Learning Outcomes
- Identify the long term value of devising KPIs for an audiology practice
- Implement a comprehensive strategy of incremental improvement through collection and use of KPI data
- Explain the interconnectedness of culture, goals and KPIs and the impact each has on overall financial performance of a practice
Introduction and Background
Historically, audiologists did not have the capability to systematically measure any part of their business. Sure, they had a general idea of their return rate, gross margin or annual revenue, but oftentimes it was more of a guess than a cold, hard fact. The daily operation of their practice was left completely to intuition and chance. In fact, leaving the performance of the business to chance was a standard business practice in many practices.
Today, due mainly to relatively inexpensive, web-based office management systems, audiologists have a virtual arsenal of data at their fingertips. With a swipe of a finger on their smartphone or the click of a mouse on their laptop, an audiologist can gauge the effectiveness of their latest marketing campaign, or the need to fill their schedule with more patients. In many ways, this ocean of data reflects both a surge in technical sophistication driven by the ever-improving microchip as well as a society preoccupied with lists and numbers. Charts, graphs, stats and other types of numbers are all around us. From tracking your favorite fantasy sports star to following the popularity of your last Tweet, there is no escaping the sheer breadth and depth of data, all of it readily available at our fingertips. Nevertheless, based on our experiences, many audiologists, who have access to heaps of data about their practice either chose to ignore it, or fail to use it to make decisions about their business. Perhaps a failure to act on the abundance of this data is a side effect of having too much information. An example of just how much data can be loaded onto a single dashboard is shown in Figure 1.
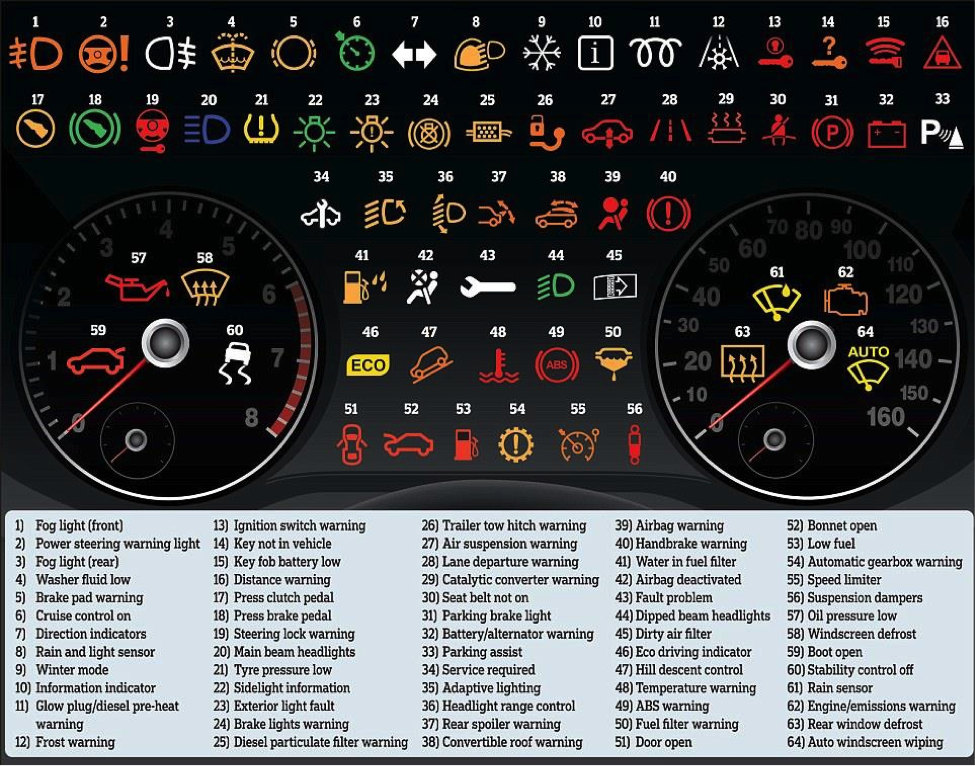
Figure 1. Dashboards can provide an abundance of information. Much of the data may be overkill for the busy clinician.
No one would argue that the data shown in Figure 1 is unimportant. After all, if your car’s brake pads are malfunctioning and light #5 above is flashing red, it’s an indication to take immediate action. The real challenge with the availability of so much data, however, is understanding what key performance indicators contribute to making intelligent decisions about your practice. In other words, what data provides you with the best bang for your buck? Sticking with the example above, it takes time to evaluate 64 different data points. It might be okay for driving your car, but if you’re trying to conduct all the necessary elements of managing a practice, dealing with this amount of information is likely to lead to analysis paralysis. This tutorial will address KPIs that allow clinician to take meaningful action without being flooded with too much information and avoid paralysis through too much analysis. The ability to strike a balance between obsessively analyzing every possible data point collected by a cloud-based office management system and intuitively managing these numbers is a key to the long-term sustainability of any business. As we hope to demonstrate, by identifying a group of balanced KPIs managers can begin making better, data-driven decisions about their practice.
Let’s start by addressing the most basic of questions. What is a KPI? Key Performance Indicators (KPIs) help a practice define and measure progress toward a goal. Once a practice has identified its mission, its strategic imperatives and clearly defined its goals, KPIs are needed to gauge progress towards those goals. In many ways, it simply doesn’t make sense to measure any KPIs without first establishing some clear goals in your practice. There is nothing magical about KPIs. In their purest sense, KPIs are numbers that reflect what has already happened in your practice, and, perhaps provide some insight about what needs to happen in the immediate future. To really understand the power of a good set of balanced KPIs it’s essential to step back and address the importance of office culture and goal setting.
For any audiology (or hearing aid dispensing) practice there are two major types of goals. First, the practice needs to establish financial goals. Financial goals involve examining revenue and profitability of a practice over a specific period of time. Without revenue and profit a practice cannot hope to sustain itself over time, thus financial goals are critical. Most financial KPIs, as we hope to demonstrate, are a yardstick for measuring some derivative of revenue and profitability. Since the delivery of hearing aids is such an integral part of revenue generation in most practices, it’s common that many KPIs involve them. For example, the most common KPIs usually include some variation of average selling price, units sold and opportunities to dispense products.
A second set of KPIs can be created by measuring the patient’s experience in your practice. Yes, this second type of goal is more existential, and maybe a little harder to measure, but these types of KPIs, we have found, are essential to obtaining a market leadership position in your area, or what some have called “pillar of community” status. These are known as quality KPIs. Given the importance of word-of-mouth referrals, which is largely driven by highly satisfied patients, it’s critical for a practice to create some KPIs around patient satisfaction, benefit and willingness to refer. Since revenue and profit are the foundation of maintaining a business, this tutorial will focus on financial KPIs, but many of the principles described here can be applied to quality KPIs.
Hierarchy of Practice Success
The ability to develop and manage KPIs effectively doesn’t exist in a vacuum. Practices that have taken the time to foster a culture of trust and accountability are more likely to make better use of KPIs. In simple terms, there is a distinct hierarchy of attributes successful practices seem possess. This hierarchy, which is shown in Figure 2, is culture, goals and KPIs. The important point is that these three attributes - culture, goals and KPIs - are intimately linked. In other words, the more time spent developing a culture based on trust and accountability, the more likely you will meet your goals and KPI targets.
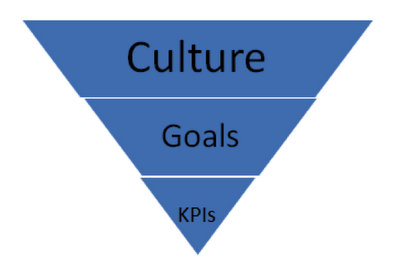
Figure 2. The hierarchy of practice success.
The daily work environment in your clinic and the way in which individuals interact and relate to one another are essential components of any sustainable business. The quality of the work environment and its relationships may be even more important in healthcare businesses where staff is expected to interact with patients and talk about personal matters with patients, such as the long term emotional consequences of hearing loss or payment for services. These daily tasks require a high level of interpersonal communication among staff. Thus, the foundation of effective communication between staff is culture. In straightforward terms, your office culture is defined by the quality of these day-to-day interactions, and it is primarily up to the practice manager and other leaders within the organization to define your culture.
In a world awash in a sea of data, building an effective office culture requires employees to take action on the data that is collected. This begins by asking good questions about how data can be used to make decisions about the practice. Additionally, access to data even allows audiologists to conduct informal experiments that contribute to greater efficiency and success. Rather than view data as an albatross, clinicians would be wise to think of ways to use data creatively. For example, today, it is easy to gather real time data about specific hearing aid models and patient outcomes in any practice. In this era of Big Data, this type of customized information about the daily operation of a practice allows clinicians to make more intelligent decisions about what products might contribute to better patient outcomes, or which specific clinical tests lead to more efficient office flow.
Six Steps to Getting Most from Goals and KPIs
Beyond the collection and utilization of data, there are dimensions of a practice’s operations that are the cornerstone of long-term success. The cornerstone of office culture profoundly influences goal setting and the construction of KPIS. Although the manager is not solely responsible for determining the culture of the office, she can establish expectations and set the stage for a thriving office culture. The following 6-step process for creating an office culture committed to effective interpersonal communication, high quality patient care and continuous improvement is a proven approach to utilizing KPIs to help navigate your daily business operations. In our experience, we have found these six steps contribute in big ways to the development of goals and KPIs.
Articulate a clear mission. As you look out over the next two to three years, how will your practice be known in the community? The answer to this question will help you articulate your long-term vision and mission of your practice to your staff. Some examples of a clear mission include being recognized in your community as a leader in providing comprehensive medical care to everyone or offering the most engaging patient experience in your marketplace. Notice both of these mission statements are simple, yet broadly focused. They are meant to define your mission and engage your staff in developing it over time.
Determine your roadmap for success and share it with your staff. In other words, you need to paint the picture of success and how you plan to achieve with the actions of your staff. This step is likely to require you to create an organizational chart and make some financial projections. That is, a financial comparison of your practice today (e.g., gross profit & revenue per month) compared to 1-2 years from now. How many patients will you need to see each month to meet these projections? How many hearing aids will need to be dispensed and at what ASP, so that your business is profitable? And, how will the organization be structured to best meet these demands. This step will provide clarity of purpose for your entire staff.
Clearly define roles, daily routines and goals. This is the critical step that provides granularity for each person on your team. It requires that you customize a job description for each person. What specific daily routines must be conducted and how will staff improve? The second part (and more difficult) aspect of step 3 is to carefully define specific tasks and behaviors that contribute to successful patient outcomes and a profitable practice. Take the time to map out the exact details of these tasks and behaviors for each staff. Once each member of the staff has a clearly defined role and firmly understands their role each plays in the practice, it’s essential to set goals.
Facilitate routine engagement with your staff. Meet with each staff member individually at least one time per month and as a group every other week. Establish a rhythm for these meetings by scheduling them in advance at the same time and day of week. The main objective of this step is to ensure people are involved in each step of the process. Here are some questions you can ask your staff during the one-on-one meetings: Where are we going as a practice? Where are you going as a professional? What do you think we are doing well? What are some suggestions for improvement? How can I help you achieve your goals? What suggestions do you have for me and the practice?
Bathe your staff in feedback. Feedback provides even more clarity of purpose, especially when it’s delivered on a routine basis. The goal of providing real time feedback is to build a culture devoted to continual improvement of all the routines, tasks and behaviors that are instrumental to running a successful practice. Step 4 described a more formal approach to communication with your staff. Step 5, on the other hand, is there to remind managers that have the responsibility of provide insight and guidance as to the staff’s daily routines. As a rule, 80% of feedback should be positive and encouraging…. “When you stood up and personally greeted that gentleman today, I saw how his face lit up. Great job!” On the other hand, when you see something that needs to be improved or not in alignment with your culture the manager has the responsibility to provide constructive (or adjusting) feedback that is designed to improve day to day tasks and behaviors. It sounds something like this: “Mary, can I give you a little feedback?” Assuming the employee says it’s okay, you would then say, “When you had your back turned on that patient this morning as he was trying to schedule another appointment, I noticed that he appeared annoyed…what could you have done differently to avoid that situation?” Providing this type of adjusting feedback is how we talk about performance in a non-emotional, productive manner.
Re-evaluate your vision and roadmap about every six months. Adjust other steps as needed. Beyond setting goals and objectives, these six steps will help you build a local brand cemented in quality and continuous improvement. The bottom line is KPIs are more meaningful in a culture of accountability and results.
We have found that methodically executing these six steps help practices attain two critically important things: sustainable, year-over-year financial results, and staff engagement in a high level of patient care.
The Critical KPIs
Once a manager has established a culture of accountability and results, it’s imperative to identify a handful of KPIs that can be evaluated on a daily or weekly basis. For the ENT medical practice, we have found there are three overarching KPIs that need to be routinely measured. For each of the three KPIs listed here, we also have listed several derivatives of it. Although there is a lot of chatter about personal sound amplification devices (PSAPs) and other types of direct to consumer amplification products, the traditional hearing aid remains the standard bearer of revenue generation for audiologists. Thus, the hearing aid needs to have its own set of KPIs, which are summarized below.
1. Hearing Aid Revenue
a. Average Sale Price - The average retail price per hearing aid sold before discounts. (Gross Hearing Aid Revenue divided by total units)
b. Revenue by Provider
c. Revenue by Department
d. Binaural Rate
2. Hearing Aid Volume: The number of hearing aids units sold over a finite time period.
a. Units by Provider
b. Units by Practice
c. Conversion Rate (number of devices sold relative to opportunities, expressed as a ratio or percentage)
d. Unit Return %
3. Hearing Aid Gross Profit: The percentage of gross revenue from hearing aids dispensed.
a. Gross Profit %
b. Gross Profit per Unit
c. Cost of Goods %
d. Cost per Unit
e. Gross Profit by Provider
When creating your list of KPIs it is important to understand the relationship between each of the three broad hearing aid KPI categories: gross profit, volume and revenue. For example, say, gross profit and revenue is at 100% of target, while volume lags behind at 70% of target. This constellation of numbers is likely going to require the practice focus on boosting consultative selling skills in order to capitalize on converting more opportunities into hearing aid wearers. On the other hand, if volume is at 100% and gross profit and revenue are below target, this set of numbers suggests that the practice’s price strategy needs to be carefully evaluated. Perhaps the practice needs to negotiate a better cost of goods with their vendors or examine their retail pricing structure. Without these three KPIs it would be difficult to know what to target. Figure 3 shows several important KPIs from one practice and how they compare to benchmark data. The pattern on the spider-gram pinpoints areas in need of improvement. It’s also worth noting it is oftentimes helpful for an individual practice to rely on the expertise of an independent business consultant to device KPIs and benchmarks. Not only are consultants helpful at winnowing all of the data generated by office management systems into actionable chucks, but they can offer valuable input on how to narrow gaps relative to benchmarks.
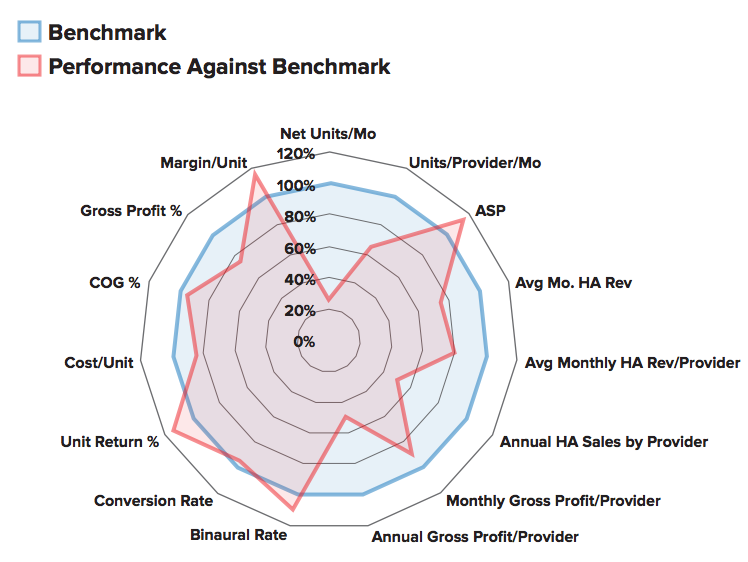
Figure 3. A spider-gram comparing a practice’s KPIs to benchmark data.
The Importance of Benchmarking
KPIs without a benchmark are meaningless. A benchmark is a standard of performance against the performance in your practice can be measured or judged. It’s important to choose KPIs that are representative of your practice. For example, if you’re in an ENT practice with 4 full-time audiologists, the benchmarks in which you judge your practice should be derived from practices of a similar size. There are several sources of benchmarking information. Each year Phonak sponsors a benchmarking survey (e.g., Rawn, 2013). In addition, Gleitman (2015) has authored a paper on industry benchmarks. There are other good sources for industry benchmark data, including buying groups, office management system vendors and other hearing aid manufacturers.
Although there are no shortages of benchmarks, care must be taken to choose those most representative of your practice’s mission and goals over the next two to three years. Once a solid group of benchmarks are in place, the challenge becomes devising a plan to narrow any gap between actual performance and the benchmark. Let’s examine some specific strategies for narrowing those gaps.
Strategies for Moving the Needle
Once you have identified a gap between a benchmark and the actual performance in your practice judged against that benchmark, it is vital to put a specific plan in place to close the gap. After all, it makes no sense to establish a benchmark and measure performance against it, if you don’t take action with the information you are gathering. One of the most common gaps in an ENT practice’s audiology business revolves around retail pricing.
Let’s say, for example, that your audiology clinic’s average selling price and average margin per unit are remarkably low compared to the benchmark for a practice of similar size and location. The first step to shoring up this pricing gap would be to gain better insight and awareness of the market. This process would include comparing your practice’s performance in these areas to others of similar geographic location and demographic variables (e.g., age and income). Other dimensions that need to be carefully evaluated when trying to move the needle on a gap related to a low average retail price include looking at the existing product mix of the practice and a need to keep price points simple for patients to understand. All possible causes of this ASP shortcoming should be evaluated with the staff. After deliberation and guidance, this practice implemented a plan in which more time was taken to carefully explain the benefits of mid and upper end technology to patients. Using more of a comprehensive, lifestyle approach to the hearing aid selection process, implemented over time with thoughtful coaching and feedback resulted in a marked improvement in the average selling price (ASP) per unit in this practice. These results are shown in Figure 4. Notice that the total hearing aid volume was unchanged, but ASP increased substantially. Clinicians in this practice were able to equate improved technology with the communication needs associated with more active lifestyles in their counseling approach with patients. Although not depicted in this Figure, patient outcomes were reported to have improved along with the ASP.
Figure 4. A comparison of ASP before and after coaching and training in one ENT practice.
The Role of Effectiveness Managers
Effective management is not complicated, nor is it necessarily time consuming. It does, however, require some measure of tenacity and discipline to carefully choose a group of KPIs, follow them over time and devise strategies for improvement. Regardless of the exact KPIs a practice decides to put into place, it is the responsibility of managers to ensure that missions and goals are communicated clearly. Based on our experience working with a variety of medical practices around the country there are three critical roles an effective manager plays when trying to improve overall business performance of audiology in the ENT practice.
Setting Targets
After agreeing on a core set of financial KPIs, such as those shown in Figure 3, apply the mission and goals of the practice to devise targets for each member of the staff. These targets should be in alignment with the culture of the practice. Additionally, the target must account for the three core components of hearing aid KPIs: volume, revenue and profit.
Measuring Results
Using a computer-based office management system, measure the results of your core set of KPIs. Using a graph or dashboard similar to the one in Figure 3, generate reports on a weekly basis that compare results to the target and benchmarks you have established.
Create a Culture of Performance Centered on Patient Outcomes
Talk about performance, keeping patients top-of-mind. Produce an office culture that has an obsession with doing what’s best for patients without losing sight of the financial goals of the practice. In a successful practice staff is constantly talking about ways to incrementally improve clinical skills and performance so that patients’ outcomes can improve. Thus, increases in financial performance are a by-product of patient success.
Summary
In today’s world, data is instantaneous, ubiquitous and abundant. We are flooded with information, much of it irrelevant, in the form of dashboards, survey data and top 10 lists, often broadcast through various forms of social media. Even though data is everywhere, it is still seldom used by audiologists to make decisions about their practice. By following some of the straightforward rules outlined in this article audiologist’s in an ENT or other similar medical practice can achieve higher levels of success.
References
Gleitman, R. (2015). Your business and practice benchmarking. Hearing Review,22(8), 18-21.
Rawn, K. (2013) US Hearing industry benchmarking survey: How do top performers drive growth? Audiology Practices,5(3), 5-19
Cite this Content as:
Taylor, B., Grant, B., & Boyer, J. (2015, November). The numbers don’t lie: Audiology key performance indicators in an ENT practice. AudiologyOnline, Article 15691. Retrieved from https://www.audiologyonline.com



