Editor’s Note: This text course is an edited transcript of a live webinar. Download supplemental course materials.
Learning Objectives
- Participants will be able to describe questionnaires with psychometric data that allow us to ask questions that will lead to signal processing and feature selection in modern hearing aids based on patient needs.
- Participants will be able to describe the evidence currently available to support the use of signal processing and hearing aid features for specific communication challenges.
- Participants will be able to discuss cases where the evidence base does not apply to individual patients.
Introduction
Dr. Catherine Palmer: Today’s topic of matching technology and features is near and dear to my heart, because of my work both in directing a research lab at the University of Pittsburgh, as well as fitting hearing devices and working with communication challenges with patients. We know that our patients have specific needs, and now we can use the evidence base to guide our clinical decisions as we try and address those needs. I want to thank Jenifer Fruit, Au.D., who works with me at the University of Pittsburgh Medical Center and helped put together this presentation.
Assessing Patient Needs
I will review techniques to assess individual patient communication needs that go beyond asking the patient, “Why are you here today?” More than ever, it is critical to document what we do and how we do it. I’ll be discussing a few measures to help you meet those kinds of requirements, but I also want to help you elicit more from your patients so you can understand their communication needs up front, so that you can use this information to match the required features and technology.
We will first examine the current evidence base to support various signal processing strategies. We have picked common strategies that are offered from all hearing aid manufacturers. Then we will look at the challenge of applying the evidence to individual patients. I will share a few case studies that highlight what happens when the strategy is not straightforward, and why we need expert clinicians as part of the hearing aid fitting process. While it is important to understand the evidence base, the evidence as a whole does not give us a recipe to apply to every patient. We need expert clinicians looking at that evidence and applying it to individual patients. We have some examples from our clinic to demonstrate how to go about making these decisions.
Standard Measures
Let's start with some of the standard measures and forms we can use to assess patient needs. As experienced clinicians, we usually believe we are pretty good at talking to patients. I think audiologists are already doing a lot of what is captured in these measures in an informal manner, but there are a couple of reasons why you still might want to use more formal measures. I am interested in any comments you may have of what measures you have found helpful and how you use them in your practice.
Figure 1 is an example of the Client Oriented Scale of Improvement (COSI; Dillon, James & Ginis, 1997). It is a fairly popular measure and it is incorporated in the software from some of the hearing aid manufacturers. It is also available as a standalone form. Interviewing with the COSI helps you find specifically what patients want to be able to do once they are wearing their hearing devices. It is important for these interview questions to be very specific statements. You do not want the patient to tell you that they want to hear and understand in background noise. Clearly, every patient wants that, but you are looking for measurable outcomes. You want something more specific such as, “I want to be able to hear at the dinner table with my immediate family. I want to hear my friends talking when I play bridge.” You want to capture the patient’s most important, specific goals. In a sense, you and the patient are saying up front, “These are the most serious goals of this treatment.” With the COSI, when used during the pre-fitting process, you identify the situations where the patient would like to see improvement with his or her new amplification. Post-fitting, you measure the patient’s reported change in hearing function for each situation, as well as his or her final hearing ability. Those are your post measures to see if you succeeded in meeting the goals of the fitting. The COSI is an effective way to structure an interview and capture with the patient what you mutually agree to work on.
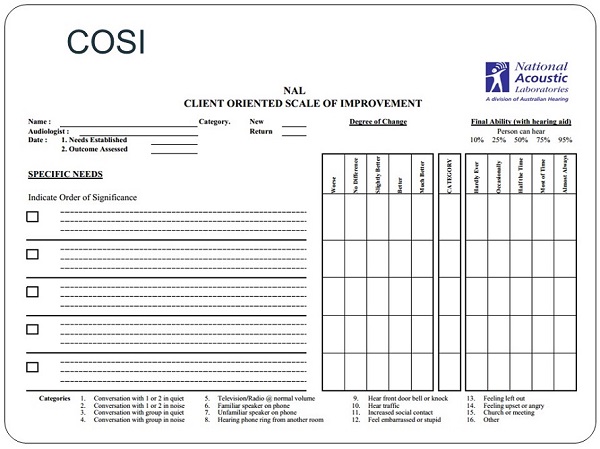
Figure 1. COSI interview form. View larger version of image (pdf)
A similar form called the Patient Expectation Worksheet (PEW) was developed in my lab at the University of Pittsburgh (Figure 2). It was done in parallel; we did not know the COSI was being developed and they did not know that we were working on the PEW. The two groups came out with slightly different ways of looking at patients’ needs, but the goal of the two questionnaires is similar. With the PEW as with the COSI, you are trying to capture the few primary reasons as to why this person came in for new hearing devices. We have conducted research with this measure, and found that people are only reliable at repeating their top two goals. If you push someone to give you five goals, and two weeks later you ask them what their goals are, they probably will only be able to tell you the top two. So, the PEW captures two primary goals. This does not mean that there are no other goals, but these are the two things we will address when we are selecting hearing aid features and levels of technology. That is very similar to the COSI. The difference with the PEW is that we also consider how the person is doing currently.
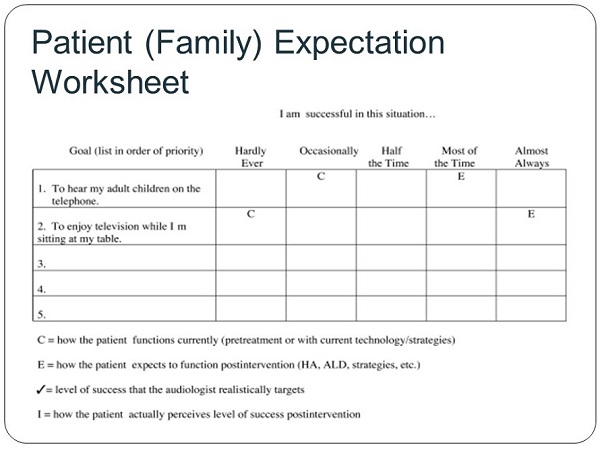
Figure 2. Patient (and family) Expectation Worksheet. View larger version of image (pdf)
The C used on the PEW form is for “currently.” We are asking, “Are you successful in this situation?” with answers of “hardly ever” to “almost always.” This is different from the COSI. We also have a pre-measure where we say, “Tell us how you are doing now” We also attempt to reveal their expectations. Based on the treatment they have chosen, what is their expectation of how well they are going to do post treatment? We have found this helps in managing expectations. For example, consider a person who needs bilateral power behind-the-ear hearing aids (BTEs) but has chosen a monaural completely-in-the-canal (CIC) device, and expects to do well. In this case we would take a pause in the conversation and align their expectations with the choice they have made. That helps post treatment, and it may help shift them to a different treatment, which can also be beneficial. The person will say what their expectation is, and we will record that on the sheet shown in Figure 2.
Evidently, in this example (Figure 2), we have agreed with them, because we have left those expectations alone. This is a nice way to see if you have met or exceeded people's expectations. That is one way to look at it. The other way to look at it is to see if you have moved categories beyond how they were doing at the onset.
The next scale I’d like to discuss is the Abbreviated Profile of Hearing Aid Benefit (APHAB; Cox & Alexander, 1995). If you are in the market for either pre- or post-test measures, you will want to go on Robyn Cox’s website (www.memphis.edu/ausp/harl/). There you can download some of these measures for patient use. Hers is certainly the lab that has produced most of our outcome measures that are psychometrically tested and have reliability and validity data. They are powerful measures in that sense. The APHAB has 24 questions. For example, one is, “When I am in a crowded grocery store talking with a cashier, I can follow the conversation.” Patients will indicate how they are doing at the present time without the hearing aid, and in the post-test, will indicate how they are doing with the hearing aids. They can see their previous answers; that is part of how this is validated. If they are current hearing aid users getting new hearing aids, they can compare old with new technology.
The result is four subscale scores for ease of communication, reverberation, background noise and aversiveness to sound. I think this is a powerful measure. In our busy clinic, and maybe yours too, we have never found a good way to get this answered and scored in a timely manner as a way to use it to help select technology. We definitely use it more as a post-test measure. If we are trying to use it as a quality indicator for the clinic, it works. But we have found it cumbersome to use as part of the counseling. For counseling, I think it would be helpful to have it on a tablet. People can click away and receive scores automatically each time they come to the appointment. We are not set up to do that at our clinic, and some of our population would have a hard time with that. We find that patients want to sit with us and go through all 24 questions, which does not work well with our scheduling. If it works with yours, it is certainly a measure that will give you a lot of good information about how the person is doing with amplification.
Next, we have the TELEGRAM from Linda Thibodeau at the UT Dallas Callier Center (https://www.utdallas.edu/~thib/). I think this measure will start being used more with all the accessories that are now integrating into hearing aids. In the past, accessories were more like add-ons that were not specific to the hearing aid; now manufacturers are working hard to make integrated systems. This questionnaire reminds you to to talk about specific situations such as using the phone, ask about hobbies, and discuss alerting systems. It goes beyond focusing on just the hearing aid, or how you hear others in everyday conversations. It looks at all the auditory signals that might be important in addition to speech. Note that the TELEGRAM is not a post-test; rather, it positions you to consider accessories in your recommendation for technology.
Reviewing the Evidence
Let’s think about the evidence now and some terms we will use when we talk about evidence. We talk about efficacy, effectiveness, and less commonly, efficiency; although, I think we should be talking about efficiency more often. Efficacy is the kind of research that tells us if something can work. This is research that is generally conducted by the manufacturers, because they do not want to release products and features that cannot work. An example of an efficacy test would be testing the directivity index of directional microphones in an anechoic chamber. You present sound and noise at certain levels from specific locations, and you show that the signal processing does work under ideal circumstances.
Effectiveness means, “Does it work in the real world for an average patient?” Effectiveness is more about obtaining real-world results or experiences from people who are using technology out in the field.
Efficiency means, “Is it worth it for my patient?” Maybe it works under ideal circumstances and in the real world, but if there is a big cost differential, would that be worth it? For example, say there was some kind of powerful feedback management system that made you purchase a high-end hearing. That technology added $1,000 on to the price of the hearing aid, when a more closed fitting might have solved the same feedback problem for some patients. That would not be worth it. It might be better to have a tighter ear mold than to have an open ear mold and pay that much more for a technology feature. For another patient, it might be very well worth the extra money. That is where you come in as a clinician, to determine what is important to each individual patient.
Meta-Analysis
Meta-analyses are the most powerful evidence a clinician can use to answer clinical questions. A meta-analysis means someone has taken several data sets from different publications and combined them, which has given them more power to answer a clinical question. For example, the clinician might wish to answer the question, “Does noise reduction improve speech intelligibility?” There are 20 or more publications addressing this, and they may be able to combine some of these data and have a more powerful answer. Unfortunately, we do not find many meta-analyses related to the selection and fitting of hearing aids. Likely the most common barrier is that so many studies use different outcome measures, and as a result the data cannot be combined. To combine data, you have to have the same or very similar outcome measures. There has been a push from different research labs to try to standardize some of our outcome measures so we can combine information. However, there are not an abundance of meta-analyses published in our field to date.
Systematic Reviews
A systematic review means someone has asked a very specific clinical question and then they have looked at the most recent literature and answered that question. You can look at the question, and if you are not interested to see how the systematic review works, you can skip to the end and get the answer to that clinical question. Then you apply it to your specific patient, keeping in mind all the things that make your patient different from the average. That is a nice starting point. There was an issue of the Journal of the American Academy of Audiology (JAAA) dedicated to systematic reviews in 2005, which is almost 10 years past, and we hope to see some of those updated. In 2012, Ryan McCreery from Boys Town published a set of systematic reviews. If you are interested in pediatrics, you can read his reviews of recent data behind frequency shifting, noise reduction, and directional microphones in the 2012 American Journal of Audiology, volume 21.
Scoping Studies
Scoping studies are not new, but it seems they have recently become more popular. A scoping study is broader than a systematic review. It is a report on everything we know about a topic at this point, but it does not necessarily provide an answer. A scoping study often comes up with more questions, and points to the kinds of studies that need to be done. For a clinician, a scoping study may be more frustrating than not. It can be helpful if you want to know the status of the area of interest, but it does not give you answers to apply on Monday morning.
Figure 3 shows the categorization, or levels, of evidence as well as the grades of recommendation. These were first described by Robyn Cox in 2005. You can see that systematic reviews and meta-analyses are the highest level of evidence. Next is randomized controlled trials, which we are seeing a little more often in our field. We see more nonrandomized intervention studies. The levels span all the way down to expert opinion, which is sometimes used, but is not how we want to base our clinical decisions. We want to have a higher level of evidence than “opinion.”
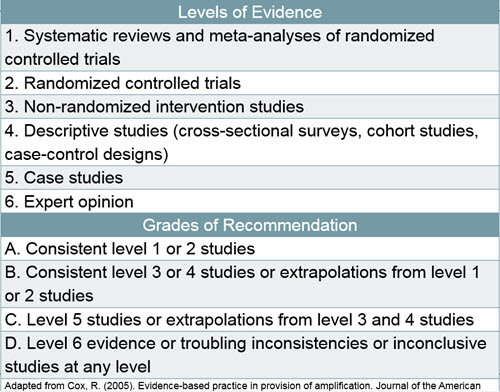
Figure 3. Levels of evidence and grades of recommendation.
The grades of recommendation help you determine how compelling is the evidence. If you are conducting research and you cannot find a systematic review that answers your clinical question, you should search for the answer. It has to be something that is done in a timely manner. It used to be that people frowned upon Google Scholar and said the research had to be in PubMed, but the opinion has changed on that. Google Scholar seems to be a good way to quickly get information. You want to do a very specific search and pull up one or two articles that answer your question. It is not like being in graduate school. If you are interested in studying about directional mics, you do not want to read everything ever written about directional mics. You want to know how the directional mics on current hearing aids are working.
Figure 4 is a screen shot from a Google Scholar search. Go directly to scholar.google.com to do this. By selecting “since 2013”, we are asking for the most recent information. I do not care how directional mics worked a decade ago, because technology changes rapidly. This particular search took 24 seconds and turned up about 1,400 results. You can prioritize the results by which are most relevant. The first page is often sufficient and should have an article that will answer your question. It is empowering for a clinician to do this kind of search every now and then to keep up with current trends and areas of interest.
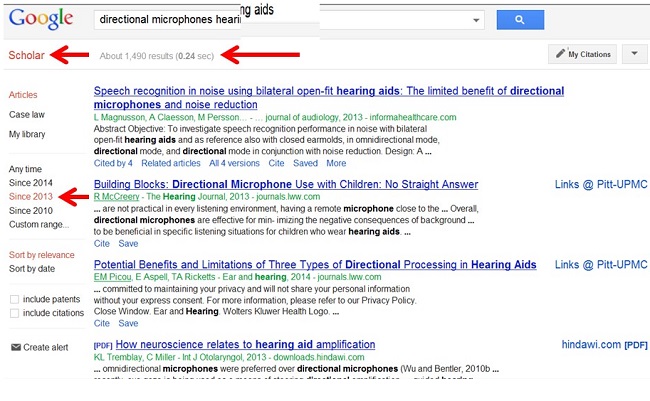
Figure 4. Screen shot from Google Scholar on “directional microphones.”
Current Evidence
As we talk about current evidence, I am going to ask you to vote true or false in response to some statements:
Editors Note: Online polling was conducted during the live webinar.
The first statement is, We currently have evidence to support the use of open fittings when possible. That is a true statement, with the appropriate patient. We certainly have some data now to show that it makes a difference for people related to sound quality and listening comfort.
Next, do we have evidence to support the use of frequency shifting or frequency transposition? Two-thirds of you have indicated that you believe we do have evidence to support frequency shifting and one-third of you do not. I am going to say that this is false, as we do not have evidence to support this. However, I am going to come back to it, because it could be true or false, depending on the specific question you ask and the supporting research you look at.
Automatic adaptation is when you set the hearing aid to automatically raise gain over time without having to go back into the fitting software and make gain adjustments. Do we have evidence to support this? I have listed this as false. However, just because we do not have evidence on something does not mean it does not have benefit. Sometimes we have pre-evidence, and we will talk about that. Also, having evidence does not mean it will work for your individual patient.
The next question is on gain training. Gain training means the person is fit with a hearing aid and they have a remote control with a volume adjustment. The hearing aid will learn over time and change the fitting based on the user’s preferences; it will do this automatically for different input levels and different listening conditions. Do we have data to support gain training? We do have some data on gain training that would suggest it is a reasonable feature to use for patients. Findings show that they do not reprogram the hearing aid to unreasonable levels. We have some evidence to suggest that it is a helpful fine-tuning feature, with the caveat that the fitting needs to start with a match to NAL or DSL targets, and then people train to their preferences from that point.
The next question is on noise reduction for comfort. Do we have evidence that noise reduction increases listening comfort? Yes, we have compelling evidence that noise reduction can lead to listening comfort, and that informs our clinical judgment regarding how to apply it. Each hearing aid company implements noise reduction differently, and that is one of our challenges as clinicians. We have to understand how each particular manufacturer uses noise reduction in their products. In general, it does increase ease of listening and listening comfort.
Do we have data to say that noise reduction will improve speech recognition? No, we do not have data to support that. In fact, the data suggests noise reduction, on average, does not increase speech intelligibility. This makes sense, as most noise reduction schemes reduce gain, which can negatively impact speech intelligibility. We keep hoping for different results on that question, but we are still seeing that it does not increase speech intelligibly. There are studies, however, noting that it does not decrease speech intelligibility either, which could be just as powerful a finding. The fact that noise reduction increases comfort without decreasing speech intelligibility is positive.
Do we have evidence to support the use of directional mics? This should be a no-brainer for you. Yes, we certainly do have evidence that directional microphones increase understanding in noise if the person wearing the technology is manipulating their environment appropriately.
What about adaptive directionality? Do we have data to suggest adaptive directionality is more useful than fixed directionality (fixed meaning you have one polar plot, adaptive meaning it is changing depending on the origin of the speech signal)? While there is not a lot of real-world data available, we do have some good simulated real-world studies that support the use of this technology. For example, with the earlier adaptive technology, where the polar pattern null would fall somewhere in the rear hemisphere, Ricketts, Hornsby and Johnson (2005) showed that in a reverberant room, the adaptive directional technology provided a significant improvement for a moving noise source (when the noise source moved across the rear hemisphere). The application of adaptive directional has been extended to the extent that today, the focus of the polar pattern can also be to the sides, or even to the back. Regarding the latter condition, under ideal conditions, Mueller, Weber and Bellanova (2011) showed that this anti-cardioid pattern provided a 5 dB SNR advantage over omnidirectional and a 10 dB SNR advantage over traditional directional when speech was presented from behind the listener.
The most common use case for the anti-cardioid condition is talking to passengers in a car while driving, including someone talking from the back seat. To simulate this condition, Wu et al, 2013) conducted speech-in-noise recordings on the KEMAR seated in a van traveling the Iowa Interstate highway. Three different pairs of hearing aids employing this technology were used on the KEMAR for the recordings. When the recorded signals were presented to a group of hearing-impaired listeners, again, the adaptive technology provided a significant SNR advantage compared to traditional directional and omnidirectional.
Next is the topic of remote microphones, or a microphone that is put near the signal or talker you want to hear. Do we have data to support the use of remote microphones? Yes, we do. I am someone who promotes evidence-based practice all of the time, but I think we can sometimes take it too far. We may think that we need a mass of studies on every type of feature and every type of signal processing, when sometimes it comes down to simple physical or acoustic facts. A remote microphone is a great example of an acoustic fact. It is an acoustic fact that if I pick up the signal from the source, therefore bypassing the noise, and put the signal directly to the ear, I will improve the signal-to-noise ratio (SNR), often as much as 10-15 dB, or even more. Improving the SNR will improve speech intelligibility. I do not need a randomized controlled study to verify that. I think as we want to continue to look to an evidence-base for what we do, we also have to use common sense and good judgment when acoustic or physical facts support a clinical decision.
Another example of using good judgment would be in fitting earmolds to children. It is widely known, even amongst evidence-based pediatric fitting protocols, that children will need to obtain new earmolds every few months when they are infants and toddlers. We do not need a massive study to prove that. Children grow; that is a physical fact. Therefore, we know they need new earmolds. Keep this in mind when you are searching the literature for an answer to a clinical question. You may be searching for an answer that does not need a well-controlled study to support it.
Binaural synchronization refers to when you change the volume or program on one hearing aid and the same change is made synchronously to the other side. Do we have data to currently support the use of this feature? Except for a couple of Trade Journal articles, the answer is no. We do not have data to suggest that it makes a difference in communication. We do not have data to imply that it hurts anyone, either. This is another good example of a feature that may not have proven benefit to the patient, although today it often is included without extra charge, even for entry level products. As a clinician, however, you would not want tell your patients that there is a specific evidence-based benefit as that would not be an accurate statement.
Next is the increased number of channels for speech understanding. Does having more—10—20—30 or more channels in a hearing aid mean better speech understanding? No, the data does not support this. The fairly compelling data suggest that two to four channels are all that is needed for fine tuning for speech understanding, and the benefit does not increase beyond that. With that said, having many channels can be beneficial to manage feedback.
Lastly, what about real-ear probe-microphone measurements? Do we have data to support the use of this verification approach? Most of you are going to say yes on this, and that is indeed the case. I added this topic because I want to point out that conducting probe-mic measurements, in and of themselves, is not a treatment. Everything else on this list is a treatment. Real-ear measures are not a treatment, but a way to measure if we have achieved our goals with a treatment, and the treatment is audibility. There is compelling evidence that sounds have to be audible in order to be understood. That may sound like a ridiculous statement as it is common sense, but there is evidence. Currently real-ear measurements are the most efficient and accurate way to measure that we have achieved audibility with a hearing aid fitting.
There are recent studies indicating that using manufacturers’ first fit or patients’ opinions do not lead to an appropriately audible signal. Three studies published in 2012 and 2013 showed that real-ear measurements increased people's performance with hearing aids, and had other positive benefits. I’ll discuss these studies when we talk about verification. Again, it was not the real-ear measurements alone; it was using them to fine-tune the hearing aid to produce appropriately audible signals at soft, moderate, and loud levels. I added this so you would be aware that evidence is always about a treatment, not a measurement. You then pick the measurement that allows you to verify the specific treatment that you are using.
Frequency Shifting
Let’s start with frequency shifting. We previously indicated that we do not have enough evidence to support that. Three studies (Ching, Day, Zhang, Dillon, VanBuynder, Seeto, et al., 2013; Alexander, 2013; McCreery, Brennan, Hoover, Kopun, & Stelmachowicz, 2013) are shown in Figure 5 which do give you the right level of evidence. The Ching et al. (2013) and McCreery et al. (2013) studies are a level two, meaning they are randomized control trials, and the Alexander (2013) article is a meta-analysis, so it is a level one. They are also given grades of A and B. The asterisks tell you that we have lowered the grade on the Ching et al. (2013) study, because that was conducted with pediatrics, and today, I am focused on adults. That does not mean she did not do a good study; it just means that it does not directly apply to the population I am talking about. There are two asterisks by the McCreery (2013) study, which is a great study, but it was done with normal-hearing individuals. That was a prototype processing at the time, and it will be interesting to see how this algorithm performs for people with hearing loss.
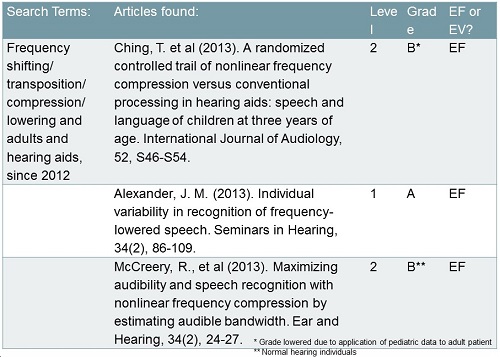
Figure 5. High-level evidence pertaining to frequency shifting.
Ching’s (2013) study tells us that on average with their group, there was no evidence to support the use of frequency shifting. Alexander (2013) and McCreery’s (2013) studies would indicate there is evidence to support the use of frequency lowering. Let's think about why that might be. Figure 6 is an example of a patient I have seen with a severe, precipitously-sloping, high-frequency hearing loss. You are not going to be able to give adequate gain for this person at 1500 Hz and above. This is exactly the patient you would think would benefit from frequency transposition. This is where I think you have to interpret the current evidence depending on your goal. Some of the studies, like Ching et al. (2013), are looking at many different types of hearing losses, and their point of using frequency shifting is because they believe the bandwidth of hearing aids is still too limited. When you look at the many studies of Pat Stelmachowicz, we clearly see the need for a wider bandwidth, and therefore the shifting is used for all patients to pick up some of those high frequencies. When you look at that group of subjects, you do not find a positive result. You do not find a negative result, but you do not find a positive result. When you look at Ryan McCreery’s (2013) work and specifically target people with this hearing loss, they can achieve benefit. This is why I think we are seeing both. We are applying this to two different populations. This is certainly the population to which I would think about applying the technology. Part of Ryan McCreery's (2013) article talked about how we have to verify that.
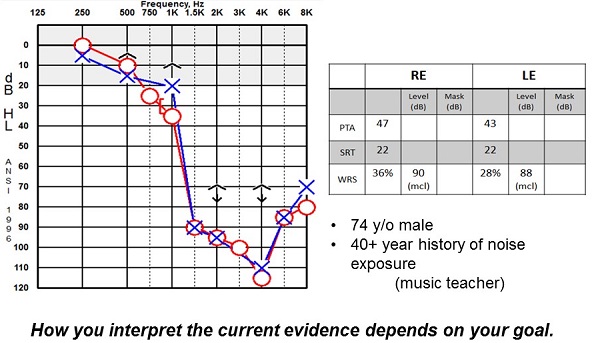
Figure 6. Example of a patient with precipitously sloping hearing loss who would seem to benefit from frequency shifting.
Figure 7 is a picture of the Siemens programming screen. However, this type of programming screen is similar to other manufacturers. This is how we set the frequency shifting point and the compression ratios, meaning where and by how much we compress that sound down.
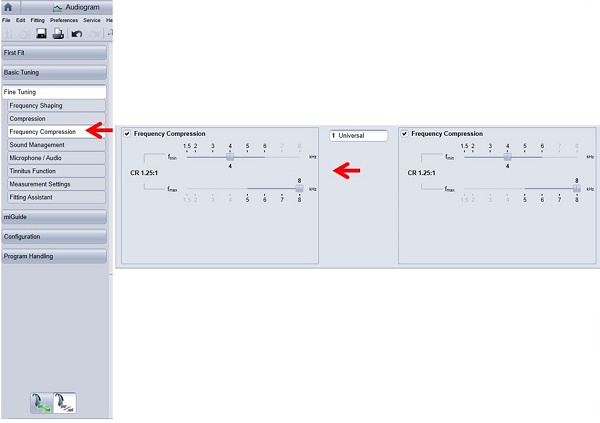
Figure 7. Example of Siemens programming screen to adjust frequency point and compression ratio.
Figure 8 shows a Verifit screen, to back up with what McCreery et al. (2013) reported. We do have to verify this. If you use the default from the manufacturers, you do not know that you have made the signal audible, and therefore, it is definitely not going to help the person. It will not hurt them, but it will not help them. I think that is why we may hear clinicians say, “My patient did not say it sounded distorted at all.” That was probably because they did not hear it at all. The compression is a distortion, but it is a purposeful distortion. We are trying to distort the high-frequency sounds so we bring them into a range of audibility. You can play very specific bands of sound on the Verifit and physically see the shift (Figure 8).
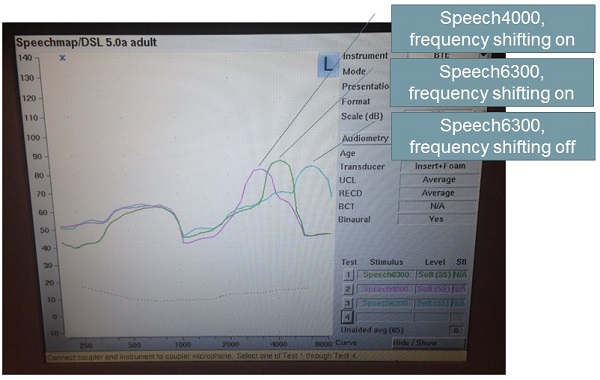
Figure 8. Speech mapping from the Verifit, showing filtered runs with frequency compression turned on at 4000 Hz 6300 Hz and again with frequency compression turned off at 6300 Hz.
You can see the 6300 Hz has shifted down when the compression is turned on. When you overlay the audiogram, you can see if you have made the sound audible for the patient. You do want to verify this feature with every patient.
Noise Reduction
We mentioned that noise reduction does help with listening comfort, and there are three supporting studies shown in Figure 9 (Liu, Zhang, Bentler, Han, & Zhang, 2012; Magnusson, Claesson, Persson, & Tengstrand, 2013: Brons, Houben, & Dreschler, 2013). These studies are levels three and four. They are not randomized controlled trials, but they are nicely done. Two received a grade of B, which is a solid grade, and one is a grade C. The top two studies are the most compelling. They looked at different kinds of noise reduction and the fact that it makes people more comfortable during listening. Liu et al. (2012) specifically looked at transient noise.
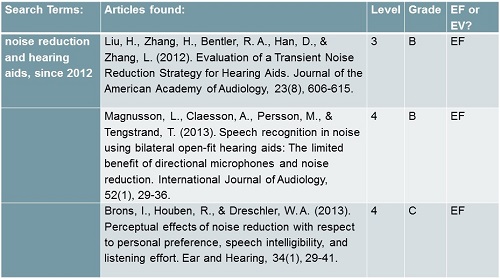
Figure 9. Three studies supporting the use of noise reduction for listening comfort.
I pulled the file of a hearing aid patient I see. He is happy with his hearing aids and says that he receives benefit in many situations. He has moved into independent living, where they dine in a dining room each evening so people can socialize. He finds the sounds of the dishes and silverware to be very uncomfortable. This is the kind of real-world example to which these articles about transient sounds would apply. They provide compelling evidence that this technology works. Of course, each manufacturer implements noise reduction differently so you have to be familiar with what parameters are used.
Figure 10 is another screenshot from the Siemens programming software. There are small icons showing a cup and saucer, which is exactly the kind of sound my patient was describing. I can make the noise reduction much more aggressive. Siemens calls this type of noise reduction Sound Smoothing. There is evidence to say that this does help with transient sounds. If that is the complaint your patient has, it is great to be able to say, “I can help you with that. There is something I can do to change that.”
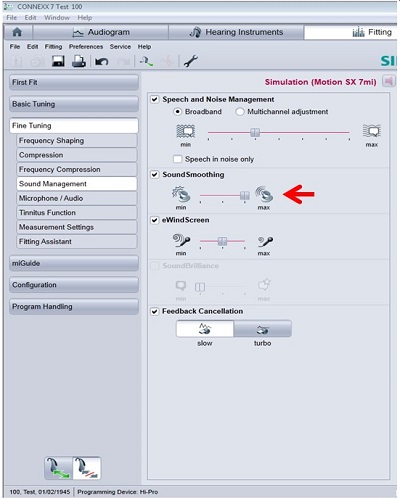
Figure 10. Siemens fitting screen where transient noise reduction (Sound Smoothing) can be adjusted.
Remote Microphones
I mentioned the acoustic fact that if you put the sound by the source, you are going to have an improved signal-to-noise ratio. The two level-four articles seen in Figure 11 are old (Fitzpatrick, Seguin, Schramm, Armstrong, & Chenier, 2009; Hawkins, 1984), especially Hawkins (1984), who did the seminal article with FM systems. I think the reason we are not seeing newer articles is because it is an acoustic fact. It is not that interesting to study this. We know remote microphones help as a function of their location. Linda Thibodeau (2014) is starting to produce research that looks beyond the remote microphone to the technology that is used to transmit the signal. This will be an important area to pay attention to as we have different transmission choices.
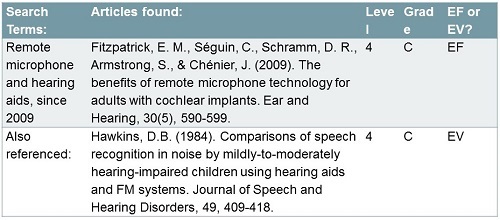
Figure 11. Research evidence for remote microphones.
Figure 12 shows some pictures of wireless systems from different manufacturers, with Siemens in the middle. We are seeing a lot of integrated systems that do not have to be purchased at the same time as the hearing aid. This can be nice if your philosophy is to get a patient fit with the hearing aid and see how much advantage that gives them, and then add on an accessory. In this way, you do not feel like you are retrofitting, because the hearing aid is ready to accept these devices whenever you put them on. In our clinic, we are struggling a bit with the timing of appointments, and when to add these things and how much time to add in order to explain and demonstrate them. You are probably all struggling with the same. The timing is changing our model a bit, but in a good way. It is helping people.

Figure 12. Examples of wireless microphone and FM technology from different manufacturers.
There are a couple of companies now who work with the iPhone. Right now, these connections are not doing any more than any other connections we have been using, but it certainly points to the way of where we are going. We will see an increase in smartphone technology with our hearing aids. Currently, the model of using your smartphone as the remote microphone is a little problematic in my opinion. I am trying to picture myself handing someone my phone at the end of the table so I can use it as a microphone, and then my 16-year-old texts me something totally inappropriate, which the user of the “microphone” will see. You have to figure out how your patient uses their phone and how comfortable they would be to use it as their microphone.
Automatic Adaptation
We talked about the fact that we do not have evidence for automatic adaptation, but that is because we are pre-data. My lab is one of a few doing a rather large study on automatic adaptation that will be published soon. We will have some data for how we use this and how it impacts people. This does not mean that automatic adaptation is not working or a bad feature; it means we do not have data published on that. One study that we do have is by Schum (2001), but it was a level-six, grade-D study.
Figure 13 is an example of an audiogram of someone for whom you might consider using automatic adaptation. They have a high-frequency hearing loss and are not used to all those high-frequency sounds. We all know that those patients probably will not like the hearing aid in the beginning. We often hear the complaint that the sound quality is tinny and sharp. If there is someone who cannot get into the clinic on a regular basis, it might make sense to use the adaptation feature and slowly build up the gain of high frequencies over time, as long as your fitting was correct in the first place by verification of targets. Of course, you do have to consider the interaction of the automatic gain increase and the volume control—if the patient has one.
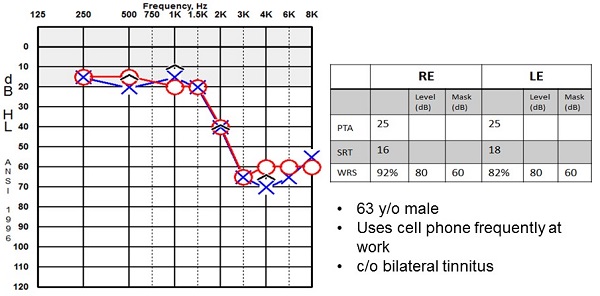
Figure 13. Example of a patient with a high-frequency sensorineural hearing loss that might benefit from automatic adaptation.
I think adaptation, gain training, and use of volume controls and programs can increase patient participation. There are data now in different fields about how important it is that the patient is an engaged, full partner in their care. This is permeating all of healthcare. We have to make sure the patient is part of these decisions. As we see more controlled reimbursement for patient care, that will be the theme. The patient has to think about their options. We want to think about that in what we do as well, whether it is reimbursed or not. Research suggests better uptake of and adherence to whatever the healthcare recommendation is made, which would be device use in our case.
When you are matching technology to people’s needs, it pushes you towards patient-centered care, especially if you are starting with an interview using one of the forms we talked about previously, where it is clear to the patient that you are gathering information. You are respecting their opinion on things that pertain to their life and creating solutions around it. Patient-centered care is a buzzword, and I think we are and have always been good at it. I think we want to promote that and quantify it a little more than we have in the past. We should have it work to our benefit.
Verification
Figure 14 shows recent studies that addressed verification of hearing aids (Abrams, Chisolm, McManus & McArdle, 2012; Leavitt & Flexer, 2012; Aazh, Moore, & Prasher, 2012; Boymans & Dreschler, 2012). In a sense, you do not need evidence for verification, but you need evidence for treatment, and again, the treatment is audibility. These authors did a nice job in showing how verification impacted fittings. People were more adherent to their use of hearing aids; there were fewer returns; they had better performance. These studies made compelling arguments for the use of real-ear measurements as a way to verify audibility. Currently, it is the most efficient way, and if tomorrow someone comes up with a better way, then we will all use that. It is the best thing we have at the moment.
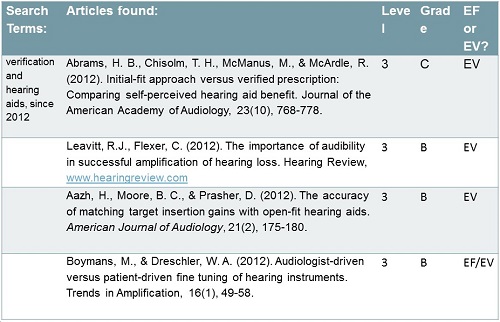
Figure 14. Research evidence for verification measures.
Audibility is the treatment, and without audibility, patients cannot benefit from any features or signal processing schemes. Every now and then, you will see a publication that indicates that there is no evidence to support some kind of treatment. If you read carefully, you realize they did not verify audibility, so that is an unfair statement. One study about a year ago looked at open fittings with directional microphones and stated that you get no benefit from directional microphones with an open fitting. However, when looking more carefully at the article, they had not made the gain in the high frequencies audible. If you do not have audibility of sounds, then your directional mics are not going to help. You have to be careful about some of what you are reading and be a critical consumer of the research.
You also want to measure hearing aid features. If you turned on directionality, you want to measure it. You can measure it on the real ear or in a test box, if that is easier. If it is an important feature that you have chosen to use with your patient, you want to measure it and know that it is functioning. When they come in a year later, you want to measure it again. One thing we do know is those microphones can get out of calibration, dirt and debris can become lodged in the inlet ports, and you do not have the directionality that you think you do. There are quick ways to measure that.
The same goes for the telecoil. Not too many people use telecoils for the phone anymore as there are better technologies, but we are seeing an upsurge of looped theaters in the United States. We have a couple in Pittsburgh now, and having a telecoil can be useful to people. You want to measure that response, because some telecoils have very limited responses. You need to ensure a broad telecoil response, especially if the person is going to try to listen to a symphony or a play. Phone-only listening does not require as broad a response, because the phone itself does not output a broad response. You can measure telecoil response on the real ear, but you can also measure it in the test box if that is faster for you.
We have talked about several different technologies and the evidence behind them, with some examples of people with hearing losses. So what do we do with that? You have provided an intervention, such as hearing aids, and the patient has been using it for a while. Maybe you fine-tune it little bit, and now you want some kind of outcome measure. We are all going to be pushed, whether we are reimbursed or not, to have outcome measures. This is going to be a big piece of healthcare. I would suggest as audiologists that we position ourselves as the people collecting outcome measures, so that when we are put in the position of why to go to an audiologist versus someone else, we have these data. We can accumulate them together and talk about why. The outcome speaks to whether or not we have been successful. Did we meet our goals and the patient’s goals? Is the patient satisfied? Those are probably the two biggest issues. If you have met someone's goals and they are satisfied, it is hard to do better than that.
Outcome Assessment
One way to look at devices through outcome assessments is by using the Psychosocial Impact of Assistive Device Scale (PIADS; Day & Jutai, 2002). This looks at how the treatment impacts a person with regard to their daily life. I do not think this is a measure used a lot in our field, but it is simple and quick. Also the Device Oriented Subjective Outcome Scale (DOSO; Cox, Alexander, & Xu, 2009) is the same kind of thing. This looks to be a little more performance based, with subscales such as listening effort, pleasantness, quietness and convenience. If I had to choose between the two, I would use the DOSO more than the PIADS. I would not use both, but I am showing these examples so you can choose which one is best for you.
I also like the Satisfaction with Amplification in Daily Life (SADL; Cox & Alexander, 1999). That is a direct outcome measure also out of Robyn Cox’s lab. The scores can be compared to normative data, which is another compelling point for patients. The COSI, the PEW and the APHAB can be used as both pre-tests and post-tests. An example of a post-treatment PEW completed by the patient is found in Figure 15. This patient said that we have met their expectations post treatment and that they are doing well.
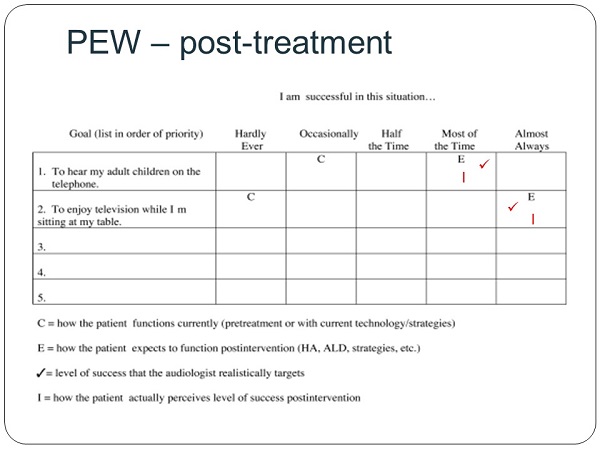
Figure 15. PEW post-treatment patient questionnaire. View larger version of image (PDF)
The International Outcome Inventory-Hearing Aids (IOI-HA; Cox & Alexander, 2002) is a seven-question form. We use this in our clinic as a quality control for the entire clinic. Everyone who obtains a hearing aid from us or our satellite clinics is given this measure. I look at this as more of a global measure of how our clinic is doing with people. It also has normative data and we plot that. Our goal is to hit or exceed the norms.
Application
I like this quote by Oliver Wendell Holmes, Sr.: “The young man knows the rules, but the old man knows the exceptions.” That is where the clinician comes in. Here are a couple of examples. We had a patient with macular degeneration. When he would look straight ahead, he only had peripheral vision, with no central vision. He liked people to be on his side when they talked to him. This would be great example of using adaptive directionality, which, in a sense, does not have evidence to say it is better than fixed in this type of situation, but for this patient, it will be far better. If the speech comes from the side, we want that directionality to move over to the side, and that is indeed what we did with this patient.
The following (Figure 16) shows where we click on those things to make that happen in the directional screen of the Siemens software. We can make the choice to default to automatic adaptive directionality.
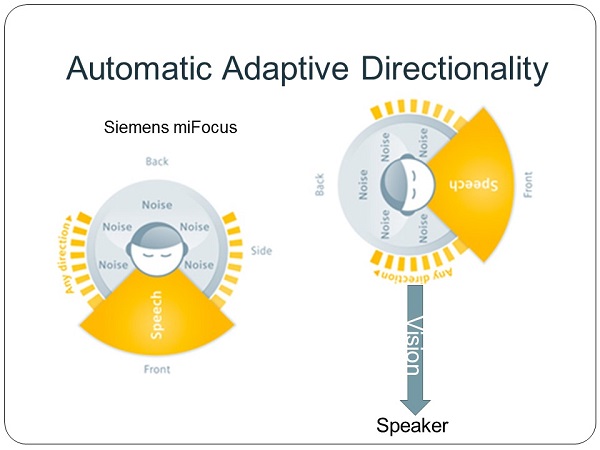
Figure 16. Siemens miFocus automatic adaptive directionality function.
The next example is a patient with limited right-arm mobility. In this case, we used binaural synchronization so she could have use of her hearing aid controls on the left side. Again, it is a technology that does not necessarily have evidence, but for this patient, it was a perfect match.
Conclusion
I would like to leave you with this thought. What we need to do is ensure audibility, comfort, and signal-to-noise ratio improvement. That is standard for every patient. It also matters how we do this specific to each patient’s lifestyle.
Questions and Answers
We are all concerned about being responsible and best meeting our patients’ needs. How, as busy professionals, do we keep up with the latest evidence?
I think systematic reviews are our best friend. If you are interacting with people who are the editors of our journals, you can tell them you want to see those things. We do not have many systematic reviews published in our journals. There are disciplines who do have entire journals dedicated to systematic reviews. I do not know if we need that, but it would be great to see a systematic review in every JAAA edition.
I think we also can empower ourselves with quick searches. I think we have never been in a better position to do that. You do not have to have a connection to University, just an Internet connection. You can ask questions and get very quick answers. You have to get out of that graduate school mentality and realize you do not need to know everything ever written about a topic; you just need the most recent kinds of things.
The other thing you can do is push the manufacturers with whom you work to publish evidence as opposed to marketing. They should publish marketing; that is what they do. But you do want to see the evidence of how their study was designed and what they found. Quite a few of the manufacturers are doing a much better job of that.
If increased channels help to achieve a good real-ear target match, doesn’t that help speech intelligibility?
I understand where you are going with this. What the research suggests, when you look at the various shapes of hearing losses we have, is that having four channels will give you as good a match as having more channels than that. You are correct in what you are saying, and the only caveat is that 4 channels lets you get as good a match as 20 channels. You are trying to match your targets, and you can generally do that with four channels. You may have that one patient where you cannot, and that is a great example of you having to look individually at each patient and recommend something that fits them more appropriately. That would be perfectly reasonable.
Does the symphony in Pittsburgh have looping?
They have not perfected the looping, but have looped at Heinz Hall. That is our symphony. It is not quite working yet. There are some interference issues, but they are working on it. We are excited that it is coming down the pike.
I would like more information on directional mics. Do you recommend any one article?
Even if you are not interested in pediatrics, I think Ryan McCreery's most recent systematic review (2012) would be a great place to start. The title is An Evidence-based Systematic Review of Directional Microphones and Digital Noise Reduction in School-age Children with Hearing Loss. He provides a nice summary of what we really know about directional mics at this point.
References
Aazh, H., Moore, B. C., & Prasher, D. (2012). The accuracy of matching target insertion gains with open-fit hearing aids. American Journal of Audiology, 21(2), 175-180. doi: 10.1044/1059-0889(2012/11-0008)
Abrams, H. B., Chisolm, T. H., McManus, M., & McArdle, R. (2012). Initial-fit approach versus verified prescription: Comparing self-perceived hearing aid benefit. Journal of the American Academy of Audiology, 23(10), 768-778. doi: 10.3766/jaaa.23.10.3
Alexander, J. M. (2013). Individual variability in recognition of frequency-lowered speech. Seminars in Hearing, 34(2), 86-109.
Boymasn, M., & Dreschler, W. A. (2012). Audiologist-driven versus patient-driven fine tuning of hearing instruments. Trends in Amplification, 16(1), 49-58. doi: 10.1177/1084713811424884
Brons, I., Houben, R., & Dreschler, W. A. (2013). Perceptual effects of noise reduction with respect to personal preference, speech intelligibility, and listening effort. Ear and Hearing, 34(1), 29-41. doi: 10.1097/AUD.0b013e31825f299f
Ching, T. Y., Day, J., Zhang, V., Dillon, H., VanBuynder, P., Seeto, M., et al. (2013). A randomized controlled trial of nonlinear frequency compression versus conventional processing in hearing aids: speech and language of children at three years of age. International Journal of Audiology, 52(Suppl 2), S46-S54. doi: 10.3109/14992027.2013.858281.
Cox, R. M. (2005). Evidence-based practice in provision of amplification. Journal of the American Academy of Audiology, 16(7), 419-438.
Cox, R.M., & Alexander, G.C. (2002). The International Outcome Inventory for Hearing Aids (IOI-HA): Psychometric properties of the English version. International Journal of Audiology 41(1), 30-35.
Cox, R. M. & Alexander, G. C. (1999). Measuring satisfaction with amplification in daily life: The SADL Scale. Ear and Hearing, 20(4), 306-320.
Cox, R. M., & Alexander, G. C. (1995). The Abbreviated Profile of Hearing Aid Benefit. Ear and Hearing, 16, 176–86.
Cox, R. M., Alexander, G. C. & Xu, J. (March, 2009). Development of the Device Oriented Subjective Outcome Scale (DOSO). Refereed poster presented at the Annual Meeting of the American Auditory Society, Scottsdale, AZ.
Day, H., & Jutai, J. (2002). Psychosocial Impact of Assistive Device Scale (PIADS). Technology & Disability, 14(3),107-111.
Dillon, H., James, A., & Ginis, J. (1997). Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. Journal of the American Academy of Audiology, 8(1), 27-43.
Fitzpatrick, E. M., Seguin, C., Schramm, D. R., Armstrong, S., & Chenier, J. (2009). The benefits of remote microphone technology for adults with cochlear implants. Ear and Hearing, 30(5), 590-599. doi: 10.1097/AUD.0b013e3181acfb70
Hawkins, D. B. (1984). Comparisons of speech recognition in noise by mildly-to-moderately hearing-impaired children using hearing aids and FM systems. Journal of Speech and Hearing Disorders, 49, 409-418.
Leavitt, R. J., & Flexer, C. (2012, December 1). The importance of audibility in successful amplification of hearing loss. Retrieved from www.Hearing Review.com
Liu, H., Zhang, H., Bentler, R. A., Han, D., & Zhang, L. (2012). Evaluation of a transient noise reduction strategy for hearing aids. Journal of the American Academy of Audiology, 23(8), 605-615. doi: 10.3766/jaaa.23.8.4
Magnusson, L., Claesson, A., Persson, M., & Tengstrand, T. (2013). Speech recognition in noise using bilateral open-fit hearing aids: the limited benefit of directional microphones and noise reduction. International Journal of Audiology, 52(1), 29-36. doi: 10.3109/14992027.2012.707335
McCreery, R. W., Brennan, M. A., Hoover, B., Kopun, J., & Stelmachowicz, P. G. (2013). Maximizing audibility and speech recognition with nonlinear frequency compression by estimating audible bandwidth. Ear and Hearing, 34(2), e24-e27. doi: 10.1097/AUD.0b013e31826d0beb.
McCreery, R. W., Venediktov, R. A., Coleman, J. J., & Leech, H. M. (2012). An evidence-based systematic review of directional microphones and digital noise reduction in school-age children with hearing loss. American Journal of Audiology, 21(2), 295-312.
Mueller, H.G., Weber, J., & Bellanova, M. (2011). Clinical evaluation of a new hearing aid anti-cardioid directivity pattern. International Journal of Audiology, 50(4), 249-54.
Ricketts, T.A., Hornsby, B.W.Y., & Johnson, E.E. (2005). Adaptive directional benefit in the near field: Competing sound angle and level effects. Seminars in Hearing, 26 (02), 59-69.
Schum, D. J. (2001). Adaptation management for amplification. Seminars in Hearing, 22(2), 173-182.
Thibodeau, L. (2014). Comparison of speech recognition with adaptive digital and FM remote microphone hearing assistance technology by listeners who use hearing aids. American Journal of Audiology, 23(2), 201-210.
Wu, Y. H., Stangl, E., Bentler, R. A., & Stanziola, R. W. (2013). The effect of hearing aid technologies on listening in an automobile. Journal of the American Academy of Audiology, 24(6), 474-485. doi: 10.3766/jaaa.24.6.4.
Cite this Content as:
Palmer, C. (2015, May). Siemens Expert Series: matching technology & features to patient needs. AudiologyOnline, Article 14063. Retrieved from https://www.audiologyonline.com.