Editor's note: This is a transcript of a live webinar. Download supplemental course materials.
Casie Keaton: I am Casie Keaton, and I am Clinical Sales Manager with Neuromonics, Inc. We also have Marta Hecocks presenting today. She is a Clinical Specialist and will answer any clinical questions that you have regarding patient candidacy or treatment. We are both here as a resource should you need anything when starting this process and with the launch of our new product, the Neuromonics Sanctuary.
In today’s presentation, we are going to go over some fitting concepts so that you feel comfortable explaining the Sanctuary to your patients. We want to also make sure that you understand candidacy and how to fit the device. The Neuromonics signal uses music as the carrier for tinnitus management. The Sanctuary is a tinnitus management tool. We are offering situational relief, on demand, for the mild-to-moderate tinnitus sufferer. Our Neuromonics Oasis is a treatment modality for patients with more severe or debilitating tinnitus. The Sanctuary offers a management tool for patients on the lower end of the disturbance scale, those who need situational relief or have specific times when their tinnitus is bothersome.
The wonderful thing about the Sanctuary is that we are using the clinically proven Neuromonics signal in order to help these patients. With the Sanctuary, we are utilizing a customized acoustic signal, which is spectrally modified music based on your patient’s hearing profile. We are providing the patient with wide-frequency stimulation. You will be able to choose from three hearing profiles that will best match your patient’s hearing profile in order to maximize their tinnitus relief. The device provides a user-friendly set-up. You can fit this device within minutes, and many clinics are already speaking to us about having one or two in the office ready to fit on the patient the same day as their tinnitus evaluation. As you might imagine, that is a huge advantage to be able to deliver that immediate sense of relief and control to your patients.
The American Tinnitus Association reports that 50 million individuals in America suffer from tinnitus. Of those, there are about 16 million that will seek medical treatment for their tinnitus, and of those, there is a smaller subset of 2 million who have what is deemed severe or highly disturbing tinnitus. That is still a very large number. To break these numbers down, the Sanctuary is designed more for the 14 million who have definite need for relief but still have the ability to obtain a sense of control over their tinnitus. They need a management tool. For those who have highly disturbing tinnitus, the Oasis product is indicated as a formal treatment protocol and for long-term reduction of a patient’s disturbance and awareness of their tinnitus.
In today’s session, we are going to make sure that we cover candidacy considerations and who makes a good patient for the Sanctuary. We are going to take a look at the device, specifically, and make sure that you have a good orientation to what the device is and how it works. We are going to look at the fitting profile selection and how you will choose that profile for your patient for optimum relief. We are also going to take a look at some counseling topics, which, in my work with providers across the country, tends to help patients understand their tinnitus and be able to better manage and overcome its impact. We will look at device usage guidelines, how your patient is going to use the Sanctuary for optimum effect, and some follow-up considerations. At the very end, we will take some questions.
Candidacy
One candidacy requirement is that these patients have symmetrical hearing. They will need to have thresholds no greater than 20 dB between the right and left ears. You will see why that is when we look at the fitting profiles in just a moment. If asymmetries are present, then the Neuromonics Oasis product may be a better choice because it has the ability to account for the asymmetries by programming the device for each ear specifically.
With the Sanctuary, we do not want patients to have any indication of reactive tinnitus. Reactive tinnitus accounts for a rather small portion of the tinnitus population, but it is very different in nature. With reactive tinnitus, low-level to moderate-level sounds will aggravate or make a patient’s tinnitus worse. Loud sounds generally exacerbate the perception of "typical tinnitus", if there is such a thing. You are going to identify reactive tinnitus by reviewing the patient’s history. We provide a history questionnaire with our patient documents. A question on the history asks, “What makes your tinnitus worse?” Red flags would be, “The tinnitus is worse after a car ride,” or “The tinnitus is worse from listening to my computer fan.” Low-level sounds that would not typically increase a patient’s tinnitus perception are red flags for reactive tinnitus.
One of the tests that we recommend completing during your tinnitus evaluation in the office is the Residual Inhibition Test. You can get some strong indicators from that test if there is reactive tinnitus. We are going to delve more into that Residual Inhibition Test in just a moment to help you identify these patients better. We also want to make sure that there are not any significant psychological issues with depression, anxiety, or severe disturbance with the tinnitus.
In addition, we are recommending a Tinnitus Reaction Questionnaire (TRQ) score of 34 and below. The TRQ can be a great candidacy tool in helping you to understand the patient’s quality-of-life impact as a result of their tinnitus. Using the guideline of a score of 34 and below was chosen based on our own experience with patients, as well as feedback from many of our experienced providers. With a score under 35, there is not a significant daily impact on life due to a patient’s tinnitus. With a score above 35, you are getting into debilitating tinnitus where a treatment protocol is more appropriate, as opposed to the Sanctuary management tool. Additionally, we always want to make sure there is a 0 on the TRQ for question number 24, which is the question that deals with suicidal ideation. Candidates for the Sanctuary device should score a 0 on that question.
Another measurement that we recommend during the tinnitus evaluation for your patient is loudness discomfort levels.
Hyperacusis calls for a much more rigorous follow-up and treatment plan for patients, and with the Sanctuary offered at such a lower price point, it is probably not the best fit or product choice for a patient with hyperacusis. The Sanctuary does not have data logging, which the Oasis does, and as a clinician, I find that the data logging feature is helpful in working with patients who have decreased sound tolerance.
Reactive Tinnitus
I wanted to take a couple of minutes and delve into reactive tinnitus a little more. It is a rare condition, but can be quite extreme. It is based on a patient’s tinnitus perception worsening after exposure to mild to moderate levels of sound. The reactive increase tends to last for more than one day. Some indicators that raise the possibility of reactive tinnitus would be if the patient reports that their tinnitus perception has increased after completing the Residual Inhibition Test. Reactive tinnitus is also suspected in patients who report a history of overuse of hearing protection when not indicated. These are not patients who are wearing ear protection appropriately while mowing the lawn or during exposures to loud sounds; these are patients who are wearing it to the grocery store or in their car to try and limit their exposure to some of their reactive triggers. You will also see a large portion of these patients having decreased sound tolerance. The problem typically goes hand-in-hand. This is certainly a patient that we want to identify when looking at candidacy so we know which product is going to be the best choice for them.
There is a standard procedure for completing the Residual Inhibition Test. That procedure states that you give a binaural presentation of narrow-band noise at the tinnitus frequency match. The presentation level is suggested to be somewhere between 65 and 75 dB HL, but it has to be at least 10 dB over the patient’s threshold; they have to be able to hear it. Another consideration is that you do not cross their loudness tolerance level and present at a level that is too high, which would certainly increase their tinnitus perception. You present that narrow-band noise for one minute, take the headphones off, and ask the patient, “Has your tinnitus changed?” Some patients will say no. There are patients who report that their tinnitus has decreased or even gone away for a period of time. Those can be good prognostic indicators, although the literature is quite mixed on what the tests for residual inhibition indictate from a practical perspective.
There is another method for measuring residual inhibition that we feel might be a better way to identify reactive tinnitus. That is by presenting narrow-band noise 10 dB over that tinnitus frequency-match threshold. Let’s say a patient has normal hearing, and their threshold at their tinnitus frequency is 20 dB. You would present this narrow-band noise at 30 dB, providing more of a low stimulus. After one minute you ask if their tinnitus changed any. If you find that it has increased, that can be an indication that there is some reactive tinnitus there. We do have a reactive tinnitus protocol with our Oasis product where you would remove the shower sound that is embedded in the Sanctuary stimulus, or the Phase-1 stimulus. We definitely want to understand the most appropriate product for these patients.
Neurophysiology
I wanted to touch briefly on the neurophysiological model behind the Sanctuary. We know there are three elements involved with severe tinnitus patients. One has to do with the auditory portion, where there is some damage to the auditory system. The brain is trying to compensate for a poor signal, and that is where the tinnitus signal is generated. We then have the emotional aspect, where there is a stress response associated with the tinnitus perception. The third piece has to do with our attentional system, where our brain chooses to focus on certain sounds and then filter certain sounds into our subconscious.
With the Sanctuary, we are really focusing on two aspects of the tinnitus cycle. We want to give the patient that spectrally modified broadband stimulus in order to address the auditory component and counteract the compensatory mechanism the brain is trying to complete to counteract the tinnitus. We also want to give the patient the ability to cope and relax so that they can gain a sense of control, allowing them to feel better and have the opportunity to manage their tinnitus. With the Sanctuary, we are focusing on the auditory and emotional aspects. The Oasis treatment for tinnitus really includes all three. If you have a patient who is looking for long-term reduction in their disturbance and awareness, the Oasis is going to be a good choice for those patients.
Figure 1 illustrates the signal that is utilized in the Neuromonics Sanctuary. You can see a schematic of intensity over time. As I said, the music is the carrier for this process. Music is a wonderful tool in helping patients to overcome their tinnitus. It is a very dynamic stimulus. There are times when it is louder and times when it is softer. In order to give the patient a high level of interaction and maximum neural stimulation, we add in a shower sound that helps to cover the troughs of the music when the music is softer. It gives the patient maximum relief, and the ability to facilitate that sense of control and feel better. We are looking for reduced awareness during listening sessions. We are not looking to see a lot of carryover with the device off. We provide four musical tracks from which the patient can choose, and we also provide a wide-frequency stimulation out to 12.5 KHz.
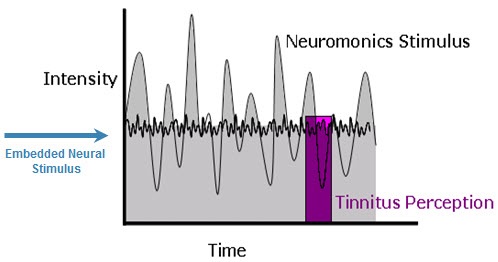
Figure 1. Customized acoustic signal in the Sanctuary management device.
Fitting Profiles
Marta Hecocks: I will be talking about some of the specifics regarding the fitting profiles, as well as some device mechanic specifics. There are three hearing profiles (Figure 2) that are preprogrammed into the device that you use to customize the device to be appropriate for your patient’s thresholds. Our experience at Neuromonics is that roughly 75% of audiograms will be accommodated by one of these fitting profiles. As Casie mentioned earlier, it is a requirement that Sanctuary patients have symmetrical hearing. If a patient does not have symmetrical hearing, the Oasis treatment device would be more appropriate because it is programmed ear-specifically to account for any differences between ears. The Sanctuary programs both ears to the same level.
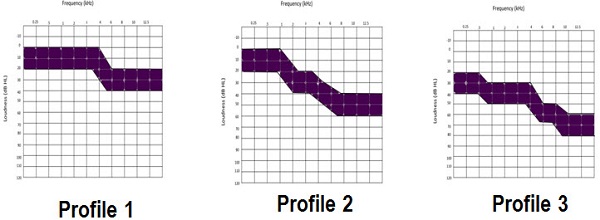
Figure 2. Three fitting profile selections; 75% of audiometric thresholds should fall within one of these fitting ranges.
We are going to talk about these profiles in depth, but I can say here that we are recommending that 75% of your patients’ audiometric thresholds fall within one of the profiles that you choose. We would recommend that you choose a profile that provides your patient with the most adequate stimulation so that they are able to obtain relief from their tinnitus at a comfortable listening volume. I will also add that testing the ultra-high frequencies of 10,000 Hz and 12,500 Hz is not a requirement in order to fit your patient with a Sanctuary device. They are necessary for the Oasis device, but for the Sanctuary, it is included in the prescription.
The first fitting profile will accommodate symmetrical thresholds from normal hearing through 4,000 Hz with borderline normal hearing or a mild loss in the ultra-high frequencies. The second profile shows that it will accommodate symmetrical thresholds from normal hearing in the low frequencies, sloping to thresholds of about 40 to 60 dB in the ultra-high frequencies. The third fitting profile will accommodate patients with symmetrical thresholds with hearing loss in the mild range in the low frequencies, sloping to thresholds of 60 to 80 dB in the ultra-high frequencies. These three profiles are going to audiometrically be appropriate for a large number of patients. We will talk about some of the practical aspects of how to choose these fitting profiles a bit further on in the presentation.
Getting to Know the Sanctuary
How does the device work? I will review some of the basic mechanics. We think you are going to love that there is no software required in order to program the device to the patient’s fitting profile. There are buttons on board that you will use to navigate through a menu structure in a quick and straightforward manner. The Sanctuary has a rechargeable medical-grade lithium ion battery that will operate for approximately 24 hours. Patients may only have to charge it once a week or so. It comes with either a wall recharger or a micro-USB cord that the patient can plug into their computer for convenience. The device can also be used while it is being charged, which is different from the Oasis device, which could not be used during the recharging process.
The center button (Figure 3) is going to be used to power on the Sanctuary; it is also used to start and pause the four music tracks. Let me mention that the music tracks last for approximately 60 minutes. Patients have the option to skip between tracks if they prefer certain selections over others, or they can listen to them one after the other. The center button also allows access to the set-up menu. That is where you are going to find the sleep timer, which we will talk about in a minute, and where you will find the play mode selection.
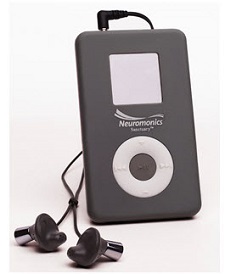
Figure 3. Sanctuary device.
This is where the patient can choose to play the tracks either in a continuous fashion or at a single time only. When the patient selects the continuous mode, the entire track list will play continuously until the device is turned off by the patient. If they choose the single mode, the track that they choose will play through once, and then it will fade out and end. This is a good selection that the patient can use at bedtime for falling asleep.
The center button is also going to allow you to access the clinician menu. The clinician menu is where you are going to select the headphone model and one of the three fitting profiles. This menu is only able to be accessed by the clinician, as there is a password. The patient is not going to be able change their hearing profile or the headphone type.
The forward and backward arrows can be used to select the tracks. There are four tracks. Two of them are baroque-type music, which patients tend to report they like for concentration activities, and two of the tracks are more spa-like, which patients report liking for relaxation. Some patients prefer to listen to a variety of tracks or to a single track several times. This will also be used to select the desired time for the sleep timer. The sleep timer has an ability to play from 5 minutes to 120 minutes before it shuts off. If a patient knows they can fall asleep in a half hour, they could select 30 minutes, and then their device would shut off after that time.
The plus and minus buttons can be used to adjust the volume incrementally. Each time the patient starts a session or turns on the device, the volume will be starting at a minimum volume level. The volume will need to be increased incrementally to a comfort level every time the patient turns on the device for a listening session. The plus and minus buttons are going to be used to highlight the headphone selection area. The reason that the headphone model must be selected in the device is that the music profiles have been exactly matched to the spectral profile of the headphones. This means that headphones other than the ones we are going to include are not designed to deliver the appropriate acoustic stimulus. You will also use the plus and minus buttons for highlighting the hearing profile. We will talk about how to make to that clinical decision.
There are two headphone choices (Figure 4). On the left are the Sony headphones, which come standard with the device. We like the Sony option because they are durable, easy to use, and easy to keep clean. However, it is always nice to have options. On the right you can see the Bose IE2 headphone option. This could be ordered by the patient as an upgrade for an additional charge. These headphones may be good for patients who have fit concerns with the Sony phones. The nice thing about the Bose is that they come with three different ear tip sizes. It is another option for patients. We talked about the fact that you need to select the appropriate headphones that the patient is using within the device.
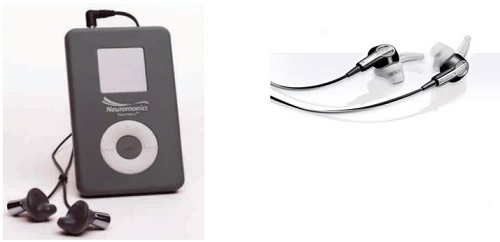
Figure 4. Two headphone choices offered by Neuromonics: Sony (left; default), Bose (right; upgrade).
Another option that we are excited about offering with the Sanctuary is an auxiliary speaker. That is available to patients for a small additional charge. We see it being used at times when patients need exposure to the music stimulus when they are not wearing the earphones. A good example of this would be during bedtime, if they cannot use the earphones comfortably. This is a practical solution to help patients find relief while they are trying to fall asleep, which is the number-one complaint of tinnitus disturbance.
Fitting Profile Selection Guidelines
Let’s talk about how you will make the decision as to which profile (Figure 2) to select for your patient, based on their audiometric needs. On your assessment form, you will have this graph (Figure 5) that you can use to help you make this decision. After completing the audiogram, you are going to use the threshold data that you acquired at each frequency, and you are going to see if the threshold range is included either in fitting No. 1, No. #2, or No. #3. You will circle the range in which the patient’s threshold is included. You are going to be looking for equal to or greater than 6 circles in a fitting threshold if you have assessed out to 8,000 Hz. You are going to be looking for 7 or more circles if you have assessed the patient out to 10,000 and 12,500 Hz.
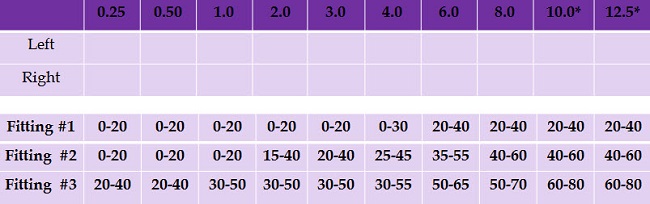
Figure 5. Fitting profile selection chart, which is completed after measuring the patient’s audiometric thresholds.
Here is an example in Figure 6. Let’s look at 250 Hz. You can see that the patient has a threshold of 10 dB for the left ear and a threshold of 5 dB for the right ear. Since these thresholds of 5 and 10 would fall into a 0 to 20 range, you can see that at 250 you would be able to circle fitting range No. 1 and fitting range No. 2. I was not able to use circles on the slides so I have indicated this is red. You can see that in fitting profile #1, based on these thresholds, you would be able to circle 4 of the ranges. In fitting profile No. 2, you can see based on this patient’s audiogram that you would be able to circle 8 of the ranges. Then in fitting profile No. 3, you can see that 2 of the ranges are circled. Therefore, we can see that this patient is a nice candidate for fitting profile No. 2. Again, our recommendation is that if you have tested out to 12500 Hz, you would want to have 7 or more circles indicated.
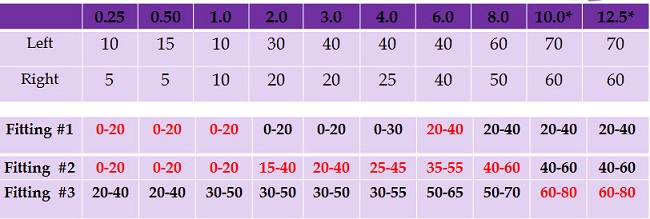
Figure 6. Example of fitting profile selection for a patient with normal sloping to severe hearing loss. Red numbers indicate into which fitting range the patient’s thresholds fall.
There may be patients who are going to fall into a gray area. If this is the case, it would be left up to your clinical judgment as to the best fitting profile selection. You want to make sure that the patient is going to experience enough relief through having adequate stimulation to cover their tinnitus at a volume that is comfortable to them. You will have a demo device there, and you will be able to try this out with the patient.
Counseling Topics and Device Usage Guidelines
Neuromonics’ approach is that tinnitus education and device expectation management is a crucial and an integral part to the overall success of a tinnitus management program. To assist the clinician with patient education, we have some topics that we recommend, and we provide several supplemental materials to address these topics. Some of the topics from which all tinnitus patients will benefit include understanding tinnitus in a general way and as it relates to their specific history, understanding how the Sanctuary will address mild-to-moderate tinnitus disturbance, and its scientific mechanism of action. It is also important that patients understand the goals and expectations that are associated with Sanctuary use. We also talk about general tinnitus management strategies that patients can use such as stress reduction, avoiding common tinnitus triggers, et cetera. Then patients will need good instruction on how to use the device in its most effective manner to receive situational relief from their tinnitus perception, as well as contraindicated activities that can impede relief. Additional counseling points include a phenomenon known as relief contrast and conditions that aggravate tinnitus.
We have lots of information and supplemental materials that will assist the patient. One important book we have is the Tinnitus Management Handbook, and another is the Sanctuary User Manual. The Tinnitus Management Handbook has sections such as "Understanding your Tinnitus", and "Changing How you Think About your Tinnitus", and it has the schematic of the stimulus that Casie covered earlier (Figure 1). It has some good tips for success and talks about how to set the volume level on the device. The user manual has a very nice section on effective usage, covering things like when to use the device, how long to use the device and how to listen. Both resources are excellent for the patient to take home so that they can have written information to reinforce your counseling topics.
I am going to turn this back over to Casie and she will talk about some of the management goals and expectations.
Casie Keaton: When you are educating your patient at the fitting appointment, we want to make sure we cover the goals and expectations when wearing the Sanctuary device so we can set them up for success. As we have said before, the Sanctuary is a tinnitus management tool used to provide relief from tinnitus perception while the device is being worn. Having been a Neuromonics clinician now for several years, I know the powerful effect that the Phase-1 stimulus can have on patients in helping them to gain a sense of relief when they are experiencing that extreme stress response; they need a tool to be able to manage that impact at that time. I think this is going to be a huge asset to your patient in that way.
One of our experienced providers who has had wonderful success with the Neuromonics Oasis and has had many patients overcome their tinnitus asked me, “Why the Neuromonics Sanctuary when we know the Oasis works so well?” The answer to that is very simple. Through our experience with working with patients and providers over the years, we have found that there is a whole subset of patients that do not have a daily tinnitus disturbance and do not require the daily usage schedule required in the Oasis protocol. There are a lot of patients who only need situational relief - something that is going to give them the ability to overcome their tinnitus at that point in time. As you know, there are quite a few products that fall short in achieving this goal. We are paring down what we know works for tinnitus patients and providing a device to those who need it in order to help them manage the impact of their tinnitus. The Sanctuary is not a long-term protocol.
With the Sanctuary, we are looking to achieve a sense of empowerment and control when using the device. It definitely can help with relaxation and concentration. We want to provide patients with a listening experience that is comfortable, pleasant, and relaxing. We sometimes take for granted that many of these patients are not able to relax. A lot of them spend much of their life on edge, working so hard to tune out the signal that is causing them so much distress. To be able to give them the ability to take the edge off, to take a deep breath and to relax, is hugely powerful in this process.
We also want to provide a perception of music that is comfortable, pleasant and in stereo when listening to the device. We also need the ability to carry on most everyday activities while listening to the device. Because the music has been spectrally modified based on their hearing profile, part of the algorithm applied to the patient’s audiogram attenuates the low frequencies and then gives the emphasis in the high frequencies where most patients have the greatest difficulty. A lot of patients are able to listen to the Neuromonics stimulus without it impacting their speech intelligibility. They can typically carry on a conversation and not have to take the device off to do so. The goal is to fit this into their lifestyle as seamlessly as possible so that they can get the most benefit from it.
Next, we will talk about some of the Sanctuary usage guidelines. We are directing patients to use the device in situations that are most impacted by their tinnitus to obtain relief. We want them to use it at a volume that is comfortable while still providing as much relief from the tinnitus as possible. The goal is not necessarily to completely cover the tinnitus; it is designed to provide a distraction. Patients may worry that this does not fully cover their tinnitus. That is not always the goal, however. Sometimes a freight train is not going to cover the tinnitus. The goal is to have something that is pleasant and relaxing that can take the edge off, and give the brain another stimulus to focus on so that the patient is not so impacted by the tinnitus.
We are asking patients to place the music in the background of their awareness and avoid tuning in to the music during a listening session. We want them to "set it and forget it". We also will ask them to use more volume to give them more relief from the tinnitus as long as it is comfortable. As I said, some patients will work very hard to cover the tinnitus as much as possible. Whenever you are using something at a very high volume, it definitely takes away from the relaxation and the pleasant aspect of the stimulus, which defeats the purpose. We want to make sure that they are not listening to it in that way.
Relief Contrast
There is another instruction having to do with relief contrast. This is a common perception that many tinnitus patients experience whenever they are using any sound source to mitigate their tinnitus. Let’s look at relief contrast a little more specifically. It does not matter if you use the Neuromonics stimulus, music, fan noise, some type of sound generator, water running, or a fountain, as long as you are able to give the patient good coverage of their tinnitus. The second that sound source is removed, the patient’s tinnitus perception can seem increased. The reason is that there is too stark of a contrast from that comfortable place of relief from the tinnitus to zero sound source whatsoever. The tinnitus can seem much more noticeable. This perception is typically short-term. But in my experience with patients, although it is short-term, it can definitely affect them negatively and cause a lot of anxiety, when we could help prevent it by giving them some education.
First, I always educate my tinnitus patients as to what this is so they understand this phenomenon. Some patients will experience it and some will not. If you can head off that anxiety before giving it a chance to take hold, your patient is certainly in a much better position than if you did not share the information at all.
A strategy to minimize relief contrast is to advise the patient to decrease the volume setting a few minutes before ending their listening session. This essentially puts the device on a dimmer switch, much like your light switch. If you think about it, when your light is on at its full setting, the light may be very comfortable. However if someone turns the light out for a few minutes and then quickly flips that switch back on, it takes your eyes a few minutes to adjust, and that process is not always comfortable. The same thing can happen with using a sound source to give a patient relief from their tinnitus. If they will gradually transition from the relief that the device provides back to their tinnitus, it provides a much more comfortable transition and can help to head off any anxiety they have about turning off that sound source. Advising the patient to remove the device in an environment that is not completely quiet, so there are some environmental sounds, can help them to mitigate their tinnitus perception, and it is not such a black-and-white transition. Those are things that we have found to be helpful to patients over the years.
There are a few contraindicated activities with the Sanctuary, just as there are with the Oasis. We do not want them to use the device when they are straining to hear conversation or the television. They can watch TV, but we do not want them to try to be tuned into any dialogue, especially if they have significant hearing loss, because it turns out to be too competing of a signal. Their brain is straining to decipher what is being said, and we know that to be a cause of increased perception of a patient’s tinnitus.
If we think about what the device is working to do (slow the resting heart rate, counteract the patient’s stress response associated with their tinnitus, give them that ability to relax), it does not make sense for them to wear this while they are exercising strenuously and getting their heart rate up. We want to make sure that they use their Neuromonics for those times when they are able to relax and work to counteract the stress response. We also do not want them to use it while they are driving. There are many states that have headphone laws where they are not able to use headphones while driving. Also, I do not know about where you live, but in my area, driving is not the most relaxing of activities. We always want to pair our Neuromonics products with the ability to take the edge off, to be able to relax, and driving is typically not one of those activities.
If patients have difficulty with their tinnitus in the car while they are driving, because traffic is a stressor (and we know stress to be a trigger for tinnitus), we will often suggest some sort of ambient music, whether it is the spa-relaxation type of music or classical; it is very personal. We encourage patients to look for music that will provide them that relief from their tinnitus in that situation and save their Neuromonics for alternative times. Lastly, we do not ever want to get the device wet.
Counseling Aspects
Here are some additional counseling points. The following are scenarios that we know may temporarily make a patient’s tinnitus perception worse: recent cold, flu or allergy, Eustachian tube dysfunction, excessive ear wax, new or changed medication, noise exposure, extended periods of straining to hear clearly, and periods of acute stress. These are things that we always want to troubleshoot if there is any increase in perception. We always want to have patients work closely with their primary care providers, and if a patient is not progressing as we would like or has plateaued with the device, then that is an area that we may want patients to investigate with the supervision of their physician; perhaps trying a different medication or dose to help in mitigating their tinnitus. Excessive noise exposure is a big point. We have to make sure that these patients are protecting their hearing appropriately and preventing any further damage to their auditory system. We know that to be the genesis of tinnitus perception. Any time they are continuing to expose themselves to excessive noise, it resets any headway that we were able to make with Neuromonics products.
Extended periods of straining to hear clearly can be tricky. You could have a patient that has an aidable loss, but due to their current situation, they do not really perceive any communication difficulties. Things change. Jobs change. Lifestyles change. If they suddenly find themselves in a different situation where their lifestyle is requiring them to hear better, that can definitely increase a patient’s tinnitus perception. We want to make sure that any untreated hearing losses are being addressed. To help with stress, we want to check in with the patient and ask what they are doing to mitigate and manage stress in their everyday life. Suggestions like exercise and taking a personal time out are things that we often do not take the time to do in our busy lives. But ask them to do whatever it is that they enjoy, such as walking in the neighborhood or reading a novel or taking a bubble bath. Make sure patients are having some time to decompress. That is completely necessary in this process.
Resources
We want to touch briefly on some of the clinical resources that we provide you to streamline this process and help patients to understand their role. We have a Clinician Resource Guide that includes fitting criteria, user protocols, warranty/loss/damage information, and some of the business aspects including conditions of sale, service and repair policies. We are happy to provide this to you in an electronic format prior to your first Sanctuary order. A hard copy always ships with the first order. We also have a patient handbook that is being dispensed for the Neuromonics Sanctuary. This is a patient education handbook to help understand what tinnitus is and how to optimize benefit with the device. Having this in written format certainly goes a long way in helping them to understand and remember those concepts that you discussed verbally, and to be successful with the device.
Follow-Up Considerations
We will quickly go over some follow-up considerations with the Sanctuary. Follow-up is going to be dictated based on patient needs and your own clinical judgment, as it should be. We are suggesting a one-week phone call post-fitting to make sure the patient does not have any questions and is on the right track, and then potentially a four-week post-fit check to put together some outcomes from the Sanctuary usage. You should identify three or four patient goals at the fitting appointment so that the patient understands how to use the device and what to expect from it, and then you make sure the patient is getting relief and meeting their goals at those follow-up calls. We provide the TRQ to use as a follow-up outcome measure, a patient feedback form, as well as for checking on those patient goals.
We are suggesting a retail price for the device, and we strongly encourage you to consider a fee-per-visit follow-up model. We have thought about the different types of patients that you are going to encounter with the Sanctuary, and I think there are going to be quite a few that will require little to no follow-up. Maybe the initial fitting fee plus the cost of the device is appropriate. Then there may be some patients who require more follow-up for counseling or suggestions on how to use the device; you may want to have them pay on a per-visit model. We are happy to talk to you more in depth about this, because it needs to be the right model for your practice. We are certainly not dictating one way or the other; you have the choice as to how to do this.
Consider that because the Sanctuary is offered at a lower price point, you may have patients who are truly Oasis candidates but may try to get away with utilizing the Sanctuary to address their tinnitus needs when it is probably not the most appropriate choice. We do have a waiver that says something to the effect of, “because of your TRQ score and possible need for further psychological evaluation or therapy, you are not a good Sanctuary candidate, but you have decided to go this route and these are some of the things you can expect from using the Sanctuary.” Then you, the clinician, and the patient sign the document. This is a great way to have everyone on the same page so patients understand what they are getting into, and you are protected in terms of your recommendations to patients.
Summary
The Sanctuary is a tinnitus management tool, providing situational tinnitus relief for those patients who have mild-to-moderate tinnitus disturbance. It is for those with TRQ scores of 34 and below as a guideline, but if you would like to talk about patients more specifically, Marta and I are happy to do so. Product selection is not always black and white, and we are glad to talk about patient specifics and help you in making those choices. The device is a customized stimulus, and we are offering a same-day fitting opportunity, giving patients an immediate sense of relief and positive impact on their tinnitus. Also to mention, it is at a much lower price point than we have ever been able to offer in the past, with the Oasis being a much more involved treatment protocol. The Sanctuary is being offered at a lower price point, opening a solution up to many more patients that you see in the clinic every day. We think this is going to be a great option, and we would love to work with you.
Questions and Answers
How can the speaker be selected on the device?
There is a clinician menu that you will use to select the fitting profiles. From here, you will also choose the headphone selection so that all of those things will line up, because the frequency responses are different for each transducer and you want to make sure that you have selected those appropriately. There is not a selection on the device for the pillow speaker. We are currently in further development as to how to do that, but I would say it is to come shortly.
Cite this content as:
Keaton, C., & Hecocks, M. (2013, June). Fitting the Sanctuary device: A New tinnitus management tool by Neuromonics. AudiologyOnline, Article 11947. Retrieved from https://www.audiologyonline.com

