their family room at different input levels, depending on the time of day and her mood. He, on the other hand, tended to prefer a fairly equal earcanal SPL all the time. Note in Table 1, had he consistently set his hearing aids for the inputs of 60, 65, and 75 dB SPL, and training was implemented, the hearing aid would have applied around 15 dB of gain for the 70 dB signal, and this could be predicted from the training that occurred from the other input signals (e.g., he tended to prefer an output around 85 dB SPL)
Artist Output in room Patient Gain Setting
Mumford and Sons 65 dB SPL 20 dB
Lumineers 75 dB SPL 10 dB
Dawes 70 dB SPL ?
Avett Brothers 60 dB SPL 25 dB
Table 1. Example of relationship between different inputs to hearing aid for music and the patient’s adjusted hearing aid gain.
The first generation of trainable hearing aids only trained for overall gain. As we’ve mentioned, today, many products train specifically for different input levels and classifications. It’s therefore important that the product has a good classification system, or situation-specific training will not work very well. Some situations are fairly easy to classify, such as speech in quiet; you can expect that that will be classified correctly in 95-100% of the cases. For various types of speech-in-noise situations, however, correct classification will not be this high.
Prescriptive Targets and Trainable Hearing Aids
Let’s talk about prescriptive fitting targets. Research has shown that the commonly used validated targets are a good starting point. But, we know that what has been determined to be the best for the average patient, isn’t going to be the best for everyone. And, some patients have listening goals that simply are not consistent with the goals of the fitting algorithm. We may use a fitting algorithm that is geared more towards maximizing intelligibility when the patient’s priority is listening comfort. We also know that the clinic is not a good place to determine what is best for everyday listening. Those of you who do clinical measures of loudness discomfort levels (LDLs) know that you can have a patient who listens to loud sounds in the clinic, and provides the desired rating of “Loud, But Okay.” But then, they go out the door and come back saying that things are too loud, even though in the clinic things were just right. The point is, the more that we can get our patients out in the real world making judgments about speech, noise, reverberation, environmental sounds, etc., and then adjusting the hearing aids accordingly, the happier the patients will be (well, it should work that way). If the patient can find their best setting in the real world, they should obtain maximum benefit from their hearing aids.
The Trainable Hearing Aid: Yes or No?
I titled this lecture “Friend or Foe” because I find that some audiologists are keen about trainable products; they like them and use them regularly. I also find that there are other audiologists who are dispensing hearing aids equipped with the trainable feature, but rarely or never implement it. Why is this? I’ve summarized some opinions I’ve collected over the past few years (often over late-night discussions) from audiologists on both sides of the fence.
Trainable Hearing Aids are a Good Thing
Here are some reasons why audiologists say they like trainable hearing aids:
- Gain and output adjustments: As we discussed earlier, preferred listening levels for many patients will be somewhat different than what has been determined by prescriptive algorithms.
- Loudness for different inputs: Compression training allows for the patient to shape the aided loudness growth function the match their specific levels.
- Hands-free operation: Training for different listening situations means the patient will no longer have to physically switch programs when they move from one setting to another.
- VC replacement: Many hearing aids are fitted without a VC control. For these patients, a loaner remote control device during the first few weeks of use will allow them to zero in on their desired gain and loudness levels.
- Taking “ownership”: The training process allows the patient to be part of the overall fitting, and to “buy in” to the outcome. The fitting process is now a partnership, and the patient is partly responsible for the success.
- Reduce patient visits: Many patients return to the clinic several times, often without appointments, during the first few weeks of the fitting for minor tweaking. This should be reduced with trainable hearing aids.
Trainable Hearing Aids are Maybe not Such a Good Thing
While the items listed in the previous section all sound pretty good, the fact is that most audiologists do not use trainable hearing aids. Why is this?
- Mental and physical skills: Many patients do not have the cognitive or dexterity skills to do the training.
- Hassle factor: It’s just one more thing to explain to a patient, who often is confused by the technology already. Patients want things to be simple.
- Who is doing the work: The patient is already paying the audiologist to program the hearing aid. They might question the audiologist’s abilities if they have to do much of the work.
- Turn a good fitting into a bad one: Considerable time often is spent on the day of the fitting getting everything programmed correctly. What if the patient messes everything up with training?
- Reduce patient visits: In theory, if training works, the patient will require less post-fitting visits. While some consider this good, other audiologists do not. It is during these post-fitting visits that they get to know their patients, demonstrate to the patients that they are problem solvers, which then leads to follow-up purchases and word-of-mouth referrals.
- OTC hearing aids: Some audiologists believe that trainable hearing aids are just another step in eliminating audiologists from the dispensing process.
What does the Research Say?
Although trainable hearing aids have been out for about eight years now, you will not find many published studies which have examined the use of trainable hearing aids. Why is this? It could be that this technology is simply not as exciting as, or viewed as less important than directional technology, digital noise reduction, frequency lowering, or the other features which have been more commonly studied. A contributing factor could be the complexity of research with trainable products. The subjects needs to use the hearing aids in the real world for at least a couple weeks, and you need a pair of hearing aids for all the subjects—if there are 20 subjects in the study, someone needs to fund 40 hearing aids. Compare that to a lab study with directional technology, where all data for a given participant often is collected in a few hours, and only two hearing aids are required for the entire group of subjects (e.g., the same pair of BTE instruments are re-used for all participants).
We do have some research to discuss, so let’s start with one I was involved in, conducted in 2006 and published in 2008 using first-generation trainable hearing aids (Mueller, Hornsby, & Weber, 2008). We included 22 participants and used a cross-over design, which means that all subjects were fitted with both conditions, but not at the same time. They were first in one group and then crossed over into the other group mid-way through the study; the starting group was counter-balanced. Each participant was fit to either 6 dB above or below NAL-NL1 targets, which was verified with probe-microphone measures. The participants used their hearing aids for 10 to 14 days at home. We activated all the special features because we wanted to make it as close to a typical hearing aid fitting as possible. At the conclusion of the study, we looked at their final gain setting, as well their listening conditions (e.g., quiet, noise, etc.), number of VC changes, and a few other things that could be collected through data logging.
The primary question we were trying to answer was, "Would the subjects train gain back to the NL1 prescription targets?" There had been several studies published prior to this about users’ preferred gain; most all of these studies concluded that people tended to prefer the NAL prescription. The interesting thing in almost all of these studies, however, was that the people started out at the NAL prescription. Our thought was that if they prefer the NAL and we start them out at above or below the NAL, then they should train back to the NAL if that is what they liked in the first place. In other words, we wanted to know if the starting gain for training matters.
What did we learn? First, we learned that there is a large variability among patients. We had some people who trained to 14 dB above the NAL and we had some trained to 14 dB below the NAL. Perhaps this was just coincidental, but if we combine the data for the two different training sessions, the mean and the median trained settings for the group were within a dB or so of the NAL-NL1 prescription.
The second point we wanted to explore was the effect of the starting point. When we started the subjects 6 dB above the NAL, they tended to settle in at approximately 2-3 dB above the NAL. When we fit them at 6 dB below the NAL, they tended to settle in at about 4 or 5 dB below the NAL. Again, these are the same people for each condition. It did not matter what setting they received first, as we did also analyze that. You might think that if they started off at 6 dB above, and stayed close to that setting for two weeks, and then switched to 6 dB below, they would train back up again, but they did not. There seems to be a wide range of “acceptable settings” for these people. The skeptics among you may say that perhaps they never trained at all. We analyzed this and found that to be untrue, because some people manipulated settings all the way down to -14 and up to +14 dB.
There are a few other points to mention about this study. On average, subjects used their hearing aids for 135 hours, with a maximum of 226 hours. There was no correlation, however, between use time and degree of gain learning. In other words, the people who used the hearing aids less did not have less gain learning. There also was no correlation between use time and deviation from the NAL target, or the time spent in different listening situations and the deviation from NAL targets. We believe that it was not that they were not training the hearing aids; the starting point does have an impact.
We recently did a follow-up with second-generation trainable hearing aids (see Mueller and Hornsby, 2014, for review). One factor of the first study (Mueller, et al., 2008) was that subjects were all previous hearing aid users. Perhaps the users tried to adjust the hearing aids back to the settings they were used to? Also, in the first study, we did not know if people trained the hearing aids based on soft sounds, which would have impacted average sounds, when maybe average sounds were adequate to begin with (e.g., because it was overall gain training, all inputs would be altered by gain adjustments).
In this second study, we fitted the participants to the NAL-NL1 before the onset of training. Again, they conducted training in their home environment for two weeks, although this generation of hearing aids had compression training, so the participants could train the gain different for soft, average and loud inputs. All subjects had used hearing aids for at least two years and were satisfied hearing aid users. We measured their preferred gain for their current hearing aids prior to starting the training, so we were able to use this as a reference. We questioned if the subjects would train gain differently for soft, average and loud inputs? Would they train the gain to match the gain they were using with their personal hearing aids? And, since we started them at the NAL-NL1 would they tend to stay close to this fitting?
Subjects could also train the frequency response for this hearing aid, and for data analysis, we averaged the training effects into two groups: a low band (below 2000 Hz) and a high band (2000 Hz and above). The more interesting findings occurred for the high band, so that’s what we’ll look at now. Figure 2 shows a comparison of trained gain to previous use gain and the NAL target gain for soft, average and loud inputs. This is the average real ear aided response (REAR) that you are looking at since we used speech mapping, not insertion gain, in this particular study. Note that there were no large differences between the NAL prescription, previous-use gain or trained gain for loud inputs (75 dB SPL). Things changed a little bit for average inputs, however. I should mention that all of the participants previously had been fitted at the same clinic. Their fitting philosophy was patient-driven, and as a result, you will see that they tended to under-fit their patients compared to the NAL-NL1 for both soft and average speech inputs.
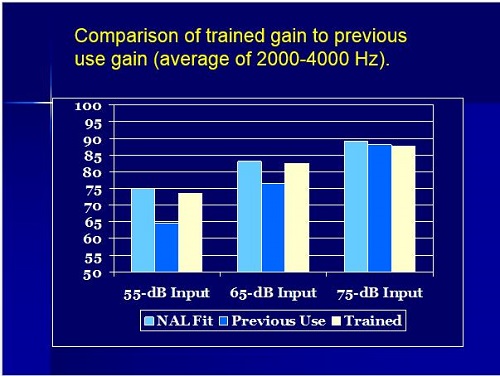
Figure 1. Comparison of average outputs for soft, average and loud inputs (2000, 3000 and 4000 Hz) for trained gain and previous-use gain with personal hearing aids. The average NAL-NL1 target is shown as reference.
The NAL fit is shown in turquoise (Figure 1); their previous-use gain looks to be about 6 dB lower, however, their average trained gain is very close to the NAL targets. The most interesting finding was for soft inputs (55 dB SPL). Observe that on average, they previously were using about 10 dB below the NAL-NL1 targets. However, they did not train down to their previous fitting; the final trained gain was fairly close to a NAL fitting.
We recognize of course, that if these participants never trained their gain, the outcome would be fairly similar to what is shown in Figure 1. Our data logging did show that on average, there was over 100 gain changes/participant during the duration of the training, but we thought we would also examine individual training data. Since the 55 dB input was where the deviation was the greatest from previous hearing aid use, those data are shown in Figure 2. These data show that 45% of the participants trained at least 3 dB or more; about 6 subjects trained higher, a few of them trained lower, and one outlier trained down about 17 dB. Recall that I mentioned earlier that some audiologists are not fond of trainable because they fear that a patient could mess up the fitting? Well, here is a case where it did, but his was only 1 person out of 20.
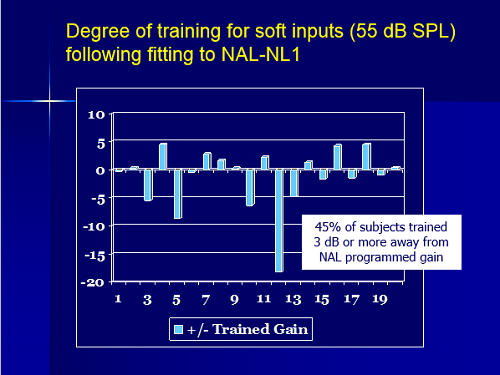
Figure 2. Degree of training for soft inputs (55 dB SPL) following fitting to NAL-NL1.
Remember that the subjects were people who used hearing aids for several years and were happy users. Figure 2 compared their final trained gain for soft inputs compared to what they previously were using for this input level. We noted that 55% of the subjects were now using 10 dB more gain than they had been with their previous instruments (Figure 3). You would have to think that 10 dB of audibility for soft sounds would have an impact on their life. For a detailed description of this research see Mueller and Hornsby (2014).
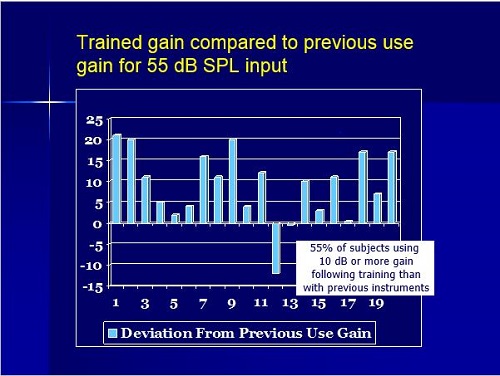
Figure 3. Trained gain compared to previous-use gain for 55 dB SPL inputs.
Other research on trainable that I think you’ll find interesting is from Catherine Palmer and her and her lab at the University of Pittsburgh, and published here at AudiologyOnline (Palmer, 2012). Catherine’s primary interest was if you going to use trainable products, when is the best time to start training? Todd Ricketts and I recently addressed this same issue in an AudiologyOnline publication (Ricketts and Mueller, 2014). Most audiologists seem to suggest starting training from day one, but Catherine speculated that maybe you should fit them to target, allow for a month of acclimatization, before you start training. Perhaps acclimatization to the NAL targets would influence their training down the road. A very good research question with important clinical implications.
All participants were new hearing aid users, and both groups were initially fitted to NAL-NL1. For the control group (n=18), training was turned off at the initial fitting and then activated a month later at the second visit. The experimental group (n=18) had training activated from the very beginning. Accordingly, the first group only had one month of total training while the second group had two months of training. Prior to training the HINT (aided, fitted to the NAL-NL1) and the Profile of Aided Loudness (PAL) was administered to both groups. The PAL is a subjective measure of loudness for different environmental sounds (See Mueller and Palmer, 1998, and Palmer et al, 1999 for review). Pre-training performance showed no difference between groups for the HINT.
The findings of this research revealed that gain for soft sounds was reduced slightly for both groups, and was reduced a bit more for the experimental group that had the longest amount of training. The speech intelligibility index (SII) for the control group was reduced by about two percent, as calculated by the AudioScan Verifit. The SII for the experimental group that trained for two months was about four percent for real-ear soft inputs. Unfortunately, we don’t know if this slight difference is because the one group trained longer, or if using the NAL-NL1 fitting for a month influenced desired gain levels.
Real-world loudness measurements after training using the PAL also were conducted. Palmer (2012) found no differences from programmed to trained gain for either group, and no difference between the control and experimental groups. Post-training HINT performance also was the same as pre-training for both groups.
You could view these findings in two different ways: because the results were no better, training does not work, or you might think of this as a positive—training did not make the fitting any worse. Patient preferences help make this determination. Following the HINT testing, the participants went out in the real world for 10 days. They were able to go use one program for one day, another program for another day, and so forth. At the end, they had to pick what program they would use if they could only use one. There was one subject who would not make a decision, but for the people who did, 65% favored the trained gain over the original gain. That is not overwhelming, but indeed, there is something to be said about the individual training. I believe Palmer stated that the main reason for this was listening comfort. Indirectly, these findings also are a validation of the NAL-NL1 for new hearing aid users, as on average, participants did not stray far from the original fittings. They did prefer slightly less gain, which may have simply made the fitting closer to NAL-NL2, which is now commonly used.
Editor’s Note: Since the time of this live AudiologyOnline presentation, another well-designed study on trainable was published by Keidser and Alamudi (2013), which may be of interest to readers. See Mueller (2014) and Palmer (2014) for a review of this research.
Audiologist-Driven Training
Most practicing audiologists who routinely fit to prescriptive target have encountered patients who are not happy with the gain and output provided. This is of course expected, given that it’s a target for the “average” person. Often, the complaint centers on the fact that there is too much gain. We’ve then all probably used the counseling technique that goes something like this: “You will get used to it in no time. You are just used to living in a quiet world. You’re really just hearing what all of us with normal hearing commonly hear.” Some patients, however, do not “get used to it” and simply stop using their hearing aids, or return them for a refund during the trial period.
A possible solution would be to use audiologist-driven training rather than patient-driven training. This is based on the notion that if we introduce something gradually it will be more acceptable than if we introduce it all at once. What I’m referring to is an automatic gradual increase in the hearing aid gain over time. Manufacturers have marketing terms for this, some make sense, others don’t. I am going to simply call it automatic gain increase (AGI), because that is essentially what happens.
AGI differs from the patient-trainable approach that we have been discussing. With traditional trainable hearing aids, you program to a validated prescription that is close to what you believe is best, but then allow the patient to fine tune louder or softer depending on their preferred listening levels. For AGI, the audiologist makes a determination of what he or she thinks is “best,” and then programs the hearing aid to less gain than this. Then the AGI is programmed to automatically increase gain gradually over weeks or months, so that at the end of this training, the gain is at the level which was initially desired (by the audiologist, not the patient).
Advantages of AGI
There are some new hearing aid users that seem to be gain-shy, and it’s pretty obvious on the day of the fitting that they would not be willing to use the gain which would seem to be appropriate. While you might feel guilty sending them out the door with the gain that they desire, yet you also sense that if you sent them out with the correct gain, they may never wear their hearing aids. AGI allows the audiologist to initially program the hearing aids at a level below what is desired, but at a level that is “acceptable” to the patient. Then depending on where you want your final gain to be, you can set the AGI to increase the gain in small increments. For example, if you were starting 8 dB below the desired setting, you could program a 1 dB/week increase over the next 2 months. A fitting tip: Before you send the patient out the door, be sure that the final gain destination will not create a feedback problem.
In my opinion, this feature will only work with hearing aids that do not have a VC, or a remote method to adjust the volume. If a patient has control of the gain, it seems probable that every week when the gain goes up 1 dB, they will just turn it down 1 dB, resulting in no gain changes for use conditions. I should mention that some people refer to this training process, or even the feature itself as “acclimatization,” but we have no way to know if there is going to be acclimatization. The software will not automatically cause acclimatization; it only employs an automatic gain increase. Acclimatization is an individual occurrence within the brain.
Audiologist-Driven and Patient-Driven Training
We have talked about two different kinds of training. Should we use both with the same patient? At the same time? In what order? We really have three options:
Option #1: We could implement both patient-training and AGI at the time of the fitting. That seems like a poor choice to me, as you have two different things going on, which could be working in opposite directions.
Option #2: You could use AGI first. This might help you push gain to a higher level than the patient might initially accept, which might take a couple of months. Then after they arrive at that higher level, you could implement training to fine-tune compression and obtain preferred gain for different listening situations. This seems reasonable to me, would be good for the patient who initially is not fond of much gain.
Option #3: The third option would be to use patient-training first. This would be for patients who initially accepted an appropriate amount of gain—recall the starting point does influence the ending point. Allow the patient to settle on a preferred gain for different listening situations; that might take a couple of weeks. Once this has been established, conduct probe-mic testing to determine how the fitting looks. If audibility is not optimal, you could then implement AGI.
AGI is something that you have in your back pocket to pull out for either Option #2 or Option #3, and the use would seem to depend on the patient’s first perceptions, or the outcome of training. I am mostly talking about new hearing aid users for these scenarios. We assumed that experienced users are fairly settled on their preferences. This might not be true, however, if they were under-fit for gain, and have been using hearing aids that did not have gain adjustments. Recall from the Mueller and Hornby data (2014), experienced users were using considerably more gain after training (when they were re-fit to more gain). Implementing these training procedures does usually involve a few more trips back to your office, but that is not necessarily a bad thing.
Clinical Implementation of Patient-Training
To successfully implement trainable hearing aids, you first have to ensure that the patient is in agreement that this strategy is good for them. You have to ensure that the patient is able and willing to make the necessary changes in real-world settings. Research studies on this topic are somewhat misleading, as we tend to only recruit patients who we’re fairly sure can conduct the training. In the clinical world, I would say about 80% of people could do the training. As you’ve noticed, even the elderly use smart phones and various remote controls more now than they did 10 years ago, and many people are more capable than you might think.
My recommendation would be to start with a fitting that is as close to your desired ending point as possible. Remember the starting point does matter. There is no reason to start below and think they will train up. Our research showed that they will not (Mueller et al, 2008). Here are some other considerations from a Keidser et al. (2007) study:
- When they surveyed a typical clinical population about trainable hearing aids, they found that 59% of adult hearing aid users were interested in training their own hearing aids.
- They found that the people who would be most successful were younger adults who have a strong interest in technology, people who have a milder hearing loss, and people who have less symmetrical hearing loss.
- They also found that 54% of those surveyed wanted to train using a remote, while 46% wanted on-board control. I think remotes are becoming more and more common.
- Interestingly, 82% of all those surveyed, whether they used training or not, thought that training would make the hearing aid fitting better.
When initiating training, I would encourage you to give the patient some detailed instructions. Ask them to go to different listening situations, and suggest they make gain changes whenever necessary to optimize loudness, listening comfort or intelligibility. That should result in a better overall fitting. I would also give them a diary where they could make a checkmark if they listened to loud music, soft music, loud noise, soft noise, etc., to give them some structure to the training process. This has worked well in our research projects. I’d suggest you monitor progress at about two weeks post fitting. Look at the data logging to make sure that they have been in different listening situations and see what changes are being made. At a one-month interval, assuming all is well, training likely can be discontinued if you want. You may have to implement AGI at this point.
At periodic intervals, you probably will want to implement training again for at least three reasons.
- The patient’s hearing loss may have changed.
- Their listening situations may have changed. Maybe the guy who was retired is now working part-time and is in a lot of background noise; he may need new training.
- You will also want to account for overall acclimatization. At some point, your new user will become an experienced user. It is difficult to determine on what day, or year, exactly, that a user becomes “experienced,” but when they do, they probably are going to want more gain.
Summary
Validated prescriptive fittings are a good starting point, but they are mostly geared toward certain attributes of amplification for the average patient, with an emphasis on intelligibility and appropriate loudness. Those may not be the attributes that your patient believes are most important, or, your patient may not be average. They may like more gain, less gain, have a different loudness contour, or have different listening interests. Trainable hearing aids will allow your patients to train the fitting to their environments and to their fitting goals.
References
Keidser, G., Dillon, H., & Convery, E. (2008). The effect of the base line response of self-adjustments of hearing aid gain. The Journal of the Acoustical Society of America, 124(3), 1668-1681.
Keidser, G., Dillon, H., Dyrlund, O., Carter, L., & Hartley, D. (2007). Preferred low and high frequency compression ratios among hearing aid users with moderately severe to profound hearing loss. Journal of the American Academy of Audiology, 18(1), 17-33.
Keidser, G., & Alamudi, K. (2013). Real-life efficacy and reliability of training a hearing aid. Ear and Hearing, 34(5), 619-629.
Mueller, H. G. (2007). Data logging: It’s popular but how can it be used to help patients. The Hearing Journal, 60(10), 22-31.
Mueller, H.G. (2014, January). 20Q: Real-ear probe-microphone measures - 30 years of progress? AudiologyOnline, Article 12410. Retrieved from: https://www.audiologyonline.com
Mueller, H.G., & Hornsby, B.W. (2014). Trainable hearing aids: The influence of previous use-gain. AudiologyOnline, Article 12764. Retrieved from https://www.audiologyonline.com
Mueller, H. G., Hornsby, B., & Weber, J. (2008). Preferred hearing aid gain using trainable hearing aids. Journal of the American Academy of Audiology, 19(10), 758-773.
Mueller, H.G., & Palmer, C.V. (1998) The Profile of Aided Loudness: A new “PAL” for '98. Hearing Journal, 51(1), 10-17.
Palmer, C. (2012, August). Siemens Expert Series: Implementing a gain learning feature. AudiologyOnline, Article 11244. Retrieved from https://www.audiologyonline.com
Palmer, C. (2014, May). 20Q: A review of 2013 hearing aid research—tips for the clinician. AudiologyOnline, Article 12672. Retrieved from: https://www.audiologyonline.com
Palmer, C. V., Mueller, H. G., & Moriarty, M. (1999). Profile of aided loudness: a validation procedure. Hearing Journal, 52(6), 34, 36, 40-42.
Ricketts, T.A., & Mueller, H.G. (2014, March). When is the best time to activate the 'training' feature in hearing aids? AudiologyOnline, Ask the Expert 12350. Retrieved from https://www.audiologyonline.com
Cite this content as:
Mueller, H.G. (2014, July). Siemens Expert Series: Trainable hearing aids - friend or foe for the clinician? AudiologyOnline, Article 12774. Retrieved from: https://www.audiologyonline.com