Learning Objectives
After this course, participants will be able to:
Describe the steps involved with insurance enrollment.
Describe the important questions to consider in a managed care agreement.
Describe the role of CAQH in the credentialing process.

Dr. Kim Cavitt: My philosophy when discussing how to deal with insurance: "A pessimist complains about the wind; the optimist expects it to change; but the realist adjusts the sails". Regarding insurance, we need to be a realist. We need to read and look over things thoroughly. I may repeat one phrase over and over again about having an excellent understanding of your contracts, because again, we need to be a realist. Think about the insurance environment which we are working in. If any of the terms that I am speaking of are foreign or uncommon, please view the course in the Billing and Coding Bootcamp series entitled, Managed Care Terms. That course covers different nomenclature that I am using today.
Coverage vs. Reimbursement
There is a difference between coverage and reimbursement. Coverage is when a third-party is paying in whole or in part for the cost of the item or service. Reimbursement is when you, the provider, receive payment for the cost of the item or service. Reimbursement can come from a third-party payer or from the patient. Lack of coverage does not mean lack of reimbursement, and lack of coverage does not mean you do not render the services. We should be conducting evaluations for our patients that are evidence-based, medically reasonable and necessary. Lack of coverage for those items or services does not mean that you should omit the service if the other two criteria are met. When it is evidence-based and medically necessary for the patient, that means it is benefiting them. We need to care more about reimbursement and less about coverage, again, because the lack of coverage does not mean the lack of reimbursement.
Audiologists need to let go of the age old adage of "free". We need to follow the guise of our colleagues in Physical Therapy, Occupational Therapy, Dentistry, Optometry, Chiropractic and Medicine. These professions are comfortable charging patients privately for performing items or services that are evidence-based and medically reasonable and necessary. Let us think about insurance contracting in terms of reimbursement and a little less about coverage.
Third-party Reimbursement
Other than Medicare, you are a voluntary participant in managed care. Participation in managed care is a business decision. You do not have to be enrolled in plans. Each clinic must make the decision to be an in-network or out-of-network provider. Some patients do have out-of-network benefits that they can access. The ones that tend to not have out-of-network benefits are those patients in an accountable care organization or patients in a Health Maintenance Organization (HMO). Again, the determination to be in-network or not is the first decision. Providers must be credentialed with a payer before they can bill a payer as a participating in-network provider. If you are not, the insurers contract with facilities and providers. If you are not contracted, you are an out-of-network provider, and the patient would pay in full for the items or service they received on the date the item or service is provided.
The patient should be informed of your network status as it pertains to insurance prior to making an appointment and be informed of their resulting financial responsibilities. You do not want to just assume when the patient schedules that they are in or out-of-network and just hope for the best when they arrive. Patients would prefer clinics being upfront with them at the time the appointment is scheduled.
Medicare
Audiologists can not opt-out of Medicare. We can not enter in to private contracts with Medicare beneficiaries for items or services that would have been covered by Medicare. One can not charge a Medicare beneficiary for something that Medicare would have covered. Medicare beneficiaries have the right to access their benefits, again, for Medicare covered services. Before you can start seeing a Medicare beneficiary, you need to be enrolled as an individual with the electronic version of the 855-I and your practice also needs to be enrolled with the electronic version of the 855-B. If you plan to receive reimbursement for diagnostic testing, you will also have to sign a form, the electronic version of a form called the 855-R which is the Reassignment of Benefits form. Audiologists must have an NPI, a license and a place of business before proceeding with Medicare enrollment.
You should enroll in Medicare electronically via this link, https://pecos.cms.hhs.gov/pecos/login.do. If you want to end up in a Medicare black hole, the best way to get there is by doing a Medicare enrollment that you submit by paper. If you are a paper person, print out the application and fill it out. Then, take your answers, go into the Provider Enrollment, Chain, and Ownership System (PECOS), create an account, if you do not already have one, and submit the enrollment electronically. At the end of the electronic enrollment, the contractors will ask you to send items to them, very specific items, (e.g., copy of license, liability insurance, diploma). They might also ask you to do it in a very specific manner, (e.g., a white envelope, yellow or manila envelope, priority mail or certified mail). Do it exactly the way they tell you to do it and do it in a timely manner. The PECOS site has amazing tutorials. If you scroll down to the bottom of that site, there are some fantastic tutorials to walk you through how to enroll electronically in PECOS.
Medicare Opt-out
Approved providers, generally physicians, physician assistants, and nurse practitioners, may enter into private contracts with Medicare beneficiaries for Medicare covered services. When the patient opts-out, the services are not covered by Medicare. The physician has to formally opt-out, with a formal opt-out agreement and a private contract that is written by an attorney. The private contract should be signed by the provider and the patient. When a physician has opt-out of Medicare, they can collect payment from patients. Neither the provider nor the patient can file claims to Medicare. Once the provider is officially opted out of Medicare, they are opted out for two years. A provider can not re-enroll for two years, so it is a commitment that the individual or clinic needs to take. However, Audiologists are not on the opt-out list. We are listed along with other professions such as, Occupational Therapists, Physical Therapists, and Speech-Language Pathologists that cannot opt-out of Medicare. In summary, you cannot charge a Medicare beneficiary privately for an item or service that Medicare would have covered.
If you want to be reimbursed for diagnostic testing, if you want to be able to submit claims to Medicare for denial or you want to be able to contract with a Medicare Part C plan, Medicare Part C is Medicare Advantage, you must be enrolled in traditional Medicare. Medicare will not allow you to submit a claim to them, even for denial, if you are not enrolled. Thus, Audiologists are not allowed to opt-out of Medicare enrollment. Audiologists are not able to accept orders from physicians or other ordering healthcare providers who are not enrolled in Medicare or who have not formally opt-out. If you put on your claim, as the ordering provider on a traditional Medicare claim, a physician who is not enrolled, then your claim will be denied and you can not bill the patient for that item or service. Ensure that all of your ordering physicians are properly enrolled in Medicare as a participating or non-participating provider or have formally opted out.
Medicare Enrollment Process
Medicare enrollment, if you will be participating or non-participating, is determined on your 855-R or your Reassignment of Benefits form. The options when dealing with a traditional Medicare patient are to be enrolled as a participating provider, to be enrolled as a non-participating provider, or to not be enrolled. We will talk discuss each of those individually.
A participating provider is a provider that accepts assignment. Accepting assignment is accepting the Medicare allowable as payment in full, except for co-insurance and deductibles. If you are a participating Medicare provider, you are listed in the provider directory. If you are a participating provider, the claim will roll after it is processed by traditional Medicare to any Medicare supplementary policy that exists. So it will automatically be forwarded over to that secondary payer to pay that Medicare co-insurance of 20%. Medicare pays out 5% more when they are dealing with a participating provider. They do not necessarily pay you 5% more, but they pay out 5% more, and you will see the difference in a moment.
A non-participating provider can accept assignment. Or they can accept the Medicare allowable, as payment in full on a claim by claim basis. If you have a patient who may be financially-challenged and you do not want to have them pay upfront. This might be a scenario where you accept assignment on that claim. Another option is to not accept assignment and you can charge the patient upfront the Medicare limiting charge which is 115% of the allowed amount. When you are a Medicare non-participating provider and accepting the limiting charge and not assignment charge, the patient pays you on the date of service. So they would pay you the limiting rate, which is readily available on every Medicare fee schedule that is online. Then, you would submit the claim to Medicare and the patient would be paid directly from Medicare 95% of the Medicare allowable. So the patient will not be reimbursed all of their money back, they will receive a large portion of their money back. The claims typically do not forward or roll over to the secondary payer. So typically once a non-participant claim is processed, you will then have to send that claim yourself electronically to the secondary payer.
The third option is to not be enrolled. Essentially you are functioning as an educated hearing instrument specialist since they, too, cannot enroll in Medicare. So in other words, all of your testing, all of the time, is no charge, regardless of the patient or payment source. This is due to the fact that most managed care agreements say, please do not charge for something that you are giving to your general population at no charge. If you charge one person, you need to charge all. Again, if you are not enrolled, that means that your testing is non-covered and you cannot collect payment from patients, it is free.
Medicare Enrollment Options
So first, let us talk about participating providers. When you are a participating provider with Medicare, and you bill out your usual customary amount for that item or service for example, $125. The Medicare allowed amount is $100. As a participating provider, Medicare will to pay 80% of the allowable, in this example, that is $80. The $20 left, or the 20%, would be the co-insurance. That is either paid by the patient, if they do not have a Medicare secondary or supplementary policy, or it is paid by the supplemental policy. Your total payment would be $100 as shown on Table 1.
However, as a Non-Participating provider who accepts assignment on this particular claim, your billed amount is still $125. The Medicare allowed amount for "non-par" providers in this instance is $95. 80% of that will come from the Medicare contractor and 20% will by paid by the Medicare secondary, supplemental insurance, or patient. With a total reimbursement of $95. Again, since you are Non-Par, so you only receive 95% of the Medicare allowable.
Most Non-Participating providers do not accept assignment on the claim. Thus, you bill what you are supposed to receive, the limiting charge of $115. That would be what you would collect from the patient at the time of service. Medicare would refund the patient, or reimburse the patient, $95, again, 95% of the allowable. Medicare will pay $76, or again, 80% of that $95. Their secondary or supplement will pay the additional $19. If they do not have a secondary or supplement, even though the patient paid you $115, the patient will receive $76. The patient will not be reimbursed in full as shown in Table 1.
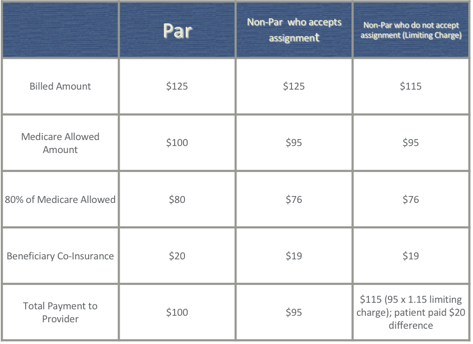
Table 1. Medicare Enrollment Options.
PTAN
When you enroll in Medicare, you will receive a Provider Transaction Access Number (PTAN). Upon application to a Medicare Administrative Contractor, you are will be issued this PTAN. While only one National Provider Identifier (NPI) can be submitted on claims, the PTAN is a critical number directly linked to a provider or a supplier's NPI. Providers will only have one NPI, but generally, will be assigned a different PTAN for each practice or contractor they are connected with or submitting claims to. PTAN is explained in more detail here: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/SE1216.pdf
Medicare Revalidation
For those who are enrolled in Medicare, either as a participating or non-participating provider, you will need to revalidate every three to five years. This is Medicare's attempt to ensure they have the most updated location and address on file. You are will receive a letter or email, depends on the contractor, that will state you have 60 days to revalidate. You want to revalidate online and need to do so within 60 days, because on day 61, they will close your Medicare account. Please, when you receive a revalidation request, complete immediately and online via the PECOS portal.
Third-party Contractors
Which third-party contractors (i.e., third-party payers), (e.g., Blue Cross Blue Shield, UnitedHealthCare, Humana, and Cigna) should my practice contract with? First, you need to perform a market analysis to analyze and make a informed decision about how you want to proceed. Questions to consider when enrolling with a contractor include:
- What are the socioeconomics of your community?
- Can they absorb your practice not being in-network?
- Are they are willing pay upfront and privately for the items and services provided?
- What insurers represent the major employers in your area?
- What insurances do your referral sources and local hospitals accept?
- Which insurers offer lucrative hearing aid benefits?
Keep in mind that some referral sources can not, by contract, refer out to out-of-network providers. They are required to refer their patients to someone who is in the insurance network, especially if they are affiliated with that insurance network, (i.e., Kaiser Permanente).
Step #1 to Contracting: Request Information from the Payer
Step one to contracting, you want to request information from the payer. Start with a Google search. Most payers have fantastic websites that contain great information about enrollment and guidance. You can find information about their payment policies, provider manuals, and administrative guidance. All of this information is readily available and open access on their website. You can also often begin the application enrollment process directly from the payer website.
Step #2: You Will Receive a Reply from the Payer
The payer may reject your application of enrollment and state their network is closed. That means that they are not accepting new providers. They can and do say no, and some of the reasons they say no is because of anti-trust rules in state and federal insurance laws. So, they can and do say no for legitimate reasons. In some instances, instead of saying no, they can send you a provider agreement and a payer fee schedule or access to a payer fee schedule.
Rejections. First, you could reach out to the Human Resources Department of the employer that is providing these benefits. Do so with data. Information to submit after a rejection might include:
- How many of their members are seeking your services?
- How underserved your community is?
- How far does a patient have to drive to see an in-network provider or to get in-network provider specific services?
- How your practice offers services or products not provided by other providers, (e.g., auditory processing, vestibular management, tinnitus evaluation, pediatrics or implants)?
For example, if you are a vestibular clinic, but there is not another in-network vestibular provider for 40 miles, I would bring that up in a request to Human Resources. You can periodically attempt to re-enroll if the participation with this payer is lucrative. Some practices are sold, some practices close, sometimes they have a boost in population, they have a boost in an employer group that they need more providers, keep trying to periodically re-enroll. You can have patients advocate for your inclusion in the plan. They can contact customer service or their human resources department. You can purchase a practice that is in-network. This is something that is really common in medicine. Again, before you make that leap, this is important, please have an attorney and an accountant assist you in ensuring that you are making the correct type of business purchase that enables you to retain their managed care agreements. Not every type of business purchase allows you to keep the managed care arrangements.
CAQH. The Council for Accessible Quality Healthcare (CAQH), it is a credentialing clearinghouse. You can use this to enroll with multiple payers, it is free to participate in, and I have provided the link for CAQH, https://www.caqh.org/. To participate, you must be a credentialed provider with at least one of the CAQH participating providers and then you must be invited by CAQH participants.
Step #3: Understanding the Provider Agreement
What many audiologists have done in the past, which is how they ended up in some of the situations they are in, is they have signed it and sent it on without fully understanding the provider agreement. I would advise strongly against that. Instead, you should read the entire agreement and review the fee schedule. Most fee schedules that providers receive initially do not have all the codes contained on them that you will bill. So you need to keep going back and access all of the codes for the various products they offer before you sign that agreement. Any questions you ask an insurer in this process you want in writing. They will not be able to deny if it is the form of an email. Focus on asking our contracting and credentialing questions in writing only.
General questions to consider when reviewing a provider agreement:
- What products does this contract obligate the practice to participate with?
- Does it have a state managed Medicaid product?
- Do they have HMOs?
- Do they have PPOs?
- Do they have an indemnity?
- What type of products? (Each product has a different allowable schedule, and some actually have different rules or amendments specific to that product, so you want to know what products they have and what signing that is obligating you to).
- What are the organization predetermination requirements if offering a managed Medicaid or Medicare Part C product?
- Does it allow for patient upgrades for hearing aids? (Give specific examples in writing).
- Does the practice, again in the upgrade, have to offer a basic or standard device first?
- Is there a waiver process for upgrades if they do allow it?
- Is there a waiver process?
- Does it recognize or process S1001, which is a deluxe item, patient notified code?
- And if they do recognize that, does that code then help reflect on the explanation of benefits to a patient who can upgrade what their out-of-pocket expense is?
- And does, again, because how does that upgrade reflect on the EOB the patient receives?
Organization predetermination is the Medicare Advantage term for an advanced beneficiary notice. So you want to know how detailed their advanced beneficiary notice process is, how it works in this enrollment process. Again, a good time to remind folks, there is one code for a set of binaural digital behind-the-ear hearing aids, whether those hearing aids invoice cost is $200 or $3,000. Insurers are responsible to what is medically reasonable and necessary and not what is for the comfort of the patient. So, to be able to live stream, or stream from a hearing aid to their phone, is not necessarily medically necessary. If it is not in your contract that they can upgrade, or pay the difference, that would be deemed balanced billing and that is often times not allowed by contract.
Specific Audiology Related Questions to Consider
Does the payer allow for hearing aid rentals? Can a patient rent a hearing aid rather than purchase a hearing aid? Does it require any specific modifier use? How many line items are allowed on a hearing aid claim? There are some Blue Cross Blue Shield plans, especially in Texas, that Blue Cross Blue Shield will only cover two line items and will deny everything else and will not allow that to be moved to patient responsibility. So again, are there line item restrictions on a hearing aid claim?
Does the provider agreement require patients complete notices of non-coverage before non-covered services are provided? That answer is typically yes, they typically need to be in writing, but again, you want to know that in the contract.
Is the hearing aid benefit inclusive of all the items or services associated with the dispensing piece fittings, batteries, and repair services? There are some inclusive benefits, for example, the federal benefit is inclusive of all the items or services related to dispensing and fitting. You want to know if the hearing aid benefits they offer are inclusive. UnitedHealthcare benefits are also inclusive, but you can see UnitedHealthcare benefits online once you are enrolled if you are enrolled in their online portal.
Can student externs or technicians see members of this plan for covered services? That answer is not always yes. I have had that answer be no, because they are unlicensed. So again, are they allowed to see members of this plan, and if yes, are there any supervision requirements? (e.g., general, direct, or personal supervision). Just like Medicare requires personal supervision for coverage, some payers can require that as well.
Can hearing aid dispensers see members of this plan for covered services? If you employ a hearing aid dispenser, you should not assume. I would like to highlight that services should not be billed out under the audiologist's NPI unless services were rendered by them personally or you are allowed to do so by the payer.
Can audiology assistants see members of this plan? Again, if you ask are there supervision requirements, that answer is also many times no because they are unlicensed. But again, that's a payer by payer determination.
Is hearing aid coverage contingent on receipt of a medical clearance? This is a new thing we are seeing being brought back into insurance. Does that medical clearance have to be from an otolaryngologist (i.e., ENT)? Does the patient have to be physically seen by the otolaryngologist? And what evidence needs to be provided of that ENT visit if that is a requirement?
Can certain services be carved out of the contract? For example, if you offer hearing aids in your practice, but your contract with payer X does not include hearing aids in the contract. Carve-outs used to be very common 20 years ago but they are very rare now. So, it is not unheard of but, it never hurts to ask, if they be carved out?
What are the termination or renegotiation terms of the agreement? Those are very clearly defined in managed care agreements. For hearing aids, is a practice required to supply a manufacturer's invoice? And again, does that invoice have to have a dollar amount on it? Now you have packing slips and you have an invoice with dollars, can you just send them the packing slip? That would be a question that I would ask.
What are the renewal terms? Does this contract evergreen or automatically renew every year?
Does the payer cover telehealth services required by an audiologist? Are there only specific services the payer covers via telehealth?
Does the payer require a modifier if you are doing telehealth? And are there any other specific telehealth requirements? Again, you do not jump into telehealth, and that includes the remote programming of a hearing aid or cochlear implant, without meeting HIPAA requirements, liability requirements, licensure requirements, and most importantly, how does the payer manage it? Do not try to pass to a payer that you saw this patient face-to-face when you didn't, that would be a false claim.
How is medical necessity defined? What does this payer deem as medically reasonable and necessary, because medical necessity is required for coverage.
What are the requirements for standard processes and procedures? What that means is there is typically language in a contract that will say what the anti-discrimination is, and it goes beyond race and religion and gender. It is about price at times, that you can not charge my patient differently than you charge your general population. For example, you want to know if there's language about anti-discrimination or standard processes and procedures.
What are the means of provider notification of substantive changes to the agreement? This is really important because agreements change and there are guidance in every contract about what that process is when they make substantive changes to the agreement, which they will do, sometimes monthly. So how are you notified of that? You need to know that so that you look at that because if you do not respond to how the contract tells you to when a substantive change comes to be, they assume that that is acceptance of that change, so you need to know how you are notified of that.
What are requirements for a standard fee schedule or charge master? Some contracts will be very clear that you have to have a standard fee schedule that is used for all of your patients. Can the practice bill differently to the payer than they bill their general population? Are there timely claims filing requirements? How many days do you have to complete a clean or perfect claim? How long do they have? Because on the next day, they do not have to pay you if you are outside the timely claims filing requirements.
Are there any other claims filing requirements? For example, will you accept paper claims? How do you want additional documentation sent to you?
Are there clinic hour requirements? I do not know how many of my clients have signed a contract that says that they are available seven days a week, 24 hours a day.
What are the medical record retention requirements? Medical record retention is first set forth by HIPAA, which is six years, but then there is state medical record retention laws. But a payer can make medical record retention laws for their members that exceed state or federal guidelines, so you want to know what those are.
Does the payer allow for, or cover, evaluation of management service provided by an audiologist? If not, does it allow for the financial responsibility to be assigned to the patient? You want to know that in advance and in one tentative evaluation management coding.
Does your state allow you to evaluate a manage in your licensure? Because technically, what the codes say is that you can not use them unless allowed by scope of practice, and your scope of practice as an audiologist is defined by your state.
Do they require hearing aid patients to be referred to a third-party administrator to access their hearing aid benefit? If you are signing an agreement thinking that you will get hearing aids from it but all the hearing aids, like a Cigna contract, all the hearing aids are funded through a third-party administrator.
Does the fee schedule address all the items or services you provide? You want to make sure that you know the allowable for every HCPCS and CPT code for the items or services that you provide or might want to provide in the future. And you especially want to know how the unlisted codes of 92700, L9900, V5298 and V5299 are processed. If you want to know about the codes, there is a module specific on the specifics of the codes.
Step #4: Understanding the Fee Schedule/Chargemaster
You also want to know, again, about the fee schedule. This is what the payer allows, per contract, for each specific item or service you provide for each specific product you are contracted to provide. You never want to accept less than you can afford to receive unless you have a significant volume or it is leading to something significant or manageable. You need to know what your breakeven plus profit amount per hour is to properly analyze a third-party fee schedule, and again, in our pricing module, we will talk about how to come up with your breakeven plus profit. And do the participation of benefits outweigh the costs? And I am a big fan, when you are looking at a contract, that you look at them each individually and that you do a SWOT analysis, what is the cost versus benefits?
You want to be careful, when we are talking about a fee schedule and when we are talking about a contract, of inclusive hearing aid benefit coverage amounts. How much is included? How long you would have to manage this patient for this allowable rate? You want to know about restrictions on the number of line items allowed. Large hearing aid discounts, so if you submit, oh, we pay by billed amount. Okay, great. So your billed amount has to be your usual and customary, if they have language that you can not bill them differently, and they are then will take 40% off of that. You know, you have to be aware of those large discounts or percentages off of dollars billed. And fitting fee only or invoice plus arrangements where you are getting a dispensing or fitting fee only. They are buying the hearing aid, they are not allowing you to, again, reap more benefits for that fitting. In that fitting fee only arrangement, sometimes you do not buy the aid or that means that they are requiring you, like Blue Cross Blue Shield of Georgia, for example, they are requiring you to submit an invoice. Again, sometimes it is a better business decision to be out-of-network as patients pay you in full on the date of service and can often still access some of their benefits.
Third-party Administrators
Third-party administrators (TPA), is a contracting and management entity that either exists between the provider and an employer or between the provider and an insurer. They are a middleman and they are there for these reasons.
First, They allow payers a single point of contact and payment for hearing aid related items or services. So let us say that Blue Cross Blue Shield, for example, has a funded benefit through a third-party administrator. Blue Cross Blue Shield will receive one bill from the TPA and the TPA will already have determined that these items or services are reasonably necessary and that they were provided to the patient in question. They have verified everything. So this is easier for that payer to have one point of contact. Second, it defines risks for the payer because they have contracted with that third-party administrator a singular allowable that applies everywhere, they know exactly what their risk is. Third, it is cost containment for the member and this is especially when we are talking about a discount plan or a plan that allows upgrades. We, as Audiologists and hearing aid dispensers, can be are own worst enemy and it is because we did not contain costs. That is one of the big reasons why third-party administrators have now come to be. It establishes a standard of care for the member. A third-party administrator can require a standard of care that is part of the fitting and that is part of that dispensing fee. Thus, they know that every patient will receive the same treatment. For example, TruHearing allows for three visits. Every patient will receive three follow-up visits as part of their agreement which is included in the dispensing fee. Audiologists help create the need for these programs and help maintain their existence through their continued participation with a third-party administrator.
When you are considering third-party administrator participation, before you sign, although these contracts have a much easier out-clause, you want to consider these points. Just like enrollment, ask questions about the third-party administrator contract in writing only, do not just talk on the phone. Third-party administrators tend to have excellent provider manuals and administrative guidance. They provide much of their information in writing, so please read everything before you sign. Go back to the managed care agreements, read the contract, provider manual, administrative guidance, and bulletins.
Important Questions to Consider Before Agreeing to Participate in TPA
Can I afford to provide the level of care at the agreed upon rates required by the plan? If a plan has a dispensing fee of $350 and you have to manage that patient for one year for $350 dispensing fee per ear, and provide your standard of care, can you afford to do that? That's a question that only you can answer for yourself.
Is the plan offering a funded or unfunded? A funded plan is one where the third-party is paying in whole or in part towards the cost of the item or service. An unfunded or discount plan is where the employer or insurer negotiated a discount but they are not paying anything towards the cost of the item or service. TPAs are generally unbundled, especially after that first year, if you are unbundled and it is merely a discount plan in your area, you may be able to offer a competitive price offering to match. Create a product line for people who want that level of technology that you can match that program.
What is your responsibility in informing the patient of their benefits either funded or non-funded? So typically, third-party administrators rule of thumb is that you are responsible to have a patient access their TPA benefits if the third-party administrator referred the patient to you. If this is a patient that self-generated from your office, you do not have the obligation. Generally, this could vary plan by plan, but the legal obligation by contract is to refer that patient to that third-party administrator. In most cases, you have no contractual obligation to notify someone of their TPA benefit unless the plan refers the patient to your office. What are the ethical considerations of that?
Do any of their policies conflict with your other managed care agreements? For example, free hearing tests. If the third-party administrator wants you to provide the hearing test as part of the dispensing fee, before you agree to that, please have your counsel review that agreement on a mirror as it pertains to your other managed care commitments. Nationally, we have had attorneys look at this and we cannot have one attorney make a national decision on this because so much of it is influenced by state and federal laws. More importantly, it is influenced by your own managed care commitments. Before you sign an agreement where they want you to give away the audiogram, please have your council review this agreement to make sure it is not violating any other agreement that you are in.
What products does the plan offer? Is every manufacturer or every product available? Many of them do not address Lyric. Some have very restricted products. What if the member wants a product that's not in the program? How do they handle or address that? And how many patients do you stand to potentially lose if you do not enroll in the program?
Can I charge a patient or their healthcare insurer for the hearing test? There are many plans where the hearing test has nothing to do with the discount plan. Certain plans, (e.g., Amplifon, TruHearing, and Epic), where the audiogram is not included in that dispensing fee. Read the agreement and have counsel look into it. Can I charge separately or bill their insurance separately for the audiogram?
What items or services are included in the fitting fee? Because not everything is included in the fitting fee, it depends on the third-party administrator. If it is not included in the fitting fee, are there limits to what I can charge? If there was a limit as what you could charge and the patient had the right to opt-out. You would need to notify the patient in advance of performing it, tell them how much it would be, and they could opt-out of it (e.g., real-ear measurement). Give patients notice upfront and in writing for any addition charges not included in the fitting fee.
Do I receive a greater fitting fee if I am a member of a specific buying group or membership organization? There are scenarios where if that buying group also has, under the same ownership umbrella, a third-party administrator that you are part of, not only can get a higher dispensing fee but you can receive more access to the referrals.
How long is the trial period? What do I receive if the patient returns the aids for credit? In some cases, the answer is nothing, but if they return the aids for credit, you actually receive nothing for your time. How long do I have to manage the patient for that fitting fee? And are there limits as to what I can charge outside of the fitting fee window? Enroll in all of the payer's online portals. Some have very detailed benefits information, most have all real-time deductibles and many have access to allowable rates. Ask questions in writing when you lack answers and do not sign things until you get the answers you need to make the informed decision for yourself. Do not be afraid to negotiate because the worse they can do is say no. If you are going to negotiate, you need to have your line in the sand of when you are will say no.
What are the pros and cons of contracting with each payer? It is not always the payer's responsibility to have a copy of your contract. If you can not locate it, request in writing a copy of their current agreement. Also request in writing a copy of the current fee schedules or access to their current allowable fee schedule in a web portal.
Renegotiation
Again, you are will have more leverage for your services. The more services you bring to the payer and the more locations you offer, know what you want and defend why you deserve it. Have a knowledge of your current agreement and your Medicare fee schedule in your area. Follow the guidance in the contract on termination, but instead of sending a termination letter, send a request for renegotiation. You must be willing to walk away in any negotiation or you have no power or leverage over this payer, just like any other negotiation. Follow all the same contract evaluation process you would follow if you were signing up for the very first time.
Non-participation
Again, other than Medicare, you are a voluntary participant in managed care. It is an option to not participate in third-party managed care plans and be an out-of-network provider. But again, please know, because some networks close, that once you terminate, you may not be able to get back into a plan if you change your mind later on.
Before terminating, consider:
- How many patients are represented by this payer?
- How many dollars are represented by this payer?
- How many referral sources are represented by these patients who are represented by this payer?
- Does this payer contracturally allow for hearing aid upgrades?
- Does the payer offer lucrative, audiology direct, hearing aid coverage and benefits?
- Does the payer utilize a TPA for the third-party hearing aid coverage and benefits?
- What are the socioeconomics of your area?
Do your homework before you terminate because you may not be able to get back in. When out-of-network, the patient pays in full on the date of service with the exception of one exception with someone who is Medicaid dually eligible. In many of these situations, the patient does not, Medicare/Medicaid, you do not collect the co-insurance or deductible if you are non-participating with the Medicaid plan. Another exception may be seen with Medicare Part C patients. Many of these plans do not let you collect anymore than the Medicare limiting charge for the Medicare allowed services. The explanation of benefits will guide you in these situations. Your office can submit claims to a payer as a courtesy to a patient as a non-participating provider. The patient will be reimbursed from the payer their out-of-network benefits if they exist. You often see this in mental health, dental and optometry offices, that you are out-of-network. They will submit the claim for you, the you will receive a check back in the mail.
Separate Business Entity
The final option, which I have to stress, requires the assistance of an attorney and an accountant. Certain clinics choose to create two separate legal business entities. This option is often selected when the practice has a large physician referral base or a large diagnostic practice, and they do not want to be out-of-network for diagnostics. This is an option that many physician or ENT practices choose to make their hearing aid or auditory rehabilitative practice off into a separate business entity with a separate legal structure. It cannot be a DBA, it has to be a separate legal structure and a separate tax identification and facility NPI. As a result, the second entity would not be encumbered by the managed care obligations of the original business. This new second business could be strategically enrolled in various managed cared enterprises, if they could get into the network. While avoiding poor coverage and benefits for treatment, including hearing aids. No one can guarantee that if you spin off, that the new entity can strategically enroll in anything because the network could be closed. This is becoming more common in Audiology practices as well. You must have an attorney and an accountant evaluate this option for your situation effectively and legally. They will assist you in creating the new business entity for your location, state, federal regulations.
Citation
Cavitt, K. (2018, February). The rules of the game: contracting, credentialing and negotiating with managed care in audiology. AudiologyOnline, Article 22392. Retrieved from https://www.audiologyonline.com

