Editor’s Note: This text course is an edited transcript of a live webinar. Download supplemental course materials.
Dr. James Hall: We will be discussing evidenced-based clinical applications of otoacoustic emissions (OAEs) in children and adults. In the first lecture in this series, I made some assumptions about the audience, but also about audiologists in general. One of the assumptions, based on my conversations with thousands of audiologists over the years, is that most audiologists underutilize OAEs.
One way they underutilize OAEs is by simply not applying them where there is evidence that they help. That is the focus of today’s lecture. I hope by the end of this lecture, some of you will recognize that you are not using OAEs as much as you could. You would not be overusing them in these populations, and there is research evidence to support it.
Learning Objectives
The learner objectives are to identify four evidence-based applications of OAEs in children, identify four evidence-based applications of OAEs in adults, and list three clinical advantages of OAEs in the auditory assessment of children.
Agenda
Today I will begin with an introduction to clinical application of OAEs and move into listing their many advantages. We use OAEs because of their clinical advantages in assessing both children and adults. In one hour, I do not have time to cite all of the literature in support of the applications in children and adults, but I will highlight some of the evidence-based literature. I encourage you to do your own literature review by using a search engine. From time to time, I will make reference to searches that I have done and how many articles these searches have yielded. You can do the same to keep up with current literature.
Cross-Check Principle
The cross-check principle underlies most of what we do in diagnostic audiology, and certainly with children. The same principle does apply to adults. OAEs are now a critical part of the test battery and fit right into the cross-check principle. When Deborah Hayes and Jim Jerger were seeing patients, OAEs had not been discovered. Even in 1978 when they made their debut, clinical audiologists did not have access to them. That did not come for another 15 years or so. OAEs, are now a very integral part of the cross-check principle.
The original test battery described in Jerger and Hayes’ 1976 article was a good test battery at that time. This included:
- Behavioral audiometry
- Immittance (impedance) measurements
- Tympanometry
- Acoustic reflexes (contralateral only with SPAR)
- Auditory brainstem response (ABR; brainstem-evoked response audiometry or BSER)
- Click stimulus air conduction
- Click stimulus bone conduction
The main point was that you cannot rely on behavioral audiometry entirely to evaluate children’s hearing. They were relying on objective tests or electrophysiological tests like immittance measures and ABR.
Forty years later, we have a more powerful, comprehensive test battery. Every audiologist should take the opportunity to utilize whatever procedures might contribute the diagnosis of auditory dysfunction in a patient. You will not use all of these procedures with every patient, but you should be prepared to.
One of the biggest flaws in diagnostic audiology today is that audiologists keep using the same limited test battery, dominated by behavioral tests. The more appropriate procedures you apply in a patient and the more carefully you analyze the results, the easier it is to make the diagnosis. You get to the point where there is no other option but one diagnosis when you have enough tests and test findings.
OAEs
OAEs are an integral part of today’s test battery for both children and adults. Clinical guidelines include OAEs. These clinical guidelines are our blueprint for how to assess patients. In fact, from a medical-legal point of view, our professional liability is high if we do not follow clinical guidelines. You can find these guidelines on the internet. Any non-audiologist can track them down quickly. All the lawyer would need to do is say, “I am going to subpoena all of your test results on this child.” Those results will be reviewed and they will have the guidelines on one side and all the tests you did on the other, and they will match them up. If there is a gap and a patient ended up being misdiagnosed and mismanaged, then you would be found negligent. You would be found guilty of not following standard of care.
The Joint Committee on Infant Hearing guidelines (2007) specifically require OAEs; infants are defined as birth to six month, or longer if the baby was premature. The American Academy of Audiology (AAA) Clinical Practice Guidelines for Childhood Hearing Screening (2011) also include OAEs. The Guidelines for Identification and Management of Infants and Young Children with Auditory Neuropathy Spectrum Disorder (ANSD; 2010) specifically mention OAEs. The AAA Pediatric Amplification Practice Guidelines (2013) also make reference to OAEs. They are an important part of our test battery.
The way we categorize and describe OAEs has changed in recent years. The current taxonomy or categorization system is mechanism based rather than spontaneous versus evoked. We talk about how OAEs are produced and then put them into different categories. As we discuss clinical application of OAEs, do not assume that transient and distortion product OAEs are the same or are giving you the same information. If you have the equipment and the option, I would recommend that you record both transient and distortion product OAEs in all diagnostic patients, especially children. You can charge for the diagnostic OAE code, which would be met by performing both types of OAEs. You will get more clinical information from both types of OAEs than just one.
OAEs: Mechanism Based
OAE mechanisms are different for transient versus distortion product. There are cases where one OAE can be normal and the findings for the other OAE type was abnormal. Using just one could have mistakenly led to misdiagnosis of patients.
Remember that we are not just evaluating outer hair cells - we are getting a more accurate diagnosis when we use OAEs. Depending on the pattern of findings and how they relate to the other test findings, we may be able to discover problems with stereocilia, the motor protein Prestin, the stria vascularis, or any other number of structures within the cochlear or the peripheral auditory system.
OAE Advantages
Evaluate Outer Hair Cell Function
What are the clinical advantages for OAEs? They are diverse and they are powerful. First, we know that there is no better way to evaluate outer hair cell function than to record OAEs. The audiogram provides us with very little information about hair cell function. Studies show that only a couple of working hair cells are required in a critical band of the cochlea to obtain a normal threshold. However, for OAE amplitude to be entirely normal, virtually every outer hair cell has to be functioning. Almost everything that can go wrong in the cochlea initially involves the outer hair cells, such as noise exposure, ototoxic medications, or presbycusis. They are like “canaries in a coal mine” for hearing. If the OAEs are normal, you can be assured that outer hair cells are still functioning well, but as soon as there is a problem with the OAEs, you know there is dysfunction in the cochlea.
Every time you have a powerful advantage, there will be a downside to the technique. In this case, site specificity is a big advantage. When OAEs are abnormal and we have ruled out a middle ear problem, we can be certain there is an outer hair cell problem. An abnormal audiogram does not tell you anything about the outer hair cells. But with OAEs, we can be confident that the outer hair cells are not functioning normally if the OAEs are abnormal, assuming we have ruled out technical problems and middle ear dysfunction.
Objective
OAEs do not require a behavioral response. That is a huge advantage for infants and young children. It is good for patients who cannot participate in traditional testing due to factors such as language, cognitive function, motivation, and attention. It is the lack of a requirement for behavioral response that OAEs were so quickly adapted for newborn hearing screening.
Ear Specificity
They are ear specific. Imagine you have a two-month-old infant where hearing loss is suspected. Most likely, attempting behavioral audiometry will yield non-ear-specific sound field findings. However, if you have normal sound field responses to speech and some tones and perfectly normal OAEs for each ear, the likelihood of that child having hearing loss is now very slim. Sound field responses to speech alone without the OAEs would not rule out hearing loss of some kind in both ears. The ear specificity can be used to your clinical advantage.
Frequency Specific
They are highly frequency specific. With an audiogram, you test information at octave frequencies. From 1000 to 2000 Hz, there are a thousand Hz in between. But with OAEs, you can start exploring inter-octave regions, and with transient OAEs, you can go about every 40 Hz to get another data point. With distortion products, using 10 frequencies per octave gives you a data point every 100 Hz. Take advantage of the frequency specificity. You will see that it comes in handy with a lot of different patient populations.
No Sound-treated Room Required, Portable
Another advantage is that you do not need a sound-treated room, but you do need a quiet patient. They are portable, so you can take them to the patient in most cases. There is an averaging process involved which reduces background noise, but also the ear is being sealed up tightly with a probe. There is a lot of ambient noise, but it will not interfere with responses. You can record OAEs with some modification of the protocol in a nursery or in a Head Start program.
Time Efficient
OAEs can be quick. If you are doing OAE screening in preschools, kindergartens or on infants, thirty to forty-five seconds per ear is not uncommon.
Adds Validity
There is also more value when you are combining it with other technologies. When you combine OAE and automated ABR screening, the screening validity, sensitivity and specificity are high in comparison to just one of those technologies.
Inexpensive
Another advantage is that OAEs are relatively inexpensive. You can use the screening OAE code. Your time commitment in performing the task is relatively short, and it is an efficient way to gain a lot of information.
Crystal Ball Effect
One of the big advantages is that OAEs are almost like looking into a crystal ball for a patient’s hearing. The research clearly supports this statement. In other words, today their audiogram may be normal, but if the OAEs are beginning to show a notch in the 3000, 4000, or 5000 Hz region but the audiogram does not show it yet, we are looking into their future. We can foresee problems for them down the road. Based on this information, we can counsel patients effectively on how they can prevent more hearing loss from happening.
Preneural
Another important concept about OAEs is that they are preneural. All of the OAE activity we are recording occurs before the very first synapse in the afferent auditory system. When you record OAEs, they can be perfectly normal in a patient who has no auditory nerve, whose auditory nerve has been severed or who does not have proper neurotransmitters for between the inner hair cells to the afferent fibers.
OAE Disadvantages
Noise
OAEs are susceptible to noise. The more sound there is in the ear canal, the harder it is to detect what we are trying to record.
Middle Ear Dysfunction
Middle ear status is a big factor. Because we are putting sound through the middle ear and recording small sounds that have to come back through the middle ear, any middle ear dysfunction can stifle that response.
Site Specificity
The specificity of OAEs to outer hair cells has a downside. We only get information about the outer hair cells. That is not a problem if we use OAEs with other procedures that do give us information on inner hair cells, the auditory nerve, and other structures.
Predicting Degree of Hearing Loss
The disadvantage associated with high sensitivity to cochlear to dysfunction is that the OAEs may be abnormal or absent in someone who does not have bad hearing. You cannot predict degree of hearing loss with OAEs. Some of the best and the brightest hearing scientists and audiologists have used all kinds of statistical attempts to predict hearing loss with OAEs, but you just cannot do it. In fact, anyone with a sensory hearing loss due to outer hair cell dysfunction more than 40 dB will not have OAEs. That does not mean they cannot hear.
In fact, sometimes you will not see OAEs in patients with a 20 dB hearing loss. We cannot use OAEs to estimate hearing loss, but that is okay, because we have other ways to do that. We are not measuring hearing with OAEs. That is the important point. We are measuring outer hair cell integrity or function. You can have a profound hearing loss and normal OAEs. We see this with auditory neuropathy. You can have abnormal OAEs and good hearing sensitivity. OAEs are not a test of hearing, nor do we ever want to imply that they are.
Pediatric Applications of OAEs
One of the most valuable applications of OAEs is infant hearing screening, although we are not going to talk about that today. We are going to talk about the diagnosis of children and use of OAEs in other applications. If you would like to know more on OAEs and automated ABR entirely for infant hearing screening, register for the course here. I am confident in the screening outcomes of all three grandchildren because OAEs have been studied since the early 1980s as a screening technique.
The Joint Committee on Infant Hearing (2007) includes numerous references to OAEs in the document. OAEs are a critical part of the screening program. They are in the test battery for infants zero to six months, but they are also in the test battery for six-month-old to two years old. They do not have quite the same role, because these behavioral tests that are minimally important in the infant, perhaps not even feasible, become more important in children older than six months. That does not mean that OAEs are no longer important, however.
Diagnosis of Auditory Dysfunction
Diagnosis of auditory dysfunction is essential and depends on the use of OAEs. Newer hand-held screening devices are very reliable and durable, and you can use them diagnostically. I no longer say that someone should have to make a decision between a screening device and a diagnostic device as now you can get the best of both worlds in a single device.
If you are evaluating a young child for the first time, always suspect auditory neuropathy and you will never miss it. I never say this to the parents, but in the back of my mind, I am saying that I want to prove that this child does not have auditory neuropathy. By the end of the test battery, I want to be confident that we are not dealing with auditory neuropathy or a false hearing loss in older children. One easy way to do that is to record OAEs in every patient. The clinical guidelines for diagnosis of auditory neuropathy spectrum disorder (ANSD) always include OAEs.
Ototoxicity
There is almost no better way to monitor ototoxicity, particularly with young children, than with OAEs. Many audiograms of patients who receive ototoxic medications on a frequent basis (e.g., cystic fibrosis, chemotherapy) will have a ski slope hearing loss after about 1000 Hz, where not only do you have poor sensitivity, but also distortion in the cochlea and very poor word recognition. It is a problem in terms of management, because a hearing aid may not help, yet there is such good hearing in the low frequencies that a cochlear implant might not be immediately considered. This kind of hearing loss can be prevented, and OAEs can be a big part of that prevention.
The AAA guidelines for ototoxicity monitoring (2009) were written by a task force of well-recognized audiologists. In these guidelines, you will see a reference to distortion product OAEs. This type of OAE is well-suited for ototoxicity monitoring because it provides information to the highest frequencies, sometimes up to 16,000 Hz. With transient OAEs, because of the nature of the stimulus and recording OAE activity from the basal part of the cochlea, there is still stimulus in the ear canal, and we cannot detect OAEs for the highest frequencies, which are coming back from the cochlea so quickly that they are mixed in with the stimulus. You must use distortion product OAEs.
The rationale for OAEs as a technique for monitoring for ototoxicity and assessment for ototoxicity are as follows:
- Highly sensitive to cochlear (outer hair cell) dysfunction
- Most ototoxic drugs first damage outer hair cells
- Aminoglycosides (e.g., gentamicin)
- Loop diuretics (Lasix or furosemide)
- Cisplatin
- Objective (can be performed on sick patients)
- Brief test time (one or two minutes)
- High degree of frequency detail (selectivity)
- High-frequency limit up to 10,000 Hz (DPOAEs only; TEOAE limit is about 5000 Hz)
- Earlier detection of cochlear auditory dysfunction compared to audiogram
I do not know of a single drug that selectively damages the inner hair cells. They are all going to affect the outer hair cells. OAEs are quick. If you have a child that is very sick, they can be sleeping and do not have to be motivated or paying attention. You can take OAEs anywhere. If there is a pediatric clinic seeing a lot of children getting ototoxic drugs, have them put an OAE device into their budget. Give them an in-service and they can do all the screening. The nurse can do this every time the child comes into the clinic.
Any audiologist in any pediatric setting should be monitoring for ototoxicity. Very often, the physicians who are giving the patient potentially ototoxic drugs come to the audiologist and ask if they can do the monitoring for the patient.
General Diagnostics
For other diagnostic applications, we record a baseline OAE and then any time the OAE decreases more than the test/re-test variability, particularly in the highest frequencies, we immediately alert the physician.
School Screenings
Another pediatric application is preschool and school-age screenings. Even if you are in a state where 99.5% of the children are undergoing screening, the percentage of those children who fail the screening and should get the diagnostic assessment is far less than 99%. In some states like Texas with rural areas, less than 40 to 50% of the children who failed the screen came back for the diagnostic test.
One way to find these children who have hearing loss and did not come back after they were screened at birth is to perform preschool screening. At least then, they will be detected. You will also be detecting the 15% of all children with hearing loss who have a delayed onset or progressive loss. In other words, if you take 100 children with hearing loss and look back at their status at birth when they were screened, 15 of those 100 children passed the hearing screening, but now have a significant hearing loss. You will pick those children up with preschool screenings, and school screenings will pick up older children.
Back in 2004, there was only one article from the University of Queensland in Brisbane, Australia by Lyons, Kei, and Driscoll on this topic. It showed that distortion product OAEs were just as good as using pure-tone screening, particularly when combined with tympanometry. There is controversy in some of the guidelines for childhood screening. Some are negative about OAEs, saying that they best way is pure-tone screening and that every preschool child who is screened should be screened with pure tones. Keep in mind that no screening recommendation is going to be implemented if it is not feasible.
The first thing any clinician asks is if they can do it. They do not care how good the recommendations are for the screening; they want to know if they can do it. You cannot expect a non-audiologist to comply with something they cannot do. The failure rate for preschool screening in the hands of non-audiologists, and even in the hands of some audiologists, using pure-tone techniques is sky high. OAEs get around this. I have never had a single child simply refuse an OAE screening. I take a middle ear analyzer, the handheld OAE machine, and an otoscope. That is all I need to do preschool screenings.
The literature on this is growing. In one study (Kreisman, Bevilacqua, Day, Kreisman, & Hall, 2013), students went to schools and preschool settings and started screening almost 200 children. They collected the data with pure-tone conditioned play audiometry plus OAEs. The screening time was a fraction of what it was with pure tones alones. The screeners in this case were students who had had much more experience with pure-tone audiometry than the average nurse or non-audiologist.
When we look at the time it takes to perform these procedures, high-frequency distortion product OAES from 2000 to 5000 Hz took less than one minute for the whole screening protocol compared to pure tones. There is no instruction that requires time and there is no problem with reliability. We know we are going to get good results.
When we looked at the pass/fail rate, we found that we are failing more children with OAEs than with pure tones. The pure-tone proponents will say that means that pure tones are more accurate. I say it does not. OAEs are more sensitive to cochlear dysfunction. We are missing children with cochlear dysfunction or mild middle ear dysfunction using just pure tones. We are picking them up with the OAEs. The more sensitive screening technique is always better, and with pure tones, you will have some children who simply refuse to cooperate. But we can screen virtually every child with OAEs.
If we are using OAEs in the preschool screening application, we want the OAEs to be validated compared to pure tone audiometry, if it could be done. We are not just saying that any child who had any serious problem with their ear needs to be detected. We want to detect children who would have failed a pure-tone screening. We want to pick up any child with hearing loss of 20 dB or more. The way you do that is to use an absolute criteria of 0 dB for the DP (Stover, Gorga, Neely, & Montoya, 1996). In other words, they pass if their distortion product is greater than 0 dB at all frequencies. They fail if the OAE is in the negative region. That is different than saying they pass if the OAE is 6 dB above the noise floor. The 0 dB cutoff is a much more rigorous criteria. We know that the cochlea with normal outer hair cells will produce an OAE greater than 0 dB. Here we are trying to find any child with a cochlear problem rather than just children with significant permanent hearing loss.
False or Exaggerated Hearing Loss
We need to make sure that every patient we think has a hearing loss has a true hearing loss. The identification of a false hearing loss or exaggerated hearing loss goes far beyond malingering. I am not talking about malingers, necessarily, and it is a term I do not use with a patient or in a report. It is a very negative term. You could probably be sued for implying that a patient is a malingerer when they were not.
False hearing loss can occur in anyone, not just adults. In fact, it is quite common in children. Doing a quick Medline search will yield several results for a review of the literature on the topic of pseudohypacusis. In children, particularly younger children, whenever you are recording normal OAEs but the audiogram is abnormal, you will suspect a false hearing loss. You need to investigate audiologically to prove whether or not they have hearing loss, and you need to get a thorough history.
The most common explanation for a false hearing loss in a young child, sadly, is emotional trauma or abuse. You may be the first person to realize that something unpleasant and traumatizing is going on in that child’s life when you find normal OAEs and they are giving you an abnormal audiogram. You need to follow up on this.
One of the other important reasons for identifying false hearing loss is that you do not want management to be implemented assuming there is a hearing loss, because that management may actually cause a hearing loss. Examples of this include a child being fit with hearing aids when it looks like they have a hearing loss, but it is not permanent, and the audiologists did not do OAEs, or a child gets steroids for what appears to be a sudden onset of hearing loss, when in fact it is a false hearing loss.
With older children and adults, you can confront them with your normal OAEs and perhaps some other normal findings such as normal acoustic reflexes. Then when they know that you are on to them, they may come clean. Again, there is a lot of literature on OAEs and false hearing loss and the advantages of accurately diagnosing hearing in these patients.
Adult Applications for OAEs
OAEs are not just of value in children. There are evidence-based applications of OAEs in adults. Research articles that support these applications. These applications include:
- Diagnosis of cochlear versus retrocochlear auditory dysfunction
- Identification of false and exaggerated hearing loss, including malingering
- Monitoring ototoxicity
- Hearing screening
- Industrial settings
- Military personnel
- Early detection of cochlear dysfunction in noise/music exposure
- Diagnosis and management of tinnitus & hyperacusis
If in an adult OAEs are normal and there is a hearing loss, one of the first things you want to think about is a retrocochlear pathology. False and exaggerated hearing loss can certainly happen in an adult, as well, sometimes in worker’s compensation cases. OAEs are not quite as useful in monitoring for ototoxicity in adults because some adults may not have had OAEs at the beginning of treatment because of presbycusis or noise exposure. If the patient has normal hearing and OAEs at baseline, then they can be used in adults to monitor ototoxicity.
Hearing Screening
Hearing screening with OAEs has a role in adults. In an industrial setting, once you have proven the audiogram is normal and the OAEs are normal, then the patient can be monitored with OAEs without having to undergo audiometric screening constantly. This is the same for the military population. Early detection of noise exposure or music exposure is a good application of OAEs in adults, as well as the diagnosis of tinnitus.
Noise-Induced Hearing Loss
We are trying to preserve normal outer hair cell function and prevent irreversible damage; we can do that by using OAEs. In Pretoria, South Africa, I did an experiment with my colleague to record the intensity of a vuvuzela (Figure 1). The output of the vuvuzela was 130 dB at a close distance. If this colleague were a spectator in front of me, his ears would be hit by that, as well as by hundreds or thousands of these vuvuzelas at sporting events.

Figure 1. Measuring the output of a vuvuzela.
We have many articles on noise and the damage it does to hearing (see www.audiologyworld.net for references). Sources could be football games, automobile racing, target shooting, power equipment, motor vehicles or motorcycles particularly with straight pipes, loud computer games, as well as all kinds of music, including band and marching band. The percentage of people in the general population exposed to potentially music or noise-induced hearing loss is phenomenally high. OAEs can help determine whether that exposure to sound is causing any problems.
Case study. The following case is a 62-year-old woman plays the violin, teaches the violin, and plays in a community orchestra. Her hearing was quite unremarkable with a very slight dip in only the left ear where the violin is located (Figure 2).
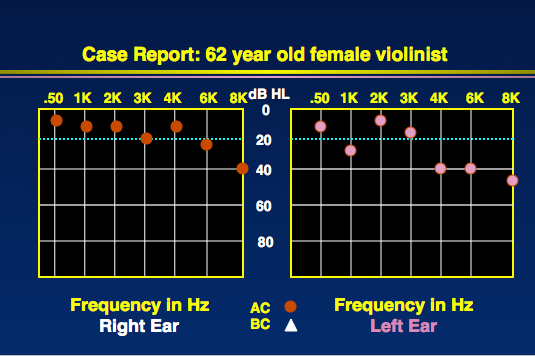
Figure 2. Audiogram from 62-year-old musician.
However, OAEs were very abnormal, even at frequencies where her hearing sensitivity was normal (Figure 3). At one frequency, she did not have an OAE. If we compare the audiogram versus OAEs, the OAEs will always detect problems more than the audiogram.
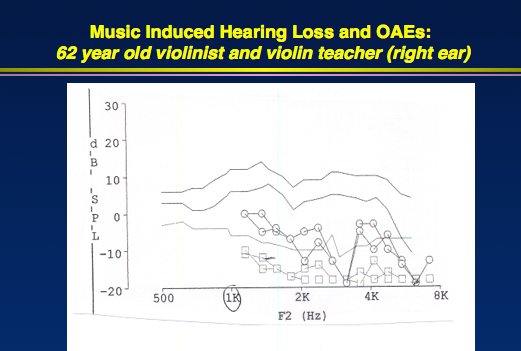
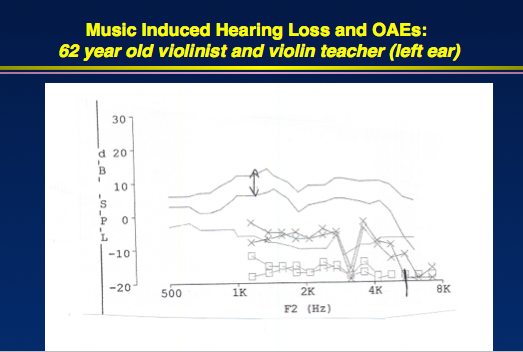
Figure 3. OAEs from 62-year-old violinist, indicating cochlear dysfunction that did not manifest on the audiogram (right ear, top; left ear, bottom).
False Hearing Loss
I saw a 49-year-old patient who came from the Department of Labor. He had been seeking compensation after saying he had been electrocuted and had noise exposure, which was why he lost his hearing. His audiogram in Figure 4 shows 50 to 60 dB thresholds, worse for the right ear. Reflexes were almost at the same level as his pure-tone thresholds. There was a huge difference between the pure-tone average and the speech reception threshold (SRT), however.
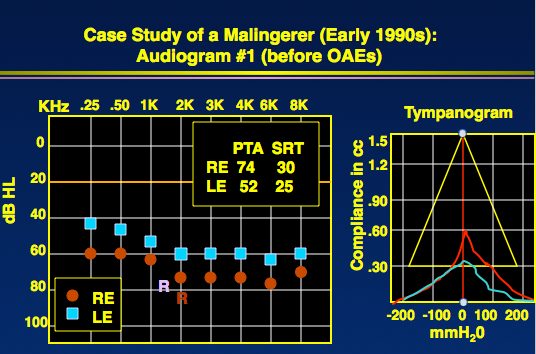
Figure 4. Audiogram and tympanogram of a patient suspected of false hearing loss.
I performed transient OAEs after the audiogram, which were normal. When I told him that I knew he had normal hearing, I took him back in the sound booth, and he did, indeed, have normal hearing.
Other Applications
Meniere’s disease is another application for OAEs, as is tinnitus and ototoxicity monitoring, which we do not have time to cover extensively today.
Summary
There are many valuable and evidence-based applications of OAEs. I hope each of you review your test protocol in your clinical setting and begin to use OAEs. Take advantage of them. They can help you to more accurately identify, diagnose, and manage patients with hearing loss.
Questions and Answers
How soon after the administration of the ototoxic drug can OAE changes be seen? Is there a timing issue to consider when monitoring?
This is a good question, and it highlights the real reason why OAEs are so important in ototoxicity monitoring. You cannot predict who is going to develop a problem and who will not. There are genetic explanations for who is going to get an ototoxic hearing loss. If a person has ever had ototoxic drugs in the past, they are more likely. If they have any hearing loss or if they are getting more than one ototoxic drug, which is common in some settings, they are more likely. It also depends on renal function. The timing is highly variable. I have seen patients go through a one-month course of an ototoxic drug wherein that month we start to see changes. In some cases, they can be rapid and in other cases, very slow. If the OAEs are done at least at the baseline and after the first round of an ototoxic drug, such as cisplatin, you will always pick up changes with OAEs well before the audiogram shows any change. There is still time to stop the process.
Do you see a day when OSHA standards are rewritten to include OAEs for industrial monitoring of threshold shift instead of pure tones?
I think the OSHA standards take so long to develop and is such a conservative process that I do not see that ever happening. There is nothing keeping you as an audiologist or a hearing conservation program from supplementing OSHA standards with OAEs. OSHA standards are basically geared toward documenting noise-induced hearing loss rather than preventing it. We have done some experiments and have a publication that came out in South Africa with people working in gold mines, and there have been other studies showing that if you follow OSHA standards in the United States and add in OAEs, you can be more effective in getting people to wear their hearing protection because you will be seeing changes in their cochlea from not wearing the hearing protection properly before the audiogram goes bad. It makes the hearing conservation program far more effective to use OAEs, and you can still be in compliance with OSHA standards, which are not as rigorous.
References
American Academy of Audiology. (2011). American Academy of Audiology clinical practice guidelines: Childhood hearing screening. Retrieved from https://audiology-web.s3.amazonaws.com/migrated/ChildhoodScreeningGuidelines.pdf_5399751c9ec216.42663963.pdf
American Academy of Audiology. (2009). American Academy of Audiology clinical practice guidelines: Ototoxicity monitoring. Retrieved from https://audiology-web.s3.amazonaws.com/migrated/OtoMonGuidelines.pdf_539974c40999c1.58842217.pdf
American Academy of Audiology. (2013). American Academy of Audiology clinical practice guidelines: Pediatric amplification. Retrieved from https://audiology-web.s3.amazonaws.com/migrated/PediatricAmplificationGuidelines.pdf_539975b3e7e9f1.74471798.pdf
Jerger, J. F., & Hayes, D. (1976). The cross-check principle in pediatric audiometry. Archives of Otolaryngology, 102(10), 614-620.
Joint Committee on Infant Hearing. (2007). Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics, 120(4), 898-921. doi: 10.1542/peds.2007-2333.
Kreisman, B., Bevilacqua, E., Day, K., Kreisman, N., & Hall III, J.W. (2013). Preschool hearing screenings: A comparison of distortion product otoacoustic emission and pure-tone protocols. Journal of Educational Audiology, 19, 82-91.
Lyons, A., Kei, J., & Driscoll, C. (2004). Distortion product otoacoustic emissions in children at school entry: a comparison with pure-tone screening and tympanometry results. Journal of the American Academy of Audiology, 15(10), 702-715.
Stover, L., Gorga, M. P., Neely, S. T., & Montoya, D. (1996) Towards optimizing the clinical utility of distortion product otoacoustic emission measurement. Journal of the Acoustical Society of America, 100(2 Pt 1), 956-967.
Cite this Content as:
Hall, J.W.III. (2015, October). Evidence-based clinical applications of OAEs in children and adults. AudiologyOnline, Article 15471. Retrieved from https://www.audiologyonline.com.


