Learning Outcomes
After this course, learners will be able to:
- Summarize the critical features of Miller’s Pyramid Model and the Educational Scaffolding Model.
- List the reasons why using Miller’s Pyramid and Educational Scaffolding makes learning more effective.
- Summarize multiple ways in which you can utilize the educational models discussed to improve patient education in your clinic.
Introduction
“See you in 6 months!” said Mr. Jones’ Audiologist at the end of his bi-yearly hearing check up. Hearing aids professionally cleaned and serviced? Check! Updated audiogram? Check! Real Ear Measurements (REM) performed for verification? Check! Mr. Jones left the clinic with an ample supply of domes, filters, and batteries, only to have his hearing aids end up in a drawer two weeks later. Data logging at the next check up? 0.3 hours a day.
What went wrong? This may lead us to the million dollar question: Why is hearing aid usage low with a seemingly perfect fitting? Even though we meet best practice guidelines, some patients continue to have poor hearing aid usage.
As an audiologist, I am always trying to find innovative and effective ways to improve my patient’s hearing ability and efficacy with their hearing devices. I have interacted with a variety of patients in various audiological environments, including private practice, hospital units, and busy ENT clinics. I’ve observed a spectrum between individuals who are excited to finally hear better with their new devices and others who may feel embarrassed of their hearing loss and thus not take full advantage of their hearing aids. Some patients are excited to stream podcasts and music with their new devices, whereas other patients may find their hearing aid app confusing and intimidating and therefore not want to use it. Finally, some patients may nod their head and claim they understand all of their new hearing aid features during the fitting appointment, but when they get home and try to use it on their own, they discover “It sounded easy when the clinician showed me how to use it, but now I’m lost.” How do we best support a patient like Mr. Jones with his hearing aid, with a goal to maximize his hearing aid usage from day one?
I believe the answer to the million dollar question is better education. Helping patients use effective educational tools can lead to a win-win for both the patient and my clinic. Let’s dive in.
Back to Basics - How Do We Learn?
Remember what it is like to learn something new - whether it was learning how to perform REM, learning how to swim, or learning how to solve an algebraic equation in grade 8 - it wasn’t as easy as a teacher telling you how to do it, and immediately being able to apply it (and if that was you, then I’m jealous!). Typically, you had to enter a period of ‘trying it for yourself before you felt comfortable doing it on your own. For swimming, that may mean practicing with a flutter board or floaty until you get the strokes right while an instructor supervises you. For algebra, that may mean going home and doing an algebra worksheet where you apply what you learned and review your answers the next day. However, when we get older, we seem to forget these most basic fundamentals of education. Perhaps our patient, Mr. Jones, isn’t a problem-patient who does not want a hearing aid. Maybe Mr. Jones needs a more collaborative, effective, and patient-centered approach to learning hearing aid related skills, one in which he can get hands-on training and experiment with the hearing aid, all with the clinician present before he goes home.
I will focus on two basic models to frame how we can design a better educational experience for our patients. The first model being the “Knows, Knows How, and Shows How” model, and the second is the “Educational Scaffolding” Model. I propose that keeping these models in mind during your time with patients will help drive better hearing aid usage, reduce easily avoidable hearing aid problems, and provide a better and more unique patient experience.
The “Knows,” “Knows How,” “Shows How” Model
This model was first popularized by psychologist George Miller, who developed the framework for assessing clinical competence (1). Miller used a pyramid to describe how clinical skills must be learned from the ground up (Figure 1). The basic premise is that to learn a new skill effectively. You must make your way up the pyramid during your learning and progress from “Know” to “Know How” to “Shows How” to “Does.” If we look to apply this framework to our own educational journey through hearing healthcare and learning something like REM, first we “Know” what REM is and why we need to do it. Second, we “Know How” to conduct REM and the steps you must take. We don’t stop there - next, you need to “Show How,” which involves getting hands-on with the equipment. This can be done on models/simulators or on patients/classmates. Finally, we arrive at the “Does” stage, where it is now muscle memory, and you can easily complete a REM fitting. Once the skill is imprinted in you, you truly have mastered it. But skipping any of these steps is a recipe for struggle. Think about it - If you went from learning how to do REM from a PowerPoint lecture to working with patients, how well would you have done?
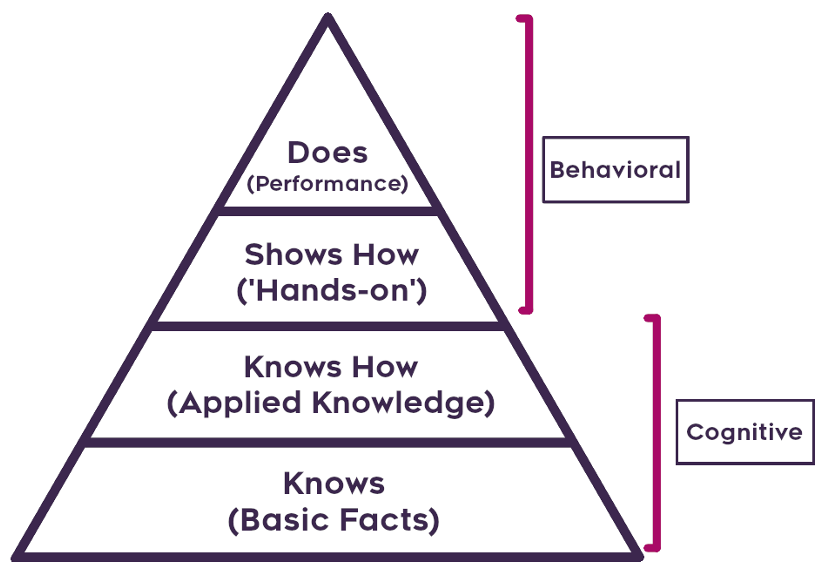
Figure 1. Miller’s Pyramid, showing the progression from “Knows,” “Knows How,” to “Shows How.”
Now to apply this to hearing aid education: do your patients “Know” about their hearing aids? Do they “Know How” to use them and how to make them function properly? Finally, can they “Show How” they will use them at home? Often, much of our clinical time is spent on helping the patient “Know” about their hearing aid, but little time is spent on “Knows How” or “Shows How” so they can’t remember how to “Do” at home. Leaving a patient at “Know” is a little like teaching someone how to swim with a 5 minute seated lecture and throwing them in the deep end with no supervision - not great for anyone!
The Educational Scaffolding Model
Now that we understand the “Knows, Knows How, Shows How” model, how do we apply this to a multi-step skill? For learning to swim, you cannot go from “Knowing How” you should move your arms and legs directly to “Showing How” to tread water in the deep end of a pool. Instead, you need to be eased into it and learn a small piece of the total skill at a time until you can put all the pieces together yourself. In most modern education systems, this is called “Educational Scaffolding” (2). Scaffolding is used to teach learners new skills, from solving mathematical problems to shooting basketball free throws. To facilitate learning with scaffolding, there are three essential features to keep in mind.
Collaborative learning. This first feature ensures that the interaction between the learner and the expert is collaborative. Collaborative learning focuses on a learner’s exploration of a skill and not on a teacher’s presentation of it. This method is a significant shift away from the typical teacher-centered, lecture style instruction typically employed decades ago. In a collaborative learning environment, traditional lecture-style instruction can still take place, but it is used alongside a learner’s active work with the new skill. When you think back to university classes, high school courses, or even recent workshops, in what types of educational settings did you learn best? Did you learn and retain the course material from a traditional lecture-style course, or was it the courses where the instructor made time for active discussion, collaborative demonstrations, debates, hands-on activities, and effective group work? In “Knows, Knows How, Shows How” language, this means getting to “Shows How” as soon as possible in the learner’s journey. Facilitators who use collaborative learning approaches tend to think of themselves less as expert transmitters of knowledge, and more of expert designers of intellectual experiences for learners.
Zone of Proximal Development. The second feature states that learning should be done in the learner’s zone of proximal development. Learning in the zone of proximal development is a fancy term for the difference between what a learner can do on their own, and the most that can be achieved with the support of a knowledgeable instructor. The goal of an educator using the scaffolding model is to implement various resources, referred to as scaffolds, to allow a learner to further develop their knowledge. To do this effectively, it’s important that an educator correctly identifies where a learner’s current level of knowledge is. After identifying this information, an effective educator would then work to facilitate learning beyond that point. Imagine that a child with minimal swimming skills needs to learn how to tread water for two minutes. Having the child jump into the deep end and start treading water would be beyond their zone of proximal development, even with proper instruction from the side lines. In this case, the student was expected to learn outside of their zone of proximal development, which is an ineffective (and very dangerous) learning approach. However, having the child first practice arm and leg movements outside of the water, then practice these movements in the water with a lifejacket, then with a pool noodle, then unassisted, would be more effective because each step of the process is inside their zone of proximal development. Remember, this emphasizes the need to move away from “Knows” and “Knows How” and get to “Shows How” as soon as possible in small, manageable chunks.
Gradual Removal of Scaffolding. Finally, the third feature is utilized as the learner becomes more proficient. When buildings are being constructed, scaffolding is erected to provide critically important support for the raw materials and workers, but the scaffolding eventually needs to be removed when it provides no purpose. In the Educational Scaffolding Model, the resources used to assist learning at a more complicated level should be removed (or replaced with different scaffolds) once the learner has out-grown them.
To apply this to both hearing aid education and to the “Knows, Knows How, Shows How” model, we can make the following conclusion - Easing the transition from “Knows How” to “Shows How” is crucial, along with getting a patient to “Shows How” as soon as possible. Get them hands-on.
Are We Done Talking About Models Yet?
Almost! My goal with this article is for you to “Know” proper educational frameworks, and “Know How” to apply this to hearing aid education to improve your clinic and patient experience. Also, remember that something that may seem easy to you may not be for others. You may have already progressed up the pyramid, and used scaffolding to make each transition to the next step even easier, while others have not. It is scaffolding that helped progress you through the various stages of Miller’s Pyramid (Figure 2). People new to hearing aids or new to their hearing health will need to make their own way up the pyramid while using best practice scaffolding as soon as possible to ease their transition to multi-step tasks/instructions.
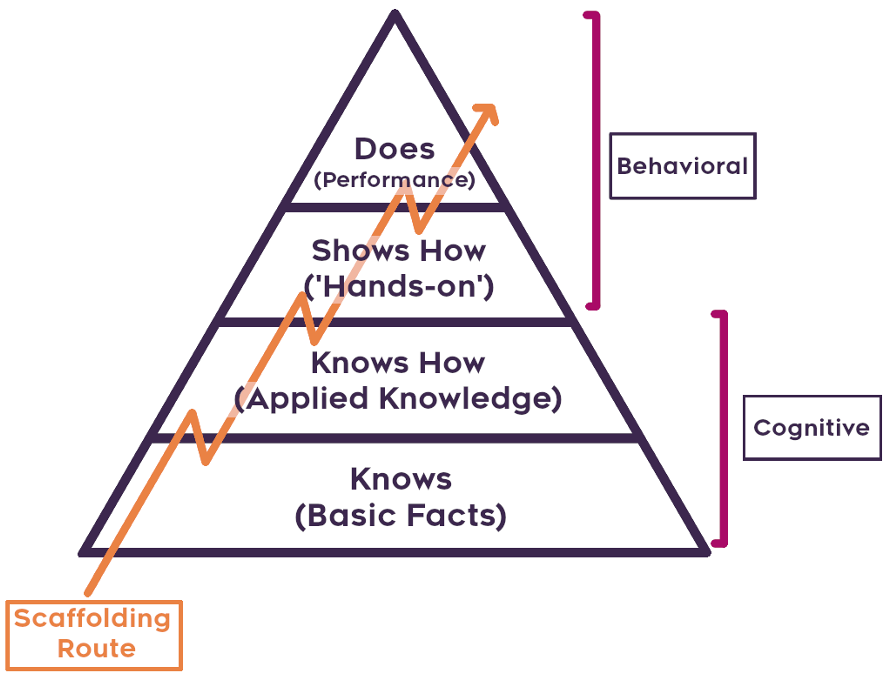
Figure 2. Visual illustration of the Scaffolding Model interacting with Miller’s Pyramid.
Applications to Hearing Healthcare
Hearing aids can bring many benefits to patients with hearing loss, but if patients are not given proper and effective instruction on their appropriate use, frustration and discouragement will ensue, and the hearing aids will end up in a drawer. There are several tasks that patients need to do in order to successfully utilize their hearing aids. Some of these tasks are quite complicated, and include multiple steps, tiny parts, and strengthened manual dexterity skills. Difficult patient tasks in audiology include putting hearing aids on, cleaning the filter and dome of a hearing aid, changing the batteries of a hearing aid, or using the hearing aid’s app and advanced features.
Let’s focus on one of these issues - hearing aid insertion. Seems simple enough to learn right? But, have you ever fit hearing aids on a patient with amazing day-of-dispensing results only to find them arrive at their one-month follow-up appointment with the hearing aids half sticking out of their ears and low data logging? You taught them how to properly insert a hearing aid into their ears, but it seems as though they completely forgot. Think about your approach when teaching this skill - Did you lecture and explain the proper way to put a hearing aid on, show the patient how you would put a hearing aid on your ear, then have the patient do it? Perhaps this approach expected the patient to sprint up Miller’s Pyramid, gleefully understand, and apply it immediately on their own.
I’m going to make a bold statement here: The most important part of a hearing aid dispensing appointment is properly teaching a patient how to put hearing aids on their ears. Real-ear measurements, fine-tuning, and programming is effectively useless if a patient cannot properly insert their hearing aids in their ears. Properly placing a receiver-in-the-canal hearing aid is a deceivingly difficult task. During this task, patients cannot directly see what they are doing, and they may even have dexterity issues or loss of feeling in their fingers. Remembering to implement both “Knows, Knows How, Shows How” and Educational Scaffolding can effectively guide patients to hearing aid success.
Below are a range of recommendations for how to implement these models at your clinic to facilitate greater hearing aid success. On the theme of scaffolding, it is not reasonable to assume that you and your clinic will overhaul your entire patient consultation right away - you will need to ease into it. Recommendation 1 is the easiest and simplest way to implement (Scaffold #1), while Recommendation 2 and 3 are the next step-up scaffolds to design a brand new patient experience all around effective patient education and making the most effective use of our time with the patient.
Recommendation 1: Uncovering the patient’s current level of understanding
Remember, we want to ease our patients up the pyramid while getting them hands-on (“Shows How”) as soon as possible. I often find that a generalized verbal explanation and a simple demonstration on how to put a hearing aid on is not enough. For most patients, this type of instruction is beyond their current comfort level and understanding of their hearing aid (zone of proximal development).
As a first step into this new model, you must learn where the patient’s current comfort level is. Do they understand the purpose of the hearing aid and what it’s doing (“Know”)? Do they know how to use it and handle it already (“Know How”)? Where are they currently on the pyramid? If you instruct at too high of a stage, learning is ineffective. If you instruct at too low of a stage, valuable clinical time is wasted and patients may get bored during the process.
This zone of proximal development will vary largely between someone who is a first time wearer and someone who is upgrading their hearing aid. This will also vary if you’re speaking with a loved one of a patient, or if you’re doing community outreach to teach individuals outside of your clinical appointments. No matter the scenario, the absolute best thing you can do here is to empathize with the individual, get on their level, ask questions, and listen. How can you best help them, considering their zone of proximal development today?
Recommendation 2: Get your patients hands-on by putting hearing aids on a model
Everyone has a display ear sitting around at a clinic, and while some are better than others, they all can be used as a prop ear to experiment on. Place a hearing aid on the ear. Place different styles of hearing aids on the ear. Give your patient the ear and the hearing aid and allow them to become comfortable putting the hearing aid in the prop ear (hands-on as soon as possible!).
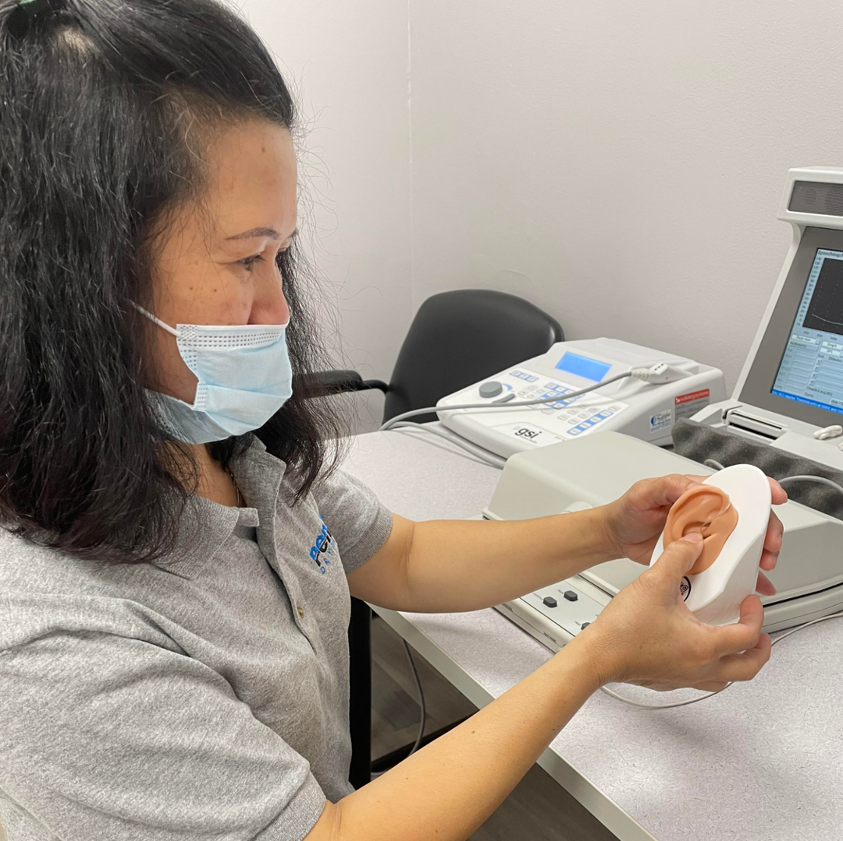
Picture 1. A patient using a prop ear to practice receiver-in-the-canal hearing aid placement.
A hand-held display ear model is a very useful tool. A patient is able to easily manipulate the prop ear, look at the hearing aid from different angles, and use different leverages to properly insert the hearing aid into the model. Using a realistic model ear is also very helpful in showing patients how an ear canal can change in shape depending on how the pinna is pulled or manipulated. The display ear is an excellent introductory scaffold for most patients. Mixing in some basic collaborative learning will also help them “Demonstrate to You” how they should insert the hearing aid in the ear, and where the hearing aid should be resting. Just like that, you completed your first scaffold.
The next step is getting your patient closer to placing the hearing aid in their own ear and walking out the clinic door. But is it reasonable to assume that jumping from a display ear to their own ear is ‘easing’ them into it, or is that still a big jump? Only you can answer that question after you have determined your patient’s new zone of proximal development. In my clinic, I find that most patients significantly benefit from an additional scaffold discussed below, with a difficulty level somewhere between a display ear and putting hearing aids onto their own ear.
Recommendation 3: Use Scaffolding with CARL!
It is important to remember that there are a different set of skills involved when placing a hearing aid on an ear model in comparison to in your own ear. I find an extra higher level scaffolding is beneficial and often needed to bridge this gap. For my clinic, that next scaffold has been CARL.
CARL is a head model from AHead Simulations that simulates both a head and ear model. While it is typically used for training the next generation of clinicians, I use it to train my patients! Here’s how CARL is the next best scaffold - CARL is attached to a desk and cannot be manipulated in space as the display ear can. CARL has a patient-specific ear model so the hearing aid will fit as close as possible to how it will fit on an actual patient. They can effectively view how they would be inserting a device in their own ear, in third-person.

Picture 2. A patient using a CARL head to practice receiver-in-the-canal hearing aid placement. Hearingbeyond.ca, own photograph.
Want to take it up one more notch? Put a mask on CARL. By doing this, the patient needs to see in third-person how a hearing aid interacts with a mask on CARL’s ear, and what it looks like to both insert and remove the hearing aid, as well as place and remove the mask. Is there a family member at the appointment as well? Get them to try it on CARL too to learn all the same skills! Now, how easy will it be for your patients to place a hearing aid on their own ear?
My Scaffolding Patient Experience with CARL
I have been executing this scaffolding approach in my clinic for approximately 12 months now and have heard nothing but positive things from my patients. Is this a result of the scaffolding, display ear, or the CARL? I am currently collecting data to try to determine just that - what is the impact of this new methodology on clinic results? I believe that this is the future in-clinic differentiation. This method offers an experience to users that is vastly more valuable and meaningful than just buying a hearing aid.
To summarize, the following teaching stages are what I find effective when instructing most patients on hearing aid insertion techniques:
Stage 1: I explain to the patient how to properly insert a hearing aid using a display ear.
Stage 2: The patient attempts inserting the hearing aid on the display ear, while I provide verbal guidance if required. I generally like to wait until the patient feels that they are done inserting the hearing aid before providing guidance, allowing for incidental learning. Periodically, a patient can benefit from verbal guidance during the process as an additional scaffold.
Stage 3: Remove the display ear as a scaffolding, and replace it with a CARL head. The patient then practices inserting a hearing aid on an ear that is not as easily manipulated as the display ear, but instead has similar challenges to their own ear.
Stage 4: Remove the CARL as a scaffold - now it’s the real deal. The patient places the hearing aid on their own ear using everything they’ve learned from the previous scaffolds. Once they do this without any problem, they have officially “Showed you How” they insert their hearing aid. If they have any questions or difficulties, you can re-introduce a scaffold again (the CARL head) to support and facilitate learning, then take it away and get them to apply that knowledge on themselves.

Picture 3. A patient inserting a receiver-in-the-canal hearing aid on her own ear correctly, after learning how to do this skill through scaffolding. Hearingbeyond.ca, own photograph.
A quick note on timing - this is not supposed to extend a consultation/time with patients. All these 4 steps can happen in a matter of 5-10 minutes.
As next steps, I would encourage you to think (or speak with your clinic team) about where your current zone of comfort/knowledge is with patient education. Have you thought about it before? Do you think about it every day? Only once you do this, can you look to improve.
With so many looming changes in the industry (which may or may not come to fruition), one thing can be for certain - providing a unique and tailored patient experience that emphasizes education first and utilizes these models will differentiate you and your practice better than any new technology.
References
Miller G. E. (1990). The assessment of clinical skills/competence/performance. Academic Medicine : Journal of the Association of American Medical Colleges, 65(9 Suppl), S63–S67. https://doi.org/10.1097/00001888-199009000-00045
Berk, L. E., & Winsler, A. (1995). Scaffolding children’s learning: Vygotsky and early childhood education (NAEYC Research into Practice Series, Volume 7). Washington, D.C.: National Association for the Education of Young Children.
Citation
Talarico, F. & Koch, R. (2022). Keeping hearing aids out of the drawer: emphasizing patient education to improve your practice. AudiologyOnline, Article 28146. Retrieved at https://www.audiologyonline.com



