Learning Outcomes
After this course learners will be able to:
- Describe the concept of Exception Discovery and how it can lead to alternative treatment strategies.
- Explain how fitting remaining hearing as opposed to hearing loss may improve benefit with ski-slope, rising and irregular audiograms.
- Explain which factors other than audibility may affect the response to amplification for patients with atypical audiogram shapes.
Introduction
This is the second of a three-part series on fitting hearing aids in complex versus standard situations. Each webinar builds upon the next, so if this is the first one you're dialing into, you might consider stepping back and doing part one. However, if you want to dive in now, I'll provide enough background material to ensure this should be a useful session for you.
The purpose of this series is to give you new ways to approach fitting cases that are more challenging and less common than you might be used to. Hopefully, by going through this material, you'll end up in a place where you might have some better ideas about how to tackle trickier fitting scenarios.
Over the years, the rules that we've set up to fit hearing aids have been based on more standard situations that are seen in the clinic. For example:
- Patients with mild-to-moderate hearing losses, gently sloping losses, or flat but gently sloping
- Patients with symmetrical hearing (i.e., no asymmetries)
- Patients with reasonable dynamic ranges to work with
- Patients with etiologies such as presbycusis, with a little bit of other things mixed in
These types of hearing losses are typically used when setting up clinical procedures in our field. However, most clinicians spend a significant amount of their time working with patients who don't necessarily fit those neat criteria. We put this series together in order to deal with these complex cases that do not fit into the "standard" scenarios, where some of our approaches that we would use on typical fitting might not necessarily apply.
It is important to note that not much research exists on these complex fitting situations. As such, I acknowledge that the recommendations made in this series of presentations might feel a bit thin, in terms of solid clinical data. Many of the ideas and conclusions that you'll hear over the course of this series are based on some amount of data and insight, in addition to a certain amount of speculation. Without a doubt, these are not the most verified or research-backed recommendations; but in a vacuum, at least it's a way to start thinking about treating some of those losses.
Exception Discovery
In a busy clinical field like audiology and hearing aid fitting, clinicians often don't have a lot of time to reinvent the wheel whenever a patient walks in the door. As clinicians, we like to believe that we treat every patient with the same amount of insight and clinical knowledge as we possibly can. The reality is that in a busy practice, we often end up using generalizations or heuristics about how we treat typical conditions. If a child presents with a middle ear problem, or any other relatively common medical condition, we usually recommend standard, by-the-book, well-proven treatment approaches, because that's the most efficient way of doing things. If treatments have stood the test of time and have proven to be effective, if a patient meets those criteria, we will likely use those treatments.
When fitting a patient, clinicians need to be ever mindful of paying attention to clues and characteristics where they might need to take a step back and think the situation through a bit more. It may be that the standard approaches, or the typical way of dealing with conditions might not be sufficient for this particular patient. Exception Discovery involves being efficient in applying standard approaches when it makes sense, but always being aware of less common characteristics that might lead you down a different path. Hopefully, as we work through individual conditions that I'll be presenting, this idea of Exception Discovery will become clear to you.
Some examples of hearing conditions that you may need to think about differently include:
- Patients who have poor word recognition scores, even in quiet
- Patients with significant asymmetries in their hearing
- Patients whose hearing loss is unstable
- Patients with severe threshold losses, where complications might be deeper
Today, in part two of this series, we're going to deal with three types of audiograms that might challenge the way we normally think about fitting a hearing loss (Figure 1):
- Steeply sloping losses (i.e., ski-slope losses)
- Rising sensorineural hearing loss
- Irregular shaped losses (e.g., cookie bites, W losses, V losses, U losses, etc.)
1.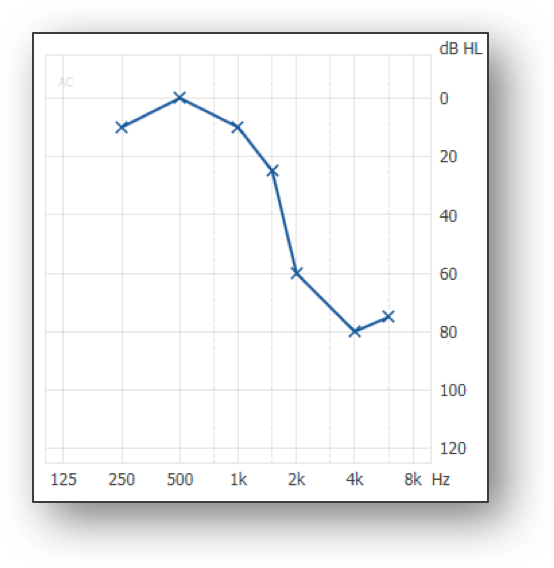 2.
2. 3.
3.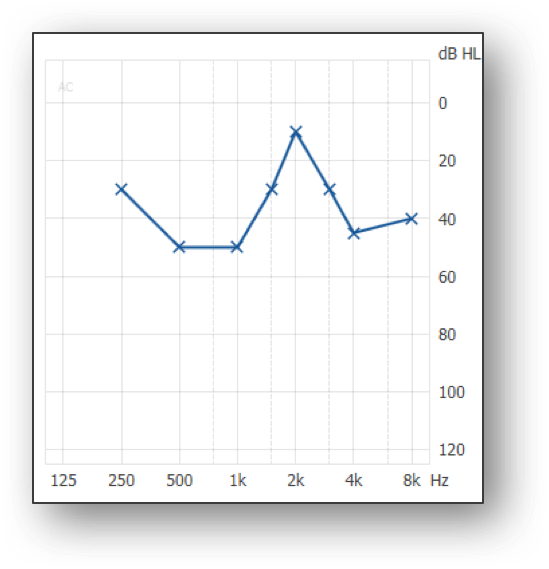
Figure 1. Three types of audiograms that can challenge how to approach a fitting.
Assumptions When Fitting Hearing Aids
In part one of this series, I laid out the assumptions that we typically use when we go through a standard hearing aid fitting process. For the purposes of today's session, I will focus on a few of these assumptions and challenge some of these notions in relation to the audiograms I just showed you. The assumptions that are particularly relevant for today's session are:
- Restore Audibility
- Correct for Threshold Loss
- Measurable Hearing is Usable Hearing
- More Bandwidth, the Better
These assumptions exist because they work well. However, Exception Discovery the concept is that there are conditions that would cause one to rethink some of these assumptions.
Residual Capabilities
I introduced the concept of residual capabilities in part one of this series. The idea with residual capabilities is that we don't fit hearing loss. The hearing that the patient has when they walk into office is the hearing they have when they walk out. We don't fundamentally change the way the person's hearing mechanism works. We manipulate sound so that the patient can get the most use out of that sound, whatever remaining hearing the patient has.
In a classic, gently sloping loss (Figure 2), you have thresholds, you have UCLs that you either measured or predicted, and you have an amplified speech spectrum that falls nicely within the patient's dynamic range. For the most part, things should be fine for a patient like that, assuming that the patient has relatively stable symmetrical hearing between the ears, reasonably good word recognition in quiet, and there are no other complicating conditions. In that case, a broadband with fully audible, amplified, moderate speech spectrum should be useful for the patient and you would expect success. The problem is that these conditions don't apply in every case. This whole series is about those situations where something else might be going on.
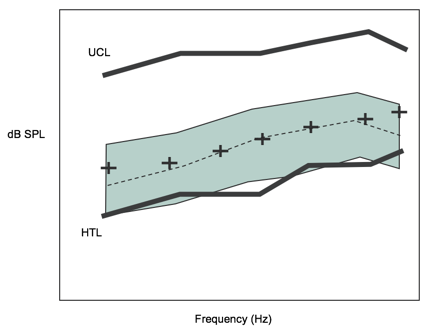
Figure 2. Audiogram of gently sloping loss.
Remember, although we measure audiograms, we're talking about a disordered physiology. We know what the auditory system does when it's healthy and intact and working well. We also know that the vast majority of hearing aids are fit to patients with sensorineural hearing loss. By definition, sensorineural hearing loss means that there is some damage or disorder somewhere in the auditory system. Very commonly, it involves hair cell loss, to some degree, outer hair cell loss, possibly some inner hair cell loss, damage disruptions. We need to keep in mind that if we are going to amplify sound and put it in the patient's auditory system, how much can we expect the damaged system to make use of that sound? Like I said, in more typical hearing loss cases (e.g. flat to gently sloping, mild-to-moderate, moderate), we expect that auditory system to still be able to use amplified sound. The goal in those losses is to get a clear and audible speech signal. When you start dealing with some of the more complex conditions, the ability of the damaged system to use an amplified signal might be more compromised. When that's the case, where do you turn? What do you think of next?
Ski-Slope Losses
Let us disucss how we approach ski-slope losses. Back in the 1960s and '70s, people with ski-slope losses were not fit with hearing aids. At that time, hearing aids had very limited bandwidth. We didn't fit all patients with ski-slope losses, because the hearing aids did not provide the patient enough benefit. In the late '70s, researchers began studies to determine whether or not patients with ski-slope losses could benefit from hearing aids if the devices had enough bandwidth. Much of this work was done by the late Margo Skinner at CID in St. Louis. Her basic conclusion was that if we had hearing aids with enough bandwidth, we could fit ski-slope losses. More importantly, she pointed out that it's not simply a matter of restoring audibility; that amplifying complex cases needs to be approached in a subtler manner. After Skinner's work, subsequent research was conducted by Turner and Hogan. Additionally, Brian Moore and others studied dead zones. Collectively, the work done by these researchers put the focus on the quality of the patient's remaining hearing.
Skinner wanted to draw attention to the fact that just because you measure an audiogram does not mean that the hearing is useful to the patient. Ski-slope losses are particularly interesting losses to analyze, because you have a region of normal thresholds and you have a region of very poor thresholds. In other words, there is a region within the inner ear with relatively intact mechanisms, and then you have part of the cochlea where the hair cell damage is extensive and complicated. To think that you can solve the problem by stimulating the remaining hair cells in the high frequencies is a simplistic approach.
Skinner had some interesting observations about how ski-slope losses should be approached. For example, if you try to amplify and restore audibility up in the high frequencies, sometimes it might help patients; other times, it can lead to situations where you're just making it harder for the patient to hear, because the damage is so great that the patients can't make any use of that information. The problem is once you start adding distortion into the patient's auditory experience, it complicates how well they perceive sounds in the parts of their auditory system that are working well. You can make things harder for the patient by trying to over-restore audibility in the high frequencies.
In Skinner's study, she provided each patient with a variety of different aided speech spectrums, to maximize the use of the dynamic ranges as best as she could, given the equipment limitations of the late 1970s. She used high frequency consonant test material to see how much potential there was for the patient to use high frequency information.
For example, one subject scored 54% correct on the high frequency weighted test. Skinner then modified how much gain she gave in the low, mid and high frequencies to see how it would affect the patient's scores. As the amount of high frequency audibility increased, the patient's consonant recognition scores decreased. In other words, trying to over-correct for the hearing loss made things harder for the patient, because the quality of that remaining hearing was such that the patient couldn't make use of it. In fact, it was probably detracting from the ability of the patient to understand what was being spoken.
Not all patients in Skinner's study reacted the same way. Some patients did fine with the restored audibility, but several of them had a similar reaction where if the high frequencies were driven too hard, things became more difficult. Subsequent work in the 1990s (by Turner, Hogan and others) was able to replicate the same sort of effect for patients with these ski-slope losses. In short, there is no one-size-fits-all solution for patients with ski-slope losses. For some patients, the remaining hearing is good enough to make use of amplified signals; for other patients, it's a little bit more difficult.
Although our focus with ski-slope losses is often in the very high frequencies, Skinner emphasized how important it was to pay attention to what's going on in the mid-frequency transition region. If patients still have usable hearing in that mid-frequency transition region, that might be where they are receiving their speech understanding. Typically, these patients have already acquired speech and language skills before they developed the ski-slope loss. Because understanding isolated words is not the same thing as understanding ongoing conversation, perhaps hearing better in that mid-frequency transition region is adequate to help patients do the task. Skinner's work reminds us not to overemphasize the highs, and to pay attention to what's going on in the low- and mid-frequencies, because that might be exactly where the patient has learned to use their hearing. Again, this leads back to the notion of residual capabilities. The patient is going to use whatever hearing they have left, and so we want to make sure that we are maximizing the hearing that the patient brings to the task.
Dead Zones
One of the discussions that has occurred in the hearing industry over the last 10 years has been on the topic of dead zones. Specifically, once you get above a moderate to severe hearing loss in the high frequencies, how viable is the patient's remaining hearing? For example, think about Brian Moore's TEN test, used for detecting the presence of dead zones and defining their limits. As a result, much of the dead zone work over the last 10 years have concluded that it's not so much whether or not the region is usable or unusable; rather that there are a lot of gray areas. How usable the high frequencies are varies from patient to patient.
Previous work that was done at the University of Memphis, the TEN test does not necessarily predict how usable high frequency information is to a patient. If you have a result on the TEN test suggesting that a patient has dead regions and the hearing is unusable, it would seem logical that applying amplification up there would be of no use to the patient. However, the data hasn't quite ruled that out. There are cases where patients have a TEN test result to suggest they cannot utilize the high frequencies, but for some reason, they are able to use it with hearing aids. There have been cases of the opposite, where TEN test results show that high frequencies should be usable. However, when a patient is provided a high frequency hearing aid, they aren't necessarily able to benefit from the information. As it currently stands, we don't know how viable the hearing is for a patient unless we attempt a fitting, which is not as black and white as a lot of people would hope it would be.
When you talk about ski-slope fittings, it's important to know the patient. In other words, where does this patient come from? What's their experience? With ski-slope fittings, you're typically talking about patients with some amount of noise-induced loss, possibly recreational (e.g., listening to loud music, riding a motorcycle) or industrial (e.g., factory or construction work). Due to the circumstances of their hearing loss, patients tend to be a little bit younger than typical patients who lose their hearing due to age-related effects. Because of the normal thresholds in the low to mid frequencies, patients with ski-slope losses hear a lot of sound. In quiet, they probably get along well-enough because of the redundancy of speech. They could most likely follow ongoing conversation in quiet without struggling too much. They probably start to struggle more when in noisier environments.
Goals of Ski-Slope Fitting
When fitting a ski-slope patient, you have to understand where they are coming from and what they might be thinking about, in terms of their hearing. These are the main goals for fitting patients with ski-slope loss:
- Maintain comfort
- Maintain acceptable sound quality in quiet
- No dramatic frequency responses
- Vented fitting
- Modest audibility enhancement focused on transition region
- Will be appreciated in quiet
- May be quite helpful in noise
As the first goal, it's important to maintain comfort, as well as maintaining acceptable sound quality in quiet. These patients can get along without hearing aids well enough in quiet that they often believe they don't need hearing aids. They may wait 10 to 20 years before they think about pursuing hearing aids. If they do come in to your clinic for hearing aids, make sure to avoid fitting them with a hearing aid that is unnatural or uncomfortable for them. Before feedback cancellation became available in hearing aids, we used to fit these patients with closed ear molds, with BTEs, with high gain in the high frequencies. As a result, they were fighting feedback all the time, creating a lot of occlusion, which is worse when you have usable hearing in the low frequencies. When we create an unnatural, uncomfortable fitting for these patients, it becomes easy for them to reject their hearing aids.
At Oticon, for the last 20 years we have been using an approach where we focus on a modest audibility enhancement in the mid-frequency region. We want to focus on the transition region of the patient's hearing, the area of the audiograms that Margo Skinner pointed out as being important. This allows us to provide an open fitting. This also allows the patient to have natural sound quality, because they're not running into occlusion. By not using an aggressive approach in the very high frequencies, we are maintaining a better sound quality out of the hearing aid, but it still might be enough to allow them to feel like they're doing better in noisy situations than without hearing aids. It's a gentler hand approach fitting these patients. Often, when we present this idea to clinicians, they feel that we are not being aggressive enough in the high frequencies. If we're not going after a full bandwidth speech signal, their view is that we might not be doing enough for these patients. Remember that ski-slope loss patients are typically adults with acquired hearing losses. They have fully acquired speech and language abilities. When you start thinking about how important high frequencies are for adults, they're not going to be as dependent on the very high frequency parts of the speech spectrum, as perhaps a child learning speech and language, within the auditory system. They've learned to compensate, they've learned to use other speech cues, and they've learned that in ongoing conversation, you don't necessarily need the far end of the speech spectrum.
Let me put this in a different perspective. Figure 3 shows a typical ski-slope loss between 1000 to 3000 Hz. The hearing loss drops off significantly. As stated earlier, with ski-slope losses, you have normal hearing in the low frequencies and significant hearing loss in the high frequencies. However, one of the things that we often forget in audiology is that you also have this transition region (indicated by the shaded area). In this situation, you have this region where the hearing loss is dropping but has not totally bottomed out yet. That typically can be an octave or wider in most losses. I'm not talking about the true cliff audiograms that would occur in some of the ototoxic events. I'm talking about the typical ski-slope losses that are secondary to noise-induced hearing loss.
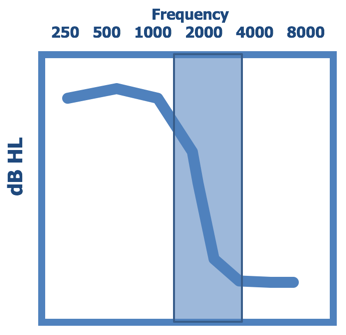
Figure 3. Ski-slope loss.
Figure 4 shows the Speech Importance Function generated from the Articulation Index, or the Speech Intelligibility Index. The dark blue background is the relative importance of the different frequency regions of the speech spectrum. Not all speech has equal importance. The region from 1500 Hz to about 3000 or 4000 Hz is the frequency region containing the most important parts of the speech spectrum. In this graphic, I've overlaid the frequency regions where the different acoustic cues that differentiate specific phonemes can be found. For example, the plosive bursts that would differentiate P, T, and K fall somewhere from 1500 Hz out to 4000 Hz. It is the same with the affricate bursts. With F2 transitions (going from a consonant to a vowel or the vowel to a consonant), we know that the second transitions could be an important speech cue (from 1000 out to 4000 Hz). If you take a look at the speech spectrum and the importance of the different parts of the speech spectrum in this way, and then overlay that transition region for the typical ski-slope losses (the light blue shaded area), you can see something very interesting. If you focus in at 2000 Hz and go a half octave above or below from 2000 Hz, you capture different classes of phonemic differentiations that occur in the speech signal. In other words, if you have hearing around 2000 Hz, there are different things that are happening in that active region. Many different contrasts in speech occur right in that region. When you talk about having a modest audibility enhancement in the mid-frequencies or the transition region, you see that modest audibility enhancement can bring a lot of information along with it. What we have found to be very successful in fitting ski-slope loss is that a modest enhancement often is enough to bring in the information that patients need to feel like they're hearing better in those difficult listening situations.
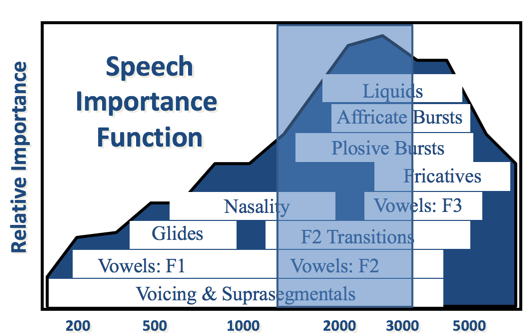
Figure 4. Speech Importance Function overlaid with the ski-slope loss transition region.
Figure 5 shows the typical response that you would see from Oticon, in terms of a ski-slope loss. Admittedly, this particular ski-slope loss is not terribly dramatic for the patient, only bottoming out around 60 dB. However, it makes the point that we are not going to be chasing the very last bit of audibility out here beyond 4000 Hz. It's not to say that this might not be useful for the patient; but in order to get an overall usable, comfortable solution, we are more focused on giving this modest audibility enhancement (from 1500 Hz out to 4000 Hz). That extra little bump of audibility often is enough for those patients with ski-slope losses to notice perceivable benefit.
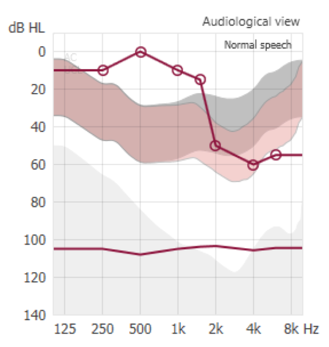
Figure 5. Modest audibility enhancement for a ski-slope loss patient.
Two Sound Sources
One of the things to remember about ski-slope losses is that patients are going to be hearing two sound sources. They're not hearing just what the hearing aid is providing, but they're also hearing what's coming in directly in the open ear canal. For example, if you try to fit the NAL-NL2 response, and provide gain completely consistent with the NAL target fittings, and you try to fit that with an open fitting, you're amplifying in a region where the patient is hearing sound in the lows to mid-frequencies pretty naturally anyway. In cases like that, we recommend that you don't worry so much about the low frequencies, because they're going to get that information fairly well. You need to remember that the patient is going to have to somehow mix the amplified sound with the direct sound. If you create too much amplified sound and drive the high frequencies hard because you're trying to track down a good aided response at 6000 or 8000 Hz, you end up forcing the patient to take an artificially enhanced high frequency sound and mix it with a more direct, natural sound in the lows and low to mid-frequencies. Whereas if you take a more modest approach to this mid-frequency transition region, it becomes much easier for the patient's system to mix those two sound sources together and end up with a more legitimate overall sound picture.
Frequency Lowering
One of the common questions that we are asked relates to how much frequency lowering should be used for patients with ski-slope losses. Ultimately, that determination is up to the clinician. Oticon's recommendation is that for patients with acquired hearing loss, you should try to go without frequency lowering first. We do have frequency lowering available in our Opn products (Speech Rescue), and certainly in the products for severe hearing loss. However, our default recommendation is to go without it. For most of these patients (because of their acquired speech and language skills, their desire to have a natural sound quality and because they are "at risk" for rejecting amplification), we want to try to keep the perception they receive from their hearing aids to be relatively natural sounding. Therefore, as the default, we suggest that you do not start with frequency lowering. Now, if the patient continues to struggle, if they're looking for more help, especially in noisy environments, and you think using Speech Rescue and some frequency lowering would help them, go ahead and try it. That being said, it definitely is not something that we would push very strongly for the typical patient being fit with these ski-slope losses.
Advanced Signal Processing
Another question that sometimes comes up with ski-slope loss patients is whether advanced signal processing makes a difference for these patients. Sometimes it does, sometimes it does not, because the amount of gain in the mid to high frequencies is more modest and because it's an open fitting. Should you be using as much environmental noise control as you possibly can? Of course, because that cleans up the signal before it ever gets into the hearing aid. However, it might not be completely obvious to the patient how much advanced signal processing is happening in the hearing aid, because of this mixture of two sound sources. That being said, anything that you can do to clean up the signal-to-noise ratio for the patient is going to be beneficial (e.g., using directional systems, noise reduction systems, or combined systems like OpenSound Navigator). It just might not be terribly apparent to the patient how much those are working, because of this mixture issue going on with the way these patients are fit.
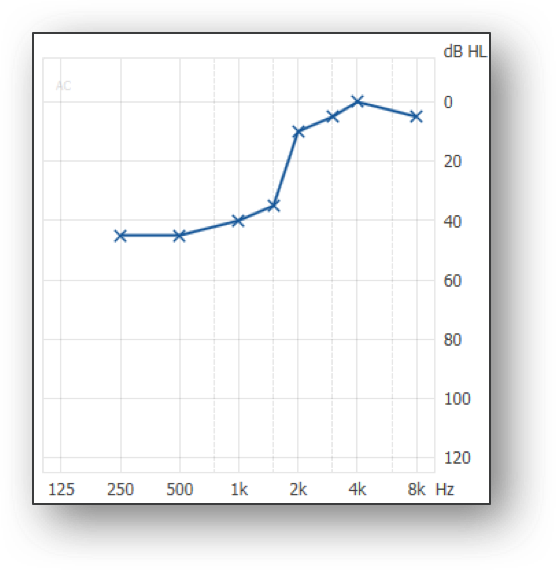
Rising Audiograms
For the purposes of this lecture series, when we talk about rising audiograms, we are referring to patients with rising sensorineural hearing loss (not conductive or mixed losses). These patients generally have moderate hearing loss in the low frequencies, rising to normal or near normal hearing in the mid to high frequencies. Often, the cause of these rising audiograms is linked to a genetic component.
In part one of this series, I talked about one particular patient with a rising audiogram who was the subject of research I was involved in with some colleagues. After a lot of experimentation with different frequency responses, we found that this patient was very well-served using a modest amount of gain in the mid to high frequencies, even though the patient had normal thresholds up in that area. In fact, this patient self-selected audibility enhancement in the mid to high frequencies. The explanation for why someone would do this goes back to this idea of what does the patient want to be listening to? The patient has threshold loss in low frequencies, but there's not a lot of information to be had in that area. There is sound in that region that adds sound quality, loudness, and some elements of the speech signal or a sound in general. In terms of understanding the speech signal in challenging environments, especially for someone who has significant demands on their hearing, that's going to happen in the mid to high frequencies.
This patient self-selected audibility enhancement in the region where his hearing worked well-enough for him and where the response of the hearing aid allowed him to better hear the important parts of the speech signal. Again, that runs a bit contrary to what many hearing care professionals might think: "patient has normal hearing, why would he need gain?" As an analogy, think of what it's like when you're driving in the car, and something comes on the radio that you're very interested in hearing. The first thing that you're going to do is turn up the volume. There is no part of the dynamic range of a person with normal hearing that necessarily works better than another part, unless you're at the very high end or the very low end. Within most of the dynamic range of normal hearing, you could use it any way you want. Even people with normal hearing listen to signals at different volume levels, depending on what they want out of it. If they want to be able to hear and understand speech, one of the things they typically do is turn up the volume. You have a volume control on your phone. If you're trying to get exactly what someone is saying, often times you'll turn it up. Essentially, this patient was wearing a hearing aid that turned up the volume in the frequency region where there's a lot of information to be had, and he was very happy with that response.
This patient was part of a bigger project that we were working on where we were looking at different frequency responses for patients with normal or near normal hearing in the high frequencies, and some sort of rising element to their audiogram. For this particular study, six patients were tested, most of them had normal or near normal hearing in the high frequencies, most of them had moderate hearing loss in low frequencies, one patient had sort of a U-shaped audiogram.
With this group of six patients, we administered four different frequency responses on a variety of subjective and objective listening tests (Figure 6).
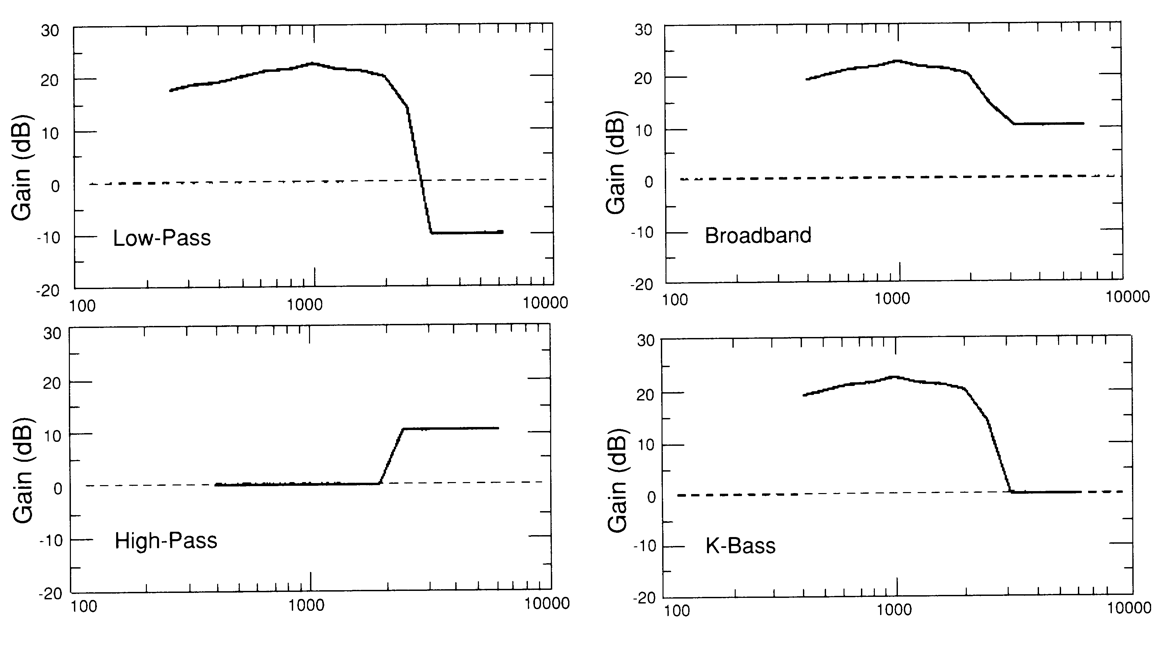
Figure 6. Subjective and objective listening tests (from Schum & Collins, 1992).
First, we tried a low-pass test, which was gain proportional to their hearing loss in the low frequencies, along with a bit of insertion loss added in the high frequencies. Traditionally, what ends up happening if patients are fit with low frequency gain hearing aids, and nothing in the high frequencies. However, if we're not careful about acoustics, we could give them a little bit of hearing loss in the high frequencies. Again, this work was being done 20-plus years ago, primarily to answer the question of why patients with rising audiograms don't do well with hearing aids. That's why we gave them a little bit of insertion loss in the high frequencies. Next, we gave them a high pass response. We gave them a modest amount of gain in the high frequencies, even if they had thresholds that were normal, in order to give them something to listen to up in the high frequencies. We then did a broadband response which combined the two different frequency responses, low-pass and high-pass. Finally, we used the K-Bass, which was pioneered by Mead Killion. He wanted to emphasize that for rising audiograms, we should provide patients significant gain in the low frequencies, while making sure we don't cause a hearing loss in the high frequencies. That was in reflection to this idea of being more aware of what's happening in the high frequencies. For the purposes of our study, we were concerned with whether or not patients were interested in having something in the high frequencies (e.g., the high-pass response and the broadband response).
We also tested these patients with intelligibility ratings for ongoing speech (Figure 7). You can see unaided (UA), low-pass (LP), high-pass (HP), broadband (BB) and K-Bass (KB). Notice that all of the conditions, even unaided, were better than low-pass. This result brought up the fact that if you start cutting away high frequencies from these patients, even if it's done accidentally, they notice it and they don't like it. These patients responded equally as well, if not better, to getting something out in the high frequencies, even if they had normal or near normal hearing.

Figure 7. Average intelligibility ratings (Schum & Collins, 1992).
Then, for each patient, we took the best alternative response based on the intelligibility ratings and compared that to the traditional low-pass scheme. Figure 8 shows a significant improvement in high frequency consonant scores. In general, we were trying to demonstrate the importance of making sure that the patient gets something clear to hear in the high frequencies, and we should not be so worried about just restoring audibility based on the audiogram in the low frequencies.
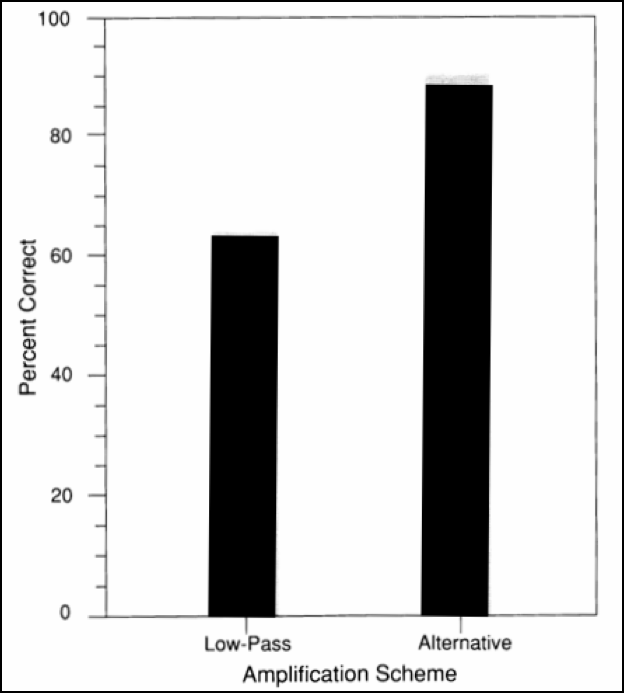
Figure 8. High frequency consonant discrimination scores (Schum & Collins, 1992).
Adjustments
Based on that work, there are some specific recommendations we can make in terms of how to approach these losses. Enter in the audiogram, you will typically see a response that shows a moderate amount of gain in the low frequencies and no gain in the high frequencies. What we would recommend is that in the high frequencies, give the patient at least 10 to 15 dB of insertion gain. Make sure that the patient has something to hear in the high frequencies. Again, it does not matter if they have normal hearing out there. Multi-channel non-linear hearing aids do plenty of protection against loudness for higher level inputs that these patients are not going to be bothered by a modest amount of gain out in the mid to high frequencies. Then, you will probably want to turn down the low frequencies. If you put a rising audiogram into most fitting softwares, you're going to see something that looks like the blue response (Figure 9): a lot of gain in low frequencies, nothing in the high frequencies. We recommend that you turn down the lows and turn up the highs. Although this is very counterintuitive for a lot of hearing care professionals, you'll be surprised if you run into these sorts of patients that it is going to sound like night and day to them. All of a sudden, now they start hearing a brighter, more clarity-enhanced sound and they can start utilizing the sound better. You don't see a lot of these patients in clinic, but if you happen to see them, I would strongly encourage you to try doing something like this if you haven't already come across this as a solution.
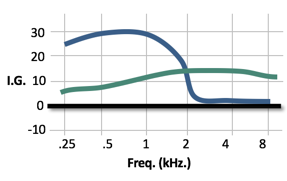
Figure 9. Adjustment recommendations for rising audiograms.
Fine Tuning
When it comes to fine-tuning, each patient may want something different (Figure 10). There are those who may want some low frequencies. Some patients respond well to more of a broadband response. Others may want you to take the low frequencies out entirely. It's going to be very rare that they want you to turn down the high frequencies. Often times, they may allow you to turn it up a little bit, because they're looking for more of that clarity boost.
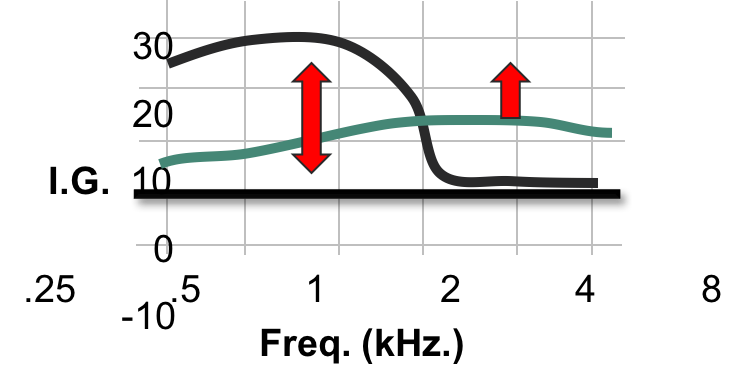
Figure 10. Fine tuning.
Rising audiograms are the perfect example of implementing the notion that we want the patient to use their remaining hearing the way they see fit. We don't necessarily want to try to restore their threshold, but rather assess the hearing that the patient has, and determine how the patient wants to use that hearing. For example, the speech signal is most important in the mid to high frequencies. I want to make sure that this part of the speech signal comes through very clearly. What do I need to do in a hearing aid response to make sure that this comes through most clearly? If you approach those hearing losses in this way, you will see a different sort of response from your patients. If your experience is anything like mine, I think you'll find that this is an easy and effective way to get a better response.
Advanced Signal Processing
Again, the question comes up whether advanced signal processing is important for these patients with rising audiograms. Of course, it is. It might be a bit subtle, in terms of the perceived effect for the patient, especially if they're not using a lot of low frequencies. In general, anything that you can do to improve signal-to-noise ratio for the patient, either through directionality or through some sort of good noise management system, is going to be appreciated. Similar to patients with ski-slope losses, it might not be terribly apparent to them at the time.
Irregular Audiograms
Lastly, I want to talk about patients with irregular audiograms (also commonly known as alphabet audiograms, cookie bite audiograms). The observations that I have to present are not necessarily all that earth-shattering, but I do want to point out one important aspect about dealing with these patients.
One of the things that we know about super threshold loudness perception is that the MCL and UCL curves are typically much flatter than the audiogram shape (Figure 11). Even in ski-slope losses, you'll run into the situation where the UCLs in the high frequencies, where the thresholds are worse, are not dramatically different then the UCLs in the mid to low frequencies. With irregular audiograms, you will likely see the same effect, if you measured MCL or UCL, you're going to see a much flatter response than the HTLs. The important thing to remember is that we don't listen to amplified speech at threshold; we listen to amplified speech typically somewhere in the middle of the dynamic range, often times projected to hit where the most comfortable loudness level would be. Again, it depends on what the fitting rationale does, and I'll talk about that in a few moments. The overall observation is that you want amplified speech to be somewhere in the middle point of the dynamic range, typically around most comfortable loudness for the moderate speech input. Because of that, you don't have to respond dramatically to thresholds that are changing dramatically across frequency. You can ignore those dramatic changes in thresholds, and think about what the super threshold curve would look like.
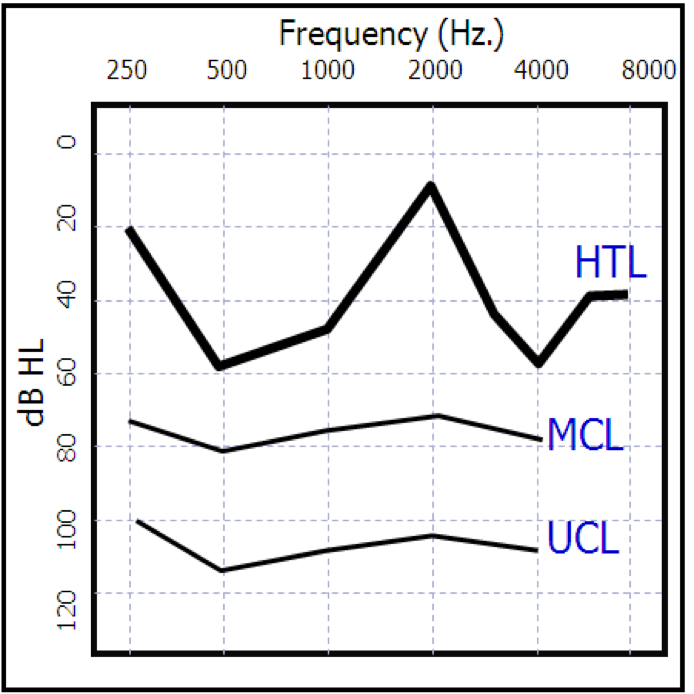
Figure 11. Irregular audiograms.
This goes back to some basic psychoacoustic principles. If you look at the equal loudness curves for normal hearing that we all studied in graduate school, you'll recall that curves are flatter at high intensity levels as compared to the curves for intensity levels near threshold. In other words, you see a relatively flat curve somewhere around the MCL. That's typically where we try to amplify the moderate input speech signal.
Fitting Rationales
Let's take a look at what fitting rationales would do in cases like this. Figure 12 shows the DSL i/o response compared to the NAL NL-2 response, as they relate to the audiogram in the center. DSL i/o is a threshold-based response. It takes a look at the threshold and the UCL pattern (that's either measured or predicted for the patient) and tries to make everything fit within that remaining dynamic range. Because of that, you're going to see a very dramatic response to thresholds that change dramatically across frequencies. A more complex way of calculating their gain and compression ratios, they are taking into account the patient's loudness perception (the predicted loudness growth of the patient) and then recognizing that the MCL curve is going to be flatter. That's just what we know about loudness growth in the presence of sensorineural hearing loss. The NAL response as it relates to this audiogram is a flatter response. The NAL response is not quite as threshold-reactive to changes across thresholds. It probably does not even need to be that threshold-reactive (in a few moments, I'll talk about modifications that I would suggest). Hopefully, you get the idea that you don't have to necessarily respond dramatically to odd-shaped audiograms.
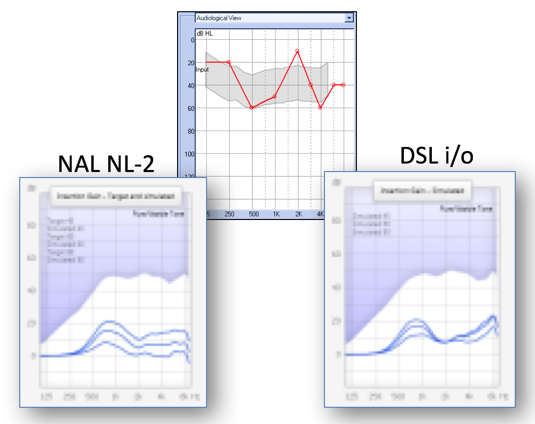
Figure 12. NAL NL-2 vs. DSL i/o responses.
I participated in the fitting for the patient whose NAL-NL2 modification is represented in Figure 13. The modification is shown on the bottom. Even with the NAL-NL2 response, I turned down the amount of gain between 500 and 1000 Hz that NAL was asking for, and turned it up a bit to around 2000 Hz. This revisits the idea of thinking about what the patient wants to use their hearing for, which is to hear speech, especially in the mid to high frequencies. I ended up smoothing out the response for this patient, and the patient was fine. The patient didn't have any sort of reaction that would suggest that they were receiving too much gain at 2000 Hz and not enough gain at 500 Hz. Patients don't hear that way. They experience sound at super threshold levels, and those curves are much flatter once you get up to those levels. In general, with losses like these, don't be so tied to the audiogram and be willing to make some smoothing responses.
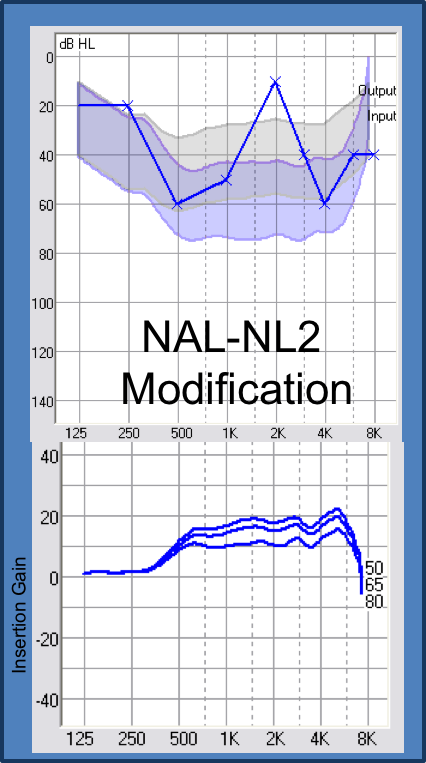
Figure 13. NAL-NL2 modification.
Remember, the reason why smoothing responses are important is that the speech signal is changing in frequency all the time. Speech is made up of a series of rapidly-changing, narrow-band bursts of energy, depending on the consonants and vowels. If you are overly-reactive to threshold changes that are irregular, you could be unnecessarily bending and twisting the speech signal, perhaps overlaying some of those regions where the thresholds are normal at one point. By smoothing out a response, I'm treating the speech signal with a little bit more of a gentle hand.
In Figure 14 you see a prescribed response that will call for excessive gain from 1000 and 2000 Hz, and little to no gain in the high frequencies. I think that's an overly-dramatic response. There is a lot of information in the region from 1000 to 2000 Hz, and there's going to be a certain amount of loudness of the speech signal carried there. For this patient, given that they have hearing loss in the low frequencies, you need to build some loudness into the response of the hearing aid. The adjusted response that I used for this patient didn't completely remove the gain hump at 1000 Hz. I was focused on providing something useful for the patient to listen to above 2000 Hz, and not totally rolling the response. Admittedly, for these types of irregular-shaped audiograms, they're all so different and the clinical research behind these recommendations is light. These are observations that I think are important for you to keep in mind for these patients.
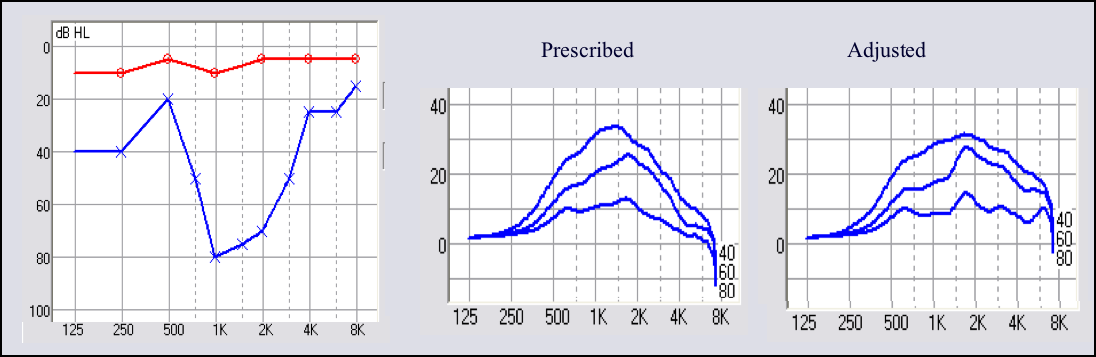
Figure 14. Prescribed v. adjusted frequency response for an irregularly shaped audiogram.
Advanced Signal Processing
Is advanced signal processing relevant for patients with irregularly shaped audiograms? It is, because anything you can do to improve the patient's signal-to-noise ratio is important.
Conclusion
After today's session, hopefully you have an appreciation for and understanding of residual capabilities. To reiterate, residual capabilities are the aided signal in relation to the patient's remaining auditory abilities. It does not matter what the hearing loss looks like becuase that is lost. As the clinician, you need to figure out a way to make use of the patient's remaining hearing. When we look at the atypically-shaped audiogram of a patient, whether ski-sloped, rising or irregular, we need to adress the existing hearing of that patient. We need to determine what they want to listen to and how we can do our best to modify sound so the patient can get the most out of the remaining hearing that they have. Again, it goes back to the idea of Exception Discovery. We know that the rules work a lot for typical losses, and in general, they're a good way to make effective use of our clinical time and mind space. However, if you run into patients whose unique audiograms require you to think outside the box, the traditional rules might not be fully relevant.
If you found the information in part two of this series useful, I would encourage you join us for part three where we discuss other types of auditory conditions that might cause you to take a look at these rules a little bit differently. As always, if you have any questions or comments, please feel free to reach out to me at d.schum@oticon.com. Thank you for your time.
References
Collins, M., Schum, D., Yanda, J. & Fryauf-Bertschy, H. (1985). Low-frequency hearing loss: benefits from three types of linear amplifcation. Paper presented at the Annual Meeting of the American Speech-Language-Hearing Association, Washington, D.C.
Schum, D. & Collins, M.J. (1992). Frequency response options for people with low-frequency sensorineural hearing loss. American Journal of Audiology, 1, 56-62. Available at https://aja.pubs.asha.org/journal.aspx
Skinner, M. (1980). Speech intelligibility in noise-induced hearing loss: effects of high frequency compensation. Journal of the Acoustical Society of America, 67, 306-317.
Citation
Schum, D. (2018, Februrary). Complex versus standard fittings: Part 2. AudiologyOnline, Article 21836. Retrieved from www.audiologyonline.com


