Learning Outcomes
After this course, learners will be able to:
- Explain the relationship between etiology and damage pattern in the peripheral auditory system.
- Describe how the role of nonlinear processing can be adapted to losses with a severe distortion component.
- Explain how fitting approaches may need to be modified in cases of asymmetrical hearing loss.
Introduction
Today, we are going to discuss some of those difficult cases that occur when there is an increased level of distortion in the auditory system. These types of cases are not typically covered in research or clinical literature. Hearing aid procedures developed over the years have been fine-tuned and honed for more standard fitting situations. When a clinician runs into cases where all the typical conditions are not met, those cases can be complicated. In addition, we will discuss the etiologies of more complex cases and provide some fitting tips about how to approach some of these more difficult situations.
What is a "Standard" Fitting?
In regards to this course, a standard or typical fitting involves patients with moderate or mild-to-moderate sensorineural hearing loss (SNHL). The shape of their audiogram is usually flat to gently sloping. Normally, these patients have symmetrical thresholds and symmetrical word recognition scores. In quiet, these patients seem to have pretty good word recognition as long as sounds are loud enough. They will have various amounts of trouble in noise, but nothing terribly dramatic. The status of the auditory system is relatively stable. Standard fittings are usually long-standing, slowly progressive hearing losses due to some combination of presbycusis, with a little bit of noise-induced loss. It may involve what is known as socioacoustics, which is related to living in a modern world. Those are the typical progressive situations that you see in a clinic. However, patients often show up in the clinic and do not meet all the criteria.
Assumptions When Fitting Hearing Aids
In part one, I laid out several assumptions that we use when following standard hearing aid fitting protocols and examining where some of them might not always be appropriate for particular cases. In this course today, I want to talk specifically about how the following five assumptions may not be fully met:
- Prescriptive, Not Adaptive
- Measurable Hearing is Usable Hearing
- Fine Tuning is a Movement Away from Optimal
- Both Ears Contribute (Equally)
- Two Monaural Fittings
Assumptions four and five will be very important when we discuss asymmetrical losses. When discussing Prescriptive, Not Adaptive and Fine Tuning we call into question the accuracy of fitting rationales for patients with a severe amount of distortion in their auditory system. Another issue underlying this discussion relates to the idea that just because you can establish a threshold in a patient, does not mean that frequency region in the auditory system is usable. We typically follow the course that if a threshold is established with measured or predictive UCLs, that you have a viable playing field. However, when you talk about distortion aspects of hearing loss, we need to question how good that playing field is.
Residual Capabilities
Another aspect that underlies this discussion is the notion of residual capabilities. As hearing care practitioners, we do not treat hearing loss. Instead, we treat residual hearing. The mindset that I have encouraged is we want to figure out how we can integrate technology into the remaining function that the patient has. Of course, that remaining hearing is not normal; it is changed. The sensitivity has changed and sounds have to be made intense in order to be audible for the patient. Additionally, the residual hearing might or might not be viable. In any case, we need to take into account the patient's residual capabilities and view the aided signal in relation to their remaining auditory abilities.
To use an analogy, we can look at modern prosthetic devices as compared to the more primitive peg leg. Peg legs simply compensate for what was lost, whereas modern prosthetic devices are designed to be fully integrated into the patient's remaining physiology (e.g., their bone structure, muscular structure, etc.). What's gone is gone, and we do not bring that back when we fit hearing aids. We do manipulate sound to work optimally with the remaining hearing that the patient has. This course is discussing how to obtain the most out of that remaining hearing.
Exception Discovery
One of the other principles that underline this three-part series is the idea of Exception Discovery. Exception discovery is knowing when you need to pivot away from the traditional approaches to fitting hearing aids. Those assumptions are logical for standard cases. However, when you run into extraordinary situations, you need to recognize when to approach the situation differently. This course is about using the principles of Exception Discovery and paying attention to when you might be required to think outside the box.
A and D Components of SNHL
Professor Reinier Plomp from the Netherlands wrote an important paper where he talked about the A and D components of sensorineural hearing loss. The A component is the attenuational aspect of hearing loss, meaning that sounds have to be more intense to be audible (Plomp, 1986). That is the component that we commonly think of regarding hearing loss. The aspect of hearing loss that we correct when using fitting rationales that are based on thresholds. The D component is the distortional aspect of hearing loss. The distortional aspect takes into account the remaining hearing. In other words, once sounds are above a threshold, how well does the auditory system take in that stimulation to properly code it so that the cognitive system can make use of it?
Most patients with sensorineural hearing loss are going to have some amount of distortion. Plomp (1986) discussed the functional way of measuring the D component by using signal-to-noise ratio testing. The distortional component in more fundamental terms as it relates to the quality of the remaining hearing. Yes, it is going to show up in terms of the ability to function in a noisy environment. Even more fundamentally, I believe it is more tied to the remaining physiology that the patient has. How intact is that remaining physiology? How well can that compromised ear take in a complex signal like speech, especially in a background of noise, and code it properly so that the brain can make use of it? The enhanced distortional aspect of sensorineural hearing loss will be the focus of the cases that I'll be talking about today. When something goes wrong in the ear that is beyond the typical, what do you do about it?
We normally talk about sensorineural hearing loss from the hair cell perspective. A mild hearing loss is usually the loss of some outer hair cells (that improve the sensitivity of the inner hair cells). Beyond a mild-to-moderate or a moderate hearing loss, then you are likely also dealing with compromised inner hair cells. A lot of the discussion is around the nature of sensorineural hearing loss and that is usually a hair cell analysis. It is a good way of understanding multi-channel nonlinear compression. The reality is that the peripheral auditory system is a very complex system. There are things that have to go right mechanically, neurally and electrochemically. All those parts must be working together in the right way in order for sound to be properly coded and sent up the eighth cranial nerve and to the auditory cortex. When examining these more traumatic, medically complex etiologies, we see different parts of the system that can break down. For example, in cases of meningitis, there may be bony growth within the inner ear that distorts the mechanical reaction. There might be an electrochemical imbalance of the endolymph and perilymph, such that the hair cells cannot fire within that electrochemical bath that they sit in. There may be improper connections between the hair cells and the nerve fibers. The cochlea may not be fully developed and fully formed into 3 1/2 turns. All those things that have to be right in order for the peripheral auditory system to work. When we talk about severe distortional aspects of hearing loss, these cases involve more than just hair cell loss. In such cases, there are usually additional changes, in terms of the way the peripheral auditory system functions.
Who Are We Talking About?
Physiologically, these patients may have Meniere's disease or some sort of structural failure within the inner ear. Also, the sudden or rapidly progressing hearing losses, which can leave a significant distortional aspect to the hearing loss, whether it is autoimmune, vascular or viral. Those three components together are usually behind the sudden or rapidly progressing hearing losses and end up leaving more damage to the auditory system beyond just changes in thresholds. We are also talking about some of those long-standing severe hearing loss cases, where the quality of the remaining function is poor and has always been poor.
Functionally, these patients usually have poor word recognition scores, even in quiet. You can have fluctuations or instabilities not only with Meniere's but also with other conditions. You often see asymmetries, located in the system. Sometimes, you are working with patients who have extremely reduced dynamic ranges, characteristic of Meniere's cases and other more atypical losses, resulting in less residual hearing with which to work.
Medically Complex SNHL
I often use the term medically complex sensorineural hearing loss to distinguish it from the more traditional presbycusic/noise-induced loss cases. Another term that can be used is severe distortional sensorineural hearing loss. Almost everyone with SNHL has some degree of distortional element. If that distortional element seems to be more dramatic in some patients, “severe distortional SNHL” is an accurate way of functionally describing what they are facing.
Variability among patients increases with greater degrees of hearing loss. These etiologies typically show more threshold-based loss, but that is not always the case. In general, increasing degrees of distortional aspects of hearing loss will also increase the variability from patient to patient. We like to follow a prescriptive approach when we fit hearing aids; but when you are dealing with patients with severe distortional loss, prescriptive approaches might not be successful. There's nothing wrong with starting with prescriptive targets for these patients. But I think it is important to have an attitude that this fitting is going to be more adaptive. Adjustments to the fitting are needed in order to make the best use of the remaining auditory abilities that that patient has. Those remaining abilities vary greatly from patient to patient.
Generally, the greater the damage, the more variable the damage. That is a pretty broad statement, but fairly accurate. When you talk about patients with mild hearing loss, the sort of changes that have occurred in the auditory system (e.g., outer hair cell loss) is pretty easy to predict and manage. However, when you start talking about some of the other changes (e.g., membrane disruptions, neural cell death, mechanical and metabolic disruptions and disrupted coordination), that is where the variability goes up, the damage becomes greater and the complication for doing something to fit the hearing aids becomes greater.
Case Examples
When I worked at the University of Iowa Medical Center in the ENT Department we would see many patients with medically complex hearing loss situations (e.g., Meniere's patients, sudden losses, etc.). The medical staff would do everything they could to restore the hearing or at least slow the process. As you know, in many cases there is nothing that can be done. The medical staff would often counsel patients that their hearing loss was going to remain the way it was, and then be referred for a hearing aid evaluation. I saw a large number of patients who fell into this category. Again, I was faced with situations where standard fitting approaches did not seem to be enough for these patients. There was so much change in their auditory system that something different had to be done. The medical center was also a cochlear implant center. You'll see some of the patient audiograms and you might think they would be an implant candidate. Many of these patients were eventually in line to become implant candidates. Since this was 20 years ago, perhaps today even more of them would become implant candidates. However, at the time, not all of them were implant candidates, nor did all of them want to get implants. They did certainly want to start with hearing aids as an approach, and I was put in the position to figure out how to work through a lot of these cases. We will walk through a few of these difficult cases.
Patient PH: A 52-year-old female with an unknown progressive loss that continued to decrease month after month. When we use the word "progressive" with most sensorineural hearing loss cases, we usually mean one that is slowly progressing over a number of years. When referring to medically complex cases, progressive can mean that a patient's hearing is declining rapidly (e.g., on a month-to-month basis). The medical staff will do what they can to stop or slow the progression (e.g., provide steroidal treatments). Ultimately, these patients are often left with some sort of permanent damage. Hopefully, the thresholds in the auditory system stabilize at some point in time but there will likely be some sort of damage to the system.
One aspect that is typical of patients with rapidly progressing hearing losses is the word recognition scores in quiet are even more depressed than the thresholds (Figure 1). In the case of Patient PH, she has a mild sloping to profound hearing loss. The word recognition scores in quiet are worse than you would expect based on those thresholds. In other words, if you made speech audible to the patient, there is no guarantee that they will perceive benefit from amplification.
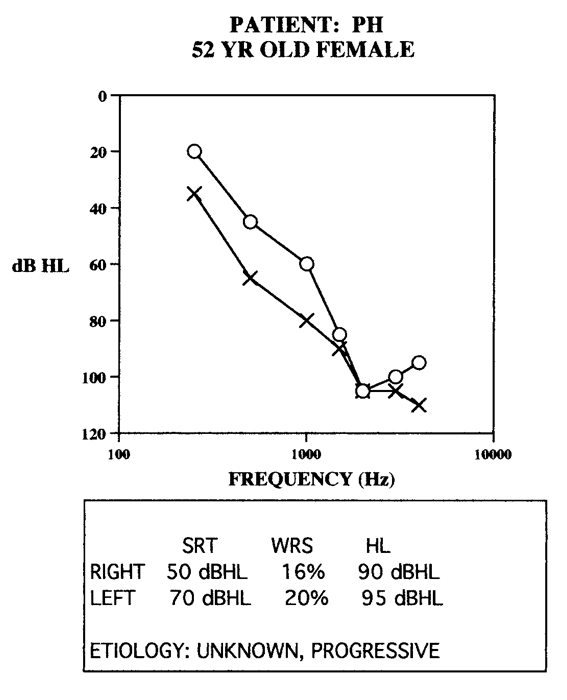
Figure 1. Case example: Patient PH.
Patient ST. A 45-year-old female with bilateral Meniere's disease (Figure 2). Based on the thresholds and word recognition scores, her right ear is more significantly affected than her left ear. During the time I worked with her, this patient's hearing remained stable, but that was no guarantee that it would remain this way. This patient had depressed word recognition scores in both ears, but it was more dramatic in the right ear. Patient ST wanted to use hearing aids in both ears, and she certainly was a candidate to use hearing aids in both ears. However, programming the hearing aids to address for her asymmetry took extra effort.
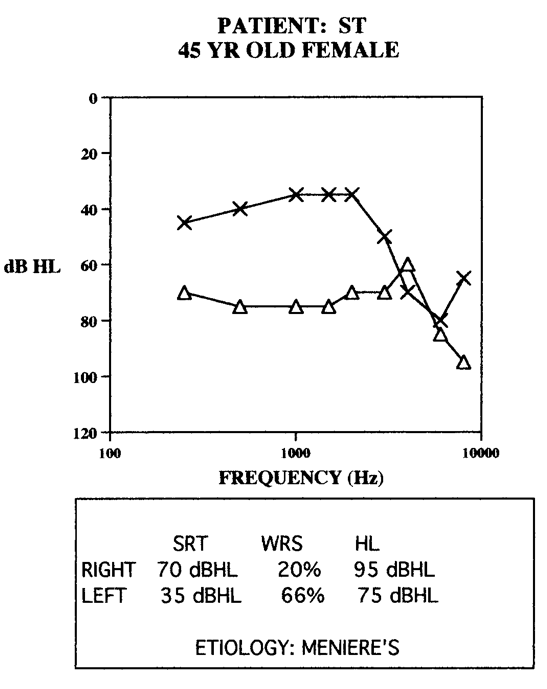
Figure 2. Case example: Patient ST.
Patient RS. A 68-year-old male (Figure 3) had an unknown progressive loss with depressed word recognition scores. Although his thresholds were steeply sloping, one thing to note is that he had relatively symmetrical hearing loss. This gentleman was lucky because his hearing was changing throughout the course that I was working with him. The hearing loss stabilized at this point in time. His physicians were not able to pinpoint the cause, which is often the case with these patients.
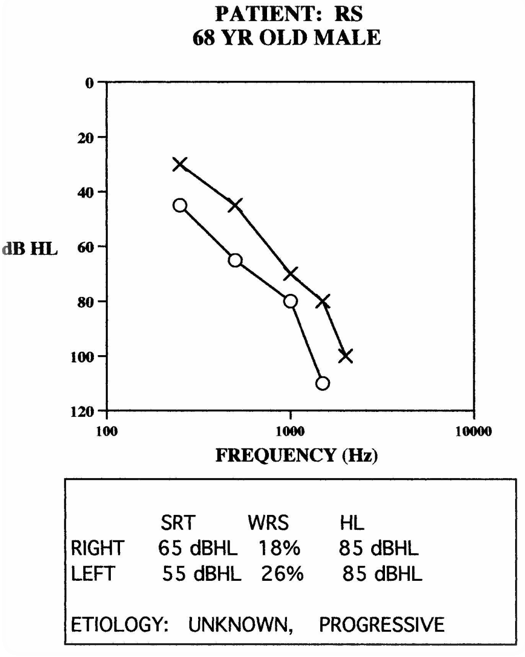
Figure 3. Case example: Patient RS.
Fitting Strategies Study
At the University of Iowa Medical Center, I conducted a fitting strategy study to learn how to deal with these types of patients. I gathered a group of 15 patients who had a variety of medically complex etiologies. The purpose of the study was to examine whether linear or nonlinear amplification provided benefit to these patients and whether they should use a full-bandwidth hearing aid or a more limited-bandwidth hearing aid. My working hypothesis was that different regions of their hearing did not work particularly well, and as such, we wanted to avoid those regions of hearing. I used both linear and nonlinear strategies with the subjects, and they were evaluated using a broad range of both objective and subjective evaluations. I did not know how they viewed the value of their hearing aid ahead of time, and so I wanted to try to capture outcome using different methods.
We performed band limited filtered speech testing with the subjects to see which frequency regions seemed to work better, and if there seemed to be some regions to avoid or not avoid. I anticipated that some of the subjects might have regions of hearing that were so distorted that you wanted to avoid them, but that did not seem to show up in any of the test cases. However, there were differences in comparing linear versus nonlinear approaches. The reason why linear versus nonlinear was an interesting question is that many of these patients have significant threshold loss. Typically, the thought may be that you need a power linear approach in order to make speech audible to the patient. As you know with these etiologies, their remaining hearing tends to be relatively sensitive. They are sensitive not only in terms of loudness perception but also sensitive in terms of being stable, non-fluctuating, as well as tolerance to sound. With these patients, I was interested in contrasting a strong, powerful, linear approach with more subtle, multi-channel nonlinear approaches.
Nine different approaches were evaluated in the study: five linear and four nonlinear (Figure 4). The nonlinear approaches were typically multi-channel nonlinear, although one of them was a little bit more of an output-limiting approach. This was a while ago (mid-1990s), and the way the nonlinear systems worked back then was a bit different than today. During that time period, we weren't sure if high threshold output limiting compression approaches seemed to be the way to go with patients, or if wide dynamic range, multi-channel approaches seemed to make more sense. I wanted to include one of the output-limiting approaches. The linear approaches were broadband, a rising response or a series of band-limited response based on the filtered speech testing performed. Again, the focus was to figure out what parts of the auditory system seemed to work best for the patients.
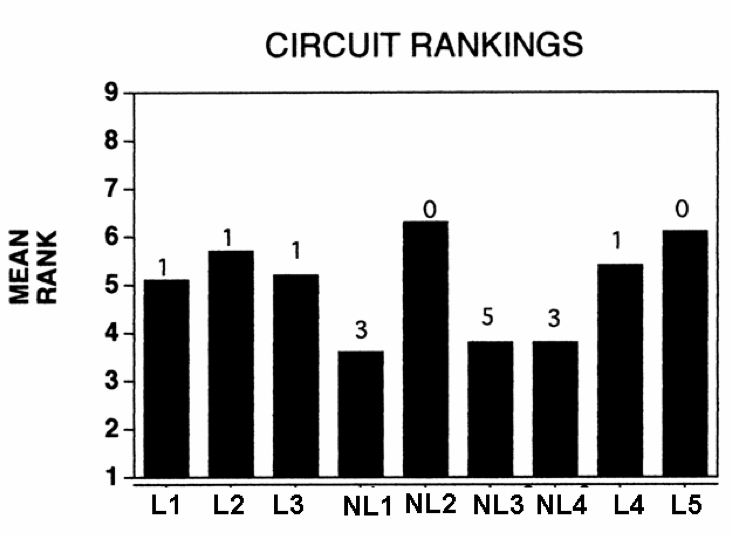
Figure 4. Circuit rankings.
The mean rank for each of the linear and nonlinear approaches across the patients are shown in Figure 4. As stated earlier, these patients were tested using a variety of different subjective and objective measures. The mean rank is across all nine measures, and also across the15 patients. A lower score is better. You can see that three of the nonlinear approaches (NL1, NL3, and NL4) scored significantly better than the other six approaches. The output-limiting compression and the five linear approaches performed statistically similarly or poorer than the three nonlinear approaches. The nonlinear approaches were three different versions of multi-channel nonlinear compression.
Each participant was fit with their own pair of hearing aids at the conclusion of the study. The numbers above each bar refer to the number of patients who took that circuit home as their final choice. Eleven of the 15 patients chose a multi-channel nonlinear as their take-home product. The remaining four patients each took home a linear approach. Overall, the results would suggest that a multi-channel nonlinear approach benefits most of these specialized cases. Remember that many of these patients had significant threshold loss and intuitively we lean towards fitting power linear approaches. Due to the sensitive and unstable nature of the hearing, there's significant distortion occurring. Fitting with a gentler approach with these patients may provide increased benefit.
Case Example: Patient PH. When Patient PH came in (refer back to Figure 1), she had a bilateral power linear fitting. She reported the left aid was useful but the right aid was a hindrance in any amount of competition. Throughout the project, she felt that the multi-channel nonlinear approach seemed to work best, which is the way I ended up fitting her bilaterally.
Coming into the project, her aided word recognition score was 34%. Her unaided word recognitions cores were 10% and 24%, in the left and right ears respectively. Even though the thresholds in her right ear were better, the hearing aid did not seem to provide as much benefit on the right ear versus the left ear. The right device was a high peak gain linear hearing aid. Again, we fit the high peak gain in a linear hearing aid to achieve those thresholds, especially in the low to mid frequencies.
After this project, Patient PH ended up being fit with a multi-channel nonlinear hearing aid. This was a less aggressive approach, especially for louder inputs and provides a broader, smoother response. The goal was to be subtler and gentler. She did significantly better with the WDRC approach versus the linear approach. Through working with this patient, it became very clear that for patients with medically complex losses, we often need to use a gentler hand.
Fitting Ideas: Medically Complex SNHL
Some fitting ideas to keep in mind when dealing with medically complex SNHL include:
Be careful with the gain. We need to recognize how much threshold loss there is and be sensitive to the fact that we are going to need gain in order to restore some audibility. Due to the significant hearing loss, we are not going to be able to restore as much audibility as we would like to in these patients.
Role for medically complex SNHL. There's probably a significant role for multi-channel nonlinear fitting approaches. Perhaps we need to back off our expectations of how much audibility the patient is going to receive. This is most important for soft to moderate inputs in order to make sure that we're not overdriving their hearing.
May need to "over-compress" or control dynamics. Normally, most audiologists are very careful about using too much compression. However, when dealing with more complex cases (e.g., Meniere's, progressive HL), we might need to use more fast-acting compression then we are used to because the inner ear may be more sensitive to a highly dynamic signal. This goes against the trend that we're seeing in our field which is to use short-term linear approaches or slow-acting compression. Oftentimes, clinicians use compression approaches that allow the full dynamics of the speech signal to come through. For these patients, there may be situations where it is appropriate to provide more compression than we are typically used to.
More adaptive than typical losses. Without a doubt, these fittings become more adaptive. We just have to spend time with these patients to try to find which works best for them.
Environmental control. Due to the amount of distortion that they have in their hearing loss, these patients are thrown by any amount of competition. As such, we need to make sure we're trying to use the very best environmental control (e.g., noise reduction, directionality) that we possibly can in the hearing aids.
Asymmetrical SNHL
Next, I want to discuss a specific subset of these patients: those with asymmetrical hearing loss. Hearing loss where each side of the auditory system works differently. This could present as asymmetry in thresholds or speech recognition abilities in noise and quiet. These patients have one better ear and the other is not working as well. When asymmetries exist in the peripheral auditory system, the goal is to figure out how to create a single unified sound perception. Often, this means wearing hearing aids in two different ears but finding a way to blend those hearing aids to work well together. This part of the lecture will share strategies that might be helpful when working with the auditory system to work together.
Types of Asymmetries
There are three types of asymmetries:
- One ear normal, the other aidable
- One ear dead, the other aidable
- Both ears aidable, one ear is better
One normal, one aidable. To illustrate this case, let's look at an example (Figure 5). Here's a person with Meniere's disease in the right ear, and normal hearing in the left ear. Patient AM has poor word recognition in the right ear. The dilemma is, can you fit a hearing aid on the right ear that won't compete with the normal hearing on the left ear? Remember the goal is to provide one single unified perception of sound that is taking components from both sides of the head. However, considering the amount of distortion in the right ear, how do we provide amplification without competing with the normal ear? In the case of patient AM, she appreciated access to sound on her right side but had realistic expectations she was not going to rely on her poor ear for speech understanding. It was more the idea of exposing the patient to the world of sound coming from that side of the environment. Depending on how much distortion occurs on the poor side, will drive whether or not that ear becomes a communication ear or more of a sensitivity/awareness ear.
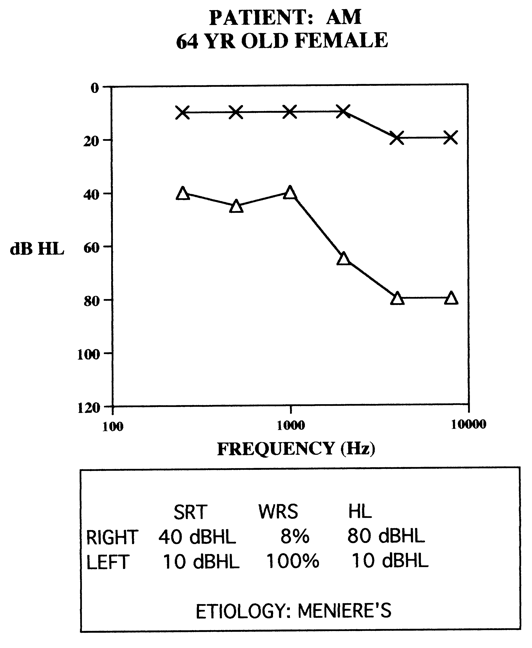
Figure 5. Case example: Patient AM.
One dead, one aidable. For a person who has one dead ear and one aidable ear, for the most part, they will be a one-sided listener. A BiCROS set-up will provide access to sound on the dead side. However, everything will be processed by the aidable ear. It is unfortunate that these individuals only have one ear, but in some ways, it uncomplicates the situation because you simply need to focus on the one aidable ear.
A Word of Caution. Feldman and Oviatt (1993) worked with a patient whose left ear had a sloping hearing loss with reasonably good word recognition scores, given the shape of the audiogram. The patient's right ear had a severe flat hearing loss, with no measurable word recognition at any level. This patient wore a hearing aid on just the left ear, or a BiCROS hearing aid. He was never given the opportunity to try anything on the right ear. Feldman and Oviatt felt that it was worth attempting a fitting on the right ear for that patient. They turned up the hearing aid on the left ear and then fit a hearing aid onto the right ear and gave the patient an opportunity to adapt to the hearing aid for a while.
In Figure 6, the graph shows the aided results for both listening situations with the left ear only, and hearing aids bilaterally. You can see a significant improvement, especially in noise, when going from a monaural to a binaural fitting. Again, that right ear had no measurable word recognition ability in quiet, and, for a lot of clinicians, would normally be considered to be an unusable ear. Then you see these aided results when fitting the poor ear.
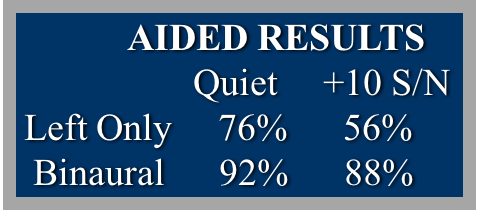
Figure 6. Aided results for Feldman and Oviatt subject (1993).
Again, it only takes one or two cases like this to understand that you do not know how the person's going to use aided sound, even on a severely compromised ear. In this case, somehow the cognitive system was able to merge the amplified sound from both ears to achieve a better signal. It does not always turn out this way, but once you see a case like this, it reminds you that you can't rule out the idea of trying hearing aids on an ear that is deemed "unaidable".
Both ears aidable, one better. This is a situation where the focus is on how you go about fitting these aids so that you can get a significant benefit for the patient overall.
Fitting Ideas: Asymmetrical
Some fitting ideas to keep in mind when dealing with asymmetrical SNHL include:
Do not say "no" until you know. The only way you know that an ear cannot benefit from amplification is when you try to fit a hearing aid on that ear. There is no justification for predicting that an ear cannot use amplification. It only requires a little bit of time investment by you and the patient.
Aim for a fused, binaural image. Even though you have asymmetries, with two ears that are working at different levels, the whole idea is to merge those two ears to work together in an effective way.
Targets are a place to start. However, do not be surprised if you end up using less gain in the poorer ear. Often, the ear that is working better is the ear that is going to be doing the heavy lifting, as far as communication goes. The idea is to incorporate the poorer ear, but not compete with the better ear. Frequently, you'll end up backing down the gain on the poorer ear, and your temptation is to drive the gain up. The problem with that is, as you increase the gain, you also have the potential to increase audible distortion in that ear. Although targets are a reasonable place to start, through the adapter process, you might end up finding that you have to back off in order to get that fused auditory image that the patient is seeking.
Consider serial monaural fittings. Although you may target a patient with a bilateral asymmetrical hearing loss as being a patient who can wear hearing aids in both ears that does not necessarily mean that you have to fit both hearing aids at the same time. When we fit hearing aids, it is assumed that we should fit them both at the same time. However, it is important to remember that a lot of these patients have one ear that works better than the other. Somehow, you are trying to get them to use both ears together. What can sometimes happen is that if you try to fit both hearing aids at the same time, you can create confusion: Confusion about which ear is hearing what, and which ear needs adjustments, and how the whole thing is coming together. Consider a situation where you target the better ear first. You know you are going to put a hearing aid on that ear. The better ear is probably going to do the heavy lifting for the patient. Once you are certain that the hearing aid is successful (after one or two weeks), then amplify the second ear. When you add that hearing aid to the second ear, what you are trying to accomplish is having that ear contribute and be part of the fitting, but never to the point where it is competing with the better functioning ear. You may not utilize as much gain in the secondary ear, because you already have a successful fitting in the better ear. This case is not viewed as a traditional binaural fitting; rather should be considered as two monaural fittings leading to a binaural result.
Let's take a look at cases where patients were successfully fit using a serial manner. A 72-year-old female (Figure 7) with an unknown etiology has never been fit with hearing aids. We approached the left ear first. After a successful fitting, then amplified the right ear. This patient ended up being an excellent binaural user. Both ears performed well, even though the patient needed a more positive signal to noise ratio on the right ear than the left ear. This was not surprising, as the distortion component was worse on the right ear than the left ear. This patient easily adapted to two hearing aids.
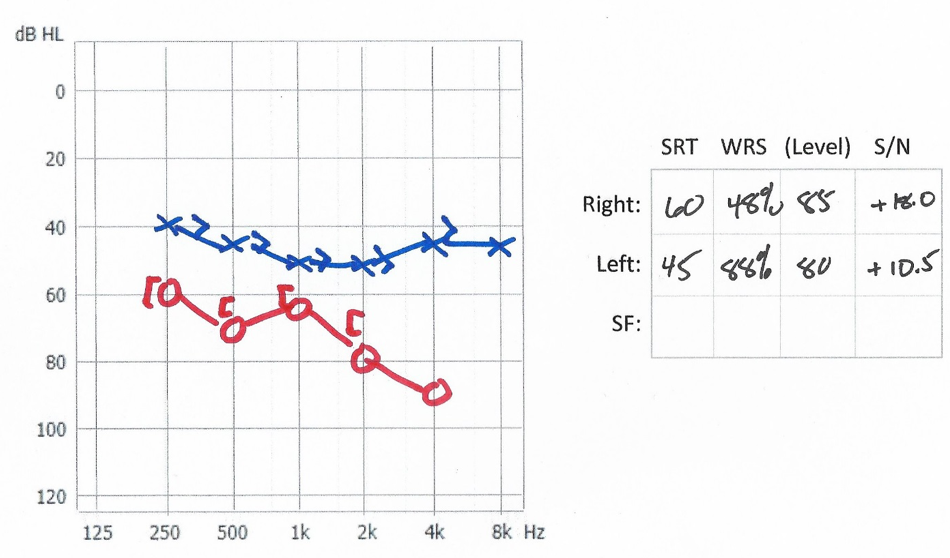
Figure 7. 72-year-old female.
In a second case, a 42-year-old female (Figure 8) with bilateral Meniere's had a significant difference between the two ears. Word recognition scores in both ears were depressed. We couldn't establish a signal to noise ratio level in the left ear. This patient did end up wearing two hearing aids because we were able to work with this patient to provide perceived benefit from both ears.
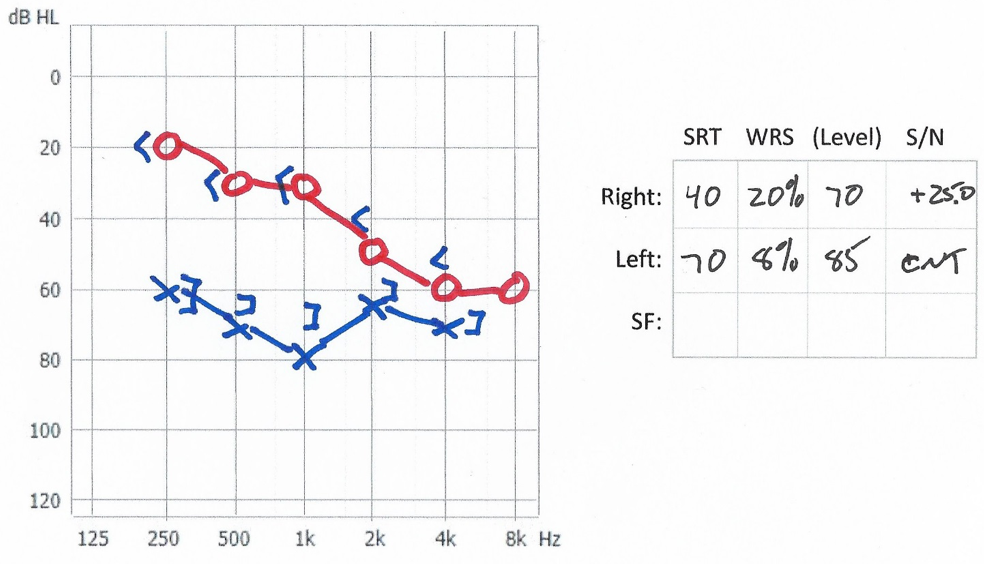
Figure 8. 42-year-old female.
Case #3: 68-year-old male (Figure 9) with a sudden sensorineural hearing loss six months earlier, and has stabilized in the past four months. No measurable word recognition in the right ear. This patient ended up wearing a hearing aid in the left ear. He was a part-time user of the hearing aid on the right ear, more for awareness than anything else. He felt amplification was valuable and he wanted to keep the hearing aid for his right ear.
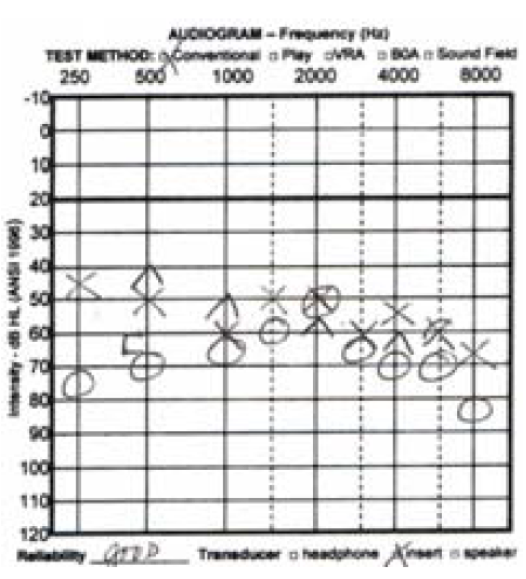
Figure 9. 68-year-old male.
Case #4: 79-year-old female (Figure 10) with a rapidly, progressive hearing loss which occurred nine months earlier, and stabilized for two months. I worked with this patient a significant amount as she had trouble adjusting to amplification. She started by wearing hearing aids bilaterally. But I wasn't sure that she was benefitting from the amplification on the left ear all that well. By stepping back and using the approach of serial monaural, I was able to fit the right ear first. I then added the left ear in a way that did not compete with the right ear.
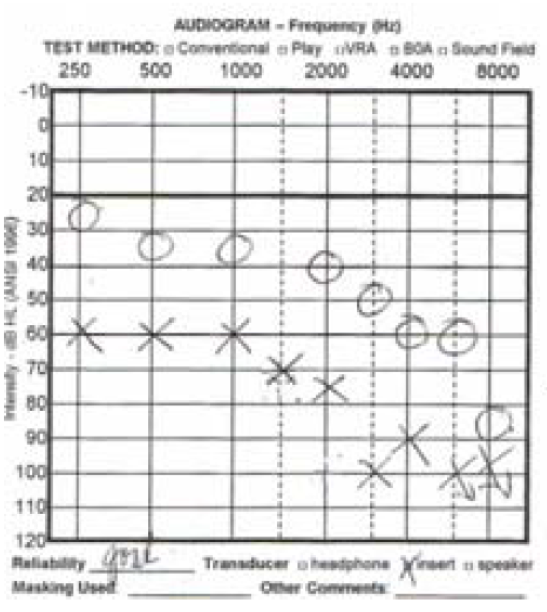
Figure 10. 79-year-old female.
Severe SNHL
In this section, we are talking about patients with long-standing hearing losses, perhaps congenital or developed during childhood, and who did not end up with a cochlear implant and thus still require amplification. Perhaps they did not receive an implant due to a medical condition, or by personal choice. As the severity of hearing loss increases so does the variability and distortion. Lamore, Verweij and Brocaar (1990) collected data in terms of word recognition in quiet as a function of average hearing loss at the frequencies 0.5, 1, and 2 kHz. They found that up to about 50-60 dB of hearing loss, the average word recognition in quiet is still pretty good. There's not a wide, wide range of variability for patients. However, once you pass about 60 or 70 dB hearing loss, the average word recognition score in quiet starts to drop dramatically, but then you also start to see a lot of variabilities. You have some patients who can still do very well for speech understanding in quiet, but you also have some who do very poorly with speech understanding in quiet.
Davies-Venn, Souza, Brennan and Stecker (2009) collected similar data for speech in noise by conducting a QuickSIN test on patients to measure their ability to hear in noise. With QuickSIN, lower scores are better. Patients in the mild-to-moderate range have a relatively limited range from patient to patient. Once you get up into the severe hearing loss category, there is a much greater range of auditory ability. For some of these patients with severe loss, the distortion aspect of their hearing loss is similar to patients with mild-to-moderate loss; but in general, the grouping tends to be much more significant signal to noise ratio losses.
Why Do We Use Compression?
One of the dilemmas about dealing with severe hearing loss is whether or not to use nonlinear with these patients. Over the last 10 years, it has become very clear that nonlinear has a place in the treatment of severe hearing loss, whereas back in the day, that notion wasn't necessarily well accepted. In the past, the focus was on using fast-acting compression, but patients did not necessarily respond well to that. Now, we're seeing improved uses of compression with a severe hearing loss.
I want to give you an idea of the compression trade-off because we do not necessarily use compression to make speech more intelligible. A compressed speech signal is never more intelligible than an uncompressed speech signal, but we use compression to make the speech signal fit in the remaining dynamic range of the patient. Often, we assume that if we could fit the speech spectrum into the remaining dynamic range of the patient, the better off the patient will be, but that is not always the case.
De Gennaro, Braida, and Durlach (1986) applied four different fast-acting compression techniques to a speech signal for a group of patients with a severe sensorineural hearing loss in hopes to fit the speech into the remaining dynamic range of the patient. What they found for some patients was no significant improvement as you force more and more of the speech spectrum into the remaining dynamic range of the patient. This shows us that compression-audibility trade-off, in order to get more of that speech spectrum audible to the patient, you have to use a lot of fast-acting compression, and some patients cannot utilize that signal very well.
Some patients with severe hearing loss can use a compressed signal pretty well, but not all of them can. The take away about severe hearing loss is to be careful about how much compression you use. Earlier, when discussing unstable losses, I talked about the idea that you might need to over-compress the signal just to make sure that it is tolerable to the patient. In regards to severe hearing loss patients where loudness sensitivity does not seem to be an issue anymore, then be cognizant about how much compression you add to the signal. Ultimately, you might be detracting from their ability to extract information.
Fitting Ideas: Severe SNHL
In general, follow these guidelines when dealing with long-standing severe hearing loss patients:
Multi-channel nonlinear advantages. You might want to use more of a power multi-channel approach, and that usually means that you want to be careful about the amount of compression you use. Play with the knee points and ensure that you are not compressing the signal so much that they can't get any information for it.
Linear approach. Sometimes these patients are more classic, where they need just a linear response. Patients might prefer more of a low-to-mid frequency linear response.
Explore the dynamic range. If they have a limit to their dynamic range, check to see if you can adjust for this as well. You might find that they really do not have a tolerance issue at all.
Consider "manual override" thinking. These days, hearing aids fit to severe hearing losses have volume controls. If the patient has issues with audibility but sensitive to compression, by using a manual override approach, you are telling the patient to use the prescribed settings for the fittings for moderate speech. If they need to hear the soft speech, they can simply turn up the volume. Patients typically have no problems following that approach to managing their own hearing.
Conclusion
This course and series encourages hearing care professionals to think about fitting atypical losses from a different perspective. Fit the patient with amplification by thinking about their residual capabilities. Consider how to manipulate sound so that the patient can get the most out of the aided signal with their remaining hearing. You cannot restore their hearing to normal again. Hopefully, you have a few more tools to use when you are dealing with patients who challenge our conventional notions of how we fit hearing aids.
References
Davies-Venn, E., Souza, P., Brennan, M., & Stecker, G.C. (2009). Effects of audibility and multichannel wide dynamic range compression on consonant recognition for listeners with a severe hearing loss. Ear and Hearing, 30(5), 494.
De Gennaro, S., Braida, L.D., & Durlach, N.I. (1986). Multichannel syllabic compression for severely impaired listeners. Journal of Rehabilitation Research and Development, 23(1), 17-24.
Feldman, A. & Oviatt, D. (1993). Bicros or binaural: a case study. Seminars in Hearing, 14(3), 229-233.
Lamore, P.J., Verweij, C., & Brocaar, M.P. (1990). Residual hearing capacity of severely hearing-impaired subjects. Acta Otolaryngologica, Supplement, 469, 7-15.
Plomp, R. (1986). A signal-to-noise ratio model for the speech-reception threshold of the hearing impaired. Journal of Speech and Hearing Research, 29(2), 146-154.
Schum, D. & Beck, D. (2006). March 2006. Alternative fitting approaches for special populations. News From Oticon, available from Oticon.
Schum, D. (1995). Amplification options for severe distortional hearing loss. Final report to the U.S. Department of Education.
Citation
Schum, D. (2018, April). Complex versus standard fittings: part 3. AudiologyOnline, Article 21997. Retrieved from https://www.audiologyonline.com


