This article is an edited transcript of a Signia webinar on AudiologyOnline.
Learning Objectives
After this course, participants will be able to:
- Provide a definition of tinnitus and its mechanisms.
- Describe various acoustic treatment protocols currently available.
- Demonstrate how to program the Signia tinnitus therapy feature.
Tinnitus Overview
First, we're going to take you through the epidemiology and mechanisms of tinnitus. Then, we will explain how to adjust the Signia tinnitus therapy feature for your patients. This may be review for many of you, but we think it's important that we are all on the same page with regard to our tinnitus patients.
Definition
There are two types of tinnitus: subjective and objective. For the purposes of this presentation, we will be mainly focusing on subjective tinnitus, as that is the type for which patients usually require treatment. Subjective tinnitus has been defined as the “perception of a sound in the ears or in the head without the presence of an external source generating that sound.”
Epidemiology
The American Tinnitus Association (ATA) estimates that 50 million Americans have some degree of tinnitus. Of those, 20 million experience symptoms severe enough to seek medical help. The Tinnitus Practitioners Association (TPA), which promotes best practices in tinnitus for audiologists, suggests that 30% of patients over the age of 65 report tinnitus.
We know that tinnitus goes hand-in-hand with hearing loss; as such, the incidence of tinnitus will rise with age. Tinnitus effects 10-17% of the general population, but 30% of people over the age of 65. According to the TPA, 5% of those who report that they have tinnitus are seeking care, and 2.6 million feel that their tinnitus is a debilitating problem.
Causes
As hearing care professionals, we're very familiar with the causes of tinnitus that occur along the auditory pathway, including (but not limited to):
- Cerumen
- Otitis
- Otosclerosis
- Acoustic neuroma
- Meniere's disease
- Acoustic trauma
- Noise exposure
- Ototoxicity
- Presbycusis
We may not be quite as familiar with other causes for tinnitus that occur outside of the auditory pathway, such as:
- Metabolic issues
- Cardiovascular conditions
- Neurological disorders
- Pharmacological reactions
- Temporomandibular Joint Disorders (TMJ)
- Psychological trauma
- Dietary factors (e.g., caffeine)
A person experiencing tinnitus may have a combination of these conditions (including others that we did not highlight). A person may have had tinnitus symptoms that at one point, they did not find bothersome. However, combined with other conditions, their symptoms were exacerbated, increasing their tinnitus to an uncomfortable level.
The Tinnitus Research Initiative (TRI) has a very informative website that we recommend you visit. You can spend quite some time searching through all of the different causes and workflows for treatment that are available. There is a flowchart that puts into perspective the areas on which hearing care professionals need to be focused when it comes to management of a person with tinnitus, as well as the importance of an multidisciplinary approach. Specifically, we can address sensorineural hearing loss that may accompany tinnitus, and provide auditory stimulation via amplification and/or sound therapy.
Impact on Daily Life
Why is it that tinnitus affects some people and not others? Seidman and Jacobsen (1996) looked at the impact of tinnitus, and it hasn't changed much over the last 20 years. According to their data, of patients who report some level of tinnitus, 80% say that it’s not having a significant impact in their life and so they do not seek care. About 20% of tinnitus sufferers are looking for some remediation of their tinnitus. Out of that population, 15% that feel that it has an impact and they would like to do something about it. About 5% of people that feel their tinnitus is incapacitating; it's affecting their lives so much that it’s preventing them from functioning in a normal way.
What are the possible repercussions on a patient’s life if they have tinnitus? There are four different areas that Dr. Rich Tyler at the University of Iowa has identified: sleep disturbance, difficulty concentrating, poor emotional balance, and decreased socialization. If a person is experiencing one or more of these disturbances, it may have a significant impact on their quality of life.
Why Do Individuals Have Different Reactions to Tinnitus?
Why is it that 80% of people who have tinnitus are not bothered by it, while 20% seek help? To understand why, it is helpful to refer to the neurophysiological model of tinnitus. If you are at all familiar with tinnitus therapy, then you will likely have heard the name Pawell Jastreboff. In the 1990s, Dr. Jastreboff introduced the neurophysiological model of tinnitus. According to this model, our central nervous system can suffer persistent functional changes in its circuitry secondary to a loss of input in the auditory system, and these changes can manifest as tinnitus.
If the cause of the tinnitus comes from the cochlea itself, the patient has some hearing loss. As such, they have a lack of stimulation due to that hearing loss, resulting in overstimulation that causes them to perceive tinnitus, which is detected on a subcortical level. We know that the majority of people (80%) who perceive tinnitus will dismiss it as no big deal and go on with their lives.
However, if you attach an emotional association to that tinnitus, then you can start having a different reaction. When we look at that 15% that feel that the tinnitus is affecting their lives, it's usually because they have some kind of a negative emotional association with it. For instance, maybe they woke up one morning, and all of a sudden they have tinnitus. Usually, when something happens like that with sudden onset, people get worried about it. They wonder, "Is there something wrong? Do I have a tumor? Am I always going to hear this?" They start to attach negative emotional associations with the ringing sound. When they do that, the perception of the tinnitus gets caught in a loop of anxiety, which exacerbates the problem.
In the 5% of people who become incapacitated, it starts with a reaction from the autonomic nervous system, and now they have a physical response associated with tinnitus.
One example that I will share is with ringtones. Many of you have individual cell phone ring tones for different people in your lives. Imagine that you have a friend who only calls you when they are in some kind of trouble and need help. As a result, you may develop an emotional reaction to the ringtone and every time you hear it; you worry that it is bad news from your friend. It can quickly become an autonomic nervous system reaction; when you hear the ringtone, you get sweaty palms, your heart rate goes up, etc.
The treatment for that kind of reaction would be to change that ringtone and then try to deal with the problem. It's a good example of how someone can have an emotional reaction to a stimulus, and end up with a physical reaction as well.
Habituation
The way to eliminate the emotional and physical reaction to the symptom of tinnitus is to use habituation. Habituation is a natural process that we go through. It is the reduction or elimination of central nervous system activity in response to repetitive stimuli. We manage a lot of input to our nervous system throughout our days, and the brain cannot attend to everything at once. Your brain will naturally pick out those things that stand out from the environment and habituate, or not pay attention, to other things.
For example, during a telephone conversation, my air conditioner may automatically turn on. My brain recognizes, "That's just the air conditioner. It's no big deal. It's a new sound, but I don't need to attend to it." I will naturally habituate to it and stop noticing it after a few seconds or minutes.
According to the neurophysiological model of tinnitus, if there is no emotional association to the tinnitus, habituation will naturally occur. The brain will dismiss it as not important. If you do have an emotional association, then you can spark activity in the limbic system and the autonomic nervous system. This activity can lead to needing treatment to help facilitate habituation.
Visual Analogy
To help patients have a realistic expectation of tinnitus treatment, it is important that they understand we are not going to cure the tinnitus. We can't remove tinnitus altogether. We can take away the focus on it. Think about a candle in a dark room as compared to a candle in a lit room. When you are focusing on your tinnitus, it is like having a candle in a dark room. That's the only source of light, so that is all you see, and it is a prominent feature. If we add another light source to the room, then the candle becomes less significant; it's still there, but it's not providing all of the light. That's what we want to do with auditory stimulation for someone with tinnitus. We want to ensure that they have a well-rounded and enriching auditory environment. In doing so, we can help them habituate to their tinnitus.
Clinical and Audiologic Evaluation
Let's look at the clinical evaluation of someone reporting this symptom of tinnitus. First, the patient should receive a complete workup to rule out a medical cause for the tinnitus (a tumor, cardiovascular issues, etc.). Then, we consider auditory stimulation. In addition, we need to consider using cognitive-behavioral therapy in conjunction with auditory stimulation.
Medical Management of Tinnitus: Role of the Physician
At times, patients may seek your services after they've already had a medical workup for their tinnitus. However, you may have patients who come to you first, before they see a physician. It's important to know when to refer to relevant specialists for evaluation and treatment. Shi and colleagues (2014) explain the reasons for a multidisciplinary approach in managing tinnitus. They highlight five reasons for a physician referral for tinnitus patients:
- Suggestion of underlying disease, including unilateral tinnitus or sudden onset of tinnitus. If someone has not seen an ear, nose and throat physician and they're reporting tinnitus that's unilateral in nature or that has occurred suddenly, they should be referred for a medical workup.
- Clinical and audiometric testing suggests otologic or neuro-otologic conditions. If it looks like a person could have an acoustic neuroma (for example if acoustic reflexes are absent), we have to refer. If there are signs of a middle ear condition such as otosclerosis, or conductive hearing loss, a referral is indicated. In some cases, treatment of the underlying medical condition may resolve the tinnitus.
- Comorbidities such as anxiety, depression, or insomnia. Know when to refer to a psychologist or a psychiatrist if your patient is exhibiting these issues.
- Systemic diseases: a medical referral can rule out hypertension, autoimmune disease, and abnormal thyroid functioning as possible contributors to the tinnitus. Refer to a physician to rule out an underlying physical issue that could be the cause of the tinnitus.
- Other non-auditory factors, such as financial hardships, personality/behavior problems, relationship difficulties, stressful situations. These conditions are often overlooked. Refer to the appropriate professionals, such as psychologists or other support professionals, who can offer assistance with hardships.
Tinnitus Clinical Practice Guidelines – AAO
The American Academy of Otolaryngology (AAO) has produced clinical practice guidelines for ear, nose and throat physicians (Tunkel et al., 2014). On the panel of experts to help develop these guidelines, were prominent audiologists within the field of tinnitus research: Dr. James Henry, Dr. Craig Newman and Dr. Richard Tyler. What they have recommenced is to first gather a proper case history, perform a physical exam and a comprehensive audiology evaluation. Educate the patient on the key points of tinnitus. Conduct a hearing evaluation. Cognitive-behavioral therapy is recommended; the AAO guidelines indicate it is useful in tinnitus management.
Per the AAO guidelines, an optional recommendation is the use of sound therapy or sound generators. The research has suggested that hearing evaluations and hearing aids do help in the remediation of tinnitus. Hearing aids that have sound generators also help in the remediation of tinnitus. However, the research has not been able to definitively prove whether or not sound generators produce a better response than the hearing aid alone. There's more research going on in that area and we may see new evidence emerge in the future on this topic. The fact that it's optional does not mean that you should not use it; it's just that not every patient may need it. We want to fit hearing aids on those that need them. We want to fit sound generators on those that need them as well.
Finally, the AAO guidelines indicate that there is no evidence to support medications or supplements to treat tinnitus. They also do not recommend transcranial magnetic stimulation, or routine imaging studies. With regard to acupuncture, they offer no recommendation. The guidelines indicated that some people find acupuncture useful and some people don't, so AAO took a neutral stance on the use of acupuncture in tinnitus management.
Clinical Practice Guidelines – AAA
The American Academy of Audiology (AAA) suggests using a multidisciplinary approach to manage tinnitus. The AAA clinical practice guideline can be found here. AAA recommends gathering your usual case history as you would for any hearing patient, but also obtaining medical history, specifically looking at the symptom of tinnitus. Conduct a complete audiologic evaluation, in addition to the psychoacoustic measurements for tinnitus. Many of us have learned how to do these, but we may not be performing them regularly. We will discuss why and how to do these psychoacoustic measures later in this presentation.
Tinnitus Evaluation
Questionnaires and Scales
If a patient comes into your office reporting hearing loss and also symptoms of tinnitus, it is helpful to administer a questionnaire to specifically focus on the tinnitus. There are several great tinnitus questionnaires available and we will review some later in this presentation. They tend to be very lengthy because there are a lot of things that we want to be able to rule out. A questionnaire can help get to the root of the problem and know whether you need to refer this person to other professionals. For example, if a patient is experiencing tinnitus that's due to cervical spine issues, there are questions on the intake that ask if there is anything the patient can do to make their tinnitus worse or better (e.g., moving their neck in a different position).
Psychoacoustic Measurements
Psychoacoustic measures for tinnitus are important for counseling. Measuring pitch, loudness, and minimum masking level do not have a relation to the diagnosis or prognosis of treatment. Whether or not you can mask tinnitus in a minimum masking level test is not going to predict how they're going to do with habituation treatment. An important part of habituation is the counseling. A pitch match helps to assure your patient that you understand the sound they describe that they're hearing. A loudness match helps your patient understand that the sound they are hearing is only slightly above their hearing threshold level, even though they may perceive the sound as very loud and invasive.
Minimum Masking Level (MML)
MML indicates whether or not tinnitus can be masked or partially masked. In addition, it may provide the patient with hope of treatment. This may be the first time someone has been able to mask out or eliminate the tinnitus that they hear. This can give them hope that there is a treatment available in the future. Keep in mind that not all tinnitus can be masked. It is possible that you will get to a point at which the masking sound is so loud that you need to stop testing but the tinnitus is still be there. That's okay, because with habituation, the goal is not to fully mask the tinnitus at any point in time.
Procedures: Pitch Match, Loudness Match, MML
Today’s course handout includes some of the procedures highlighted on the Tinnitus Research Initiative website. You can also find them in your audiology textbooks. They include the procedures for doing a pitch match, a loudness match and a minimum masking level. Follow the steps in the handout and you can add these psychoacoustic measures to your office protocol. If you bill insurance for hearing testing, you may also be able to bill for tinnitus evaluations. It's important to note that all three of the measures need to be done in order to bill for a tinnitus evaluation.
Annoyance Evaluation
Evaluating a patient’s level of annoyance is highly subjective and difficult to measure. We need to find out how handicapped the patient feels from their tinnitus. For that, we're going to use self-reported tinnitus questionnaires, such as the Tinnitus Handicap Inventory, the Tinnitus Primary Function Questionnaire, and the Tinnitus Reaction Questionnaire. These are just a few of many questionnaires that are available.
Questionnaires
Let's go into a little more detail regarding questionnaires. These questionairres can be used both as intake measures and as outcomes measures.
Tinnitus Reaction Questionnaire (TRQ; Wilson, Henry, Bowen, & Haralambous, 1991)
The Tinnitus Reaction Questionnaire is comprised of 26 questions and measures the change in coping ability before and after treatment. The patient simply reads the question, and using a scale (0-4) rates whether their tinnitus has no impact on them, or if they experience this almost all the time.
Tinnitus Handicap Inventory (THI; Newman, Jacobson, & Spitzer, 1996)
The Tinnitus Handicap Inventory measures the patient’s distress associated with tinnitus. It consists of 25 questions. Your patient is going to respond in one of three ways: "Yes, this is a problem," "No, it's not a problem," or, "Sometimes it affects me." When they are finished, you score their test. The result is an outcome level as to whether their case of tinnitus is affecting them very lightly, mildly, moderately, severely, or if it's catastrophic.
Using Inventories as Outcome Measures
Surr and colleagues (1999) conducted a study using the Tinnitus Handicap Inventory to see it could be used to measure a significant difference after treatment. There were 34 participants, all of whom were hearing aid users with complaints of hearing loss and tinnitus. Outcome measures were obtained six weeks after the hearing aid fittings using the THI and Abbreviated Profile of Hearing Aid Benefit (APHAB). The results found that hearing aid use significantly reduced tinnitus handicap for participants as a group, although the effect was typically small. Further, the benefit for tinnitus handicap did not increase systematically with the severity of unaided tinnitus handicap. Overall satisfaction ratings were weakly related to THI benefit, and overall satisfaction ratings were significantly related to benefit on the speech scales of the APHAB.
These results are significant in that you always want to show outcomes to reinforce to your patient that habituation is working. It's also important to show outcomes from a billing standpoint. If you're billing for tinnitus therapy, you want to have something to back up and validate the procedures that you're using.
It's also helpful that the Tinnitus Handicap Inventory correlates well with the Visual Analogue Scale (VAS). Hospitals frequently use scales like this to assist patients in rating their pain, to determine when to give pain medication. You can use this scale to help create a better workflow for your tinnitus patients. Rather than have your patient sit down and fill out all of that paperwork right then in your office, you can have them simply rank on a scale of 1-10, "How does your tinnitus make you feel?" If they're scoring above a 4, you may have them come back for a complete tinnitus evaluation. Or, you can use the VAS to evaluate your workflow. If you have one particular provider on your staff that likes to specialize in tinnitus patients, you might cycle patients that are scoring more highly on the VAS into their schedule. Use of the VAS can help to create a better workflow.
Tinnitus Primary Function Questionnaire (TPFQ; Tyler et al., 2014)
The Tinnitus Primary Function Questionnaire was developed the University of Iowa. Its purpose is to address workflow. The TPFQ is a quick, 12-question tool that looks at four areas in which tinnitus can affect a person’s life: emotions, hearing, sleep, and concentration. It has been shown to be valid and sensitive to all four of those areas. It can help you to determine where to concentrate your treatment and your counseling for the patient.
We have a tinnitus mentoring program at Signia, and we can provide you with copies of questionnaires and handicap inventories. Contact your field sales representative for more information about the tinnitus mentoring program.
Acoustic Treatment Protocols
After you have established protocols and processes for a comprehensive clinical evaluation for patients with tinnitus, you can begin developing acoustic treatment protocols that you will offer. The following is a list of considerations for acoustic treatment protocols.
- Regardless of what traditional protocol you may adopt, it is always recommended that you start with amplification alone. You always need counseling as well.
- Tinnitus Activities Treatment (TAT) was developed by Dr. Rich Tyler and his team from University of Iowa (Tyler, Gogel, & Gehringer, 2007). TAT is accessible on the University of Iowa's website.
- Tinnitus Retraining Therapy (TRT) was developed by Dr. Pawell Jastreboff (1990). TRT certification is offered a few times a year. TRT follows a very directive approach with counseling.
- Progressive Tinnitus Management (PTM) was developed by Dr. James Henry for the VA. Information can be found at www.ncrar.research.va.gov
- Cognitive Habituation Tinnitus Treatment (CHaTT) was developed by Dr. Natan Bauman. It is a modified TRT program which also includes cognitive behavioral therapy, pictorial representation and music for distraction and relaxation. More information can be found on Dr. Bauman’s website, including CHaTT courses. They're offered all around the country at different times of the year.
- Finally, we'll review some general sound therapy alternatives. As a rule, you should always start off using amplification alone, and you may adopt another protocol or a combination of protocols. However, when the patient or the tinnitus sufferer takes off their amplification, they still need something to get them through the night. That’s where these alternative therapies are useful.
Acoustic Treatments - Visual Analogy
The following cartoon presentation has been adapted from a presentation by our colleague Gyoergy Varallyay from Germany that he has allowed us to share. This is a visual analogy that demonstrates how acoustic treatments address tinnitus.
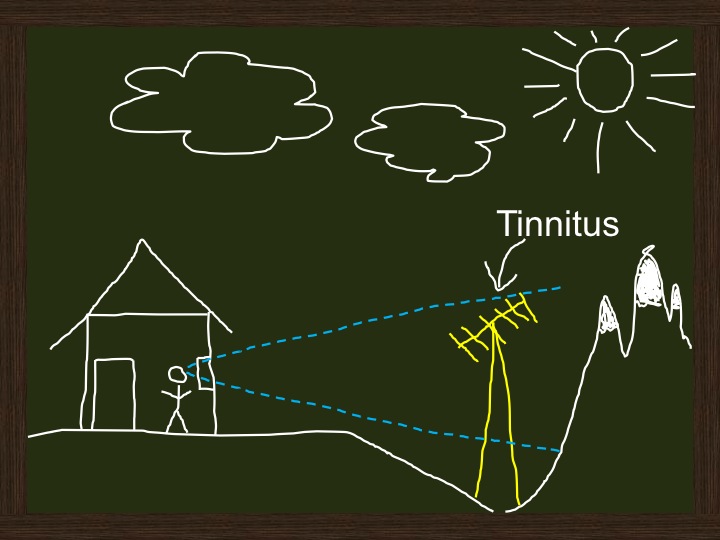
Panel 1. Tinnitus visual analogy from Dr. Gyoergy Varallyay.
In panel 1, you see our subject who loves to go to the mountains. That is his happy place. He buys some land in the mountains and builds his dream home and enjoys his view to the fullest. Then one day he goes outside, and something is obstructing his view. It is an electrical tower. This makes him sad and very anxious. It has affected his happy place; it has affected his life. This electrical tower can be compared to tinnitus itself. When tinnitus has an especially sudden onset or if you're living with it, and it can negatively impact your life.
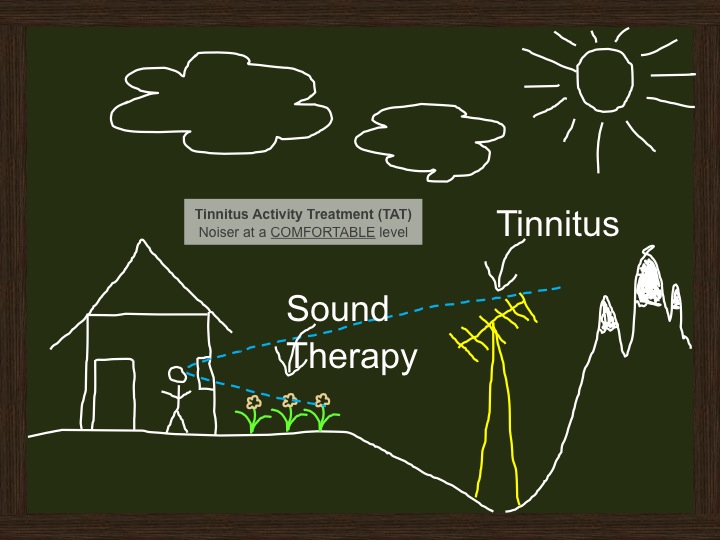
Panel 2. Tinnitus visual analogy from Dr. Gyoergy Varallyay.
He talks to his friend, who suggests, "You know, maybe you still have a beautiful view. Sure, you have that tower to deal with, but what if you plant a little garden? Plant some flowers, take your mind off the tower, brighten up your surroundings, and see how that impacts you." The garden is analogous to sound therapy in general, as you can see in Panel 2. It’s like putting tinnitus on the back burner and trying to provide some relief. TAT strives to offer a comfortable level of noise. TAT can be analogous with the kind of sound therapy where you would keep the noise at a comfortable, low level to allow the patient to habituate to their tinnitus. You are giving them something more pleasing to listen to, and you are not overwhelming them with noise. The noise can be complete masking of the tinnitus, but typically it starts out as a partial masking, and not just one signal is recommended. Lots of different signals can be used with TAT.
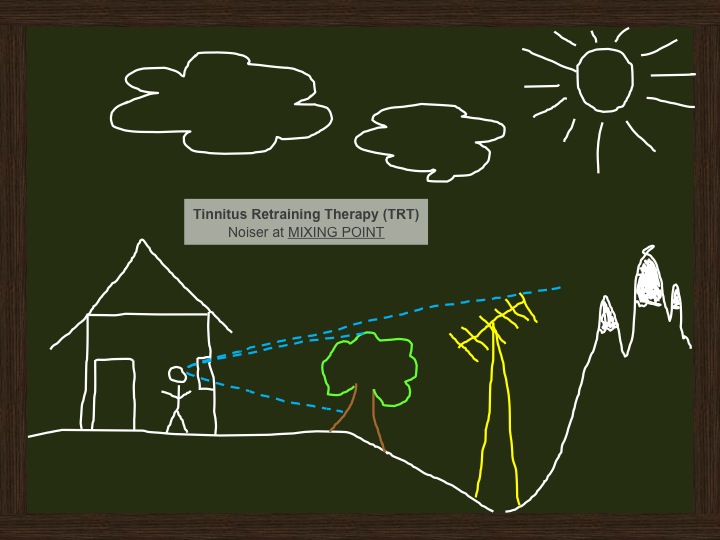
Panel 3. Tinnitus visual analogy from Dr. Gyoergy Varallyay.
What if you want to try something else? His friend says, "Let’s try planting a tree." In Panel 3 you see that he plants a big tree, and tries to take his mind off the tower with a larger obstruction.
The tree could be analogous to Tinnitus Retraining Therapy (TRT), because with TRT, the noise is at a higher level. Daily, you're finding a mixing point, which is still partial masking. It's still below the tinnitus, so you're not completely masking out the tinnitus, but it is at a higher level. Jastreboff's notion about TRT and using the mixing point is that you're not involving more central processing with a noise that is too low, or a signal that is too low. Mixing point is very important if you're doing traditional TRT.
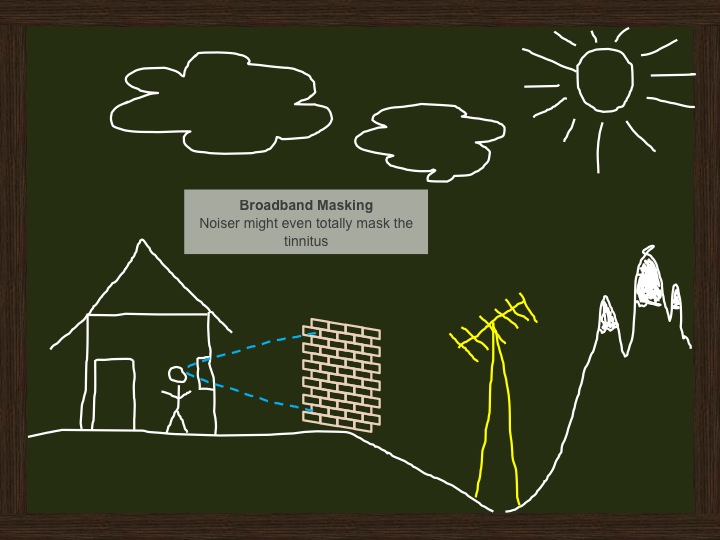
Panel 4. Tinnitus visual analogy from Dr. Gyoergy Varallyay.
Our subject is not quite satisfied with the tree. He talks to his friend. His friend suggests building a brick wall that completely blocks the tower, as you can see in Panel 4. The solid brick wall is analogous to broadband masking. In this case, the wall is completely blocking the tinnitus; but you also might use broadband masking as a partial masking. Broadband is more what we use at Signia; white noise and pink noise. You can have different filtering of broadband masking, but if you use that broadband to mask out the tinnitus completely, then it's called complete masking rather than partial masking.
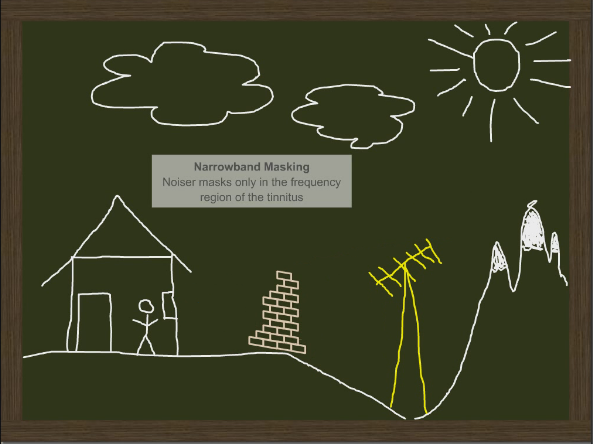
Panel 5. Tinnitus visual analogy from Dr. Gyoergy Varallyay.
What if we peel away some of the bricks and we customize the wall, as in Panel 5? Then we're thinking more about narrowband masking. Noises can be masked only in the frequency region of the tinnitus. Narrowband masking can still be used as partial masking, or you can start to pitch match and find what kind of narrowband masking you want to use. In this case, narrowband masking may be partial in an attempt to match the tinnitus. The use of narrowband masking is being explored for suppression of tinnitus, however, at Signia, we're still using the approach of habituation. Whether you use partial masking with broadband or narrow noise, the main goal for us is still habituation. With habituation approaches, the patient still hears the tinnitus, as the level of the signal is just below the level of the tinnitus.
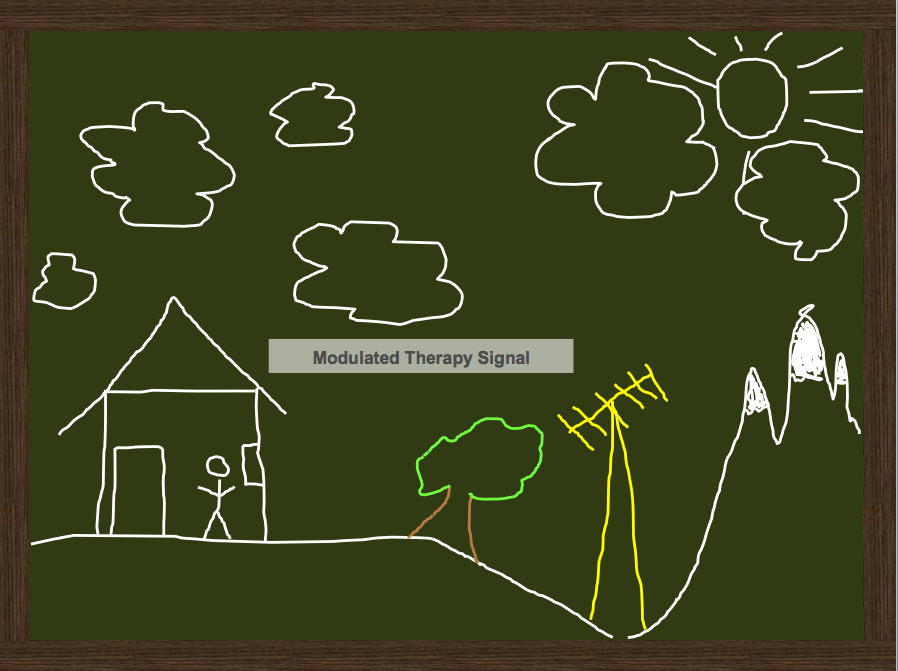
Panel 6. Tinnitus visual analogy from Dr. Gyoergy Varallyay.
In Panel 6, we still have the tree, but imagine there is motion due to the clouds floating by. This is analogous to a modulated sound therapy signal. At Signia, we have four different ocean wave patterns as sound therapy options. With modulated therapy, a partial masking approach or a complete masking approach is used; not a suppression approach. There is currently some research into tinnitus suppression with modulation-based signals but what we're talking about today is habituation.
Progressive Tinnitus Management Flowchart
Progressive Tinnitus Management includes a flowchart for managing the tinnitus patient. It is available here. Tinnitus management begins at Level 1, Triage. From here, you determine what support and services, if any, the patient may require. The next level is an audiologic evaluation (Level 2). If it is determined that the patient needs it, Level 3 is Group Education. The group education approach has worked very well for the VA. It might be something that you can consider in your practice. From here, patients who require an interdisciplinary evaluation, for example if they have an emotional component and a referral to psychology is indicated, move to Level 4. Level 5 is individualized support for those patients who require it.
Level 2 Audiological Evaluation. The following components are involved in Level 2 audiological evaluations:
- Hearing evaluation
- Written questionnaires
- May screen for mental health conditions and notify primary care physician
- Hearing aid fitting as required: -may fit combination instruments, but leave noise generator off-recommended until level 3 counseling (See Appendix J for “Special Considerations”)
- Screening for sound tolerance problem (hyperacusis)
- Patient participation in STEM (Sound Tolerance and Evaluation & Management) protocol
- Reassess need for Level 3 group education after completion and resolve of hyperacusis
Cognitive Habituation Tinnitus Treatment (CHaTT)
As mentioned, CHaTT takes a multifaceted approach to managing tinnitus. It not only involves sound therapy, but it also includes a brain component, instructional counseling and cognitive counseling.
How to Set Up Acoustic Therapy in Siemens Hearing Instruments
With Signia, you do not have to fit a niche or specialized tinnitus product. All primax, binax, micon & Orion hearing instruments can be used as a simple masker for patients who have normal hearing, and in a mixed mode for patients with hearing loss. Within the micon platform, the Aquaris (waterproof device) offers the tinnitus therapy feature. Even Orion, which is part of the Essential product line, has white noise available.
The therapy signal is always software activated so no special ordering is required. You have full flexibility. The therapy signal is accessible in all technology levels, with different amounts of flexibility in shaping the signal for the therapy, similar to the frequency shaping.
Therapy Signal Options
Figure 1 is a screenshot of the Tinnitus Therapy tab in Connexx. I have checked the box to access the tinnitus therapy. I can put this in the universal program or in a separate program. The options for the signal are modulated ocean waves as well as five static signals: white noise, pink noise, speech noise, high tone/high-frequency noise, and Brownian noise (which sounds like a light rain). You can mix the signal with the microphone, and you have full control over the master volume, or you are able to customize it.
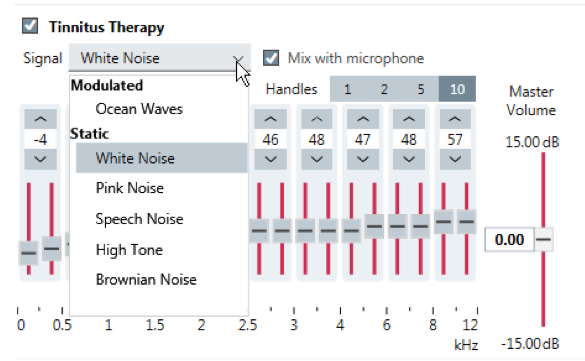
Figure 1. Therapy signal options.
In Figure 2, you see 20 handles in the highest level of technology that you can use to shape the therapy signal individually. You can also use the filtered, canned program, programmed signal filtering. Each signal has a different filtered pattern.
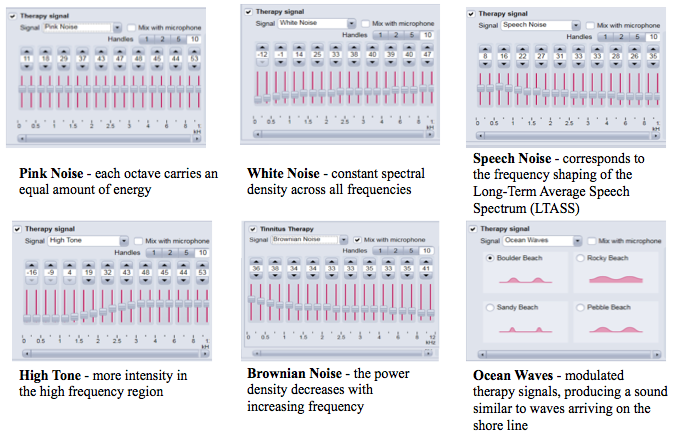
Figure 2. Therapy signal options.
With pink noise, each octave carries an equal amount of energy. White noise is more broadband, with constant spectral density across all frequencies. Speech noise corresponds to the Long-Term Average Speech Spectrum (LTASS) frequency shaping. High tone has more intensity in the high-frequency region. Brownian noise has a power density that decreases as the frequency increases. Brownian noise sounds like a light rain, as if you had the window open on a rainy day, and it is a pleasing sound. Again, you're able to choose any of these therapy signals with whichever protocol you wish to follow.
The ocean waves are modulated therapy signals that produce sounds that are similar to waves arriving at the shoreline. There are four different types, because waves sound different in different parts of the country: boulder beach, rocky beach, sandy beach and pebble beach. They have different timing characteristics. For instance, there may be a gap between the waves, and some of the waves may be stronger. You can use choose to customize these options for your patient.
Once you have determined the type of therapy signal to use, there are two ways to adjust it (Figure 3) – you can use the Master Gain control or the individual slides to customize the frequency response. The easiest way to proceed is to have the patient select whichever signal is most pleasing, and then simply adjust the Master Gain control. Reduce the volume of the signal until they don’t hear it at all, and then slowly raise the signal until it starts to mix with the tinnitus for a partial masking approach. It’s very flexible if you do work with the handles to customize the frequency response of the signal. Once you change the individual handles that you see, then the label changes to "custom" because you've deviated from that filtering.
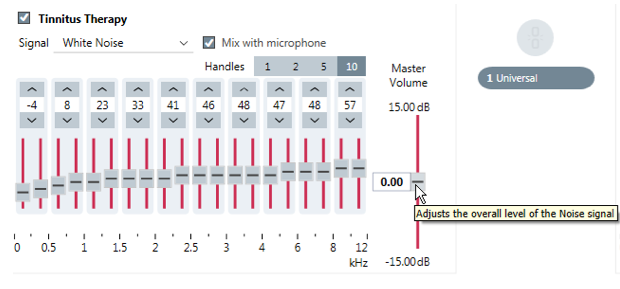
Figure 3. Two ways to adjust the therapy signals.
Activating Tinnitus Therapy
If you're not familiar with our software, we can set up a virtual online training with you. We call it Signia Virtual Assistance, and we can walk you through your first fitting, either before your first patient arrives or while you're doing your first tinnitus fitting of the therapy signal.
To activate tinnitus therapy, under the Fine Tuning option, go to the Tinnitus Therapy Tab. Check the box for Tinnitus Therapy if you want to use it in the Universal program (Figure 4).
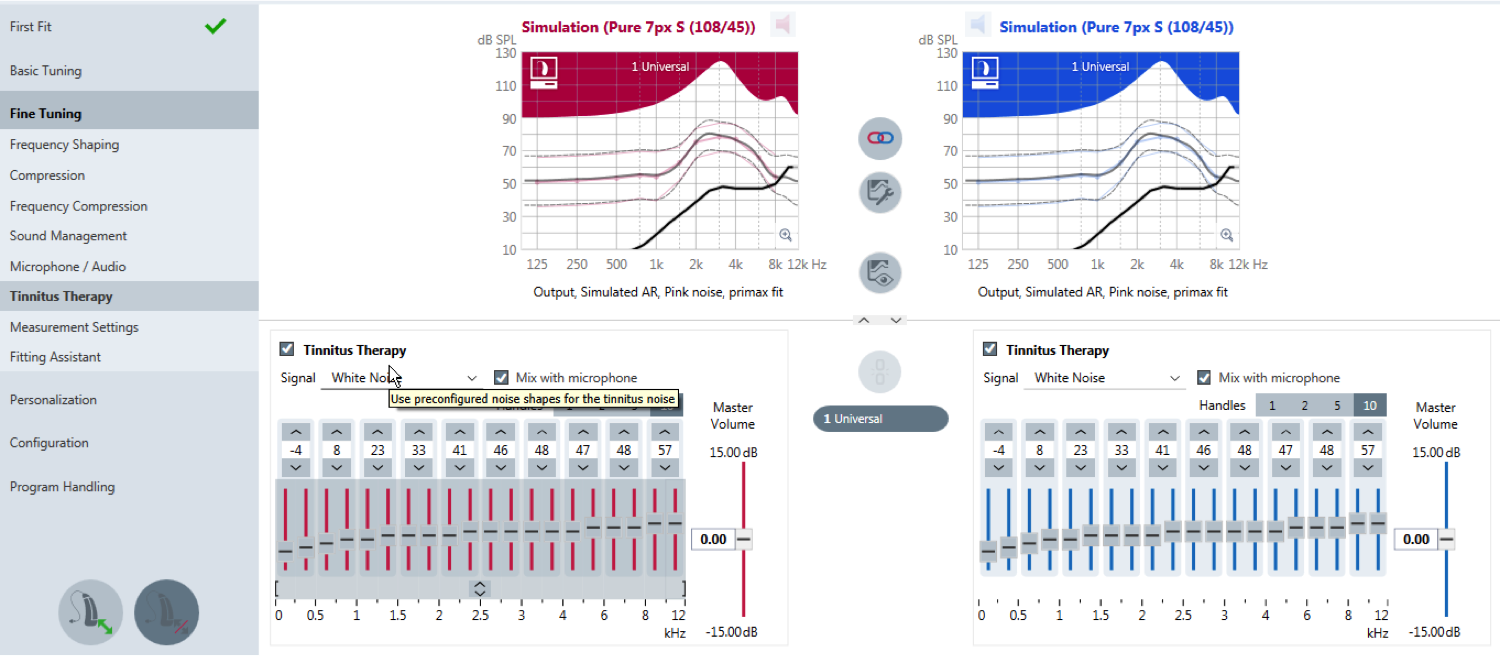
Figure 4. Activating a therapy signal in the universal program.
If you'd like to use a multi-program approach (Figure 5), go to the Fine Tuning section. On the bottom left-hand side of the screen, select Program Handling and simply add a tinnitus program. It's a canned program to get you started. Then, you can decide to have a tinnitus program in addition to the Universal program. With patients who have fluctuating tinnitus or their tinnitus changes based on the environment, you can offer multiple signals. This is also a great option for patients who need to be in control of their therapy signal.
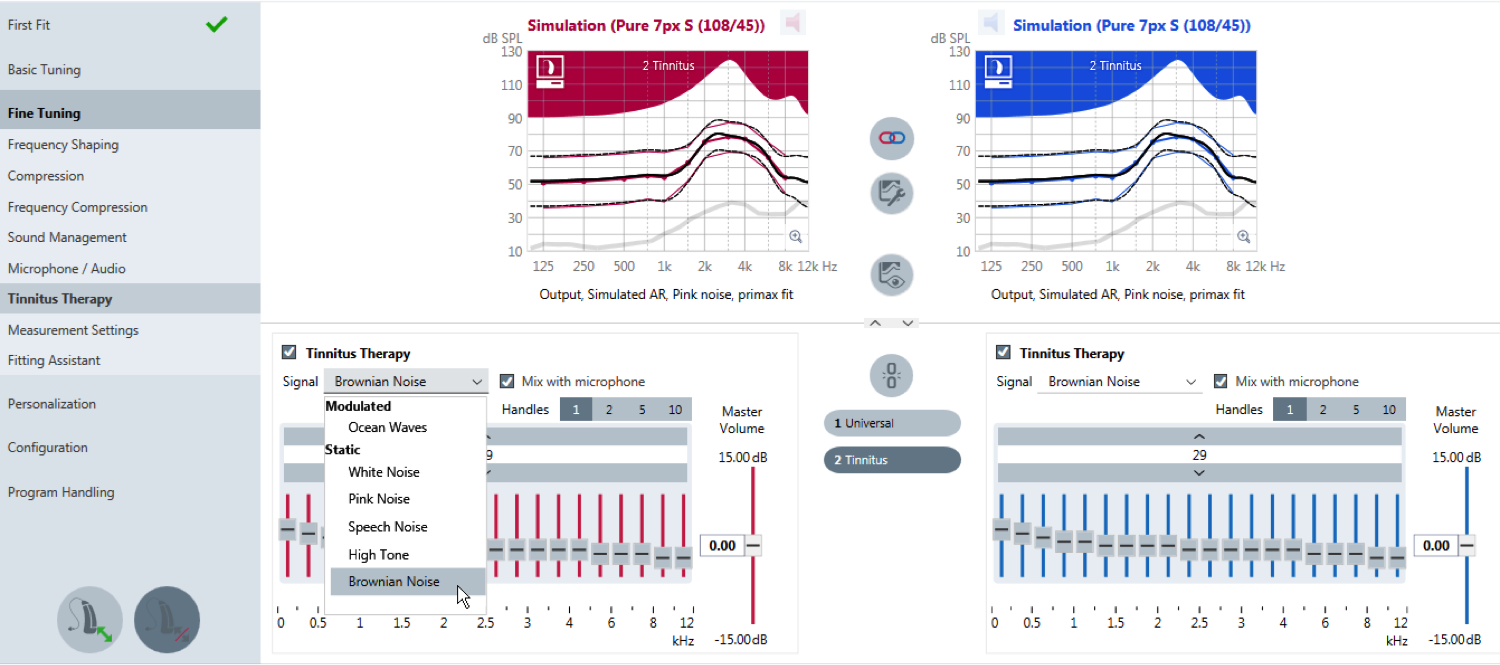
Figure 5. Activation when multiple programs are desired.
With a multi-therapy signal approach with multiple programs, you may want to customize the names of the programs (Figure 6). With the touchControl app downloaded to the patient's phone, they can set the programs to their preference and see the names of the programs that have been customized. For example, I had a patient whose tinnitus changed based on the noise level of the environment (e.g., on an airplane, in the car, in a restaurant). She had a need for multiple programs when she first got started with the therapy signal. If the patient doesn’t have a smart phone, we have a remote and easyPocket for which you are able to also program the custom names.
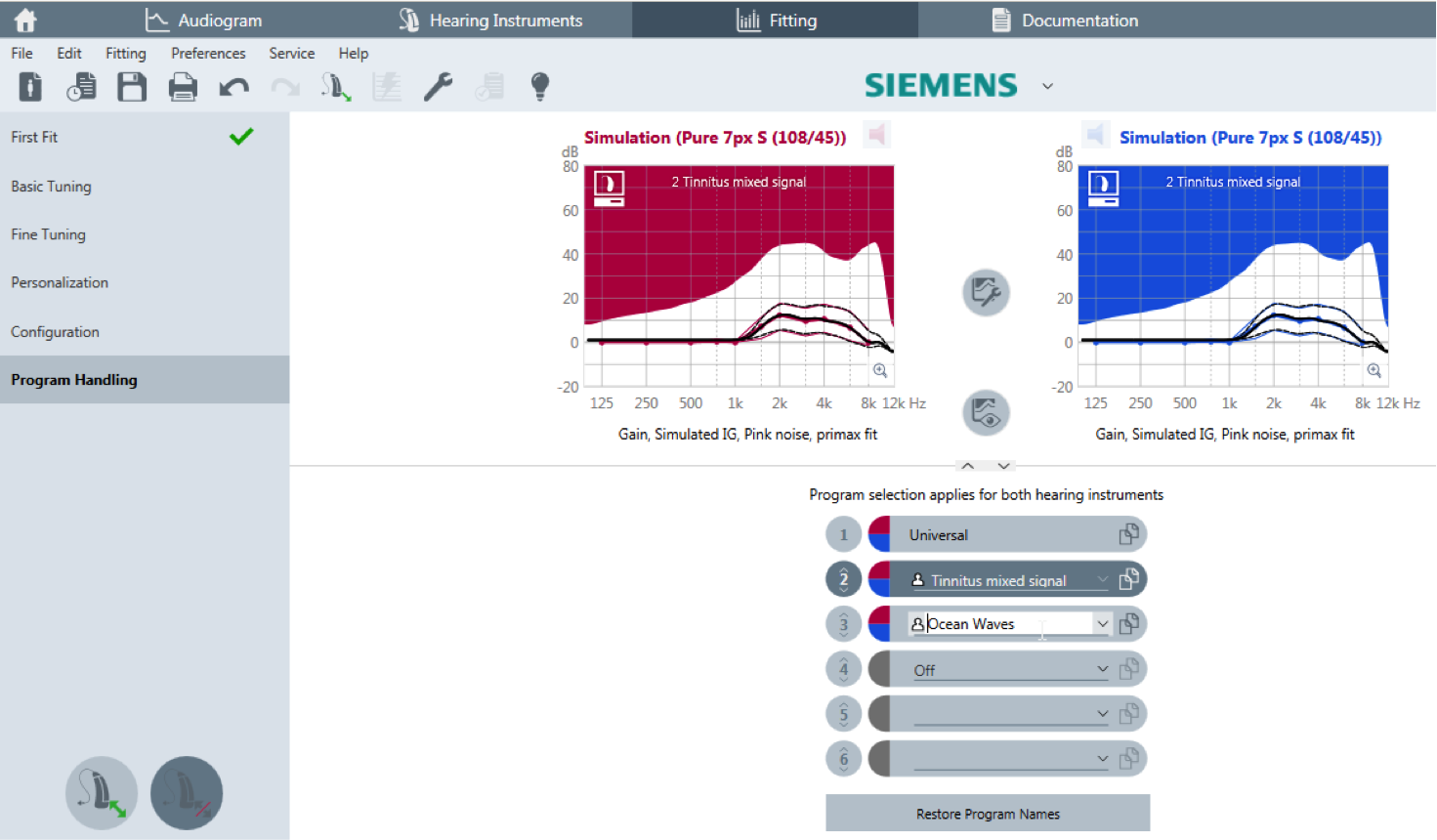
Figure 6. Creating custom program names.
The patient can also use the rocker switch to control volume at ear level (Figure 7). Under the configuration screen of the instrument, you can enable the rocker switch so that it can be used to adjust tinnitus therapy volume. Because we have hearing aids that communicate ear to ear, we're able to set up one volume control to be a tinnitus therapy volume, separate from the gain volume on the opposite ear.
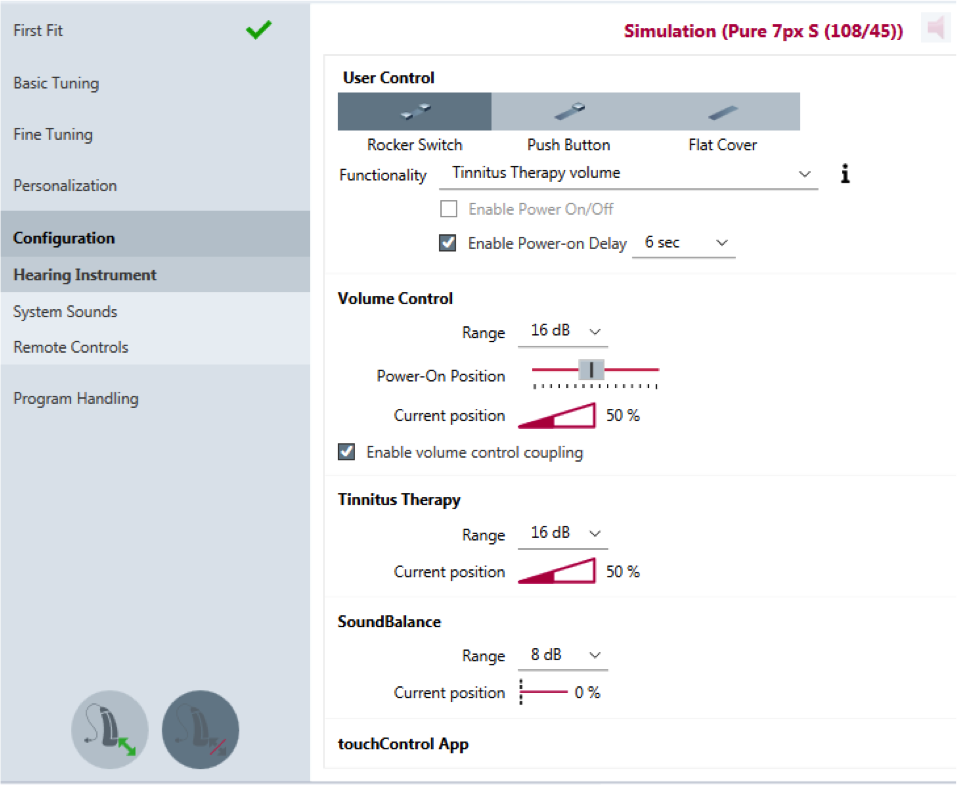
Figure 7. Configuring the rocker switch.
You also have the ability to change the range of the tinnitus therapy signal. The tinnitus therapy range is set at 16 dB, so it can go up 8 dB and down 8 dB, just like the volume control. It is sometimes recommended to increase the range to 24 dB so the patient can tell the difference between when they make a volume control change for their tinnitus therapy signal.
The Remote Control screen will enable you to program the easyPocket remote control. You can configure the side buttons on the remote to control tinnitus therapy volume. Simply connect the easyPocket, and then you can rename the programs and configure the side buttons.
Figure 8 is a screenshot of the touchControl app. It's free, and it is both Android and Apple compatible. You simply download the touchControl app from either store. If you have a tinnitus therapy program in the, you will see the control for the therapy signal in the app.
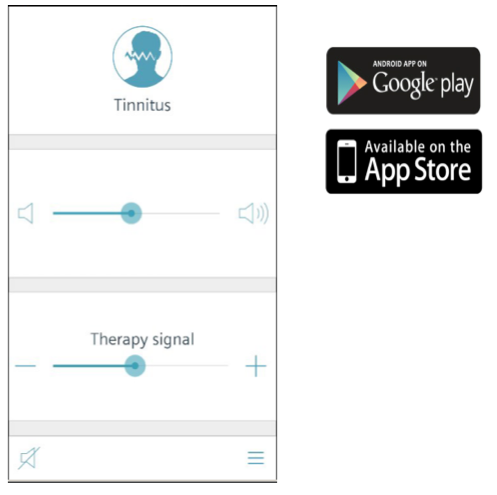
Figure 8. Downloading the easyTek or touchControl apps.
Tinnitus Therapy Alternatives
Before adding a tinnitus therapy signal, you may want to try adjusting the hearing instrument settings. With a hearing aid user who does not have tinnitus, we aim to provide amplification that has very low amounts of circuit noise and that reduces environmental noise. When we are working with a tinnitus sufferer, we need to take a different approach that focuses on sound enrichment. Adjusting the hearing aids to allow more sound to reach the wearer may be more beneficial for the tinnitus sufferer.
Here are some suggestions for programming hearing aid settings that may be helpful for tinnitus sufferers.
Increase environmental noise. Increase the environmental noise in the Universal program. With respect to understanding speech and increasing acceptance of hearing instruments, we aim to reduce noise within hearing instruments. As a result, our hearing aids are very quiet. However, we want tinnitus sufferers to avoid quiet. Within the Basic Tuning section of Connexx, you may increase the gain for soft sounds to try to provide more ambient input as a tinnitus treatment. This is one way to address tinnitus within the Universal program without offering an additional tinnitus signal.
Reduce noise reduction. With regard to Sound Management in Connexx, you may also consider using environmental noise as a natural masker by reducing the level of noise reduction. You may also use a multichannel adjustment to the noise reduction and apply less noise reduction in the lower frequencies where room noise is typically present. You can find these options in Speech and Noise Management within the Sound Management section of Fine Tuning.
Directionality/omnidirectionality. An omnidirectional setting may be beneficial for the tinnitus sufferer as there is no reduction in sound from any direction. You can also choose alternative trigger points for the directional microphone modes as well as varying levels of directionality. In Finetuning, go to Microphone/Audio to adjust directional settings. Next to the word “Directional,” there is a wrench icon; click the icon to change the settings that determine when the instruments go into full directionality mode. The options are "standard", “low” and “high.” In the “high” setting, it will stay in omnidirectional a little bit longer. You can choose a fixed omnidirectional mode when tinnitus is more intense, by adding an additional program.
Sound equalizer adjustments. Sound equalizer adjustments are available in our premium level of hearing instruments. You can increase the gain within the Quiet classification. That's a great way to be able to keep the tinnitus therapy in one automatic Universal program, and give the tinnitus sufferer more sound enrichment when they are in quiet settings.
Additional Products
When a tinnitus sufferer takes their instruments off at night, they might need something to help them sleep, so that tinnitus noise is not a distraction. One option is to use a desktop device for nature sounds or a wave machine. Also, we have our easyTek streamer to play relaxing sounds from a mobile phone or mp3 player. In addition, there are lots of apps out there that play relaxing sounds, or you can stream music into your hearing instruments. Many choices are available when it comes to apps that you can stream using the easyTek directly into the instrument.
We have provided a few app suggestions currently found in the app stores – some are free and some have a charge.
- Bloom: “Zen” sounding tones, but presented in stereo.
- Relax Noise 3: Masks nerving ambient noise and also your tinnitus with white noise. It sounds similar to waterfalls, heavy rainfalls or the sounds of the sea.
- Naturespace: A holographic audio journey.
- Nature Sounds Relax and Sleep: Relaxing sounds of nature.
- Ambiance: A huge catalog of sounds, everything from white, pink, and blue noise to fan noise, animal sounds, and crowd noise.
This information is subject to change. There are probably hundreds more similar apps out there; you can browse them by searching the app stores for "tinnitus," "relax," and "audio”. They can be streamed through the easyTek.
Resources and Support
We're here to help to get you started with your tinnitus therapy program and to support you. We have more tinnitus courses on AudiologyOnline, and an Expert Series of online courses presented by leading experts in the profession. Browse our online course library here. Thank you for attending this course today.
References
Jastreboff, P.J. (1990). Phantom auditory perception (Tinnitus): Mechanisms of generation and perception. Neuroscience Research, 8, 221-254.
Newman, C.W., Jacobson, G.P., & Spitzer, J.B. (1996). Development of the Tinnitus Handicap Inventory. Archives of Otolaryngology-Head and Neck Surgery, 122, 143–148.
Seidman, M.D., & Jacobson, G.P. (1996) Update on tinnitus. Otolaryngol Clin North Am, 29(3), 455-65.
Shi, Y., Robb, M.J., & Michaelides, E.M. (2014). Medical management of tinnitus: Role of the physician. J Am Acad Audiol, 25(1), 23-8. doi: 10.3766/jaaa.25.1.3.
Surr, R.K., Kolb, J.A., Cord, M.T., & Garrus, N.P. (1999). Tinnitus Handicap Inventory (THI) as a hearing aid outcome measure. J Am Acad Audiol 10, 489-495.
Tunkel, D.E., Bauer, C.A, Sun, G.H., Rosenfeld, R.M., Chandrasekhar, S.S., Cunningham, E.R.,...Whamond, E.J. (2014). Clinical practice guideline: Tinnitus. Otolaryngology-Head and Neck Surgery, 151(2S), S1-S40.
Tyler, R.S., Gogel, S.A., & Gehringer, A.K. (2007). Tinnitus activities treatment. Prog Brain Res, 166, 425-34.
Tyler, R., Ji, H., Perreau, A., Witt, S., Noble, W., & Coelho, C. (2014). Development and validation of the tinnitus primary function questionnaire. Am J Audiol, 23(3), 260-72. doi: 10.1044/2014_AJA-13-0014.
Wilson, P. H., Henry, J., Bowen, M., & Haralambous, G. (1991). Tinnitus reaction questionnaire: psychometric properties of a measure of distress associated with tinnitus. Journal of Speech and Hearing Research, 34(1), 197-201.
Further references and resources can be found in the course handout.
Citation
Powers, L., & Gehlen, J. (2016, November). Helping your patients with tinnitus: Signia tinnitus therapy feature. AudiologyOnline, Article 18530. Retrieved from https://www.audiologyonline.com.