Back in QuickTakes Volume 6 (Part 1 and Part 2), we provided a toolbox that was filled with various clinical tests that could be conducted during various stages of the fitting process. We started with pre-fitting testing and continued the journey through selection, fitting, verification, and validation methods. We’re pleased that the contents of our toolbox were appreciated, as this Volume quickly became the most read of our QuickTakes series.
The toolbox really wasn’t filled, however, so for Volume 8, we are back with Hearing Aid Fitting Toolbox v2. This will be a little different, as in many cases, we’ll be reviewing articles that deal with counseling, concepts and construct, and maybe not directly with a specific test that you will administer. If you’re the type who doesn’t like all the numbers that we typically toss out in our QuickTakes series, you’ll be pleased to see that there aren’t too many in this Volume—very little math is required!
8.1: Hearing Loss Prevalence and Hearing Aid Adoption
Periodically, the National Health and Nutrition Examination Survey (NHANES) compiles data on audiometric hearing loss, self-reported trouble hearing, and the use of hearing aids. Recently, audiologist Larry Humes (Humes, 2023) reported on the findings for the three most recent surveys (2011-12, 2015-16, and 2017-20). The data (n=8,795 with complete audiograms) were for adults ranging in age from 20 to 80-plus years. The prevalence of hearing loss, measured audiometrically and self-reported, is provided for males and females by age decade.
Self-reported Hearing Problems
Hearing-related questions on the survey concerned “the frequency of difficulty following conversation in noise” and “how frequently hearing caused frustration when talking.” Each of these questions included responses on a 5-point scale: always, usually, at least half the time, seldom, and never. An analysis of the responses to these questions, combined with the answer to the question “Would you say that your hearing is excellent, good, that you have a little trouble, moderate trouble, a lot of trouble, or are deaf?” resulted in forming the subgroup of those respondents who have trouble hearing. A summary is shown in Figure 1.
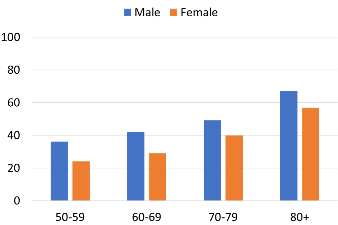
Figure 1. Percent of male and female respondents reporting “trouble hearing.” Data only shown for four oldest groups (adapted from Humes, 2023).
As expected from previous research, the self-report of hearing trouble increases systematically with age. The hearing problem is slightly more common for males than for females for all age groups. Overall, ~26% of males and ~20% of females, aged 20 to 80+ years, had self-reported trouble hearing.
Audiometric Hearing Loss
The definition of audiometric “impaired hearing” was a PTA (500, 1000, 2000 and 4000 Hz) in the better ear =/> 20 dB. The male and female findings for the four oldest groups are shown in Figure 2.
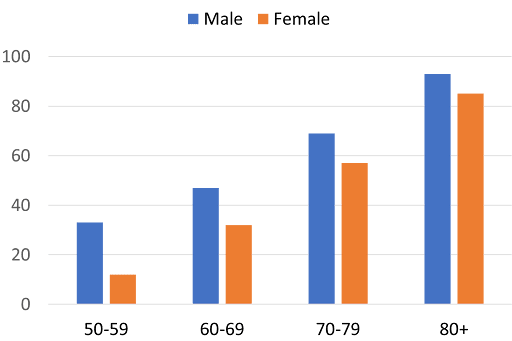
Figure 2. Percent of male and female respondents that had audiometric hearing loss (PTA =/> 20 dB for 500, 1000, 2000 and 4000 Hz). Data only shown for four oldest groups (adapted from Humes, 2023).
When compared to the data shown in Figure 1, in Figure 2, we see a similar male vs. female pattern, with more hearing loss for males. Also note, that for all age groups, the percent of audiometric hearing loss is greater than the percent of those reported hearing problems (See Figure 1). Overall, about 23% of adult males and 17% of adult females between the ages of 20 and 80+ years had impaired hearing.
Humes (2023) reports that there are large increases in the odds of PTA4 ≥ 20 dB HL with increasing age decade—those aged 70 to over 80 years had about 10 times higher odds of having self-reported trouble hearing relative to the 20-29 year-old group. The odds of audiometric hearing loss in these oldest age decades were at least 100 times higher than for the youngest age decade (although the effects of age and sex were smaller for self-reported trouble hearing compared to audiometric hearing loss). As expected, positive histories of noise exposure increased the odds of having trouble hearing by 50–75%. A positive history of hypertension, a positive history of diabetes, and lower education level all increased the odds of having self-reported hearing trouble by about 20–40%.
Unmet Hearing Care Needs
By comparing those who reported hearing trouble, and those who audiometrically had a hearing loss, to those reporting hearing aid use, Humes (2023) identified what he termed “unmet hearing care needs.” These findings are shown in Figure 3 for three hearing loss levels.
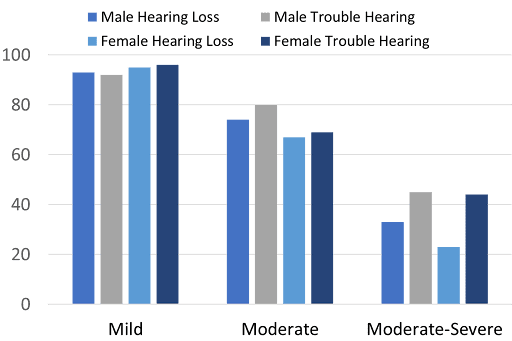
Figure 3. Percent of “unmet hearing care needs” determined by those who are using hearing aids and the overall report of hearing trouble or the presence of an audiometric PTA =/> 20 dB. Results shown for both males and females for three different severity groups (adapted from Humes, 2023).
As expected, as both the measured hearing loss and the reported hearing problems became greater, the unmet hearing care needs are reduced, but are still 60-80 percent for the moderate category. In general, the results are similar for those with measured hearing loss vs. those with reported hearing trouble, except for the moderate-severe category, where those with measured hearing loss tend to be more likely to use hearing aids (i.e., fewer unmet needs).
Humes used these data for project the estimated numbers of adults with unmet hearing care needs based on a total population estimate of 234.2 million adults in the U.S. in the age range 20 to 80+ years. This was based on the audiogram, or the trouble hearing data for the respondents reporting never using hearing aids. The lowest number of adults with unmet needs was found for the audiometric definition of needs: about 21 million males and 17 million females. For unmet hearing care needs based on the respondents report of trouble hearing, it’s projected that in the U.S. there are about 23 million males and 19 million females.
The bottom line, based on Humes (2023) analysis of the NHANES data, is that there remains an incredible amount of unmet need: a high percentage of individuals, especially those with mild and moderate hearing loss might benefit from intervention from a hearing care professional. Although this finding is unsurprising (many other studies over the past several decades yield similar results), it reminds us there is a large pool of individuals who can use our help. Lastly, given the immense unmet need of those with mild and moderate hearing loss, as illustrated in Figure 3, new devices like hearing aids sold over-the-counter, and new service delivery models using teleaudiology might be effective ways to move the needle.
Time Course: Candidacy to Hearing Aid Adoption
We’ve just reviewed data discussing the number of individuals who are candidates for hearing aids but are not using them. An important concern related to this, is the delay from the time that a person is identified as a candidate to the time that they adopt hearing aids. Various numbers have been tossed out over the years, but one of the most comprehensive studies on this topic was published by Simpson et al. (2019). These authors defined hearing aids candidacy as an SRT ≥30 dB HL in at least one ear, or thresholds at 3000 and 4000 Hz ≥40 dB HL in either ear. This resulted in a total sample of 732, with two comparison groups of hearing aid candidates: those who never adopted hearing aids (n = 514) and those who adopted hearing aids while they were in the study (n = 218). Individuals who adopted hearing aids during the study were classified as “successful” or “unsuccessful” users, based on self-report.
Demographic information was collected for: age, chronic health, race, retired, education, socioeconomic status, and marital status. In addition to the pure-tone audiometry and SRT conducted to determine candidacy, participants received monosyllabic word testing in quiet (NU-6), speech-in-noise testing (SPIN) and also completed the HHIE/A.
The unadjusted estimation of time from hearing aid candidacy to adoption for the full participant cohort (N = 732) was 8.9 years. In stratified analysis of time to hearing aid adoption the following was observed:
- A trend toward earlier adoption as age categories increased, with individuals aged 65 or younger averaging 9.2 years to adoption and those older than 76 years averaging 6.6 years to adoption.
- Females averaged 8.7 years to adoption compared with 9.0 years for males.
- Individuals in the low socioeconomic status (SES) category averaged 10.7 years to adoption compared with 8.7 years in the middle and 8.3 years in the high SES categories.
- Statistical significance for race was observed. Non-white participants took an average of 15.2 years to adopt hearing aids compared with 8.6 years for white participants.
Regarding the audiologic measures:
- As low-frequency PTA increased from ≤10 dB HL to >30 dB HL, the average time to hearing aid adoption decreased from 11.2 to 4.3 years.
- For the high-frequency PTA, when the average was ≤45 dB HL, the estimated time to hearing aid adoption was 11.5 years, however, for those with PTAs >65 dB HL, estimated time to adoption was 5.9 years.
- For the HHIE/A, relatively small differences in scores had a surprisingly significant effect on adoption time; the 25-item version was used, and scores therefore could vary between 0 (best) and 100 (worse). When scores were =/< 10, estimated adoption time was 11.1 years. When HHIE/A scores were >16, adoption time dropped to 4.3 years.
- Speech-in-noise testing revealed what might be predicted, that those participants with poorer word recognition had less time in adopting hearing aid use. Adoption time went from 12.2 years for those with scores over 70%, down to 5.8 years for those with score =/<42% (See Figure 4).
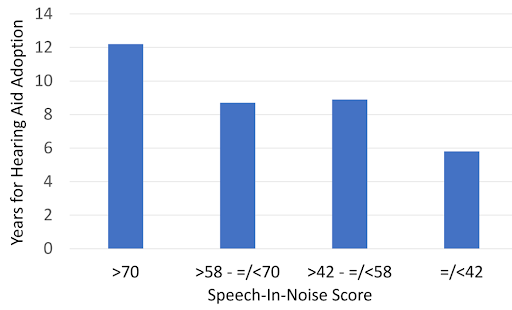
Figure 4. Shown is the relationship between the time for adoption of hearing aid use and the participants’ speech-in-noise score. The scores shown are for the keyword recognition for the low-context sentences of the Speech In Noise Test (SPIN). The SPIN sentences were presented at 50 dB SL relative to the participant’s calculated babble threshold, with babble presented at a +8 dB signal-to-noise ratio. (Adapted from Simpson et al., 2019).
Most of the data from this work by Simpson et al. (2019) agrees with previous studies of this type; their overall finding of 8.9 years is consistent with thoughts from past decades. While we of course would like the adoption rate to be 0 years, their findings do point out nicely what factors to consider with new patients who are “on-the-fence.” In particular, the predictability gleaned from the speech-in-noise testing and the HHIE/A cannot be ignored. Could it be that simply the act of taking these tests, doing poorly, and then counseled about the results, speed up the adoption process? We think it is quite possible.
MarkeTrak Data: Factors Impacting Hearing Aid Adoption
As we’ve just discussed, there are many factors that impact the adoption of hearing aids, and often, this topic is part of the MarkeTrak surveys. Such was the case for MarkeTrak10, and a summary of some of these data were provided in an article by Jorgensen and Novak (2020). For much of the findings, the group was divided between hearing aid owners and non-owners. As expected, the non-owners did not report as much hearing loss as the owners, but the difference was not as great as one might think (See Figure 5). Indeed, considerably fewer of the owners stated that their hearing loss was “mild,” but for those reporting moderate hearing loss, there was little difference between owners vs. non-owners (i.e., 54% vs. 49%)—if we include the severe and profound categories, 63% of the non-owners state that their hearing loss is moderate or greater.
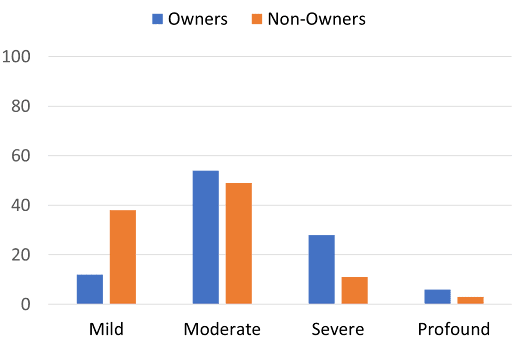
Figure 5. Percent of owners vs. non-owners who report hearing loss for four different hearing loss categories (adapted from Jorgensen & Novak, 2020).
By comparing owners to non-owners, it was estimated that 42% of those over the age of 65 with self-reported hearing problems own hearing aids. This adoption rate drops to 23% for the 35-64 years group, and 30% for the younger than 35 group. Yes, you read that correctly, the younger group had a higher adoption rate than the middle-aged respondents, a finding that also was present in MarkeTrak2022, and something that we have discussed in a previous QuickTakes article (Volume 7; Taylor & Mueller, 2024). Data from the MarkeTrak10 survey projected that in the U.S., there are approximately 11 million nonadopters with moderate-to-severe hearing loss. This value is only about ½ of the projection we referred to earlier from Humes (2023) but recall that he included those with mild and moderate losses.
The MarkeTrak10 findings suggested that the time course for obtaining hearing aids is somewhat faster than found by Simpson et al. (2019). Recall that Simpson et al. (2019) reported 9.2 years for individuals aged 65 or younger, and 6.6 years for those older than 76. The MarkeTrak10 survey (median age of hearing aid owners was 71 years) found that from the time that the individual first noticed a hearing problem to the time that they were tested was 4.2 years, and that the first set of hearing aids was purchased at 6.2 years. In other words, after seeing an HCP (testing), on average, hearing aids were purchased within 2 years. These data of course are based on the person’s memory (unlike the Simpson et al. data), and it’s also possible that the respondent didn’t want to admit how long they really waited to obtain amplification.
Some MakeTrak10 findings which impacted adoption (Jorgensen & Novak, 2020):
- Men are more likely to have self-perceived hearing loss—12.8 of total sample vs. 8.9% for women. The rate of hearing aid adoption was 34% for both groups.
- For many general questions regarding hearing difficulty, the responses from owners vs. non-owners was quite similar. Two questions where the problems were considerably higher for the owners was: “I have trouble understanding things on TV,” and “I have trouble understanding the speaker in a large room.”
- Both ENT and general physicians recommended only 12% of people self-identified as having hearing problems consider pursuing hearing aids. In contrast, those who reported that the first person they sought information from was an HCP, 52% had confirmed hearing loss, and 41% reported that hearing aids were recommended.
- When asked why they made the appointment to seek help with their hearing, 52% of hearing aid owners stated it was because of a recommendation from a friend, whereas only 27% of non-owners gave this reason. On the other hand, 53% of non-owners stated it was because of the recommendation of a spouse/partner; only 25% of owners gave this reason.
In Summary
In this first section of Volume 8, we have provided some background regarding the prevalence, and the projected “unmet hearing care needs.” Research shows that even for those who recognize that they have a hearing loss, adoption of hearing aid use is often postponed, or simply doesn’t occur. As shown in the MarkeTrak10 survey, many non-owners report having a hearing loss, and have had their hearing tested by an HCP. In the following sections of this QuickTakes Volume, we’ll discuss tools some that can be used to further evaluate these individuals, and hopefully move them into the hearing aid owner category.
8.2: Theories and Models Related to the Patient Journey
In the previous section we discussed the unmet need for hearing health care in the U.S. If we include those individuals with a mild impairment, it is estimated that the total is 39-42 million (Humes, 2023). Interestingly, MarkeTrak data tells us that a large percent of these individuals with unmet needs—people who state they have a hearing loss but do not use hearing aids—have been evaluated by a hearing care professional (HCP). We can assume, that in most cases, the use of hearing aids was recommended at the time of this visit, but for one reason or another, the patient didn’t follow through with the recommendation. Why is this? If we look carefully at the “why,” it might be possible to speed up the journey to hearing aid use.
Stages of Change Models
Stages of change models are common in various areas of psychology, counseling, and health care, dealing with such issues as smoking, alcohol abuse, addiction, weight control, etc. The stages of change model that most of us are most familiar with is the Kübler-Ross Stages of Grief, born from her book On death and dying (1969). As a refresher, the stages are: denial, anger, bargaining, depression, and acceptance. While this model is geared toward grief, often associated with dying, there are stages of change theories and models that can be adapted for hearing health care.
Transtheoretical Stages of Change Model
This is perhaps the most common model used relating to health behavior, going back at least 40 years to the 1980s work of Prochaska & DiClemente (1983). The Transtheoretical Model (TTM; also called the Stages of Change Model), evolved through studies examining the experiences of smokers who quit on their own, compared to those requiring further treatment. TTM focuses on the decision-making of the individual and is a model of intentional change. It operates on the assumption that people do not change behaviors quickly and decisively.
As mentioned, much of the research related to this model has centered around smoking cessation and other addictive behaviors such as alcohol and drug abuse. However, in more recent years, it has been used for numerous other applications ranging from stress management, medication compliance, exercise participation, weight control, and even preventative measures, such as medical screening tests. Given the long time-course to treatment and low hearing aid uptake rate, the TTM seems like a reasonable way to better understand how individuals cope with their condition. The model traditionally has six stages, as shown in Figure 6.
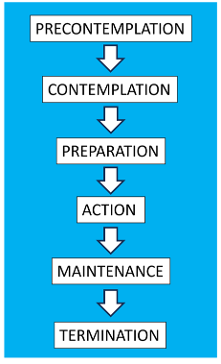
Figure 6. The six stages of the Transtheoretical Stages of Change model (from Prochaska & DiClemente, 1983).
The mostly-standardized version of this model, particularly when the model is used in conjunction with drug and alcohol addiction, sometimes has a stage referred to as “relapse.” And one stage that you see in Figure 6, labeled “termination,” is rather misleading when applied to hearing aid adoption. Even when the outcome is a successful hearing aid user, counseling and often re-programming is needed for the life of the hearing aids, and hence, the patient remains in maintenance and never really is terminated. Hence, we’ll simply focus on the first five stages shown in Figure 6. According to the TTM, a person likely to engage in health behavior change displays low Precontemplation and high Contemplation, Preparation, Action, and Maintenance scores. The following research reviews these primary five stages (see Raihan & Cogburn, 2023).
Precontemplation. These usually are people who don’t believe that they have a problem and, therefore, are very unmotivated to take action. They often lack insight regarding the consequences of their negative behavior. After all, if you don’t believe you have a problem, why would you seek help from a professional? These individuals often obsess about the negative side of change rather than recognizing the benefits that they would gain. They may exhibit elements of change (if pressure exists to do so) but will quickly return to their old habits.
Relating to hearing aid adoption. Unfortunately, this category is a large percentage of those with unmet needs. These people might be aware that they have a hearing problem, but usually are in denial, or lack awareness that hearing loss is affecting their communication ability. Individuals in the contemplation stage of change often say things during an appointment like, “Other people mumble.” Or “I hear what I need to hear.” They are quick to point out the negatives (true or not) of using hearing aids. If they do come in for a hearing test, it’s often because a family member made the appointment. If pressured enough, they will try hearing aids, with probably no intent of ever using them.
Contemplation. At this stage, the patient is aware they have a problem and understand it might also be a problem for others. But, they may not be sure that the problem is worthy of correcting. They are still hesitant to make a commitment to taking the necessary steps toward change. People can be stuck in contemplation for several months, or even years. In general, however, they might be open to receiving some generic information about the problem.
Relating to hearing aid adoption. Persons in the contemplation stage might start to admit to close friends and family members that the reason they are missing parts of conversations is because of their hearing loss. However, many contemplators are more than happy to put the onus on others. For example, it is common for some contemplators to say they don’t have a hearing problem when their spouse talks louder or when the TV volume is turned louder. They may even start to take some limited action to assist with their hearing, such as positioning themselves better for conversations, asking people to repeat when they miss something, using captioning while watching TV, etc. They are uncertain, however, if any treatment (obtaining hearing aids) is needed.
Preparation. It is during this stage the person acknowledges that a behavior is problematic and is more or less ready to make a commitment to solve the problem, recognizing that receiving treatment is probably better than the status quo. People begin gathering information during this stage, which should be encouraged. People usually intend to act in the next month or so, and usually have taken behavioral steps towards that direction over the past year.
Relating to hearing aid adoption: The person becomes more “tuned-in” to hearing aids and hearing aid use; paying more attention to television ads and conducting Google searches. People also start having conversations with friends and colleagues who are using hearing aids or have tried hearing aids. It is relatively easy to recognize someone who is in the preparation stage because they ask a lot of questions about hearing tests and hearing aids. In some cases, however, the information gathering can be excessive, including sorting out and categorizing brands, features, and prices.
Action. As the term suggests, in this stage meaningful change happens. People gain confidence in their decision and are willing to receive assistance and support. As the name of the stage implies, people in the action stage readily follow the recommendations and guidance of the hearing care professional. Importantly, in this stage, change is not only the action, itself, but all the prerequisite work required to act on changing the behavior. Prematurely jumping to this stage, without adequately preparing can lead to difficulty.
Relating to hearing aid adoption. Persons with hearing loss often need time to process or grasp the consequences of their condition before they take action. For some it might be just a few months, for others it might be several years. Hence, hearing care professionals are advised to respect the time it takes the individual to move into the action stage of change. In reality, many patients who are in the clinic for the first time having their hearing tested are probably not yet in the action stage of change. Laplante-Levesque et al. (2015) evaluated 224 adults who had failed an online hearing screening and determined that less than 5% of this group were in the action stage of change. Although it is likely that a higher percentage of individuals who are in the clinic seeking help from an HCP are in the action stage, these research findings suggest us that most first-time help seekers are probably not in the action stage. This represents an opportunity to guide these individuals into action by applying some specific counseling strategies that speed the journey. The simple act, for example, of asking a patient in one of the “pre-action” stages of change to describe the potential benefits of wearing hearing aids is one counseling strategy that could move some patients closer to the action stage of change. For more examples of counseling strategies that might guide patients into the action stage, see Taylor (2022).
Maintenance. As people progress through this stage, they become more confident that obtaining the treatment was a wise decision. They are less fearful that they will return to their old behavior. They have a new status quo.
Relating to hearing aid adoption. Following the initial fitting, the patient returns within a few weeks for follow-up counseling. Programming changes are made if necessary as well as re-instruction of patient-controlled features. The patient completes a self-assessment inventory to assess if fitting goals have been met. Future return visits are scheduled periodically, and communication is maintained through tele-audiology.
Recently, Bennett and colleagues (2024) created a specific counseling program that we think fits well into the maintenance stage of change. Their approach goes by the acronym AIMER. The AIMER counseling approach is a structured framework designed to enhance the counseling process by focusing on the emotional and social needs of the individual. Although the AIMER approach can be applied to any facet of the patient’s journey, we think it is particularly well-suited to be used during post-fitting follow-up visits. AIMER stands for Assessment, Intervention, Monitoring, Evaluation, and Review. Each component plays a critical role in ensuring effective outcomes. Here's a quick breakdown of each element:
- Assessment: This initial phase involves gathering comprehensive information about the patient’s background, current situation, and presenting issues. The aim is to develop a thorough understanding of the patient’s needs, strengths, and challenges.
- Intervention: Based on the assessment, specific interventions are designed and implemented. These interventions are tailored to address the patient’s unique needs and may include various therapeutic techniques and strategies.
- Monitoring: Continuous monitoring of the client's progress is crucial. This involves tracking changes, both positive and negative, to ensure that the interventions are effective and to make adjustments as needed.
- Evaluation: Periodic evaluation is conducted to assess the effectiveness of the counseling interventions. This involves reviewing the patient’s progress towards their goals and determining the overall impact of the therapy.
- Review: The final phase involves a comprehensive review of the entire counseling process. This includes reflecting on what worked well, what didn't, and any lessons learned. The review phase helps in refining future counseling strategies and ensuring continuous improvement.
The AIMER approach, which we will revisit later in Section 8.5, underscores that the maintenance stage of change is a dynamic process. Using AIMER ensures that the HCP’s counseling is responsive to the patient’s evolving emotional and social needs and that outcomes are continuously optimized.
More Research on the TTM
There has been some interesting research regarding how fast people move from one stage to another (Prochaska et al., 1992). Findings revealed that moving from one stage to the next within one month will double one's chances of acting on changing behavior in the next six months. If someone is still in the precontemplation stage at the of first month (and nearly all hearing candidates still are), only 3% progress to action by six months. For contemplators remaining in this stage for one month, only 20% acted by six months. This helps explain the slow adoption rate of hearing aid use that we’ve discussed.
Earlier we mentioned that we would just use the five basic stage categories, shown in Figure 6. We should mention, however, that with hearing aid use, “relapse” is more common than we would like—something that has historically been referred to as an “in-the-drawer” fitting. While we don’t usually refer to it as relapse, this is when the patient purchased the hearing aids, did not return them, but now is not using them. Dillon et al.. (2020), for example, conducted an extensive survey of hearing aid owners in the UK and determined that 20% of the respondents did not use their hearing aids at all, and another 30% of respondents reported that they used them sporadically. Hearing aid manufacturer data from the US and Europe show similar trends with 20 to 40% of hearing aid owners reporting that they use their hearing aids four hours/day or less (EHIMA, 2018-2022).
Closer to home in the US, where direct-to-consumer (DTC) products have been available for several decades, these “non-use” numbers are harder to track. Some estimate that of those who make the decision to purchase hearing aids, 10-20% do not use them. This, of course, would seem predictable with DTC products, but even HCPs following best practice will admit that they have some patients who, they might discover months or even years later, stopped using their hearing aids. Oftentimes, these are not the patients who are coming back and complaining about one thing or another, as they are somewhat reluctant to admit that they didn’t follow through with the treatment plan. Our best guess is that these are patients who skipped the planning stage, and maybe even the contemplation stage, and went directly to action—perhaps because of pressure from family members. Longitudinal studies with smoking and drug addiction have shown what might be expected . . . the longer the person stays in the maintenance stage, the less likely there will be relapse. The same is true for hearing aid use—it’s uncommon for someone who has been a regular user for over six months, or certainly a year, to abandon hearing aid use.
Health Belief Model (HBM)
The HBM is one of the oldest models and has been applied to a very broad range of health behaviors and populations. The model is based on six constructs that influence the likelihood that people will take action to prevent, screen for, or control health conditions (See Figure 7; Rosenstock, 1974). The general premise of the model is that people are more inclined to change behavior when they believe that doing so might reduce a threat that is probable, and that would have severe consequences if it occurred.
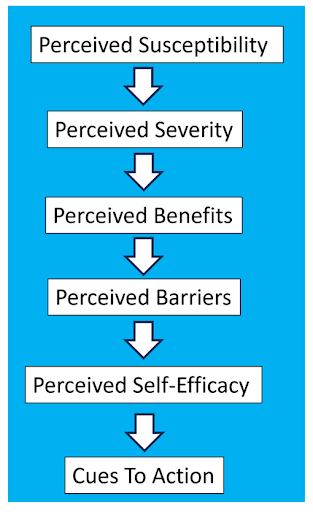
Figure 7. The six stages of the Health Belief Model.
Saunders et al. (2016) nicely review the six constructs of the HBM, and the following is taken from their work:
- Perceived susceptibility: The feeling of being vulnerable to a condition and the belief of being at risk of acquiring the condition.
- Perceived severity: Belief in the seriousness of the health and social consequences incurred if affected by the condition.
- Perceived benefits: Belief that an intervention will result in positive benefits.
- Perceived barriers: Barriers believed to be needed to be overcome to effectively conduct an intervention.
- Perceived self-efficacy: Belief in one’s ability to use and gain benefit from an intervention.
- Cues to action: Prompts to take action, which could be internal, such as symptoms of a health problem, or external such as communication from healthcare providers, other people, or media.
According to the HBM, a person likely to engage in behavior change perceives high severity, susceptibility, benefits, cues for action and self-efficacy, and has few barriers.
The impact on these stages on heath behavior have been studied extensively. Going back to 1984, Janz and Becker, using a “significance ratio” across 46 studies found that the barriers component had the most consistent relationship (89%), followed by the susceptibility (81%), benefits (78%) and severity (65%) components. Carpenter (2010), using a meta-analysis approach, examined the strength of the correlations. The barriers component was found to have the highest average correlation (r = −0.30), followed by benefits (r = 0.27), severity (r = 0.15) and susceptibility (r = 0.05). In general, studies of this type have found significant, but small correlations between the HBM and health behavior.
COM-B Behavior Model
A third model that has sometimes been used relative to hearing aid adoption is the COM-B (Michie et al., 2011). The name is an acronym for the three primary components for change: Capability + Opportunity + Motivation can change Behavior (see Figure 8).
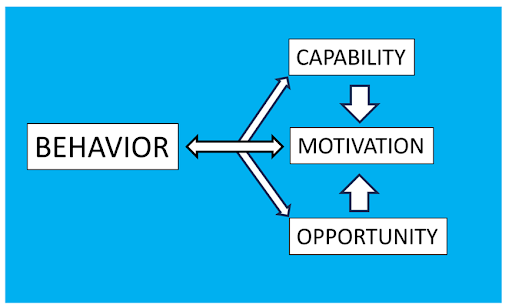
Figure 8. The components of the COM-B behavior model (adapted from Michie et al., 2011).
The steps can be described as follows:
- Capability. Refers to an individual’s psychological and physical ability to make a change, or to participate in an activity. Relating to a delay in hearing aid adoption, this could be related denial or minimizing hearing problems, a perceived stigma regarding the use of hearing aids, or the belief that hearing aids are not helpful.
- Opportunity. Refers to external factors that make a behavior possible. Factors could be things like social environments, an improved financial situation, or effective marketing regarding the cost of hearing aids.
- Motivation. The conscious and unconscious cognitive processes that direct and inspire behavior. Often, the decision to obtain hearing aids is related to positive reports from friends and family who are hearing aid users, or a significant event where the hearing loss caused more problems than usual.
This model recognizes that behavior is influenced by many factors, and that behavior changes are induced by modifying at least one of these components. Barker et al. (2016) examined, by interviewing dispensing audiologists, whether the application of the COM-B method could be used to help understand the individuals with hearing loss who choose not to use hearing aids. The respondents believed that physical capability was not an issue, but both physical and social opportunity were important. And, as we all know, they also agreed that motivation played an important role.
Health Behavior Scales and Hearing Aid Adoption
Various research studies have examined how these health behavior scales could be used to assist in the speeding of the adoption of hearing aids, for those individuals who recognize that they have a hearing problem. One study of this type was by Saunders et al. (2016), who administered several self-assessment scales to a large group of adults (n=167; mean age 69.3 years) seeking hearing help for the first time. At the six-month follow-up date, 120 (72%) had taken up hearing aids, and 47 (28%) had not. Importantly, these were individuals seen at a VA clinic, and hence, the cost of hearing care was not an issue.
One of the self-assessment scales given to all participants was the University of Rhode Island change assessment (URICA). For this study, original items of the URICA were adapted for hearing health behaviors. The adapted URICA consists of 24 items that assess readiness for change on three eight-item scales: precontemplation, contemplation, and action—note that these are three of the stages we discussed earlier taken from the TTM (see Figure 6). A higher URICA score indicates greater agreement with the TTM construct being assessed.
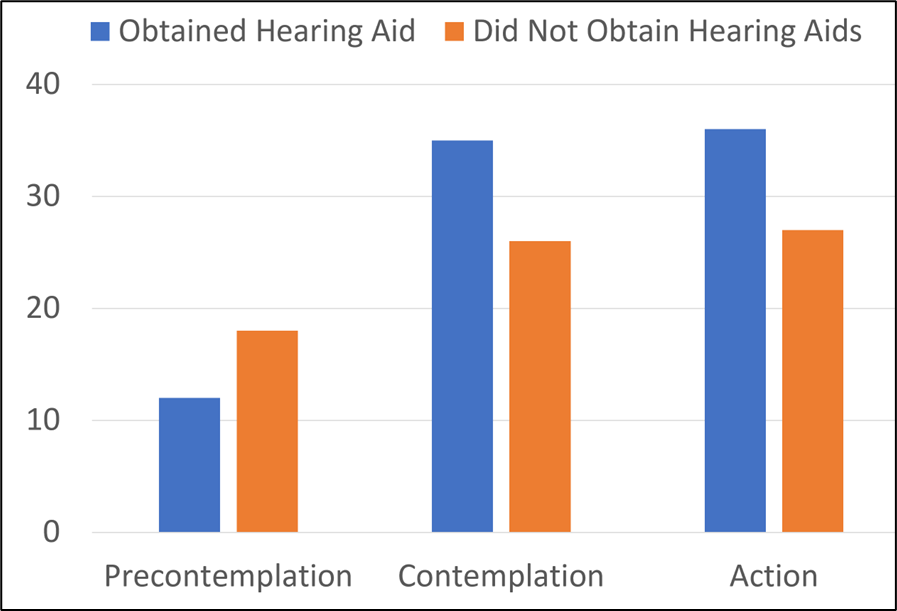
Figure 9. Shown is the relationship between the health behavior stage and the decision to obtain hearing aids. The Y-axis is the score for the modified University of Rhode Island Change Assessment (URICA) scale.
One of the findings from the Saunders et al. (2016) study is shown in Figure 9. The Y-axis is the URICA score. Note the expected findings—for those who obtained hearing aids, the URICA score was lower for Precontemplation, and higher for both Contemplation, and of course, Action. Saunders et al. also examined hearing aid uptake relative to the stages of the HBM (see Figure 7). Those participants who obtained hearing aids had higher HBM scores for Susceptibility, Severity and Benefits.
Regarding the use of the constructs of the TTM and HBM for understanding hearing health behaviors, Saunders et al. (2016) summarized that attitudes and beliefs:
- Were associated with future hearing health behaviors.
- Were effective at modeling later health behaviors.
- Change positively following behavior change.
- Are better predictors of hearing-aid outcomes than are attitudes and beliefs at the time of initial hearing help seeking.
Based on their findings, the authors conclude that a counseling-based intervention, targeting the attitudes preventing behavioral change has the potential to increase uptake of hearing health care.
As mentioned earlier, there have been several studies relating health behavior change models to audiology and the use of hearing aids. The most common perhaps has been the TTM “stages of change” which looks at the process of intentional change in behavior (see Figure 6). Manchaiah et al. (2018) conducted a descriptive literature review aimed at identifying and presenting a summary of research (n=13 studies) that used TTM to study the attitudes and behaviors of adults with hearing loss.
In general, the researchers’ conclusions were:
- There are positive associations between stages of change and help-seeking, intervention uptake, and hearing rehabilitation outcome, such as benefit and satisfaction.
- Associations with intervention decisions and intervention use were not evident.
- Understanding the readiness toward help-seeking and uptake of intervention in people with hearing loss based on TTM may help clinicians develop more focused management strategies.
Summary
The time delay for people to obtain hearing aids, following their acknowledgement that they have a hearing problem, seems to have always been a major concern for both HCPs and manufacturers. This large, underserved population in fact, has been the enticing data that has encouraged the emergence of many start-up hearing aid companies—most of which have failed. As HCPs, we are always looking for new ways to speed up the process. As we have reviewed here, taking various health behavior change models that have been successful in other health areas, and applying them to hearing aid adoption, may help in understanding the patients current thinking, and steer patient counseling in the best direction.
8.3: Before the Fitting - Understanding Patients’ Emotional and Psychosocial Concerns
As we discussed in the previous section, the journey to obtain hearing aids usually starts in the precontemplation and contemplation stages. At this point, the patients are aware that they have a hearing loss and acknowledge that this might be a problem not only for them, but for family members. Often associated with this, however, is emotional distress, which can be overlooked by the HCP, who is anxious to provide technical assistance. Research has shown that considering an individual’s experiences of living with the hearing loss disability, and the potential emotional consequences of this handicap, often will improve overall patient care. In this section, we’ll discuss how an understanding of this will assist in our patient counseling, and hopefully facilitate treatment.
Emotional Distress Associated with Hearing Loss
Psychological and emotional distress can negatively affect help-seeking for hearing loss treatment and the use of hearing aids. Bennett et al. (2022) examined the social challenges and emotional distress in relation to hearing loss and the coping mechanisms employed. Their data was collected in focus groups for 21 adults who had hearing loss and reported emotional distress due to the hearing handicap.
Their findings revealed that individuals described their social and emotional experiences of hearing loss in terms of:
- Negative consequences (social overwhelm, fatigue, loss, exclusion)
- Identity impact (how they perceive themselves and are perceived by others).
- Emotional distress (frustration, grief, anxiety, loneliness, and feeling burdensome).
Coping strategies that were reported included: avoidance, controlling the listening environment, humor, acceptance, and assertiveness. The authors report that many participants described a lack of effective coping strategies and tended to rely on avoidance of social interaction. This of course leads to increased social isolation, which we know has been associated with cognitive decline. Bennett et al. (2022) conclude by pointing out that despite the recognized need of our patients, HCPs do not have a formalized method to intervene and assist with the social and emotional difficulties that occur due to hearing loss.
Patient Interaction and Communication
We know that effective communication with our patients throughout the hearing aid fitting process positively influences adherence to treatment, patient outcomes and satisfaction, and is a vital component of patient-centered care. This has not been commonly studied, however, in the area of audiology, in particular the hearing aid fitting process. One study that did systematically examine this area was the research of Grenness et al. (2015), who explored the verbal communication between audiologists and patients/companions throughout diagnosis and management planning in initial audiology consultations. Their goal was to describe the communication in these interactions by examining the number, proportion, and type of verbal utterances by all speakers (audiologist, patient, and companion when present).
They collected data from a total of 62 audiological rehabilitation consultations involving 26 different audiologists. All patients were older than 55 years, and a companion was present for 17 of the consultations. The encounters were filmed and analyzed using the Roter Interaction Analysis System (RIAS). If you’re not familiar with the RIAS, this is a form of conversation analysis that was first introduced in 1977 (see review by Roter & Larson, 2002), used mostly for coding dialogue, and has been widely used in the U.S. and Europe for many different disciplines. It’s reported that its popularity is because of the system's ability to provide reasonable depth, sensitivity, and breadth while maintaining practicality, functional specificity, flexibility, reliability, and predictive validity to a variety of both patient and provider outcomes. The RIAS is applied to the smallest unit of spoken expression to which a meaningful code can be assigned, generally a complete thought, expressed by each speaker throughout the medical dialogue.
One of the RIAS findings relates to communication profiles, which examines mean total utterances, range, and proportion of utterances for each of the four RIAS categories. The four categories for the caregiver (audiologists in this study) are: Education and counseling, Data gathering, Building a relationship, and Facilitation of patient activation. The four categories for the patient are: Information giving, Question asking, Building a relationship, and Activation and engagement.
Data reported by Grenness et al. (2015) for the audiologist for the utterances throughout the diagnosis and management planning phase:
- Education and counseling in nature was 48%. An estimated 83% of the education and counseling was biomedical in content (e.g., “this type of hearing loss is permanent and most likely the result of aging”).
- An estimated 71% of the information given was affect-neutral (e.g., “there are two main styles of hearing aids”). An estimated 29% of the information was persuasive in nature (e.g., “You’ll notice a big difference in this hearing aid because of the speech enhancement; it’s worth the extra cost”).
- The second most common category of utterances for audiologists was building a relationship (26%).
- Audiologists spent 22% of their utterances on facilitation and patient activation, consisting mostly of procedural utterances such as transitions and orientations.
- The smallest category of utterances for audiologists was data gathering (4%); closed-ended psychosocial/lifestyle questions were most frequent.
Grenness et al. (2015) report the following summary of patient utterances during the diagnosis and management planning phase:
- Most common was building a relationship (60%); agreement utterances were the most common, followed by social talk and emotional talk.
- Patients spent 25% of their utterances giving information; slightly more than half of this information was psychosocial/lifestyle in nature.
- Activation and engagement (11%), and question asking (6%) were the least common categories of codes.
Grenness et al. (2015) summarize their findings by saying that when they interpret their results, they find that they seldom observe the desired patient-centered communication. Patients’ psychosocial concerns were rarely addressed, and patients/companions showed little involvement in the management planning process. Audiologists’ utterances categorized as education had little content explaining diagnoses or discussion of rehabilitative options (other than the use of hearing aids), and rarely engage in affective conversation. Previous research suggests that this possibly is a way of avoiding challenging emotional conversations (see Manchaiah et al., 2019 for a review). Addressing psychosocial concerns and facilitating patient engagement differentiates patient-centered from practitioner-centered consultations. These data suggest that there is considerable room for improvement among audiologists in this area.
A companion study on this general topic was conducted by Ekberg et al. (2014), which conducted systematic research exploring how patients’ concerns about hearing aids are addressed by audiologists during the clinic visit. A total of 63 consultations with 26 different audiologists (62% women) were filmed. All appointments reflected the initial hearing assessment with an adult patient (>55 years old) involving a discussion about hearing rehabilitation options; or it was a follow-up appointment in cases where rehabilitation options were not discussed during the first appointment. Companions were present in 17 of the 63 consultations. The video data were transcribed, and the transcripts included details of pauses, overlapping talk, cutoffs, intonational contours, and nonverbal communication, all found to be useful for how participants understand conversation.
Some key findings of the conversation analysis were:
- Patients raised concern about the use of hearing aids in 51% of the appointments where hearing aids were recommended.
- When patients expressed concerns regarding hearing aids, these concerns usually were psychosocial in nature.
- Typically, the concerns were expressed in a way that carried a negative emotional stance.
- Audiologists’ responses usually did not align with the psychosocial
- nature of the patient’s concern.
- Patients then, tended to escalate their concerns in subsequent speaking turns.
- Perhaps most importantly, when patients’ concerns remained unaddressed, they often left the appointment without making a decision about using hearing aids.
We know from the work of Erdman (2013) and others, that audiologists must be prepared to listen, empathize, and validate patients’ experiences and feelings about their hearing loss and possible related treatment. Ekberg et al. (2015) state that the findings from their study suggest that there appears to be a need for further development in this area within audiologic practice. There may be some hope, however, as Kris English and colleagues (1999) reported that a significant change was identified in the number of affective responses made by audiologists in their patient conversations after they had completed a counseling course.
To continue our discussion on this topic, we’ll also mention the work of Grenness et al. (2014a), who specifically studied audiologic rehabilitation from the perspective of older adults who had owned hearing aids for at least one year. Their data analysis revealed three dimensions: the therapeutic relationship, the players (audiologist and patient), and the clinical processes. They point out the critical need for a therapeutic relationship, a fundamental requirement for healthcare interactions. According to participants in this study, the key ingredient in developing a therapeutic relationship was trust. Descriptions of audiologist behaviors consistent with a trustworthy professional were interpersonal skills such as: caring, listening, friendliness, and providing ample time for the patient to respond to the audiologist’s open-ended questions. The authors point out that trust is particularly important in the context of audiologic rehabilitation due to the sale of hearing aids in many settings.
The second category identified related to maintaining a therapeutic relationship. Not surprisingly, this involves factors that have been reported in previous studies such as listening, being sympathetic, and showing emotional interest. Based on their findings, Grenness et al. (2014a) developed a simplified clinical model for operationalized patient-centered audiologic rehabilitation (Figure 10).
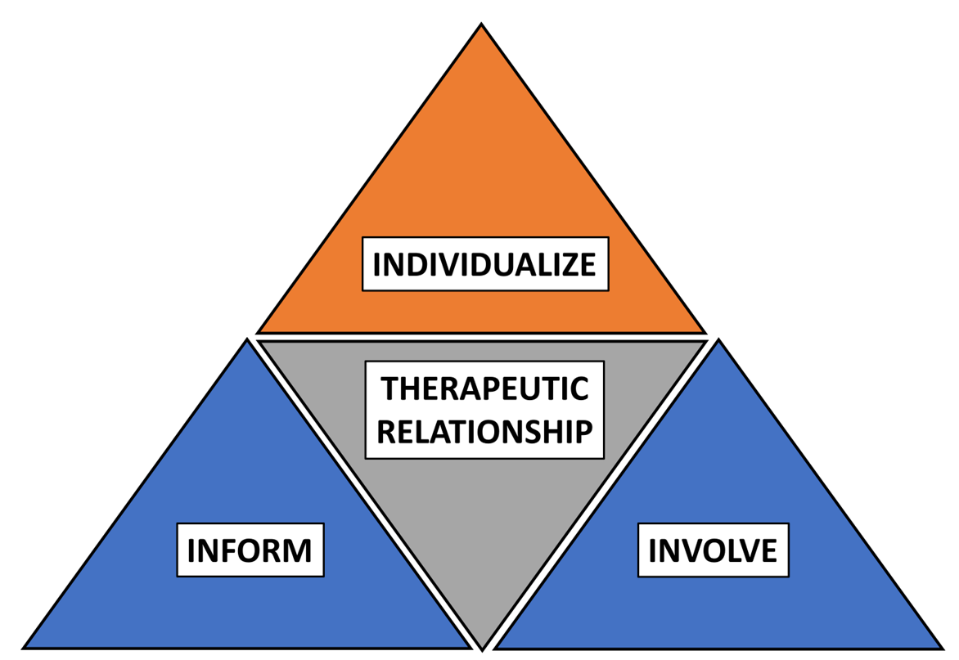
Figure 10. Clinical model for operationalized patient-centered audiologic rehabilitation where hearing aids are recommended (adapted from Grenness et al., 2014a).
Understanding Patient-Centered Care
What we have been discussing in this section all falls under the umbrella of patient-centered care. This concept has been discussed in medicine for decades but was not discussed much in the profession of audiology until the past ten years or so. Before leaving the topic, it might be useful to go a little deeper into this concept.
Grenness et al. (2014b) published an excellent review article on how patient-centered care can be applied in rehabilitative audiology. In this section, we will paraphrase much of their work. See their paper for more details and references. In their article, they address (and answer) five questions on this topic: What is patient-centered care? What are the outcomes of patient-centered care? What are the factors contributing to patient-centered care? How is patient-centered care measured? What are the implications for audiologic rehabilitation?
1. What is Patient-Centered Care?
Grenness et al. (2014b) define patient-centered care as the concept that patients should be encouraged to be active participants in their health care through the creation of a power-balanced, therapeutic relationship with their health professionals. This is contrary to the more traditional mode of health care, termed “practitioner-centered.” While there is not a well-defined model for patient-centered care specific to audiology, we can borrow from the field of primary care medicine, which was developed based an extensive review of empirical literature, and has five key components (Mead and Bower, 2000).
- Biopsychosocial perspective: Health care should take into account a person’s psychological and social states as well as the biological impact of the health condition.
- Patient as person: The health professional should try to understand the patient as an individual within his or her own context.
- Sharing power and responsibility: Importance is placed on the patient’s lay knowledge and self-expertise and encourages equality in power.
- Therapeutic alliance: The relationship between health professional and patient is important and has in itself therapeutic effects.
- Practitioner as person: The health professional brings value and subjectivity to the relationship; self-awareness is important
2. What are the Outcomes of Patient-Centered Care?
Grenness et al. (2014b) speak of the outcomes in three general categories: patient satisfaction, patient adherence and health outcomes, and practitioner outcomes.
Patient Satisfaction. Not surprisingly, numerous studies have reported an association between patient-centered interactions and improved patient satisfaction, although it’s important to point out that not all patients prefer this approach. We suggest that an agreement between the patient and the HCP regarding degree of the patient-centered approach, will help to maximize satisfaction.
Patient Adherence and Health Outcomes. We know that in most cases, adherence to treatment will result in better overall health outcomes. Involving the patients in decisions regarding their treatment has been found to improve adherence, increased self-management and the overall interest of the patient regarding their care.
Practitioner Outcomes. While we usually think of patient-centered care as a benefit for the patient, in many cases, benefits for the practitioner (HCP) also exist. For example, research shows that fewer malpractice cases are filed when patient-centered care was employed. And as you might expect, higher job satisfaction for the practitioner exists when the patient’s treatment adherence and outcomes are more positive.
3. What are the Factors Contributing to Patient-Centered Care?
Grenness et al. (2014b) list four categories of factors that reportedly influence the occurrence of patient-centered care: patient, practitioner, organizational, and research and implementation-related factors.
Patient-related Factors. Patient-related factors that have been found to influence the implementation of patient-centered care include (see Grenness et al., 2014b, for specific references):
- Gender: Women tend to be given more information, be asked more questions, and tend to respond in a more emotionally expressive style.
- Ethnicity: Caucasian patients receive more information, higher quality interpersonal connection, and more skilled questioning and empathy from their practitioner.
- Age: Older patients prefer, on average, a more paternalistic model of healthcare.
- Education: Patients with higher levels of education are more likely to be able to express their preference for involvement in decision-making to their practitioner and prefer a more patient-centered approach.
- Socioeconomic status: Patients from high socio-economic backgrounds made more attempts at active participation; patients from a lower socioeconomic background received less information and less partnership building attempts from their practitioners.
- Health status: Patients who report a better health status are more likely to receive a patient-centered interaction; patients with a lower health status acted more negatively and passively towards their practitioners.
Practitioner-related Factors. Female or Caucasian practitioners with more years of experience have been found to be more patient-centered; female practitioners seeing female patients more effectively used non-verbal cues and spent more time than with male patients. Male-male encounters yielded the least patient-centered interactions.
Organizational-related Factors. Most of the research in this area revolves around the length of the appointment. Studies have shown that patient-centered appointments do not necessarily take longer than practitioner-centered ones. While longer would seem better, two different studies have shown that the amount of time spent in an encounter was not linked to patient satisfaction (Grenness et al., 2014b).
Research and Implementation-related Factors. Most of the research regarding patient-centered care and audiologic rehabilitation has only occurred in the past ~20 years. The findings, however, are similar to that from medicine and other disciplines; trusting the practitioner, being informed and educated, and being provided with options. A separate study found that important concepts included the patients’ want for empowerment, for the audiologist to understand their needs, and their want to feel comfortable and be supported in shared-decision making.
4. How is Patient-centered Care Measured?
Grenness et al. (2014b) report that although patient-centered care has been studied for decades, there is no well-established gold standard for its measurement. Historically, methods usually have included observational techniques using audio or video footage, and patient or practitioner questionnaires—recall that we discussed the use of the Roter Interaction Analysis System (RIAS) earlier in this section. They note that over 50 instruments exist which examine the nature of the interaction through rating scales, checklists or verbal/non-verbal coding schemes. It is also helpful if the measurement of patient-centeredness is accompanied by a measure of its effect on outcome.
5. What are the Implications for Audiologic Rehabilitation?
There are some issues related to patient-centered care in audiologic rehabilitation that make it somewhat different than the application in general medicine. The most obvious, is that in most cases, the sale of hearing aids is part of the treatment process. It is very common, that this prompts the patient to enter into a discussion of cost (“I can get them for ½ the price at Costco”), which puts the HCP on the defensive, which can work against the goal of being a good listener and compassionate. Moreover, there are some dispensing offices that advance the practitioner-centered approach, as it is believed that this is more apt to result in more hearing aid sales.
With that said, Grenness et al. (2014b) had two general comments regarding increased implementation of patient-centered care for audiologic rehabilitation:
- Given that there is a lack of research in this area specific to our discipline, they believe that a definition of patient-centered care specific to audiologic rehabilitation is required, including qualitative studies that take the patient's perspective into account.
- Secondly, they suggest that through the identification of what patients want from audiologic rehabilitation, we can then investigate whether audiologic rehabilitation is patient-centered and identify the barriers and facilitators to its implementation.
Practical Applications of Patient-Centered Care
It probably goes without saying that hearing aid technology and testing are central to patient care; however, it is easy for audiologists to develop an over-reliance on them, and lose sight of the patient as a person – a person, who, according to the research cited in this section, wants a trusting relationship with their service provider. For example, Amlani (2016) found that “audiologists are falling short in creating a positive emotional communication relationship, which might be a factor in why impaired listeners are not adopting audiologic services and technology.” Although hearing care is a “technology-reliant” profession, there are a few simple things, based on the research reviewed here, HCPs can do to be more patient-centered.
- During the in-take appointment, collaborate with the patient on setting treatment goals. Record these goals on the Client Oriented Scale of Improvement (COSI; see Taylor & Mueller, 2023a). This collaborative process should permeate all appointments. As outlined by English (2022), there is a difference between standard instructions and joint goal setting. For example, at the initial fitting a standard instruction might look like this: “You will still have problems in noise. It’s unavoidable.” In contrast, joint goal setting for this standard instruction would sound like this: “It’s quiet in the fitting room right now, but let’s think about noisy situations for you. What might those be in your life? Let’s talk about some things you can do to improve communication there.” Notice that joint goal setting invites the patient to reflect on his own daily life experiences as part of the hearing aid orientation process.
- Encourage a family member to attend appointments with the patient. When making appointments say: “Our experience is that it is very helpful if you can bring a friend or a loved one along to the appointment. Who would that be?” If the patient asks for more information, we could say “There is a lot to discuss, and it helps to include family and friends in the process.”
- Ensure that the physical environment is comfortable for the patient and family members.
- Start off the appointment by encouraging dialogue and inclusiveness among all participants in the appointment by saying something like, “We are going to do a lot today. For the next 10 minutes, I want to find out about your hearing and communication (directed to the patient) and then I want to find out about this from your perspective [directed to the significant other].”
- Finally, at a minimum, we recommend that HCPs incorporate the Patient-Centered Observation Form (Cox, 2013) into their counseling approach with patients. This decision aid is a simple way to better inform patients about their treatment options and it allows for more dialogue about the pros and cons of these options.
8.4: During the Appointment: Assessment Tools Beyond Routine Audiometrics
In the previous section, we focused on the importance of patient-centered care, and how this approach will not only improve the HCP-patient relationship but is correlated to long-term patient satisfaction—including satisfaction with hearing aids. We can assume, that the more we learn about our patients during the pre-fitting process, and the better we understand our patients, the greater the probability that effective patient-centered care will result. We of course, historically, have focused on such measures as pure-tone thresholds and speech recognition testing as the cornerstones of our pre-fitting measures. Research tells us, however, that other measures—such as self-assessment scales—are equally, or maybe even more important in determining acceptance, use and satisfaction with hearing aids.
In previous volumes of Research QuickTakes, we have reviewed some popular pre-fitting scales related to the fitting of hearing aids. The most popular appears to be the Client Oriented Scale of Improvement (COSI)—see Taylor and Mueller (2023a), Research QuickTakes Volume 6 (Part 1) for review. This scale, indeed, is very useful for establishing fitting goals, measuring expectations and following hearing aid use, assessing real-world benefit. But there is much more to learn about the patient for effective treatment, and that is what we’ll discuss in this section. Fortunately, for most of our areas of interest, there is an evidence-based scale that can be used to collect meaningful information.
Perception of the Problem
As we previously have reviewed, a measure of the patient’s perception of their hearing problem can be useful in both predicting the adoption of hearing aids, and also, hearing aid benefit—in some studies, as predictive as the measurement of hearing thresholds (e.g., Humes, 2023). Most of Humes' work relied on the HHIE/A (the 25-Question version), but we have a different scale that you might like, if for no other reason than it is only one question! In a retrospective study of over 800 adults, aged 18-95 years, Palmer et al.. (2009) examined the relationship between the patient’s rating of his or her hearing ability, and their subsequent decision to purchase hearing aids. The patient was asked the following question: “On a scale from 1-10, 1 being the worst and 10 being the best, how would you rate your overall hearing ability?”
The answer to the above question was then compared with whether the patient purchased hearing aids. The results are shown in Figure 11.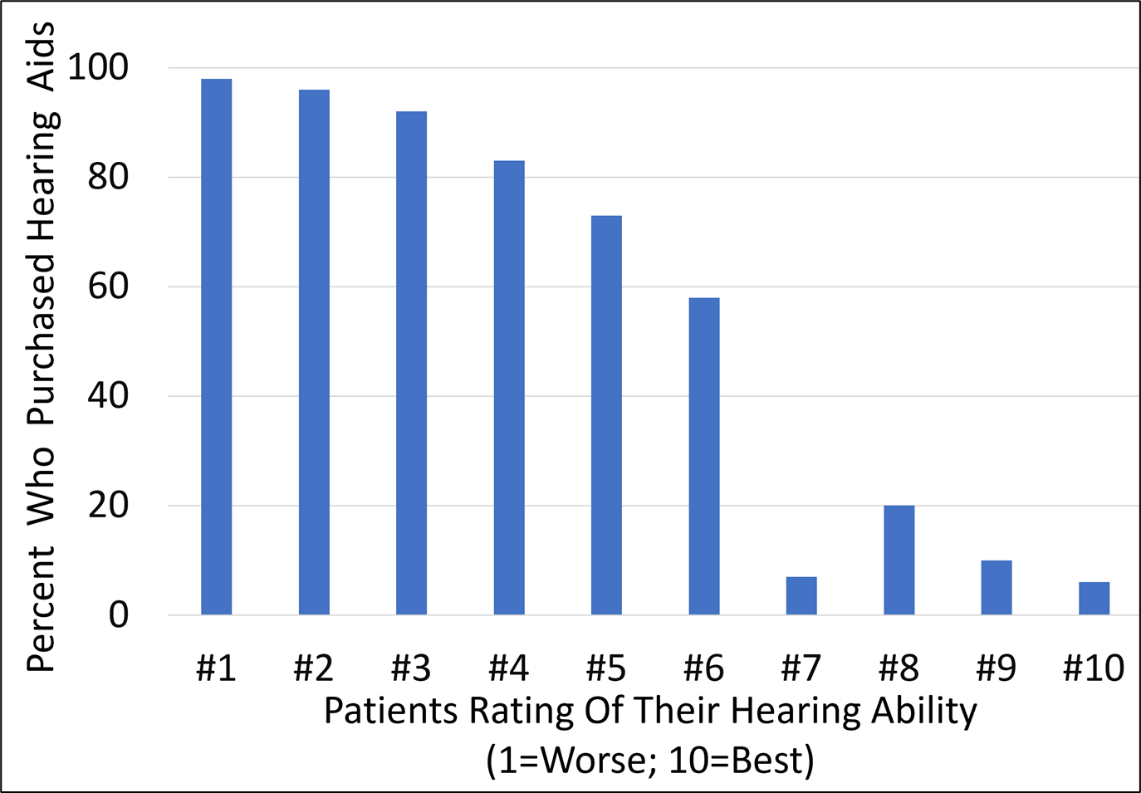
Figure 11. Hearing aid purchase compared to rating of hearing ability. (Adapted from Palmer et al.., 1999).
As we would predict, those that rated their hearing very poorly (e.g., #1, #2 or #3), were very likely to obtain hearing aids—92% or greater. And only a small percent of those who stated that had relatively good hearing (ratings of #7 to #10) purchased hearing aids (20% or less). What perhaps is most interesting in the findings, is the large difference between the #7 rating (7%), and the #6 rating (58%). While only 1 increment apart, the purchase rate increases by 51%! Obviously, there is something about that rating level, which relates to going from contemplation and planning to “action.” This simple scale is just one example of how collecting additional information can be useful and does not always require much extra clinic time or effort.
More recently, a group of researchers affiliated with the VA system modified the Tinnitus and Hearing Survey (THS; Henry, et al. 2015) to quantify the degree of self-reported hearing difficulties in a group of young and middle-aged US Service Members. Comprised of the following four questions of the THS, the THS-H was completed by study participants in about 45 seconds.
- Over the last week, I could not hear or understand what others were saying in a noisy crowded room.
- Over the last week, I could not hear or understand what was being said on TV or in movies.
- Over the last week, I could not understand people with soft voices.
- Over the last week, I could not understand what was being said in a group conversation.
Unlike the original THS, which was designed to triage hearing loss and tinnitus as the primary condition to treat, the THS-H scores each of these questions on a 0 to 10 scale, with 0 “being not a problem” to 10 “being a very big problem.” Based on their statistical analysis, only 5% of Service Members surveyed with clinically normal hearing scored above 27 on the 4-question TSH-H. Thus, a score of 27 was selected as a cutoff for “clinically significant hearing problems” (Davidson, et al., 2023).
In a related study, Davidson, et al. (2024) surveyed 186 Service Members (average age ~35) who were dispensed hearing aids for either amplification or tinnitus relief. They divided the respondents into four groups:
- Hearing loss and no self-reported hearing difficulty
- Hearing loss and self-reported hearing difficulty
- Normal audiogram and no self-reported hearing difficulty
- Normal audiogram and self-reported hearing difficulty
They found that individuals in the normal hearing/self-reported hearing difficulty group (#4 above) were the most likely to wear their hearing aids. Further, 95% of those self-reporting hearing difficulties said they wore their hearing aids every day, and those with no self-reported hearing difficulty, regardless of hearing loss, were highly likely to discontinue hearing aid use within a month or two. Because it takes less than a minute to complete, and identifies individuals with “clinically significant hearing difficulties,” we think the THS-H would be a useful tool for identifying patients with subjective hearing difficulty that might benefit from audiologic intervention.
Social and Emotional Impact
We’ve talked about the HHIE/A self-assessment scale in earlier Research QuickTakes. This is one of the first scales to be used frequently in clinics and research and includes statements that the patient rates relating to both social and emotional aspects of having a hearing loss. To refresh your memory, historically, the HHIE (E=Elderly) was for people 65 or older, and the HHIA (A=Adult) were for patients under the age of 65. In recent years, these scales have been merged and a new 18-item scale is available: Revised Hearing Handicap Inventory (RHHI; Cassarly et al.., 2020). There also is a 10-item screening version that has been shown to have acceptable reliability for clinical use (RHHI-S; see Figure 12). For the screening version, if a score of 6 or higher is obtained, a hearing problem is expected.
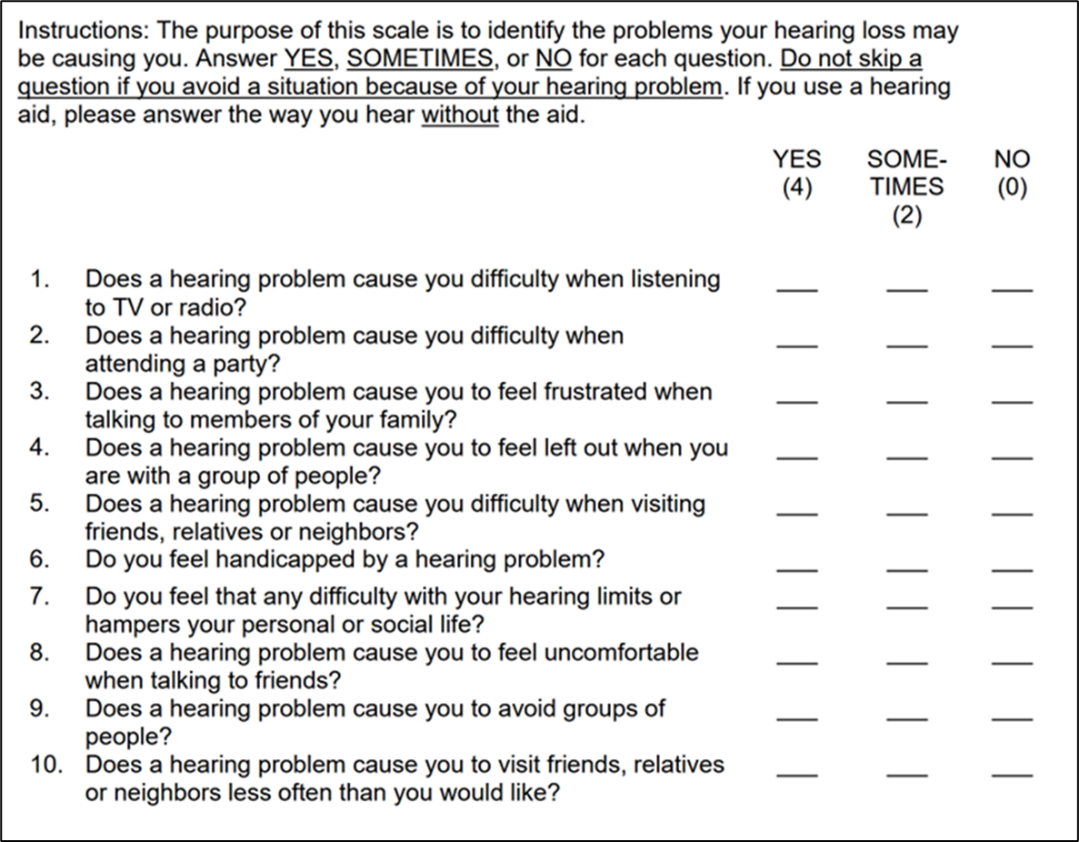
Figure 12. The Revised Hearing Handicap Inventory, Screening version (RHHI-S; Cassarly et al., 2020)
Like its predecessors, the RHHI is composed of statements related to both the social and emotional aspects of having a hearing problem. Examples from the RHHI-S:
- Social: Does a hearing problem cause you difficulty when attending a party?
- Emotional: Does a hearing problem cause you to feel uncomfortable when talking to friends?
In the earlier versions of the HHIE/A, each item was labeled as either being emotional or social (e.g., S-1, E-2, S-3, etc.), so that separate scores could be obtained if desired, although it was uncommon for there to be a significant difference between these items, and nearly always, at least in the clinic, a combined score was used. As you can see on Figure 12, this “E” and “S” labeling has not been carried over to the RHHI.
Timmer et al. (2023) reviewed the importance of considering the social-emotional well-being of our patients. Based on HHIE-S scores, they developed an Auditory Wellness Rating Scale: 0-2 Excellent; 4-6 Good; 8-14 Fair; 16-22 Poor; 24-40 Very Poor. For the various ratings, they provided action-oriented recommendations (see article for details). The authors suggest a five-step approach the help ensure the social-emotional well-being of our patients.
Step 1: Identify the patient’s social-emotional well-being.
Step 2: Include family members in audiologic rehabilitation.
Step 3: Incorporate social-emotional needs and goals in an individualized management plan.
Step 4: Relate the identified hearing needs and goals to recommendations: hearing devices, auditory, communication and social training.
Step 5: Use counseling skills and techniques to explore and monitor the patient’s social-emotional well-being.
Locus of Control
Locus of control is considered to be an important aspect of personality, and the concept has been studied since at least the 1960s (Rotter, 1966). Locus of Control (LOC) refers to an individual's perception about the underlying main causes of events in his or her life. That is, do you believe that your destiny is controlled by yourself, by external forces (e.g., God, powerful others), or things just happen by fate? In the world of health, Health-LOC refers to people's attribution of their own health to personal (Internal) or environmental factors (External). We talk about this briefly in Research QuickTakes Volume 5 (Taylor & Mueller, 2023b).
Based on the results of self-assessment questionnaires, HLOC often is classified into the three different dimensions we mentioned earlier: internality, powerful others, and chance. A patient’s locus of control is related to their self-efficacy. This is the belief that you can produce the result you want in a specific area—how much control you feel like you have over a situation. People with high self-efficacy for a task will most likely have an internal locus of control for success in that task. It’s easy to see why this internal trait might be related to the adoption and use of hearing aids. In general, a more internal LOC is seen as desirable; we know that as people get older, they tend to become internal, and people higher up in organizational structure are more internal. It is a bit more complicated, however, as an internal LOC needs to be matched with competence, self-efficacy, and opportunity. If not, internals may struggle. On the other hand, externals might be more be more relaxed and lead a happier life, as they don’t have the burden of being in control of their life.
As we mentioned, self-efficacy is a desirable trait for someone obtaining hearing healthcare, such as the use of hearing aids. There has been limited research, however, in this area related to LOC. In one study, Cueval et al. (2019), surveyed a total of 114 persons who identified as hard-of-hearing. These authors found that a strong predictor of self-efficacy for this group was an internal locus of control. They suggest that individuals who are hard-of-hearing with both an internal locus of control and high self-efficacy may adjust to live better with their hearing loss (and presumably the use of hearing aids).
HLOC also has been studied to some extent in research that sought to identify factors that are associated with the ability to successfully set up a pair of commercially available self-fitting hearing aids (Convery et al., 2019). The self-fitting procedure required participants to customize the physical fit of the hearing aids, insert the hearing aids into the ear, perform self-directed in-situ audiometry, and adjust the resultant settings according to their preference. Forty-one (68%) of the participants achieved a successful self-fitting. Those who needed help from an HCP were more likely than those who self-fit independently to have an HLOC that was external. We can expect those patients with high self-efficacy and an internal locus of control to be the most successful with self-fitting. While it was not part of the study, we might guess that those with an internal HLOC would be more likely to sample the OTC marketplace.
Empowerment
We have been talking about the importance of self-efficacy, and closely related to this is empowerment. McAllister et al. (2012) address empowerment as it relates to healthcare, and they define it as “an individuals’ capacity to make decisions about their health (behavior) and to have or take control over aspects of their lives that relate to health.” Bennett et al., 2024, point out that empowerment has gained more prominence in healthcare as we have moved to a more biopsychosocial model. Patients can be empowered by their healthcare providers through education, counseling, and patient-centered care, or patients can empower themselves through self-education and help-seeking. The authors add that research shows that empowered patients have a greater understanding of how to navigate the healthcare system, experience improved health outcomes, and are more satisfied with the healthcare they receive. If that sounds familiar, these benefits are very similar to what we discussed earlier in our section on patient-centered care.
While empowerment is not commonly measured during an audiologic visit, that might change, as Bennett et al., 2024 have developed a self-assessment measure that might appeal to busy clinicians—it’s only 5 questions! The scale is shown in Figure 13. While the instructions state that the scale is for hearing aid wearers/users (see Figure 13), we believe that this scale also could be used for anyone with a hearing loss, as none of the 5 questions specifically relate to the use of hearing aids.
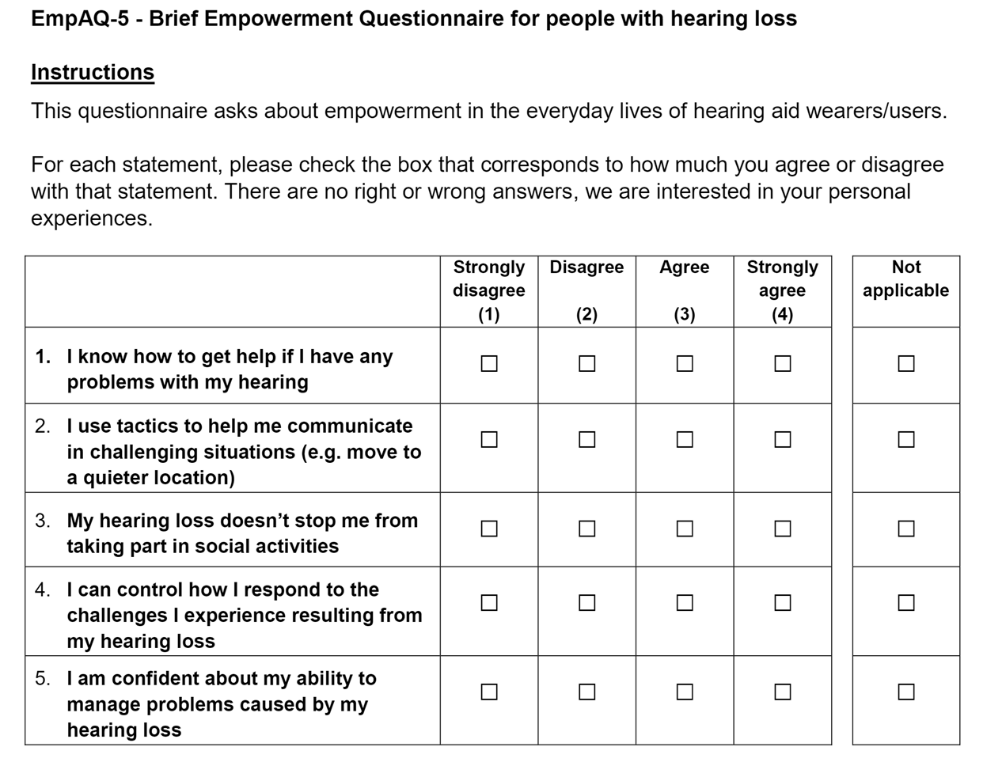
Figure 13. Abbreviated scale of empowerment (adapted from Bennett et al., 2024a).
The authors started with a 33-item empowerment scale, and as you might guess, considerable data analysis was required to obtain a 5-item scale that was valid and reliable—if you’re interested in the process, they explain it nicely in their 16-page Ear and Hearing article (Bennett et al., 2024). We should mention that their work also resulted in a 15-item scale (The EmpAQ-15 and EmpAQ-5 can be freely downloaded from https://osf.io/caj84/). The five question EmpAQ-5 evaluates five separate domains of empowerment: knowledge, skills, participation, control, and self-efficacy. We believe the EmpAQ-5 could be a valuable tool that can be used clinically to gauge just how empowered a patient might (or might not) be on the day of their appointment. This might be particularly useful during an initial appointment or even before the patient has had their hearing tested. Say, for example, your patient self-rates any of these five domains a one or a two on the 5-item scale. This provides valuable insights on exactly what “areas of concern” the HCP should address before hearing aids are fitted, or even months or years post-fitting. Given its brevity, the EmpAQ-5 might be a good questionnaire to administer during annual follow-up appointments in order to pinpoint problems that are getting in the way of successful outcomes.
Self-Esteem
It’s well known that non-audiologic factors, such as personality traits, can have a significant effect on satisfaction with using hearing aids. One of the first studies to examine this extensively, was the work of Robyn Cox et al. (2005). Self-report data were obtained from 230 older adults with bilateral hearing loss. All participants were seeking new hearing aids, and they completed a comprehensive personality questionnaire (NEO-Five-Factor Inventory) as well as questionnaires determining locus of control and preferred coping strategies. Interestingly, these researchers found that individuals who seek amplification are not simply a random sample of the general population, and moreover, also not a random sample of the hard-of-hearing population. Cox et al. (2005) found that hearing aid seekers tended to be more pragmatic and routine-oriented. These individuals also were found to feel relatively more personally powerful in dealing with life's challenges and reported using social support coping strategies less frequently than their peers.
Related to, and in agreement with the findings of Cox et al. (2005) is our previous discussion of empowerment and self-efficacy. We’re now going to add yet another personality trait—self-esteem. While seeming similar to self-efficacy, self-esteem refers to your respect for your own value and worth, whereas self-efficacy refers to how you feel about your ability to succeed in different situations. A person could have low self-esteem, but yet have high self-efficacy for some aspect of their life. In general, high self-esteem is associated with good coping skills and persistence—two factors that would seem to relate to the use of hearing aids, and indeed, this has been studied.
In a recent publication, Ceyhan and Ture (2023) conducted testing with 86 hearing aids users, which included a measure of self-esteem, and hearing aid satisfaction was assessed using the IOI-HA outcome measure (see QuickTakes Volume 6 (Part 2) for review of this scale; Taylor & Mueller, 2023c). Rosenberg’s self-esteem scale was used (see Figure 14). This is a 10-item scale; 4-point Likert, containing 5 positive and 5 negative items. Scores on the sale range from 0-30. Typically, scores between 15 and 25 are within normal range; scores below 15 suggest low self-esteem. Interestingly, given that scores greater than 25 are not in the “normal” range, this suggests that having “too much self-esteem” isn’t good either. An alternative method of interpreting the findings: 21-30 points: High self-esteem; 15-20 points: Moderate self-esteem; and 0-14 points: Low self-esteem.
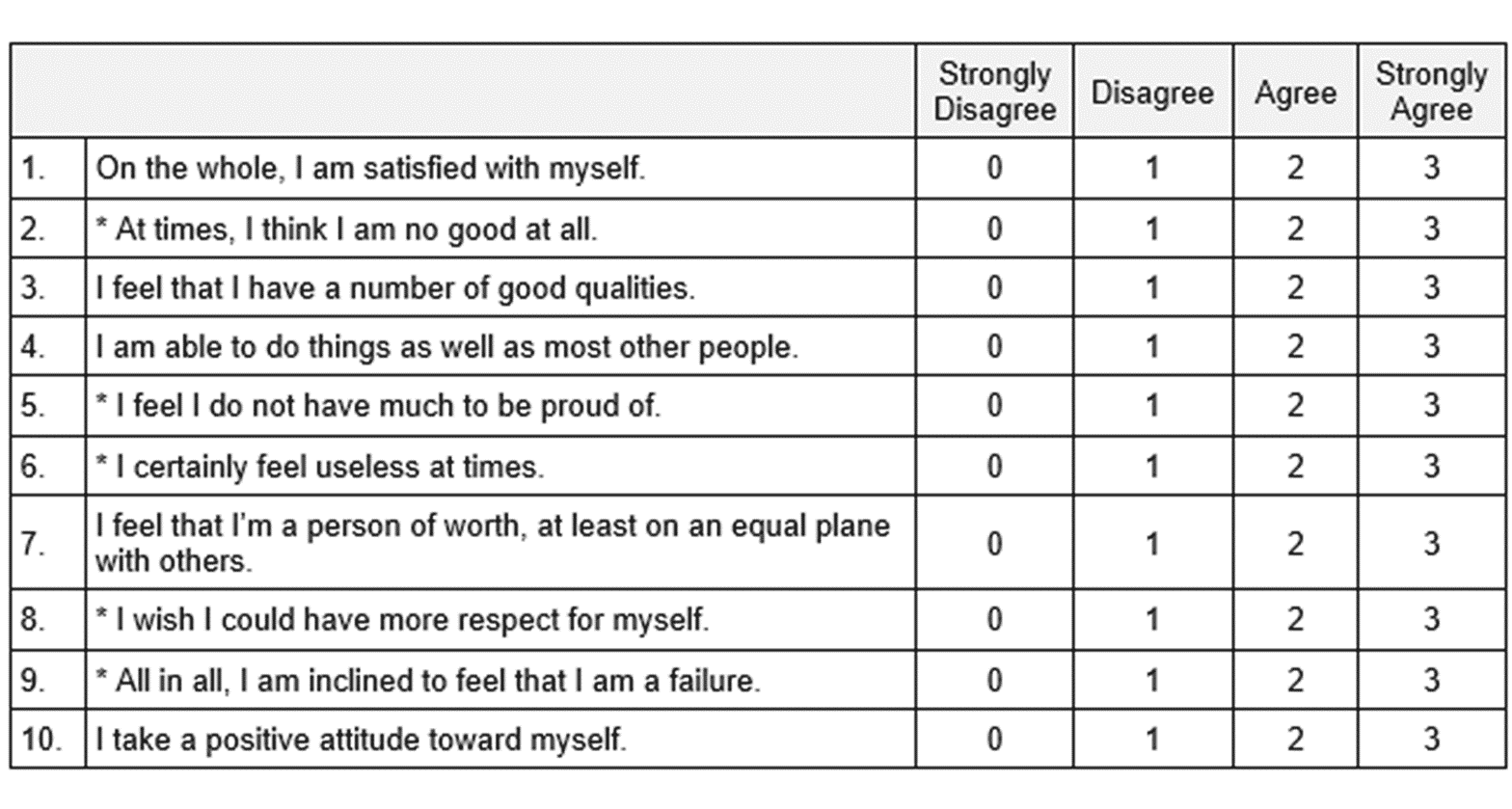
Figure 14. The Rosenberg Self-Esteem Scale (adapted from Rosenberg, 1965).
There was a significant positive relationship between the level of satisfaction with hearing aids (IOI-HA score) and the Rosenberg Self-Esteem Scale Score (p<.001); self-esteem explained 26.2% of the variation in satisfaction. The authors conclude that the self-esteem of hearing aid users is a prominent factor in satisfaction with hearing aids, and important for enriching audiologic rehabilitation (Ceyhan & Ture, 2023).
Listening Fatigue
You might recall that a decade or so ago, there was a burst of research that studied listening effort. How does hearing loss impact listening effort? What listening situations required the most effort? Could the effort be reduced through the use of hearing aids? Are specific products better than others for reducing listening effort? Could listening effort for those who are hard-of-hearing be no worse than those with normal hearing if the hard-of-hearing individuals are wearing the right hearing aids? The answer to that last question is yes—see the work of Littman et al. (2017).
The assessment of listening effort typically has been reserved for research studies. What has become more common to assess in the clinic is listening fatigue—something which of course, is often related to listening effort. At one time or another, most all of us have experienced fatigue after extended listening—for this very reason, many people with normal hearing use closed captioning when watching a movie that has talkers who are difficult to understand. It's simply when we become mentally and/or emotionally drained from working hard to hear and understand; feel like we need a rest, and simply give our brain a break. If a hearing loss is present, the onset of fatigue will be more rapid. When listening-related fatigue is recurrent and/or severe it can have significant negative effects on quality of life in people with hearing loss (Hornsby et al., 2023).
In recent years, there has been considerable study of listening fatigue conducted at Vanderbilt University, originally focused on children, but now also including adults (Hornsby 2013, Hornsby & Kipp 2016, Hornsby et al., 2022). Prior to their work, there were no validated scales specifically developed to assess listening-related fatigue. There currently are three pediatric versions of the Vanderbilt Fatigue Scales (the VFS-Peds)—a child self-report version (VFS-C), a parent proxy-report version (VFS-P), and a teacher proxy-report version (VFS-T). A 40-item version of the VFS also has been developed for the adult population, which has been shown to have good test reliability and construct validity (Hornsby et al., 2021). While effective, a 40-item self-assessment scale might be more than a busy clinician would like to deal with, and the good news is that there now is a 10-item version of this scale available (Hornsby et al., 2023).
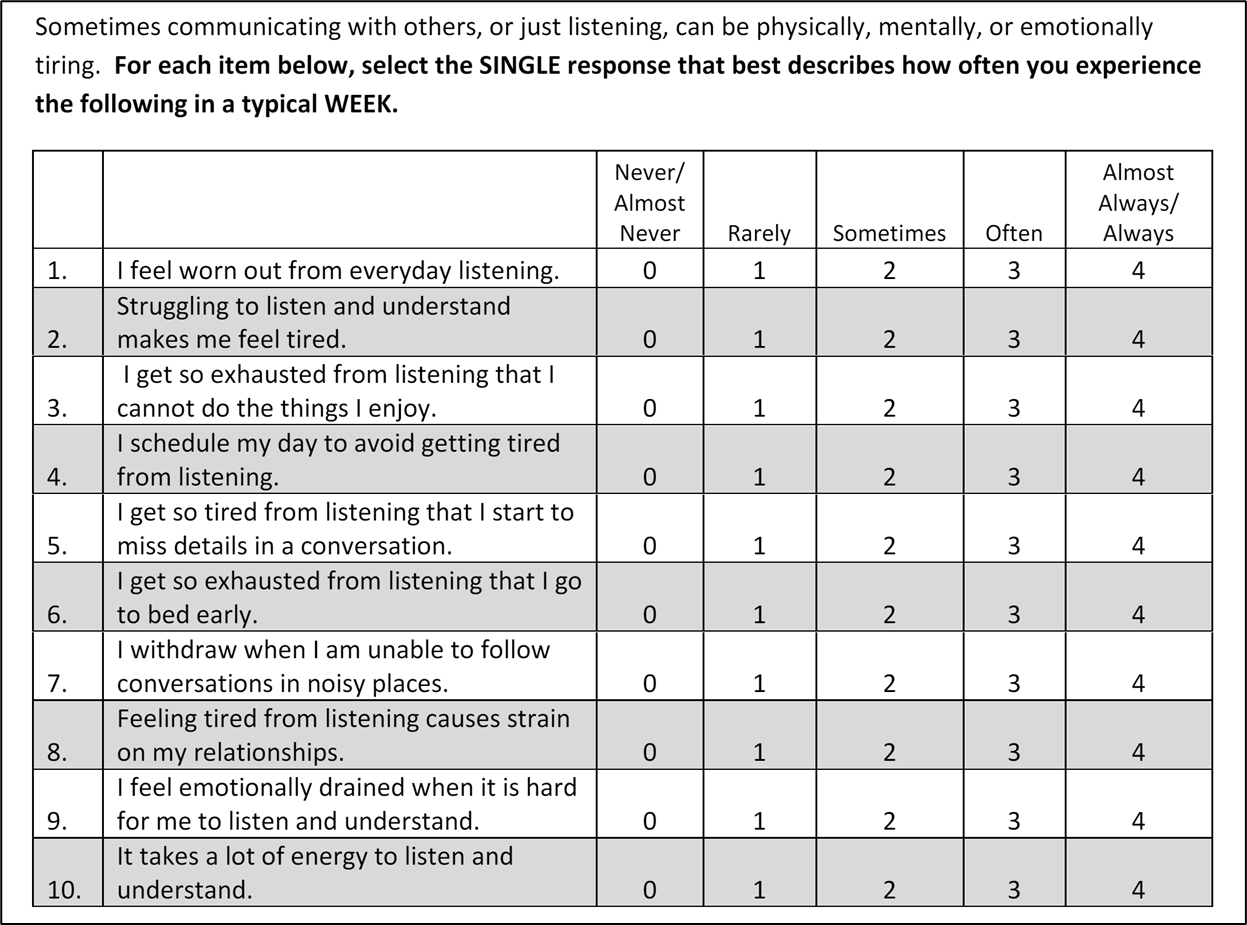
Figure 15. The Vanderbilt 10-item Fatigue Scale for adults (VFS-A-10). (Hornsby et al., 2023).
The VFS-A-10 is simple and easy to use. The patient is instructed to respond to the frequency of listening-related fatigue problems being experienced in a typical week. Most adults can complete the scale on their own in 2 to 3 min. It is scored by simply summing the responses for the 10 items—a maximum score is 40 (excessive fatigue). Summed scores ≤10 means the respondent experiences problems with listening-related fatigue, but the problems are relatively rare. A score at or near 0, suggests that they never or almost never occurred. In contrast, a score ≥30 means this individual is experiencing listening-related fatigue issues often or almost always (Hornsby et al., 2023).
The data of Hornsby et al. (2023) found that adults who reported no hearing loss had VFS-A-10 scores ≤26; the majority (~53%) had VFS-A-10 scores ≤5, and ~88% had scores ≤15. In contrast, for respondents with self-reported hearing loss, ~25% had scores >26, and ~13% had scores ≥30, suggesting their problems were occurring often to always.
The authors suggest that this tool will be useful for identifying those individuals most affected by listening-related fatigue and for assessing the effectiveness of any interventions designed to reduce their fatigue—research has shown that well-fitted hearing aids can reduce listening-related fatigue in new hearing aid users (Holman et al., 2021). They further suggest that the VFS-A-10 could also be useful as a screening instrument for other populations who struggle with listening and understanding: individuals with auditory processing deficits, and/or individuals with hidden hearing loss.
Recently, Taghvaei and Taylor (2024), collected VFS-A-10 scores on 42 patients pre- and post-hearing aid fitting. The mean score on the VFS-A-10 in the unaided condition was 13, with seven of the patients having an unaided score of 25 or higher. Approximately one month after their fittings, the VFS-A-10 was re-administered. The mean aided score was six. Interestingly, all seven patients with an unaided score of <25 had aided scores of 10 or less, showing substantial improvement on the VFS-A-10 with hearing aid use.
Patient instructions and Counseling
In this section of Volume 8, we’ve talked about several “patient factors” that often are important to consider on the day of (or days before) the fitting. Things like perception of problem, social and emotional factors, locus of control, empowerment, self-efficacy, self-esteem, and fatigue. We’re now going to shift gears a little and talk about how the instructions and counseling provided by the HCP can impact hearing aid adoption, use, benefit and satisfaction. Interesting research on this topic was just recently published (e.g., Lelic et al., 2023), but this of course is not a new topic of research interest, with publications going back at least 4 decades. So, before we get to today’s studies, we’ll go back to the 1980s.
While bilateral fittings are quite common today (e.g., 85-90%), they were only fitted at a 33% rate in 1985, which by today’s standards, seems remarkably low. It is difficult to sort out if this was due to patient’s reluctance to use two devices, or because HCPs did not strongly recommend the use of two instruments (see review by Mueller, 1986). Research looking into this was conducted by Mueller and Reeder, 1987 (cited in McCarthy et al., 1990). At a major U.S. Army Medical Center, where hearing aids were provided free-of-charge to retired military individuals, over a three-month period, consecutive patients who audiometrically were candidates, were fitted bilaterally with ITE/ITC products, all from the same manufacturer. Hearing aids were programmed to a best-fit to NAL-R prescriptive targets, verified with probe-microphone measures.
Prior to the fitting of hearing aids, all participants completed a short questionnaire, where one of the questions asked if they desired to be fitted with one or two hearing aids—they were all fitted with two regardless of their answer to this question. The hearing aids were fitted by three different clinical (civilian) audiologists, and then, following the fitting and basic orientation, all participants received 10-minutes of final guidance from a different audiologist, a senior ranking active-duty officer. The participants were randomly assigned to receive one of two different types of counseling:
- Approach #1: “Doctor-Centered (DC).” The patients were informed of the research showing that bilateral use was best for them, and all the benefits were emphasized. They further were informed that they would be foolish not to embrace using two hearing aids.
- Approach #2: “Patient-Centered (PC).” The patients were told that some people preferred using two hearing aids, others preferred only using one. It was up to them to try it out and see what they liked.
The use of the different counseling then separated the participants into four groups:
- Group 1: Preferred bilateral; DC counseling.
- Group 2: Preferred bilateral; PC counseling.
- Group 3: Preferred unilateral; DC counseling.
- Group 4: Preferred unilateral; PC counseling.
Outcome measures for use, benefit and satisfaction were obtained from 100 participants 8-12 months following the fitting (mean age 69; mean HF-PTA 45 dB), fairly evenly divided among the four groups; 46 had originally chosen two hearing aids, 54 initially chose to only be fitted with one hearing aid. The results of use and benefit are shown in Figure 16 (Mueller & Reeder, 1987).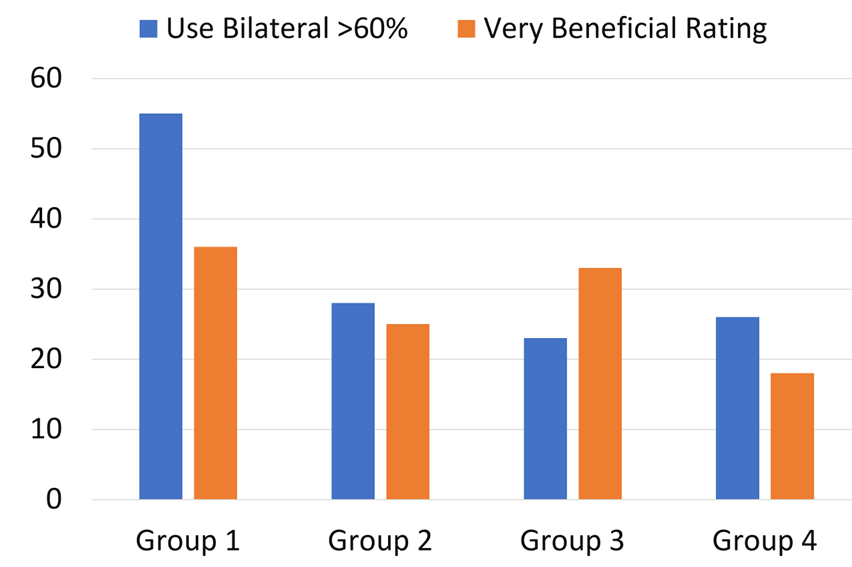
Figure 16. Percent of respondents who use bilateral hearing aids >60%/average day and those reporting the use of hearing aids as “very beneficial.” Group 1: Preferred bilateral; DC counseling. Group 2: Preferred bilateral; PC counseling. Group 3: Preferred unilateral; DC counseling. Group 4: Preferred unilateral; PC counseling (adapted from Mueller & Reeder, 1987).
The most notable finding displayed in Figure 16 is the large difference in bilateral use between Group 1 and Group 2. Recall that the participants in both groups originally preferred the use of bilateral amplification. They were all fitted using the same product, to the same fitting targets. The mean age of the two groups only differed by 1 year (69 vs. 68), and the mean HF-PTA differed by 1 dB (47 vs. 46). The only apparent difference was that the group with the significantly highest use rate, Group 1, had the DC counseling. Interestingly, the benefit reported by Group 3 participants (those desiring a unilateral fitting, but DC counseling) was nearly as good as Group 1, and considerably better than Group 4.
As you might recall, we talked a little about the impact of patient counseling back in Research QuickTakes Volume 2 (Taylor & Mueller, 2023d). A couple of articles of interest:
- From Bentler et al.(2003): For one month, participants wore hearing aids labeled “state-of-the-art digital;” the other month they wore hearing aids labeled “conventional,” although in reality they were wearing the same hearing aids. When the hearing aids were labeled “digital,” the self-report subscales of the APHAB were rated significantly higher. When asked to state a preference for continued use, 33 (83%) of the 40 participants expressed a preference for the fitting that had been labeled “digital.”
- From Dawes et al. (2013): Participants compared two acoustically identical devices, except one was described as "new" and the other as "conventional.” When using the “new” hearing aids, participants had significantly better mean speech-in-noise performance (70.9% versus 66.8%) and sound quality ratings (8.1 versus 7.4); 75% expressed an overall preference for the "new" hearing aids.
This then takes us back to the more recent publications we mentioned earlier. The work of Rakita et al. (2021) was geared toward investigating the effects of communicating narratives designed to foster positive, negative, or neutral expectations about hearing aids on short-term patient outcomes. They also examined whether the wearer outcomes could be predicted by the patient’s personality traits.
The participants had three separate research appointments, each exposing them to a different narrative: condition: positive, negative, or neutral. At each appointment, unknown to the participants, they were fitted with the same pair of hearing aids. Each time they provided their feedback about the hearing aids, including how long they thought it would take to get used to hearing aid use. Speech-in-noise testing (QuickSIN) also was conducted.
Their results revealed that the narrative condition affected how much time participants perceived they would need to get used to the hearing aids: as expected, they would need less time when the positive narrative condition was employed. There were some significant effects related to personality traits. Participants who scored more highly on agreeableness were more likely to change their subjective assessment. Participants who scored less highly on neuroticism were more likely to perceive that they would need less time to get used to the hearing aids in the positive narrative condition.
As we’ve already mentioned, there has been some previous work showing that descriptions of hearing aids, or potential hearing aid performance can actually alter the participants’ word recognition score when using the instruments (Dawes et al., 2013). This was also true in this study, except to a larger extent than has been shown before. The difference in the mean QuickSIN score was nearly 3 dB better when a positive vs. negative narrative was used; the range of scores also was much larger for the negative narrative. To put this into a clinical perspective, when two QuickSIN lists are used (60 key words), the critical difference (.05) between two scores is 2.7 dB. Rakita et al. (2021) suggest the possible explanation for why a positive narrative resulted in better QuickSIN performance was that the specific mention of the fact that the hearing aids had features to help with speech understanding in background noise, might have encouraged more guessing by the participants.
Curiously, the authors presented the QuickSIN at a very high level: ~80-85 dB SPL (the level used for unaided testing)! Normally, for aided testing, we are interested in average-level speech, e.g., 60-62 dB SPL. A speech input of 80-85 dB SPL likely pushed the products to their MPO. This probably impacted the overall QuickSIN findings, but perhaps not the narrative-driven relative differences that were of interest.
Positive Listening Focus
We have just reviewed research showing that providing positive narratives about hearing aids use can significantly improve outcomes. A somewhat related approach is to have the patient repeatedly focus on specific hearing aid experiences in their everyday lives that are positive, and report when they experience these events. This was the primary focus of recent research by Lelic et al. (2023). The authors point out, that without an emphasis on positive experiences, these benefits can be over-shadowed by difficult experiences, which can negatively influence a person’s overall hearing aid satisfaction. In some cases, the negative event takes on a much greater subjective significance than a positive event of equal objective magnitude.
To examine the effects of focusing on positive experiences using hearing aids, Lelic et al. (2023) divided 21 participants into two groups: a control group and a positive focus group. All participants were fitted bilaterally with the same model premier hearing aids, using the proprietary algorithm of that manufacturer. The participants then experienced a three-week filed trial. During the field trial, the positive focus group actively reported, via a smartphone app, each time they had a positive listening experience. The average number of reports/participant was ~1.5-2.5/day, slightly higher for the last week of the trial.
At the conclusion of the field trial, several outcome measures were administered, including the IOI-HA and the COSI (see Research QuickTakes Volume 6.2 for review of these measures; Taylor & Mueller, 2023c). Figure 17 shows the findings for the COSI (median rating; 25th and 75th percentiles). 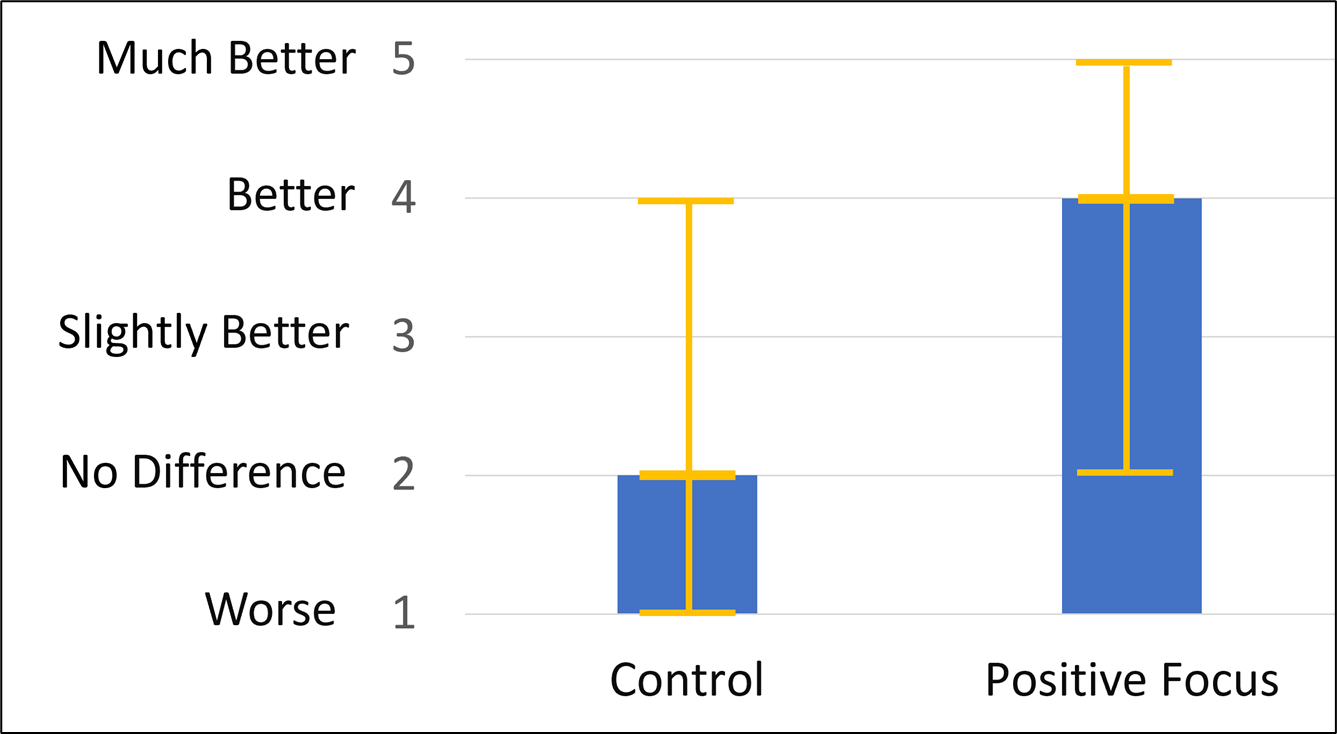
Figure 17. Aided results for the COSI. Shown are median values, with box plots representing 25th and 75th percentiles. (Adapted from Lelic et al., 2023).
Observe that for the control group, the median rating was #2 “No Difference,” whereas for the positive focus group, the COSI median rating was #4 “Better.”—a significant difference. Similar significant findings were present for the IOI-HA. For the control group, the median total score was 21 (25th-18, 75th-26), whereas for the positive focus group, the median total score was 28 (25th-27; 75th-30).
The authors add that the positive effects of simply reporting positive listening experiences was further evidenced at the exit interviews, when the participants were asked about their experiences during the trial. Not a single person in the control group mentioned anything about listening experiences with the hearing aids. On the other hand, the majority of the participants in the positive focus group talked about their pleasant experiences. In a companion study using the same control group versus positive focus group design, but comprised of a different group of wearers, Lelic (2024) found that the positive focus group maintained significantly better outcomes on the COSI compared to the control group six months after the fitting – even after the reporting and reflecting of positive experiences by the patient ended with the three-week trial.
What we have reported here is a well-controlled study, however, it would not be difficult to apply these findings to general clinical practice. Given the ease of tele-audiology, having a patient report positive experiences in an organized way would be quite easy to implement. One could even go “old-school” and use a paper-and-pencil notebook, which then could be reviewed on follow-up visits. This would seem to be very valuable for a new hearing aid user. Research certainly suggests that this approach can lead to improved satisfaction, which is most cases, directly relates to hearing aid benefit.
V8.5: After the Appointment: Promoting Consistent Hearing Aid Use
In this final section of Volume 8, we’re going to talk about a few issues to consider after the day of the hearing aid fitting. While it’s tempting to think that after appropriate pre-fitting testing, a good fit to prescriptive targets, and good counseling, our patients will become regular users of hearing aids. Maybe, but not as regular as we’d like to think. We’ll talk about a few things that we can do to help facilitate the process.
Examining Results of Systematic Review
Before we get to some specific post-fitting issues, it’s useful to review the findings of a recent systematic review (Oosthuizen et al., 2022). The authors conducted a systematic search of three electronic databases, yielding 443 published studies. After evaluation for inclusion criteria, 25 studies were used for the analysis. A narrative synthesis was conducted, and studies were grouped into three main domains related to the users’ experiences: hearing aid adoption and fitting (n = 3), hearing aid use (n = 20), and hearing aid sub-optimal use (n = 25). Hearing aid owners mainly reported on how their attitude towards hearing aids affected experiences during the fitting stage. Following the narrative synthesis, the results of the studies were classified according to the different domains. We’ve included a sample of the findings of Oosthuizen et al., 2022 here.
Experiences Related to Hearing Aid Adoption and Fitting. Three studies reported on owners’ experiences during the adoption and fitting, and three concepts were synthesized:
- Hearing aid owners report positive experiences when audiologic service delivery is perceived as at least “adequate.”
- When owners describe clinical service delivery as “inadequate,” and information counseling as limited, experiences are affected negatively.
- Owners’ self-perceived hearing loss, specifically a lack of self-awareness of hearing loss and the consequent effects of hearing loss is a barrier to adoption and fitting.
Experiences Related to Hearing Aid Use - Getting Used to Hearing Aids
Four studies explored HA owners’ experiences during the early stages of hearing aid use. Seven concepts were synthesized across these studies to summarize the key factors:
- Acclimatization was the most often reported in owners’ experiences of getting used to (note: we have a separate section on acclimatization later in this paper).
- Issues with smartphone connections also were commonly reported.
- Owners describe information counseling, advice, and training, and managing their expectations as prerequisites for positive early experiences.
- The concepts of acceptance of hearing loss, consistent use, patient attitude. Support from significant others (i.e., family and friends).
- Good relationship with the hearing care professional.
Experiences Related to Hearing Aid Use - Benefits Associated with Use
These concepts were synthesized across results from 19 studies. Improved psychosocial factors were the most frequently described, such as improved participation in social and group settings. Also reported was improved confidence in communicative abilities, enhanced emotional connectedness, and managing hearing-aid related stigma (more commonly reported by owners of smart-phone operated hearing aids).
Experiences Related to Hearing Aid Use - Facilitators of Use
Reports from 15 studies included descriptions of facilitators' use from the owners’ perspectives. The concept of social/environmental influences was reported most consistently. Owners of smartphone-connected products specifically reported on how these hearing aids helped to reduce individual and societal stigma. Other factors included acceptance of hearing loss, support from significant others, cosmetically appealing and quality of product. Audiologic service delivery was also often reported.
Experiences Related to Hearing Aid Sub-optimal Use - Device-related Challenges
Twenty-two studies contained descriptions by owners of device-related challenges. Themes and sub-themes from these studies were synthesized into ten concepts. The two most prevalent device-related difficulties, as you might expect, were handling and continuous care; practical use challenges, including maintenance and repairs, and understanding speech in background noise. There also were numerous reports of poor, unclear, or unpleasant sound quality, acoustic feedback, problems with listening to music or on the telephone, and physical fit.
Experiences Related to HA Sub-optimal Use: Non-device-related Challenges
Twenty studies with 15 synthesized concepts associated with non-device-related challenges (i.e., challenges related to clinical service delivery and/or the owners themselves). The issue of the stigma was the most consistently reported challenge. Reports reflecting a negative attitude and/or negative emotional state or hesitation towards hearing aid use were associated with avoidance of or reduced use, as was a lack of self-awareness of their hearing loss.
We have presented a brief review of the extensive findings of the Oosthuizen et al., 2022, systematic review—check out their article for many more details. If you’ve been fitting hearing aids for a while, there probably wasn’t too much in our review that surprised you. It is helpful, however, to have this information laid out in a comprehensive manner, so that we can systematically consider all these factors in our counseling.
Auditory Acclimatization
As we’ve just reviewed from the work of Oosthuizen et al. (2022), research studies have found that the #1 issue regarding getting used to hearing aids is understanding the course of acclimatization. For this reason, we’ll spend some extra time on this topic. Clearly, this is something that we need to emphasize in our counseling—the patient must realize that auditory acclimatization will most likely happen, at least to some degree, but that it takes time. Our role is pretty simple: provide appropriate gain, especially for the high frequencies and for soft inputs, which by the way, are two things that patients, particularly new users, are not fond of. In counseling, therefore, our job is to help the patient understand the following:
“You have to hear what you don’t want to hear to know what you don’t want to hear.”
Auditory acclimatization often is referred to as “perceptual learning.” That is, the brain must adapt to the new sounds, that in many cases, haven’t been audible for 10 or more years. Some of the new sounds are the result of the amplification of the high frequencies of speech. Many of these “new sounds,” however, are simply background noises of life in general—heating and air conditioning, refrigerator motor, overall ambient noise, etc. Even the littlest things come to the forefront: “I could hear myself walk on carpet.” “I could hear the pen move when I was writing on paper.” “I could hear myself breathe.” All these new sounds are novel, and therefore impact conscious attention, and as a result, are annoying and often act as maskers of speech understanding.
A Bit of History (Directly Related to our Topic Here)
Older readers will recall that it was back in 1989 when Mead Killion introduced the K-AMP. This was the first widespread application of signal processing that used an input compression circuit with a very low kneepoint (soon known as wide dynamic range compression, or WDRC). Prior to this new technology, nearly all hearing aids were linear for the speech range. That meant that if the user adjusted the hearing aid for appropriate loudness for average speech—e.g., 15 dB gain—he also had 15 dB of gain for soft speech. With WDRC, however, 15 dB of gain for average would result in ~25-30 dB of gain for soft inputs. Patients were finally hearing soft sounds as they should, but many were not happy about it, and audiologists had never experienced this counseling dilemma before—the easy fix was to turn down gain, but only for soft, which was not easy to do with the K-Amp product. In an effort to help audiologists with the counseling, Killion came up with the acronym ABONSO; Automatic Brain-Operated Noise-Suppressor Option. His point was: just give the brain a chance, and over time, it will help reduce what is now unwanted noise—the same as our point earlier. A few years later, Mead teamed up with Stuart Gatehouse to publish an article on acclimatization, with an associated acronym: HABRAT—Hearing Aid Brain Rewiring Accommodation Time (Gatehouse & Killion, 1993). The ABONSO and HABRAT discussion with each patient is as important today as it was 30 years ago.
Research Evidence
Skeptics might question if there really is evidence that HABRAT exists? We can look at this from both a loudness accommodation aspect, or, the potential impact on speech understanding. We’ll start with the following question: if patients are fitted to a validated prescriptive method that has been designed to equalize or normalize loudness, will users acclimatize to these renewed loudness sensations? Using the Profile of Aided Loudness (PAL; Mueller & Palmer, 1988), studies have shown findings that have clinical implications (Mueller & Powers, 2001; also, for review, see Taylor & Mueller, 2023d, Research QuickTakes Volume 2). In one of these studies, related to our discussion here, new hearing aids were fitted to both new and experienced users according to the NAL prescriptive method. Of particular interest was their PAL ratings for soft inputs; normative data, based on individuals with normal hearing, are PAL ratings of #2. They were followed for eight weeks, with PAL ratings obtained at Day 1, Week 1, Week 4, and Week 8 (See Figure 18). Note that the experienced group rated soft sounds appropriately (#2 on a 7-point scale) after only one week of hearing aid use. The new users, however, were still rating soft sounds #4 after a month of hearing aid use but did approach the desired #2 rating at the end of the 8-week trial. Clearly, for soft sounds, at least for this group, the adjustment period is gradual, but importantly, does happen.
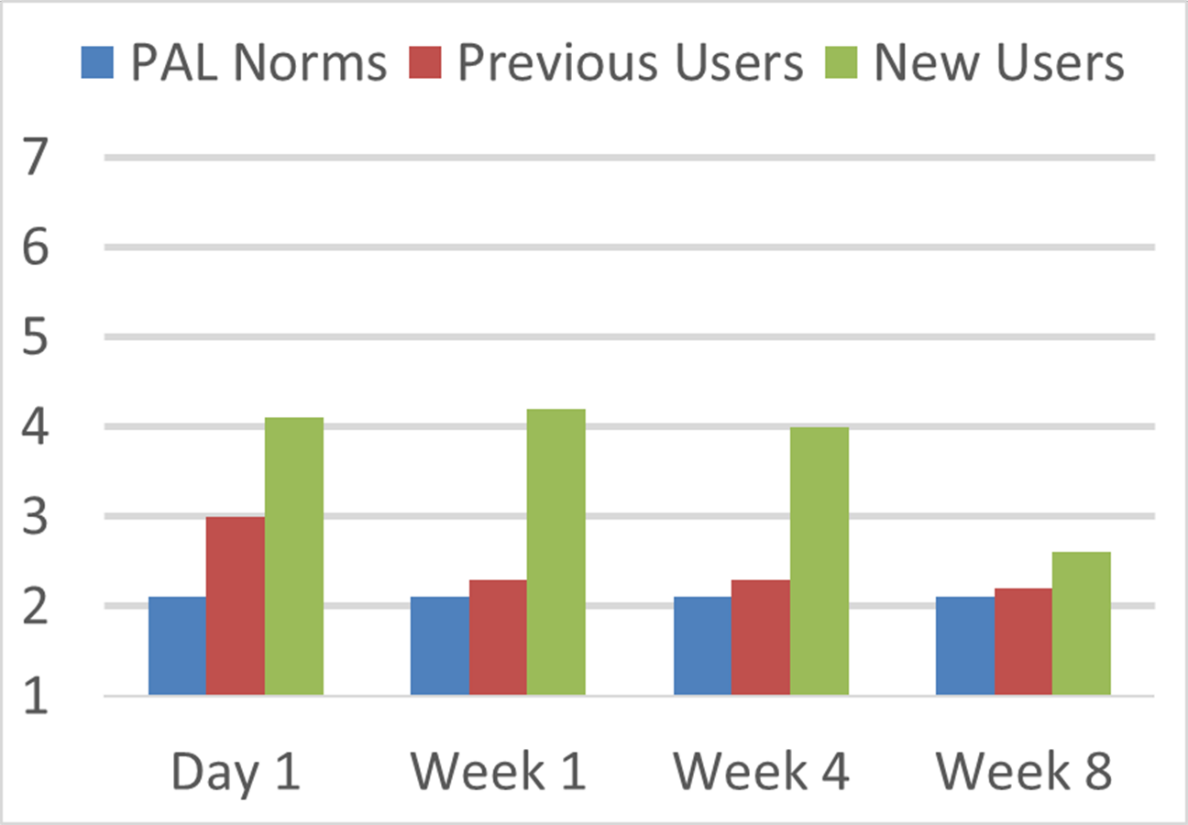
Figure 18. Shown for reference are the mean PAL ratings (blue bars) for environmental sounds judged to be soft (#2) by normal hearing young adults. Ratings displayed for both new users and experienced users at Day 1, 1 Week, 4 Weeks and 8 Weeks following the bilateral fitting of new hearing aids.
The fact that, at least based on this research, soft environmental sounds will eventually be judged as soft, doesn’t necessarily mean that they still are not bothersome. One method to examine this is to conduct speech-in-noise testing while controlling for acclimatization. Research addressing this was conducted by Dawes and Munro (2017). New adult hearing aid users (n = 35) completed a test of aided speech recognition in noise (SIN) and a test of the auditory distraction caused amplified background sounds. Testing was conducted on the day of fitting and one, seven, 14 and 30 days following the fitting. A control group of experienced hearing aid users (n = 20) completed the tests over a similar time frame.
Their findings were that a subset of new users with moderate hearing loss who wore their hearing aids at least 6 hours/day had significantly improved SIN scores (~3-dB SNR) compared to the control group; the improvements in SIN were associated with more consistent hearing aid use. Improvements in SIN also were associated with self-report of background sound being less distracting and greater self-reported hearing aid benefit. Important for clinicians to remember, is that this SNR improvement did not occur for the new users who did not use their hearing aids regularly.
Supporting Electrophysiologic Evidence
It has long been suggested that there is brain plasticity associated with acclimatization. In fact, we have an interesting anecdote from the 1940s involving Harvey Fletcher, renowned as the “Father of Stereophonic Sound,” and for many years, Director of Research at Bell Laboratories (See Figure 19; from Mueller et al., 2017).
Figure 19. Harvey Fletcher story from the 1940s (adapted from Mueller et al., 2017).
Today, we don’t have to rely on anecdotes, as considerable electrophysiologic information on this topic is available. One example is the work of Glick and Sharma (2020). These authors examined changes in a group of 28 older adults with early-stage, mild-moderate age-related hearing loss—all participants were fitted bilaterally to NAL-NL2 targets—none of the participants had worn hearing aids prior to the study. Following the fitting, the participants used the hearing aids in their everyday life for six months. A minimum use of 5 hours/day was required, verified with data logging. At the time of the fitting, and at the end of the six-month field trial, cortical visual evoked potentials (CVEPs) were conducted. A cognitive test battery also was administered pre-and post-hearing aid use.
Prior to the use of hearing aids, the group showed the expected occipital lobe brain activation for the CVEPs, but also, there was additional activation of the auditory regions of the brain, suggestive of cross-modal re-organization. Moreover, participants showed recruitment of the frontal cortex during this task, which is believed to reflect increased effort or cognitive load, and in fact the authors found that this cross-modal reorganization was associated with poorer cognitive functioning at baseline testing (See Figure 20, left panel; Sharma, 2021).
Of the 28 participants initially enrolled, 21 met minimum daily use requirements and returned for 6-month follow-up testing. The CVEPs were significantly different than the baseline obtained weeks earlier. There was a reversal in cross-modal reorganization, with a reduction in temporal and frontal cortex activity, and restoration of more typical visual processing patterns in response to visual activation (Figure 20 right panel; Sharma 2021). There also were significant improvements in the domains of global cognitive function, processing speed, executive function, and visual working memory.
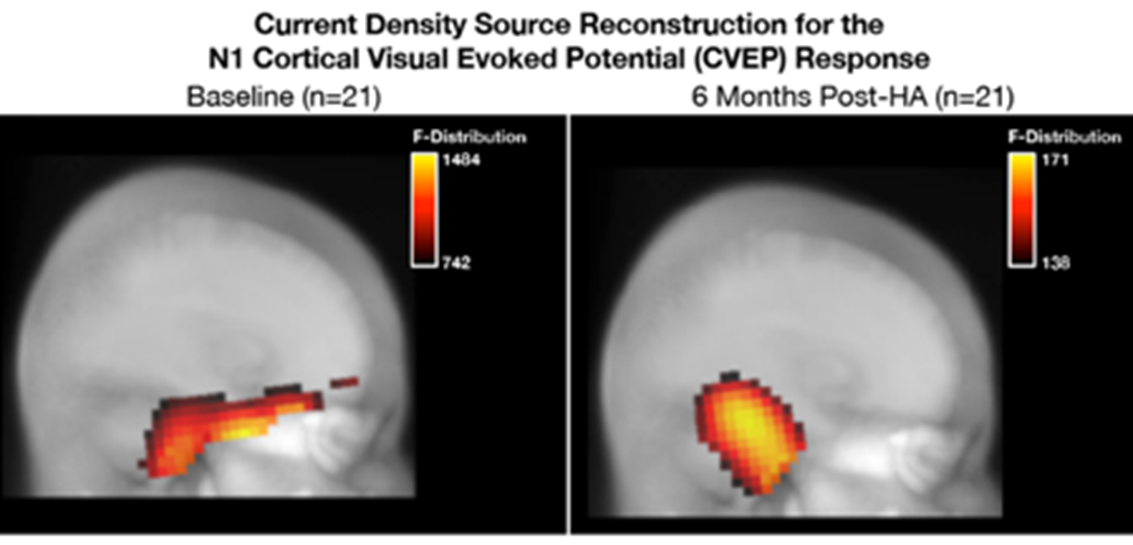
Figure 20. Density source reconstruction for the N1 cortical visual evoked potential (CVEP) response at baseline and 6 months post hearing aid use. Left Panel: Cross-modal re-organization, as evidenced by recruitment of temporal cortex and frontal cortex in addition to the occipital regions typically associated with visual motion processing. Right Panel: At 6-month post-treatment with amplification, there is a reduction in temporal and frontal cortex activity and restoration of more typical visual processing patterns (Adapted from Sharma, 2021).
In several of our previous Research QuickTakes, we have stressed the importance of ensuring that patients are correctly fitted to prescriptive targets using probe-microphone measures. This primarily is because the “first-fit” from manufacturers woefully underfits, especially in the higher frequencies. Unfortunately, there are many HCPs who do not believe that this verification is necessary. Consider the following quote from Sharma (2021): “. . . neuroimaging evidence from long-term hearing aid users who were “underfit” showed persistent cross-modal re-organization even after extended periods of hearing aid use. This suggests that correctly fitted hearing aids are important for providing the necessary gain to the auditory cortex to reverse cross-modal changes.” Yes, folks, you do have the patient’s brain in your hands!
Patient’s Mental Health
Speaking of the patient’s brain, one area that often is overlooked by HCPs, is the general mental health of our patients—it’s pretty easy to just focus on the ears, yet the overall mental health can be a significant component of hearing aid adoption. We know from several studies that adults with acquired hearing loss have greater social isolation and loneliness than their peers—factors that certainly could contribute to mental health issues. As reviewed by Bennett et al. (2024b) there are data showing that mental health is not addressed effectively by general practitioners—something that is often referred to as the “rule of diminishing halves.” Half the patients presenting with symptoms are recognized; half of those recognized are treated; and half of those treated are effectively treated—if our math is correct, that leaves us with 12.5%! All the more reason why this area should not be ignored by HCPs.
A structure that has been used over the years to evaluate the implementation of health behavior change is the RE-AIM, an acronym for Effectiveness, Adoption, Implementation, and Maintenance (Glasgow et al., 1999; Bennett et al., 2024):
- Reach— Did the targeted population receive the intervention?
- Effectiveness—Was the intervention effective?
- Adoption—Was there support to deliver my intervention?
- Implementation—Was the intervention delivered properly?
- Maintenance—Has the intervention become a part of routine organizational practice?
Related to the RE-AIM is the AIMER: Ask, Inform, Manage, Encourage, and Refer, something we discussed in an earlier section. The AIMER program is a behavior change intervention that is specifically designed to increase the frequency with which HCPs ask about and provide information regarding mental wellbeing within adult audiology services (Bennett et al., 2024b). Recently, research was conducted using the AMER program to determine whether the intervention achieved the desired changes in HCP behaviors. Importantly, the overall goal of the AIMER program is to improve mental well-being outcomes for adults with hearing loss; this initial study, however, evaluated clinician outcomes and not patient outcomes.
Figure 21. Components of the AIMER (Adapted from the Ear Science Institute of Australia, 2023).
Participants received training over a ~1.5 year period. Data were collected that included both quantitative and qualitative measures: observation reports, staff surveys, clinical diaries, clinical file audits, and interviews. Comparison between pre- and post-implementation data showed that the AIMER intervention successfully increased:
- The HCP skills and confidence for discussing mental wellbeing.
- How often HCPs asked about mental wellbeing during the audiology patient visit.
- How often HCPs provided personalized information and support regarding mental wellbeing within and audiology appointment.
- How often HCPs used mental wellbeing terms within clinical case notes and general practitioner reports.
Bennett et al. (2024b) report the key findings of this study:
- The AIMER program was effective at changing clinician’s behaviors related to provision of mental wellbeing support within routine audiologic appointments.
- Implementation of the AIMER program in a real-world setting was feasible. HCPs enjoyed receiving AIMER training and felt that it benefitted them and their patients.
- The RE-AIM provided a comprehensive framework for the planning and evaluation of the implementation effort.
Using AIMER in the Clinic. We sometimes forget that hearing loss impacts people in different ways, and those with hearing loss might cope with the condition in their own unique manner. Unfortunately, routine audiologic care (testing hearing and fitting hearing aids) doesn’t always address the well-being aspects of hearing loss. AIMER provides a framework for how we can engage our patients to talk about their well-being as it relates to hearing loss and hearing aid use. A good example of how Bennett’s AIMER approach can be applied clinically relates to social well-being.
Most people have a desire to socialize, minimally once or twice a month, and that ability is often compromised by hearing loss. When we fit someone with hearing aids, many patients don’t automatically regain the ability to socialize. We can’t simply assume that wearing hearing aids will improve this ability. The role of the HCP is to better understand what obstacles might be getting in the way of socializing, even after hearing aids have been fitted. That is where an approach like AIMER can be quite helpful. Applying the AIMER to a patient who has been wearing hearing aids for a few months, but has yet to regain their ability to socialize in a way that is acceptable to her might look something like this:
- Ask the patient about her willingness and ability to socialize in the places that have been targeted on the COSI.
- Inform the patient: Discuss in general terms how hearing loss affects her ability to socialize and hearing aids, when worn properly, can improve this ability.
- Manage the process: Provide personalized examples of positive coping strategies. For example, demonstrate how to locate the quietest place in a noisy restaurant or how to discretely leave a crowded noise for a few minutes to “rest your ears and brain” before rejoining a conversation. Managing the patient’s social well-being can also take the form of supplemental technology such as live-voice-to-texts apps and remote microphones that can be personalized to improve the ability to understand conversations in noisy environments.
- Encourage behavior change: This often takes on the form of motivating patients to take action. As an example, the HCP demonstrates some of the coping strategy behaviors mentioned above, and then proactively follows-up with the patient to assess their progress and offer support and guidance.
- If a patient’s well-being is being affected by other mental or cognitive health challenges that cannot be improved with hearing aids, referring to another credentialed specialist is warranted. For example, older individuals with hearing loss are more at-risk than the general population for developing depression (Chakrabarty et al., 2024). If the HCP suspects the patient has depressive symptoms, then a referral might be necessary.
In Closing
Well, folks, that takes us to the end of Volume 8 of Research QuickTakes. For those of you who have read, or at least skimmed, some of our previous seven Volumes, you know that generally we like to work with numbers. Optimum SL for word recognition testing? Critical differences for the QuickSIN? How to program the appropriate MPO? The dB differential for custom vs. instant-fit earmolds? The dB deviations from target allowed for the NAL-NL2? But yes, sometimes, for even us, we need to step back and look at the big picture. I think all of us would agree that helping patients re-connect with life through better hearing is much more than numbers. It certainly is true, that in some cases, dealing with the patient’s emotional and psychological needs is more important than nailing NAL-NL2 targets at 4K within 3 dB!
Going back to the start of our journey, in section one of this Volume, we talked about the prevalence of hearing loss and the significant unmet hearing care needs. This led us to the discussion of the patient journey—and we presented some popular “stages of change” models. All this, of course, relates to patient-centered care, in which we reviewed specific areas that often are not addressed by HCPs, such as: percept of problem, locus of control, listening fatigue, empowerment, and self-esteem—all factors that can impact the adoption, and subsequent benefit from hearing aids. Finally, we addressed the issue of mental health, and how HCPs can be involved with this important issue.
So, not so many numbers, but a lot of things that hopefully spur some of you into action. To make that process easier, we’ll leave you with a short “to-do” list, inspired by some of the research we’ve covered in this Research QuickTakes volume 8.
- Given the immense unmet need and lengthy time course related to hearing aid use, outlined in Section 8.1, we encourage clinicians to provide tele-audiology services that could speed the journey from contemplation to action for some, especially middle-aged adults with mild-to-moderate hearing loss.
- Speaking of contemplation and action stages of change, something we covered extensively in Section 8.2, we recommend that clinicians ask a scaling question like the ones reviewed in Section 8.4, that probes for the patient’s perception of their hearing problem. This scaling question is a great addition to any in-take form.
- Beyond the X’s and O’s of the audiogram and the percentage correct on any word list, there are many components of the individual’s lived experience of hearing loss that can be quickly and accurately assessed in the clinic. Several tools, including the RHHI-S, VFA-A-10 and EmpAQ-5, discussed in Sections 8.4 and 8.5, are great additions to any assessment protocol. These tools are supported by research and contribute in a big way to the therapeutic relationship and patient-centered care – topics we covered extensively in Section 8.3.
- Finally, as we discussed in Section 8.5, there are several ways HCPs can promote successful hearing aid use after the fitting. Besides ensuring that cross-modal plasticity is reversed with well-fitted hearing aids by matching a validated prescriptive gain target, HCPs can improve social and mental health well-being by applying the AIMER counseling approach to their practice protocol.
References
Amlani, A. M. (2016). Application of the consumer decision-making model to hearing aid adoption in first-time users. Seminars in Hearing, 37(2), 103–119.
Barker, F., Atkins, L., & De Lusignan, S. (2016). Applying the COM-B behaviour model and behaviour change wheel to develop an intervention to improve hearing-aid use in adult auditory rehabilitation. International Journal of Audiology, 55(sup3), S90-S98.
Bennett, R. J., Saulsman, L., Eikelboom, R. H., & Olaithe, M. (2022). Coping with the social challenges and emotional distress associated with hearing loss: A qualitative investigation using Leventhal’s self-regulation theory. International Journal of Audiology, 61(5), 353-364.
Bennett, R., Larsson, J., Gotowiec, S., & Ferguson, M. (2024a). Refinement and validation of the Empowerment Audiology Questionnaire: Rasch analysis and traditional psychometric evaluation. Ear & Hearing, 45(3), 583-599.
Bennett, R., Bucks, R., Saulsman, L., Pachana, N., Eikelboom, R., & Meyer, C. (2024b). Evaluation of the Ask-Inform-Manage-Encourage-Refer intervention and its implementation targeting the provision of mental wellbeing support within the audiology setting. Ear and Hearing, 45(3), 600-616.
Bentler, R., Niebuhr, D., Johnson, T., & Flamme, G. (2003). Impact of digital labeling on outcome measures. Ear & Hearing, 24(3), 215-224.
Carpenter, C. (2010). A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Communication, 25(8), 661-669.
Cassarly, C., Matthews, L., Simpson, A., & Dubno, J. (2020). The revised hearing handicap inventory and screening tool based on psychometric reevaluation of the hearing handicap inventories for the elderly and adults. Ear & Hearing, 41(1), 95–105.
Cox, R., Alexander, G., & Gray, G. (2005). Who wants a hearing aid? Personality profiles of hearing aid seekers. Ear & Hearing, 26(1), 12-26.
Cox, R. (2013). Decision aid: Options in the hearing clinic. Retrieved July 12, 2024, from http://www.harlmemphis.org
Ceyhan, A., & Ture, L. (2023). Non-audiological and audiological factors as indicators of hearing aid satisfaction in adults. Journal of Ear Nose Throat Head Neck Surgery, 31(2), 69-74.
Chakrabarty, S., Mudar, R., Chen, Y., & Husain, F. T. (2024). Contribution of tinnitus and hearing loss to depression: NHANES population study. Ear & Hearing, 45(3), 775–786.
Cuevas, S., Chia, V., Chen, R., & Saladen, S. (2019). Determinants of self-efficacy among individuals who are hard-of-hearing. Journal of Rehabilitation, 85(2), 37-46.
Davidson, A., Ellis, G., Sherlock, L. P., Schurman, J., & Brungart, D. (2023). Rapid assessment of subjective hearing complaints with a modified version of the tinnitus and hearing survey. Trends in Hearing, 27, 23312165231198374.
Davidson, A. J., Ellis, G. M., Jenkins, K., Kokx-Ryan, M., & Brungart, D. S. (2024). Examining the use and benefits of low-/mild-gain hearing aids in service members with normal hearing thresholds and self-reported hearing difficulties. Healthcare (Basel, Switzerland), 12(5), 578.
Dawes, P., & Munro, K. (2017). Auditory distraction and acclimatization to hearing aids. Ear & Hearing, 38(2), 174-183.
Dawes, P., Hopkins, R., & Munro, K. (2013). Placebo effects in hearing-aid trials are reliable. International Journal of Audiology, 52(7), 472-477.
Dillon, H., Day, J., Bant, S., & Munro, K. J. (2020). Adoption, use and non-use of hearing aids: A robust estimate based on Welsh national survey statistics. International Journal of Audiology, 59(8), 567–573.
Ear Science Institute of Australia. (2023). Understanding the emotional impacts of hearing loss. https://www.earscience.org.au/2023/03/14/understanding-the-social-and-emotional-impacts-of-hearing-loss/
EHIMA. (2018-2022). EuroTrak country market surveys. www.ehima.com/surveys/
Ekberg, K., Grenness, C., & Hickson, L. (2014). Addressing patients' psychosocial concerns regarding hearing aids within audiology appointments for older adults. American Journal of Audiology, 23(3), 337–350.
English, K., Mendel, L. L., Rojeski, T., & Hornak, J. (1999). Counseling in audiology or learning to listen: Pre- and post-measures from an audiology counseling course. American Journal of Audiology, 8, 34–39.
English, K. (2022). Guidance on providing patient-centered care. Seminars in Hearing, 43(2), 99–109.
Erdman, S. (2013). The biopsychosocial approach in patient-and relationship-centered care: Implications for audiologic counseling. In J. Montano & J. Spitzer (Eds.), Adult audiologic rehabilitation (2nd ed., pp. 159–206). San Diego, CA: Plural.
Gatehouse, S., & Killion, M. (1993). HABRAT: Hearing aid brain rewiring accommodation time. Hearing Instruments, 44(10), 29-32.
Grenness, C., Hickson, L., Laplante-Lévesque, A., & Davidson, B. (2014a). Patient-centered audiological rehabilitation: Perspectives of older adults who own hearing aids. International Journal of Audiology, 53(sup1), S68–S75.
Grenness, C., Hickson, L., Laplante-Lévesque, A., & Davidson, B. (2014b). Patient-centered care: A review for rehabilitative audiologists. International Journal of Audiology, 53(sup1), S60-S67.
Grenness, C., Hickson, L., Laplante-Lévesque, A., Meyer, C., & Davidson, B. (2015). Communication patterns in audiologic rehabilitation history-taking: Audiologists, patients, and their companions. Ear & Hearing, 36(2), 191–204.
Henry, J. A., Griest, S., Zaugg, T. L., Thielman, E., Kaelin, C., Galvez, G., & Carlson, K. F. (2015). Tinnitus and hearing survey: A screening tool to differentiate bothersome tinnitus from hearing difficulties. American Journal of Audiology, 24(1), 66–77.
Holman, J., Drummond, A., & Naylor, G. (2021). Hearing aids reduce daily-life fatigue and increase social activity: A longitudinal study. Trends in Hearing, 25, 233121652110527.
Hornsby, B. (2013). The effects of hearing aid use on listening effort and mental fatigue associated with sustained speech processing demands. Ear & Hearing, 34, 523–534.
Hornsby, B., & Kipp, A. M. (2016). Subjective ratings of fatigue and vigor in adults with hearing loss are driven by perceived hearing difficulties not degree of hearing loss. Ear & Hearing, 37, e1–e10.
Hornsby, B., Camarata, S., Cho, S. -J., Davis, H., McGarrigle, R., & Bess, F. H. (2021). Development and validation of the Vanderbilt Fatigue Scale for Adults (VFS-A). Psychological Assessment, 33, 777–788.
Hornsby, B., Camarata, S., Cho, S. -J., Davis, H., McGarrigle, R., & Bess, F. H. (2022). Development and evaluation of pediatric versions of the Vanderbilt Fatigue Scale (VFS-Peds) for children with hearing loss. Journal of Speech, Language, and Hearing Research, 65, 2343–2363.
Hornsby, B., Camarata, S., Cho, S.-J., Davis, H., McGarrigle, R., & Bess, F. H. (2023). Development and validation of a brief version of the Vanderbilt Fatigue Scale for Adults: The VFS-A-10. Ear & Hearing, 44(5), 1251-1261.
Humes, L. E. (2023). U.S. population data on hearing loss, trouble hearing, and hearing-device use in adults: National Health and Nutrition Examination Survey, 2011-12, 2015-16, and 2017-20. Trends in Hearing.
Janz, N., & Becker, M. (1984). The health belief model: A decade later. Health Education & Behavior, 11(1).
Jorgensen, L., & Novak, M. (2020). Factors influencing hearing aid adoption. Seminars in Hearing, 41(1), 6–20.
Kubler-Ross, E. (1969). On death and dying. Macmillan Publishing Co.
Laplante-Lévesque, A., Brännström, K. J., Ingo, E., Andersson, G., & Lunner, T. (2015). Stages of change in adults who have failed an online hearing screening. Ear & Hearing, 36(1), 92–101.
Lelic, D., Parker, D., Herrlin, P., Wolters, F., & Smeds, K. (2023). Focusing on positive listening experiences improves hearing aid outcomes in experienced hearing aid users. International Journal of Audiology. https://doi.org/10.1080/14992027.2023.2190006
Lelic, D., Nielsen, L. L. A., Pedersen, A. K., & Neher, T. (2024). Focusing on positive listening experiences improves speech intelligibility in experienced hearing aid users. Trends in Hearing, 28, 23312165241246616.
Littmann, V., Wu, Y. H., Froehlich, M., & Powers, T. A. (2017). Multi-center evidence of reduced listening effort using new hearing aid technology. Hearing Review, 24(2), 32-34.
Manchaiah, V., Hernandez, B. M., & Beck, D. L. (2018). Application of transtheoretical (stages of change) model in studying attitudes and behaviors of adults with hearing loss: A descriptive review. Journal of the American Academy of Audiology, 29(6), 548–560.
Manchaiah, V., Bellon-Harn, M. L., Dockens, A. L., Azios, J. H., & Harn, W. E. (2019). Communication between audiologist, patient, and patient's family members during initial audiology consultation and rehabilitation planning sessions: A descriptive review. Journal of the American Academy of Audiology, 30(9), 810–819.
McAllister, M., Dunn, G., Payne, K., Davies, L., & Todd, C. (2012). Patient empowerment: The need to consider it as a measurable patient-reported outcome for chronic conditions. BMC Health Services Research, 13, 157.
McCarthy, P., Montgomery, A., & Mueller, H. G. (1990). Decision making in rehabilitative audiology. Journal of the American Academy of Audiology, 1, 23-30.
Michie, S., Van Stralen, M., & West, R. (2011). The behavior change wheel: A new method for characterizing and designing behavior change interventions. Implementation Science, 6(1). https://doi.org/10.1186/1748-5908-6-42
Mueller, H. G. (1986). Binaural amplification: Attitudinal factors. Hearing Journal, 39(11), 10-24.
Mueller, H. G., & Reeder, P. (1987). Success with binaural amplification: Two important contributing factors. ASHA, 29, 161.
Mueller, H. G., Ricketts, T., & Bentler, R. (2017). Speech mapping and probe microphone measures. San Diego: Singular Publishing.
Oosthuizen, I., Manchaiah, V., Launer, S., & Swanepoel, D. (2022). Hearing aid experiences of adult hearing aid owners during and after fitting: A systematic review of qualitative studies. Trends in Hearing.
Prochaska, J. O., DiClemente, C. C., & Norcross, J. C. (1992). In search of how people change: Applications to addictive behaviors. American Psychologist, 47(9), 1102-1114.
Raihan, N., & Cogburn, M. (2023). Stages of change theory. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK556005/
Rakita, L., Goy, H., & Singh, G. (2022). Descriptions of hearing aids influence the experience of listening to hearing aids. Ear & Hearing, 43(3), 785-793.
Rosenberg, M. (1965). Rosenberg Self-Esteem Scale (RSES) [Database record]. APA PsycTests. https://doi.org/10.1037/t01038-000
Rosenstock, I. (1974). Historical origins of the health belief model. In M. Becker (Ed.), The health belief model and personal health behavior (pp. 1-8). Thorofare, NJ: Charles Slack.
Rotter, J. (1966). Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs, 80(1), 1-28.
Roter, D., & Larson, S. (2002). The Roter interaction analysis system (RIAS): Utility and flexibility for analysis of medical interactions. Patient Education and Counseling, 46(4), 243-251. https://doi.org/10.1016/s0738-3991(02)00012-5
Saunders, G., Frederick, S., Silverman, S., Nielsen, C., & Laplante-Lévesque, A. (2016). Health behavior theories as predictors of hearing-aid uptake and outcomes. International Journal of Audiology, 55(sup3), S59-S68.
Sharma, A. (2021). 20Q: Harnessing neuroplasticity in hearing loss for clinical decision making. AudiologyOnline, Article 27826. Available at www.audiologyonline.com
Simpson, A., Matthews, L., Cassarly, C., & Dubno, J. (2019). Time from hearing aid candidacy to hearing aid adoption: A longitudinal cohort study. Ear & Hearing, 40(3), 468-476.
Taghvaei, N., & Taylor, B. (2024). Clinical application of the Vanderbilt Fatigue Scale for Adults (VFS-A-10): Feasibility and ease of use in a dispensing practice. Poster presented at the American Academy of Audiology Conference, Atlanta, GA.
Taylor, B. (2022). Relationship-centered consultation skills for audiologists: Remote and in-person care. Plural Publishing.
Taylor, B., & Mueller, H. G. (2023a). Research QuickTakes Volume 6 (Pt. 1): Hearing aid fitting toolbox – Important pre-fitting measures. AudiologyOnline, Article 28707. www.audiologyonline.com
Taylor, B., & Mueller, H. G. (2023b). Research QuickTakes Volume 5: OTC hearing aids—Pros, cons, and implementation. AudiologyOnline, Article 28695. www.audiologyonline.com
Taylor, B., & Mueller, H. G. (2023c). Research QuickTakes Volume 6 (Pt. 2): Hearing aid fitting toolbox - verification and validation. AudiologyOnline, Article 28708. www.audiologyonline.com
Taylor, B., & Mueller, H. G. (2023d). Research QuickTakes Volume 2: After the hearing aid fitting - Important considerations. AudiologyOnline, Article 28676. www.audiologyonline.com
Taylor, B., & Mueller, H. G. (2024). Research QuickTakes Volume 7: Useful clinical nuggets mined from recent hearing aid research. AudiologyOnline, Article 28939. www.audiologyonline.com
Citation
Taylor, B., & Mueller, H. G. (2024). Research QuickTakes Volume 8: Hearing aid fitting toolbox v2 - non-audiologic considerations in the selection and fitting of hearing aids. AudiologyOnline, Article 29093. www.audiologyonline.com



