Editor’s Note: This text course is an edited transcript of a live seminar. Download supplemental course materials.
Dr. Bankaitis: Today’s presentation is Infection Control and Why Audiologists Need to Care. From my experience, it is necessary to establish a foundation of why infection control is relevant to audiology. Without this appreciation, it is much harder to implement infection control principles. The goal of today’s presentation is to review necessary information that will enable you to answer the following three questions:
- What is infection control?
- Why should we, as audiologists, care?
- How do you initially prepare to create and implement an infection control plan in your clinical practice?
There is a second infection control course that accompanies this presentation, which focuses on what to do and how to do it.
What is Infection Control?
What do we mean by infection control? As defined by Bankaitis and Kemp (2003; 2004), infection control refers to the conscious management of the clinical environment for the specific purposes of minimizing or eliminating the potential spread of disease, regardless of how remote that possibility may seem. This is a very straightforward definition, and as a result, clinicians tend to jump quickly to the conclusion that integrating an infection control plan will be equally as straightforward. While creating and implementing an infection control plan is not rocket science, it is a process that involves conscious management of the clinical environment. Infection control is a very intentional process that requires thinking through clinical procedures and assessing how those procedures may need to be modified to minimize the potential spread of disease.
It is usually at this point where you, as the audiologist, can become very quickly frustrated. You are suddenly forced to think through clinical procedures that have otherwise become so automatic. In addition, there is a tendency to overthink the process to the point where you conclude that the only way to achieve infection control goals is to wear a HAZMAT suit to work. Once you get to that point, the path of least resistance naturally leads us to abandoning infection control efforts and to erroneously perceive them as unnecessary. The good news is this infection control roller coaster is a natural progression of the learning process. Hopefully, with the information that is covered in Part 1 as well as Part 2, you will have the necessary information and tools to create and integrate an effective infection control plan in your practice with minimum frustration.
Why Should you Care?
Now that we know what we mean by infection control, the next logical questions to ask is, “Why should you care?” To answer this question, we first need to acquire a basic understanding of a few things, including the immune system and how it works and human immunodeficiency virus (HIV) and how it affects the immune system. We need to take a step back to recognize the lessons that we learn from HIV. Finally, I want to share how all this information applies to the audiology setting.
The Immune System
Starting with the immune system, human beings are continually challenged by microorganisms readily found throughout the environment as different bacteria, viruses, and parasites, vigorously pursuing a resource for growth and reproduction. As such, it is the job of the immune system to defend and protect us from these microorganisms. The immune system is comprised of two major subsystems, the natural immune system and the adaptive immune system.
Natural Immune System
The natural immune system provides the first line of defense against any type of microorganism, and it is represented by a variety of physical barriers, such as cells and soluble factors that react to all infectious agents in the same way each and every time, without any regard to the structural or chemical property of the agent. For example, your skin serves as a preliminary barrier to any kind of microorganism, regardless if it is bacterium, a virus, a parasite, or fungus. Because the natural immune system responds in such a nondiscriminatory fashion, it provides us with what are referred to as non-specific immune responses. Although relatively effective, the non-specific immune responses generated by the natural immune system are not foolproof, and as a result, we significantly rely on the adaptive immune system to defend and protect us from infection.
Adaptive Immune System
The adaptive immune system is a bit more complex as it involves the meticulous recognition of antigen. Antigen refers to any substance or molecule that the adaptive immune system interprets as foreign. When the adaptive immune system detects the presence of antigen, it calls upon different groups of immune cells to do very specific things. As such, the adaptive immune system generates specific immune responses. We are going to dissect some of these specific immune responses, but we need to go over some general anatomy first.
Anatomy of the Immune System
The organs of the adaptive immune system are positioned throughout the body, and they include a number of organs, such as the bone marrow, the thymus, the lymph nodes, et cetera. The bone marrow refers to the soft material that is found within the hollow shaft of bone, while the thymus is a very small butterfly-shaped organ that is located slightly above the heart. Both the bone marrow and the thymus are locations where these specialized immune cells of the adaptive immune system develop and mature. Once these immune cells develop and fully mature, they assemble in the lymph nodes, which are located in the neck, armpit, abdomen, and groin regions. While the immune cells of the adaptive immune system mainly congregate in the lymph nodes, they do continually mobilize throughout the body via two interconnected systems. These two systems are the lymphatic system and the blood stream.
Lymphatic System
The lymphatic system is a network of vessels responsible for channeling the clear tissue-bathing lymph fluid to the lymph nodes. As the lymph fluid is channeled to the lymph nodes, the lymph nodes work like filters to determine if there is any antigen present. From the lymph nodes, the lymph fluid is directed to flow towards the chest where it empties into the blood stream by way of the thoracic and lymphatic ducts. Once liberated in the blood stream, the lymph fluid is eventually reabsorbed by the bodily organs and tissues, and the lymph fluid is once again re-directed to flow through the lymphatic system. In other words, immune cells of the adaptive immune system are designed to continuously flow throughout the body. As a result of these connections, an immune response that is generated at one specific area of the body will ultimately be communicated throughout its entirety. It is a very beautiful system. However, these connections do serve as a double-edged sword.
Because of these very same connections, if appropriate infection control protocols are not implemented and followed, what we do as audiologists, at the level of the patient’s ear, cannot only affect the health of the ear locally, but given the right conditions, can affect the health of our patients systemically. This is a very critical concept to appreciate and recognize, because it drives home the point that what you do or do not do, from an infection control perspective in your clinical practice, can certainly impact the health of your patients.
Blood Stream
Immune cells of the adaptive immune system also continually mobilize via the blood stream. Blood is comprised of two distinct cell populations. Erythrocytes are more commonly referred to as red blood cells. The second group is called leukocytes, or more commonly referred to as white blood cells. The category of white blood cell pertinent to today’s discussion is the lymphocyte. Lymphocytes are a special group of white blood cells that are responsible for executing and managing all the activities of the adaptive immune system. The two types of lymphocytes that we are going to focus on today include the B-cell and the T-cell lymphocyte.
B-cell lymphocytes. Let’s start with the B-cell lymphocyte. The B-cell lymphocyte develops and fully matures in the bone marrow. An easy way to remember this is that bone marrow starts with the letter B, which is why they are referred to as B-cells to begin with. The job of the B-cell is to recognize the presence of antigen. Once the B-cell recognizes the presence of antigen, the B-cell is triggered to mass-produce an antigen-specific antibody and then to send that antibody throughout the body’s fluids so that the antibody can neutralize and kill the antigen. Figure 1 gives a crude representation of what happens in this process.
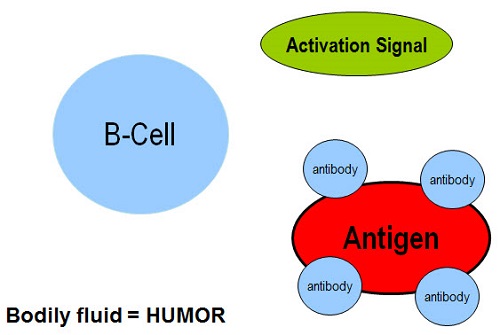
Figure 1. B-cell activation to an antigen.
The red oval in Figure 1 represents the antigen. The big, bad B-cell comes in and detects the presence of antigen. Even though it detects the presence of antigen, the B-cell needs to be triggered. It needs to receive an activation signal before it can do anything. Once the B-cell receives the activation signal, it starts mass-producing antibody and sends it throughout the body’s fluids so that the antibody can attach to the antigen, and then neutralize and kill the antigen. Another term for bodily fluid is humor. This entire process is referred to as humoral immunity.
T-cell lymphocytes. All T-cells initiate their development within the bone marrow. However, in order for a T-cell to become a T-cell, it must pass through the thymus where it fully matures. An easy way to remember this is that thymus starts with the letter T; this is probably why they are called T-cells. There are several different categories of T-cells, but we are going to focus on the CD-4 T-cell. The CD-4 stands for cluster designation 4. It is a very scientific way to refer to the unique suction-cup-like receptors that are found on that outer surface of this cell. Like the B-cell, the job of the T-cell is to detect the presence of antigen. However, unlike the B-cell, the T-cell is responsible for destroying the antigen.
In the presence of antigen, the T-cell not only recognizes its presence, but also attaches itself to the antigen, where it then neutralizes and kills the antigen. This process (Figure 2), whereby the T-cell attaches itself to the antigen, is referred to as cell-mediated immunity.
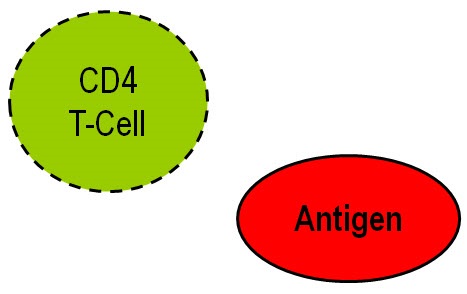
Figure 2. T-cell activation to an antigen.
Let’s put these two visual concepts together to get a better appreciation of what happens (Figure 3). Both the B-cell and the T-cell come in. Both recognize the presence of antigen. At this point, the CD-4 T-cell is able to attach itself to the antigen. In the meantime, the B-cell will sit dormant until it receives an activation signal from the CD-4 T-cell. The CD-4 T-cell sends the signal to the B-cell that says, “You need to start producing massive amounts of antigen-specific antibody.” The B-cell then does that and sends the antibody throughout the bodily fluids. That is how the B-cell and the CD-4 T-cell work together in order to neutralize and kill the antigen.
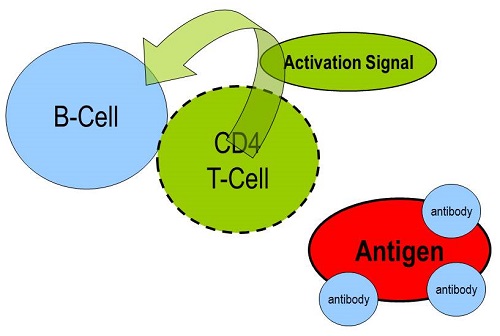
Figure 3. Cell-mediated immunity via B-cell and T-cell mobilization.
HIV
Now that we understand how the healthy, intact adaptive immune system works, let’s look at what happens in the presence of HIV. HIV is the virus that causes Acquired Immunodeficiency Syndrome, or AIDS. Unfortunately, HIV mainly targets the CD-4 T-cells. By saying that, you can already visualize in your head what happens in this specific patient population to their overall immunity. Figure 4 provides a visual representation, with a red square acting as HIV. The big, bad B-cell comes in. It recognizes the presence of HIV and just sits there. Unfortunately, since the virus attacks CD-4 T-cells, whether it is because there are not enough CD-4 T-cells or whether it is because the CD-4 T-cell is too weak to generate an activation signal, the individuals infected with HIV lose their cell-mediated and humoral immunities because the B-cells cannot be activated. This patient population becomes extremely susceptible to infections, including those that are caused by ever-present microorganisms that we tend to take for granted.
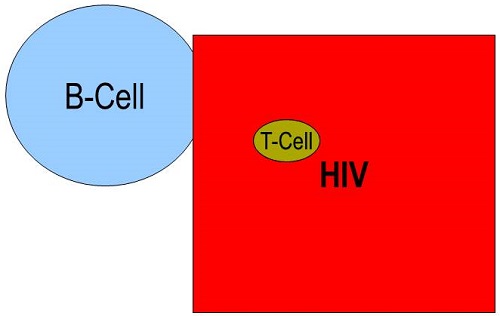
Figure 4. Representation of HIV attacking and destroying the T-cells.
HIV served as the disease to teach us many lessons about infection control, and in my mind, probably the three most important lessons for us as audiologists. Lesson #1 was learned early on in the 1980s. HIV was the catalyst of change when it comes to infection control. With the discovery of HIV, the concern for cross-contamination resulted the Occupational Safety and Health Administration (OSHA) and other regulatory bodies enacting regulations that provided healthcare workers with guidelines on how to reduce or eliminate the risk of exposure to infectious agents. Although the risk of transmitting HIV in the audiology clinic is extremely rare, HIV transformed how healthcare and medical professions approached infection control.
Lesson #2 became evident in the early 1990s, when it became obvious that audiologists were indeed providing services to HIV-positive and AIDS patient populations, both knowingly and most of the time unknowingly. Here is why. The HIV/AIDS population is prone to developing various types and degrees of hearing loss. Quantifiable audiological changes can occur either as a direct or indirect consequence of HIV. In terms of direct effects, HIV maintains a preferential affinity to the central nervous system, with nearly 100% of manifestations involving the areas of the head and neck. Considering the extensive representation of the auditory system through these regions, auditory manifestations are to be expected, and they have been consistently documented throughout the literature. Furthermore, ototoxicity and opportunistic infections are two examples of how HIV may indirectly cause hearing loss and balance issues.
With regard to ototoxicity, in the absence of a vaccination, the medical management of HIV relies on numerous pharmacological interventions that incorporate both FDA-approved and experimental antiretroviral medications. Furthermore, HIV-infected individuals are additionally prescribed medications as a prophylaxis or treatment of opportunistic infections. Many of these drugs are known to cause hearing loss, tinnitus, dizziness, and decrease in hearing. This patient population is also extremely susceptible to opportunistic infections that are known to be associated with hearing loss. Opportunistic infections originate from very commonplace organisms that do not typically cause disease in those with intact immune systems. Rather, these microorganisms take the opportunity to infect a body that is exhibiting some degree of immunocompromise.
Figure 5 lists the most common opportunistic infections contracted by HIV infected individuals. These infections are independently known to cause varying forms and degrees of hearing loss. While this table is summarized from a 1996 publication (Bankaitis, 1996), the information remains relevant even to this day. What we learned as audiologists in the 1990s was that the HIV-infected patient population remained extremely susceptible to developing hearing loss and vestibular disorders. Audiologists were and will find themselves in a position where they will be providing services to HIV-infected patient populations.
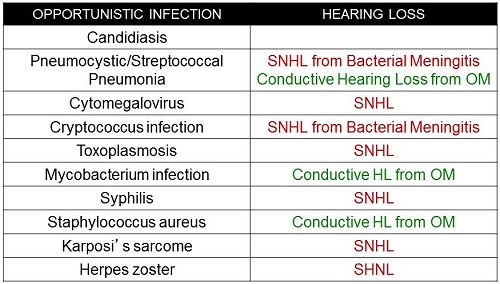
Figure 5. Summary of opportunistic infections that are known to be correlated with hearing loss.
We are no longer living in the 1990s. The third and likely most important lesson we learned from HIV is the one that must resonate with all of you from this point forward. Audiologists are exposed to various microorganisms other than HIV, as well as various immunocompromised individuals other than those infected with HIV. This brings home the following critical point.
Infection control is NOT about keeping you and your patients safe from HIV. There are many other microbes readily found throughout the audiology clinic and on hearing instrument surfaces that you need to be more concerned about. For example, audiologists are routinely exposed to various microorganisms that put us at risk for potential exposure to hepatitis B, which is a very resilient virus that can survive for at least week in dry blood at room temperature on floors, tables, and other hard surfaces. Other microorganisms, such as various forms of Candida, the 30 or so different strains of Staphylococcus that are ubiquitous, as well as Pseudomonas, are all of concern. The recent outbreak of Methicillin-Resistant Staphylococcus Aureus (MRSA) serves as an additional reminder to us of the importance and relevance of infection control in the clinical environment.
MRSA is a type of bacterium that is resistant to certain antibiotics including methicillin, penicillin, and amoxicillin. In the past, this genetic mutation of Staphylococcus was typically manifested as a nosocomial, or hospital-acquired, infection. Unfortunately, it has found its way into the general population. Just like in the 1980s, when HIV seemed to pop out of nowhere, many now ask, “What do we need to do differently now that MRSA is here?” The answer to this question may surprise you, but, truthfully, it is nothing different than what you should be doing for infection control anyway.
Just as there are other microbes to be concerned with in audiology clinics, there are many other patient populations who remain susceptible to opportunistic microorganisms. As audiologists, we provide services to a wide range of patients, many of whom exhibit varying degrees of immunocompromise that may or may not be overtly evident. Geriatric patients, as well as pediatric patients under the age of two, are automatically considered immunocompromised based on the factor of age alone. Diabetic patients exhibit varying degrees of immunocompromise, as do patients undergoing or who have undergone chemotherapy or radiation, and those taking certain medications. The list goes on and on. The bottom line is that we provide services to patient populations that are vulnerable to common microorganisms residing in abundance throughout the clinical environment, making it much more critical to implement effective infection control procedures.
Why Should We Care?
Let’s go back full circle and answer the question of why we should care about infection control. First and foremost, infection control is a federal mandate. In other words, it is the law. OSHA is the federal regulatory body that is responsible for overseeing the implementation of safety procedures in the workplace, and infection control falls under that umbrella of safety in the workplace. OSHA has issued specific guidelines on how to reduce exposure to potentially infectious agents. Audiologists are legally and ethically obligated to uphold these established, federally mandated infection control standards. These requirements also apply to students, because students are not exempt from infection control protocols and requirements.
Second, audiologists come in contact with bodily fluids and substances on a daily basis during routine procedures. For example, cerumen is a bodily substance that is considered infectious when it is contaminated with blood, blood by-products, ear drainage, pus, et cetera. Given the color and viscosity of cerumen, the audiologist is not in a position to determine with any predictable accuracy whether or not cerumen is contaminated with any of these things. As a result, we need to treat cerumen as a potentially infectious bodily substance.
Third, the audiologist comes in contact with numerous patients and reusable objects throughout the day. This is an issue of concern since multiple contacts inherently increases the potential for disease transmission to occur.
Microbial Transmission
In order for a microbial transmission to occur, two main things need to happen at the level of the outside environment. A microorganism requires a mode and a route of transmission. Mode of transmission refers to how a microorganism travels from point A, which is somewhere in the clinical environment, to point B, which is somewhere within the vicinity of the human body. Mode refers to how the microorganism moves.
There are four general modes of disease transmission. They include contact, vehicle (when organisms catch a ride on contaminated food or water), airborne (when an organism travels via dust particles throughout the air), and vector-borne transmission (microbes are carried by an infected animal or insect such as a tick or mosquito).
Of the four modes of transmission, contact transmission represents the most common mode of disease transmission in the clinical environment. There are several different categories of contact transmission including direct and indirect. Direct contact transmission occurs when the clinician comes in contact with a microbe found in the environment. For example, if you happen to touch a draining ear with your bare hand, that is direct contact transmission. Indirect contact transmission occurs when handling or reusing a contaminated object. For example, using the same listening stethoscope to conduct a hearing aid listening check on two different hearing instruments without first cleaning and then disinfecting the bell between listening check. The critical point is not so much what differentiates direct from indirect transmission, but rather what activities you, as an audiologist, perform throughout the day that can potentially offer microorganisms an opportunity to travel from one location to the next.
Once a microbe has established a mode of transmission, it then requires a route of transmission. Route refers to a portal of entry into the body. Common portals of entry into the body include dry, chapped hands or any other skin surfaces that may be dry or exposed with cuts or scratches. In addition, natural body orifices serve as portals of entry into the human body, including the nose, eyes, mouth, and ears.
Once the microbe enters the human body, a million different things need to happen in order for disease to occur. Whether or not disease manifests is a moot point. From an infection control standpoint, our responsibility, as audiologists, is to control the external environment by performing diagnostic and rehabilitative procedures in a manner that eliminates potential modes and routes of microbial transmission.
Finally, why should we care? The concept of opportunistic infections represents a very critical element regarding the relevance of infection control to the field of audiology. As previously mentioned, an opportunistic infection is a disease state that is caused by commonplace ubiquitous microorganisms that are readily found throughout the environment. Opportunistic microorganisms do not cause diseases in those with healthy, intact immune systems. Rather, as the name implies, these microorganisms take the opportunity to infect a body with some degree of immunocompromise. The hallmark of immunocompromise is susceptibility to the very same microorganisms that are considered essentially harmless to healthy individuals.
Microbial Study
To put all of this into a more meaningful context, it is appropriate to review the findings of a study that was published by Bankaitis in 2002 in the Hearing Journal entitled, “What is Growing on Your Patient’s Hearing Aids?” The purpose of this study was to identify the presence or absence of microbial growth on hearing instrument surfaces. If microbial growth was detected, the secondary purpose was to simply identify the type of bacterium and/or fungi that were recovered from these surfaces. Ten custom hearing instruments were randomly selected from one ear of ten different patients, all of whom were binaural wearers of amplification. The hearing instrument surfaces were swabbed, utilizing the Baxter Culturette System as seen in Figure 6. Essentially, this is a very expensive sterile Q-tip. Two culturette systems were used to simultaneously swab the hearing instrument. Two swabs were necessary for purposes of microbial differentiations. One swab was used by the microbiology lab to identify bacterial growth, whereas the other swab was used to identify the presence of any fungal growth.
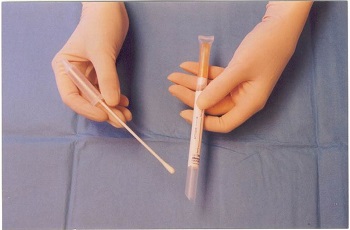
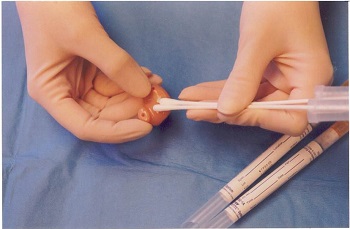
Figure 6. Specimen collection swabs and collection procedure.
Once the specimen was collected, the individual cultures were reinserted into their individual capsules and activated by crushing the ampule, which saturated the swab in preparation for analysis. The cultures were then labeled, placed in a biohazard specimen pouch, and dropped off at the St. Louis University Medical Center’s Microbiology Lab for analysis within 15 minutes of specimen collection.
The tables in Figure 7 show the microbes that were recovered from each hearing aid device. Any listed microbe appearing in red indicates that heavy amounts of the microbial growth were found. Anything appearing in yellow indicates moderate amounts, and anything appearing in green indicates light amounts of microbial growth.
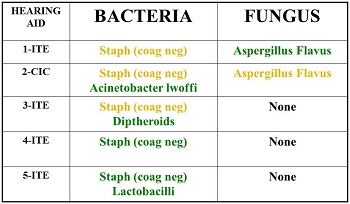
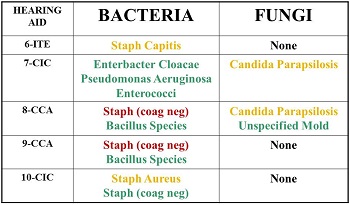
Figure 7. Results of microbial growth on hearing aid specimens (red= heavy amounts; yellow= moderate amounts; green= light amounts).
The left-hand column (Figure 7) lists each hearing instrument along with a more specific indicator as to the type of custom device, whether it was an in-the ear (ITE) or completely-in-the-canal (CIC) device. The middle column lists recovered bacteria corresponding to each of the hearing instruments, and the far right column reflects any kind of fungal growth that may have been recovered from each of the hearing instrument surfaces.
Let’s look at hearing aid #2 (Figure 7). The results indicate that we found moderate amounts of Staphylococcus on this hearing instrument, as well as light amounts of Acinetobacter. These are two different types of bacteria. In addition, we found moderate amounts of Aspergillus on the same hearing instrument. In contrast, if we look at hearing aid #5, there was no fungal growth, but there were light amounts of Staphylococcus and the bacterium Lactobacillus. Hearing aid #7 had light amounts of three different bacterium, including Enterbacter, Pseudomonas, and Enterococci, as well as moderate amounts of Candida. If you look at #10, there was no fungal growth, but we did find moderate amounts of Staphylococcus Aureus as well as your everyday Staphylococcus.
Figure 8 provides a visual illustration of the results from these tables. There you see 10 circles that represent each of the 10 hearing instruments that were swabbed in the study. At this point, all of the circles are the same color because we have not applied the results of the study yet. If we start assigning a specific color to each and every specific microorganism recovered from the hearing aid surfaces, it starts to look like Figure 9.
Figure 8. Result synopsis from study, showing all 10 hearing aids individually.
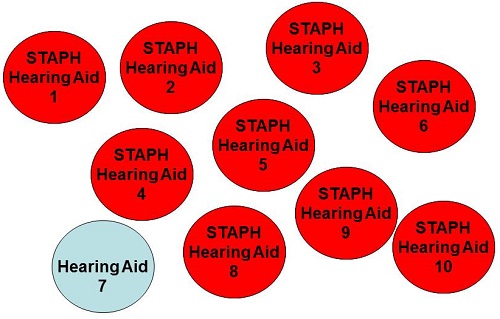
Figure 9. Result synopsis, showing each hearing aid that revealed one specific type of bacteria. In this case, staph was found on 9 of the 10 hearing aids.
First and foremost, 9 of the 10 hearing instruments were contaminated with some type of Staphylococcus. There are 29 different forms of Staphylococcus, and we simply did not have the funds to differentiate the different types of Staphylococcus. Beyond Staphylococcus, it is important to note that there were several other bacterium that were recovered as well. Not only were there seven different additional bacterium recovered from the hearing aid surfaces, but each hearing aid surface contained very different combinations of those different bacterium.
Furthermore, 4 of the 10 hearing instruments were also contaminated with some type of fungal specimen. In Figure 10, each color represents either a different microbe and/or different bacterial fungal combination. All 10 hearing instruments, which initially started out blue in color, have a completely different color from one another, representing the presence of very unique combinations of microbial contamination on each of the hearing instruments. In other words, none of the 10 hearing instruments were contaminated with the same organisms.
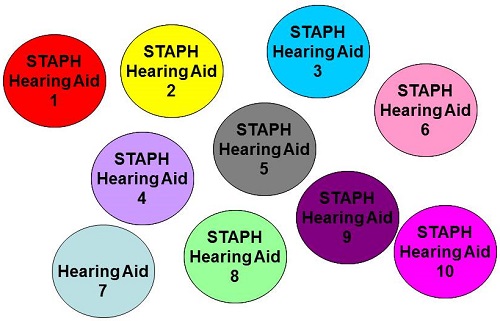
Figure 10. Visual representation of different combinations of bacterium on each of the 10 hearing aid specimens.
A very logical question at this point would be, “Are these findings surprising?” I will tell you the results of this study are not surprising when you take into consideration the normal flora of the external auditory canal. At the end of the day, if I were to take a Baxter Culturette System and put it in someone’s ear and send it off for analysis, we would find some of the same stuff growing in everyone’s ears, including various forms of Staphylococcus, diphtheroids, as well as occasional fungal spores.
On the other hand, if you thought these results were surprising, you are correct as well. Given the fact that each of the 10 hearing instruments reflected a very unique microbial combination, these findings are surprising. From an infection control standpoint, keep in mind that the external auditory canal is more prone to infection than virtually any other skin surface. While cerumen may have some antimicrobial properties, the efficacy of cerumen’s antimicrobial properties will most likely be challenged in the population who wears hearing aids.
In the absence of a hearing instrument, the ear canal is already a very warm, dark, and moist place. When you plug it up with an ear mold, custom hearing instrument, iPod earphones or cellphone accessories, the ear canal becomes an even warmer, darker, moister place, which causes it to retain moisture. When the ear retains moisture, acid ions are depleted from the canal skin, raising the surface pH to a more neutral or alkaline level, which results in the creation of an environment that is more conducive to microbial growth.
With that in mind, opportunistic infections become a very realistic concern if infection control procedures are not followed. For example, recall that 9 of the 10 hearing instruments were contaminated with Staphylococcus. This is a ubiquitous bacterium readily found throughout the environment. However, this same bacterium accounts for the highest rates of hospital-acquired infection. How can something found so readily throughout the environment cause so much disease in hospitals? Well, who goes to hospitals? Typically, it is sick people who possess some degree of immunocompromise, who are extremely susceptible to bacteria or fungi that healthy individuals are not.
Pseudomonas was recovered from one of the hearing instruments, specifically hearing aid #7. While Pseudomonas may be part of some patients’ normal ear canal flora, it is not necessarily considered part of every patient’s normal ear canal flora. This bacterium is highly virulent, and it can cause otitis externa, which can quickly progress to malignant otitis externa, also known as osteomyelitis, in diabetic and HIV-infected individuals, given the right set of circumstances.
While Staphylococcus and Pseudomonas may be considered expected components of ear canal flora, some of the microorganisms that were recovered from these hearing instruments are not considered normal microbes found in human ears. For example, Lactobacillus, which was found on hearing aid #5 in light amounts, is a bacterium that is specifically isolated from urine. We found urine on hearing aid #5. Enterobacter was found on hearing aid #7, and this specific strain of Enterobacter is found in human feces. Yes; we found feces on a hearing instrument.
What is my real point? Each hearing instrument reflected a unique microbial composition, and it is important to realize that no two hearing aids are the same. From an infection control standpoint, if you were to handle hearing instrument #7, which belongs to one patient, and in the absence of any infection control procedures started handling hearing aid #6, which belongs to a totally different patient, anything residing on hearing aid #7 will now cross-contaminate hearing aid #6. When you reinsert that now cross-contaminated hearing aid #6 into the ear canal of your 80-year-old diabetic patient, you just provided microorganisms a very easy route for disease transmission.
A similar study was conducted by Sturgulewski and colleagues at Rush University (2006), whereby the findings of my original study were duplicated, and further, a subsample of hearing instrument pairs swabbed from the same patient revealed different microbial compositions between the same patient’s ears, which opens a completely new can of worms.
How Do I Prepare?
All of this brings us to the third and final objective of today’s presentation which is “How do I prepare?” What is it that I need to do tomorrow? In order to prepare for an infection control plan, the first thing you need to do is assess the scope of service. What services do you and your staff provide specifically? For example, if you dispense hearing instruments, you need to take out a piece of paper and pencil and start listing every type of service that is associated with dispensing hearing instruments in your clinic. If you or anyone in your clinical setting creates ear mold impressions, write that on your list. If you do the actual hearing instrument fittings, put that on your list. Hearing instrument modifications, listening checks, electroacoustic or real-ear measurements, drop-off services, loaner hearing instruments and stock ear molds are just examples of different services that fall under hearing aid dispensing. Everyone in a clinic needs to review each of the services that are provided in order to come up with a comprehensive list.
Making a List of Services
If you perform audiological assessments, you most likely perform otoscopy, air conduction audiometry, speech audiometry, bone conduction audiometry, immittance audiometry, and perhaps otoacoustic emissions (OAEs). You need to write all the services that you provide pertaining to cerumen removal, including mechanical removal, suction or irrigation, use of cerumen softening agents, and what steps you take in the event of a bleed.
The reason this is so critical is that this list of your scope of services is going to dictate the number of work-practice controls that you will need to create for your written infection control plan. A work-practice control is a profession-specific procedure that is designed to reduce the likelihood of cross-contamination. Your homework assignment prior to you looking at Part 2 is to create your own list of services that is unique to the clinical environment in which you are working. Every clinic will differ in terms of the scope of services that they provide. Once you create this list, it will dictate the number of work-practice controls that you are going to have create and insert in your written infection control plan. That written procedure is going to outline how you and your staff will perform that procedure in a manner that is consistent with minimizing the spread of disease.
Standard Precautions
In order to ensure that the written procedure integrates the necessary infection control principles, the work-practice controls are going to be based on the universal precautions that have been issued by the Centers for Disease Control and Prevention (CDC). The CDC originally set universal precautions in 1987. In response to HIV, the CDC created a list of recommendations that were intended to reduce the cross-contamination of blood-borne pathogens. Specifically, the universal precautions focused on the severe blood-borne pathogens, such as HIV and hepatitis. The universal precautions were expanded to include any and all potentially infectious microorganisms, including the ones that we recovered from hearing aid surfaces. Instead of the term universal precautions, you now hear the term standard precautions used.
You need to have the mindset that every patient is considered a potential carrier of an infectious disease. Each procedure that you perform must be consistently performed with each and every patient, each and every time. As issued by the CDC, the standard precautions include the five following guidelines:
- Appropriate personal barriers, such as gloves, masks, eye protection, gowns, must be worn when performing procedures that may expose one to infectious agents.
- Hands must be washed before and after every patient contact and after glove removal.
- Touch and splash surfaces must be pre-cleaned and disinfected.
- Critical instruments must be sterilized.
- Infectious wastes must be disposed of appropriately.
These are the five standard precautions from which we are going to use as the foundation for writing the work-practice controls, which are an extremely important element of the written infection control plan. These steps are going to be covered in Infection Control Part 2.
Take Home Message
First and foremost, infection control requires consciously managing your clinical environment. You are going to have to think through processes that otherwise seem very automatic to you, and there is going to be a level of frustration where you are going to want to give up. Please do not give up. In the event that you get frustrated, rely on available resources or get in touch with me. Infection control is a very important element of best practices for audiology. As previously mentioned, infection control is also the law. You are legally, as well as ethically, obligated to implement infection control requirements into your clinical practice.
Finally, in order for you to get the most out of Part 2, you must understand that infection control requires preparation. You must identify the scope of services that you or anyone else in your clinic will provide and have that exhaustive list available. That is going to be the one piece that will be critical in helping you develop a specific portion of the written plan. When it comes to a written infection control plan, 95% of it can be copied. You have to read it and understand it, but I can give you the information. The other 5% to which you need to pay considerable attention are the work-practice controls. This is the part of the infection control plan that will differ from clinic to clinic. It is driven or dictated by the scope of services that are provided.
Questions and Answers
How does one get a hold of the infection control textbook?
There are two infection control textbooks, which I call the purple book and the yellow book. The purple book is Infection Control in the Hearing Aid Clinic (Bankaitis & Kemp, 2003), which addresses everything you need to know about infection control, including work-practice controls associated with hearing aid dispensing only. The second book, which is the yellow book, is Infection Control in the Audiology Clinic (Bankaitis & Kemp, 2004). That book includes everything that the purple book includes, along with hearing aid dispensing, as well as all aspects of audiology practice including intraoperative monitoring, cochlear implants, vestibular testing, electrophysiology, et cetera. The easiest way to order the book is to go to oaktreeproducts.com. If you do not have an account, it is easy to set one up. If you want to email me and ask me how to set up an account, you can do that. You can buy it online, and it is found in our Infection Control section. If you prefer to talk to a person, you can call customer service at 800-347-1960.
Does infection control change? Do I need to review my processes on a regular basis?
We are going to cover some of that in Part 2. The basic principles of infection control rarely change. It is a requirement per OSHA to go over them annually. You also need to review your procedures when you have new hires or if your clinic introduces a new procedure or a new technique. For example, when I was director of Audiology at Saint Louis University Medical Center, we had a written infection control plan, but when we decided to start doing otoacoustic emissions, we had to review infection control specifically as it related to how we performed otoacoustic emissions.
We use bins to place hearing aids when they are dropped off. Aside from cleaning with Lysol, how else can we prevent contamination from one hearing aid to another?
I see a lot of clinics implementing either an envelope or a Dixie cup, so the person transferring it to the next place does not have to handle it. If you are re-using a bin that is going to accommodate different hearing instruments, between patients or possibly at the end of the day, you want to clean and disinfect those bins. It is more critical for you to make sure that the hearing aid that is removed from the bin is immediately cleaned and disinfected prior to handling it. That is more critical than worrying about what kind of grubby stuff is growing inside the bin.
You could technically wait until the end of the day to clean the inside of the bin, assuming that every hearing instrument that you remove from that bin is immediately cleaned and disinfected. The best way to clean and disinfect a hearing instrument is to initially use a paper towel or Kleenex to clean the surface, followed by the use of a disinfectant towelette, preferably one that is not alcohol based. Alcohol tends to denature acrylic, plastic, rubber, and silicone, which are very common in the audiology clinic. Specific procedures for cleaning and disinfecting will be are going to be covered in Part 2.
References
Bankaitis, A.U. (2002). What’s growing on your patient’s hearing aids? A study gives you an idea. Hearing Journal, 55(6), 48-54. doi: 10.1097/01.HJ.0000293278.53653.ac
Bankaitis, A.U. (1996). Audiological changes attributable to HIV. Audiology Today, 8(6), 7-9.
Bankaitis, A.U. & Kemp, R.J. (2003). Infection Control in the Hearing Aid Clinic. Boulder, CO: Auban.
Bankaitis, A.U. & Kemp, R.J. (2004). Infection Control in the Audiology Clinic. Boulder, CO: Auban.
Sturgulewski, S., Bankaitis, A. U., Klodd, D., & Haberkamp, T. (2006). What’s still growing on your patient’s hearing aids? Hearing Journal, 59(9), 45, 46, 48. doi: 10.1097/01.HJ.0000285827.98823.87
Cite this content as:
Bankaitis, A. (2014, October). Infection control - why audiologists need to care. AudiologyOnline, Article 12916 Retrieved from: https://www.audiologyonline.com


