Editor’s Note: This text course is an edited transcript of a live webinar. The recorded webinar is also available on AudiologyOnline. Download supplemental course materials.
Dr. Kim Cavitt: Today's webinar will cover ICD-10 and its implementation in an audiology practice.
Learning Objectives
As a result of this continuing education activity, participants will be able to list the implementation date of ICD-10, list the common ICD-10 codes used in audiology, and describe how to locate ICD-10 codes when presented with an uncommon diagnosis.
ICD-10: Monster or Mystery?
I want to demystify the entire system and procedure of ICD-10. It is just a new code set. Those of you who use paper superbills will just have a new superbill where you will circle a new code, although I will talk later about why you should consider moving away from paper superbills. Those of you with office management systems or electronic medical records (EMR) will load in the new codes that that you use most commonly in your practice and select the codes in the same manner you have done before. Most of us select the diagnosis code by description. Many of the descriptions are virtually the same, but all that is going to be replaced in the new code.
I want everyone to take a breath, because in audiology, this should be a straightforward transition with the right training and the right tools. ICD-10 goes into effect on Wednesday, October 1, 2015. That is the hardest part of this whole process because it is immediate from one day to the next. On Tuesday, September 30, your coding for that date of service will be in ICD-9. On October 1 and after, you will use ICD-10.
It is just a new set of codes, albeit more, and is nothing to be afraid of. The reason why there are more codes is because everything will be identified as either right, left, or binaural. A number of trainings will be available through the national associations of which you are a member. Below are some links to the three largest of audiology associations and the materials they have available on ICD-10.
- Academy of Doctors of Audiology - https://audiologist.org/ (members can log in to view ICD-10 resources and materials)
- American Speech, Language Hearing Association - https://www.asha.org/practice/reimbursement/coding/icd-10/
- American Academy of Audiology - https://www.audiology.org/practice/coding/ICD-10-CM/Pages/default.aspx
Differences between ICD-9 and ICD-10
By sheer numbers, ICD-9 is about 14,000 codes and ICD-10 is over 69,000 codes. There is more information that they are gathering in this code set. In our case, it is more ear distinction. There are more diagnosis and symptom codes. The code length is longer at up to seven characters. There is greater coding specificity, and the V and E codes we have used are now part of the regular code set. I want to note that although V72.19 (routine exam of ears and hearing) is now in a Z code set, it does not mean that the Z codes will be covered.
We should code diseases and conditions as well as symptoms whenever possible, and a Z code should also be utilized when appropriate, especially when it is related to failed screening or family hearing loss, as those are legitimate, medically necessary reasons for further hearing testing.
We do not know yet about how ICD-10 will affect payment or coverage. What I can tell you is that it is our responsibility is to code things based upon what we see at that time of visit, not as a rule-out. We are to code what the patient presents with or what we have found. As long as we stick with that mindset and explain that to patients, we should be okay. We do not code for coverage. The ICD-10 codes are alphanumeric except for the U. We are lucky, out of sheer coincidence, that many of the codes that we are going utilize will start with the letter H.
Remember not every insurance plan pays for routine or preventative tests for hearing loss. Because of that, you need medical necessity, and some of those diagnoses are not driving medical necessity, which could lead into a denial.
What You Need for ICD-10
Reporting
First, you will need to consult your local coverage determinations and Physician Quality Reporting System (PQRS) measures to know how ICD-10 influences these programs. For those of you who are not aware about either of these, I will talk about them briefly.
Local coverage determinations are where your Medicare Area Contractor, which is the entity that pays the Medicare claims in your state, has made coverage rules for specific procedures. That means is they are only going to pay for X CPT code procedure if a patient has a diagnosis of Y. You need to be aware if you have local coverage determinations in your locality, and if so, how those coverage determinations impact your ICD-10 coding.
PQRS does have some diagnosis-code-driven aspects when it pertains to the referral mechanism for acute and chronic dizziness. You are going to need to have the new ICD-10 codes for dizziness and benign paroxysmal positional vertigo (BPPV) that will drive that PQRS measure.
It is also important that you train your providers on the codes and these uses. Unless you have a certified coder, audiology services need to be coded by the provider themselves. It is important that the front office staff or billing staff know this, but it is much more important for providers to be educated on ICD-10 coding and how to do it efficiently and correctly.
Terms
One term used is "initial encounter". That is the first time you see a patient for this diagnosis. The "subsequent encounter" is the second time you see that patient for that diagnosis or condition. The "long-term follow-up" is the third visit and beyond for a single patient for that diagnosis.
An "unrestricted hearing loss in the opposite ear" means there is no hearing loss; in other words, the hearing in that ear is normal.
ICD-10 Examples
I have put together some of the codes that you might see commonly in audiology. Please refer to slides 5-20 in your handout as we go through these codes. (Note: The example codes provided in the text are for the bilateral condition for those with ear-specific classifications).
The first code is for abnormal auditory perception (H93.293), which is ear specific. People ask me often when to use this code, so this is my opinion. I would use abnormal auditory perception if I had a patient who came in for a hearing test suspecting hearing loss, specifically because of difficulties hearing in noise, especially if that patient reported a hearing handicap in the absence of a hearing loss. To me, abnormal auditory perception is a precursor of a central for processing deficit. For example, you have not yet assessed whether or not they have an auditory processing difficulty but you have determined that they have normal hearing and significant difficulties in noise. That is when I would use abnormal auditory perception.
Acoustic nerve disorder (H93.8X3) is something you could use for any acoustic nerve abnormality or problem. Acquired deformity of the pinna (H61.113) is a deformity that you were not born with; congenital is something you are born with. Acquired stenosis of the external ear canal (H61.303) can be collapsing canals or narrowing of the canal. If you are following your handout, you will notice that all of these codes have bilateral, right, and left designations.
Auditory recruitment bilateral (H93.213), right (H93.211), and left (H93.212) is next. Aural atresia (Q16.1) does not have a right/left correlate. On this list, barotrauma is the first procedure where we see the initial encounter (T70.0XXA), subsequent encounter (T70.0XXD) or second encounter, and then the long-term follow-up (T70.0XXS) for a patient. Bell's palsy is G51.0 and does not a right/left correlate. BPPV is a code that is going to correspond to PQRS measure 261. You need to make sure that you have this diagnosis as it will affect PQRS. Central auditory processing disorder (H93.25) is obviously not ear specific and is only used once you have done testing and have diagnosed the disorder.
Next is conductive hearing loss bilateral (H90.0), conductive hearing loss left ear with unrestricted hearing in the right (H90.12), conductive hearing loss in the right ear with unrestricted or normal hearing in the left ear (H90.11), and conductive hearing loss, unspecified (H90.2). There are different ways that you can code different hearing in different ears. Conductive hearing loss, unspecified is a way that you can code different hearing losses in different ears.
Delayed milestone in childhood is R62.0. A perfect example for using this code is you have a three-year-old who is not talking and they are coming to you for hearing testing. That means they have missed a milestone that would warrant audiological testing. Diplacusis is hearing multiple tones in an ear and is one of our codes (H93.223).
Dizziness (R42), again in my opinion, is a diagnosis that you use the initial time you see a patient. They have not been evaluated for that dizziness. With the focus on falls risk and with the importance of making sure that your patients are referred accordingly due to PQRS, remember that dizziness is one of the eight warning signs of ear disease that should be looked at before you fit hearing aids. It is important, regardless of our work setting, that we ask patients about dizziness and that we code dizziness when it is presented. Dizziness can be unsteadiness, falling, vertigo, spinning, and unsteadiness or spinning on your feet. That is a very catch-all diagnosis.
Eustachian tube disorder, unspecified (H69.93) is another set of codes with right, left, and binaural designations. Exostoses (H61.813) are bony growths in the ear canal, and they now have their own ear-specific diagnosis codes.
The next code is a Z code. Z codes in ICD-9 were in the V code set. I do have to state that in ICD-9 the use of a V code, especially in isolation of any other code, often times did drive denials. We do not know what that is going to mean in ICD-10, but I want people to be reticent, especially when a V code in ICD-9 was used in isolation with no other diagnosis code with it, about using this code and expecting reimbursement. Family history of hearing loss is Z82.2.
The next is foreign body in the ear with initial and subsequent encounter, for both left and right ears. Hearing conservation and treatment (Z01.12) is a code for a visit for which the sole purpose is hearing conservation treatment. The next is Z01.110, which is hearing examination following a failed screening. This code can be used whether it was a failed newborn hearing screening, a failed school screening, a failed occupational screening, or a failed screening in your audiological practice. It can also be used in conjunction with other codes to show why you did what you did.
People have asked for many years about whether or not there is a code for normal hearing. Now there is in ICD-10. The code for normal hearing is Z01.10, hearing or vestibular examination without abnormal findings. This is used if you have done hearing or vestibular testing and everything is normal. I want to stress that the people for which you can use this is not that common. Many people come in because they have tinnitus, dizziness, or pain, all of which have their own diagnosis codeS. You would use those symptom codes or what you found before you would use this. This is when all else fails. We have no idea how these Z codes will be processed.
There is also Z01.118, which is a hearing and vestibular examination with other abnormal findings. You may have not found audiological or vestibular abnormalities, but in their case history you found another abnormality that you would like to report. Also included are hematomas of the pinna (H61.12) for right, left, and binaural, and hyperacusis (H93.23).
Next is impacted cerumen (H61.23), which I would like to talk about briefly. There is a difference between impacted cerumen and cerumen in the ear canal. Impacted means covering clinically significant portions of the ear canal so that you cannot visualize the tympanic membrane (TM). It is often hard and requires professional removal. A little ball in the ear that still allows visualization of the vast majority of the ear drum which you need removed for testing or because of hearing aid is not considered impacted cerumen. The code should only be used in cases of true impaction.
There is a code for a labyrinthine fistula (H83.13), a code for malingering (Z76.5) which means feigning or exaggerating a hearing loss that does not exist to the degree that they reported. There is a code for Meniere’s (H81.03), but the classification of active and inactive has gone away. It is just Meniere's and is also coded by ear.
There is a code for mixed hearing loss, bilateral (H90.6). For clarification, mixed hearing loss is when you have both conductive and sensorineural components to the hearing loss. The ICD-10 makes distinctions for mixed hearing loss left ear with normal hearing in the right (H90.72), mixed hearing loss in the right ear with normal hearing in the left (H90.71), and mixed hearing loss, unspecified (H90.8), which is a code you could use to identify different hearing losses in different ears.
There is now a classification for noise effects on inner ear (H83.3X3). You might use this if someone has had a blast with hearing loss or a sudden hearing loss due to firing a gun or siren or something of that nature. Noninfective disorders of the pinna are ear-specific codes (H61.193). Next are otalgia codes (H92.03), otorrhea codes (H92.13), and perforation of the eardrum H72.93)
Ototoxicity
Ototoxicity is a set that is going to be coded very differently than other code sets. It is now a two-code combination (Figure 1). Not only do you code that the hearing loss is due to toxicity, but you also have to code what the toxic agent was. This set also includes the initial encounter where you make that diagnosis, subsequent visits or second visit, and the long-term follow-up.
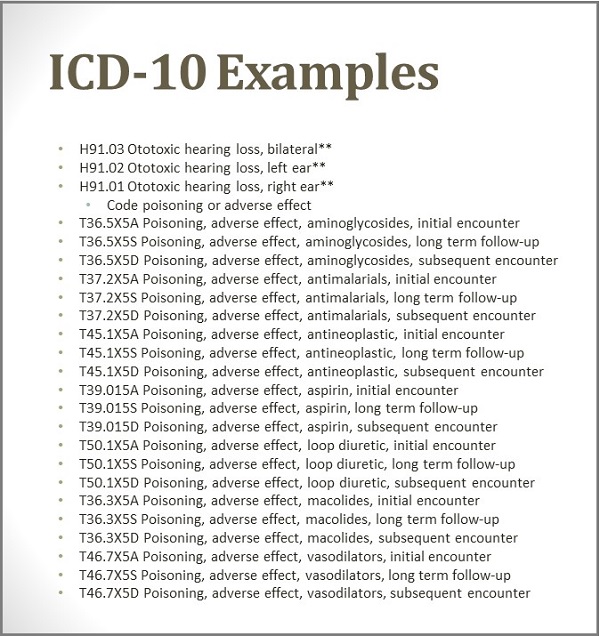
Figure 1. ICD-10 codes for ototoxicity and toxic agents.
You are going to see the most common of the ototoxicity agents: aminoglycosides in the antibiotic family, the antimalarial drugs, antineoplastics which are in the chemotherapy family, aspirin, loop diuretics such as Lasix that you encounter with high blood pressure and heart and vascular conditions, macolides in the antibiotic family, and vasodilators such as Cialis and Viagra. It is important that when we code an ototoxic hearing loss that that code does not stand alone. It needs to have with it the encounter and the toxic agent.
Next is sensorineural hearing loss, bilateral (H90.3), which is an important one for our everyday use. This will replace the ICD-9 code of 389.18. This is one you are going to need to remember. There is sensorineural hearing loss in the left ear with normal hearing in the right (H90.42), sensorineural hearing loss the right ear with normal hearing in the left (H90.41), and then sensorineural hearing loss, unspecified (H90.2).
Now we have speech and language delay due to hearing loss (F80.4). This is typically a child who has a speech delay and is hearing impaired. That would be a very viable code to use in pediatric settings.
Next are codes for sudden idiopathic hearing loss, bilateral (H91.23), left (H91.22) and right (H91.21). Another common code family we will use is for tinnitus: H93.13 bilateral, H93.12 left-ear only, and H93.11 right-ear only. These codes are used for both subjective and objective tinnitus.
Lastly, we have vertigo codes, which are made up of aural vertigo (H31.313), central vertigo (H81.43), and peripheral vertigo (H81.393). This would be coded after you have performed vestibular testing and you have come to a diagnosis. Once you have the diagnosis, you stop using the code for dizziness (R42) and instead use a code for BPPV or labyrinthine fistula or whatever kind of vertigo you determine. Vertigo peripheral will be something that you will commonly use if you do vestibular testing.
Coding Know-How
There are going to be some different ways to code different things. I want to make sure that everyone understands the most common codes that we will use, how to code different hearing losses in different ears, and how the code the two-code combination.
One of the codes you can use when you have different hearing losses in each ear is H90.8. This is an example of a mixed hearing loss, unspecified. For example, say you have a mixed hearing loss in your right ear, and then use H90.5 for sensorineural hearing loss in the left ear. You can also use the conductive hearing loss, unspecified, H90.2 if that is what existed in that ear.
There is also a set of codes that are called “other specified hearing loss” and that would be a code like H91.8XI. This means you have other specified hearing loss in your right ear. Then you could then go with H91.8X2, which is other specified hearing loss in your left ear. That could be a different way to code different hearing losses in different ears. Another code that you might use is H90.2, which would be a conductive hearing loss, unspecified.
This is a good time to bring up the fact that this is not our dream sequence of code. Are there codes changes we would like to make? Absolutely. Just because you want to make changes does not mean that we get to do so. We have been told that at the earliest we may be able to make changes that would go into effect is 2017. This is another opportunity for me to say that it is very important that to read the releases and education materials about coding and reimbursement from your national associations when you receive them. There are many of us spending a lot of time trying to create materials to be educational for our people. Read the materials and follow the guidance as closely as possible.
Coding Ototoxicity
Let's talk about toxicity from a vasodilator such as Viagra. To code this, you would document the first date that you notice the condition. A typical toxicity from Viagra is a sudden hearing loss; it is not an uncommon occurrence with Viagra. You would first code H91.02, which is ototoxic hearing loss left ear, and then you would need to add the toxicity agent T46.7X5A, which is poisoning or adverse effect of the vasodilator, initial encounter. That is your first test date that you diagnose this ototoxic hearing loss.
Unrestricted
Again, unrestricted means that you have normal hearing in the opposite ear. You are only going to use those diagnosis codes that have “unrestricted” when the other ear is normal. This is how we will code normal hearing, but only in the absence of other symptoms and diagnoses with which the patient may present. This is because we have no idea how this will be handled in terms of reimbursement.
This is how we will code normal hearing, and again is the hearing and vestibular exam without abnormal findings. However, this code should only be used in the absence of other symptoms and no other diagnosis, because we have no idea how this will be handled for reimbursement.
Commonly Used Codes in Audiology
I want to focus on the wheelhouse codes that we will use often in our practices.
The first is abnormal auditory perception. This is a code whereby you will need to determine how you are going to use it and use it consistently. This will be for your acoustic nerve disorders, vestibular schwannoma or acoustic neuroma. BBPV will be common, and it is tied to a PQRS measure 261. A diagnosis BPPV would come after you have done the Dix-Hallpike maneuver.
The conductive hearing loss families are ones that you will need to pay close attention. Dizziness is also one of the two diagnosis codes embedded in to PQRS measure 261. The other two PQRS measures with which we are involved are documentation of current medications and screening for clinical depression; those do not have diagnosis code markers, but are done regardless of the diagnosis. Again, you need to be aware of dizziness and BPPV for measure 261.
It is important that you have an encounter form that reflects all the codes you use most commonly. Impacted cerumen will be common, as will Meniere's, the mixed hearing loss family, ear pain or otalgia, ototoxicity if you do ototoxicity monitoring, the sensorineural family, and the tinnitus family.
Practice Preparation
Transition
You need to start thinking about how you are going to transition to ICD-10. If you use a paper superbill, then you need a new paper superbill with ICD-10 code defined down for your practice. If you use an audiology office management system like Sycle, TIMS, Counselor Complete, Hearing Fusion, HEAR form, Simply Hearing, or Blueprint, you need to make sure that the codes that you utilize are loaded in the database. It is not the responsibility of the office management system to make sure that the ICD-10 code that you need is loaded.
For electronic health records, such as EPIC, you need to talk your administrator or IT person to make sure that the codes that are related to hearing loss are loaded and readily available to you. It is of utmost importance that you take that step so that you are ready to go on October 1.
Education
Review and read the material sent you by national associations of which you are a member. Educate your staff and providers on new code set. The beauty of AudiologyOnline is that it is open platform where your staff can register and view any of the materials that relate to ICD-10. You can do internal testing with your providers where you spend a day and you code. You do not submit those claims, but you code those visits in ICD-10 so you feel comfortable and ask your questions to people like me or others in the field who are working on this.
Budget
Create a budget for implementation costs. How much, if you have paper superbills, will that cost? How much are you going to need to spend on IT time? How much you going to need to spend on training? If you read a lot about ICD-10, the medical community is having people focus on whether or not you have the financial resources to withstand slow payer payments as a result of ICD-10 implementation. We know that this is going to throw some payers, especially small payers and the Medicaids of the world, for a loop. It may result in unnecessary denials and slow payments because they are having trouble processing claims. You may need to have set aside a financial reserve if your cash flow is affected by slow payments.
Electronic Claims
This is another great opportunity to stress that the days of paper claims are over. If you are submitting to insurance via paper claims and not submitting electronically via an office management system, this ICD-10 transition will become a nightmare. Paper claims will be the last thing processed. Many payers, if you are signing a new agreement as a new provider, do not allow paper claims.
There is little to no reason for paper claims in this day and age. Almost every insurance payer, such as Blue Cross/Blue Shield, United Healthcare, Aetna, and CIGNA have mechanisms where you can submit claims directly to them through their websites. There are many affordable audiology office management systems that are available to purchase so you can submit claims electronically.
Resources
There are a lot of resources available for your use. You will need a manual or software to access for reference. I use materials from the American Medical Association (AMA) bookstore or from Optum, which is a subsidiary of United Healthcare and used to be called Ingenix. You can buy Encoder Pro from Optum or Code Manager from AMA, which gives you electronic access to the manuals. Some people still do like touching and feeling of a paper manual, but again there are ways to do it via software access.
There is also a website called www.icd10data.com. This is a free website where you can type in the condition and look up a code. You want to get the most specific code possible, just like we needed in ICD-9. The problem is that it will not let you visually look at an entire code set of the audiologic code family. It is search tool; it will not show you whole lists.
The national associations all have ICD-10 code lists that are common to audiology available on their websites. However, we are all going to be presented with situations where we need a diagnosis that is not every day to audiology. Remember that If it is documented by a physician, you can use that other diagnosis, like otitis media, but audiologists cannot diagnose otitis media. If that is put on the order or referral from the ordering physician, or if that is in the EMR of why that physician is seeing that patient, that code is available to you. That is when you may need to go look up diagnoses in a software search engine or the manual.
Questions and Answers
What ICD-10 code do you report when results are normal?
As discussed, that is the code Z01.10, hearing and vestibular examination without abnormal findings. I cannot stress enough that is a Z code. If the patient reported tinnitus, you would use that instead. If the patient reported dizziness, you would use that instead. Any other condition they report is the primary code you use. Z01.10 is the code to use when you have no other option.
Some of these codes are for medical diagnoses like Meniere’s. Since audiologists cannot diagnose medical disorders, can we use these codes?
Yes. You can use those codes if they have been documented by a physician or someone who is practicing within their scope of practice either via the order, a report that they sent to you, or in a shared medical record or EMR.
How many codes can you bill at each encounter, especially if the patient presents with multiple symptoms?
On the new CMS 1500 form, you can have up to 12 diagnoses. HIPAA 5010 allows now up to 12 diagnoses. That could vary payer by payer, and we will see how that flushes out as time goes on.
What happens if you need to resubmit a claim after October 1 for a date of service prior to October 1?
You would use ICD-9. It is all about the date of service, not the date you submitted the claim.
Is there a chance the implementation date of October 1, 2015 will change?
Yes, there is. However, when the bill for the Medicare fix was passed, there was no mention of pushing the implementation date back, and this is where we expected that date change to have occurred. That bill is still has to go through appropriations for its funding. Could the date change during that process? Yes. Do I think it is likely based upon what I have read? No. Given how close now we are how much time and money has been invested, I do not believe that it will get pushed back again.
What code would you use if you are removing earwax in the canal, but it is not impacted?
This is just my opinion, but I would use foreign body in the ear.
How long will payers accept claims on ICD-9 on HCFA 1500?
The HCFA 1500 form has not been accepted for over a year now. You need to be using a CMS 500 form. They will accept it as long as you are timely claims filing. Every insurance payer has something called timely claims filing, which means that you have so many days to submit to them a clean or a perfect claim. They will accept dates of service prior to October 1, ICD-9 as long as you are in the timely claim filing limit. For Medicare, it is 365 days. There are some insurers for which it is 30; some are 90; some are 120. You need to determine what the timely claims filing is, and that can vary payer by payer.
I want to stress that a lot of paper claims never make it to claims processing. That is just not how it is handled in this era. You really need to be submitting claims electronically. There is no excuse not to be doing it, because there are free systems available from the payers themselves to submit claims to them electronically. Medicare, I believe, will say no more paper claims eventually. So they will accept a CMS 1500 form within the timely claims filing limits with ICD-9 codes.
Is there a chance of nonpayment if the physician sees the patient first and uses a more specific code, such as BPPV, when they have not yet been tested? For example, the MD should use dizziness and then after the audiology test, it becomes BPPV.
Is there a chance of nonpayment? No. You can use a rule-out diagnosis until you have ruled it out. In the case of the physician, they are using BPPV because it has not been ruled out. In our case, if the physician uses BPPV first and then you use dizziness, that will not affect payment. Remember that they typically are going to be on different claims, unless we are billing Medicare. It is not going to make a difference. We would not use BPPV unless we actually diagnosed it. We could use it as a rule out diagnosis until we actually determine that they have it or not.
Rule-out diagnoses should really not be used. These codes are how the World Health Organization and the Centers for Disease control determine incidence of a condition. Using rule-out diagnoses for things we know the patient does not have changes the incidence of these conditions on paper. It is more important to be as specific as we can once we know something, but until that time, we use things like dizziness, which are more benign. This should not drive a denial. You should be responsible for your code and not what the physician is using. You can use the physician code if you need something better, but audiologists should really focus on coding things for themselves. We have an expansive scope and things that we can code without relying on the physician.
Cite this Content as:
Cavitt, K. (2015, August). ICD-10: effective implementation in an audiology practice. AudiologyOnline, Article 14492. Retrieved from https://www.audiologyonline.com


