Learning Outcomes
After this course learners will be able to:
- Define an acoustically challenging social situation and its impact on communication for older adults with hearing loss.
- Describe four ways to optimize the performance of hearing aids in acoustically challenging social situations.
- Describe how various noise reduction features work in sync to optimize patient performance in acoustically challenging social situations.
Introduction
Artificial intelligence, machine learning and simple-to-navigate software have made the hearing aid fitting process so seamless and easy that it might be tempting to think that a pair of hearing aids, taken right out of the box and placed on a patient’s ears with little involvement from a clinician is going to lead to peak performance in noise. However, as the third and final part of this tutorial demonstrates, for most patients to experience optimal benefit in noise, the clinician must tailor several facets of device functionality and performance.
“Guess what? I got a fever, and the only prescription is more cowbell.” - The Bruce Dickinson, played by Christopher Walken, in the Saturday Night Live sketch "Behind the Music: Blue Öyster Cult" (April 8, 2000).
We begin the third and final part of this series by taking a careful look at the hearing aid (the product) itself. You don’t have to be a fan of Blue Oyster Cult or Saturday Night Live to appreciate the importance of how well prescription hearing aids perform in noise -- when they are fitted properly. Hearing aid manufacturers like to tout the effectiveness of their noise reduction features, and rightly so; modern hearing aids have never been better at minimizing background noise. For evidence to support this claim, look no further than the trend, clearly outlined in Figure 1. If 30-plus years of MarkeTrak survey data reflect the experience of most patients, it demonstrates that today’s hearing aids have made remarkable inroads when it comes to improving satisfaction in many challenging listening situations. We believe for clinicians to observe these high levels of wearer satisfaction consistently in noisy social situations, they must do more than unbox the hearing aids and rely on first-fit programming.
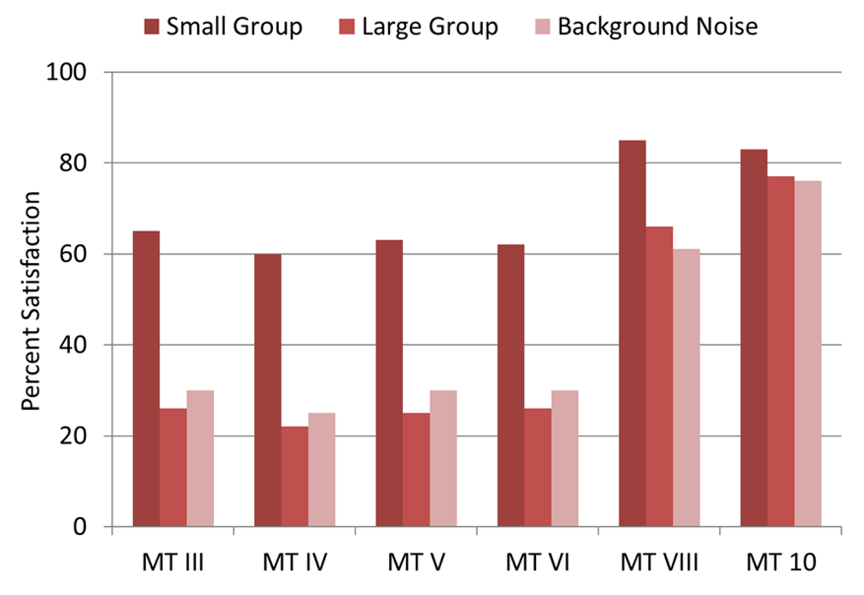
Figure 1. The changes in hearing aid satisfaction as measured by MarkeTrak from 1991 to 2019 for three different types of listening situations. Note the increase in satisfaction in large group and background noise, two acoustically challenging listening situations, in the two most recent MT surveys. MT 10 data comes from Picou 2020Thanks to Gus Mueller for creating this Figure.
The Indispensable Role of the Clinician
We now live in a world where a person with perceived mild to moderate hearing loss could acquire a pair of hearing aids, self-fit them and expect to experience some degree of nominal benefit (Perry & Nelson, 2022). However, we believe for most patients, even those with perceived mild to moderate hearing loss, to experience peak benefit, especially in acoustically challenging social situations, a clinician must be an integral part of the road to an optimized outcome. It is the thoughtful clinician, one who consistently implements best-practice standards, which takes an ordinary, “out-of-the-box” fitting and makes it exceptional. Here we provide four concrete ways clinicians can squeeze the most benefit from hearing aids in noisy social situations.
Signia’s Augmented FocusTM technology found in the Augmented Xperience Platform Part 3 of this series provides tips on optimizing hearing aid benefit in noisy social situations. All the principles discussed apply to fitting any prescription hearing aid, however, Signia’s unique beamforming approach warrants some special attention here in Part 3. Also known as split-band technology, Augmented Focus forms the core of Signia’ AX platform. Augmented Focus splits the incoming sounds into two signal streams. One stream contains sounds coming primarily from the front of the wearer, while the other stream contains sounds arriving primarily from the back. Both streams are then processed independently with different amounts of compression applied to each stream. A recent white paper (Taylor and Jensen, 2022) summaries the efficacy of split-band processing in the AX platform. |
More-Customized Coupling System
“If Bruce Dickinson wants more cowbell, we should probably give him more cowbell.” - Gene Frenkle, as played by Will Ferrell
Today, about 80% of total hearing aids sales are receiver-in-the-canal (RIC) devices (Strom, 2021). Anecdotal reports suggest that upwards of 90% of these RIC devices are dispensed in the U.S. with non-custom, instant fit ear tips. Available in several options, from completely open and flanged to double-domed and closed, there are a few advantages of instant fit ear tips, including physical comfort and cosmetic appeal.
There are potential downsides to instant fit ear tips, all stemming from the unpredictable nature of slit leak venting. Unlike custom earmolds in which the parallel vent diameter is quite uniform and relatively predictable, instant fit ear tips are prone to considerable variability in their venting. This problem is illustrated in Figure 2 where Balling et al. (2019) compared the venting effects of five different types of common RIC ear tips. Figure 2 shows the mean and range of vent effects for five different types of instant-fit ear tips and domes. Note that for the double dome coupling (bottom right panel), one that would seemingly be providing the most closed fitting and commonly recommended for patients with flat, moderate hearing loss, has the largest mean variability in low frequency gain, with up to a possible ~8 dB reduction in gain at 500 Hz, and another ~16 dB of gain reduction possible at 250 Hz.
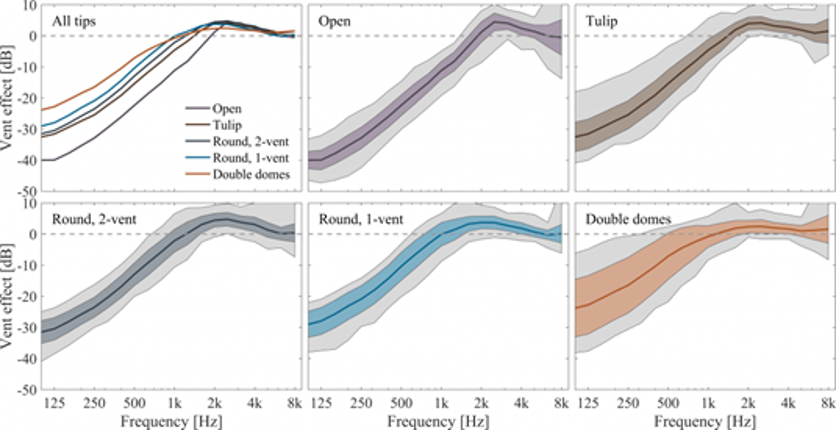
Figure 2. The mean and range of vent effects for five different types of instant-fit ear tips and domes. Note the high variability in low frequency roll-off associated with all the ear tips (Balling et al., 2019).
Instant fit ears tips, with their tendency for slit leaks, can make what looks to be a closed fitting much more open than expected. This can affect directional microphone and digital noise reduction performance in a big way. When slit leaks are large, low frequency sounds (and often mid-frequency sounds) pass directly through the large vent directly to the eardrum without being processed by the hearing aid. Froelich and Littmann (2019) studied how different earmold configurations would affect directional benefit, as measured by hearing impaired listeners’ performance for a speech in noise test. Four different earmolds were used, differing in the degree of tightness, as illustrated in the top panel of Figure 3. Note that as the venting for each earmold becomes larger (more open), the performance, shown in the bottom panel, becomes progressively worse. From most-open to most-closed in Figure 3 we see an SNR improvement of ~3 dB by doing nothing more than making the coupling system more closed.
The same trend holds true for digital noise reduction algorithms. As we know, most annoying background noises, including background speech, tend to have dominant low-frequency sound energy. If a patient is fitted with a “more open” fitting, either intentionally or unintentionally with an unaccounted slit leak in an instant fit ear tip, it is likely that patient will not experience the anticipated noise reduction effects. This occurs for two reasons. First, due to venting effects there is likely little to no low-frequency gain—we can’t “take away” gain that isn’t there. Second, if the fitting is mostly open, noise has a direct path to the eardrum, and much of it remains unprocessed by the noise reduction algorithm.
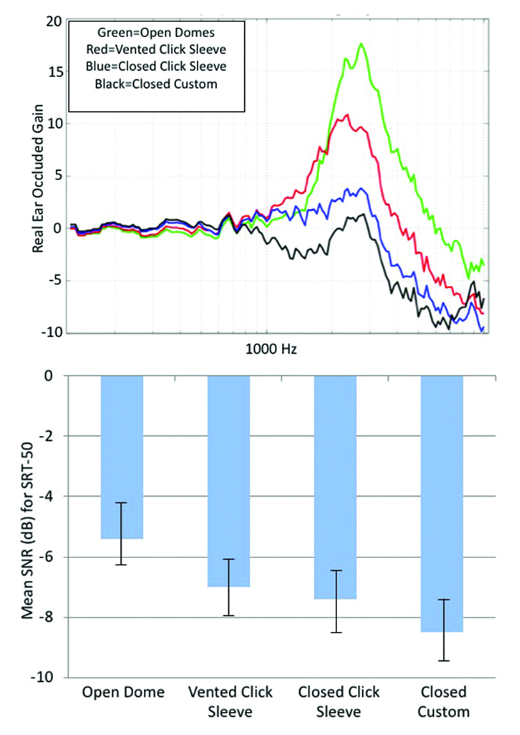
Figure 3. Top panel: The mean of REOGs of four different earmolds. Bottom panel: Mean SRT-50 findings for a speech-in-noise test with the participants fitted with the four different ear coupling systems. Note that as the coupling becomes more open, directional performance is reduced (Froelich & Littmann, 2019).
Through proper earmold selection and by simply accounting for slit leak vents with a real-ear occluded response (REOR) measure (Pumford, 2018), speech understanding in noise can be improved significantly. Seasoned clinicians certainly know the pitfalls associated with a more closed earmold, such as occlusion-related, own voice problems. In many cases, even for milder hearing losses, the best solution would be to fit the patient with custom-made earmolds. Besides providing a more predictable vent diameter, easier insertion and removal by the wearer and secure retention in the ear, fitting a more closed earmold with Signia’s Own Voice Processing 2.0 enables all the noise reduction technologies to work their best while minimizing own voice type problems.
The use of custom made earmolds, even for RIC wearers with mild hearing loss, is best summarized by the aphorism, “good things happen for those who wait.” A customized ear mold might add to the wait time for the patient, but we believe the more predictable noise reduction benefits that come from a custom-made coupling system are worth it – benefits that certainly cannot be purchased over-the counter from a pair of devices that come with a package of assorted pre-molded, instant fit ear tips.
Signia’s Own Voice Processing 2.0 By using machine learning principles that recognize the wearer’s own voice, Own Voice Processing 2.0 adjusts the processing when the wearer speaks; thereby enabling for a more closed fitting that is more likely to optimize performance of the noise reduction features without compromising the quality of the wearer’s own voice. |
More Closely Matched Targets
“Guess what? I got a fever and the only prescription is more cowbell.” - Bruce Dickinson
In Part 2 we addressed the importance of audibility as a cornerstone for performance in background noise. Here we expand on this by discussing the importance of closely matching validated gain targets. By placing a thin tube down into the ear canal and using speech-like sounds as the input, we measure the sound pressure level (SPL) at the ear drum and see how closely it matches a pre-determined target. Much has been written recently about the value of matching an individual’s aided gain to within +/- 5 dB of a validated prescriptive target (Dao et al., 2021) and how to counsel patients about its real-ear measures (Ryall et al., 2021). We encourage clinicians to read these articles and view AO courses (e.g., Mueller, 2017) to gain further insights on the clinical value of real ear measures (REM) for verifying targets.
The aim of this section is to discuss why matching a pre-determined target within 5 dB for soft, average and loud “speech-like” input, minimally as a starting point, directly contributes to improvements in speech understanding in noise. There are several recent studies demonstrating a strong relationship between optimizing audibility by matching a validated prescriptive gain target and improved performance in noisy situations.
Valente et al. (2018) examined individual soundbooth performance for speech recognition in noise. Their work showed significantly better speech recognition ability in noise for a NAL-NL2 fitting compared to a manufacturer-derived first-fit. Specifically, they showed a mean aided speech intelligibility score of approximately 62% when hearing aids were matched to a proprietary gain target, while a mean aided score above 80% was achieved for the same devices when matched to the NAL-NL2 target. In addition, this study had a real-world component in which self-reports of real-world benefit showed significantly greater preference for the NAL-NL2 fitting for 79% (19 of 24) of study participants.
Amlani et al. (2016) took a slightly different approach to addressing the value of optimizing audibility through target matching. They used a 14-item questionnaire that measured attitude and behavior toward perceived value along five dimensions: emotion, perceived quality, price, perceived value, and behavioral intent for three groups of participants. Group 1 were “experienced” wearers who consisted of those with more than one year of hearing aid use experience. Group 2 were “In-the-Drawer” wearers who had previously purchased amplification but did not wear their devices. Group 3 consisted of “first-time” wearers of amplification. Their results demonstrate that probe microphone measures used to confirm that match of a prescriptive target reduced emotional distress and improved perceived quality of service and value of the hearing aid fitting experience compared to the first-fit method in the three groups of participants. Perhaps simply taking the time to conduct real-ear measure is enough to demonstrate to patients the value of the both the product and the clinician.
Using the APHAB, a validated 24-question self-report of benefit, Abram et al (2012) found that when the NAL-NL1 starting point was compared to the manufacturer’s first fit starting point, there was significantly more benefit for the NAL fitting in real-world use. Additionally, this study found 68% of wearers preferred the NAL fit to the manufacturer-derived first-fit approach, compelling evidence that matching the NAL yields relatively good first-fit acceptance.
Perhaps the most persuasive evidence that matching a validated prescriptive target translates into improved speech intelligibility in noise comes from Leavitt (2021). As shown in Figure 4, initially, when the hearing aids were fitted to the manufacturer’s proprietary first fit, aided Quick SIN performance was relatively poor, but when the same hearing aids were re-fitted to more closely match NAL targets, performance in noise improved upwards of 10 to 12 dB. By simply taking the time to optimize audibility by relying on a prescriptive target and confirming it with REM, a hearing aid performing poorly in background noise was transformed into one that performed well in noise – with just a few clicks of a mouse by the clinician.
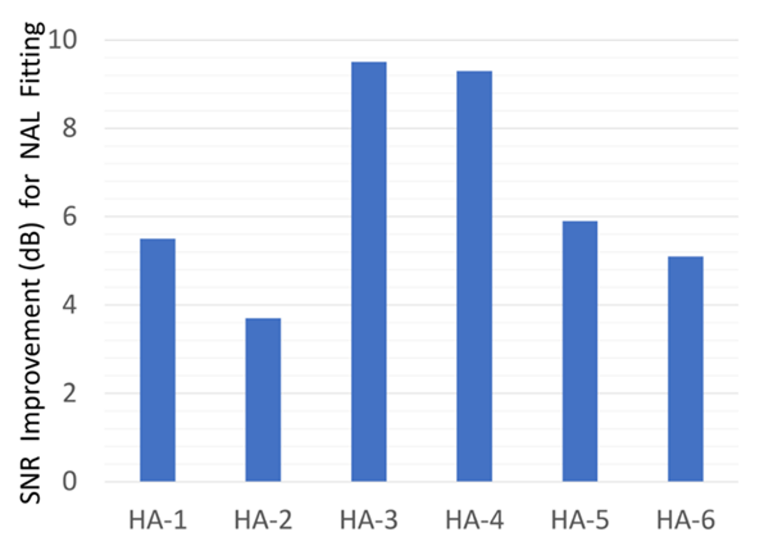
Figure 4. The mean signal to noise improvement for premium devices from six leading manufacturers when adjusted from proprietary first-fit to match the NAL fitting targets (Leavitt, 2021). adapted by Gus Mueller.
So far, we have addressed the importance of matching an individualized gain target for soft, average and loud speech and how that translates into improved performance in background noise, but it is important to also properly match the upper limits of the dynamic range using the wearer’s measured loudness discomfort level (LDL). Thus, it is critical the hearing aid’s maximum power output (MPO) is properly set. Just as matching targets for soft sounds ensure that the quieter parts of the dynamic range are audible, we want to ensure that the upper ends of the dynamic range are also audible and just under the wearer’s unaided individual LDLs. As Mueller et al. (2021) demonstrate most hearing aids default to an MPO setting well below most wearer’s unaided LDL. Therefore, taking the time to use a swept pure tone to get the hearing aid’s MPO just below the wearer’s unaided LDL is critical to customizing or shaping the entire dynamic range.
All of us are familiar with the consequences of an MPO setting that is too high. When the MPO is set too high, patients are likely to turn down gain and receive no benefit from restored audibility in any listening situation. When the MPO is set too high for the individual and gain is turned down for all inputs, a vicious cycle is established in which patients who reduce gain miss out on important conversational speech sounds, stop wearing their hearing aid in these situations, and ultimately, report to others that hearing aids are ineffective in social situations. However, we forget that a similar vicious cycle arises when the MPO is set too low, which, according to the Mueller et al. (2021) data, is a more likely occurrence than an MPO set too high. When the MPO is set too low because peaks of input sounds are clipped, speech is missing many of its necessary dynamics and music is likely to sound “dull.” To make matter worse, when the MPO is set too low, the entire loudness range of speech is limited, as average and loud sounds often differ by less than 5 dB.
Acoustically challenging social situations are among the most likely places where an MPO set too low can cause real problems and actually make the signal to noise ratio of the listening environment worse. To illustrate this point, we paraphrase an example Signia senior consultant, Gus Mueller, uses in his lectures: Let’s say your patient is having dinner in a restaurant and the overall intensity level of the room is 75 dBA. As we mentioned in Part 1, this is a common noise level inside many popular restaurants, bars or cafés. Now, let’s imagine that your patient is wearing hearing aids in which the MPO is set at 75 dB -- a common “out of the box” setting. When the noise level is 75 dB, the talker will raise their voice to 80 dB, which creates an SNR of +5 dB. For most listeners, even many hearing aid wearers a + 5 dB SNR is favorable enough to carry on a conversation. But when the MPO of the hearing aids are 75 dB and the talker raises their voice, the MPO clamps down on it and the talker’s voice remains at 75 dB, keeping the SNR at a much more adverse 0 dB SNR. In short, one of the most effective strategies for maintaining a favorable SNR in noisy places is to set the MPO so that it aligns with the listeners unaided LDL. For more detailed information on measuring patient unaided LDLs, converting to hearing aid MPO values and verifying with real-ear measures, see Chapter 5 of the Ricketts, Bentler and Mueller text, Essentials of Modern Hearing Aids.
In sum, to give patients the best chance of successfully hearing speech in noisy social situations, gain and output should be re-packaged so that soft sounds are perceived by the wearer as soft, average sounds are perceived by the wearer as average, loud sounds are perceived by the wearer as loud. And finally, the entire dynamic range fits just under the individual’s LDLs – a process that requires the use of scientifically derived prescription targets, verified with REM.
There is one final point on target matching that warrants consideration. In this section, we have emphasized the importance of matching a validated NAL (or DSL) fitting target when the primary goal is optimizing audibility and speech intelligibility. (We use the term “validated” to mean the institute that created the prescriptive formula has collected data on thousands of hearing aid wearers to demonstrate their formula works as intended and the creators of the target has published their results for others to evaluate.) This is a sensible approach when fitting any prescription hearing aid; however, when fitting Signia AX hearing aids, and the primary goal is optimizing wearer benefit in noisy social situations, we believe that to squeeze the absolute best performance from the AX platform, it makes sense to use Signia’s proprietary formula: Augmented Xperience-fit (AX) Fit.
To improve the audibility of speech while simultaneously separating background noise (non-speech), the AX platform applies lower compression settings than what’s typically found on other devices. This approach, which is unique to the AX platform, leads to higher overall gain for speech. Therefore, the AX Fit formula requires less gain to achieve audibility and speech intelligibility when compared to other devices. In fact, when the AX Fit target is matched and verified with REM, speech intelligibility results compare favorably to those of the previously cited Valente et al. (2018) study in which hearing aids were matched to the NAL-NL2 target (Best et al., 2021). This reassures us that the results obtained when the AX Fit target is used it is on par with the NAL-NL2 target results.
More Time to Allow the Brain to Rewire
"Really explore the studio space this time" - Bruce Dickinson imploring Gene Frenkle for more cowbell
In the previous section, we emphasized the critical role target matching plays when trying to maximize speech understanding in noise. Here, we address how patients, who have been fitted with devices that fully optimize audibility should be counseled about the brain rewiring process. A process that underscores the importance of “getting used to new things.”
Most of us, at various points in time, spend time getting used to things. When we buy a new car, we often must get used to the feel of the new brakes. When we take a twice weekly exercise class at our local gym, we might need time to get used to the routine of a new instructor. No matter what you’re trying to get used to, there is usually a process that takes you from frustration and annoyance to familiarity, contentment and maybe even happiness. The time course from irritation to satisfaction can take considerable time and effort, and there is of course a lot of individual variability.
Likewise, patients must be given ample time to adjust to hearing aids. Generations of hearing care professionals have recognized the need of patients, especially new ones, to “get used to it,” too. Who among us has not relied on the phrase, “you need to wear them a while to get used to them” when working with a patient who recently acquired a new pair of hearing aids? The process by which a hearing aid wearer re-learns how to make use of acoustic information is commonly referred to as adaptation or acclimatization.
Regardless of the term, acclimatization usually refers to a combination of auditory factors to which the patient may have trouble adjusting to. These range from low-level ambient noise which is now louder following the use of hearing aids, to louder-than-usual soft sounds, to loud sounds that now sound too loud, to the newly acquired audibility of high-frequency speech signals, to the renewed awareness of environmental sounds that were long-forgotten by the new wearer. The underlying mechanisms that allow acclimatization to occur may not be the same for all these conditions, but we do know that many patients need an extended time course to experience optimal results with their newly acquired devices.
Since most patients judge the success of hearing aids by their ability to understand speech in noise, this section focuses on the acclimatization process associated with speech understanding in background noise. The acclimatization associated with speech understanding in background noise has been a topic of research since the advent of the profession when Watson and Knudsen (1940) outlined the basic principles of selective amplification. About 50 years later, Stuart Gatehouse was one of the first to use the term acclimatization to describe his observation that speech recognition in noise improved over time following hearing aid use. Those initial observations, which stem from his studies (Gatehouse, 1992 and Gatehouse, 1993) in which the wearer’s gain and frequency response were well-controlled, provide us with valuable insights on the role of the clinician in setting proper expectations about the wearer’s gain settings.
Those two studies, authored by the late Stuart Gatehouse, indicated that speech recognition ability in noise, although initially stable in the first days of a fitting, continued to improve as the individual continues to wear their devices. His work demonstrated improvements in speech understanding in noise continued to improve over a period of six to 12 weeks after the initial fitting for some individuals.
Importantly, these improvements in speech recognition over time tended to occur in individuals fitted with wideband hearing aids, matched to a NAL target. Results of one of Gatehouse’s acclimatization studies are shown in Figure 4. Note that differences in performance between the wideband NAL and the narrowband “first fit” fittings started to become apparent at six weeks post fitting. Also note his results for the narrowband fitting plateaued at six weeks, while the wideband NAL fitting showed continued, gradual improvement between six- and 12-weeks post-fitting. Although hearing aid processing has become more sophisticated over the past 30 years, there is good reason to believe, based on Mueller ad Picou (2010) survey data and our own clinical experience, that a high percentage of hearing aids fitted today are apt to resemble the narrowband “first-fit” used in Gatehouse’s research; thus, patients fitted with the narrow-bandwidth device might be at-risk for poorer than expected speech understanding results following extended use of hearing aids. In contrast, patients fitted with the wideband, NAL-matched devices, and given ample time to acclimatize to these new sounds, are likely to benefit from the oversight and guidance of a clinician who understands the time course associated with “getting used” to new sounds.
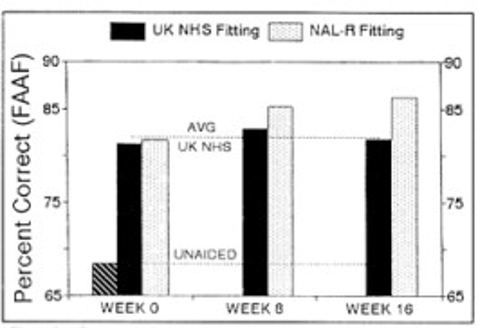
Figure 5. Speech identification in noise scores comparing a wideband, NAL-matched response to a narrowband (UK NHS) fitting (Gatehouse, 1992).
In the early 1990’s, Mead Killion created the mythical Dr. ABONSO avatar to help illustrate the effects of acclimatization. Dr. ABONSO (an acronym that stands for Automatic Brain-Operated Noise Suppressor Option) coined the term Hearing Aid Brain Rewiring Accommodation Time or HABRAT to describe this phenomenon. Killion and Gatehouse (1993) went to great lengths to state that HABRAT was more than merely “getting used” to hearing aids. At its core, as they explain, HABRAT is a fundamental perceptual process in which hearing aid wearers, when exposed to new speech information through their recently fitted devices, need ample time to learn to make use of the new speech cues to eventually optimize benefit. They asserted, thirty years ago, that the brain is plastic and needs time to rewire to the new sound inputs. A concept that only recently we have begun to better understand.
Recently, Anu Sharma and colleagues at the University of Colorado Boulder demonstrated that the adult auditory cortex is a highly adaptive system that re-organizes itself quickly in response to changing inputs. Known as neuroplasticity, the capacity for the human auditory system to adapt to changes results from several factors including learning, maturation, injury, disease, sensory stimulation, and sensory deprivation.
According to Sharma (2021), the cortex of individuals with hearing loss exhibit signs of cross-modal plasticity in which portions of a damaged auditory region of the brain are taken over by unaffected regions. That is, when a peripheral hearing loss deprives the auditory cortex of sound stimulation, other areas of the brain commandeer that area and repurpose that cortical space for other activities.
These cross-modal neuroplastic effects seem to occur in all individuals with hearing loss even those with mild hearing loss, including persons who do not self-report hearing loss. Further, their research shows that with proper auditory stimulation the effects of cross-modal plasticity often can be reversed quickly. To illustrate this critical point, we quote Sharma (2021) at length, “age-related hearing loss participants were fitted with state-of-the art hearing aids at baseline using prescriptive targets. They were provided with counseling regarding how to use the hearing aids and were instructed to wear the hearing aids for 6 months (minimum of 5 hours/day) to remain in the study. ….Six months later, we observed a reversal in cross-modal reorganization, such that there was a reduction in temporal and frontal cortex activity, and restoration of more typical visual processing patterns in response to visual activation.” This vein of research provides compelling evidence that carefully matching prescription gain targets and allowing ample time for the brain to rewire go hand-in-hand.
Signia Acclimatization Manager A sometimes-forgotten feature, one that probably doesn’t get the attention it deserves, is the acclimatization manager, found in the Signia Connexx fitting software. Clinicians can use this feature to bridge the time between initial acceptance of new sounds and providing ample sounds that fully restore audibility and ensure optimal brain rewiring is occurring. |
Today there is ample evidence to suggest that when hearing aids are fitted, the brain begins the process of re-wiring itself and the time course in which this re-wiring occurs, although highly variability across individuals and not completely understood, unfolds over three to six months. Given these neuroplastic effects and their potential association with properly fitted hearing aids, it is recommended clinicians not only carefully match a prescriptive target, but they provide counseling as well as ample time (upwards of 6 months) for this brain rewiring to fully occur. The lesson for clinicians is this: Rather than blithely counseling all hearing aid patients to “wear them a while to get used to them,” a more thoughtful approach, based on evidence, would be to optimize audibility through target matching, say over a relatively short time course of one to four weeks, and then counsel patients that it will require upwards of six months of consistent use (6 or more hours per day) to fully re-wire the brain to new sounds.
More Use of Manual Programs
“Why don’t you lay down that cowbell with us ….. together.” - Eric, lead guitarist
Imagine walking into a crowded cocktail party. One moment you might be trying to follow a small group conversation over the din of several other talkers, while the next moment you might want to enjoy the music of a live jazz band. As recently reviewed by Peele and Wingfield (2022), the human auditory system has the remarkable ability to identify sounds of interest innately and seamlessly in any soundscape - and shift to the sound of interest automatically. The uncanny ability to differentiate between acoustic scenes, which we take for granted when we are young and have normal hearing, begins to wane as individuals age and gradually lose their hearing – a topic we covered extensively in Part 2.
Prescription hearing aids use sophisticated automatic signal classification systems to compensate for the natural ability of individuals to differentiate between these rapidly changing soundscapes. Wide dynamic range compression (WDRC), digital noise reduction (DNR) algorithms, and bilateral beamforming systems are among the essential hearing aid features that, when used in combination, compensate for the wearer’s diminishing ability to hear in acoustically challenging social situations.
We have known for decades that different soundscapes require different settings from these core features for the wearer to experience optimal results. For example, when listening to conversations in quiet the features listed above are working in a much different way, than say, when listening to multiple talkers in a noisy restaurant. To improve performance across a wide range of soundscapes, most modern hearing aids employ multiple programs or destinations, each geared to optimize listener performance in a different soundscape. Each program has a group of features tuned to optimize processing within each program. Signal classifiers, found on all prescription hearing aids, allow for these programs to switch automatically without direct wearer interaction with the hearing aids. No matter the listener’s soundscape, at the heart of automatic program switching is the signal classification system, an often-underappreciated feature of hearing aids.
Signia Manual Programs: Pro Tip In this section we discuss the pros and cons of manual program selection when listening in acoustically challenging noisy situations. A good rule of thumb is to remember that manual programs are selected by the wearer, usually with the help of the clinician, while the sound classifier parameters which determine destinations (also known as automatic programs) are pre-determined by hearing aid engineers in the lab. The clinician and wearer must work together to decide on the use of any manual program. For Signia wearers, in need of a manual program there are a couple of good options that can serve as a starting point.
|
Hearing aid wearers depend on the signal classifier to accurately categorize their soundscape and when that soundscape shifts it’s the job of the classifier to change the processing scheme of the device seamlessly and transparently. Many clinicians probably don’t realize they can set and fine tune the hearing aid features perfectly, but if the signal classifier, which drives the automatic program switching mis-categorizes the soundscape differently than what the wearer might want in any given listening situation, none of those painstaking adjustments made by the clinician are likely to matter. Thus, accurate and precise classification of an individual’s soundscape is an essential part of the wearing experience: when the classifier gets it wrong the wearer is likely to be unsatisfied with the results, and no number of adjustments to the basic sound processing scheme will make a difference.
Just how much variability there is across manufacturers’ signal classification systems was recently illustrated by Yellamsetty et al. (2021). They evaluated the automatic signal classification system of several premium devices in several different listening situations, including speech in quiet, speech in noise and music. Their results showed considerable variability across the various brands on how they classified these differing soundscapes. For example, in more complex listening situations, say speech in the presence of adverse noise, Brand A’s signal classifier might “think” this is a high noise situation demanding aggressive noise reduction that lowers gain for all sounds including speech. In contrast, Brand B might “think” this soundscape is one in which speech must be optimized in the presence of noise and apply more gain than Brand A, while Brand C’s classifier may “think” the listening situation is music and process the incoming sounds in yet another way. The key point is that acoustically complex social situations can yield different combinations of features being activated (or not activated), depending on how the manufacturer’s signal classification system was designed.
Automatic classification systems that drive the selection of different signal processing are, in general, a benefit for the patient, allowing the hearing aid wearer to move from one acoustic scene to another with effective signal processing for each situation. However, because signal classifiers, especially in more complex listening environments, as previously mentioned, differ across manufacturers, there is bound to be places where the automatic classification system gets it wrong for the wearer.
To avoid mis-classifying the wearer’s soundscape, Signia relies on its Universal program, which doesn’t automatically switch into another destination or program as often as other manufacturer’s devices. For Signia, the sound classes combined with the various sensor outcomes (e.g., Motion Sensors) offers a complex set of operating states (not just a few single sound classes) within one Universal program.
Because of how Signia’s Universal program operates, it often provides optimum signal processing in many noisy listening situations. In many acoustically challenging social situations, however, it is possible the listener’s intent at any given moment may be different than how the hearing aids “think” the incoming sounds in that situation should be classified. For this reason, many wearers who find themselves in noisy social situations might benefit from the ability to manually change to a custom-made program dedicated to optimizing performance for a specific noisy listening situation. For some savvy patients, it is advisable to provide them with a manual switch or button on the hearing aid, a remote control or smartphone app that allows them to override any “mistakes” the signal classification system might make by selecting a manual program designed for a certain specific listening situation, like music, speech in noise, etc. A clinician with exceptional listening skills and the ability to navigate the subtle adjustments must work together with the wearer when customizing a manual program to ensure the signal processing inside the product is aligned with the intent of the wearer in these challenging surroundings.
Finally, it is worth considering that while the classification systems might not always get it right, the outcome still might be better than what hearing aid wearers would select manually for themselves – another task that requires careful consideration from a thoughtful clinician.
Signia’s Dynamic Soundscape Processing and Universal Program Signia’s signal classification system is known as, Dynamic Soundscape Processing (DSP) 2.0. Dynamic Soundscape Processing identifies the direction of speech and noise signals and provides better input for determining various noise reduction features on the hearing aids. One way to avoid many of the pitfalls associated with automatic program switching is to seldom automatically switch programs. Because of the effectiveness of DSP 2.0, Signia’s Universal Program allows the devices to effectively process sounds without making unnecessary automatic program switches. However, no signal classifier is smart enough to know the intent of the listeners in noisy social situations. For technology savvy wearers, who find themselves in busy social situations, a dedicated manual program that can adjusted with a remote control, button on the device or smartphone app is the effective way to ensure the hearing aids are fine-tuned to match the intent of the individual wearer. |
More (and Better) Performance in Noisy Social Situations
“Never question Bruce Dickinson.” - Bruce Dickinson
When hearing aids are fitted by following best practices and wearers are effectively counseled on how to wear their devices, outcomes in noisy social situations can be on par with individuals who have normal hearing. This claim is supported by evidence gathered by Jensen et al (2021) on 37 hearing aid wearers using the SSQ (see Part 2 for details on the clinic-friendly, SSQ-12). Ratings on specific questions on the SSQ that involve listening in noisy social situations were compared to ratings made by a group with normal hearing. Observe in Figure 6 that the hearing aid wearers reported outcomes in these challenging listening situations that were equal to or slightly below the group with normal hearing. Common sense suggests that any hearing aid wearer’s ability to communicate in noisy situations, like the situations shown in Figure 6, should be benchmarked to similarly aged individuals with normal hearing.
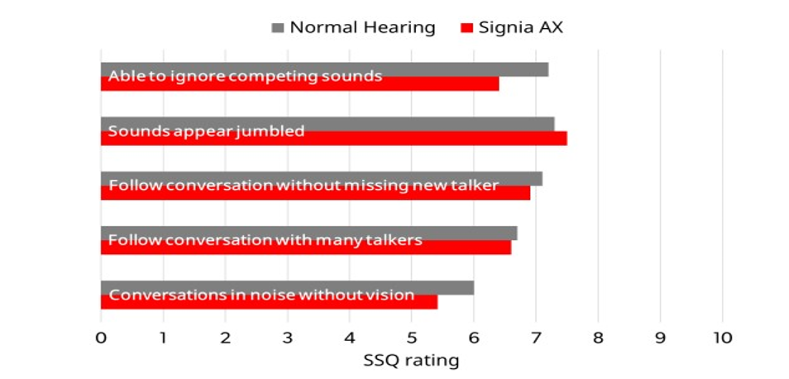
Figure 6. Mean SSQ ratings comparing Signia AX wearers to group with normal hearing (Jensen et al., 2021).
Signia’s Augmented FocusTM Technology in the AX Platform Given the abundance of clinical evidence, outlined by Taylor and Jensen (2022), clinicians can have confidence that when recommending Signa AX technology and following the practical guidance provided across this 3-part series, wearers will experience the highest level of outcomes when communicating in any noisy social situation. |
References
Abrams, H. B., Chisolm, T. H., McManus, M., & McArdle, R. (2012). Initial-fit approach versus verified prescription: comparing self-perceived hearing aid benefit. Journal of the American Academy of Audiology, 23(10), 768–778.
Amlani, A. M., Pumford, J., & Gessling, E. (2016). Improving patient perception of clinical services through real-ear measurements. Hearing Review, 23(12), 12.
Best, S., Serman, M., Taylor, B., & Hoydal, E. (2021). Backgrounder augmented focus. Signia Professional Library. Retreived from https://www.signia-library.com/scientific_marketing/backgrounder-augmented-focus/
Balling, L. W., Jensen, N. S., Caporali, S., Cubick, J., & Switalski, W. (2019). Challenges of instant-fit ear tips: What happens at the eardrum? Hearing Review, 26(12), 12-15.
Dao, A., Folkeard, P., Baker, S., Pumford, J., & Scollie, S. (2021). Fit-to-Targets and aided speech intelligibility index values for hearing aids fitted to the DSL v5-adult prescription. Journal of the American Academy of Audiology, 32(2), 90-98.
Froehlich, M., & Littmann, V. (2019). Closing the open fitting: an effective method to optimize speech understanding. Hearing Review, 26(4), 16-20.
Gatehouse, S. (1992). The time course and magnitude of perceptual acclimatization to frequency responses: evidence from monaural fitting of hearing aids. The Journal of the Acoustical Society of America, 92(3), 1258–1268.
Gatehouse, S. (1993). Role of perceptual acclimatization in the selection of frequency responses for hearing aids. Journal of the American Academy of Audiology, 4(5), 296–306.
Gatehouse, S., & Killion, M. (1993). HABRAT: hearing aid brain rewiring accommodation time. Hearing Instruments, 44(10), 29-32.
Jensen, N., Powers, L., Haag, S., Lantin, P., & Høydal, E. (2021). Enhancing real-world listening and quality of life with new split-processing technology. AudiologyOnline, Article 27929. Retrieved from https://www.audiologyonline.com
Leavitt, R. (2021). 20Q: In pursuit of audibility for people with hearing loss. AudiologyOnline, Article 27848. Retrieved from www.audiologyonline.com
Mueller, G. (2017). Hearing aid verification: what you can't buy over the counter. AudiologyOnline, course archived at https://www.audiologyonline.com/audiology-ceus/course/verification-what-you-can-t-29787
Mueller, H. G., & Picou, E. (2010). Survey examines popularity of real-ear probe-microphone measures. The Hearing Journal, 63(5), 27-28,30,32.
Mueller, G., Stangl, E., & Wu, Y. H. (2021). Comparing MPOs from six different hearing aid manufacturers: Headroom considerations. Hearing Review, 28(4), 10-16.
Peelle, J., & Wingfield, A. (2022). How our brains make sense of noisy speech. Acoustics Today, 18(3), 40-48.
Perry, T. T., & Nelson, P. B. (2022). Self-adjustment of hearing aid amplification for lower speech levels: independent ratings, paired comparisons, and speech recognition. American Journal of Audiology, 31(2), 305–321.
Picou, E. M. (2020). MarkeTrak 10 (MT10) survey results demonstrate high satisfaction with and benefits from hearing aids. Seminars in Hearing, 41(1), 21–36.
Pumford, J. (2018). Considerations in real-ear measurement: points to ponder. Canadian Audiologist, 5(3).
Ryall, A., Jenstad, L. M., Pumford, J., Howe, T., & Grosjean, G. (2021). Counseling during real ear measurements: the clients' perspective. Journal of the American Academy of Audiology, 32(2), 107–115.
Strom, K. (2021). A brief history of hearing aid technology types, 1979-2020. Hearing Journal. Retreived from https://hearingreview.com/hearing-products/hearing-aids/a-brief-history-of-modern-hearing-aid-technology-types29-32.
Taylor, B., & Jensen, S. (2022). Evidence supports the advantages of Signia AX's split processing. Signia White Paper. Retrieved from Signia Professional Library
Valente, M., Oeding, K., Brockmeyer, A., Smith, S., & Kallogjeri, D. (2018). Differences in word and phoneme recognition in quiet, sentence recognition in noise, and subjective outcomes between manufacturer first-fit and hearing aids programmed to NAL-NL2 using real-ear measures. Journal of the American Academy of Audiology, 29(8), 706–721.
Watson, N., & Knudsen, V. (1940). Selective amplification in hearing aids. Journal of the Acoustical Society of America, 11, 406-419.
Yellamsetty, A., Ozmeral, E., Budinsky, R., & Eddins, D. (2021). A comparison of environment classification among premium hearing instruments. Trends in Hearing. https://doi.org/10.1177/2331216520980968
The authors would like to thank Navid Taghvaei, AuD, Sr. Clinical Education Specialist, Signia for his valuable comments and suggestions.
Citation
Taylor, B. & Jensen, N. (2022). Optimizing patient benefit in acoustically challenging social situations, part 3: product. AudiologyOnline, Article 28438. Retrieved from https://www.audiologyonline.com