Learning Outcomes
After this course, learners will be able to:
- List three limitations of pure tone hearing screening in young (birth to 3 years) preschool hearing children.
- Cite three factors contributing to loss-to-follow up of infants who yield a refer outcome for initial hearing screening.
- Describe three specific advantages of OAEs in preschool hearing screening.
Introduction
Dr. James Hall: This course will cover the following topics:
- Introduction to Early Hearing Detection and Intervention (EHDI)
- Guidelines for preschool hearing screening and limitations of pure tone screening
- Summary of research in support of OAEs in preschool hearing screening
- Evidence-based strategy for applying OAEs in preschool hearing screening
I'm going to assume that most of you are audiologists and that you are familiar with Early Hearing Detection and Intervention (EHDI). I'll review EHDI as well as various guidelines for screening preschool children, as well as the limitations of using pure tone audiometry for this population. Then, I'll cover otoacoustic emissions (OAEs). I will summarize the research supporting their use in preschool hearing screening, including a study that I participated in. Next, I'll talk about a practical, feasible strategy that can be implemented in preschool programs, daycare centers, and Head Start programs using OAEs. One of the biggest advantages of OAEs is that you don't need an audiologist to do the screening. It can be conducted by a nurse, a technician, a volunteer or a preschool worker. Finally, we'll have time for questions and answers.
Early Hearing Loss Detection and Intervention: The 1-3-6 Approach
To begin discussion of EHDI, let's review the 1-3-6 approach. This approach has evolved since we first started using universal newborn hearing screening in the United States and many other countries. Before the child is one month old, the goal is to conduct a hearing screening and identify if there is a hearing loss. Most of the time the initial hearing screening is done within a day or two after the child is born, before they are discharged from the hospital. Once the child is discharged, it is more difficult to track them down for screening. While we try to conduct hearing screening for newborns in the hospital, as long as the screening is completed by one month, we are meeting the EHDI goal.
For those children who do not pass the infant hearing screening, the next step is to diagnose the hearing loss by three months after birth. If the child is born one month prematurely (e.g., at 36 weeks' gestational age instead of 40 weeks), we usually extend the screening to four months after birth. Certainly, the screening can be done earlier than three months. In my practice, I've always encouraged parents whose child failed the hearing screening to bring them back in by two months of age. If there is a missed appointment, you still can reach the three month goal. It's sometimes even easier to administer the hearing screening at two months of age, because they sleep much of the time at that age. If you have to do auditory brainstem response (ABR) testing, or other tests to complete the diagnostic assessment by two months, it's much easier when the children are in a deep sleep.
The hearing screening and the diagnosis is not meaningful without intervention. For the child who fails screening and who has a confirmed hearing loss by diagnostic assessment, we need to intervene, in many cases, with amplification or other forms of audiological habilitation. Intervention should begin by six months of age. In the United States, if the child needs a cochlear implant, that will not be done until the child reaches 12 months of age.
The Problem of "Loss to Follow Up"
The 1-3-6 approach is a noble objective. Between 90 and 98 percent of newborn infants do undergo hearing screening at birth. However, there is a small percentage of children who are not screened at birth. Furthermore, according to the Centers for Disease Control, over 40% of children who fail the hearing screening at birth do not undergo timely evaluation, and are not diagnosed by three months of age. They are considered "lost to follow up" or "lost to diagnosis." Additionally, there are children who get through the diagnostic process, but then never receive intervention. There are a variety of reasons why infants do not receive screening and/or diagnosis, including:
- Newborn infants discharged from nursery before screening
- Infants transferred to another hospital before screening
- Infants screened in one state and living in another state
- Failure to document screening or diagnostic findings
- Family reasons
- Transportation problems
- Misunderstanding about need for follow-up
- Infant has no primary care physician (medically homeless)
In a nutshell, this is why we are talking about using OAEs in preschool hearing screening. You can't begin intervention for hearing loss without a diagnosis, and many children who do need follow up simply don't get it. For the EHDI program to be successful, it is important that all children who have a hearing loss are identified as early as possible and intervention begins by six months of age.
There are multiple solutions to help reduce the number of children lost to follow up, such as:
- Well-organized systems for data management and tracking
- Education of:
- Hospital personnel
- Primary care physicians and pediatricians
- Combination OAE/AABR hearing screening approach for lower failure rate and early diagnosis of hearing loss
- Diagnostic assessment immediately following screening failures in hospitals with audiology clinical services
- More qualified audiologists widely distribution throughout each state to provide diagnostic evaluations
- Tele-audiology strategies for diagnostic evaluations
- preschool hearing screenings
All of these strategies will help. For the purposes of today's presentation, however, I'm going to focus on preschool hearing screenings.
Preschool Hearing Screening
Logically, preschool hearing screening should be conducted wherever babies are found. One ideal place to do preschool screenings is in a physician's office. This is where OAEs are very handy. Pure tone audiometry as a screening technique is simply not feasible in primary care physician's offices, but OAEs are a feasible option. Sooner or later, most children come in to see their pediatrician or their family doctor, for well-child visits, immunizations, treatment for ear infections, and a variety of other reasons. That's an excellent time for screening hearing, if it's indicated.
In the United States, hundreds of thousands of children are enrolled in Head Start programs. Head Start is a program of the United States Department of Health and Human Services that provides comprehensive early childhood education, health, nutrition, and parent involvement services to low-income children and their families. For Early Head Start programs, the age of enrollment is from six weeks to two years old. As they get older, children can be enrolled in the Head Start program at three to four years of age, before they enter kindergarten and public school. Preschool hearing screenings are being done in many Head Start programs, but not all of them. In addition to Head Start, there are many other preschool programs, mother's day out programs, and daycare facilities that would be appropriate places to conduct hearing screening using OAEs.
Rationales for Preschool Hearing Screening
What are some rationales for preschool hearing screening? A small percentage of babies (2-3%) who should have been screened at birth, do not receive screening. This may seem like a trivial amount. However, in the United States alone, there are four million babies born every year. If you calculate 3% of four million, that adds up to 120,000 babies. In some countries, many more millions of babies are born each year than in the U.S. Those children who do not undergo hearing screening at birth may eventually be identified as having hearing loss, if we conduct preschool screenings. In larger states, such as Texas, 50% of babies who undergo screening at birth and fail are "lost to follow-up (LFU)." Preschool screenings would potentially catch some of these children before they enter school, so that hearing loss can be properly diagnosed and treated.
Another problem separate from universal screening relates to delayed onset hearing loss or progressive hearing loss in children. There are children who start out with normal hearing and pass early screenings. If you take 100 children with a confirmed hearing loss coming into first grade or kindergarten, and you look at their status at birth, 15% of them had normal hearing screening findings. Even if you had the perfect universal screening program, and even if every child who failed a screening underwent diagnostic testing, 15% of those children will develop a hearing loss at some point. That's one of the strongest rationales for implementing preschool hearing screening.
Up until now, we've been talking about permanent sensory hearing loss and progressive sensory hearing loss in children. However, there is another group of children who need to undergo preschool hearing screening: the large percentage of children who develop middle ear dysfunction during the preschool years. In the United States, almost every preschool-aged child ends up with an ear infection, some of which become chronic ear infections. Hearing loss due to ear infections affects a child's speech and language development, auditory processing development, and academic performance. These are all strong reasons for why we need preschool hearing screening in general.
Risk Indicators for Delayed Onset or Progressive Hearing Loss
If you want to know more about risk factors for delayed onset or progressive hearing loss in infants (or any infant hearing loss for that matter), the best source of information is the Joint Committee on Infant Hearing (JCIH) position statement, available at www.jcih.org. Although it was published in 2007, it is still very relevant. I would expect that they would be putting out a revised version sometime soon. You can download a PDF version of this from the Internet. It is the clinical practice guideline for early identification of hearing loss in infants.
If you go to the Joint Committee statement, they reference to two types of hearing loss that occur after a child is born. The first is delayed onset, or late onset, a form of acquired hearing loss often associated with a family history. The child is born, and passes the infant hearing screening. At some point, they develop a unilateral or a bilateral hearing loss. There may be an obvious etiology, such as meningitis or ototoxicity, or there may be a family history. There may not no obvious risk factor except the family history. Children with delayed onset hearing loss may go from normal hearing to a profound hearing loss almost overnight.
The other type of hearing loss that can be acquired during childhood is a progressive hearing loss. Again, the child starts out with what appears to be normal hearing and they end up with a hearing loss, but the hearing loss becomes more serious over time. Some children with progressive hearing loss may have had some evidence of cochlear dysfunction at birth, which the screening techniques simply didn't detect. We can't be sure that all progressive hearing loss started after the neonatal period, but it doesn't make much difference. In any event, we know they have developed a hearing loss that may be getting more serious. There are numerous factors for progressive hearing loss, like cytomegalovirus or ototoxicity, as well as genetic factors.
I mentioned that 15% of children with a hearing loss entering school passed their infant hearing screening. Figure 1 cites a few key studies with evidence in support of that. The first study is from England, published in the British Medical Journal (Fortnum, Summerfield, Marshall, Davis, A.C, & Bamforet al, 2001). This study is cited quite often. It shows that the prevalence of hearing loss increases throughout the preschool years. At birth, the prevalence of hearing loss is usually estimated around two or three children out of a thousand. By the time the child gets to age three, it increases to 1%, which is 10 times higher than one out of a thousand. By the time they reach school age, it increases to 2%. There is ten-fold increase in the prevalence of hearing loss from birth to school age. Another study out of the Netherlands (Grote, 2000) shows that 10 to 20% of permanent hearing loss will not be detected by universal newborn hearing screening, because the hearing loss is acquired later. Finally, in 2010, Karl White presented data showing a great increase in the prevalence of hearing loss in the preschool years. All of these studies are arguments in favor of preschool hearing screening.
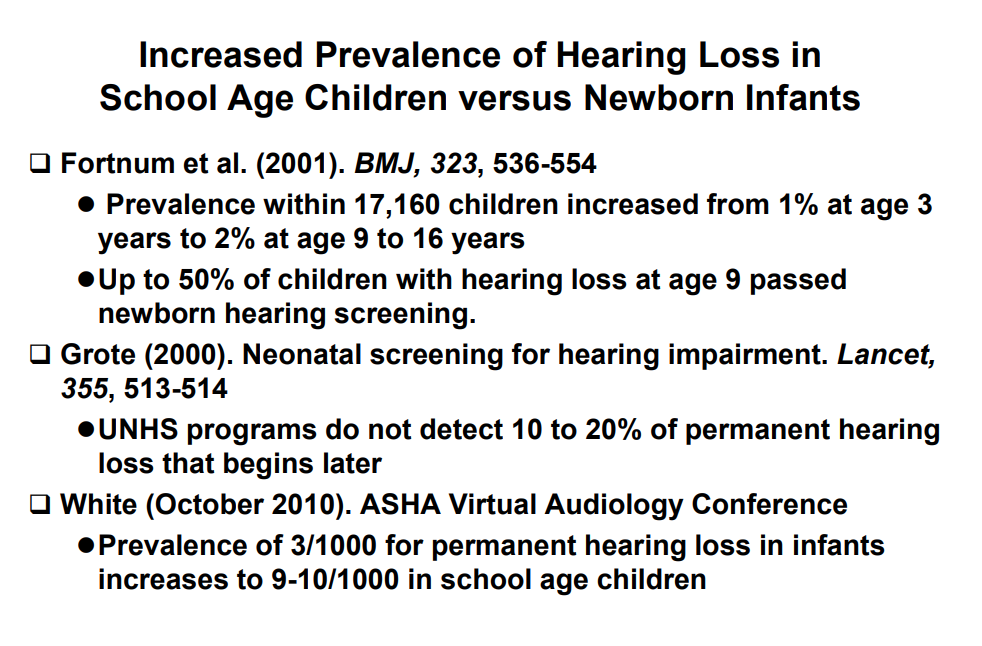
Figure 1. Studies to support that 15% of children with hearing loss pass their newborn hearing screening.
Guidelines for Preschool Hearing Screening and Limitations of Pure Tone Hearing Screening
Next, we will discuss the different guidelines that exist for preschool hearing screening, specifically focusing on one that has been used most often. We will also examine some of the limitations of pure tone hearing screening. Invariably, you will encounter people who are skeptical when you mention OAEs as a screening technique. It will be helpful for you to have the information to support the rationale that pure tone screening is not the answer during the preschool years.
Going back to the early 1980s, you can find references to the importance of and recommendations in favor of hearing screening in preschool children. There are several different sources for these guidelines, such as American Academy of Pediatrics, American Speech Language and Hearing Association (ASHA), and other groups. To this day, the most commonly cited guidelines are the 1997 ASHA Guidelines for Audiologic Screening. That was 20 years ago, but people still rely on them. I'm going to summarize why these 1997 ASHA Guidelines are out of date and no longer feasible. For the sake of time, I'm not going to talk much about more recent guidelines, although there are some. The American Academy of Audiology (AAA) has some clinical practice guidelines for childhood screening that can be downloaded from www.audiology.org. However, they are based heavily on the 1997 ASHA Guidelines. You might say that that AAA guidelines, to some extent, are an updated version of the earlier ASHA Guidelines.
When you look at the ASHA guidelines closely, particularly the reference to hearing screening of the younger children (seven months up to two or three years), you can see the problem arise right away. The panel (i.e., the people that wrote the guidelines) pushed the role of audiologist in hearing screening. In many parts of the guidelines, there are references to how screening should be done by an audiologist, particularly for the younger children. It's not easy to screen hearing of younger children. Certainly, someone without much experience (e.g., a volunteer, a nurse, or a worker in a Head Start program) will have a hard time performing pure tone screening on a one- or two-year-old. You can see the rationale for why the ASHA Guidelines call for audiologists to do this. The problem is that there are no audiologists in these facilities. You don't have audiologists where these children are located. As such, it is not feasible. Guidelines are of no value if they can't be implemented.
The ASHA Guidelines even talk about using conditioned play audiometry for screening younger children. That simply is not feasible for non-audiologists who are not familiar with conditioned play audiometry. Additionally, time is an important element in hearing screening. If you have 100 children in a preschool program that need to be screened using conditioned play audiometry, that is going to be very time consuming. They also talk about other strategies, like visual reinforcement audiometry, which involves use of a sound booth. There aren't sound booths in Head Start programs or physicians' offices. It is clear that these guidelines have serious problems in terms of feasibility.
Research Studies in Support of Pure Tone Screening
When looking at studies documenting the effectiveness of pure tone hearing screening in preschool children, there are several questions we need to ask.
- First, we want to know who performed the screening and what are their qualifications. Was it an audiologist, a graduate student, another health professional or a trained non-health professional? The best-case scenario results would be achieved if the screening was done by an audiologist.
- What were the ambient noise levels in the test environment? If you're conducting a screening in a quiet environment, perhaps it might work. Of course, in many preschool settings, there isn't a quiet test setting where you can conduct the screening.
- What was the screening protocol? What kind of earphone did they use (supra-aural versus insert)? What were the test frequencies and the response criteria?
- How many children could not be tested (CNT)? This can be very misleading when you read the literature. Often they'll indicate that they screened 300 children using pure tone audiometry, but in the fine print, they'll disclose that another 50 children could not be tested. My concern is that all 350 children could have a hearing loss. We have to be able to test every child that needs to be tested. We can't arbitrarily reject some and say, "Well, they couldn't be tested so we won't worry about them."
- Finally, we need to ask what were the PASS and FAIL (did not pass) rates?
In the research studies that we will review, the screening was conducted by audiologists, audiology students, or speech pathology students. The outcome for these studies should be best case scenarios, because these were professionals who knew how to accurately screen babies or young children.
Krishnamurti, Hawks, & Gerling (1999). This study used a sample of 100 preschool children, ages 36 to 60 months, of moderate to high socioeconomic status. The screening was done by a PhD student. They found that the pure tone hearing screening failure rate was 24%. One out of four children failed the screening. We know that the hearing loss prevalence in this population is certainly not 24%. An ideal failure rate for children might be between 5% to 10% max, including the children who fail because they have temporary middle-ear problems. We have an audiologist PhD student doing the screening, under ideal circumstances, with older children of high socioeconomic status, and we still have an unacceptably high failure rate.
Another important variable to consider with screening techniques is time. In this group of 100 children, instructing for pure tones took close to one minute per child, and the actual testing took considerably longer, adding up to about two to three minutes' minimum per child. When you multiply that by 100 children, you can see that it's time consuming. When screening older preschool children (ages 3-4) using OAEs, you can often screen both ears in a matter of 60 to 90 seconds.
Serpanos & Jarmel (2007). This study was conducted in the New York and Long Island area. Audiology and speech pathology graduate students administered the pure tone screenings. Settings included public preschool, day care or head start centers. They had a large sample of close to 35,000 subjects. The outcome of the screening resulted in 18% of children being referred (i.e., they failed the screening). Again, this is much too high.
Allen, Stuart, Everett, & Elangovan (2004). This study was conducted in North Carolina. The sample size was 1462 older preschool-aged children (3-4 years of age) in Head Start programs. The failure rate for pure tones was 29%. Clearly, using pure tone screening even under ideal circumstances, the failure rates are unacceptably high in the preschool population. The younger the child, the higher the failure rates are.
Halloran, Wall, Evans, Hardin, & Woolley (2005). Perhaps the most condemning study regarding pure tone screening of preschool children was conducted by a group of pediatricians in 2005. They screened more than one thousand children. The pure tone screenings were performed in exam rooms in pediatric practices, and the screening personnel were well-trained. One finding was that the pure tone screening worked well for children ages 4-5. However, with younger children, things started to fall apart. Only 55% of the screenings could be completed in the three-year-olds. For children younger than three, the percentage of successful screening was even lower. That is a serious problem. How can we have early identification of hearing loss if we can't screen children three years and under? Another serious concern was that most of the children with a failed screening result were not referred on for further screening or treatment, because the pediatricians began to distrust the screening results. The pediatricians were so leery about these failures that they began to believe that the children truly didn't have a hearing loss after all. The whole purpose of screening was undermined by the high failure rate. Every time they referred a child with a failure, they came back with normal test results. After a while, they stopped referring children because they believed that the screenings produced false failures.
Halloran, Hardin, & Wall (2009). This same group of pediatricians conducted a follow-up study four years later of the same group of children. Of the 1061 children who underwent hearing screening, a group of 130 children received a complete audiological evaluation. Usually you try to achieve high sensitivity, even if specificity is not so good. Or you want to have specificity; you want to make sure you don't say there is a hearing loss if a child doesn't have one. Unfortunately, as evidenced by this study, with pure tone screening you get the worst of both worlds: poor sensitivity (50%) and poor specificity (78%). Furthermore, none of the 28 children who could not be tested had a hearing loss, which adds more questions about why you're doing the screening to begin with.
Finally, a national survey of general pediatricians found that screening "guidelines were more likely to be followed if they were simple, feasible in the population, and demonstrated improved outcomes" (Flores, Lee, Bauchner, & Kastner, 2000). I would argue that OAEs meet these criteria; pure tone screening does not.
Research Studies in Support of OAEs
Up to this point, we have been a bit negative in our criticism of pure tones. If there were no alternatives, we would have no choice but to do pure tone screening. However, there is an alternative method: otoacoustic emissions. We have plenty of evidence and studies to support the use of OAEs in preschool screening. I will highlight some of the recent studies (Figure 2). Note that I'm limiting the evidence to those studies where the results were published in a peer-reviewed journal. In other words, each of these studies has been reviewed by experts in the topic and found to be well-conducted with trustworthy results.
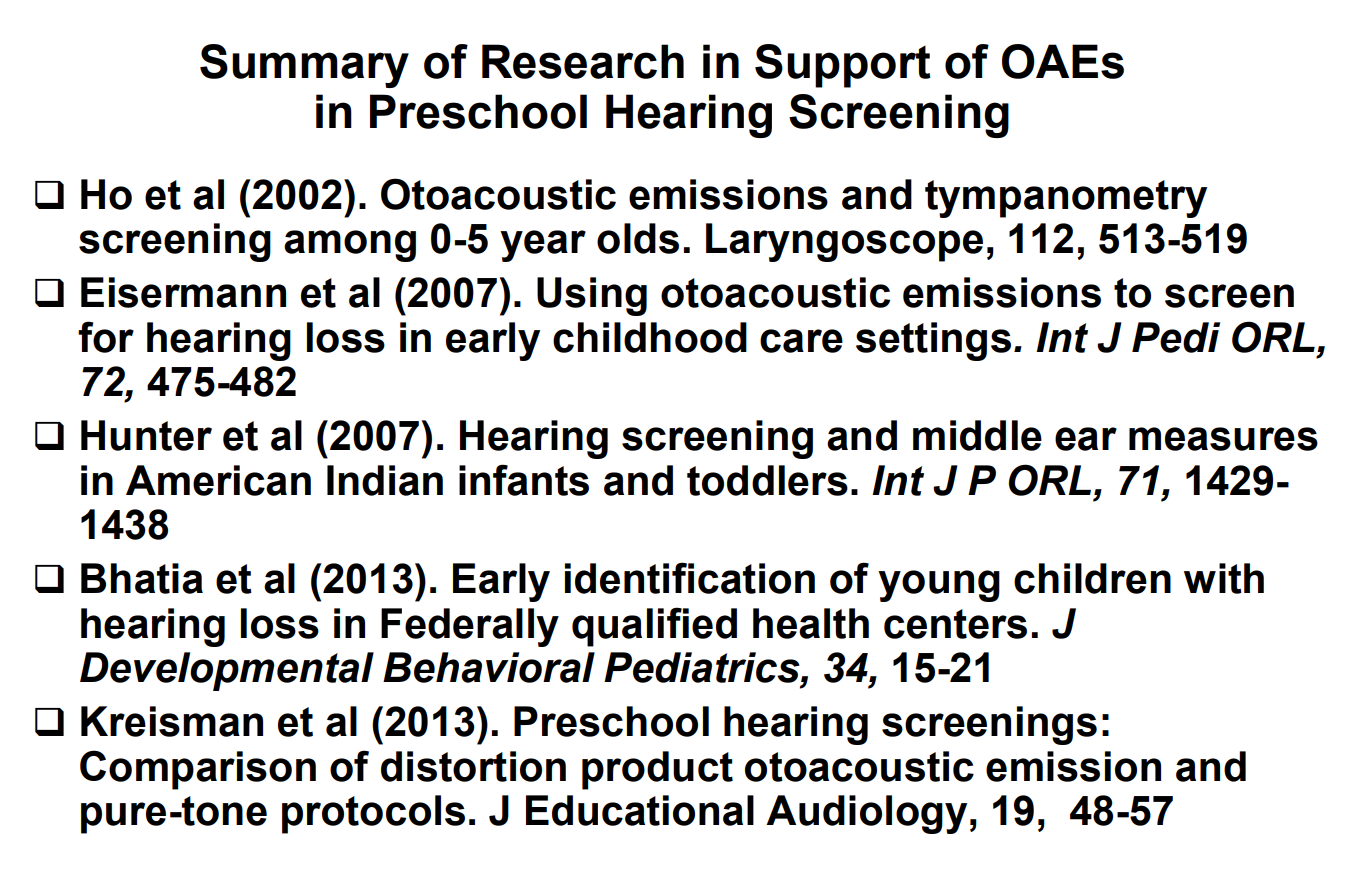
Figure 2. Studies to support OAEs in preschool hearing screening.
Ho, Daly, Hunter, & Davey (2002). This first study was published in the journal Laryngoscope. They performed OAEs and tympanometry screening in children ages zero to five.
Eisermann et al. (2007). Next, a group at Utah State showed that OAEs can be used to screen in early Head Start programs, in children aged six months to three years.
Hunter, Davey, Kohtz, & Daly (2007). Lisa Hunter conducted a study showing the relationship between OAE results and middle ear findings in American Indian infants and toddlers, a population known for their middle ear dysfunction. You can even use OAEs in that population in conjunction with tympanometry.
Bhatia, Mintz, Hecht, Deavenport, & Kuo (2013). This study demonstrated success using OAEs in Head Start centers, administered by non-audiologists.
Kreisman, Bevilacqua, Day, Kreisman, & Hall (2013). Next, I'm going to report some data from a study that I was involved in. The data was collected by Towson University graduate students, in eight different preschool facilities. The results were published in the Journal of Educational Audiology. There were close to 200 preschool children, ages three to six years. We used DPOAEs (distortion product otoacoustic emissions testing), rather than transients. This is a best-case scenario for pure tones.
One of the things we looked at was test time. The screening protocol recommended for DPOAEs is from 2 kHz up to 5 kHz, or 5 kHz down to 2 kHz. Usually, you do four or five frequencies in that region. Test time for both ears using DPOAEs was about one minute. It took quite a bit longer for pure tones, at well over three minutes per child. When testing hundreds of children, it would take one day using OAEs, versus two or three days with pure tones.
Let's take a look at pass/fail rates for DPOAEs and pure tone protocols (Figure 3).
| Protocol | Pass | Fail | Total |
| DPOAE (1-5 kHz) | 134 | 64 | 198 |
| DPOAE (2-5 kHz) | 141 | 57 | 198 |
| pure tone (1, 2, 4 kHz) | 175 | 21 | 196 |
| Note: Two children would not cooperate to be screened using pure tones. | |||
Figure 3. Pass/fail rates for DPOAEs and pure tone protocols.
You can see that more children failed the OAEs than failed the pure tones. One thing you want to avoid when using OAEs is passing a child who truly has a hearing loss. In fact, we see that children are sometimes passing pure tones who probably should have failed and they're being detected with OAEs. They might have minor middle ear problems, or they might have minor cochlear problems. In any case, we want to detect them if we can. You can also see that two out of the 200 children couldn't be screened with pure tones. If you had a thousand children, you'd probably have 20 or 30 who could not be screened with pure tones, and yet they were all screened with OAEs. This study provides strong evidence in support of OAEs in comparison to pure tones.
Advantages of OAEs
There are many advantages to using OAEs instead of pure tones with preschool children. OAEs are:
- Objective and not dependent on a child’s:
- Behavioral response
- Cognition
- Language level or native language
- Painless and even no discomfort
- Reliable
- Efficient and quick to administer (< 4 minutes)
- Simple to administer with low level of technical skill (does not require an audiologist)
Furthermore, OAE measurement does not require an acoustically treated environment. The equipment is hand-held and portable. Test outcomes are documented electronically or can be printed out. With pure tone screening, someone needs to judge whether there is a result, and then record that result, leaving more room for error. With OAEs, you automatically get a pass/fail outcome that can be reviewed later by anyone.
New Strategy Using OAEs, Tympanometry and Acoustic Reflexes
We've given you some good solid reasons to use OAEs in preschool screening, as well as several reasons not to use pure tone. Now let's change gears and talk about a strategy. When you go out to a Head Start program or go to a preschool center, and you are giving training to non-audiologists who are going to conduct a screening, what strategy will you use?
First of all, in the preschool population (six months up to three years), where you cannot rely on pure tones, you want to have multiple objective techniques. We're going to primarily use OAEs. For the majority of children, OAEs will give us the information we need. The child will pass the OAE screening and we're not going to worry about their hearing. However, some of the children (10-12%) will not pass the OAE screening. For those children, our goal is to find out why they are failing this OAE screening. Is it because they have a cochlear loss that's may be permanent? Or, are they failing the OAE screening because they have what might be a temporary middle ear abnormality? The way we can sort that out is with tympanometry and acoustic reflexes.
These techniques aren't new. They've been around clinically since the early 70s. However, this idea of using OAEs, tympanometry and acoustic reflexes in newborn hearing screening is definitely a new strategy. I've used it and it works. I'm not saying every child will need to be screened with OAEs, tympanometry and acoustic reflexes. As I mentioned, 85% to 90% of the children are only screened with OAEs. They pass the screening, and we're not worried about any ear problems with those children. For the 10% or so who do not pass the OAEs, our next goal is to try to determine which ones have middle ear problems and which ones have a sensory hearing loss that may be permanent.
GSI Corti
We want to combine the OAE screening techniques using a device like the GSI Corti (Figure 4). It is light and portable. You can see the probe in the child's ear. We want to combine that with another technique, such as tympanometry and reflexes. You might find some devices that have both tympanometry and OAEs in the same system, and those would work well too. There is an advantage of having two different systems for the two technologies, one for the OAE and one for the tympanometry and reflexes. For example, you may be paired with another screener who is a non-audiologist. The non-audiologist could quickly do the OAE screening for the majority (90%) of babies. For the other 10%, an audiologist could come through later with a tympanometer and a machine to measure acoustic reflexes to determine whether the problem could be in the middle ear or the cochlea.

Figure 4. GSI Corti.
Combining these three techniques (OAEs, tympanometry and acoustic reflexes) is a real advantage. First, they're all objective. You don't worry about the child's age, whether they understand the instructions, their cognitive level, their language level or which language they speak. You can get the results from young children regardless of those conditions. Furthermore, these techniques are all reliable and easy to administer. You don't need an audiologist. Acoustic reflexes could even be recorded by a non-audiologist with a screening device. All the advantages we cited for OAEs apply to all of these techniques. By combining OAEs, tympanometry and acoustic reflexes in the children who do not pass, we now have a sensitive measure of middle ear function, of cochlear function (outer and inner hair cell function) and ANSD (auditory neuropathy spectrum disorder). If you have a child who may have a risk factor for ANSD, such as a neurological disorder, or perhaps a family history of ANSD, then you could combine OAEs and acoustic reflexes. Half of all children with auditory neuropathy have a genetic factor. Any child who has normal OAEs and no acoustic reflexes probably has ANSD, or at least is at great risk. That combination of normal OAEs and absent reflexes is a combination that you don't see very often in any child, except a child with a bilateral neural problem.
JCIH Protocol: Evaluation of Infant Hearing Loss (Birth to Six Months)
If you do combine tympanometry, OAEs and acoustic reflexes, you will be consistent with clinical practice guidelines. Referring again to the Joint Committee on Infant Hearing, they recommend OAEs, tympanometry with a high frequency probe tone in very young children (above age six months, you could use a 226 Hz probe tone). As a supplemental procedure, you would be totally within your rights and within clinical guidelines to use acoustic reflex measurements. The complete JCIH recommended protocol for evaluating infant hearing loss is outlined as follows:
- Child and family history
- Evaluation of risk factors for congenital hearing loss
- Parental report of infant’s responses to sound
- Clinical observation of infant’s auditory behavior
- Audiological assessment:
- Auditory brainstem response (ABR)
- Otoacoustic emissions (distortion product or transient OAEs)
- Tympanometry with 1000 Hz probe tone
- Supplemental procedures, for example:
- Electrocochleography (ECochG)
- Auditory steady state response (ASSR)
- Acoustic reflex measurement (for 1000 Hz probe tone)
Time does not permit a review of the acoustic reflex pathways, but we do know how the acoustic reflex is generated and which structures are involved. By using acoustic reflexes in combination with OAEs, we're getting a tremendous amount of information, even though we're performing hearing screening.
Acoustic Reflexes in Neonates (Kei, 2012)
I want to cite one of my favorite studies involving acoustic reflexes. It is by Joseph Kei at the University of Queensland in Brisbane, Australia. It is a simple study and the results are so practical. The subjects of the study were 66 full-term infants with confirmed normal hearing. Using a 1000 Hz probe tone, they all had acoustic reflexes.
If you focus just on the broadband noise (BBN) stimulus, you'll notice that the average acoustic reflex threshold (ART) is 55 dB, which is quite good compared to pure tones (Figure 5). It was never more than 75. Essentially, if you use OAEs, and the OAEs are absent, and then you perform reflexes, you can almost always confirm whether the hearing is normal or if there's a hearing loss, by just using one stimulus: broadband noise. If the broadband noise reflex threshold is 90 or 95 dB, or there is no broadband noise reflex, then that combined with absent OAEs and normal tympanometry almost always suggest that there is a sensory hearing loss. Although we're not going to be using acoustic reflexes in every child, and it would not be feasible to use as a screening technique for that small percentage of children who do not pass the hearing screening with OAEs, acoustic reflexes can help sort out which children are more likely to have a hearing loss.
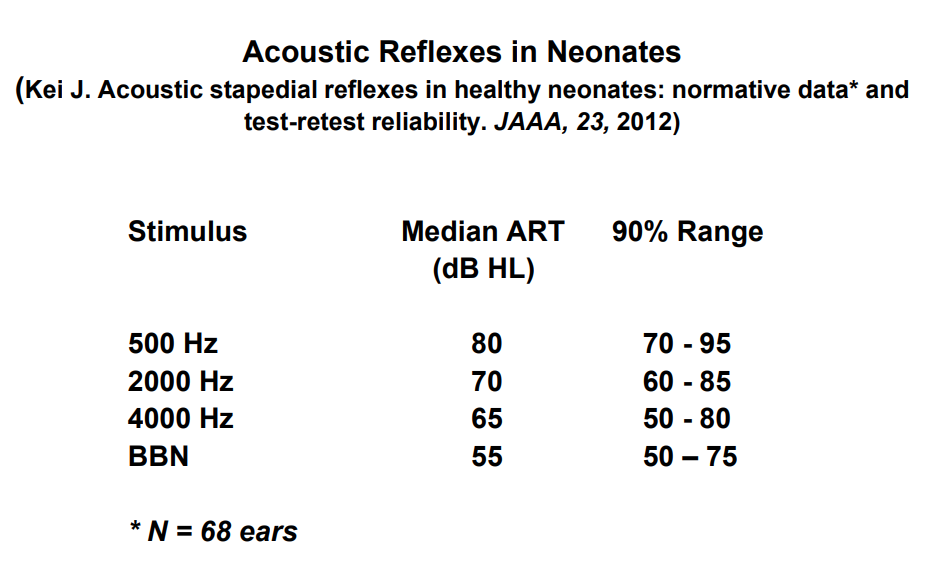
Figure 5. Acoustic reflexes in neonates (Data from Kei, 2012).
Simplified Sensitivity Prediction by the Acoustic Reflex (Hall & Koval,1982)
In 1982, I co-authored a study showing that if you look at the broadband noise acoustic reflexes threshold in a group of children with normal hearing and hearing loss, that the children with the normal hearing (20 dB or better) almost always had broadband noise thresholds or reflex better than 80 dB (Figure 6). As you get into the above 80 dB acoustic reflex threshold for broadband noise, you start worrying about a hearing loss.
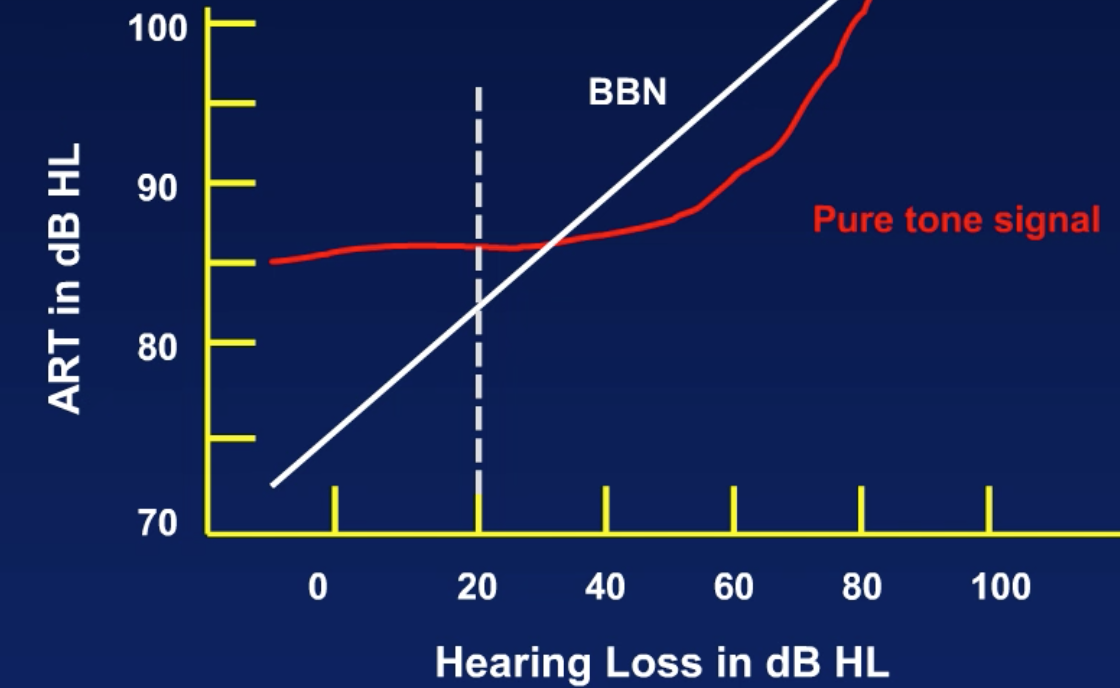
Figure 6. Simplified SPAR (Hall & Koval, 1982).
By combining OAEs with these other techniques, we can screen every child, even if they're very young (birth to three years). We'll start out with OAEs. If they pass, they pass. For this particular population, a "pass" would mean OAEs, not just six dB above the noise floor, but OAEs that have an absolute amplitude of greater than 0 dB (Figure 7). That's a little bit different than using OAEs for screening newborn infants, where we're just looking for a OAE to noise floor difference of more than 6 dB. This technique, using a criterion of more than 0 dB for the absolute amplitude for DP, brings OAE screening or into alignment with what we're doing with pure tones. With pure tone screening at 20 dB, our goal is to pick up anyone with hearing 15 dB or better. Our goal with OAEs then is to make sure we're picking up the same children, with hearing of 15 dB or better. We don't want to pass someone with DPs unless their hearing is normal. If they fail DPs in this very young group, then we go on with other measures, like tympanometry and acoustic reflexes.
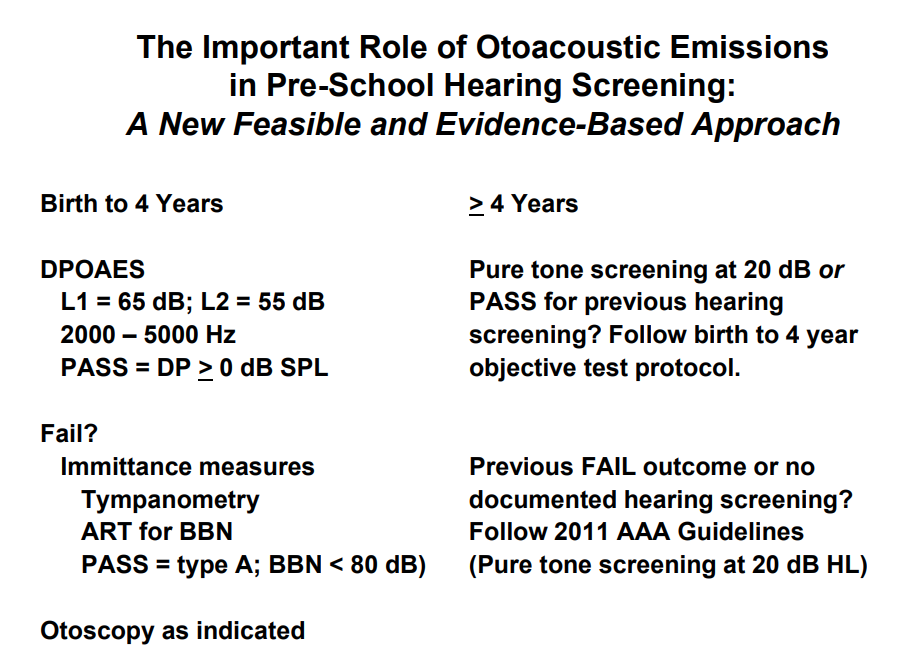
Figure 7. Pass/fail criteria, birth to 4 years and greater than 4 years.
For the purposes of today's presentation, I don't have time to discuss this in great detail. I have included references in your handout which explains it further. If a child's OAE exceeds 0 dB in amplitude, their hearing is most likely normal (Figure 8). If the OAE is less than 0 dB, they're probably going to have a hearing loss, although, some of those may be normal. This is criteria that we use for OAEs that's based on research to separate those with sensorineural hearing loss from those with normal hearing (Gorga, Neely, Ohlrich, Hoover, & Redneret, 1997).
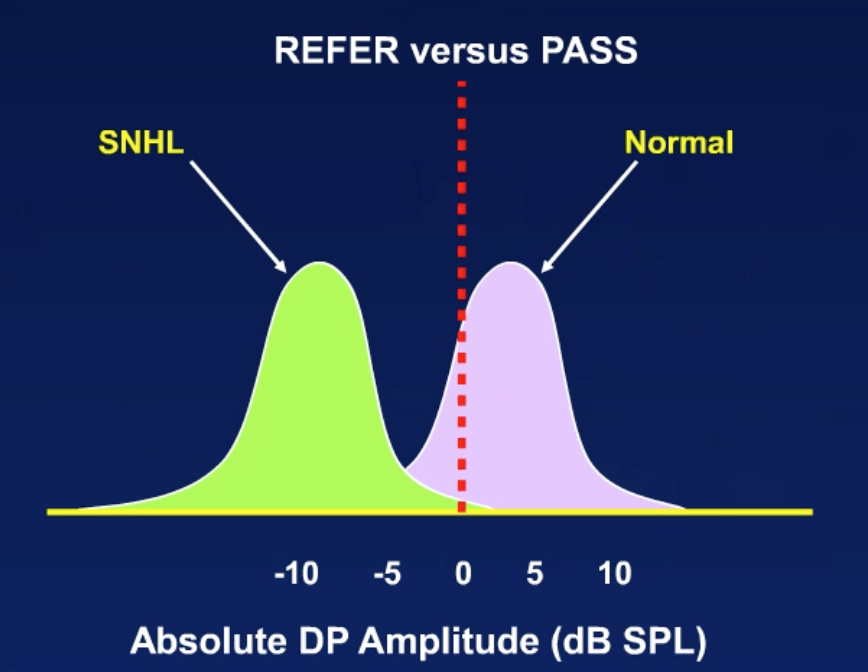
Figure 8. Refer vs. pass (SNHL vs. normal).
One neat thing with the GSI Corti is that it's a diagnostic device, so you can control the criteria that you use to pass and fail children (Figure 9). You can pick your frequency region, give it a name, and use whatever frequencies you want. For screening, we're usually going from 2000 up to 5000. You can create whatever pass or fail criteria you want, or you can have GSI do that. You have the flexibility of setting criteria that we want for preschool screening.
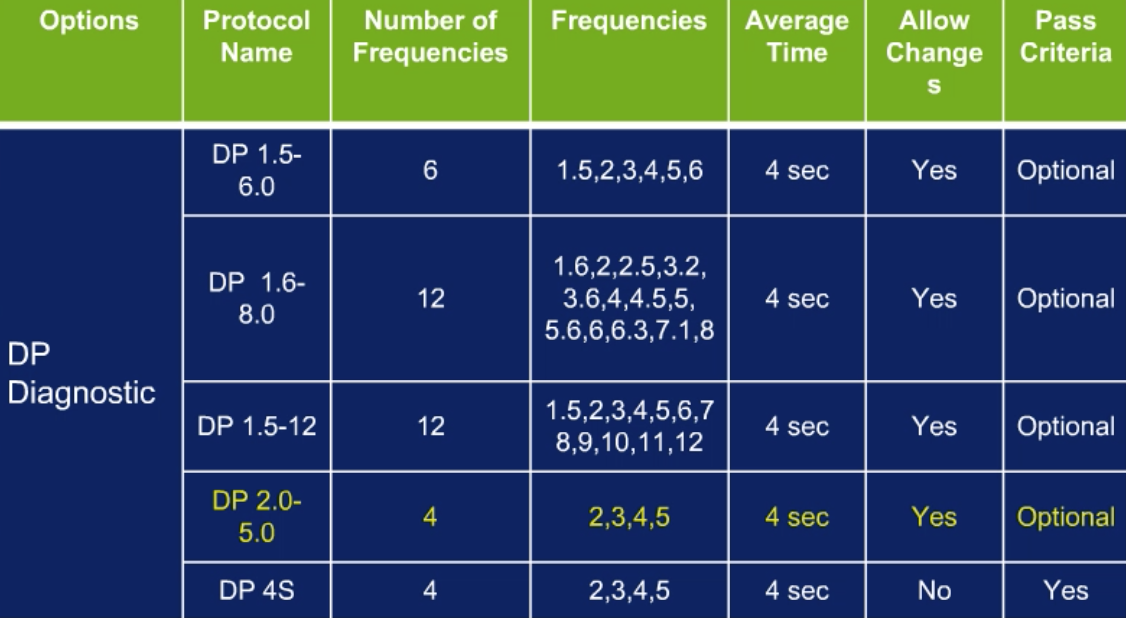
Figure 9. Creating a preschool DPOAE screening protocol (GSI Corti).
Summary and Conclusion
In summary, preschool hearing screening is essential for successful Early Hearing Detection and Intervention. Because of the loss to follow up problem, we can't rely on newborn hearing screening and the diagnostic assessment of those who do not pass. Some children are not getting the diagnostic testing like they should. Some children get the diagnostic testing, but they are lost to follow up before the intervention begins. We cannot ignore the fact that 15% of all children with hearing loss do pass their newborn screening. We need to have to have some way of detecting these children in their preschool years. We can't simply jump from the neonatal screening to school-age screening.
Additionally, as evidenced by the research, pure tone screening is not feasible for young preschool children. There are too many problems. In most cases, it must be done by an audiologist, and there simply are not enough audiologists to go around for all these preschool programs. OAEs are a feasible option, and there is a great deal of evidence in support of that. If we combine OAEs with other objective techniques, we can almost always sort out among the failures those with permanent hearing loss versus those with temporary hearing loss, like middle ear problems.
I recently published an article in the Journal of Early Hearing Detection and Intervention (JEHDI) which I encourage you to read. The article is titled "Effective and Efficient Preschool Hearing Screening: Essential for Successful Early Hearing Detection and Intervention." If you are interested, I'd be happy to send a copy to you. Finally, if you have any questions, you are welcome to email me at any time in the future (jwhall3phd@gmail.com). Thank you for your time and attention today.
Questions and Answers
I agree that OAEs are the gold standard for testing children. However, the majority of studies you cited involved children over the age of three who are more likely to be cooperative. In my practice, I find a large percentage of 10-month to two-and-a-half-year-olds that don't easily cooperate for OAE screening.
First of all, if we're going to be talking in relative terms, you'll still find far more young children cooperating with OAE screening than with pure tones. I would recommend that you select your protocol carefully, so that you are only focusing on higher frequencies (2000 to 5000 Hz). Stay away from the low frequencies, because background noise will interfere with OAE measurements. Start at a high frequency and work from there down lower. Make sure you have a protocol that can be completed in 30 seconds with most children. You don't need cooperation for more than a minute or two. Make sure that the child is as comfortable as possible. I prefer to test young children while they're sitting in a caregiver's lap, so they feel protected and comfortable. I don't perform OAEs after tympanometry. I don't want to traumatize the child by trying to get an airtight seal, and then attempt to do OAEs. I've screened probably over one thousand children over the years in Head Start programs in preschool. A lot of it has to do with preparation of the children. For mass screenings, their teacher can tell them what's going to happen. Once one child allows you to screen them, the others will usually go along with it as well. Although you may run into some children who are not totally cooperative, it should not be a common problem.
Do you recommend the same protocol for school-age children?
It depends on how old the child is. If the child is between two and four years old, pure tone screening would be just fine. Many school systems have pure tone audiometers for screening, but they don't have OAEs. In kindergarten, children can be screened with OAEs, but you're going to find that with 4-5% of children, it's very difficult to get pure tone screening. This is particularly true if you're doing the screening at the beginning of the kindergarten year, where the children are early five-year-olds. The younger the child, the more I will rely on OAEs. Another feasible other option is to use pure tones as your primary screening technique, but as soon as you can't get good pure tone results, have an OAE device available. That way you're not deviating from the standard that's been used, but you're able to screen all children.
Do you think that this could be expanded to school screenings throughout fourth grade, to take the burden off the nurses?
Absolutely. Here's the way I would recommend that you do it. Let's say you have a child in kindergarten and they're going to be in the same school over the years. You try to screen with the pure tones, but you keep OAEs handy. If they can't be tested with pure tones, use OAEs. From then on, in subsequent grades, that child always is screened with OAEs. Once you've passed the child with pure tones, you could use OAEs to monitor the child to detect any acquired hearing loss. You might say, "Well, once they're in school, we don't need to worry about delayed onset or progressive hearing loss." However, that is not the case. Recently, there have been some excellent studies in journals (e.g., the Journal of the American Medical Association) showing that in teenagers, the prevalence of hearing loss is even much higher than it is in kindergarten or first grade. A lot of it has to do with noise exposure, and music that they're listening to at high intensity levels. That's a very good strategy. First, try to document that they have normal pure tone findings. Then use OAEs to screen going forward. That will take a tremendous pressure off school personnel who are not comfortable screening young children.
References
Allen, R.L., Stuart, A., Everett, D., & Elangovan, S. (2004). Preschool hearing screening: Pass/refer rates for children enrolled in a head start program in eastern North Carolina. American Journal of Audiology, 13, 29-38. 10.1044/1059-0889(2004/006).
Bhatia, P., Mintz, S., Hecht, B.F., Deavenport, A., & Kuo, A.A. (2013) Early identification of young children with hearing loss in federally qualified health centers. Journal of Developmental and Behavioral Pediatrics, 34(1), 15-21. doi: 10.1097/DBP.0b013e318279899c.
Eiserman, W.D., & Shisler, L., Foust, T., Buhrmann, J., Winston, R., & White, K.R. (2007). Screening for hearing loss in early childhood programs. Early Childhood Research Quarterly, 22,105-17. 10.1016/j.ecresq.2006.09.001
Flores, G., Lee, M., Bauchner, H., & Kastner, B. (2000). Pediatricians' attitudes, beliefs, and practices regarding clinical practice guidelines: a national survey. Pediatrics,105(3 Pt 1), 496-501.
Fortnum, H.M., Summerfield, A.Q., Marshall, D.H., Davis, A.C., & Bamford, J.M. (2001). Prevalence of permanent childhood hearing impairment in the United Kingdom and implications for universal neonatal hearing screening: questionnaire based ascertainment study. British Medical Journal, 323, 536-54.
Gorga, M.P., Neely, S.T., Ohlrich, B., Hoover, B., & Redner, J. (1997). From laboratory to clinic: A large scale study of distortion product otoacoustic emissions in ears with normal hearing and ears with hearing loss. Ear & Hearing, 18, 440-55.
Grote, J. (2000). Neonatal screening for hearing impairment. Lancet, 355, 513-14.
Hall, J.W., & Koval, C.B. (1982), Accuracy of hearing prediction by the acoustic reflex. The Laryngoscope, 92, 140–49. doi:10.1002/lary.1982.92.2.140
Halloran, D.R., Wall, T.C., Evans, H.H., Hardin, M., & Woolley, A.L. (2005). Hearing screening at well-child visits. Archives of Pediatrics and Adolescent Medicine, 159(10),949-55. doi:10.1001/archpedi.159.10.949
Halloran, D.R., Hardin, M.D., & Wall, T.C. (2009). Validity of pure-tone hearing screening at well-child visits. Archives of Pediatrics and Adolescent Medicine, 163(2), 158-63. doi:10.1001/archpediatrics.2008.526
Ho, V., Daly, K.A., Hunter, L.L., & Davey, C. (2002). Otoacoustic emissions and tympanometry screening among 0-5 year olds. Laryngoscope, 112(3), 513-9.
Hunter, L.L., Davey, C.S., Kohtz. A., & Daly, K.A. (2007). Hearing screening and middle ear measures in American Indian infants and toddlers. International Journal of Pediatric Otorhinolaryngology, 71(9), 1429-38.
Kei, J. (2012). Acoustic stapedial reflexes in healthy neonates: normative data and test-retest reliability. Journal of the American Academy of Audiology, 23(1), 46-56. doi: 10.3766/jaaa.23.1.5.
Kreisman, B.M., Bevilacqua, E., Day, K., Kreisman, N.V., & Hall, J.W.III. (2013). Preschool hearing screenings: A comparison of distortion product otoacoustic emission and pure-tone protocols. Journal of Educational Audiology, 19, 48-57.
Krishnamurti, S., Hawks, J.W., & Gerling, I.J. (1999). Performance of preschool children on two hearing screening protocols. Contemporary Issues in Communication Sciences and Disorders, 26, 63-68.
Serpanos, Y.C., & Jarmel, F. (2007). Quantitative and qualitative follow-up outcomes from a preschool audiologic screening program: perspectives over a decade. American Journal of Audiology, 16(1), 4-12.
White, K.R. (2010, October). Twenty years of early hearing detection and intervention: Where we’ve been and what we’ve learned. Presentation at National Virtual Conference of the American Speech Language Hearing Association.
Citation
Hall, J.W.III. (2018, January). The important role of otoacoustic emissions in preschool hearing screenings. AudiologyOnline, Article 22091. Retrieved from www.audiologyonline.com

