This is a transcript of a live webinar. Download supplemental course materials.
Thank you for joining us for this course which introduces the Sanctuary, the new Neuromonics tool for managing tinnitus. I am Casie Keaton, and I am going to be giving the presentation today. We also have with us Marta Hecocks, who is a clinical specialist and an audiologist providing clinical support to our accounts.
We are excited to be able to offer Sanctuary to you and your patients in your clinical practice. We will provide an overview of the Neuromonics Sanctuary today. We are also going to answer from a very practical perspective the question, “What does the Sanctuary offer my patients?” You are going to be talking to patients about what this product does in terms of expectations during the tinnitus evaluation. We will also be answering the question, “What are the Sanctuary fitting profiles?” so that you understand the types of hearing profiles that are appropriate for this product. We are also going to look at who is a candidate for the Sanctuary device.
Next, we are going to discuss when you would choose the Neuromonics Oasis treatment for your patients as opposed to the Sanctuary, which is a management tool, as well as some of the clinical tools available. We will talk about what kind of follow-up is recommended, and how you structure follow-up appointments. Another important question we get asked is, “What tests are recommended when evaluating a tinnitus patient?” We will also cover the codes that are included or recommended in the tinnitus assessment as well as the average reimbursement rate. That is a very important issue from a business standpoint.
What is the Neuromonics Sanctuary?
Sanctuary is a new tinnitus management tool for your patients. We are using the clinically proven Neuromonics stimulus to provide patients the opportunity for relief, relaxation and a sense of control over their tinnitus. However, the Sanctuary is going to be in a pared-down format for a few important reasons that we will discuss in just a moment. The Neuromonics Sanctuary provides a semi-customized, spectrally modified music, because music is the carrier for this process. The music is based on your patient’s hearing thresholds. You will choose from three fitting profiles to best match your tinnitus patient’s audiogram for relief optimization. That is an important aspect of what we are working to accomplish.
Figure 1 is the Sanctuary product itself, as well as some accessory options that are available to you when placing your order. You can see that the Sanctuary device is very similar to an MP3 player. We wanted to have that familiarity for patients. They know what this is and how to access the different musical tracks or programs and the volume control. The Sony headphones are the default choice that will ship with this option, but there is also an alternative headphone, the Bose IE2s, that can be ordered separately. There is an additional cost for those, and I see those only being utilized for patients with fit concerns due to the size and shape of their ear canal. The Sony headphones will fit most of your patients, but it is nice to have the Bose option if needed.

Figure 1. Neuromonics Sanctuary device with headphones and desktop speaker.
We also offer an auxiliary speaker. This was a big need that we learned about with our current treatment for tinnitus, the Oasis. There are times where patients need to be able to have exposure to the stimulus outside of their headphones. I definitely see patients utilizing the speaker bedside for better sleep onset. Many tinnitus patients are not able to find a comfortable position with the headphones in order to get good relief for sleep and to fall asleep quickly. They are able to sleep more soundly and stay asleep for longer periods of time with the speaker. Often, sleep is a patient’s number-one complaint in terms of their tinnitus. If you can help a person to regain sleep, not only from a quantitative standpoint, but also a qualitative standpoint, that can change things entirely.
We see many patients who have the need for a desktop speaker. They can use it to increase concentration while they are trying to work or answer e-mails; tinnitus can be a very distracting factor in their day. Just remember that the speaker is an additional accessory and does not come standard with the device. If you do need that option, make sure to specify that when you place your order.
Programs
There are four acoustic programs provided with the device. The music is spectrally modified. There is an algorithm applied to the music to shape it in order to give the patient maximum relief from their tinnitus. In addition to that spectrally modified music, we also imbed the Neuromonics neural stimulus, which is a broadband sound that gives maximum coverage of a patient’s tinnitus. That signal is very important. If you are familiar with our Oasis treatment for tinnitus which has been our tinnitus product since 2007 in the United States, there was a daily requirement usage of 2 to 4 hours in order to accomplish the long-term treatment goals with the Oasis product. We want to make sure that our Sanctuary providers understand that there is no daily usage schedule with this device. The Sanctuary is used to provide situational tinnitus relief. They are going to use it as needed to gain that sense of control, be able to relax, and counteract that stress response associated with their tinnitus.
We include two styles of music. We are trying to appeal to as many people as possible using a classical style as well as a spa relaxation style of music. Studies showed that classical pieces can have a better impact on patients being able to comprehend or concentrate, and spa relaxation type of music, such as nature sounds can help patients fall asleep faster, slow the resting heart rate and take the edge off. Patients can choose between the two types of music to maximize their benefit based on their situation and what they are trying to accomplish.
One of the biggest advantages to our Sanctuary product is that there is no software needed in order to interface with the device. Previously, we used an infrared connection that was needed to interface with the device and program it, so to speak. With the Sanctuary, there are device menus housed on the device itself. You are going to access a clinician menu and be able to choose a fitting profile for your patient, fit them within minutes, and have them out the door very quickly. You will be able to deliver that relief as soon as possible to help these patients regain their function and quality of life. That is ultimately what we are after- giving them the ability to take their life back from how the tinnitus negatively affects them. We think the ability to have this device in-house is going to be a great asset. You can order some Sanctuaries to have in the office when you are doing your tinnitus evaluations, and then be able to fit them the same day as that evaluation. The patient can go home happy, feeling better, and on their way to a better quality of life. That is an exciting piece of this new product.
Neurophysiology
I wanted to touch quickly on the neurophysiology behind the Sanctuary, our goals, and what we are working to address with this device. With severe tinnitus patients, we know that there are three components that play a role in creating this severe tinnitus. One component has to do with the damage to the auditory system. The brain is trying to compensate for the damage, and that is where the tinnitus signal is generated. There is also an emotional aspect with limbic system involvement, which is where we process our emotions, and the stress response is a result of the patient’s tinnitus perception. It truly can be a phobic response and a physiologic response where the heart rate and respiration quickens. The third piece involved has to do with our attention system, what our brain chooses to focus on, and how it can filter sounds out and place them in the background. That piece has to do with the patient’s awareness of their tinnitus and how much they hear it.
Our tinnitus treatment product, Oasis, addresses all three of those aspects, because we are looking for long-term reduction in a patient’s disturbance as well as their awareness of their tinnitus and facilitating habituation. Going back to the Sanctuary, we are working to address both the auditory and the emotional pieces of the tinnitus cycle with the Sanctuary. We are working to provide that broad-frequency stimulation with the music, customize a spectrally modified signal based on their hearing profile, and target the emotional response by providing the relaxing music and address the tinnitus response to the patient’s tinnitus perception.
With the Sanctuary, we are addressing these two components. That is the differentiating factor between the Sanctuary and the Oasis. The Sanctuary is a management tool working to help patients get that sense of control and relief while wearing the device, and the Oasis is more of a treatment protocol looking for habituation and long-term reduction of the awareness and disturbance of the tinnitus. We love to talk to you about your tinnitus patients. What are their specific characteristics? Why do you think they are a candidate for one product or the other? We would love to speak with you if you ever want to run anything by us. Often it is not a simple black-and-white answer. Sometimes we have to read between the lines and use our interview skills as a clinician to understand these patients and what is going to be the best treatment modality for them. Please feel free to reach out to us. We love to do that, and we would be glad to discuss specific patient cases with you.
Figure 2 is a schematic of the acoustic signal for the Sanctuary. Again, we are utilizing what we know is clinically proven to provide patients that high level of interaction, maximum neural stimulation, and relief and reduced awareness during their listening sessions. We are not looking to see the carryover with the Sanctuary device off, like we do with the Oasis treatment. The Sanctuary signal is the spectrally modified music. In addition to that is the imbedded neural stimulus, that broadband frequency sound, to give that patient maximum interaction and relief from their tinnitus. You can see that there are peaks and troughs to the music, translating to times when the music is louder, times when it is softer. Music is a very dynamic stimulus, and in order to cover up the troughs when the music is softer where patients’ tinnitus perception could potentially peak through, we add in that neural stimulus for that maximum interaction, control, and relief during those listening sessions.
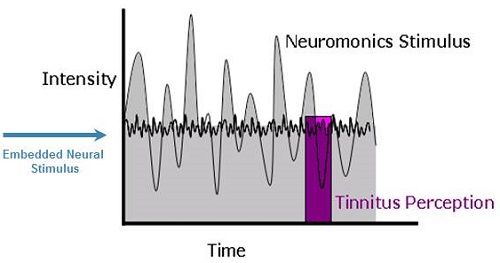
Figure 2. Acoustic signal over time, showing where the Neuromonics stimulus is embedded.
What does the Sanctuary Offer My Patients?
For me, an extremely important question is, “What does the Sanctuary offer my patients?” To answer that question, we are utilizing what we know works in providing patients a high degree of relief for their tinnitus. The Oasis has been clinically proven, both in our own clinical trials as a company, as well as 10 independent clinical studies with over a 1,000 patients included in those investigations. That is a lot of people and a great amount of data. With the Sanctuary, we are working to effectively address the tinnitus stress response, giving the patient that on-demand sense of relief and control when using the device. A big advantage I alluded to earlier is that fast, easy patient delivery, having the device in-house, and being able to dispense it same-day. After hearing reports from our current Oasis providers, we have addressed one common suggestion, and that is the need to have something in a lower price point to offer those patients who do not need a formal treatment protocol for their tinnitus.
Fitting Profiles
One provider asked me last week when we were discussing one of her Oasis patients, “Why the Sanctuary? Why are you going in this direction?” To answer very simply, we have been in the market in the U.S. since 2007. We have seen thousands of patients over that period of time and worked with providers very closely in evaluating those patients for candidacy and what treatment modality would be the best option for them. Our experience has shown us that there are a few different categories of tinnitus patients. First, we have the severe tinnitus patient who is significantly impacted by their tinnitus and who needs a formal treatment protocol. Their daily function is impacted, and they have a very high Tinnitus Reaction Questionnaire score. They need a formal programmed protocol in order to effectively treat their tinnitus. That is the simple black-and-white-category that we have encountered to date.
Next, you have this different subset of patients who may not have a daily tinnitus disturbance. Maybe it bothers them 3 or 4 times a week or only during specific situations, such as not being to sleep or having specific stresses during meetings or life events. These patients do not need to wear a device 2 hours a day. They need to be able to have the flexibility to use it as needed and get the effect that they are looking for. Additionally, these patients are not clear hearing aid candidates. They are not going to benefit much from amplification, so these patients have near-normal hearing or mild high-frequency losses where they do not perceive any communication difficulties. A formal treatment approach is not appropriate for those patients.
A lot of these people who are coming in searching for a solution have not been right for the treatment that was available at the time. Our goal is to have something that we know is clinically proven. We know it works giving by patients the ability to relax, take the edge off, and address the stress response, but it is built more as a management tool. I think this is going to be a big help from a practical, everyday perspective. Many of the patients you see are not on the severe spectrum. They need situational tinnitus relief. That is where the Sanctuary comes in and where I see it being a great asset to your practice and your clinical offerings to your patients.
Figure 3 is a nice screenshot of the three Sanctuary fitting profiles. We are recommending that 75% of your patients’ audiometric thresholds fall within that fitting range. We will have a future presentation specifically on fitting the Sanctuary device. We are going to get into these profiles more specifically and talk about how to select them. I just wanted to give you a brief introduction to them so that you can start thinking about what types of patients would be right for this product. Remember that you have those devices menus that allow you to select between the three profiles for your patient.
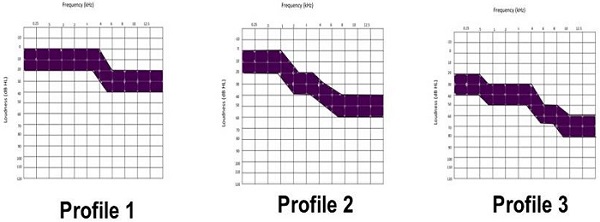
Figure 3. Sanctuary fitting profiles.
Let’s look at each one specifically. You can see in Figure 3 that Profile 1 is essentially normal hearing through 4,000 Hz, where it slopes to more of a mild loss in the high and ultra-high frequencies. That is another important part here. If you are familiar with the Oasis product, that was a requirement in the prescription and a limitation to a lot of providers, because you had to be able to have the ability to assess 10,000 Hz as well as 12,500 Hz. There was the need, in some cases, to purchase additional equipment. With the Sanctuary, those thresholds are included in the prescription, but they are not required. I think this is going to be easier for most clinicians to provide because there is not an additional equipment requirement to provide those ultra-high frequencies in the prescription.
Profile 2 is normal hearing through 1,000 Hz, then sloping from mild to moderate, and then moderately-severe in the highs and ultra-high frequencies. Again, we are asking for 75% of your patients’ thresholds to fall within that profile range.
Profile 3 is for those patients who have more significant hearing loss, mild to moderate in the lows, sloping to more of a severe loss in the highs and ultra-high frequencies. This profile covers a wide range of patients for which this is appropriate. I encourage you to look at your patient databases again. Those patients who might have been tested and were not right for the products available at that time may now be good candidates for the Sanctuary. We have had a lot of success with that.
This is a new launch for us. We have only been offering this to our clinics for the past month, but we have seen success in mining those patient databases and offering this to some patients who have already completed a tinnitus evaluation.
Who is a Candidate for the Sanctuary Device?
Let’s go over some of these candidacy points more specifically. We have designed the Sanctuary for patients who have a low to moderate tinnitus disturbance. A guideline we are using is a Tinnitus Reaction Questionnaire score of 35 and below. I am not sure if you are familiar with the Tinnitus Reaction Questionnaire, but it is the gold standard, along with the Tinnitus Handicap Inventory, in terms of assessing a patient’s quality-of-life impact as a result of their tinnitus perception. It is a 24-question candidacy tool to help you learn more about how a patient is affected by their tinnitus. Scores above 35 are typically associated with more significant issues on the psychological end with anxiety and depression. Those higher scores are typically going to indicate a need for tinnitus treatment beyond what the Sanctuary can provide as a management tool. We also want to make sure that our Sanctuary patients have a score of 0 on question number 24. That is the suicidal ideation question. Any patient who scores higher than 0 immediately needs to be addressed. They are typically not a candidate for the Sanctuary device. Patients also need to have symmetrical hearing. We define that as their thresholds not differing by more than 20 dB between ears. The fitting ranges are within 20 dB at each frequency. Beyond that, they are probably going to need the more specific prescription that the Oasis provides, because if there are huge asymmetries between ears and the device is providing an equal stimulus to both ears, that unbalanced effect can have an impact on their enjoyment of the music and their ability to relax, and it can be frustrating and distracting.
Along those same lines, we also want to make sure that these patients have no indication of reactive tinnitus. Reactive tinnitus affects a very small percentage of tinnitus patients, but they are out there. The difference between a reactive tinnitus patient and a typical one (if there is such a thing) is that with typical tinnitus, loud sounds exacerbate the tinnitus perception. With reactive tinnitus, it is typically low to moderate intensity sounds that will heighten a patient’s tinnitus perception. One red flag for me on the patient history is road noise. If they report that their tinnitus is through the roof while in the car, that is typically a tinnitus that is more reactive in nature. Other sources of noise are fan noises from the computer and water running. Typical tinnitus patients get relief when they are in the shower, or by the shower sound. Reactive tinnitus patients do not like those sounds because they heighten their tinnitus perception. A great way to identify that is through the patient history. You may just ask the patient in your interview, “What makes the tinnitus worse?”
As part of the diagnostic tinnitus assessment, there is the Residual Inhibition Test. That test provides narrowband noise at the patient’s tinnitus frequency for one minute and then the clinician asks the patient, “Has your tinnitus changed as a result of stimulation to that sound?” If their tinnitus seems worse, then that can be an indication of residual inhibition. In that fitting presentation that we are conducting this week, we are going to delve a bit more deeply into the Residual Inhibition Test and will be able to help you to identify these patients better. Remember that the Sanctuary stimulus is music with that neural stimulus imbedded, the shower sounds. That sound can be uncomfortable or have a negative impact on patients with reactive tinnitus. We want to make sure that we identify those patients at the outset before dispensing this product to them.
Lastly, a candidate for the Sanctuary device should have no significant history of psychological disturbance, depression or anxiety. That is usually going to come out on your Tinnitus Reaction Questionnaire score, by having scores in the 60s, 70s and higher. Those scores typically indicate more significant psychological components. Formal treatment is indicated more for patients who have a significant psychological component as opposed to the management tool that the Sanctuary provides.
We are also looking for those patients who are seeking situational tinnitus relief. During your interview with your tinnitus patient, ask them what areas of their life are most impacted by their perception of the tinnitus. Specific situations may include sleep, concentration or being able to relax in the evening. Those patients are going to benefit from the Sanctuary as opposed to those patients who have high awareness of their tinnitus and hear it more often than not. Patients who are seeking a device for tinnitus management as opposed to long-term treatment outcomes are good candidates for Sanctuary. I often ask patients during the evaluation, “What are your goals for this process?” By asking that question, you learn about the patient’s expectations. What are they hoping to gain out of this process? From there, you can better determine if you should recommend the Sanctuary or the Oasis.
There are a couple of different scenarios of patients who I think would be great Sanctuary candidates. These would be normal hearing patients where a hearing aid is not indicated or patients with very mild hearing losses that do not perceive communication difficulties. There are also those patients who wear hearing aids that are looking for relief beyond what the hearing aid may provide. I specifically think of patients who may get a good amount of coverage of their tinnitus while wearing their hearing aids, but in quiet or when they take the hearing aids out, the tinnitus is just as bothersome. With the Sanctuary being offered at a much lower price point, I could see offering this as a package to patients. The hearing aids can address the hearing loss, which also has an impact on tinnitus, but beyond that, the Sanctuary can provide relief in those situations where the hearing aids may fall short.
Neuromonics Oasis or Sanctuary for Treatment?
I have already been talking about this quite a bit, but I wanted to specifically answer this question. The Oasis treatment is indicated for those patients who have a severe tinnitus disturbance and high level of awareness. This is usually a daily issue, where their quality of life is impacted on a daily basis. A guideline for Oasis is those patients with a Tinnitus Reaction Questionnaire score of 35 and above. We have chosen that number based on our experience with patients, as well as on feedback from our experienced providers who have been doing this for a number of years. I have had people come in for their evaluation and say they have had to either stop working or change their line of work because of this issue. They are not sleeping. They are having relationship difficulties because they are always on edge. They are not themselves and are not functioning as they would like to be. For those patients, a daily dose of two or more hours is going to be prescribed. A formal treatment protocol is a better choice in helping them to achieve long-term reductions of their awareness and disturbance of their tinnitus. Again, we would love to talk to you about these patients and who are candidates for each. It is often not a black-and-white decision. You have to account for many different factors when making this decision and look at the patient from a global standpoint, not just their tinnitus. We need to factor in their hearing loss and any sound sensitivity issues they have. That has to be a part of your treatment recommendation in this process.
What Clinical Tools are Available to Me?
One of the things that I am most proud of as a Neuromonics clinician is that we provide a lot of materials to help support you troubleshoot and provide the most optimum treatment for your patients. We offer a Clinician Resource Guide that is specific to the Sanctuary, and in that guide we provide fitting criteria, user protocol, administrative topics having to do with the warranty, loss and damage, terms and conditions of sale, and then the service and repair policy. We can certainly send you an electronic copy of this, but a hard copy will also be shipped with your first Sanctuary. It is a great tool and resource as you are beginning to fit the Sanctuary.
The Clinician Counseling Guide is an invaluable tool when treating tinnitus patients. We provide this to you at absolutely no charge. This guide is an amazing resource for when you are treating tinnitus patients, looking at some of the issues you may encounter in their treatment process, troubleshooting techniques, counseling suggestions, and answering frequently asked questions. It helps prepare you for anything you might encounter. This was written by our Neuromonics audiologists. The marketing people were not involved, so this is truly a clinical resource for you in your practice. This is available electronically, but we can also send you a hard copy.
I love this next resource because it is literally at your fingertips. It is the Neuromonics Professional.com site. Once you are set up and certified as a Neuromonics clinician, you have this site available to you to access clinical resources. We have all of our peer-reviewed articles on there. Some patients like the ability to have those on hand. There are also patient forms which gives them advice on diet, medication, sleep and relaxation. There is a lot of great material right at your fingertips that you can use as a provider and also pass along to your patients.
How do I Provide Follow-up?
Follow-up is going to be based on your patient’s needs as well as your own clinical judgment, as it should be. We have a suggestion of making a one-week phone call to make sure that they do not have any questions and are using the device properly. Then you might give them four-week in-office follow-up to make sure that they are achieving those goals that we set with the use of the Sanctuary. Some of those goals would be the ability to relax and maintain a sense of control while wearing the device.
We have a suggested retail price for the device, but we want you to think about unbundling your services for this device. Based on our experience with patients, we feel like there is going to be a number of patients who are going to require very little to no follow-up with this device. There may be patients, however, who want to come in for additional counseling sessions and additional follow-up. We are proposing a fitting fee or a set per-office visit in addition to that suggested retail price. That way, patients are paying for the services that they need. I see it playing out in two different ways. You can have that patient who needs very little follow-up and therefore does not need to spend the extra money to do so, but then you could have a higher-needs patient who may even need the Oasis treatment, but decided to go with the Sanctuary due to its lower price point. If you bundle the cost of the Sanctuary, with it being at such a lower price point, I can see where some patients may take advantage of that by trying to achieve some of the same outcomes with the Sanctuary that are indicated with the Oasis and trying to get more office visits from you than what they are paying for. I think setting up that expectation of the fee-per-visit helps them to understand that any additional services they need will have an office visit fee. I would be happy to talk to you more about that in depth; it has to be right for your practice. You need to set up a model that is going to work best for you. We are trying to think about every scenario in order to help you be the most successful with it. We would love to hear to your feedback and are happy to answer any questions or help you in setting this up.
What Tests are Recommended when Evaluating a Tinnitus Patient?
I am often asked what tests we recommend. Our recommendation is to include the following tests in your tinnitus evaluation:
1. Tympanometry, to rule out any Eustachian tube dysfunction;
2. Otoacoustic emissions (OAEs) are a great tool because many of these patients may present with normal hearing on the audiogram, and using the OAEs may identify decreased outer hair cell function. If you are going to help a patient to pursue reimbursement from an insurance company, OAEs can be a great resource;
3. Comprehensive audiometry;
4. Assessment of tinnitus which includes pitch matching, loudness matching, minimum masking level and residual inhibition. The CPT code does not include residual inhibition, but we recommend that because of the importance of identifying a reactive tinnitus patient for this product;
5. Loudness discomfort levels are an important piece of the tinnitus assessment in identifying hyperacusis, decreased sound tolerance, and making your clinical decision.
Figure 4 shows the coding and reimbursement table, including the 2013 Medicare rates for each procedure. Medicare rates are typically bottom of the barrel; the reimbursement for four procedures totals about $140, which is not terrible for about an hour’s worth of time with a patient. Of course, private insurance carriers often include higher reimbursement rates. We want to make sure that you have those codes available and know what to expect for reimbursement so that you can factor that in to what you charge the patient.
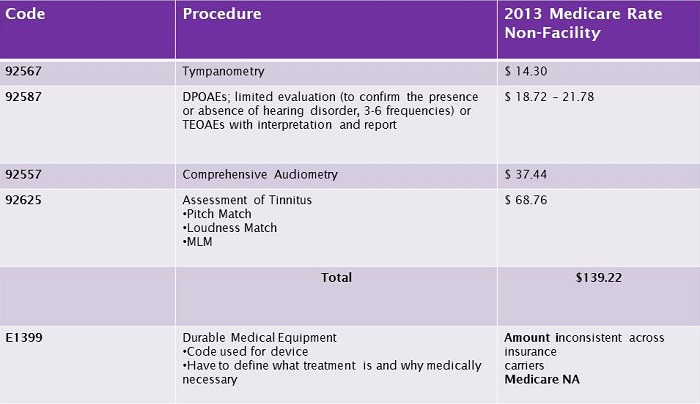
Figure 4. Codes and Medicare reimbursement rates for procedures included in tinnitus evaluation.
Also included here at the bottom of the chart in Figure 4 is the E1399 code, which is the durable medical equipment code used for the device. You have to define what the device is and why it is medically necessary, because insurance companies are typically not familiar with it. The reimbursement amount is extremely inconsistent across insurance carriers, and it is not covered by Medicare. We do have some additional resources to help you in pursuing reimbursement, so definitely reach out to us, and we can pull from our experience with providers and patients thus far.
Summary
Just to summarize, our tagline for the Sanctuary is “Providing patients relief when they want it,” and most importantly, “Relief when they need it.” We are offering this as a tool for your patients to be able to cope and manage their tinnitus in those situations where they are negatively impacted. Think about sleep issues, concentration and those specific scenarios where a tool is indicated in helping them manage their tinnitus.
I appreciate you taking the time to join us this afternoon. We are very excited about the opportunity to offer the Sanctuary to your patients and give them the ability to achieve the relief that so many patients need. We hope this is going to be a great resource to you and your patients, and we look forward to working with you and sharing the success that you have with your patients.
Question & Answer
Is there a return policy or period for the device?
We do provide a 30-day return option if the patient is unable to fit it into their lifestyle or is not achieving the relief that they are looking for with the device. You do have the ability to return the device if need be.
We are recommending some outcome measures with the Sanctuary. As an audiologist, validation of your tools is important. Our suggestion is administering the Tinnitus Reaction Questionnaire at 4 weeks, prior to the end of their trial period. I think it is a good idea to identify three or four goals associated with their disturbance or quality of life impact at your fitting appointment so that you can make sure that those areas are addressed with the Sanctuary.
Cite this content as:
Keaton, C., & Hecocks, M. (2013, June). Introduction to sanctuary. AudiologyOnline, Article 11917. Retrieved from https://www.audiologyonline.com/