Editor’s Note: This text course is an edited transcript of a live webinar. Download supplemental course materials.
Leanne Powers: Over the next hour, we are going to look at past and current views of tinnitus and the audiologic evaluation for patients who present with tinnitus. We will focus mainly on acoustic treatments that are available, because that is the prime area of interest for those of us who perform hearing instrument fittings. We will also address setting tinnitus maskers for different programs.
What is Tinnitus?
The traditional definition of tinnitus is the perception of sound in the ears or the head without the presence of an external source generating that sound (McFadden, 1982). That definition lends itself to the classification of subjective tinnitus, which is only perceived by the person hearing it. This is different than objective tinnitus, which is sound that can be identified or heard by the examiner. Of all cases of tinnitus presented, 80% are subjective in nature; those are the ones on which we focus for acoustic therapy treatments. The 20% that are objectively identified tend to be vascular (pulsatile) or muscular (myoclonus) in nature; those patients should be referred to appropriate medical professionals in those related fields.
There are over 200 causes identified for subjective tinnitus (Figure 1). We may be familiar with many of those factors that occur along the auditory pathway; however, we may not feel as familiar with changes from outside of the ear that contribute to or exacerbate tinnitus in one way or another. Some of those disorders can be metabolic, cardiovascular, neurologic, pharmacological, temporomandibular, psychological, or dietary.
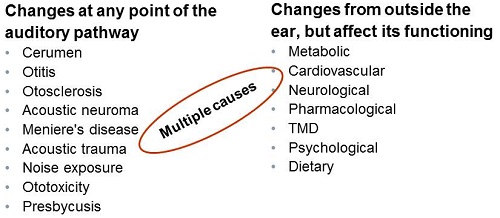
Figure 1. Various causes of subjective tinnitus.
We know that patients can present with multiple etiologies of tinnitus. For example, they may have underlying tinnitus caused by presbycusis. Then they have a change in medication for an unrelated medical condition, and all of a sudden they have a pharmacological cause that has exacerbated the tinnitus. We need to be mindful that some causes can interact with each other.
The generators of tinnitus were originally thought to be focused on the inner ear itself and the hearing nerve. Our current view of tinnitus has changed somewhat; we are now viewing the mechanisms of tinnitus generators as more central to the auditory system. The main factor is still damage to the inner ear, leading to a deafferentation of the central auditory cortex. This deafferentation can lead to alterations in the central plasticity resulting from the changing the balance of the excitatory and inhibitory reaction of the nerve. We are finding now that there are some areas of the central auditory cortex that are affected when a patient has the symptom of tinnitus. Functional MRI studies of the auditory cortex and the auditory pathway can show areas that are lit up in a patient with tinnitus as opposed to in a patient that does not have tinnitus. This has led to this change in our perspective in that tinnitus is more central than we had originally thought.
The repercussions of tinnitus can affect different areas of a patient’s life, and significant tinnitus may affect the quality of life in different manners. The patient can have disruptions in their sleep. They may have difficulty concentrating. They can have difficulty in their emotional balance and well-being. Some patients will change their social activities due to the fact that they are experiencing tinnitus. They may pull away from others. They may try to avoid noise because it worsens their perception of the tinnitus; they may change their lives in general as a result.
Seidman and Jacobsen (1996) surveyed patients with tinnitus and asked if their tinnitus had no impact, some impact, or was incapacitating. Of patients who present with the symptom of tinnitus, 80% will feel that the tinnitus is not affecting their life. They know they have it, but it does not have a significant impact on their sleep, concentration, or emotional well-being. Fifteen percent of patients will feel that it does impact their life. Tinnitus has changed their life because of the repercussions that they experience from it. Those are the patients on whom we want to focus by using acoustic therapy. There are also 5% of patients who present with tinnitus that can be completely incapacitating. These are the patients who report suicidal thoughts. They can no longer work or go about their daily life. Those patients benefit from going to a tinnitus treatment center where the prime focus is specifically on tinnitus therapy and helping people become functional again.
Unfortunately, when patients go to their primary care physicians searching a cure for treatment or answers about their condition, they are often told that there is nothing that can be done and they have to learn to live with it. For 80% of the people, as long as they have had some reassurance from their physician that their tinnitus is not going to cause debilitating side effects or death, they may still be able to move on. However, for 15% of people, the answer, "there is nothing that can be done” is not going to be enough. It affects their life, and we know that there are treatments available to improve quality of life.
We can identify different types of treatment for tinnitus, including drugs, surgery, dental, physiotherapy, psychological therapy, acupuncture, and acoustic treatments. If tinnitus is caused by an underlying disease, some drugs to treat the underlying disease may result in the symptom of tinnitus being reduced or removed altogether. That would be the extent of drug treatments. No specific drug has been identified to significantly impact the symptom of tinnitus directly, but if you are treating the underlying disease that is affecting the amount of tinnitus, drug therapy can be appropriate.
Surgical therapy works in the same way. We know that severing the hearing nerve is not going to prevent the patient from experiencing tinnitus, and oftentimes, patients that have a nerve section surgery can become your worst tinnitus patient. Furthermore, the patient can end up in that 5% where tinnitus becomes debilitating. There is not a direct surgery for the symptom of tinnitus, but again, if you treat the underlying cause, such as otosclerosis where surgical treatment corrects the condition, they can have a lessening or a disappearance of their tinnitus symptom as a result.
Dental treatments are for patients who are suffering from temporomandibular joint (TMJ) disorders. Oftentimes they can have a dental apparatus or surgeries that can help alleviate tinnitus that is caused from this area.
Physiotherapy or physical therapy can help patients who are experiencing tinnitus due to vascular conditions, muscular conditions, or stress-related tinnitus, which are areas of underlying etiology or contributing factors. Additionally, there are patients who have tinnitus who need additional psychological treatment. Some patients report that acupuncture can help or alleviate the perception of tinnitus. We do not want to rule out any treatments for this category of patients. Those who are experiencing tinnitus may have explored all of these options, or they may be willing to explore any option that is going to lessen the amount of ringing that they are experiencing. The area with which we are most concerned as hearing care professionals is acoustic treatments.
Acoustic Treatment for Tinnitus: Evaluation
When we talk about acoustic treatments, we are referring to sound therapy. Sound therapy may be as simple as prescribing a hearing instrument for the patient. For those of you who feel that you are not ready to work closely with tinnitus patients, we ask you to consider that many normal hearing instrument wearers that you have fit with hearing aids have tinnitus. A vast majority of them can experience a reduction in their tinnitus symptoms by wearing hearing instruments. Essentially, you are already working with this population.
The 15% of tinnitus sufferers who report that tinnitus has an impact on life their may require more than a hearing instrument alone. For those patients, we will talk about the addition of a masking device, tinnitus retraining therapy (TRT) and tinnitus activities therapy (TAT). Those are popular approaches to treating tinnitus with acoustic therapy.
Clinical Evaluation
We cannot start our acoustic therapy until we have done an adequate evaluation of why the patient is experiencing tinnitus to begin with. We are going to first look at the clinical and audiologic evaluation for patients presenting with tinnitus. The American Academy of Audiology (AAA; 2000) recommends that you approach tinnitus as a multidisciplinary team. When we think back to the short list of different causes that can be associated with tinnitus (Figure 1), we are very familiar with the list of audiologic causes shown there, but the medical causes that can exacerbate tinnitus or cause tinnitus house themselves with different professionals within the medical field. Treating a patient with tinnitus should be taken from a multidisciplinary team approach. You need to know when to refer this patient to other individuals, and hopefully the other individuals in the medical field will know when to refer this patient to you for treatment. We are looking for hearing care professionals to educate the medical professionals on the fact that we can treat the symptom of tinnitus with acoustic therapy; audiologists and hearing instrument specialists are a great resource in this area. We are fitting hearing aids already and now can fit devices that have masking technology. We want to educate them that we are part of this multidisciplinary team so they can refer patients for treatment when they fall within our realm.
Once we have determined that the patient’s tinnitus falls into our scope of treatment, we need to take a look at the tinnitus itself. You do need to have a separate questionnaire for tinnitus patients. Fortunately, there has been a lot of work done in this area, and there are some convenient hearing loss and tinnitus intake forms that you can use. Some are available from the Tinnitus Research Initiative, and they tend to be very extensive. We want to investigate the specifics behind the tinnitus. How did it start? Do you remember when it started? Has it changed at any point? Is it related to other things in your life? Those questionnaires can get at the heart of the symptoms and help us determine what direction we want to go with treatment.
After the intake questionnaire, you will do the basic audiological evaluation. You are going to do speech audiometry and immittance testing. It is very important to consider adding loudness discomfort levels (LDLs) for patients presenting with tinnitus, because we know patients with tinnitus often have hyperacusis also. We want to identify those patients. Doing LDLs may also help you make decisions in your immittance testing, such as whether or not you actually want to do acoustic reflexes on this patient.
Specific to analyzing the tinnitus, it is recommended that you look at the psychoacoustic measurement of pitch matching, loudness matching and minimum masking level. We are going to go through these procedures, as we recognize that this either may be the first time you have heard about them or you feel that you need to know exactly how to go about adding these to your clinical battery.
Pitch Matching
When a patient presents with tinnitus, we want to see if we can ascertain the frequency region that is most similar to the tinnitus symptom that they are experiencing. Patients experience tinnitus in different ways; some report it as crickets; some report it as steam from a kettle; some report it as a ringing sound. You may not be able to get an exact match, but we want know the approximate frequency range of where the patient feels they are experiencing their tinnitus.
To do this, you are going to test one ear at a time the normal frequency range from 120 Hz up to 12,000 Hz. From your case history, you can ascertain whether the tinnitus is low or high pitch; most patients report high-frequency tinnitus. Starting at 1000 Hz and moving up or down, based on the patient’s report of pitch, may be the best way to go. If we start at 1000Hz and go upward in frequency, we are going to present tones at 5 to 10 dB above the hearing threshold, so you need to have done your basic audiometry already. We continue to test at 5 to 10 dBSL until we can find the pitch that most closely matches the tinnitus that they are experiencing. We want to make sure that we have determined the hearing threshold at that pitch. For example, you have tested at 500, 1000, 2000, 4000, and 8000 Hz during the audiometric assessment, and you start the search for pitch matching. When you get to 2000 Hz, they say their tinnitus is a little higher in pitch. You go to 4000 Hz, and they say it is a little lower. Now you stop at 3000 Hz. If you have not tested the hearing threshold at 3000 Hz, you do need to do it at this time. We do need that when we proceed to the next step, which is loudness matching.
Loudness Matching
For determining the loudness of a patient’s tinnitus, you will use the frequency you just determined during pitch matching. Start at their audiometric threshold and increase the intensity in 1-dB steps until they feel that the stimulus is equal in loudness to the tinnitus that they hear. You can do this with pure tones or narrowband noise, but we want to make sure that it gets an equal loudness rating. Remember that if you are using a narrowband noise that your threshold may be a little different. You do need to have established the threshold for narrowband noise if that is what you are going to use in your loudness match.
The determination of loudness is going to be the match for tinnitus loudness at the frequency that best matches their tinnitus minus the threshold at that frequency. For example, my patient reported that tinnitus was closest to 4000 Hz in nature. Their loudness match was 70 dB and their audiometric threshold at 4000 Hz was 60 dB. Their tinnitus loudness sensation level is equivalent to 10 dB. It is interesting to note that most researchers have identified that in the majority of patients presenting with tinnitus, their loudness match is 10 dB or less above their hearing threshold level. This is going to be important in your counseling.
Minimum Masking Level
Moving on from the loudness match, we are going to look at minimum masking level. In this case, we are going to instruct the patient that the purpose of this test is to determine if we can cover or mask their tinnitus with another sound. We can accomplish this for some patients, but for others, we may not be able to get the masking noise loud enough to cover the patient’s tinnitus. We are going to find the patient’s threshold for white noise. If white noise is not available on your audiometer, you can use whatever noise is available, but you need to determine that threshold separately because it will be different from your pure-tone thresholds. When using white noise, start below their hearing threshold. You are going to increase in 5-dB steps and record the lowest level at which the patient reports noise to cover up their tinnitus so that they no longer hear their tinnitus anymore. The difference between this level and the threshold for noise is your minimum masking level. Because we know that some patients may not be able to be masked, stop if the patient at any time reports discomfort, even if the tinnitus is still audible.
Counseling
The information that we obtain from these three psychoacoustic measures is very valuable for the counseling. Counseling is key with patients that experience tinnitus. It is important to note though that measuring pitch, loudness, or tinnitus minimum masking level has no direct relation to the diagnosis or the prognosis for treatment. Just because someone cannot experience a complete masking of the tinnitus during minimum masking level testing does not mean they are going to do any worse or better with treatment, especially when we use treatments that focus on habituation and not solely on masking measures. Matching pitch makes the patient understand that you have an appreciation for the sound that they are hearing. Loudness matching can be crucial in explaining to the patient that, although they feel the sound is loud and disruptive in their life, it is not that much above their hearing threshold level. That can be key in having a better perspective on what they are experiencing. If the patient can experience a minimum masking level where the tinnitus is taken away for a few seconds during their treatment, they can attain the understanding that their tinnitus can change. They can take control of it, and it does not have to govern their lives. These three measures can be powerful in your counseling approach, but they are not necessary in fitting a masking device for tinnitus therapy.
Now that we have completed the evaluation and ruled out any medical contraindications, we know that this patient who can be helped by acoustic therapy. Now what do we do?
Treatment
There is no one unique treatment for tinnitus. There is no consensus that one treatment is better than another, and we are not here to tell you that you should perform Treatment A over Treatment B. In actuality, most tinnitus treatments lack the controlled clinical trials to be able to statistically say which treatments are superior. There are several different ways you can approach patients with tinnitus, and it needs to be unique to the patient and the patient’s needs.
There are two general categories of treatment: counseling and sound therapy. Other treatments tend to fall in the hands of other medical professionals, because that is really when we are treating the tinnitus directly. As hearing health care professionals, we are focusing on the patient’s reaction to tinnitus. Our prime goal is to change the reaction to their tinnitus, and that is where we can use acoustic therapy.
What do we think we can do to change the reaction to the patient’s tinnitus? The first thing we can do is something that we are already doing for patients who we fit with hearing instruments: counseling. The patient must understand what the tinnitus is in order to overcome any negative associations they have with it. This is key, no matter the severity of the tinnitus or what therapy approach you will employ. Counseling is step number one. They need to understand what tinnitus is, the mechanisms behind it, and what can be done to help overcome it. Counseling is paramount in making sure that the association between the auditory system and the limbic system are kept to a minimum.
The other essential component is sound therapy. We currently look at tinnitus as a consequence of modified neural activity. It is generated in the central auditory pathway subsequent to peripheral damage. This peripheral damage has caused changes in the central auditory system. Therefore, we are going to embark on sound therapy in hopes to avoid cortical tonotopic reorganization to keep modifications to the central auditory system to a minimum, because that will exacerbate the tinnitus in the long run.
Acoustic treatments can involve amplification alone, or it may involve a dedicated therapy program such as TRT and TAT, or it can involve general sound therapy.
Amplification Alone
We chose to discuss TRT and TAT because they are two of the most commonly talked about and used clinical treatments for tinnitus in the hearing health care field. Siemens does not advocate one program over the other, and other programs are available, but we are focusing on these two today as they are the ones that have the most research readily available.
What are the benefits of amplification alone? We already talked about counseling. In general, the counseling that we do during a hearing aid fitting or following our hearing testing helps the patient understand their tinnitus. This is the first step in tinnitus treatment. Then, if you are following a tinnitus treatment protocol, you usually have a more extensive counseling session as well. The second thing we are going to do is use hearing aids to amplify speech. Amplifying speech for a patient helps them to decrease the attention they are paying to their tinnitus. The hearing instrument also amplifies environmental sounds, which helps reduce the audibility of the tinnitus in general. We already know that most of our patients report tinnitus being louder or more intense when they are in a quiet environment. The more sound-rich you make an environment, the less audibility of the tinnitus is perceived.
We have a hope that sounds amplified by the hearing aids are going to produce neural activity by the auditory system and interfere with the representation of the tinnitus in the central auditory system. This is where we talked about using sound therapy to interrupt the tonotopic reorganization of the central auditory system. We want to give the brain other things to listen to. Oftentimes, the most effective hearing aid settings that we use for a patient when communication is the primary goal are different from those when we use amplification as a treatment for tinnitus.
For example, when communication is the goal in hearing aid fittings, we try to bring out speech and diminish other sounds and noises in the environment. We try to filter out steady-state noises such as fans and air conditioners, and different things in the environment. When tinnitus is the prime concern for a patient, sometimes the patient benefits from having those sounds audible, which are not audible without hearing aids. You may consider fitting your hearing instruments differently when the prime concern is tinnitus rather than communication. You may utilize omnidirectional microphones more often. You may set their digital noise reduction at a lower setting than you would for a traditional patient. It is important to gauge from your initial interview of the patient how much the tinnitus is affecting their life, and then you can prioritize their communication needs versus their tinnitus needs. Sometimes there is a mix between the two, but often there is a clear definition when the patient cannot think about anything other than their tinnitus. You need to focus on trying to control the tinnitus first, and then wean them back to using the amplification as a prime goal for communication.
Candidates for amplification include any patients that have hearing loss and tinnitus, regardless of the nature and extent of the hearing loss. It has been estimated that up to 90% of patients with tinnitus may receive some benefit from traditional amplification alone (Johnson, 1998). Even if you are not using any sort of masking signal, fitting the patient with the hearing aid is the first step in tinnitus therapy.
Masking Therapy
Some patients require a step above amplification to treat their tinnitus. This is where we start to talk about using masking signals or masking therapy, or different noise therapies within the hearing instrument to aid in tinnitus therapy. One very popular approach to this is using TRT, which was developed by Dr. Jastreboff (1990).
TRT is based on the neurophysiological model of tinnitus, described by Dr. Jastreboff in the 1990’s. It is the ability of the nervous system to suffer persistent functional changes in its circuitry. We know that there is neural plasticity within the central nervous system and that events in the environment can affect this neural plasticity. Physical changes in the sensory neuron take place, based on whether or not the patient has habituated to the stimulus or if they are hyper-aware or hypersensitive to the stimulus.
The definition of habituation is the reduction or elimination of central nervous system activity in response to repetitive stimuli (Encyclopedia of Neuroscience, 1987). It is a natural process of the central nervous system, and it is crucial to brain function. If we had to process all of the stimuli that were coming into our brain at the same time, we would be overloaded. Our brains are able to pick and choose what we feel is the most crucial input to perform a task or to attend to specific things in the environment.
Jastreboff (1990) was looking at why is it that two patients can have tinnitus of the same pitch, loudness and minimum masking level, yet one patient can be extremely affected by it, and one patient may experience very little effect. That is when we are looking at habituation. Remember that 80% of patients with tinnitus can report that it does not affect their life. Those are the patients that we consider having natural habituation. The tinnitus is detected by their cochlea, goes to the subcortical level, is perceived, but then it is dismissed as not being offensive or related to anything important in the environment. It is not a threat, and they will habituate to it over time. Natural habituation can typically occur within six months of first recognizing the symptom.
Criteria for Sound Selection
New sounds may provoke a different reaction in one person than another. Sounds that are not new are going to be compared to memories that we already have, and then we are going to rank them in priority. If you have tinnitus for the very first time and you think you have a brain tumor, it is going to provoke a negative reaction, which, if not demystified, could lead to a long-term reaction to tinnitus. If you had tinnitus once before, but it went away on its own, you will not have a strong reaction to it. We also know that during situations of concentration, your brain can ignore different signals that come in and we know if you are in a situation of relaxation, your brain is going to pay more attention to different things in the environment than if you were concentrating on a specific task. Depending on what was happening in your life when your tinnitus occurred, you could have a different reaction to it as well.
Signals that are contrasting are going to be heightened. It is very common for our patients to report tinnitus to be much more invasive or much louder in quiet. The easiest way to explain to a patient when you are looking at de-emphasizing the tinnitus and avoiding silence would be to compare that to a candle. If you light a candle in a dark room, it gives a tremendous amount of light and it can have a big effect. If you light a candle in a room that is lit by other lighting sources, it does not have as much of an effect. When we are looking at the Jastreboff approach with habituation, we want to take the focus off the tinnitus, and do that by having the patient avoid silence. In other words, we are going to enrich the auditory environment.
We know that some patients will attach an emotional association to the tinnitus, and that exacerbates the cycle of detection; this is the 15% of patients who say that tinnitus has an impact on their life. If the limbic system is activated, the perception of tinnitus is heightened and you become more aware that tinnitus is there, and it becomes a vicious cycle within itself. They may have associated their tinnitus with fear of the unknown, and they may have anxiety related to it. That can happen if they have thoughts of the possibility of a tumor, progressive hearing loss, or never being normal again. This will affect their perceptions.
The 5% of patients that experience a significant impact are the ones whose limbic systems have pushed them to have a reaction from the autonomic nervous system. They experience a physical reaction to their tinnitus, sometimes in the form of sleep disturbance, anxiety or panic attacks, or other manifestations that lead them to require intensive therapy to control their tinnitus.
In short, if the patient has no emotional association to the tinnitus, they are going to habituate to it on their own. If they have an emotional association to their tinnitus, then they can have effects in the limbic and autonomic nervous systems that need to be addressed.
Tinnitus Retraining Therapy
The protocol for TRT involves directive counseling. This is usually a one-hour therapy session centered on demystifying the tinnitus. We talk about the hearing loss itself and how that is related to tinnitus, including the neurophysiologic model. The patient is then placed in one of five categories. These categories are numbered 0 to 4, and that based on whether or not the patient has tinnitus with hearing loss, tinnitus with no hearing loss, tinnitus with hearing loss and hyperacusis, and tinnitus with hearing loss and hyperacusis for an extended amount of time. Those categories are going to dictate the length of time and the type of treatment. TRT often uses a sound generator, hearing aid or a combination device, and they recommend using open mold fittings.
Follow-up for these patients is going to be 18 to 20 months. Habituation takes some time to take effect, but we hope to wean the patient off their sound generator or therapy signal slowly within that time. If a hearing aid is needed for audibility, we hope that the patient would still be using that, but nothing else after 24 months. What is important to note is that habituation only occurs if the patient can hear the tinnitus. If you completely mask the tinnitus, you cannot habituate. You need to watch the masking level closely.
When we are looking at how to set a tinnitus therapy feature for TRT, we need to talk about a mixing point. The mixing point exists between the hearing threshold and where the tinnitus is completely gone or masked. Siemens micon instruments all contain a tinnitus therapy feature, and that therapy feature has a series of sliders that we are going to show you in a few minutes. You can decrease those sliders to be below the patient’s hearing threshold. You then slowly increase the noise level and instruct the patient to acknowledge when the signal is mixed with their tinnitus. We do not want the tinnitus to be completely gone, but we want to be changing their tinnitus as a result of the increasing noise. Both sounds should be heard together, and that is the mixing point. Typically, the therapy signal is set just below the mixing point. Again, try to avoid total masking. If you are giving the patient a volume control for their TRT, you need to instruct them not to increase the volume control to the point where they no longer hear their tinnitus.
Tinnitus Activities Treatment
We are going to switch gears and look at the approach developed by Tyler, Gogel and Gehringer (2004) at the University of Iowa. TAT takes a different approach; we are looking at four specific functions that can be impaired as a result of tinnitus. Those are identified as thoughts and emotions, hearing, sleep, and concentration. If you are following the TAT plan, your counseling is going to be more interactive in nature. Instead of telling the patient about the loss and the tinnitus, we are going to focus on the areas of the patient’s life that are being affected by tinnitus. We are going to highlight those areas do more extensive counseling when necessary. Sound therapy is used to help decrease the prominence of the tinnitus and help ease the patient into habituation, but habituation is not the only goal here.
Activities are also used with TAT plans. Cognitive behavioral therapy can be used. The patient may be asked to keep a tinnitus diary. They may have some relaxation exercises suggested as well. The mixing point or total masking are thought to be equally effective. In this case, we are not looking at setting the therapy signal to a specific mixing point; we are looking at what is best for that particular patient’s needs. Dr. Tyler has divided the counseling into 10 sessions, and those 10 sessions relate to the four different areas of life that can be impacted. Those are available for download from the University of Iowa web site. You can then print them out and have them bound into different notebooks for different sessions. Counseling will focus only on the areas that the patient needs. For example, if your patient is not experiencing sleep deprivation, we are not going through counseling for sleep.
TAT: No Hearing Loss
For the patient with tinnitus but not hearing loss, you are going to decrease the sliders we talked about. Figure 2 is a screenshot of the tinnitus therapy feature in a micon hearing aid by Siemens. You are going to decrease those sliders to zero and then slowly increase them. When the patient reports that the sound is audible and comfortable, that is where you are going to stop, and that is going to be your treatment level. It is important to note that we have different noise types available: white noise, pink noise, speech noise, and high-tone noise. With TAT, we choose the signal type that is going to give the patient the most relief at the lowest level. The developers want to use the lowest level of preferred masking noise possible for a patient. We want the patient to be comfortable. We are not going to use a set mixing point, and it is important to remember that total masking is an option in the TAT approach. If the patient prefers the sound of the noise to the tinnitus itself, the clinician can consider using a narrowband noise approach and doing a total masking for that patient.
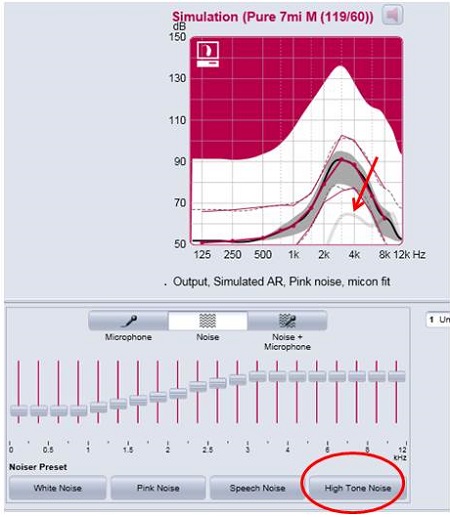
Figure 2. TAT settings in a Simens micon hearing aid for a patient with no hearing loss.
If you are setting TAT for most of the patients we are dealing with that also have hearing loss, you will likely use multiple programs. In the example in Figure 3, we are using three different programs. We have a universal program where the tinnitus therapy signal is not activated. We have program 2 set up with noise and microphone, which is a mixed mode, and then program 3 can also be set as noise only. That may be useful if the patient wants to not be attending to other sounds in the environment. They may not want those microphones on, but we still want them to avoid silence, so we give them that noise-only section. It is important to note that with the Siemens micon therapy signal, you can put the noise in one or both ears. It is going to default on in both ears, but you can use the icon that is located in the center of your software only the right or the left if the patient only wants the therapy signal in one side. It can be in one or multiple programs and presented in different ways in those programs. Our system lends itself very easily to the TAT plan approaches.
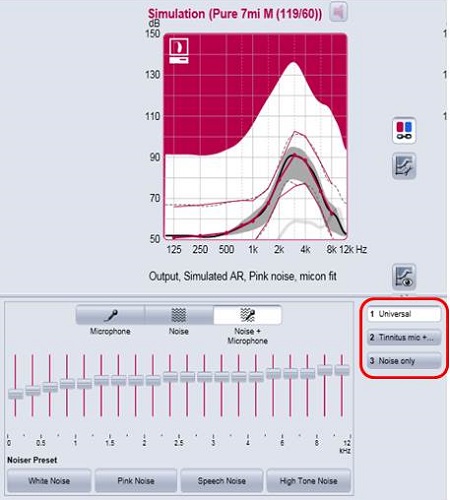
Figure 3. TAT settings in a Simens micon hearing aid for a patient with hearing loss.
General Sound Therapy
I want to end on general sound therapy. You may have a patient come in to your office with tinnitus, and they may even have mild hearing loss, but they are not willing to commit to amplification at this point. Those patients can still benefit from general sound therapy. General sound therapy uses other sounds in the environment to do that sound enrichment for us. It may be the sound of rain fall on a CD that they listen to while they are sleeping. It may be an MP3 player that they use to enrich their sound. They may use a stereo pillow. They may use a sound generator with ocean sounds. If you are going to open your office to tinnitus patients, consider having some of these devices available for them to purchase or order. Your patient may not always want to have their hearing instruments on or they may not be ready for the purchase of hearing instrument devices, but they can benefit from general sound therapy.
Conclusion
We want to transform the patient’s reaction to tinnitus, and we are going to do that using counseling. We want to also transform their perception of their tinnitus, and we are going to do that by using sound therapy.
Siemens has a complete line of hearing instruments that have the tinnitus therapy feature available. All micon instruments have the tinnitus therapy feature available with four different noise types, and the noise can be shaped with the different handles based on technology level. In Siemens hearing, our technologies are grouped into the 7 mi as the highest-end technology, the 5 mi in the middle, and 3 mi as our value-end technology; we have the treatment therapy available in all of those programs.
In addition to that, we released the Orion instrument, which is made for the essential consumers. These are patients where cost is a true stumbling block. The tinnitus feature is also available in the Orion instruments. The micon instruments with the tinnitus feature come in all different form factors. We have two different receiver-in-the-canal instruments (RICs), the Ace and the Pure. We have a complete line of behind-the-ear instruments (BTEs), including the Siemens Life, the Motion M and P, the Motion PX and SX, and the only waterproof instrument on the market, the Aquaris. We have recently introduced the Nitro, which is our super-power BTE that will also have the tinnitus feature available. Not to forget, we have Insio, which is our complete line of custom instruments. We do have the tinnitus feature available in everything from a completely-in-the-canal (CIC) to an in-the-ear (ITE), and in all performance levels.
References
American Academy of Audiology. (2000). Audiologic guidelines for the diagnosis and management of tinnitus patients. Retrieved from https://www.audiology.org/resources/documentlibrary/Pages/TinnitusGuidelines.aspx
Jastreboff, P.J. (1990). Tinnitus retraining therapy. Progress in Brain Research, 166, 415-423.
Johnson, R. (1998). The masking of tinnitus. In J. Vernon (Ed.), Tinnitus: Treatment and relief (pp.164-173). Needham Heights, MA: Allyn & Bacon.
McFadden, D. (1982). Tinnitus: Facts, theories and treatments. Washington, D.C.: National Academy Press.
Seidman, M. D., & Jacobson, G. P. (1996). Update on tinnitus. Otolaryngologic Clinics of North America, 29(3), 455-465.
Tyler, R. S., Gogel, S. A., & Gehringer, A. K. (2007). Tinnitus activities treatment. Progress in Brain Research, 166, 425-434.
Cite this content as:
Powers, L., & Ramirez, T. (2014, March). Clinical management of tinnitus. AudiologyOnline, Article 12558. Retrieved from: https://www.audiologyonline.com