This text course is an edited transcript of a live webinar, presented as part of Signia/Siemens expert series on AudiologyOnline. Download supplemental course materials.
Learning Objectives
The learning objectives for this course are to describe how pre-fitting testing can assist in the overall fitting process, describe the relationship between proprietary fitting and NAL-NL2 fittings, and describe the impact of acclimatization on the hearing aid fitting
Approximately 200 articles a year are published just on hearing aids. Most busy clinicians do not have time to read, or even skim, all of these. I personally try to take a glance at most of the abstracts at one time or another, but many are in journals that are a bit obscure. In many of these articles, there can be some important clinical points, but it may not be obvious from reading the title of the article or even the abstract as to what might be important to the clinician. Today, therefore, I have selected some key articles from the past year or two that I think have something that you might enjoy hearing about, and hopefully there will be things that you can consider applying to your clinical practice.
Acknowledgement
For the past 12 years, Catherine Palmer, Bob Turner and I have been doing a review of the hearing aid literature at the American Academy of Audiology (AAA) meeting. A couple of the topics that I am talking about today were lifted from the most recent session. Thank you to Catherine and Bob for allowing me to borrow their information. I also should mention that Catherine Palmer’s Lab at the University of Pittsburgh is very good at tracking down all of these articles which come from over 20 different journals.
I divided the articles into four general areas that we think about when we are fitting hearing aids: pre-fitting testing and considerations, selection of technology, verification of the fitting, and post-fitting follow-up, outcome measures and counseling.
Pre-Fitting Testing
Acceptable Noise Level
The first thing I would like to talk about is the Acceptable Noise Level (ANL) test that was developed at the University of Tennessee, based on the research of Anna Nabelek dating back to 1991. For those of you who are not familiar with this test, here is a quick review of how it works:
The test usually is conducted bilaterally in the sound field, not under earphones.
You first determine the patient’s most comfortable listening level (MCL) for continuous discourse. The standard material is a travelogue about Arizona. It’s a loudness task, not a speech recognition task, so the actual speech material doesn’t matter too much.
Next, you play the continuous discourse at the patient’s MCL, and then adjust the background noise, which is a multi-talker babble (although other background noises have been used in some research). You use a bracketing approach, making the background noise louder and softer, until you get to the point that the patient says it is at the level “that they can just put up with.” There are standard instructions for this which need to be used (see Patrick Plyler’s recent 20Q articles on this topic).
You then subtract the noise level from the patient’s MCL; the noise level will always be below the MCL because the instructions state that the patient has to follow the story while he or she are selecting the noise level. If the noise level was higher than the speech level, then they would not be able to follow the story.
After this simple math, you will have a single positive number, which is called the ANL. In essence, this is simply is the signal-to-noise ratio (SNR) that is acceptable for a given patient.
What we have found through many studies is that the average ANL is around 8 dB, and this tends to be the same for people with normal hearing and hearing impairment. In other words, when you have a hearing loss, your ANL does not change.
What to do with the ANL score?
How would you use these scores? Keep in mind that small numbers are good. It means your patient is not bothered much by background noise. If your patient has an ANL score of 7 dB or less, you would think they would have a good prognosis for regular use and acceptance, and they probably do not need as much post-fitting care as the average patient.
If the score falls in the average range, which we consider to be about 8 to 12 dB, you would treat this as any traditional patient with the typical amount of counseling, as they would be considered an average candidate for success with amplification.
Where this test is the most important is when the person has an unusually large ANL. This is usually considered to be 13 dB or more. These people are considered at risk for reduced hearing aid use. A score like this should be a red flag that you need to spend some extra time with them because there is a good chance they are not going to accept amplification.
The point of reviewing all this is that in 2014, Olsen and Brännström (2014) from Scandinavia did a review of the literature regarding ANL studies. What they found, was that in just the last ten years, there were an astounding 45 peer-reviewed ANL papers. Obviously, quite a popular test to research, as there probably are another 10 or so articles on the topic that were not in peer-reviewed journals! Based on this extensive review, these authors concluded that there is a predictive value for using the ANL; that is, the scores do help predict success with hearing aids. I personally suspect that one reason why all the research does not seem to agree, is that the definition of hearing aid success varies (e.g., Use? Benefit? Satisfaction?).
If you want to try out the ANL, AudiologyOnline published an article by Patrick Plyler from the University of Tennessee. He has done probably more research on the ANL than anyone else. This article and it will give you a good start if you want to start doing the ANL clinically.
Clinical Tip
The ANL can be helpful in predicting when patients may need additional counseling and follow-up. These would be the people with large ANL scores (e.g., larger than 12 dB or so). The ANL does not correlate with other commonly used speech in noise tests such as the QuickSIN or the HINT. This is good, as you are collecting information that you would not have from any other routine test.
Selection of Technology
One of the popular features in hearing aids today is binaural streaming, where the hearing aids can talk to each other with more meaningful commands than changing programs or the volume—today, they are actually saying words and sentences to each other! Many hearing aids, both BTEs and custom products with two microphones now have the ability for full audio data transfer between the two ears. What the patient will hear in each ear is the input that has been processed from four different microphones. We are then able to use more sophisticated algorithms than when we only had the information from two microphones.
Narrow Focus Directionality
One of the algorithms is called bilateral beamforming. With signals from the two sides, you can have a narrow focus for directivity. Traditional directionality has a wider angle around the front of the listener. Narrow directionality allows you to focus on the talker as long as you are looking at that talker. Not surprisingly, this is something that is ripe for research.
One of the articles published last year was on this topic, out of Vanderbilt, by Picou, Aspell and Ricketts (2014). They looked at three different directional settings. The first setting was omnidirectional, although I need to point out that most BTE hearing aids today do not have true omnidirectional; they have what usually is called something like “pinna compensation,” which is simply a mild form of directional processing. The authors therefore labeled this setting appropriately as “mild directional”, although you may think of it as omnidirectional, as that is what it probably is called in the fitting software. The second setting they studied was standard adaptive directional. That is the processing that we have been seeing in hearing aids for the past 10 years or so. This means that the polar patterns are adaptive, but it is using the standard two-mic directional algorithm with no bilateral beamforming. The last condition was bilateral beamforming, to which they refer as strong directional.
They used Robyn Cox’s Connected Sentence Test (CST), which has background noise, and evaluated two different SNRs, at two levels of room reverberation, labeled “easy” and “hard”. They also looked at gross localization, which they assessed with and without visual cues. They did this, as one might question if this narrow beamforming could interfere with localization. Another component of the study design was a measure of listening effort, which was assessed by using a dual task paradigm. Finally, they looked at subjective preference in the real world for the different directional settings.
The researchers wanted to see if there were any negative consequences of beamforming. They found some impairment in localization when the beamforming was 60 degrees on either the left or right side, but that slight disadvantage disappeared when visual cues were available. They reported that the beamformer had no positive or negative consequences on listening effort or the subjective preferences in the real world.
The primary question of course, was whether the beamforming resulted in improved speech recognition in background noise. For low reverberation in easy and hard conditions, we saw that performance improved with increasing strength of directionality. This is a trend that we would expect, although these differences were not significant. In moderate reverberation, however, some of the findings were significant in terms of the amount of speech perception increase between directional settings; that is, beamforming showed a significant improvement over adaptive directional. The findings tend to indicate that beamforming indeed does improve speech recognition in background noise, and there does not seem to be any significant negative effects for this processing.
More on Bilateral Beamforming
Another study that looked at a similar type of binaural or bilateral beamforming was published by Froehlich, Freels and Powers (2015) on AudiologyOnline. Because they wanted to make a marketing claim for this processing, this required doing testing at two different sites. They used the HINT speech material, and also the Olsa test. The Olsa is similar to the HINT, but in German, as one of the testing sites was in Germany. The hearing-impaired participants were tested with omnidirectional (mild directional), and then again with the beamforming algorithm. In this study, the researchers did not compare the beamforming to standard adaptive directional, only to the omnidirectional (with pinna compensation).
They compared the aided performance to age-matched normal-hearing individuals. For the test condition, the person listened to the HINT sentences from zero degrees azimuth and noise from seven other loudspeakers, located at 45 degree azimuth increments around the participants. The “noise” was different sentences of the same speech material as the target sentences. In other words, when one HINT sentence was being presented from zero degrees azimuth, seven other HINT sentences, were presented simultaneously at the other speakers around the patient; obviously a listening condition with considerable “informational masking.”
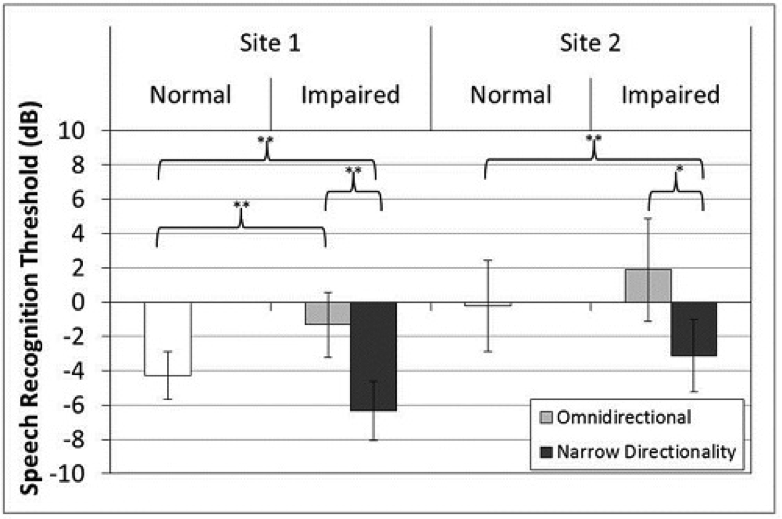
Figure 1. Mean speech recognition thresholds (dB) for the two performance sites. White bars indicate performance for listeners with normal hearing. Grey bars indicate performance for listeners with hearing loss for the omnidirectional setting (light grey) and the Narrow Directionality setting (dark grey). Error bars represent ±1 standard deviation from the mean. * indicates a significant difference of p < 0.01; ** indicates a significant difference of p < 0.001 (From Froehlich et al, 2015).
Let’s take a look at Figure 1, which summarizes the findings of this study. Remember that for the HINT, lower scores are better (i.e., a more adverse SNR for the 50% correct point). For the hearing-impaired listeners, at both sites, there was about a 5 dB improvement for omnidirectional compared to the narrow focus beamforming. There also was about a 2 dB improvement when compared to the normal-hearing group. The absolute SNR findings for Site 2 were different than Site 1 because it was a different speech test and of course a different group of subjects, but note that the relative differences for a given site were essentially the same; the benefit over mild directional was 5 dB, and the benefit over normal hearing was about 2 dB.
You might ask, and people have: How can hearing-impaired people have better speech recognition than people with normal hearing? In general I think the primary reason was information masking. The normal-hearing people seemed to be more easily confused by the background talkers—they had a tendency to pay attention to the non-target speech, particularly the sentences that were originating from 45 degrees azimuth on either side of the target. Because of the narrow beamforming, and the boost in gain for the 0 degree target (part of the beamforming algorithm), it was easier for the hearing-impaired listeners to ignore this completion.
Another relationship the authors examined was the omnidirectional performance compared to the Narrow Directionality benefit. That is, did individuals who did poorer or better in the omnidirectional mode obtain more or less benefit when using the beamforming algorithm? They conducted a partial correlation analysis between performance in the omnidirectional setting and benefit from the Narrow Directionality setting (calculated as SRT in the omnidirectional setting minus SRT in the Narrow Directionality setting; positive scores indicate more benefit). This analysis was conducted by controlling for age and pure tone average (1000, 2000, and 4000 Hz). Results from both sites, as illustrated in Figure 2, indicated a significant correlation between the speech recognition threshold in noise in the omnidirectional mode and benefit from the Narrow Directionality setting.
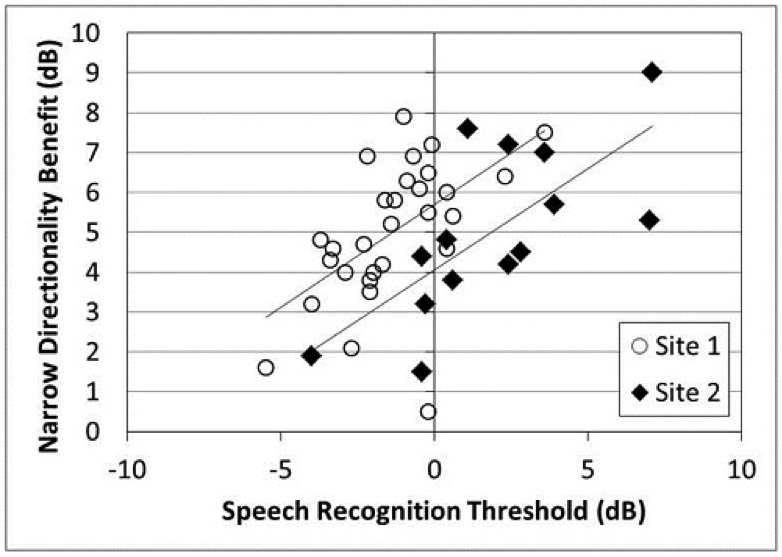
Figure 2. Relationship between speech recognition threshold in the omnidirectional setting (dB) and benefit from the Narrow Directionality setting (benefit=SRT in omnidirectional minus SRT in Narrow Directionality). Open circles indicate data from Site 1 (p<0.01) and filled diamonds represent data from Site 2 (p<0.01). (From Froehlich et al., 2015).
The authors suggest that these significant performance/benefit results indicate that listeners who tend to have the most difficulty understanding speech in background noise will derive the most benefit from the Narrow Directionality processing (see regression lines in Figure 2).
Clinical Tips. Bilateral beamforming provides better speech recognition than traditional directional for at least some listening situations. The latter study showed that some conditions may allow the hearing-impaired to perform equal to or better than their normal-hearing peers. There does not seem to be any major negative consequences of using this algorithm. Obviously, this is not an algorithm that you would use at all times. This algorithm would only be applied when you knew you were going to be listening in background noise, and facing the primary communication partner (or able to turn your head toward multiple communication partners). With some instruments, this algorithm is activated automatically, and/or can be controlled with the users smart phone.
Trainable Hearing Aids
The final technology I would like to briefly talk about is trainable hearing aids. Ben Hornsby and I recently conducted a study (2014) with this technology. By “trainable” I am referring to the type where the patient has VC, or a remote (or cell phone app) and makes their hearing aids louder or softer in different environments over a period of time so that the hearing aid can learn the listener’s preferences. We chose experienced listeners, people who had used hearing aids for at least three years, and gave them trainable hearing aids programmed to the NAL prescription. Our primary research question was to see if the listeners would want to train back to what they had been using prior to the study.
We first assessed the real ear output that they had been using for soft, average and loud speech inputs. We found that when we then programmed them to the NAL, we were giving them about 10 dB more gain for soft sounds than they had previously been using and about 5 dB more gain for average sounds. In other words, they had been underfit, if we consider the NAL prescription the general guideline.
After the hearing aids were re-programmed, they trained their instruments for several weeks. This was “compression training”, meaning that if for example, they trained soft inputs either up or down, this would have little impact on average inputs and essentially no impact at all on loud inputs. The hearing aids were set so that deviations of trained gain of +/- 16 dB were possible.
We compared average high-frequency and low-frequency output using speechmapping for the NAL prescriptive targets, their previous preferred outputs with their personal hearing aids, the initial match to NAL targets, and the final trained gain. High frequency was classified as 2000, 3000 and 4000 Hz. The findings of the study are shown in Figure 3.
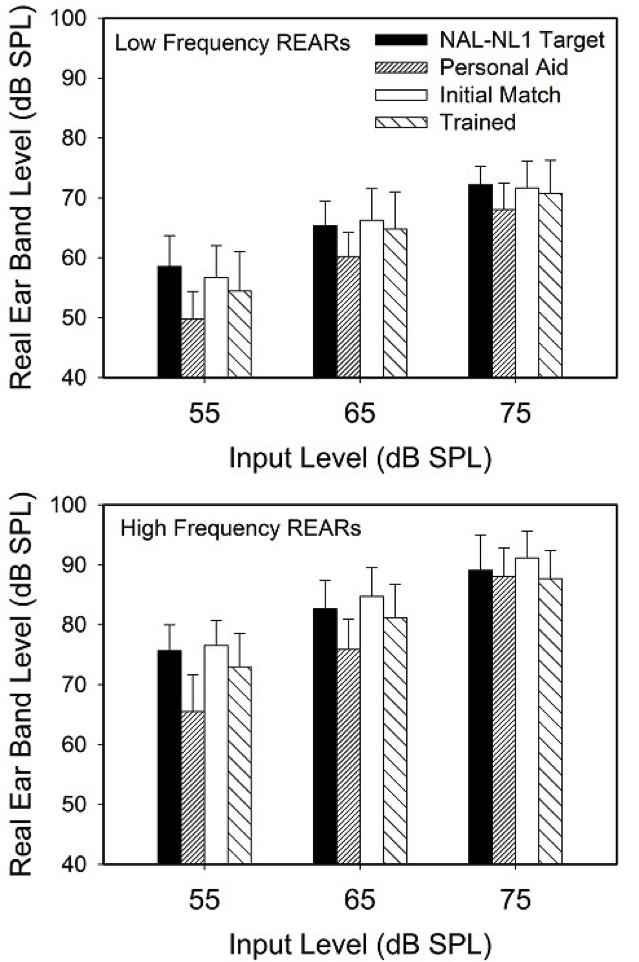
Figure 3. Mean real ear aided response (REAR; earcanal SPL) shown for the averaged low-band and high-band frequencies for the real- speech inputs for three levels. Data shown for four conditions: NAL-NL1 target, NAL-NL1 best match to target, trained gain, and average gain for the patient’s personal hearing aids (From Mueller & Hornsby, 2014).
Observe that all measures were fairly similar for the 75 dB SPL input. That is, the participants had been using gain similar to the NAL prescription, and their trained gain was similar to the NAL prescriptioin. For the 65 dB SPL input, however, we now see that they had been using gain around 5 dB below the NAL, but their trained gain was very similar to the NAL. Perhaps the most interesting finding was that for the 55 dB SPL input for the high frequencies (see lower panel in Figure 3). The personal aids were about 10 dB below NAL targets, but notice that the levels they trained to was very close to NAL targets. They did not train back to the output that they had been using for several years. For the soft speech inputs of 55 dB SPL, their output on average had been around 65 dB SPL, and now after training, it was around 75 dB SPL. Could this extra 10 dB of audibility make a difference? In many listening conditions, absolutely.
Clinical Tip. It may not be wise to assume that the gain and output that a patient is using is what actually is best for them, or even what they prefer. I remember the day when people would come in to obtain new hearing aids and someone would try to program them like their old hearing aids. Why should the output of the new ones be like the old ones? This research proves the point that they probably should not be, unless the old ones had been programmed appropriately. These findings also suggest that on average the NL1 is a reasonable starting point. We of course primarily use the NL2 today, but as would be expected (see the work of Keidser et al, 2013), trainable research using this fitting algorithm also has shown validation for the gain prescribed.
Verification of the Fitting
When sitting down to fit a patient with hearing aids, you basically have three different options for the gain and output right. First, you could pick a prescriptive fitting method like the NAL or the DSL, and then verify that the desired output was present in the earcanal using probe-mic measures. We’ll give this approach a Gold Star, as that is what is recommended by Best Practice documents. Two other options are to click the manufacturer’s NAL-NL2 button (but not verify or alter using probe-mic), or you could click the manufacturer’s default proprietary algorithm button in the software—there are no validated real-ear targets for this approach, so it would impossible to verify. Let’s look at what happens when you stray away from the Best Practice approach.
Manufacturer Proprietary Fitting
A study on this was recently published in Hearing Review (Saunders, Stoody, Weber, & Mueller, 2015) and the data also were reviewed by Mueller (2015). The results from this research should be very close to what you would see with the hearing aids that you are fitting today, as the data was collected using hearing aids and software current the summer of 2015.
Testing was conducted with the premier hearing aids from the five leading manufacturers. In the first part of the study, the manufacturers’ proprietary fitting was selected for a typical downward-sloping hearing loss that most audiologists would consider “easy to fit” (e.g., gradually sloping from 30 dB in the lows to 70 dB in the highs). All the fitting characteristics were matched for the software and the probe mic equipment. Probe-mic measures were conducted using the Verifit speechmap program for 16 ears (eight male and eight female). The results are shown in Figure 4.
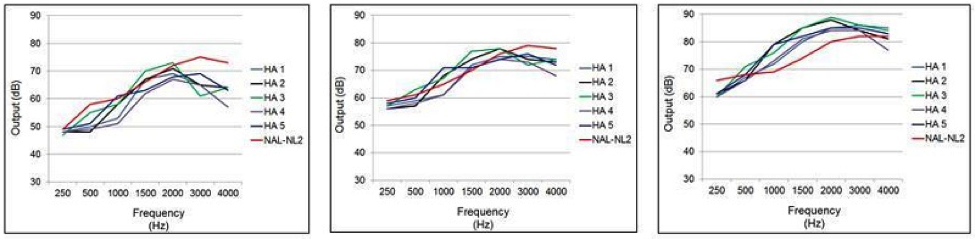
Figure 4. Mean earcanal SPL output for the proprietary fitting (experienced user, bilateral fitting) of five leading manufacturers for a mild-to-moderate downward sloping hearing loss. Data shown left to right for inputs of 55, 65, and 75 dB SPL. The NAL-NL2 targets are displayed as reference. (From Mueller, 2015).
When we look at the manufacturer’s fittings compared to a NAL-NL2 fitting (red line in each Figure), as shown, the results vary dramatically. A significant roll-off in the highs can be observed for all, and through the mid frequencies, there is about a 10 dB difference among hearing aids for the 55 dB SPL input.
For the 65 dB SPL input, there is a similar pattern, where you tend to have a peak in the mid frequencies and a roll-off in the highs. Interestingly, for the 75 dB SPL input, all the proprietary fittings now have output well above the NAL-NL2. If we compare the output for the 55 dB input to the 75 dB input (a 20 dB difference), we see that most of these proprietary fittings are nearly linear, as there also is about a 20 dB difference in output. By comparison, the NAL-NL2 output targets differ by about 8-10 dB for the 20 dB range.
We compared the SIIs for these different fittings, as this is a fairly good predictor of intelligibility. These results are shown in Figure 5.
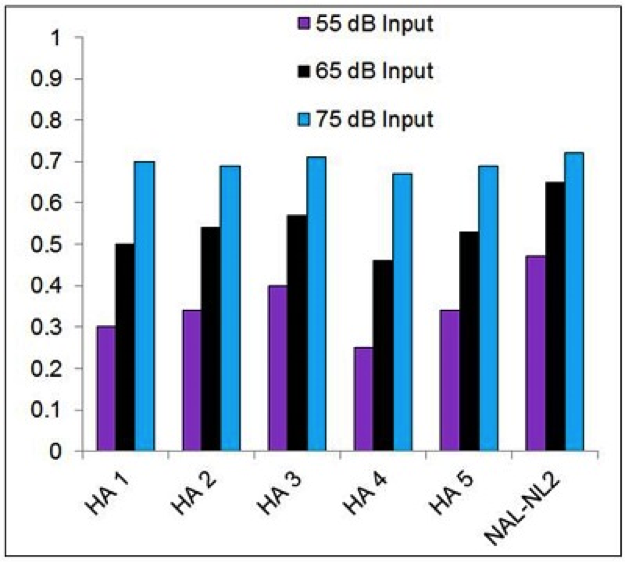
Figure 5. Mean SII values (as calculated by Audioscan Verifit) for the proprietary fitting (experienced user, bilateral fitting) of five leading manufacturers for a mild-to-moderate downward sloping hearing loss. Data shown are for inputs of 55, 65, and 75 dB SPL. The SIIs for a precise fitting to NAL-NL2 targets are shown as a reference. (From Mueller, 2015).
Using the NAL-NL2 as a reference, look across the violet bars to see the SII differences in the fittings for soft inputs; notice that all fall at least ~.10 below the NAL, with the bar for Hearing Aid 4 coming in at only 0.27. If we look at average inputs, which are the black bars, we see a similar pattern. The SIIs for high inputs are all very similar, and about the same as for the NAL, but I do want to point out that these SII predictions for loud inputs might be different for real- world use. Let’s take Hearing Aid 3 as an example. If we go back to Figure 4, we see that this hearing aid has an output about 10 dB higher than what the NAL recommends would be what the average listener would want from a loudness standpoint. If you assume that the NAL researchers, after 40 years know what they are talking about (and I do), what will likely happen is that the user, if given access to a volume control, will turn the gain down because of this peak in the mid-frequencies, which will then make audibility in the highs rather poor, and the SII is going to drop significantly for loud inputs.
All in all, it’s difficult to understand why the “manufacturer’s default” fitting approach is popular with so many audiologists.
Selecting a Prescriptive Method Without Verification
So now that we know that the default fitting approach doesn’t work, we’ll consider another alternative method to probe-mic verification: this is where you select a prescriptive method in the fitting software, but do not verify that this prescription is present in the real ear. Two articles indicate that this approach also might be risky:
- Aazh and Moore (2007) reported that only 36% of these kinds of fittings were within +/- 10 dB of the NAL prescription.
- Aazh, Moore and Prasher did a similar study in 2012 and found that only 29% were within +/-10 dB of NAL targets. This latter study was only conducted using one manufacturer, and things maybe have changed have changed a bit since 2012, however . . .
Let’s go back to the second part of the same study that we have already discussed, where Sanders et al. (2015) selected the NAL-NL2 from the manufacturer’s fitting software for the five premier hearing aids. All the other experimental parameters were as we discussed before.
The results of this testing is shown in Figure 6.
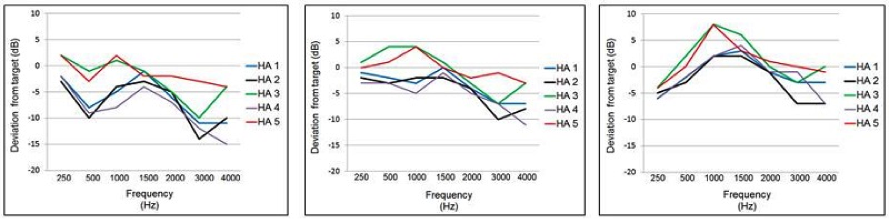
Figure 6. Mean deviation (dB) from NAL-NL2 real-ear prescriptive targets for the manufacturer’s NAL-NL2 fitting (experienced user, bilateral fitting). The zero line represents a precise NAL-NL2 fitting. Data shown for the five leading manufacturers for a mild-to-moderate downward sloping hearing loss. Data displayed left-to-right for inputs of 55, 65, and 75 dB SPL. (Adapted from Sanders et al., 2015)
For these data, the findings are displayed as deviation from target, with the zero line being a perfect real-ear fit to the NAL-NL2. As shown, except for HA-5, the output varies considerably from NAL-NL2 targets. The pattern of deviation from NAL-NL2 seems to be fairly consistent among manufacturers:
- Reduced gain for soft inputs
- Roll-off of high frequencies above 2000 Hz
- Boost in gain for mid-frequencies, to the extent that output exceeds NAL-NL2 targets for the 75 dB inputs
- A more linear fitting than prescribed by NAL-NL2
Interestingly, while the real-ear findings of 4 of the 5 manufacturers’ NAL-NL2 algorithms differ significantly from the desired NAL-NL2 targets, they are quite similar to the respective manufacturer’s proprietary fittings, and they tend to fit NAL-NL1 a little better than NAL-NL2.
As shown in Figure The large mismatch to target in the highs was a pretty common finding for all subjects, except when HA-5 was fitted. As reported by Sanders et al. (2015), individual data for the 80 fittings (16 ears x 5 products) at the 55 dB SPL input revealed that, in 59 of the 80 cases (74%), the measured output varied from the NAL-NL2 target by 10 dB or more for at least one frequency (250-4000 Hz). If HA-5 (the product that resulted in a reasonably close fitting to NAL-NL2) is removed from the calculations, of the remaining 64 fittings, 86% varied by 10 dB or more from the desired NAL-NL2 fitting targets. For these later 64 fittings, compliance with the NAL-NL2 was somewhat better for the 65 dB SPL input, but there still were 35 (55%) of the fittings where the ear-canal SPL deviated by 10 dB or more from the desired output. This was nearly always in the high frequencies.
Cinical Tip. If you believe that fitting to a prescriptive target is a good thing (which is what is recommended in Best Practice documents), it is very risky to use either the manufacturers’ algorithms or the manufacturers’ version of the NAL without real-ear verification. There is no “Plan B.”
Hearing Aid Verification and Satisfaction
We just talked about the importance of verification, but the skeptic might simply say: “Is there any proof that verification actually matters?” The MarkeTrak VIII survey data (Kochkin et al., 2010) looked at overall satisfaction by way of the fitting practices as reported by the patients - not the people doing the fitting. Then the group examined the data to determine if fitting practices influenced satisfaction. That is a reasonable question. The following is a list of many of the fitting factors Kochkin looked at in his research. The top ones are the most common; the bottom ones deal more with rehabilitative audiology:
- Hearing tested in sound booth
- Loudness discomfort measurement
- Real-ear measurement used for verification
- Measurement of objective benefit (e.g., pre-post measurement of speech understanding)
- Measurement of subjective benefit
- Patient satisfaction measurement
- Auditory retraining software therapy
- Enrolled in aural rehabilitation group
- Received self-help book/literature/video
- Referred to self-help group (e.g., HLAA)
At the end of the day, does hard work pay off? If you follow best practices, do you really have more satisfied patients? The research results agreed with all the documents of best practice—in a very systematic manner, satisfaction increased from below 2.0 to 6.0 simply by following Best Practices. I believe a reasonable protocol would be to do loudness testing, QuickSIN (or other speech-in-noise measure), probe-mic verification, some structured subjective judgements for speech, and an outcome measure such as the COSI, IOI-HA, etc.
Another related article has to do with mail order hearing aids (Kochkin, 2014). Kochkin compared mail order hearing aids to his MarkeTrak VIII data of people who had been fitted using different types of practices—what we just talked about above. A group of 2,332 people who ordered a hearing aid through the mail were compared to 1,721 people who had been fitted by an audiologist or a hearing instrument dispenser in the past few years. He looked at 14 different items related to quality of life. Interestingly, the quality-of-life changes improve as you go through the different steps of verification—more is significantly better. The satisfaction factor for direct mail hearing aids is around Kochkin’s Level 5 of verification—better than hearing aids fitted by audiologists who do little verification.
Clinical Tip. If fitting practices are poor, outcomes will be no better than obtained with direct-mail hearing aids. There is one caveat to this. Value is related to price, and value can impact satisfaction. Perhaps because these people got their hearing aids for less money, that made them happier, and maybe they answered the question a little differently. These were not specific satisfaction questions, but there could have been some carry-over.
Customer Loyalty
Another related study involves patient loyalty. We know that some of your patients love you and tell all their friends to come to your clinic. The one or two who are not happy probably tell everyone. Social media has changed this exponentially. The majority of patients today (63%) are previous users. The cost of acquiring a new patient is five times the cost of retaining a previous one.
So, patient loyalty is important. Kochkin (2014) measured seven areas on a six-point scale and then took an average and viewed it as patient loyalty. The seven areas were:
- Professionalism
- Knowledge level
- Explained care of the hearing aid
- Explained hearing aid expectations
- Quality of service during the hearing aid fitting
- Quality of service post-fitting
- Level of empathy
He also knew what tests were administered to each patient and the patients’ overall satisfaction (based on the studies we previously discussed). Now we have three things that we can compare: what tests were delivered, how satisfied they are, and what they think about the person who did the fitting. How do they all relate?
When the patient did not receive verification or validation, patient loyalty is 57%. When they received verification and validation, patient loyalty goes up to 84%. Given that previous users are a big part of hearing aid sales, this could make a huge difference in the number of hearing aids dispenses by a given practice.
Clinical Tip. The clinical tip of this article is that following best practice is not only the right thing to do, the professional thing to do, the ethical thing to do . . . but, it also is the profitable thing to do. If you do not like the first three reasons, maybe the fourth one sounds attractive.
Post-Fitting Follow-Up and Counseling
Back in 1993, an audiologist named Stuart Gatehouse suggested that the brain has a characteristic of plasticity, and this relates to understanding speech. In his classic article he said: “Clinical magnitude, following experience with the prescription, would lead to a statistically significant increase in speech understanding.” As I recall, this increase in speech recognition was around 10% in his study, which has led a lot of audiologists to suggest a period of “acclimatization” for their patients who say they still do not understand as well as they would like with their new hearing aids. Is this true? Does speech recognition get better following adjustment to hearing aid amplificatioin?
A study by Dawes et al. (2014) looked at both unilateral and bilateral hearing aid fittings and symmetrical, asymmetrical, and unilateral losses. The users could not adjust the gain of the hearing aids, and they were asked to use their hearing aids for at least six hours a day, which turned out to be about 10 hours a day based on data logging.
Uniquely, they recorded event-related potentials. The stimuli were 500 and 3000 Hz at 65, 75 and 85 dB SPL. They also measured speech recognition using the FAAF at 65 and 75 dB SPL. This is a test where a target word is embedded in a sentence and is scored in percent correct.
For the unilateral-fit group, there was no difference in recorded potential amplitude at baseline and 12 weeks. Likewise, the bilateral group was the same at baseline and at 12 weeks post-fitting. The experienced users, which were really controls, because you would not expect acclimatization for experienced users showed no changes from baseline to 12 weeks, either.
As far as speech testing, no significant improvements were noted after 12 weeks of use for any of the groups. There was no acclimatization at all for understanding speech, which agrees with the auditory potentials.
Clinical Tip
With new hearing aid fittings, it would probably be misleading to tell your patients that their brain is going to adapt and that speech recognition will improve following some use of hearing aids. You could say that 12 weeks of acclimatization may not have been long enough, although the authors argue that it should be. There may be some other adaptation for loudness, which is a different issue, but it appears that you are not going to see a change in speech recognition.
Outcome Measures
The last study we’ll discuss has to do with outcome measures. Here are four outcome measures with which most of you are familiar:
- APHAB: general benefit
- COSI: benefit obtained for specific situations
- SADL: overall satisfaction
- IOI-HA: snapshot of eight different core hearing-aid-related dimensions
Maybe we need another one; that is what Robyn Cox suggested. Her article on the Device-Oriented Subjective Outcome (DOSO) was published in 2014. From previous research, she found that how you word an item matters. For example, you might get different answers if you said, “How well does the hearing aid separate speech from noise?” versus, “How well do you understand speech in a noisy place?” One of these is device-oriented question and the other is wearer-oriented. Different questions give you different results. There is also the factor of personality that could enter in.
Robyn and colleagues wanted to come up with something that was device-oriented. Cox points out that if a manufacturer wants to look at a device, they are going to want something that is device-oriented. On the other hand, third-party payers may not want a device-oriented scale; they may want something that deals more with the wearer. Researchers probably want wearer-oriented questionnaires. For you practitioners out there, you might want both.
What we now have is the DOSO. Administration time is around eight minutes for the long form and five minutes for the short form. There are percentile scores for six subscales. I encourage you to go to the HARL website at University of Memphis (https://www.harlmemphis.org), where you can find several tools, including the DOSO. The document can be downloaded for free and scored by hand, or the scoring software can be purchased for $30.
Clinical Tip
Anything that Robyn Cox does is of course well-researched and designed. This is a great scale that you can add to your test battery, particularly when you are trying to look at differences between technology, whether it is from one company to another, or comparing a special feature such as frequency lowering “on” versus “off.”
Summary
So that’s it - a quick review of some key articles, most of them from 2014. There were nearly 200 hearing aid articles published that year, so you still have a few to dig up on your own. Again, I owe thanks to Catherine Palmer and Bob Turner for allowing me to borrow their thoughts on a couple of these articles—if you like this sort of thing, check out the review the three of us did for the Featured Session on this topic at the 2016 AAA meeting, and who knows, we may just be back in 2017! I also should mention that Catherine Palmer’s Lab at the University of Pittsburgh, particularly Jenifer Fruit, is very good at tracking down all of these articles which come from over 20 different journals.
References
Aazh, H., & Moore, B. C. (2007). The value of routine real ear measurement of the gain of digital hearing aids. Journal of the American Academy of Audiology, 18(8), 653-664.
Aazh, H., Moore, B. C., & Prasher, D. (2012). The accuracy of matching target insertion gains with open-fit hearing aids. American Journal of Audiology, 21(2), 175-180. doi: 10.1044/1059-0889(2012/11-0008).
Cox, R., Alexander, G. C., & Xu, J. (2014). Development of the Device-Oriented Subjective Outcome (DOSO) scale. Journal of the American Academy of Audiology, 25(8), 727-736. doi: 10.3766/jaaa.25.8.3
Dawes, P., Munro, K. J., Kalluri, S., & Edwards, B. (2014). Auditory acclimatization and hearing aids: late auditory evoked potentials and speech recognition following unilateral and bilateral amplification. Journal of the Acoustical Society of America, 135(6), 3560-3569. doi: 10.1121/1.4874629
Froehlich, M., Freels, K., & Powers, T. (2015, May). Speech recognition benefit obtained from binaural beamforming hearing aids: Comparison to omnidirectional and individuals with normal hearing. AudiologyOnline, Article 14338. Retrieved from https://www.audiologyonline.com
Gatehouse, S. (1993). Role of perceptual acclimatization in the selection of frequency responses for hearing aids. Journal of the American Academy of Audiology, 4(5), 296-306.
Keidser, G. & Alamudi, K. (2013). Real-life efficacy and reliability of training a hearing aid. Ear and Hearing, 34(5),619-629.
Kochkin, S. (2014). A comparison of consumer satisfaction, subjective benefit, and quality of life changes associated with traditional and direct mail hearing aid use. The Hearing Review, 21(1), 16-26.
Kochkin, S., Beck, D. L., Christensen, L. A., Compton-Conley, C., Kricos, P. B., Fligor, B. J.,...Turner, R.G. (2010). MarkeTrak VIII: The impact of the hearing healthcare professional on hearing aid user success. Hearing Review, 17(4), 12-34.
Kochkin, S., Dennison, L., & Jackson, L. (2014). What is your customer loyalty quotient (CLQ)?: Applying Deming and Heskett’s principles to hearing healthcare practices. Hearing Review, 21(9), 16-21.
Mueller, H.G. (2015, May). 20Q: Today's use of validated prescriptive methods for fitting hearing aids - what would Denis say? AudiologyOnline, Article 14101. Retrieved from https://www.audiologyonline.com
Mueller, H.G., & Hornsby, B.W.Y. (2014, July). Trainable hearing aids: the influence of previous use-gain. AudiologyOnline, Article 12764. Retrieved from: https://www.audiologyonline.com
Nabelek, A.K., Tucker, F.M., & Letowski, T.R. (1991). Toleration of background noises: Relationship with patterns of hearing aid use by elderly persons. Journal of Speech and Hearing Research, 34, 679-685.
Nabelek, A.K., Freyaldenhoven, M.C., Tampas, J.W., Burchfield, S.B., & Muenchen, R.A. (2006). Acceptable noise level as a predictor of hearing aid use. Journal of the American Academy of Audiology, 17, 626-639.
Olson, S. Ø., & Brännström, K. J. (2014). Does the acceptable noise level (ANL) predict hearing-aid use? International Journal of Audiology, 53(1), 2-20. doi: 10.3109/14992027.2013.839887
Picou, E. M., Aspell, E., & Ricketts, T. A. (2014). Potential benefits and limitations of three types of directional processing in hearing aids. Ear and Hearing, 35(3), 339-352. doi: 10.1097/AUD.0000000000000004
Citation
Mueller, H.G. (2016, May). Hearing aid selection and fitting tips gleaned from recent research. AudiologyOnline, Article 17202. Retrieved from https://www.audiologyonline.com


