This text course is not an original manuscript - it is a lightly edited transcript of a GSI webinar on AudiologyOnline. As the content was created for and intended for a webinar format, interested readers are encouraged to view the original webinar. This course was created for learning and educational purposes, and not for research purposes.
Learning Outcomes
After this course, participants will be able to:
- Describe the various types of auditory temporal processing.
- Outline clinical uses of auditory pattern perception procedures.
- Discuss clinical uses of Gaps in Noise procedures.
Temporal Processing
Temporal processing refers to the perception of time alteration or influence on an audible acoustic event(s). Most sounds, of course, are acoustic events. Temporal processing is important to everything we do as audiologists in terms of measuring hearing and responses to various kinds of acoustic stimuli. Temporal processing plays an even bigger role in more sophisticated listening tasks. There is both a peripheral and a central influence to temporal processing, more the latter as tasks get more complex. It is also the latter that will be focused on today.
Figure 1 shows the categories in which we'll find most of the central auditory tests that are available today.
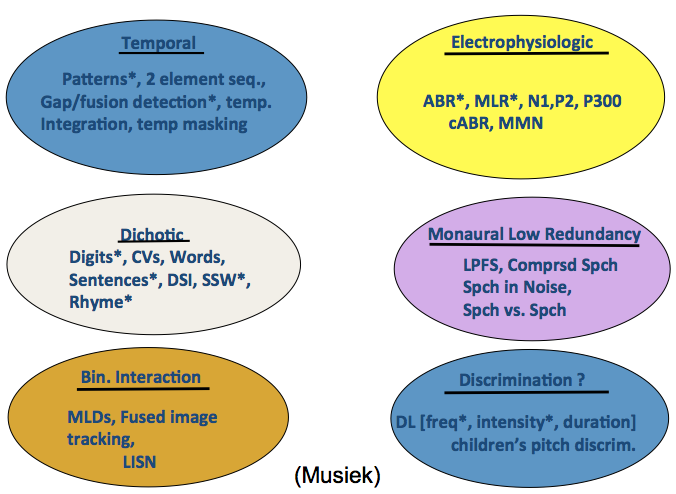
Figure 1. Central auditory test categories.
The ones on the left side are the procedures that I think give you the most information from a practical standpoint and also from a research standpoint.
Temporal processing tests are listed in the blue circle in the upper left. I believe conducting tests of temporal processing is one of the most important procedures we should do. Most people would agree that temporal processing procedures are important in evaluating the auditory system. These are the tests we'll discuss today.
Dichotic listening tests are also valuable, as are Binaural Interaction tasks, such as masking level differences, various kinds of localization tasks, spatial tasks and others.
Then we have the procedures in the second column of Figure 1. Electrophysiologic procedures can be of value, although they are not in routine use at this stage of auditory processing evaluations. In some cases electrophysiologic measures are critical, but the development in this area hasn't been quite as fast as we had predicted it would be. The Monaural Low Redundancy speech tests are possibly the oldest and the most ubiquitous tests. These include filtered speech tests, compressed speech tests, and speech-in-noise tests that are becoming routinely used. The newer procedures afford some facility and are better designed, but the underlying concept remains the same. The last category of central auditory tests are discrimination tasks. Although discrimination is an important area, there are essentially no tests that are commonly used in measuring either frequency discrimination, intensity discrimination, or duration discrimination. While there are certain labs that can and do test discrimination, tests are not available for routine clinical use; this kind of test is sorely needed.
Types of Temporal Processing
I like to categorize four kinds of temporal processing: integration, sequencing, resolution, and masking.
Temporal integration is quite simple - as one decreases the duration of the stimulus, it becomes more difficult to detect, especially below durations of 200 milliseconds. The duration of a stimulus influences threshold (or your detection). Hence, as one shortens the duration of a tone or noise burst until it is a very brief stimulus, it raises your threshold. The trade off between intensity and time (and threshold) is related to temporal integration (how sound energy is intergrated into the auditory system over time). One of the interesting tests that we'll discuss in this presentation is the brief tone frequency test (my term). The brief tone frequency test is a valuable test that was introduced a number of years ago, but unfortunately is not widely used by audiologists.
Sequencing (also called temporal ordering) and temporal resolution (such as Gaps in Noise) are the focus of today's talk.
Temporal masking refers to masking in time of a target stimulus. Temporally, it may be termed backward or forward masking of the target stimulus.
Clinical Value vs. Clinical Use: Brief Tone Frequency DLs
It's interesting to ponder as to why certain test procedures are embraced by clinicians, while other test procedures are not. Generally, the better tests are the most widely used, but that is not always the case. There have been some very good test procedures that simply haven't been utilized in the clinic, such as the temporal integration tests that look at brief tone frequency DLs (difference limen), which I termed "brief tone frequency test" earlier.
These tests show a different kind of temporal processing than what we're going to talk about today. Jerry Cranford introduced this type of test to measure brief tone thresholds. The basic procedure involves reducing the duration of the tone from about 500 milliseconds down to 20 milliseconds, and measuring how much the threshold shifts as a result. That, in and of itself, has been shown to be a fairly valuable test, but Cranford and colleagues added another task to it. They asked individuals to make a frequency discrimination between two short tones varying in duration or two long tones varying in duration. This turned out to be a sensitive procedure to central auditory involvement according to data from both animals and humans. The test was intended to be used clinically, but it never enjoyed widespread use.
Cranford used a control group and a compared them with a group of individuals with confirmed central auditory disorder (I think they were mainly stroke patients). He found a dramatic difference between the ability of these two groups to make a frequency discrimination between two tones that are relatively short. When the tones were longer, there was no difference between the two groups. This was very impressive work and I believe it is a valuable procedure to use in the clinic, but audiologists have not embraced it. Cranford's procedure shows one of the ways that temporal processing can interact with frequency. The central auditory system is an elegant time keeper, and one of the ways we can stress it is by making people listen to very short stimuli, or by asking them to do manipulations with those very short stimuli such as discriminating between two stimuli of different durations.
Auditory Patterns
Now let's talk about auditory patterns. I'm going to provide an overview of frequency patterns and duration patterns in clinical populations. Key processes that are involved in auditory patterns are temporal sequencing, which is a temporal process, and frequency discrimination, which is a spectral process.
The frequency discrimination part of the frequency pattern test, is not highly demanding (1122 Hz v. 880 Hz), but yet if a person has some disability in this regard, it may be a factor. Duration patterns don't have the pitch difference and therefore only duration is tested. It's important to note that while the two tests are similar in a lot of ways, they test slightly different processes.
These tests were developed many years ago by Marilyn Pinheiro, who was my mentor. Data from animal work done in the 1960s motivated Marilyn to initially develop these tests. Early in my career, we worked together to further refine these procedures, and to conduct clinical validity testing on both the frequency and duration pattern tests.
The frequency patterns are shown in Figure 2.
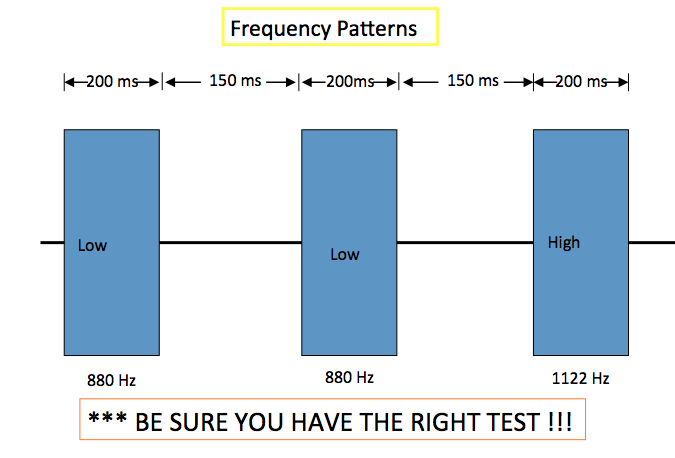
Figure 2. Frequency patterns. Source: Frank Musiek.
Figure 2 shows the duration, interstimulus interval and the change in frequency. There are a number of versions of this test, but the normative data and validity data are based upon the tests that we developed in the 1980s. I can't speak to any of the other versions in regard to normative data and validity, so it is important that you have the right test. You can see in Figure 2 that there are three distinct stimuli that vary in some way. There are six permutations of this pattern in the test; the pattern shown in Figure 2 is Low, Low, High. Low, Low, High is what the subject would report when they listened to these stimuli.
Duration patterns are shown in Figure 3. The duration pattern test may be a little bit more difficult than the frequency pattern test as you don't have the frequency cue, and that cue does make a difference in performance. Similar to the frequency pattern test, the duration pattern test has various permutations - in this case the permutations include short and long stimuli. For example, permutations include "Long, Long, Short," "Short, Short, Long," etc. The duration of the stimuli can be seen in Figure 3.
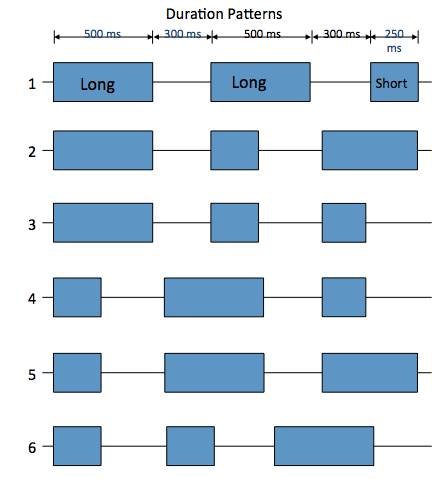
Figure 3. Duration patterns. Source: Frank Musiek.
Underlying Mechanisms for Pattern Perception
It's important to have an understanding of the underlying mechanisms for pattern perception. What does the auditory system have to do, what does the brain have to do, and what are some of the key functions involved for an individual repeat these patterns correctly? We could go into a lot of details about the different kinds of mechanisms at play, but for the purposes of today's course, I will just highlight a few. There are obviously many more but they are outside the scope of this talk (and time) of this talk (see 1980 article).
In auditory patterns, there are three main processes that happen: contour recognition, callosal transfer, and linguistic labeling.
First, the right hemisphere has to recognize the contour of the pattern. That's primarily a responsibility of the right hemisphere. The contour simply means the shape of the entire pattern - what does it look like as a whole (Gestalt processing)?
Once contour recognition occurs in the right hemisphere, it has to transfer that information across to the left hemisphere. Transfer takes place in the corpus callosum, which connects the two hemispheres.
The left hemisphere should maintain that information in a sequence so that it can be linguistically labeled. In other words, the left hemisphere, which is the speaking hemisphere, labels the pattern (such as "High, Low, High," etc.) once it is in the correct order and sequenced.
Pattern perception is likely the result of an interaction between the right hemisphere, the transfer that takes place in the corpus callosum, and then the sequencing and linguistic labeling that happens in the left hemisphere. For an individual to report this pattern correctly, all these things have to be intact. I will show you what happens when they're not intact later in the presentation.
Even though this is a monaural test, accurate pattern perception requires a number of processes to work accurately. The right hemisphere needs to be working, the transfer requires that the corpus callosum is working, and we need the left hemisphere working for linguistic labeling and sequencing, in order to verbally report the pattern correctly.
It's important to understand that when you administer this test, you have multiple things that need to function for accurate pattern perception, and therefore multiple things that could go wrong when people don't perceive the pattern. There is also an important cognitive aspect to pattern perception, but the cognitive aspect is dependent on these three (and other) auditory functions (see our 1980 article).
Site of Dysfunction and Interpretation
When people have difficulty with pattern perception, there could be a potential temporal processing problem. There are some general guidelines one can use for interpretation regarding the site of dysfunction. However, there are always exceptions and there are also multifaceted types of dysfunctions that involve many parts of the brain, so one cannot always isolate the issue. A general guideline is summarized in Figure 4.
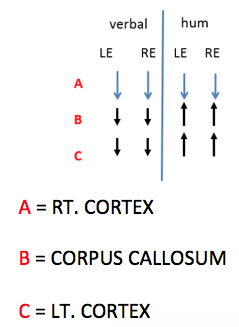
Figure 4. Site of dysfunction and interpretation. Source: Frank Musiek.
Right hemisphere lesion. If there were a lesion in the right hemisphere, what would you expect on pattern perception? As earlier research has suggested, you would expect abnormal function for pattern perception in both the left and right ears. It may not be symmetrical, but it would likely be abnormal in both ears. If you asked the person to hum the pattern, which we sometimes do, you would also find that the individual would be at a deficit. If the right hemisphere is intact, the individual can typically hum or whistle a response; aphasia research has shown some interesting findings in this regard.
A right hemispheric lesion that involves the auditory cortex or areas close to the auditory cortex, would likely show a bilateral deficit. Why? Because there isn't enough information for any of these other subsequent processes to utilize. Therefore, as we've reported many times, there often are bilateral deficits even when only one hemisphere is involved, due to the nature of the pattern perception task (as earlier explained).
Corpus Callosum lesion. If there is a lesion or some kind of dysfunction in the corpus callosum, the verbal report will be abnormal bilaterally, but they will be likely able to hum the pattern. Or, you will see a deficit for the verbal report and humming performance will be better (maybe not normal) than the verbal report. Why will humming be intact or better than verbal performance in the case of a corpus callosum lesion? As mentioned earlier, because the right hemisphere is intact and the right hemisphere can perform these processes (see 1980 article).
Left hemisphere lesion. In this case, the verbal report is affected. Why? The left hemisphere is the speaking hemisphere, and it is disrupted. Again, because the right hemisphere would be intact, humming performance would be better than the verbal report. When verbal report is poor, we often ask people to hum the pattern, if they can. Some can't simply because they are poor musicians, but we do try humming in cases where there is poor verbal performance to see if we can better localize the underlying neurological mechanisms based on our model.
Avoiding Common Errors: Administration of Pattern Perception Tests
- Verbal explanation. When administering Pattern Perception tests, it is important to give a good verbal explanation of what you are doing. In my opinion, this requires giving the explanation face-to-face in the soundbooth, especially for children and older adults. This is not a test that you can explain over the intercom of the audiometer as it can be easily misunderstood.
- Use the correct version of the test.
- Use visual cues with the voice patterns to teach patients how to take this test. For example, use your finger (or a marker, or another visual aid), along with voiced patterns to provide examples. Give plenty of examples to be sure the patient can follow along. Then, take the visual cue away, use your voice alone to mimic the patterns and see if they understand them. I can't emphasize enough how important this step is; a common error is not spending enough time to make sure that the patient understands the test and what they are to do.
- Practice items. There are practice items on the recording, but you should also provide the visual cues with voiced patterns just described, and not rely on the practice items alone.
- Monaural vs. binaural or soundfield. The test can be administered monaurally or binaurally, or in soundfield.
- Humming response. You can use a humming response, as discussed in the previous section.
- 30 test item minimum. A full test is usually a 30 test item minimum - however this is not the case for binaural/soundfield testing (we use 45 items for those conditions).
- Half lists. Half lists can be used - if the patient misses at least 14 out of 15, or get at least 14 out of the first 15 correct, you can stop the test because your results are not going to change the final determination of pass vs. fail.
- Sound field and diotic testing is sometimes used. In my opinion, it's not preferable, but it is usable. It is not as accurate as doing each individual ear, but it is probably close. More investigation is needed in this area to be confident in this application.
Scoring of Pattern Perception Tests
- Reversals are wrong. Reversals are wrong, and I don't understand why there is a misunderstanding on this as we have been saying this for 35 years. Reversals initially were not considered wrong in the early test days, but they are now. We've learned over the years that some peoples' only errors are reversals, and if they were counted correct, then they wouldn't fail the test even with severe problems. Everyone will miss a few items by reversing (even people without temporal processing issues - see Pinheiro & Ptacek, 1971), but reversals still have to be counted as incorrect and that is built into the norms.
- Extra element responses are wrong. For example, if the three elements are "Low, Low, High" and the patient says "Low, Low, High, High." In this case, even though the first three elements are correct, they added one so that is incorrect.
- Supplemented responses. Supplemented responses mean that the patient has some kind of (usually) motor response to try to help cue themselves as to what the pattern is. Some people will try to move their hands to help them figure out the pattern, others will tap their foot, etc. These supplemented responses cannot be permitted because they potentially can cross cue the individual to the correct response for the wrong reason.
- Musicians. Musicians do very well on pattern tests. In your patient history, find out if the person is a musician and take that into account as musicians will do extremely well on pattern perception tests. More research needs to be done on musicians to perhaps establish their own norms. (Early unpublished work by DeFosse and Pinheiro alerted us to this better performance by musicians but more work must be done in this area).
Children's Norms
Figure 5 shows norms for children. The variability of the procedure is quite high and that is built into these norms.
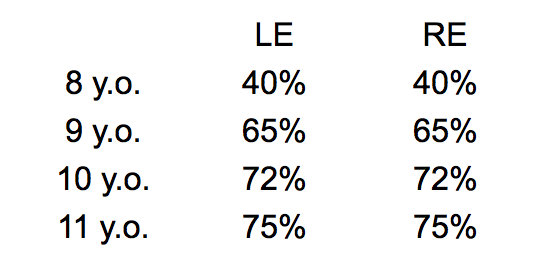
Figure 5. Frequency patterns: Children's norms (cut off scores). Source: Frank Musiek.
Significant Diagnostic Findings for Neurologically-Group Studies Using Pattern Tests
There have been a lot of studies on neurologically based groups, as well as on children with learning problems. I wanted to show you some of these references because they all show significant diagnostic findings. This is just an overview and not an exhaustive list. In these cases the subjects are neurologically involved and the tests are shown to be very sensitive; the test has some real potency for these populations.
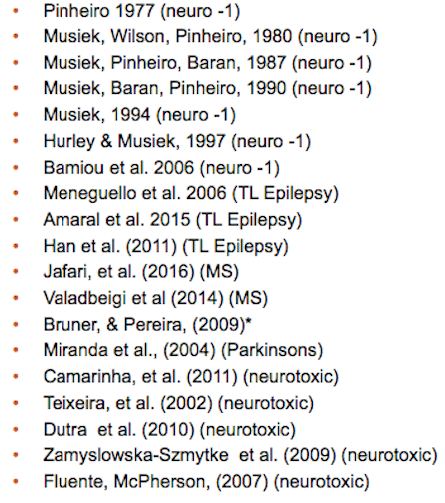
Figure 6. Selection of neurologically based group studies using pattern tests with significant diagnostic findings. Source: Musiek (2016).
Data from Hurley and Musiek (1997) show good sensitivity and specificity for the Auditory Duration Patterns Test. It is a valid procedure.
In addition, look at the data from Weihing et al. (2015) and Musiek et al. (1987), and do some interpolating, and the data tell a story. While caution is key, generally children with learning disabilities as well as people that have confirmed lesions of the auditory cortex, will show significant differences from control groups for frequency patterns.
As far back as 1982, when I was looking at frequency patterns in children with learning problems (Musiek, Geurkink, & Keitel, 1982). We found with a pediatric population, if they have language, learning and or listening problems, they often have trouble with frequency patterns.
If one does a literature search on "frequency patterns and children" or "frequency patterns, learning disabilities", you will find results from many studies. A few other key studies with interesting results on this topic are Dias (2005) and Engelmann & Ferreira (2009), and there are many more. There is a lot of evidence to demonstrate the value of pattern tests in children with learning problems.
In looking at different sites in the auditory system, we find that controls (normal auditory system), people with cochlear issues, and those with brainstem lesions or dysfunction perform reasonably well on frequency pattern testing. It's not until you test patients with cerebral lesions that one sees marked dysfunction on frequency pattern testing. This is, theortetically, because it is the cortex that perceives the whole pattern. At all levels before the cortex, it's not really perceived as a pattern but rather three successive tones. It's an interesting discussion that we don't have time for today but I wanted to mention this theoretical concept.
We did early work with split brain individuals, and found they could hum patterns but had difficulty with the verbal report. That's because of lack of transfer across the corpus callosum to the left hemisphere (the "speaking hemisphere") (see Musiek et al., 1984 for elaboration).
There are older studies looking at dyslexia and frequency patterns (King, Lombardino, Crandell, & Leonard, 2003; Walker, Givens, Cranford, Holbert, & Walker, 2006) as well as a relatively newer study from researchers in Poland (Lewandowska et al., 2013). These studies show that people with dyslexia likely have some auditory basis for their problem. Another key study on the topic of frequency patterns and dyslexia for historical context was done by Pinheiro back in 1977 (I think), and a few others show similar results are noted in recent reports.
Gaps in Noise (GIN)
The Gaps in Noise (GIN) test is a relatively new temporal resolution test. There are two main kinds of gap detection: within channel and between channel (Figure 7).
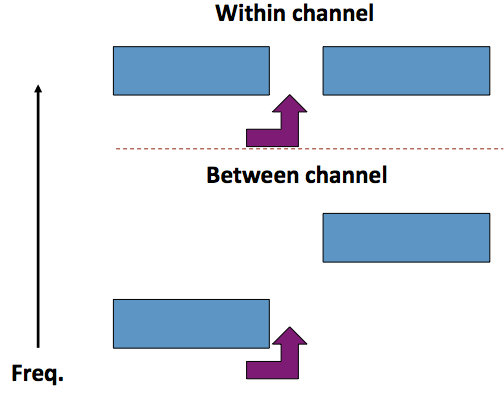
Figure 7. Gap detection - within channel and between channel. Source: Frank Musiek.
The procedure consists of a lead acoustic segment, a gap, and a trail stimulus. The lead element is a sound - it's usually a white noise but it can be tones. If the procedure is within channel, the trail stimulus is identical to the lead. If the procedure is between channel, then the lead and trail stimulus are not the same. A between channel task is much more difficult. I'm going to talk primarily about within channel today.
Why are the perception of "silent intervals", and transitions to and from silence important? These gaps are critically important for understanding speech and its related meaning. An example can be heard when you say these two sentences aloud:
- The ball was thrown by the quarterback.
- I want my quarter back.
The difference between those two "quarterbacks" is the interval between "quarter" and "back" - the gap is obvious in one but not in the other. Without good temporal resolution to perceive that gap in the speech, one may confuse the meaning of these two quarterbacks quite easily. This kind of procedure also provides insight into the temporal resolution of the auditory system, which I think is important for audiologists, regardless of what types of patients you see or the services you provide. Measures of temporal resolution provide valuable information about the auditory system, and may help us move away from just doing pure tone audiograms. I suggest looking at some of these other kinds of procedures in the general population, even if you aren't interested in the central auditory system. Gap detection can be reliably measured psychoacoustically, and now can be used clinically. It is also important to understand that noise fills gaps. When noise fills gaps, both in speech signals and in test signals, understanding becomes more difficult. Word recognition in noise is difficult because these gaps are filled. Speech perception in noise is not just compromised by noise masking the phonemes or the syllables, but also because noise fills in these gaps. As has been shown, without appropriate gaps, speech perception suffers (Snell & Frisina, 2000; Ceruti, 2015; and others).
The parameters of the stimulus that we use are shown in Figure 8.
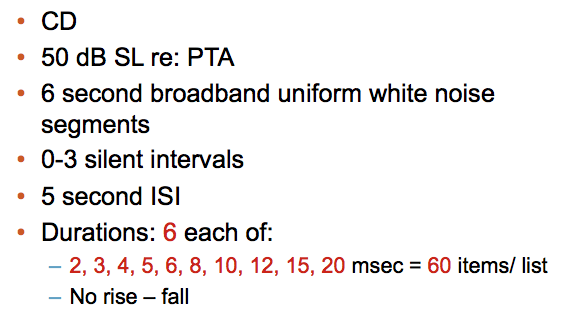
Figure 8. Stimulus for gap detection testing.
The test requires the person to listen to six seconds of broadband noise. It is pseudo-randomly interrupted (with some limitations) any time, any place, from zero to three times (0 - 3 silent intervals). The person simply reports every time they hear a gap.
Figure 9 shows examples of three stimuli. There is one gap in the first, two gaps in the second and none in the third.
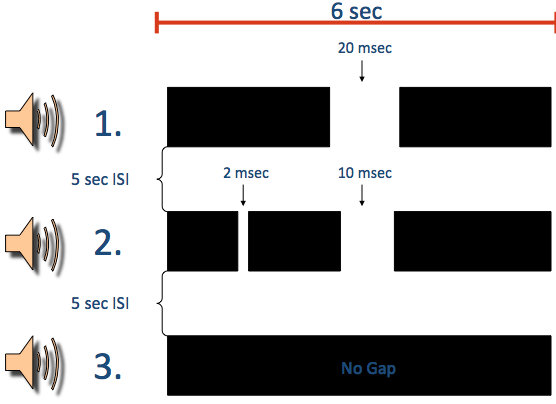
Figure 9. Examples of stimuli. Source: Musiek et al., 2005.
Scoring
The scoring is dictated by a score sheet that indicates the location of the gaps (when each gap occurs) and the duration of each gap.
Figure 10 shows how the scoring is totaled.
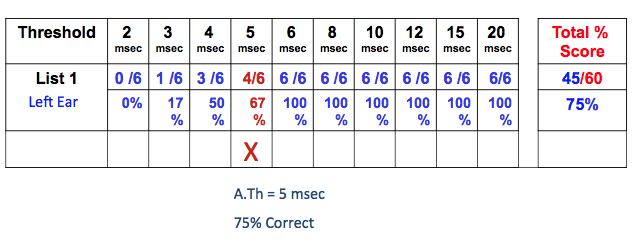
Figure 10. Scoring. Source: Frank Musiek.
When totaling your scores, there are two measures: a threshold measure and a total score. In Figure 10, the threshold measure is indicated by the red X. In this case, the person got four out of six correct (67%) at that particular interval (or gap), which is 5 msec long. Overall, they achieved a 75% correct (total score). The A.th, or approximate threshold score, is more sensitive and probably a little better measure, but the total score is useful and should not be ignored if it revelas a problem or normal findings.
Note: Our A.th criteria is reaching and maintaining 4 out of 6 correct at whatever gap duration (see Musiek et al., 2005 article).
Mechanisms
Physiologically, when people hear a simple gap in a continuous acoustic event, the whole neurological system from the periphery to the brain has to work synchronously. In other words, a critical amount of neurons must work together and be able to turn off and then turn back on synchronously within the time frame that the gap exists. Normal people with normal auditory systems can do this quite well. This is illustrated in Figure 11.
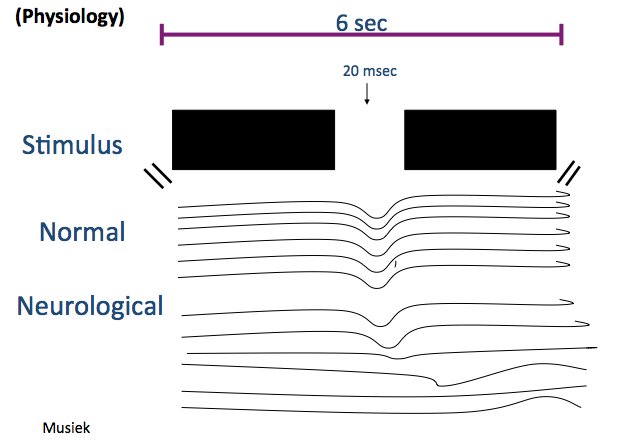
Figure 11. Illustration of neurons responding to gap. Source: Frank Musiek.
The illustration in Figure 11 shows that normal neurons (cartoon representation) respond quite well to both the width and the depth of the gap. They send this information to the cognitive system that says, "There's a change, something missing - there's a gap; there's a brief interval of silence." Then, the individual then can respond and say, "Yes, there's a gap." Patients that have damage to the central nervous system may have some neurons that respond appropriately to the gaps, but they will have many that do not, as illustrated in the figure. When some neurons do not respond to the gap, then the system is not sensitive enough to reliably and consistently detect the gap. Why? - because the neurons are not working synchronously. They may be damaged and too slow to respond, which is generally the case, or perhaps they do not respond at all. This simple stimulus, if controlled correctly, can provide us great insight as to the integrity of the central auditory nervous system.
GIN Normative Data Across Countries and Languages
Because the GIN procedure does not use a speech stimulus, rather, a noise stimulus, it is easy to compare results from research in other labs and across countries. Doris Bamiou's Lab looked at many studies in many different countries that spoke different languages, and found GIN scores were very similar. Their work will be published shortly. It is a testament to the consistency of this procedure across countries and across languages (see Figure 12).
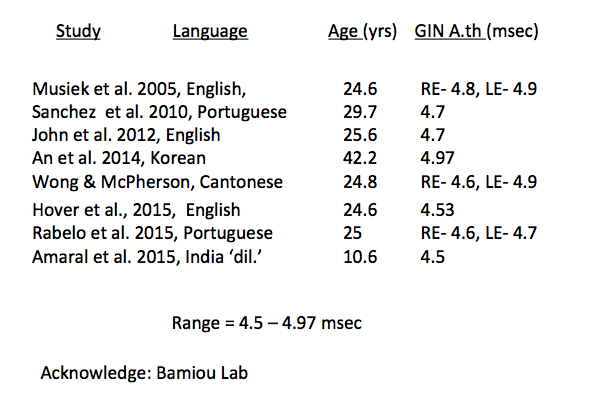
Figure 12. Preliminary normative data for GIN across countries and languages (Source: Bamiou Lab).
Maturation
The maturation curve of this test is different than most of the other tests we have worked with.
If you look at data from Shinn and colleagues in 2009, for 7-year-olds through 12-year-olds as compared to adults, you will see very little differences on the GIN procedure. There is greater variability for the 7-year-olds, however. There are also a lot of 6-year-olds that do this relatively well. Gap detection seems to mature at about age five or six. After that age, responses are similar to adults. Therefore, one doesn't have to be as concerned about a maturational curve with GIN, like we do with some of the other tests of central auditory function.
Blast Injuries
Erick Gallun and his colleagues at the National Center for Rehabilitative Auditory Research (NCRAR) at the Portland VA has done a lot of research on blast injuries. They have found that 63% of people with blast injuries report a moderate or severe hearing handicap. These same people had essentially normal pure tone audiograms.
Over a number of years they have looked at the performance of people with blast injuries on a number of tests of auditory function, including the GIN. The GIN and some of these other tests do pretty well in terms of detecting blast injury that may have affected the central auditory nervous system (CANS). The problem is that one never knows for sure if the auditory system has sustained blast injury damage because often the MRIs are essentially normal or don't confirm a site of damage. We know that people who have experienced blast injuries do have many difficulties, including auditory, and so measures are needed that will enable documentation of this. Gallun's group has found that nearly 50% of people with blast injuries show abnormal performance on some of these tests as compared to controls.
Sensitivity and Specificity
There are five major studies I would like to highlight to show you the sensitivity and specificity (or hit rate and false positive rate) of the GIN test. These studies were conducted for the most part with stroke patients and/or patients with some type of localized epilepsy where the lesions are reasonably defined (involving to some degree the auditory cortex or otehr central auditory areas). Observe the studies listed in Figure 13 along with their results plotted on the graph.
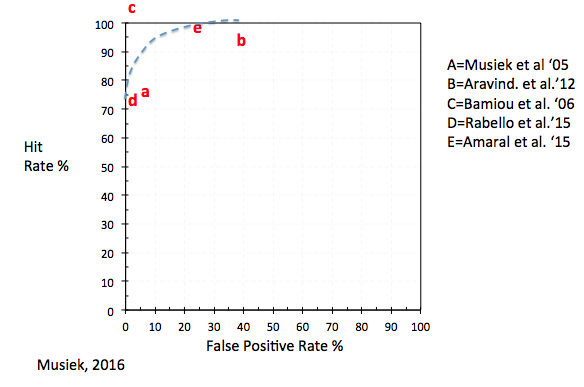
Figure 13. Preliminary data on test efficiency of GIN on patients with neurological based lesion. Source: Frank Musiek 2016 (data from studies listed in figure).
As you can see in Figure 13, the data show very good performance of the test in terms of hit rate and false positive rate.
Patients with Dyslexia
Based on recent reports, an important population of people who suffer from auditory (processing) disorders are those with dyslexia. I am very interested in using the GIN test for patients with dyslexia. While some audiologists use the test for patients with dyslexia, I am surprised that it does not have more widespread use with this population.
King, Lombardino, Crandell, and Leonard (2003) did an early study that showed that gap detection ability was quite different for dyslexics than for controls. Since that time there have been many more studies showing similar findings. I feel audiologists should try to cultivate services for people with dyslexia in their practices, however, so far this area has been generally overlooked by many audiologists.
Figure 14 is a summary of gap detection studies involving people with dyslexia.
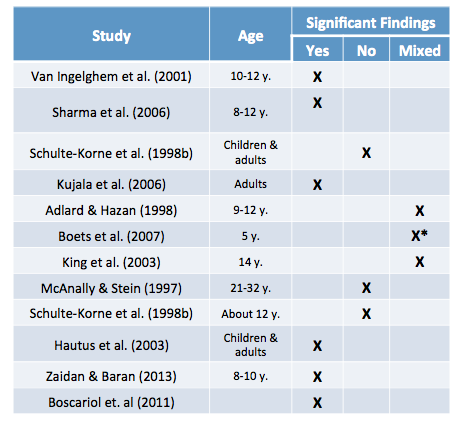
Figure 14. Gap detection-dyslexia studies.
While not all people with dyslexia have auditory-related problems, many of them do. Figure 14 shows which studies had significant findings and which had findings that were not significant. It can be seen that gap detection procedures do define children with dyslexia. It's an interesting population, and one that I think audiologists should look at carefully, if they haven't already.
Effects of Aging
There are many studies listed in your handout that show significant effects of age on gap detection or GIN procedures. As people grow older, their ability to perceive gaps may get worse. I feel this is because of such actions as demyelinization of the corpus callosum and in the primary auditory cortex. Elderly people do not do as well with gap detection tasks and that is likely one of the reasons they have trouble with speech perception - especially in noise (see Palmer & Musiek, 2014)
Audition and Cogniton
A common topic is the role of audition and cognition on these tests of central auditory processing. I'm not going to go into a lot of detail or breadth, but I will mention a recent study by Weihing and our group that was done at the University of Connecticut (Weihing et al., 2015). Central auditory tests did not show a strong correlation with WISC (Wechsler Intelligence Scale for Children) scores of various cognitive domains. I've summarized this in Figure 15.
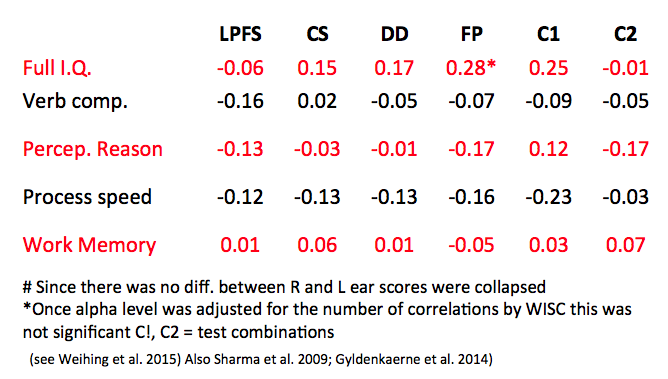
Figure 15. Pearson r values comparing the degree of association between CAPD tests and WISC scores.
Factor analysis shows there was a weak loading on frequency patterns but essentially little else in regard to central auditory tests and cognition. Thirty-five years ago we acknowledged that there was a component of cognition in central auditory processing, and that all hearing has a necessary component of cognition, but it's not what is mainly driving central auditory processing. Based on Weihing and associates (2015), one cannot explain the variance of these CAPD procedures by any of these particular subcomponents of cognition. In my view, cognition plays an important role in central auditory processing but it is not the driver. I believe that the role of cognition in central auditory processing has been a bit overstated over the past few years without a clear understanding of what is really happening in CAPD.
Future Directions
Temporal processing is absolutely critical to hearing. We need to move from simply using tests that measure detection ability at threshold to tests that are suprathreshold, and to those that measure something other than detection. We have a paper coming out entitled, Perspectives On the Pure Tone Audiogram. In that paper, we discuss the problems with looking at just a pure tone audiogram. I think one future direction is for audiologists to start integrating measures of temporal processing into their clinical armamentaria.
In addition, today we've seen how temporal processing measures can be used with various clinical populations. I think audiologists should be looking at how we can better serve these populations in our practices. The hearing aid area of our scope of practice is being disrupted by many different forces. As Jim Jerger related in a recent editorial, we really need to get back to strengthening our diagnostic abilities as audiologists. I think this is one of the ways we can begin to do that.
Another future direction is measuring gap detection electrophysiologically for patients who cannot reliably complete a behavioral gap detection procedure. Shannon Palmer and I published a paper on this topic in 2013. We recorded the N1-P2 responses to gaps in broadband noise in normal hearing young adults (Figure 16). We found that a two millisecond gap does not yield an evoked potential nor is this gap behaviorally detected. However, if the the gap is increased to 8+ msec, a low amplitude evoked potential is observed, and then if lengthened to 20 milliseconds, a large evoked potential response emerges. I think this opens up some very interesting ways of looking at these tests.
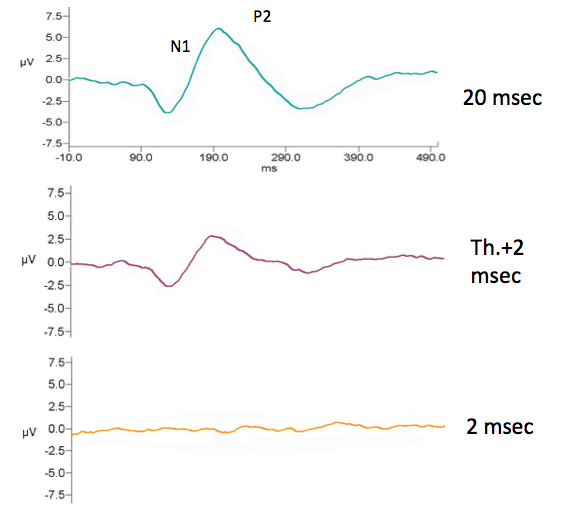
Figure 16. N1-P2 responses to gaps in broadband noise in young adults with normal hearing. (Source: Palmer & Musiek, 2013).
Shannon and I published another study in 2014 that compared the gap detection thresholds behaviorally and electrophysiologically in young adults and older adults, all who had essentially normal audiograms. When observing the grand average of these procedures, comparing the young adults to the older adults, one sees the same thing behaviorally that you do electrophysiologically. The N1-P2 is bigger, a little earlier, and is better formed in young adults, compared with the old adults. These are indications of a direct correlation to central auditory deficits, in regard to gap detection measured electrophysiologically. I think this is interesting and a definite move in the right direction for the advancement of audiology
Another interesting area in terms of future directions is recent work by Julianne Ceruti. Julianne did this work as part of her doctoral dissertation at the University of Connecticut (Ceruti, 2015). She did an interesting thing - she started to fill in gaps. This is referred to as partially-filled gap detection or decrement detection. When you fill in gaps, it clearly affects the person's ability to detect the gap. This strongly correlates to what happens to speech when you are hearing speech in noise. The natural gaps are filled in, making speech perception much more difficult. I think that partially-filled gap detection could very well be an advance in terms of identifying different kinds of hearing in noise problems (Figure 17).
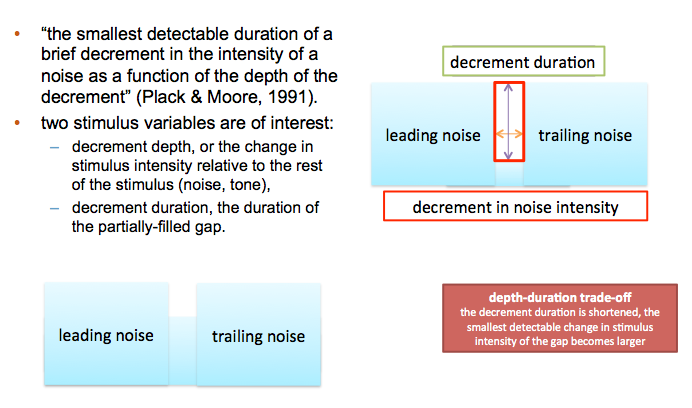
Figure 17. Partially-filled gap detection aka decrement detection. Source: Ceruti, 2015.
Up until recently, the width of the gap was examined, but the depth for the most part, had not. Depth of the gap also plays an important role that I think can be eventually be developed and categorized as a distinct measure. Another interesting part of Julianne's work (on filling gaps with noise) was the finding of a depth-duration trade-off. That is, if the gap duration is made shorter, its perception becomes more difficult, but this can be offset by making the gap deeper (into the noise) and vice versa. There is much to be learned here.
I think partially-filled gap detection is an interesting area of research. We'll be doing more work in the future to refine and use this procedure.
Questions and Answers
What specific test would you include to help with hearing aid dispensing decisions?
Good question. We've thought about this one a lot. There have been a few studies, at least one or two, that have addressed this. First you would want to rule out, in the quickest way possible, some kind of unusual or highly significant central auditory dysfunction. Spending 3.5 minutes to do a dichotic listening procedure, like dichotic digits, would be very valuable in this situation. If you see asymmetry that cannot be explained by the audiogram, it may help inform your decision for which ear to amplify, or perhaps even the kind of hearing aid. Also, remember that gap detection has a attack decay time, just like hearing aids have attack decay time that may vary. It would be interesting to see how people perform with their hearing aids on in terms of detecting gaps, especially people wearing compression hearing aids. Jeff Weihing and I once did the Dichotic Digits Test (DDT) on all hearing aid patients; I think we tested 72 consecutive people coming in for hearing aids. We were really amazed. Even though they had hearing loss, most showed relatively symmetrical performance. However, there were a few who showed a large difference on the DDT even though their audiograms were essentially symmetrical. I think it's a suprathreshold measure that tells you more than the pure tone audiogram.
What specific treatment options would you recommend for your clients with gap detection issues?
It's very simple. You would work on all kinds of temporal resolution procedures, including gap detection itself. For example, use the Cole-Jaminik words, which are what I showed you earlier with the quarterback v. quarter back example. There are hundreds of those. Work on discriminating speech signals and non-speech signals, and control the duration of the gaps or intervals of silence. Develop a systematic, high-intensity auditory training procedure for individuals both with and without hearing aids, and for those with and without either peripheral or central involvement. Doing a variety of temporal resolution tasks is important. You could also include localization, as localization is a form of a temporal task.
References
Ceruti, J.M. (2015). Behavioral and electrophysiological detection of partially filled gaps in noise. Doctoral Dissertations, 882. Retrieved from:
https://digitalcommons.uconn.edu/dissertations/882
Engelmann, L., & Ferreira, M.I.D.C. (2009). Auditory processing evaluation in children with learning difficulties (article in Portuguese). Rev. Soc. Bras. Fonoaudiol, 14(1), 69-74.
Hurley, R. M., & Musiek, F. E. (1997). Effectiveness of three central auditory processing (CAP) tests in identifying cerebral lesions. Journal of the American Academy of Audiology, 8(4), 257-262.
King, W.M., Lombardino, L.J., Crandell, C.C., & Leonard, C.M. (2003). Cormorbid auditory processing disorder in developmental dyslexia. Ear and Hearing, 24(5), 448-456.
Lewandowska, M., Ganc, M., Wlodarczyk, E., Senderski, A., McPherson, D.L., Bednarek, D., & Skarzynski, H. (2013). Central auditory processes predict reading abilities of children with developmental dyslexia. Journal of Hearing Science, 3(2), OA30-40. DOI: 10.17430/889538
Musiek, F., Baran, J., & Pinheiro, M. (1990). Duration pattern recognition in normal subjects and patients with cerebral and cochlear lesions. Audiology, 29, 304-313.
Musiek, F., & Chermak, G. (2014). 2nd Edition handbook of central auditory processing disorder, Vol. I: Auditory neuroscience and diagnosis. San Diego, CA: Plural Publishing.
Musiek, F.E., Geurkink, N.A, & Keitel, S. (1982).Test battery assessment of auditory perceptual dysfunction in children. Laryngoscope, 92, 251-257.
Musiek, F., Gollegly, K., & Baran, J. (1984). Myelination of the corpus callosum and auditory processing problems in children: Theoretical and clinical correlates. Seminars in Hearing, 5, 231-241.
Musiek, F.E., Pinheiro, M.L., & Wilson, D. (1980). Auditory pattern perception in split-brain patients. Arch Otolaryngol. Head and Neck Surg., 106, 610-612.
Musiek, F. E., Shinn, J.B., Jirsa, R., Bamiou, D.E., Baran, J.A., & Zaida, E. (2005). GIN (Gaps-In-Noise) test performance in subjects with confirmed central auditory nervous system involvement. Ear and Hearing, 26(6), 608-618.
Palmer, S.B., & Musiek, F.E. (2013). N1-P2 recordings to gaps in broadband noise. JAAA, 24(1), 37-45.
Palmer, S.B., & Musiek, F.E. (2014). Electrophysiological gap detection thresholds: effects of age and comparison with a behavioral measure. JAAA, 25(10), 9999-1007. doi: 10.3766/jaaa.25.10.8.
Pinheiro, M. (1977). Tests of central auditory function in children with learning disabilities. In R. Keith (Ed.), Central auditory dysfunction (pp 223-256). New York: Grune & Stratton.
Pinheiro, M.L. & Ptacek, P.H. (1971). Reversals in the perception of noise and tone patterns. JASA, 49, 1778-1782.
Shinn, J. B., Chermak, G. D., & Musiek, F. E. (2009). GIN (Gaps-In-Noise) performance in the pediatric population. JAAA, 20(4), 229-238. - See more at: https://www.audiologyonline.com/articles/overview-central-auditory-processing-disorders-782#sthash.rfuSHB4F.dpuf
Snell, K.B., & Frisina, D.R. (2000). Relationships among age-related differences in gap detection and word recognition. JASA,107(3),1615-26.
Walker, M.M., Givens, G., Cranford, J., Holbert, D., & Walker, L. (2006). Auditory temporal processing and brief tone discrimination by children with reading disorders. Journal of Communication Disorders, 45, 598-605
Weihing, J., Guenette, L., Chermak, G., Brown, M., Ceruti, J., Fitzgerald, K., Geissler, K., Gonzalez, J., Brenneman, L., & Musiek, F. (2015). Characteristics of pediatric performance on a test battery commonly used in the diagnosis of central auditory processing disorder. JAAA, 26(7), 652-669.
Further references in handout.
Citation
Musiek, F. (2017, June). Introduction to temporal processing, its applications to CAPD, and other aspects of neuroaudiology. AudiologyOnline, Article 20238. Retrieved from www.audiologyonline.com

