Editor’s Note: This text course is an edited transcript of a live webinar. Download supplemental course materials.
Learning Objectives
Dr. James Hall: This is the first course in a three-part series. At the end of this course, you will be able to define criteria for normal otoacoustic emissions (OAEs). You will be able to identify three measurement factors that might influence OAE test outcome. Lastly, you will be able to list the three possible outcomes for OAE analysis.
Agenda
I will start off with an introduction to OAEs and explain why the evidence suggests that you should be doing them more often than you are. We will talk about recent information on the mechanisms of OAEs. I will then review protocols and guidelines for transient-evoked (TE) and distortion product (DP) OAEs. Then we will talk about OAE analysis. Next I will talk about factors that influence OAEs. Finally, we will talk about how the OAE findings correspond to audiogram findings and what happens when they do not.
Cross-Check Principle
Nearly forty years ago, Jim Jerger and Deborah Hayes (1976) came to a conclusion that we could not put all of our confidence in a single test, which was behavioral audiometry. We needed to back up the behavioral test with other independent measures. Jerger and Hayes concluded that mistakes were being made by audiologists who were only utilizing behavioral techniques. They came up with this concept that no test result should be accepted until it is confirmed by an independent measure.
Pure-tone audiometry that is not accompanied by speech reception threshold (SRT), for example, is totally dependent on the same factors affecting pure-tone testing. Independent measures for behavioral audiometry then would have been tympanometry, acoustic reflexes, or the auditory brainstem response (ABR). Now our test battery has expanded and is very powerful. The test battery for the cross-check principle would include behavioral audiometry, OAEs, immittance (impedance) measurements including tympanometry and acoustic reflexes, and ABR using click stimulus for air and bone conduction.
OAEs are a valuable and essential component of the test battery for evaluating everyone from infants to adults. In another course in this series, I will be talking about the use of OAEs with automated ABR in newborn screening. It is an application of the cross-check principle to hearing screening. By putting together these two tests (OAEs and ABR), the results are far superior than using either test alone as a screening measure. The third part of the series will discuss evidence-based clinical applications of OAEs. We will focus on the measurement today.
Evidence-Based Practice in Audiology: Clinical Guidelines for Pediatric Assessment
Are OAEs part of evidence-based audiology? The answer is unequivocally yes for children or adults. The following clinical guidelines are specific to pediatric assessment:
- 2007 Joint Committee on Infant Hearing (JCIH) Position Statement
- 2008 American Academy of Audiology Clinical Practice Guidelines: Childhood Hearing Screening
- 2012 American Academy of Audiology: Audiologic Guidelines for the Assessment of Hearing in Infants and Young Children
- 2013 American Academy of Audiology Clinical Practice Guidelines: Pediatric Amplification
- American Academy of Audiology Clinical Practice Guidelines: Otoacoustic Emissions (in progress)
These guidelines provide us with a framework for how we should evaluate children, and you will always find OAEs in those evidence-based guidelines. We could make the same argument for OAE applications in adults.
The Joint Committee on Infant Hearing Guidelines (2007) do not suggest, but rather require, OAEs for children birth to six months. Their recommended protocol is shown sin Figure 1. Any time you see a child under the age of six months, and according to the Joint Committee under the age of 2 years, standard of care dictates that you record OAEs. You are not going above and beyond when you record OAEs. This is standard of care. If we do not practice standard of care and we fail to diagnose a hearing loss or make a mistake, we do not have a leg to stand on. Any of you who are seeing children regularly should be testing OAEs automatically on each and every child.
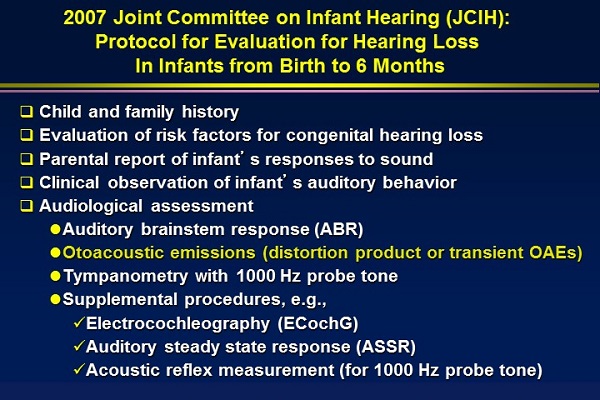
Figure 1. JCIH protocol for evaluation for hearing loss in infants from birth to six months.
A Clinician’s Guide to OAE Measurement
Assumptions
The first assumption is that OAE measurement in children and adults is evidence-based. You are justified in doing it and charging for it.
The second assumption is that most audiologists do not utilize OAEs adequately. They under-utilize them and use a screening approach when they are doing diagnostic OAE measurement. If you were to say to an audiologist, “You only need to screen a patient’s pure-tone hearing at 20 dB every time they come in rather than doing pure-tone threshold testing, because that takes too long,” they would think you completely ludicrous and consider reporting you to the licensure board. Yet, audiologists do that with OAEs all the time. They record OAEs at one level for just a few frequencies and report them as present or absent. OAEs are a diagnostic tool outside of the screening setting.
The third assumption is that when audiologists use OAEs, they simply report them as present or absent rather than fully analyzing results. We will spend a considerable amount of time on how to analyze OAEs to get the most out of that information.
Next, most audiologists do not regularly record OAEs in older children and adults. They may record OAEs in younger children, but they do not appreciate that even older children and adults should be evaluated with OAEs when they are being seen for the first time.
Most audiologists do not replicate OAEs. They record them and go on. That is a big mistake. That leads to confusion and to the identification of artifact as OAEs, or sometimes it leads to conclusions that OAEs are not consistently present when, in fact, they are. Replication is important for anything we do in audiology.
The final assumption I am going to make is that OAEs provide information that is not available from the audiogram. Research consistently supports this conclusion. If you have a patient who appears to have a sensorineural hearing loss on the audiogram, your first conclusion is that OAEs will be absent. But if we already know the test results before we even do the test, why do we even perform audiometry? Obviously, there will be cases where that hearing loss is not what you think it is, or perhaps it is not a hearing loss at all. OAEs complement the audiogram and sometimes they disagree with the audiogram. That is when the OAEs are providing value.
Generations of OAEs
In the late 1980s through the 1990s, we used to classify OAEs according to how they were recorded. Did they require a stimulus (evoked) or were they there all the time (spontaneous)? Within the evoked class, OAEs are categorized on the type of sound that is used to elicit the response. This was a convenient way of categorizing OAEs, but it had nothing to do with their mechanism. In fact, it was not accurate. It implied that the TEOAEs and DPOAEs were giving us the same information. They are both stimulus-evoked OAEs, but they provide different information that the blanket outer hair cell motility. We know more now about the generation of OAEs and their mechanisms.
Reflection Source
A lot of this started in the late 1990s. Researchers from MIT (Shera & Guinan, 1998) said that you could classify OAEs based on mechanism into two types. One was the reflection source emissions, where sound travels through the middle ear and reaches the cochlea, and the traveling wave moves along the cochlea (often in response to a clicking sound). Sometimes the hair cells in certain regions are not working uniformly. Even in a perfectly normal ear, they are not the same. If there are no OAEs functioning at all, then you will get no reflection back.
Furthermore, the reflection is not an echo. It is a physiological response that is dependent on the integrity and functioning of the outer hair cells. Each individual outer hair cell is not producing a response. It is like driving down a road. If it is a bumpy road (i.e., a problem), there will be bumps or reflections. If it is a smooth road, there will not.
Distortion Product
The second type of OAE is referred to as a distortion product emission. In this, we have two frequencies: F1, which is the lower frequency, and F2, which is the higher frequency. They reach their place in the cochlea and are so closely spaced that they produce a small distortion. The distortion product occurs at a frequency lower than the F2 or F1. The typical distortion product in the human ear that is largest occurs at 2F1-F2. There is also a partial reflection component to the DPOAEs.
Differences
These two types of OAEs are very different. The TEOAEs fall in the reflection source category, and the DPOAEs fall in the distortion source. They both involve the outer hair cells, but the DPOAEs are more directly related to motility of the outer hair cells, where the hair cells are expanding or contracting.
The two fundamental mechanisms are different for transient and distortion product. There are many different ways that you could prove that these are two types of mechanisms. One is phase. As the frequency of the transients change, the phase also changes, whereas with the distortions, you can change the frequency of the stimulus and the phase of the response is unchanged. The fundamental principle is that we should be recording transients and distortion products more often.
Other Contributing Factors to OAE Generation
In addition to the hair cells, other parts of the cochlea are also important in the generation of OAEs. Prestin, a motor protein, is critical to recording normal OAEs. Prestin is responsible for the motility of the outer hair cells. Prestin molecules are long and thin; they are responsible for the elongation or the shortening of the outer hair cells. That up and down movement drives the basilar membrane and adds energy to the stimulus. When the Prestin is damaged or genetically removed in some animal models, OAEs are present, but only at the highest intensity levels. Prestin plays a critical role in motility.
The stereocilia generate some of the distortion products that we record clinically. Related to that, if the tallest of the stereocilia is not embedded in the tectorial membrane as it should be, OAEs will not be normal. Normally, you have distortion products in the cochlea when you do have stereocilia. Without the stereocilia, all you have is stimuli. None of the distortion products are there.
Basilar membrane mechanics are involved. The stria vascularis is critical as it is where most of the blood and oxygen reach the cochlea. It is highly metabolic and it produces the endocochlear potential that powers the cochlea. When there is a problem with the stria vascularis, whether it is vascular or drug-induced by Lasix or furosemide, then perhaps you will have abnormal OAEs even though the hair cells are perfectly normal.
While the middle ear is not involved in generating OAEs, you cannot record OAEs without getting energy to the cochlea through the middle ear and back out from the cochlea through the middle ear. Even though the external ear canal is not responsible for producing OAEs, it does play an important role in their measurement as that is where the tiny responses are recorded.
Stereocilia are also very important. Normally, you have distortion products in the cochlea when you do have stereocilia. Without the stereocilia, all you have is stimuli. None of the distortion products are there.
The mechanisms of the cochlea are very important, and knowing that Prestin and stereocilia are important in generating OAEs is very useful clinical information clinically. You will encounter patients who have one or two of those problems.
If you are looking for more information on the anatomy and physiology, you can refer to a book I co-authored with Sumitrajit Dahr (2011), who is a faculty member at Northwestern University. It is very comprehensive, with in-depth explanations on the material that will be highlighted in these OAE courses. There are chapters in this book on the clinical applications of OAEs.
There are no standardized protocols, and all the clinical guidelines I talked about do not tell you exactly how to record OAEs, but there are some general principles that I would like to review with you, which have evolved from clinical experience and clinical research.
Four Fundamental Steps
There are four fundamental steps that we need to do prior to recording OAEs.
Otoscopy
First, always perform otoscopy. Anything in the ear canal may obstruct the probe that we use for presenting the stimuli or measuring the response. Make sure that there is no excessive cerumen in the ear, and in newborns, that there is no vernix. If there is, be very careful that it does not block any of the ports of the probe. If the OAEs are anything but perfectly normal in infants, first suspect that it is vernix. Debris and foreign objects can interfere with OAE measurement, even though it might not cause a problem for other auditory measures.
Middle Ear Measurements
Before you see the patient, determine their risk for middle ear dysfunction. Do they have a history of middle ear problems? Hopefully, you have conducted tympanometry, but if you have any questions, conduct tympanometry and acoustic reflexes. Acoustic reflexes are so quick and yet they provide so much information on much of the auditory system. If you think the patient has middle ear problems but the acoustic reflexes are normal, they do not have a problem with the middle ear.
The use of middle ear measurements, like tympanometry, is a requirement if your patient is an infant. The Joint Committee on Infant Hearing lists middle ear reflexes and tympanometry in the protocol. Unless the OAEs are perfectly normal at all frequencies in each ear, I would recommend performing middle ear measurements.
If the patient has any air-bone gap, any abnormality with the tympanogram and the reflexes are absent, there is going to be a problem with the middle ear. If you are trying to rule out middle ear dysfunction, do not solely use tympanometry; also use reflexes.
What about ventilation tubes? We assume OAEs will be absent in these cases, but I would caution about jumping to that conclusion. You do not know what a test is going to show until you perform the test. Research shows that some patients will have OAEs and some will not (Daya, et al., 1966; Owens, McCoy, Lonsbury-Martin, & Martin, 1993; Tilanus, Stenis, & Snik, 1995; Richardson, Elliott, & Hill, 1996; Cullington, Kumar, & Flood, 1998). If the patient has a ventilation tube and the OAEs are totally absent, then either the ventilation tube is not working, there is a residual middle ear problem, or there is an underlying cochlear problem. If the patient has normal cochlear function, the ventilation tube is in the eardrum and working well, and the middle ear is normal, they will usually have OAEs. In fact, they might be normal.
A child came into my clinic one day, and tympanometry showed a normal ear canal volume with flat tracings bilaterally. The child ended up having bilateral otitis media. This condition was causing a 45 to 50 dB hearing loss. The parents consulted an ear, nose, throat physician (ENT) who placed tubes for the child. Post-tubes, tympanometry showed large ear canal volumes, indicating patent tubes bilaterally. By definition, a tympanogram is a visual change in middle ear compliance as we change air pressure, so although we did not change the middle ear compliance at all, we were able to push air through the hole in the tube and get a volume reading. It did prove that the tubes were patent.
Figure 2 shows the child’s DPOAEs. If you look closely, you will see that OAEs were normal in the high frequencies. The two solid lines in the graph are the 5th and 95th percentile for normal. The distortion product amplitude is shown as well. They did drop off in the high frequencies in each ear, which is interesting. Perhaps there is a subtle high-frequency loss in this child, but they also dropped off in the low frequencies, which is predictable. A patient with patent ventilation tubes and no other problems should have normal OAEs. If they are not normal, there is a problem somewhere.
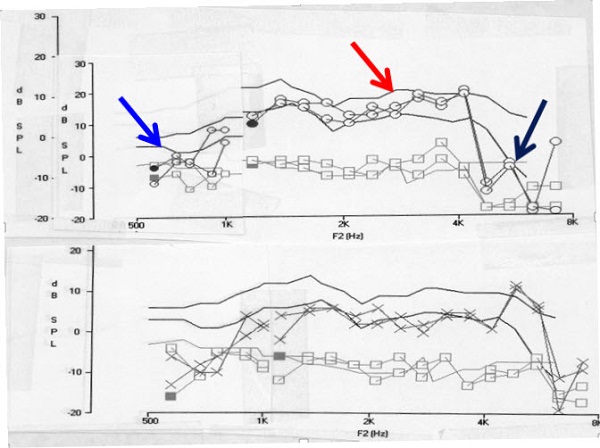
Figure 2. DPOAEs in a child with patent tympanostomy tubes.
Stimulus Calibration
You need to calibrate the probe at the very beginning of the clinical day in a hard-wall cavity. With every patient, you need to verify intensity level. The machine will do that for you, but you have to look at the numbers. If your target for intensity was 65/55 for distortion products or 80 dB SPL for transients, make sure that what you are presenting in the ear canal is within 1 or 2 dB of that. If it is not, step back and evaluate. We have included an extensive section on calibration in our book (Dhar & Hall, 2011).
Most OAE devices calibrate with the probe out of the ear canal, and yet there is a lot of volume, or ear canal space, between that and where the OAEs are coming from. There could be a substantial error in calibration of any OAE device, almost always be in the high frequencies. Part of the error in calibration will be due to traveling wave problems. You are presenting a pure-tone stimulus for the distortion products, but you are also recording an OAE that is a pure tone.
Under the worst of conditions and circumstances, you might get constructive interference, which would make the machine think there was more sound coming out than there was, or cancellation, where the machine would keep cranking out more and more stimulus intensity to calibrate, not realizing that the real OAE was being cancelled, and the stimulus intensity was being cancelled out by interference. Always calibrate. Make sure that your intensity levels are consistent throughout the test, and if they are varying, then you need to stop and correct the problem.
Monitor Noise Levels in the Canal
The fourth fundamental step is to make sure the noise levels in the external ear canal are at least lower than the 95th percentile for a normal subject before you even get started. Audiologists struggle with this one. They put the probe in and say there is noise, but there was nothing they could do about it. There is always a way to reduce noise.
You would not think of doing a pure-tone audiogram out on the street, in the waiting room, or even with the sound booth door wide open. Likewise, you should not be trying to record OAEs when there is a lot of background noise. There is no way to reliably interpret the OAE. Try to get the noise down to at least -10 dB, if not lower. Figure 3 shows the difference between the noise floor and the presence of OAE recordings. The top picture shows a compromised noise floor in the low frequencies. When this is remedied, you can see the presence of OAE recordings well above the appropriate noise floor in the bottom picture.
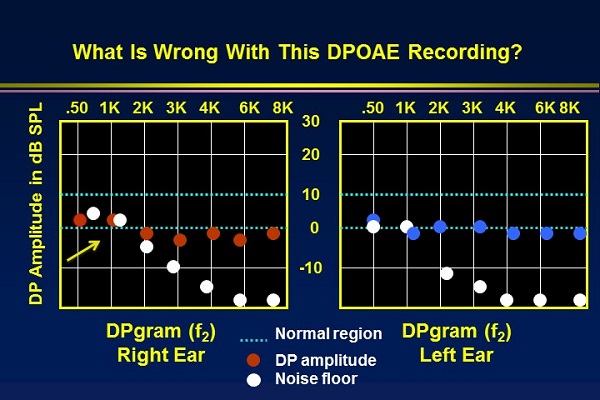
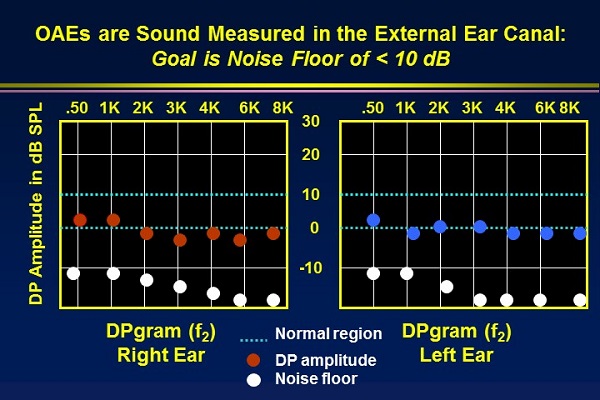
Figure 3. Comparison of noise floor recordings, with a poor noise floor (top) and acceptable noise floor with recordable OAEs (bottom).
We can reduce ambient noise. You do not have to go into a sound booth, but if you can, that is a good option. You can reduce ambient noise by closing the door to the room and turning off all equipment, asking people not to talk, and making sure that you are as far away from sources of noise as possible. Get the tightest and deepest possible probe fit. Locate the patient away from the OAE equipment as that may be producing noise. There may be a fan on the computer, for example. In the worst case scenario, do not evaluate OAEs for the very low frequencies, as this is almost where all the noise is. Noise tends to drop dramatically between 1000 and 2000 Hz.
You can almost always get rid of acoustical noise. Physiological noise can be minimized, but you cannot eliminate it. You can tell an older child or adult not to talk or chew gum and to be as still as possible. Obviously, they will be breathing and blood will be flowing through the ear, which contributes to minimal physiological noise that typically does not interfere with the OAE measurement.
Tips for OAEs
When you are recording transients, you can control to some extent the frequency range over which you are recording. You do not have as much control over the noise, because it is present for all frequencies, even those in which you are not interested.
With DPOAEs, you select the frequencies very precisely. If you do not want noise in the recording, and the noise is in the low frequencies, do not record the low frequencies. You have more control over noise with DPOAE s, but TEOAEs give you more frequency resolution. Both transients and distortion products have advantages and disadvantages. They also have different mechanisms. You are better off using both types of OAEs in diagnostic settings.
If you are using DPOAEs diagnostically, it is important to record at least five or eight frequencies per octave. It makes no sense to record DPOAEs with one or two frequencies per octave. One of the advantages of OAEs is frequency information/frequency selectivity. We learn more about how the cochlea is processing sound at many frequencies. In many cases, patients who have noise exposure and/or tinnitus will have clear dips in their OAEs that reflect cochlear abnormality within an octave (Figure4). If you only looked at each octave, you would not see this dip. Try to get in the habit of setting up protocols that have five to eight frequencies per octave. That does not take that long with a cooperative older child or an adult.
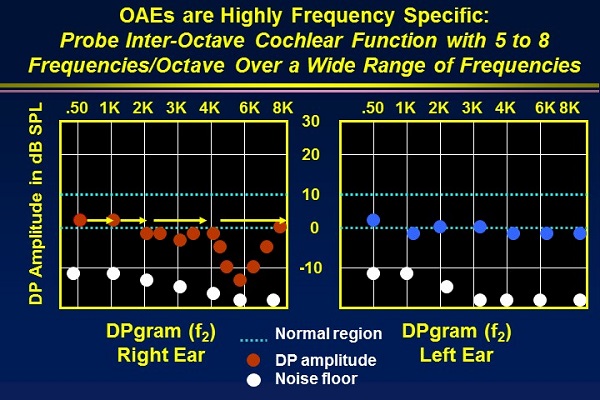
Figure 4. Including five to eight frequencies per octave will shows dips in the response due to cochlear abnormalities.
As you record OAEs, be focused and involved in the procedure. Do not just place the probe and do something else while the OAEs are being recorded. Take action whenever things are not coming out the way you expect. Minimize noise. Make sure that the stimulus intensity is adequate. Make sure you are getting the cleanest OAEs as possible. Most audiologists do not do this. You should be just as involved during OAE measurement as you are doing pure-tone audiometry. You should be critically reviewing the results as you go. Stop the test at any point if things are not working out the way they should be.
A summary of troubleshooting steps that we covered are shown in Figure 5 below.
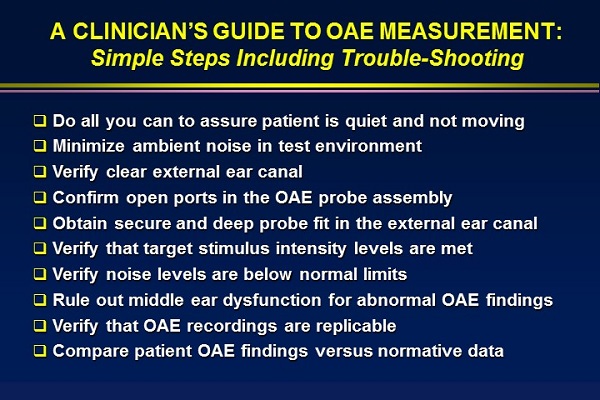
Figure 5. Simple troubleshooting steps.
Creating Test Protocols
Almost every device allows you to create protocols, which is something you should do to cover the majority of patients you see in your practice. A summary of the DPOAE protocols I will discuss is shown in Figure 6.
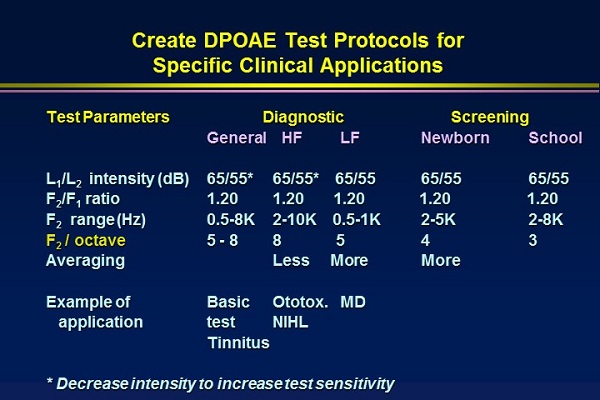
Figure 6. DPOAE test protocols for clinical applications.
General Diagnostic DPOAE
A general diagnostic should include 65/55 dB intensity. The F2:F1 standard ratio is 1.20. F2 stimulus frequencies are from 500 Hz to 8000 Hz. The true DP frequency that we are recording is a little less than 500 Hz and a little less than 8000 Hz. Again, you will include five to eight frequencies per octave. This general diagnostic protocol can be used for any cooperative patient.
If I am doing ototoxicity monitoring or I have patients who are at risk for noise-induced hearing loss or tinnitus, I like to use the general protocol for those patients, and then focus more on frequencies from 2000 to 10,000 Hz.
For a patient with suspected Meniere’s disease or a patient with a low-frequency loss in the audiogram, use low-frequency OAEs. Maybe that is a sign of auditory neuropathy spectrum disorder (ANSD). If there are normal OAEs in a patient with a low-frequency sensorineural loss, this immediately tells you that this is not an outer hair cell problem. It may very well be neural.
Screening Protocol
For a screening protocol, you limit the frequencies to those that are critical for speech understanding and away from the noise floor. Fewer frequencies per octave is perfectly adequate. I would definitely replicate the results whenever you are performing any of these OAEs.
Criteria for OAE Analysis
As I have already emphasized, make sure that the noise floors are adequately low. When someone shows me OAEs and the noise floor is around 0 dB, they ask how they can interpret them. My response is that they cannot. The solution to this problem would have been to get things quieter.
Analyze all the frequencies. If you are doing pure-tone audiometry, you would not test one frequency and then report only those results without looking at other frequencies also. Do not do it for OAEs, either. Many times, audiologists say that OAEs were present. This means that at certain frequencies there was something there, but at other frequencies there may not have been. When you are analyzing OAEs, go from one frequency extreme to the other.
Make sure they are always repeatable. If you take 10 people and record OAEs from them every other day, you will have intra- and inter-subject variability data. The inter subject variability would be comparing one patient to the next on any given day. The intra subject variability would be comparing the OAEs for one person day after day. The intra subject repeatability is extremely high. That is important. Always replicate.
Steps of Analysis
Is there an OAE-to-noise-floor difference of at least 6 dB, meaning, is the OAE at least 6 dB above the noise floor? If not, there is no evidence of any OAE when the noise is adequately low. If the OAE amplitude is 6 dB above the noise floor, that does not always mean they are normal. It simply means they are present.
Next, is the OAE normal or abnormal? The way to answer this is by comparing the OAE findings to normative data for that equipment. Before purchasing a device, I think it is fair to ask the representative of the manufacturer if they have normative data for the system. Ask them where it was collected and for background information or an article that describes the normative data. You will have to use that protocol if you are going to use the normative data.
The good news about OAEs is you can collect normative data quickly. If you are working in a school system or anywhere else where you are seeing five and six-year-old children, I would find a group who have perfectly normal audiograms with no history of ear problems and collect your own normative data. The same thing can be done with adults if you are in a VA setting. You can easily collect your own normative data with your equipment and your test setting with your protocol. Enter that data into the system and you will have your own graph for normative data.
TEOAEs. With TEOAEs, there are several steps that you can take. Make sure the stimulus is adequate. If it is a click stimulus, it should have a very distinct, abrupt temporal waveform for the click. Make sure that the spectrum of your stimulus is broad. If you have only low-frequency or high-frequency energy in your stimulus, there is no way that you can record a normal transient from a patient. You cannot get a response back from the cochlea if you did not stimulate the cochlea acoustically.
Make sure the noise is adequately low. Make sure that the stimulus stability is high. In other words, the stability is high if all the stimuli were almost exactly the same throughout the test. Ninety-eight percent for stability would be very high. If this is down between 50 and 70%, you would want to discard that measurement and do it again. The stimulus intensity was changing too much during the test.
Make sure there is a response waveform. The first response to come out is from the base of the cochlea. As time goes on, we are getting more of a response toward the apex. With most systems, there are two waveforms. Every other stimulus response is saved separately in a buffer, and then there is a correlation (%). It is essentially a mini-replication, but not a real replication. Any noise that happens during the measurement will show up here. I always recommend doing a true replication as well as looking at the correlation.
Then you look at the spectrum of the response, which is the transient energy above and beyond the noise floor. Then we look at amplitude of the OAE compared to the noise, and that is described as the signal-to-noise ratio (SNR).
DPOAEs. For analyzing the DPs, the first thing we want to do is make sure we had good, strong stimuli. Figure 7 shows the F1 (3680 Hz) and F2 (4500 Hz), and the DP occurs below both those frequencies (2F1-F2), at 2859 Hz. It looks perfectly normal and was well calibrated. The stimulus intensities were 65 dB/55dB and very stable.
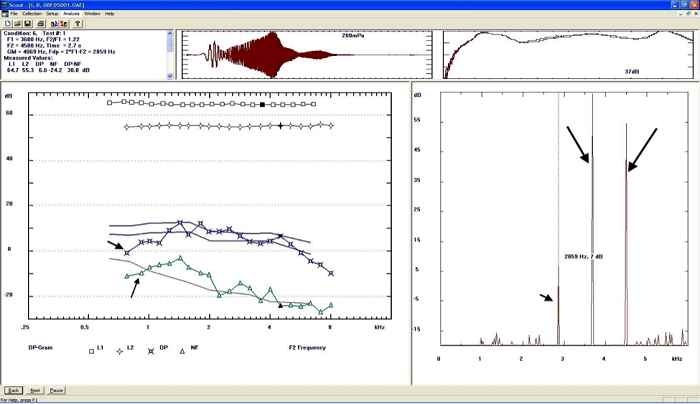
Figure 7. Analysis of DPAOEs. The large black arrows on the right panel indicate the F1 and F2 frequencies; the DPOAE is the small black arrow to the left. Calibration is indicated as the straight rows of squares and diamonds in the recording window pane. Specific intensity and measurement properties are noted in the condition box in the upper left corner.
This example does not show any replication. You can see there is a very tight “normal” level (Figure 7). The top line is the 95th percentile and the bottom line is the 5th percentile. The blue stars are definitely OAEs. Stimulus after stimulus, they look similar. The green triangles are the noise floor, which is quite good for the most part. We can clearly say there is an OAE here; it is within the normal region except for the very lowest frequencies. That is not due to noise. Maybe there is negative pressure in the middle ear. Maybe there is a ventilation tube. We would want to know what is going on there.
Figure 8 is an example from the GSI 60 DPOAE system. The normative region is the two lines at the top. The OAEs are essentially normal and repeatable out to 2000 Hz, except for a dip at 1000 Hz. Beyond 2000 Hz, they are not repeatable, and at the highest frequencies, they are absent. In this one DPgram, we should not say they are present or absent. We are getting different information at different frequencies, which is very useful diagnostically.
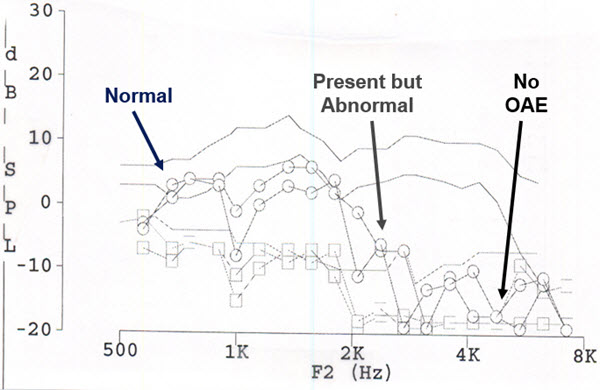
Figure 8. DPOAEs with poor high-frequency replication, low-frequency absence, and dip at 1000 Hz.
I would expect this patient has a problem with their cochlea in the high frequencies. It is not a middle ear issue, because we are getting a great OAE from the low frequencies. When I take this person to the sound booth, I am expecting to see a hearing loss. If I do not, I am still expecting there to be cochlear dysfunction. I will be talking to this patient about their history. Have they ever had ototoxic drugs? Have they ever had noise exposure? Does anyone in the family have a hearing loss? We are going to get in to that in great detail.
Another DPgram shown in Figure 9 only goes from 1000 Hz to 8000 Hz. From a screening point of view, we would say this patient passed. For many of the frequencies, certainly from 1000 Hz to 2000 Hz, the DPOAEs are more than 6 dB above the noise floor. It would be a pass, but it is not normal. You might say they are present, but they are not normal. This is a 62-year-old woman who played the violin, and this is her right ear. She had more of a problem in her left ear. This is clearly abnormal, and we are going to need to investigate.
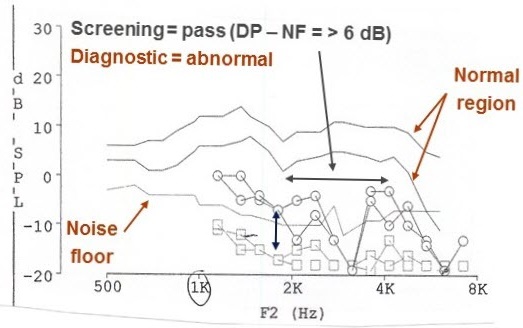
Figure 9. Abnormal screening DPOAEs.
The three possible OAE outcomes are normal, present but abnormal, and no OAEs present at all. At the bare minimum, we need to come up with these three outcomes across the frequency region. You may have a patient where it is normal at all frequencies. You may have a patient where it is absent at all frequencies, but it is not uncommon to have a patient where you get all three outcomes at some frequency region from 500 Hz to 8000 Hz. That is why I would recommend reporting OAEs.
Factors Influencing OAEs
There are some non-factors that do not influence OAEs (Figure 10). These non-factors for OAEs might be large factors for behavioral audiometry. The time of day does not make any difference for OAEs. You might say not, but the time of day does make a difference for ABR, which is likely related to body temperature. If you did an ABR every hour for 24 hours on a single patient, you would see the latencies change quite dramatically, particularly for women.
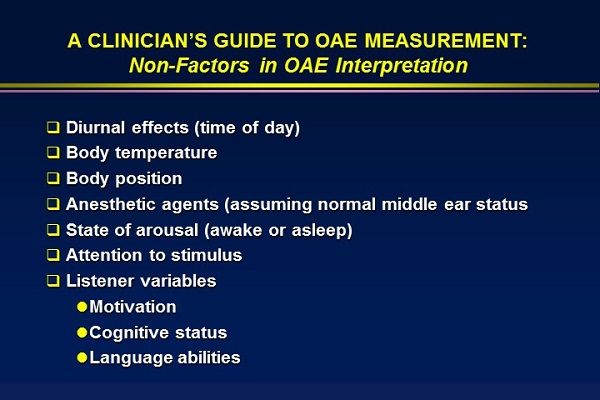
Figure 10. Non-factors in OAE interpretation.
Body position does not make any difference. That is an important non-factor. Anesthetic agents do not make a difference as long as the middle ear status is normal. Whether the patient is paying attention or not or awake or asleep makes no difference. They do not need to attend to the stimulus. It does not matter whether they are motivated, whether their cognitive status is normal or low, whether they understand your language or have delayed speech. Those things have no influence, which make them advantages for OAEs clinically.
Factors in OAE Interpretation
There are some factors that we always need to consider. We have talked about ear canal status. We have emphasized noise. We have talked about middle ear status. Age does influence OAEs in young children, but it does not influence them in older adults. Figure 11 is a TEOAE for a one-and-a-half-month-old child. The OAEs are largest in term (40 week) newborns. That is probably because they have small ear canals, and even though the stimulus is being calibrated in the ear canal, the OAE coming back out into that little ear canal may be recorded as a higher intensity than it would be in a larger ear canal. In adults, there is no aging effect on OAEs, assuming that the patient has normal hearing. Presbycusis is not normal. It is age-related hearing loss, but if the older patient has normal hearing, they will have normal OAEs.
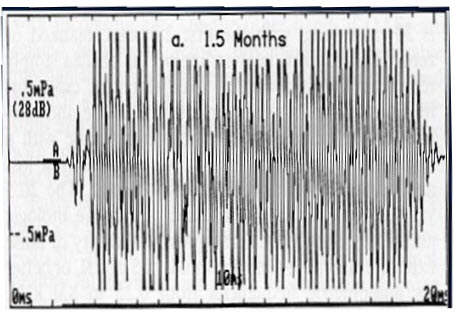
Figure 11. OAE from an infant.
When OAEs are absent, you need to find an explanation. Is it the middle ear? Is it the external ear canal, or is it the cochlea?
OAE and Audiometric Findings
One reason we record OAEs clinically is to validate the audiogram and perhaps detect cochlear problems that are not diagnosed by an audiogram. Up to 20% of the hair cells may be damaged. In fact, you can have many of the hair cells damaged within an octave or critical band in the cochlea. As long as there are a few hair cells working, the audiogram will be normal.
The OAEs in a patient who is missing many hair cells or whose hair cells are not functioning normally will be very abnormal. This is an important point. You are not measuring the same thing on an audiogram as you are with OAEs. They are independent measures of each other. If I am trying to detect cochlear problems affecting the outer hair cells, and almost all cochlear problems do affect the outer hair cells, I will trust OAEs over the audiogram. The audiogram is very insensitive. OAEs provide us with an incredible opportunity to detect cochlear function at the very earliest stages when something can be done about it.
The changes in a patient’s OAEs are like looking into that patient’s hearing future before the audiogram shows any change. If you can stop the problem at that point, they never will have a hearing loss. What a valuable service to offer.
Abnormal Outer Hair Cells and Loudness Recruitment
OAEs help us hear soft sounds normally. Without OAEs, we are left with an abnormal growth of loudness. We do not hear sounds until there are 50 to 60 dB, and at that point, the outer hair cells are not working, and the inner hair cells are activated. There is a rapid growth of loudness, or loudness recruitment. That was defined by Schuknecht (1993), based on his histopathologic studies.
We know that OAEs provide us with information on cochlear function that is reflected in tuning curves. Research has shown that normal OAEs are associated with sharp normal tuning curves, and abnormal OAEs are associated with abnormal tuning curves. Abnormal OAEs predict that the person will likely have some problem processing auditory information. Maybe it will account for complaints that are not reflected in the audiogram.
We also know that OAEs are a pre-neural response. They are produced by the outer hair cells before the synapse with the auditory nerve. It is very possible to have normal OAEs in a patient with a hearing loss. One of the things we need to rule out in those patients is auditory neuropathy, which is a neural or synapse problem that does not involve the outer hair cells.
The audiogram may agree with the OAEs, and that is a good thing. It usually means that there is normal cochlear function. However, it may not, and that is also a good thing. If the OAEs are abnormal, but the audiogram is normal, it very well may be that there is subtle outer hair cell dysfunction. It is just not detected in the audiogram. Or it may be a minor middle ear problem that does not affect the audiogram, but does affect the OAEs.
Then we have the outcome where the OAEs are normal and the audiogram is abnormal. That may be due to a technical problem. Maybe the earphones are not on the ears correctly or plugged in properly. Maybe the patient does not understand the task of pressing the button when they hear soft sounds. It also may reflect inner hair cell dysfunction. The outer hair cells are normal, but there may be a genetic and rare inner hair cell problem affecting the audiogram but not the OAEs. It may also be a neural problem. This can include but is not limited to neuropathy. I have seen dozens of patients where I would have thought it was a sensorineural hearing loss if I had not done OAEs. But with normal OAEs, I was able to make a distinction of neural hearing loss.
I do not have time to cover OAEs in patients with false hearing loss, including children. You will know it if you start every pediatric evaluation with OAEs. If OAEs are normal and their responses in the sound booth suggest s hearing loss, you can immediately suspect that it might be malingering and a false hearing loss.
Conclusion
OAEs contribute incredibly to our test battery and our ability to detect auditory problems at the earliest stage. The earlier we detect auditory problems, the more accurately we diagnose them, and the more effective our intervention can be.
Questions and Answers
How many subjects would you recommend for collecting normative data?
You want at least 10 subjects. It depends on how tightly you define your normal subjects. For example, if you are only getting normative data on five-year-old children, 10 would probably be adequate. Take a look at your data. Run some quick statistics. You can do this easily now with spreadsheets and databases. With 10 subjects you can use both ears, as the ears are independent. If you keep adding subjects and the variability is not changing, then you can stop. If you are getting normative data for children at various ages or adults at various ages, then I would say you need a bare minimum of 30 subjects. Then you would quickly rank those subjects’ OAEs at any given frequency. You can toss out the subject with the largest OAE and the smallest OAE, and that gives you the 5th to the 95th percentile.
I was once instructed to move the probe for the second recording. Is that necessary?
Interference in the ear canal and constructive or destructive interference is why we use warble tones in the sound booth. We do not want a pure tone bouncing around and interacting with another pure tone. If the OAE makes sense with your patient, case history and audiogram, that is fine. If you have spikes or dips that cannot be explained, then I would take the probe out maybe just a millimeter, and repeat. If you get the same thing a second time, then it is not a standing wave interference. If you take the probe out, put it back in, and now you are getting something totally different, that was probably a standing wave. You do not have to do that, although it is not a bad policy. With children, that can sometimes disrupt them. You may not get to the other ear if you are fidgeting with the probe several times.
References
Cullington, H. E., Kumar, B. U., & Flood, L. M. (1998). Feasibility of otoacoustic emissions as a hearing screen following grommet insertion. British Journal of Audiology, 32(1), 57-62.
Daya, H., Hinton, A. E., Radomskiej, P., & Huchzermeyer, P. (1966). Otoacoustic emissions: Assessment of hearing after tympanostomy tube insertion. Clinical Otolaryngology and Allied Sciences, 21(6), 492-494.
Dhar, S., & Hall, J. W. (2011). Otoacoustic emissions: Principles, procedures, and protocols. San Diego, CA: Plural Publishing.
Jerger, J. F., & Hayes, D. (1976). The cross-check principle in pediatric audiometry. Archives of Otolaryngology, 102(10), 614-620.
Joint Committee on Infant Hearing. (2007). Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics, 120(4), 898-921. doi: 10.1542/peds.2007-2333.
Owens, J. J., McCoy, M. J., Lonsbury-Martin, B. L., & Martin, G. K. (1993). Otoacoustic emissions in children with normal ears, middle ear dysfunction, and ventilating tubes. The American Journal of Otology, 14(1), 34-40.
Richardson, H. C., Elliott, C. & Hill, J. (1996). The feasibility of recording transiently evoked otoacoustic emissions immediately following grommet insertion. Clinical Otolaryngology and Allied Sciences, 21(5), 445-448.
Schuknecht, H. F. (1993). Pathology of the ear (2nd ed). Alphen aan den Rijn, Netherlands: Wolters Kluwer.
Shera, C. A., & Guinan, J. J. (1999). Evoked otoacoustic emissions arise by two fundamentally different mechanisms: a taxonomy for mammalian OAEs. Journal of the Acoustical Society of America, 105(2 Pt 1), 782-798.
Tilanus, S. C., van Stenis, D., & Snik, A. F. (1995). Otoacoustic emission measurements in evaluation of the effect of ventilation tube insertion in children. The Annals of Otology, Rhinology, and Laryngology, 104(4 Pt 1), 297-300.
Cite this Content as:
Hall, J. W. (2015, August). A clinician's guide to OAE measurement and analysis. AudiologyOnline, Article 14981. Retrieved from https://www.audiologyonline.com.


