Learning Outcomes
After this course, participants will be able to:
- List the candidacy criteria for Nucleus cochlear implants and list the features and benefits of Nucleus technology for school-age children.
- Select appropriate remote microphone technology, including the Cochlear Mini Microphone 2+, for Nucleus cochlear implant recipients.
- List the benefits of Nucleus connectivity in the classroom.
Introduction
My name is Amy Donaldson and I'm a professional education manager in Cochlear's Professional Education Group. I'm excited to be with you here today since we're often asked to provide information to those who work with cochlear implants in educational settings. I expect that in addition to some educational audiologists and speech pathologists, this talk might be helpful to early intervention specialists, teachers of the deaf, and other teachers, aides, and even parents.
Some years ago, I was privileged to have the opportunity to work as an educational audiologist in the schools. On a daily basis, I was able to witness the hard work that school professionals do on behalf of children with hearing loss. My goal today is to bring you up to date on the current technology available for cochlear implants, as well as provide some tips that may help you support these students in the classroom. Here at Cochlear, we are committed to the continued support for professionals in the schools
Today, I will provide an overview of what school professionals should know about cochlear implants in children. We'll update you on the latest in Cochlear technology, including our remote microphone technology for Nucleus implants. Finally, I will provide you with some resources and support so that you feel you have what you need to move forward.
Cochlear's Mission
I like to start each presentation with a reminder of Cochlear's mission. Our primary goal is to help people hear and be heard. We do this by empowering people to connect with others and live a full life. In order to do this, we must do nothing less than transform the way people understand and treat hearing loss. To be successful at both of these goals, we must innovate and bring to market a range of implantable hearing solutions that deliver on a lifetime of hearing outcomes. At the heart of our mission is an understanding that the treatment of hearing loss has evolved over time and continues to evolve.
Why Consider a Cochlear Implant?
I'd like to start by reviewing cochlear implant candidacy and providing some information on cochlear implant use in children. When a child has a severe to profound sensorineural hearing loss (SNHL), hearing aids often cannot provide the audibility or clarity that a cochlear implant can. Powerful hearing aids may provide access to part of the speech signal, but the signal may not be complete or the access may not result in clarity of sound. Portions of the speech spectrum may be missing or may be unclear, and the child may be unable to discriminate especially high frequency speech sounds. cochlear implants, on the other hand, can provide a clear and consistent signal across the frequency spectrum. This access to the sounds of speech allows for development of speech and language abilities that can approach those of normal hearing children, especially if the implant is received early enough.
Outcomes for Children
There have been hundreds of peer-reviewed studies since cochlear implants were approved for children in 1990 that have shown the effectiveness of cochlear implants - far too many studies for us to discuss today. I'd like to go over some general things we now know about children with cochlear implants. First, early research into cochlear implants in children demonstrated that it was possible and even probable that children who are prelingually deaf could develop spoken language, especially if they were provided with an auditory/oral education (Waltzman & Shapiro, 1999). This was not always a given. If you go back and read some of these early studies, there's quite a bit of surprise at how well children were doing with their cochlear implants. In early studies, children with cochlear implants were often compared to children with lesser degrees of hearing loss who used hearing aids. Researchers found that they perform just as well, although they still both lagged behind their normal-hearing peers. Remember that at this time, children were often implanted at ages that we would now consider late, often four years of age or older.
As we learned more about the outcomes that were possible, larger groups of children were implanted at younger ages and several robust longitudinal studies were able to demonstrate that the earlier an implant is received, the better the spoken language outcome possible for the child (Ching et al., 2009; Niparko et al., 2010). This is something we consider obvious today, but it took several important research studies to confirm that this was not only true for children implanted under the age of four but under the age of two or even younger.
Current research on children with cochlear implants has focused beyond just speech and language performance. Studies have shown that the earliest implanted children with no additional disabilities can approach or equal their normal-hearing peers when it comes to speech and language (Ching et al., 2017). Beyond that, studies have found favorable outcomes for children with implants in the areas of social and emotional development, academic achievement, and reading skills. The large body of research that is available today leaves no doubt that cochlear implantation for children with severe to profound hearing loss should be considered the standard of care. Knowing this, and as stated in our mission, we want people to hear and be heard, but we have a challenge to meet. Given a birth rate of four million in the United States per year, and an incidence of hearing loss at about 1.7 per 1000 people, we can assume that about 6800 children are born with hearing loss every year in the U.S. Data suggests that about 15% of the children born with permanent hearing loss have losses in the severe to profound range (CDC, 2016). In other words, there are over a thousand children born across the U.S. each year with hearing loss in the cochlear implant candidacy range. With all that we know about the benefits of cochlear implants, only an estimated 47% of those who meet the candidacy criteria are treated in the U.S (Bradham & Jones, 2008).
Early Hearing Detection and Intervention (EHDI) Goals
In the United States, we have the Early Hearing Detection and Intervention (EHDI) program through the Centers for Disease Control (CDE). EHDI's goal is to improve the identification, diagnosis, and treatment of children with hearing loss such that all babies are screened by one month of age, diagnosed by three months of age, and referred to early intervention before six months of age. Since the beginning of the EHDI program, we've made enormous strides in screening babies for hearing loss at birth and providing early diagnosis. When I first started in the industry, it was the exception that a child was fit with hearing aids before their first birthday. Now, I would say that is the rule, although we all still encounter children who have slipped through the safety net of EHDI.
In an effort to be transparent about their progress on these goals, there is data about the EHDI program on the CDC's website. Let's take a look at some of that data and what it can tell us about candidacy for cochlear implants and how we are serving those children. In 2016, 3.7 million babies underwent hearing screening. About 65,000 babies did not pass their hearing screening. Of those 65,000:
- 53% were confirmed as not having a hearing loss
- 9.7% were confirmed as having a hearing loss
- 25.4% were reported as lost to follow-up
One of the challenges of the EHDI program is that we do not know what happened to the remaining 12% due to incomplete reporting from clinics or state agencies.
Let's take a closer look at the 6,000 children who were diagnosed with hearing loss through EHDI. Where are they now? According to the data reported, 66% were enrolled in early intervention and 19% were reported as lost to follow-up. Again, due to incomplete reporting, we do not know what happened with the remaining 15% of children. If you're interested, I would encourage you to check out the CDC website for more information on the EHDI data (https://www.cdc.gov/ncbddd/hearingloss/ehdi-data2016.html).
National Childhood Assessment Project (NECAP)
Thanks to EHDI, we know much more about identification and referral for follow-up than ever before, however, we are still missing information on outcomes for those children once they're referred. One program aims to fill this gap. The National Early Childhood Assessment Project (NECAP) headed by Christine Yoshinaga-Itano and her colleagues was created to improve follow-up for a minimum of six states by implementing a standard assessment battery for hearing impaired children age birth to four. In a recent talk, Dr. Yoshinaga-Itano estimated that only one out of every two children with hearing loss are followed through intervention to outcome.
Worldwide Utilization of Cochlear Implants for Children
While we in the U.S. have been improving our identification and referral of children with hearing loss, our utilization of cochlear implants remains low when compared with other countries For example, in Australia, utilization rates for children who are diagnosed with a severe to profound hearing loss prior to the age of two has been reported at 97%. In the U.K., the rate is reported at 90%. Germany is a bit lower at 65% and, the U.S. has one of the lowest rates in the developed world, with a utilization rate for cochlear implant in children reported around 50% (Sorkin & Buchman, 2015).
Within the U.S., utilization rates vary widely by state. While the overall rate is around 50%, some states have demonstrated higher utilization rates. Colorado is estimated to have an 86% utilization rate for profound hearing loss and a 71% rate for severe hearing loss (Sorkin & Buchman, 2015). North Carolina is estimated at a 61% utilization rate (Alberg et al., 2016). Unfortunately, this means that there are some states with utilization rates much lower than 50%.
Why are utilization rates lower in the U.S.? It may be that there is a lack of comprehensive and accessible information about cochlear implants at the time of diagnosis and referral. In a recent survey of parents with children who have received cochlear implants, less than one-third of these parents indicated that they received information on cochlear implant candidacy from their early intervention professional (Sorkin & Zwolan, 2008). This isn't surprising when you consider that hearing impairment itself is not a common disability for early intervention professionals. Of those children with hearing loss, an even smaller fraction are cochlear implant candidates. Clearly, we have a challenge to make sure we provide as much support and information possible to those parents and professionals at the time they need it most. We have made great strides in the outcomes possible for children with cochlear implants, but in the U.S., we still have work to do to make sure families and professionals know about their options.
A recent article by the American Cochlear Implant Alliance reported on the state of cochlear implantation in children. Their conclusion: "Rather than delivering comprehensive, evidence-based information on language development options, the U.S. system is heavily influenced by the individual state agencies’ approach to deafness and even by the individual perspective of the early intervention professional who provides services to families; hence there is great variability in the nature of information provided…such discrepancies in the accuracy and completeness of information provided lay the foundation for the relatively low rate of pediatric CI utilization in the United States (Sorkin & Buchman, 2016)." This presents not only a challenge but also an opportunity.
Candidacy for Cochlear Implants
As professionals who work with children who have hearing loss, we truly have our work cut out for us. Professionals in the schools work tirelessly as advocates for children with hearing loss. It is our role to support you so that together, we can transform how people understand and treat hearing loss. It is the role of the educational audiologist, the teacher of the hearing impaired, the speech pathologist, the deaf and hard of hearing liaison or even the special education teacher to educate families, schools, administrators and even healthcare professionals on the importance of early and appropriate implantation. That starts with knowing which children on your caseload or in your class might benefit from implant technology.
Nucleus Cochlear Implant Indications for Pediatrics
In Figure 1, you can see the candidacy criteria in terms of hearing thresholds. In order to qualify for a cochlear implant, children 12 to 24 months of age must have profound sensorineural deafness and demonstrate limited benefit from appropriately fit binaural hearing aids. Children who are older than two must have a severe to profound hearing loss and, if possible to test, a score of less than 30% on open set word testing. Determination of candidacy for children is a multidisciplinary task. It is recommended that any children who meet audiometric criteria are referred immediately for evaluation by an experienced pediatric cochlear implant center. If you do not know the nearest pediatric CI center in your area, please visit the Cochlear website where you can use the "Find a Clinic" tool to search for clinics in your area.
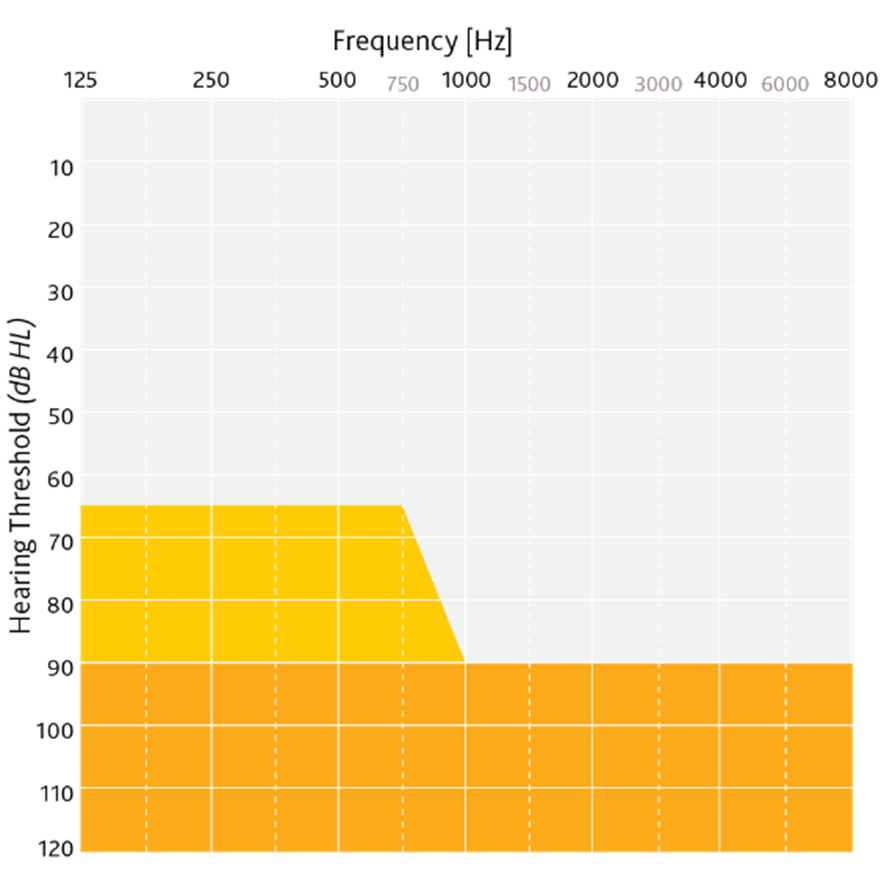
Figure 1. Candidacy criteria: hearing thresholds.
Considerations for CI Candidacy
Beyond the audiogram, I like to think of candidacy for cochlear implants as a continuum. On one end of the spectrum, there are children who are obviously not cochlear implant candidates (e.g., those with mild or moderate hearing loss). On the other end, there are children who clearly are suitable candidates (e.g., those with profound hearing loss). Sometimes, there are children who fall in the middle of this continuum, with some degree of hearing who may or may not be candidates, depending on their circumstances.
In addition to the audiogram, the following criteria should be taken into consideration:
- How well can the child hear all components of the speech signal?
- Are the child's speech and language skills progressing at a normal rate (e.g., six months progress in six months' time with hearing aids)?
- How consistently has the child used their hearing aids?
- What is the child's communication mode, or the communication skills of their family?
- What educational services have been provided in the past or are available in the future?
Determining candidacy can be much more complex than simply just looking at an audiogram. It can be beneficial for families to find out more about their child's potential for candidacy, even if they're not a cochlear implant candidate today. In my time in cochlear implant clinics, we saw many young children who were doing well with hearing aids and not within the candidacy criteria for an implant. Nonetheless, we were able to discuss the implant with the family and demystify the CI process so that if the child were to become a candidate in the future (either through expanding technology or worsening hearing loss), the family felt more informed and prepared.
One thing I have seen is that sometimes, professionals will innocently describe a child's hearing as "not bad enough" for a cochlear implant or express unwillingness to refer for a cochlear implant evaluation, feeling that a CI is only suitable for the most profoundly deaf. I'd encourage you to always consider setting children up for success no matter what happens with their hearing loss over time. Be careful of the words you use so that you are not fighting the perception that becoming a candidate for a cochlear implant is something to be avoided. This will help if a child becomes a candidate at some point down the road.
In the school environment, while you may have a child's audiogram, it isn't always obvious when a cochlear implant might be a better choice than hearing aids. It is critical not to wait until a child is demonstrating significant difficulties in school. Waiting until they fail a grade, or until a child who was previously mainstreamed is placed back in a smaller classroom is too long. The literature is clear that there is no benefit in delaying implantation once a child becomes a candidate.
Here are some practical suggestions of when you might send a school-age child (over age two) with severe to profound sensorineural hearing loss for a CI evaluation. Refer the child for assessment in the following instances:
- If they are not making appropriate progress in speech and language or auditory goals
- If they are falling behind their normal-hearing peers in school.
- If they are struggling with behavioral concerns, especially if there are new or worsening concerns (e.g., a previously well-behaved child now seems to be inattentive or frequently displays frustration).
- If a child is struggling to hear their peers and/or teacher(s) in all environments (e.g., they hear well in a one-on-one situation or a small group in a quiet room, but they struggle in a larger group or a noisy classroom).
Support for Families
Parents of children with hearing loss have a high degree of trust in their school professionals. They are looking to their teachers and therapists in school to be a source of information, emotional support, and act as a sounding board. Cochlear is committed to helping you fulfill this role and there are lots of resources available that might help your families find the support they need.
First, we have online resources available for families. Specifically for Cochlear, there are Facebook groups and our website, as well as our online community where families can find stories about people like them and meet with volunteers. That community is called Hear and Now. There are also some wonderful external organizations, such as the AG Bell and NCHAM.
There are also written resources available. The Cochlear Resource Guide is available in English, Spanish and French. A print copy can be easily requested by clicking the link on our website. I've also included an electronic copy of the most recent guide in the handouts for this course. You'll find that this guide is not just about Nucleus technology, but it's intended to be a comprehensive guide for families on hearing loss and treatment.
Sometimes, it may be best to provide families with more personalized support. That's where the Cochlear Concierge comes in. I'd recommend connecting any families who are going through the cochlear implant evaluation process, either in the learning stages or all the way to the point where they have to choose accessories, to connect with our concierge team either by phone or email. These dedicated professionals (many of whom are audiologists, recipients, or parents of recipients themselves) are available for any type of question or support.
Finally, there are local support groups and Cochlear volunteers on hand to provide support. In addition to groups like Hands and Voices or AG Bell, Cochlear also has local chapters of support groups. Your Cochlear Concierge or local engagement manager can connect families with local volunteers that are in similar circumstances. You can also find information about Cochlear events on our website or by following us on social media.
Hear Your Way: The Cochlear Nucleus Implant System
Now I'll discuss Nucleus technology you might see in the classroom setting. There are two main components for a cochlear implant system: the internal device (the Nucleus Profile Implant) and the sound processor. Our current portfolio of sound processors includes both the Nucleus 7 Sound Processor and the Kanso Sound Processor. The following video shows how the components work together to produce sound for the child.
How the Nucleus Cochlear Implant System works. The Nucleus Cochlear Implant System is designed to mimic the functions of the human ear. Sound travels to your ear and the sound processor, which sits behind the ear. The microphones on the sound processor pick up sounds and the processor converts them into digital information. This information is transferred through the coil to the implant just under the skin. The implant sends digital sound signals down the electrode into the cochlea. The hearing nerve fibers in the cochlea pick up the signals and send them to the brain which is translated as the sound you hear. Unlike a hearing aid that simply amplifies sound, cochlear implants send sound directly to the hearing nerve and onto the brain.
This video is available on our website and on our YouTube channel, so that you can easily access them to share them with other professionals or families.
Cochlear Implant Surgery
Considering surgery is a big step for families. The procedure for a cochlear implant has changed a lot over the years and it is now considered to be quite a routine procedure, similar to most other ear surgeries. It lasts about two to three hours, in most cases. The surgery requires minimal or no hair shaving and the incision is quite small. Usually, the scar is hidden in the crease behind the ear. Most children are a few days off of school and there is a fairly quick recovery time with little or no pain management needed. Major complications are very rare, especially in the hands of an experienced surgeon and in children with no anatomical abnormalities. Sound processor activation will usually happen about three to four weeks after surgery.
Pictured in Figure 2 is an image of the Nucleus CI532 cochlear implant placed in the cochlea. You can see that it is a very thin electrode taking up a minimal amount of space in the scala tympani. It's also a perimodiolar electrode, which means that it is placed close to the center of the cochlea where the auditory nerves reside. This is the best placement for a cochlear implant. Research studies have shown that placement in the scala tympani results in better performance and perimodiolar placement means that less current is needed to produce a sound for the child.
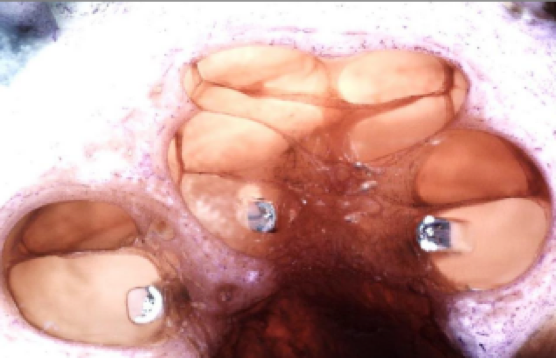
Figure 2. Image of the Nucleus CI532 implant placed in the cochlea.
Finally, it is important to consider MRI safety. Throughout a child's lifetime, it is possible they may need an MRI. Current Nucleus implants are safe for MRI with the magnet left in place up to 1.5 Tesla, which is a standard MRI strength. Stronger MRI is possible with the magnet removed, which can be done in a safe, straightforward procedure. Cochlear believes that an easily removable magnet will always be the gold standard, as the technology for MRI expands into stronger and stronger Tesla machines. For that reason, Nucleus implants have always been designed with MRI safety as paramount.
Reliability
One important aspect of the internal device is that it must be reliable. Cochlear is proud of our track record of reliability. According to reporting by recognized industry standards, we have the most reliable cochlear implants ever made. Another key thing to consider is reliability over time. We often say it's relatively easy to make a device that's reliable for one year, but it's much more difficult to make one reliable over time. The CI24RE, or "Freedom Implant", has 12 years of reliability information. Over time, it's still the most reliable device available for recipients and this is no accident. Cochlear's commitment to quality and reliability of our internal devices leads us to strive for better and better reliability with each generation of device. If you are interested, Please explore our publicly available reliability report for more information about the reliability of our implants.
Nucleus 7 Sound Processor
Next, let's switch our attention to the processor worn on the outside. It is extremely important to note that while the internal device is designed for a lifetime, the external sound processors are upgradeable over time. Cochlear is proud to have a history of making our new external devices compatible with previous generations of internal implants. The Nucleus 7 Sound Processor was introduced in July 2017 and represents the smallest and only made for iPhone cochlear implant processor in the industry, delivering proven hearing performance (Figure 3). I'm pleased to note that the Nucleus 7 Sound Processor is now available for recipients of internal devices going back to the Nucleus 24R, which was released in 1998. As such, it is compatible with the vast majority of our recipients' devices, delivering an outstanding technology upgrade even for patients who were implanted 20 years ago. When families ask me about today's technology, I often like to mention that families who chose Cochlear 20 years ago now have access to technology that none of us could ever have expected. We didn't even know what smartphones were in 1998, but Cochlear now provides made for iPhone technology and smart apps. Imagine what the Nucleus recipients of today will have available for them in the next 20 years!

Figure 3. Nucleus 7 sound processor.
SmartSound iQ with SCAN
Nucleus 7 takes advantage of state-of-the-art sound processing technology available first from Cochlear. Over the years, Cochlear has developed a range of technologies for providing great outcomes in difficult listening environments for cochlear implant recipients. We also know that recipients don't like to change programs, so our solution is to provide these technologies to all indicated recipients in a way that maximizes their outcomes automatically. Further, these technologies are backed by research and represent the only automated pre-processing technology that's FDA-approved for children. SmartSound iQ can be used in children who are six years of age or older and are able to complete objective testing in quiet and noise and subjectively report what they are hearing. This represents a huge leap forward in speech understanding in noise, even for our youngest listeners.
SmartSound iQ includes the industry's first scene classifier called SCAN. SCAN continuously scans the environment and identifies six acoustic scenes: speech in noise, speech, noise, wind, quiet, and music. It then automatically selects the best input processing based on the recipient's environment. In this way, everyone gets access to the best of what we have to offer without having to think about it. Even our off-the-ear sound processor, the Kanso, has the best hearing performance possible in SmartSound iQ.
It's important to remember that cochlear implants are not just hearing aids with coils. They require their own types of sound processing strategies. Several of our features are specifically designed to work with cochlear implants. They take the best of hearing aid technology and then couple it with the best of cochlear implant technology to provide the best hearing performance to our recipients.
Made for iPhone
The Nucleus 7 also allows our recipients to Connect Your Way better than ever before. Nucleus 7 is the first and only made for iPhone cochlear implant sound processor. Bluetooth LE technology that is present in Apple devices gives us a simple, clear, a bilateral signal that can be streamed directly to the patient without anything in between. Think of all the auditory learning that can take place while direct streaming a podcast, or listening and talking to loved ones over FaceTime. Not only does this improve connectivity, but it also has the potential to truly improve lives.
Nucleus Smart App
While only the iPhone has the Bluetooth LE technology necessary for direct streaming of sound, recipients and caregivers can control and monitor their device with the revolutionary Nucleus smart app. These apps are now available on both Apple and Android devices. For a complete list of compatible smartphones, visit our website. The Smart App allows recipients to change programs, adjust volume, track their hearing through different logging, connect to wireless accessories, and even find their sound processor if it gets lost - a feature that comes in handy with children.
To clarify, it is currently not possible to stream directly from the phone with an Android device. Apple streaming is done through Made for iPhone hearing device technology. At this point in time, it is specific to the architecture of the Apple platform. In other words, it is Apple's technology that allows for direct-to-device streaming with their products. Future capabilities with the Android platform that may allow for direct streaming are certainly possible, and with Cochlear's commitment to future compatibility, we continue to explore all the possibilities that may exist for our recipients.
Kanso Sound Processor
In addition to the Nucleus 7, the Kanso Sound Processor is also available as an option for recipients. Many recipients receive two sound processors at the time of activation and they will sometimes choose one N7 and one Kanso. This is definitely something you may see in a classroom setting. The most important thing about the Kanso is that recipients don't have to sacrifice performance to get an off the ear sound processor. The Kanso has dual microphone technology with the same Smart Sound iQ technology as Nucleus 7 in a discreet and easy to use package. With several retention options available, the Kanso is a popular choice with many of our recipients. The Kanso is compatible with True Wireless technology (which we'll discuss shortly), however, it does not yet have an app and it is not yet made for iPhone.
True Wireless Accessories
In addition to the made for iPhone and smart app capabilities of the Nucleus 7, connection is also available to all Nucleus 7, Nucleus 6, and Kanso recipients through the True Wireless accessories. These require no neck loops or dongles, and nothing connected to the sound processor. They connect directly to the processor using a robust, 2.4 GHz signal, and they're available at no extra charge at activation of a new N7 or Kanso device. Our True Wireless accessories include:
- The Mini Mic 2+: This accessory provides direct access to someone wearing it. You can think of it as kind of an affordable and portable alternative to traditional FM systems.
- The Phone Clip: This accessory can be used to stream phone calls, music, or podcasts from any Bluetooth enabled device. While users of Apple iOS devices can do this directly from the Apple device, the Phone Clip can be used with any other Bluetooth enabled device, such as Android, to make the Nucleus sound processors truly made for all.
- The TV Streamer: This accessory allows the direct streaming of a high-fidelity TV signal directly to the sound processor.
Aqua+ for Nucleus 7 and Kanso
The Nucleus 7 and Kanso Aqua+ provide waterproof protection for swimming, surfing, and so much more for both N7 and Kanso processors. If you think of children playing in the pool, there is so much language occurring in that setting. The recipient's N7 Aqua+ affords them the opportunity to stay connected in water-related environments. The Aqua+ can be used in all types of water, and it is designed to be waterproof at three meters for two hours of use. You can check out our website for instruction guides and more detailed information about the use of Aqua+.
Choosing a Cochlear Implant
Choosing a cochlear implant is different than choosing hearing aids. To illustrate, consider that children may be fit with new hearing aids every few years. Each time, they might choose a new brand of hearing aid with different features being more important to them over time. In general, a hearing aid wearer has very little direct contact with the hearing aid manufacturer. They work mostly with the audiologist or the dispenser who fit their hearing aids.
In comparison, with a cochlear implant, the child will receive their implant sometime after their first birthday. If all goes according to plan, the same device will be their foundation of hearing for an entire lifetime. The external sound processor will be upgraded over time, but recipients can't choose to change brands. They're dependent on the company they choose to devise new technology and options designed specifically for them. Current features might be important to recipients, but that lifetime of support and innovation is just as important. They want to be sure to choose a company with a long history of technological innovation and one that is dedicated to its implant recipients. Perhaps the most relevant to our discussion today, the cochlear implant has to be compatible with different types of hearing aids (e.g., bimodal recipients) and different assistive technology over time. You want to be sure that the company you choose has a tradition of compatibility with the latest and greatest technology.
Using Remote Microphone Technology with Nucleus Sound Processors
Now that we've had a chance to get up to speed on the Nucleus sound processor technology available for your students, we're going switch gears and take a closer look at working with remote microphone technology with Cochlear implant recipients.
From the literature, we know that there are a lot of factors that affect language outcomes. In a large dataset from Teresa Ching and her colleagues, she looked at children with hearing impairment who used both hearing aids and cochlear implants (Ching et al., 2017). There were two sets of factors that had an impact: patient factors and technology factors.
Patient Factors
Patient factors are things that often we can't change but we need to be aware of so we can mitigate as much as possible. The first patient factor that affects language outcomes is early fitting of hearing technology, as early amplification and access to sound are critical for language development. The second patient factor is nonverbal cognitive ability. Thirdly, the level of maternal education also plays a role in language outcomes, with more recent studies suggesting that maternal sensitivity can also be important. Finally, early activation of the cochlear implant is another factor that can have a positive impact on language outcomes.
Technology Factors
Technology factors are things that we may be able to control by making the appropriate choices. Better signal-to-noise ratio and consistent audibility of speech sounds are both critical for success in language. Also, Ching and team found that using an evidence-based protocol for selection and fitting of technology, along with an intervention that encourages greater oral communication and vocabulary can have an impact on language outcomes.
For the purposes of this presentation, we will focus on the first two technology factors, since these are critical to learning language in the classroom: consistent audibility of speech sounds and better signal-to-noise ratio.
Consistent audibility of speech sounds. Language-rich environments are crucial for hearing children to reach developmental milestones (Hart & Risley, 1995). In order to develop language, it is critical for children to have consistent audibility of speech sounds so they can access the language and speech around them. Children who are deaf or hard of hearing require increased signal-to-noise ratio to access language in noisy environments. The technology we use with our students must ensure consistent access across a variety of situations.
Cristofari and colleagues conducted an interesting study with the Nucleus 6 Sound Processor using data logging with cochlear implant recipients (Cristofari et al., 2017). The data logging in the processor gave them the opportunity to measure different types of listening environments. They were able to look at the overall wear and use time, as well as how noisy the environments were.
The graph in Figure 4 shows how noise levels change for different age groups. The bars represent the time spent in speech in noise (i.e., trying to listen to speech with background noise present), which is the most difficult listening situation.
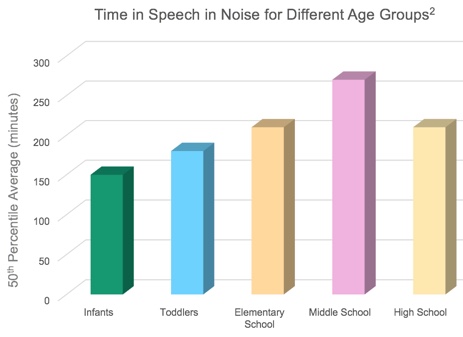
Figure 4. Time in speech in noise for different age groups.
Perhaps not surprisingly, the quietest environment was seen for infants, with noise levels steadily increasing until they peaked in middle school. In fact, the average middle school student is exposed to speech in noise 250 minutes per day (over four hours).
Better signal-to-noise ratio. Children with cochlear implants and hearing aids require an even better signal-to-noise ratio than children with normal hearing in order to achieve the same level of response. In a study by Caldwell and Nittrouer (2013), they tested children with normal hearing, hearing aids (HA) and cochlear implants (CI) on phoneme and word recognition. The normal hearing listeners recognized more words and phonemes at -3 dB SNR than the children with hearing aids and cochlear implants recognized at better SNRs. In fact, the SNR needed to be +3 to +6 dB before the performance of the HA and CI children was the same as children with normal hearing. Luckily, modern FM systems and remote microphone systems can improve the SNR for children with hearing aids and cochlear implants by up to 20 dB, which can help to equalize the playing field (Schafer & Thibodeau, 2006). There are a lot of different options for remote mic technology so let's take a look at some of the newer choices.
Mini Mic 2+ (MM2+)
The Mini Mic 2+ provides a unique option for children in the classroom setting. The small clip-on microphone is able to transmit speech and sound directly to the sound processor. It also has the ability to be plugged into any audio device using a 3.5 mm audio jack. It has telecoil capability to pick up any room loops and can also be changed to a conference mic setting simply by laying it flat on a table. This incredibly small and flexible device has a range of over 80 feet, allowing children access to sound in almost any educational setting.
Imagine a child in a classroom setting during a typical day. At the beginning of the day, they may be required to do work as a group with their peers, and later, they might need to work on a computer project and listen to the teacher's lecture. The Mini Mic 2+ can be easily placed in conference mode for the group work by lying it flat on a table, it can be connected to the computer with the audio cable, and it can connect as more of a traditional remote microphone on the teacher's lapel.
Evidence
The Mini Mic 2+ is portable and it has a lot of great features but, as an educational audiologist, we need to make sure it performs just as well as traditional remote mic systems before we can be confident in recommending it for use in a classroom setting. Let's have a look at some evidence-based research which demonstrates the effectiveness of the different remote microphone technology options for Nucleus recipients.
The first study is from Marian Jones. It was presented at the American Cochlear Implant Alliance (ACIA) meeting in 2017. They used the CUNY sentences in noise test to compare the Mini Mic 2+ (MM2+) and the Roger 20 remote microphones (RM) on the Nucleus 7 sound processor. The recipient used either the Roger or the Mini Mic 2+ in a booth with noise coming from all sides in three different conditions: 0 dB SNR, -10 dB SNR and -15 dB SNR. Using the sound processor on its own with noise reduction active, the results were less than 50% correct; however, with the addition of Mini Mic 2+ and the Roger 20, results were significantly better and about the same for both systems. At -10 dB SNR, the Mini Mic 2+ and Roger 20 demonstrated similar performances and both were much better than the processor alone. At the poorest SNR (-15 dB), there was great benefit from the Mini Mic 2+ and Roger 20, with the Mini Mic 2+ outperforming Roger in this instance. Overall, these results tell us that the Mini Mic 2+ is a good alternative for some students in the classroom, performing just as well as more traditional and expensive adapter remote microphone systems (Jones, 2017).
Multiple studies demonstrate the benefit of remote microphone technology (specifically the MM2+) when used with Nucleus cochlear implants (Razza et al., 2017; Wolfe et al., 2015). In one study from Jace Wolfe, they looked at the use of Nucleus 6 with Roger 20 and Mini Mic 2+ (Wolfe et al., 2016). Again, recipients showed significant improvement over the non-remote mic condition for both systems, with the results being fairly equivalent between the two systems. These results mean that professionals can choose systems that work best for their students in many different ways without worrying that they are compromising on performance.
Selecting Remote Microphone Hearing Assistive Technology (RM-HAT)
With all the technology available, professionals and schools are given the opportunity to customize the solution for each individual situation. Let's take a look at some of the factors you might consider when trying to customize a solution.
Considerations When Selecting a Remote Mic
There is a lot to consider when selecting a remote mic in the classroom. To assist with our choice, AAA has set forth guidelines for remote microphone fitting for school-age children. According to AAA, there are three main considerations:
- Acoustic Environment
- Academic Setting
- Student Characteristics
The first consideration is the acoustic environment. How loud is it? What is the background noise like? What will the child need to hear during the day? The second consideration is the academic setting. Modern classrooms can be dynamic places. The days of children sitting in rows and listening to the teacher are long gone. Today's classrooms might include small groups that form and reform, the teacher acting as a coach while the students do the talking and teaching. There may be multi-media experiences with videos, computers, or music or individual project work where children are required to gain knowledge and experience from each other. Given this new reality, modern remote mic systems must be flexible and easy to use. Students must be able to switch easily between listening to peer groups and listening to the teacher. Systems should be easy to set up and use, even for teachers with no prior experience with remote microphones.
The third consideration is the student's own characteristics. What is their cognitive level? Have they had any past experience with remote microphone technology? As any professional who works with children who have hearing loss can tell you, if you don't have the student's buy-in for a remote microphone system, it will be a constant battle getting them to use it, let alone succeed with it. For a more in-depth discussion of these considerations, check out AAA's remote mic guidelines which are available online. They provide a comprehensive look at the selection, fitting, and verification of remote mics for both hearing aids and implants.
Available Options for Children with Nucleus Technology
With all those considerations, let's outline the options that are available for children with Nucleus technology (Figure 5).
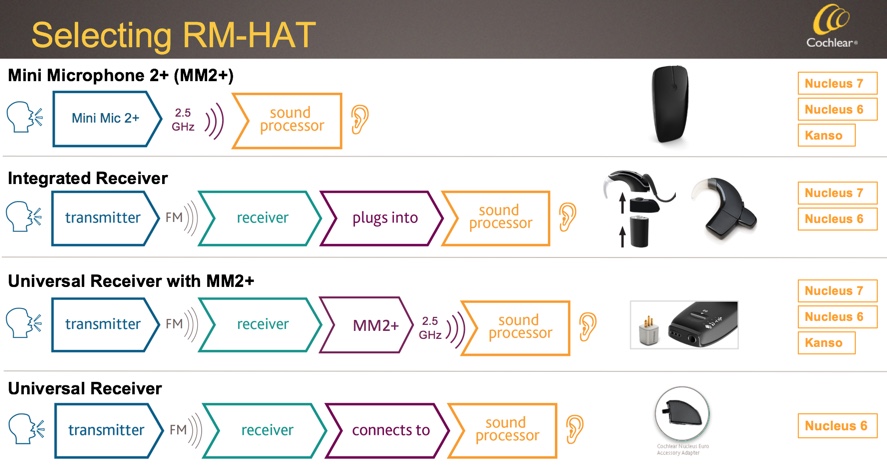
Figure 5. RM-HAT options available for children with Nucleus technology.
The first option is perhaps the most straightforward. The Mini Mic 2+ streams directly to the sound processor. This option is compatible with the Nucleus 7, Nucleus 6, and Kanso devices. It's also compatible with the most recent GN ReSound hearing aids, either bimodal recipients who wear a CI and a hearing aid, or even children who use hearing aids that are in the same classroom as a child with a cochlear implant.
The next option for students would be an integrated receiver. These are available from Phonak (the Roger 20) and connect directly to the sound processor. The teacher would then use the Phonak transmitter, such as a Roger Pen or the Inspiro, to transmit a signal to the sound processor. Integrated receivers are available for the Nucleus 6 and Nucleus 7 sound processors.
Another option available to recipients is to use a universal receiver through the Mini Mic 2+. This is a cost-effective option since only one universal receiver is needed for a Mini Mic 2+ that can transmit to multiple processors and users. It does require that the recipient know how to start and stop streaming with their device. In a traditional remote mic system, the teacher can control access to the remote mic by turning the transmitter on and off, but whenever you are using the Mini Mic 2+, the recipient must start and stop streaming on the processor. One positive aspect of this setup is that it can be extremely flexible, allowing the student to easily choose between the teacher's transmitter (i.e., the traditional FM), the Mini Mic 2+ in conference mic mode, an external input, or even maybe giving the Mini Mic 2+ to a particular soft-spoken peer. This option is available for Nucleus 7, Nucleus 6, and Kanso.
Finally, there's an option available for Nucleus 6 recipients that allows a universal receiver to plug into a sound processor through a euro adapter. Again, this option is only available for Nucleus 6.
Wireless Guide
With all the different options available for Nucleus technology, I wanted to draw your attention to a new wireless guide that we developed. It includes information about the selection of remote microphones for Nucleus recipients, and it contains information about all of the currently available sound processors with step-by-step guides on how to connect them. It also includes troubleshooting information, as well as information about using other kinds of wireless in the classroom, such as smart apps or made for iPhone technology. This guide is provided in your handouts in electronic format. There are hard copies available if you need them, which can be obtained by contacting your local Cochlear representative or Cochlear customer service.
Fitting and Verifying RM-HAT
Here is a checklist of the fitting and troubleshooting tools that you might need to fit remote microphone devices:
- Wireless Solutions for Nucleus and Baha Recipients (FUN3118)
- Smart App (for Nucleus 7 and Baha 5)
- Remote Control (CR310 for Nucleus 7 or CR210 for Nucleus 6)
- Remote Assistant (CR230 for Nucleus 6)
- Monitor Earphones (Nucleus) or Test Rod/Softband (Baha)
- User Manuals for all equipment
- Videos (www.youtube.com/user/cochlearamericas)
I would recommend keeping our new Wireless Solutions Guide handy if you're working with Nucleus recipients. The smart app, remote controls, and remote assistants may also be helpful for you, although they're not always necessary. Monitor earphones are useful for monitoring fitting (we'll discuss how they connect and work in a moment). Finally, don't forget that the user manuals for all of our equipment, as well as a lot of videos on how to use them, are available on our website. Answers to many frequently asked questions can be found in the information on our website.
Fitting Considerations for Remote Microphones
There are several different considerations when fitting any remote microphones to Nucleus technology. These considerations are mixing ratio, gain, activation of the remote microphone, and monitoring.
Mixing ratio. This refers to how much sound comes from the remote mic versus the processor itself. This can be set in the Nucleus 6 and Kanso using the remote assistant, and it can be set in the Nucleus 7 using the smart app. Generally, for most remote mic settings, this is set at a 1:1 ratio so there's equal input from the processor and the remote mic.
Gain. With most modern remote mic systems, the Roger system included, there are settings that determine the gain. The Roger has an "EasyGain" and "CI module" settings. I'd encourage professionals to pay close attention to the settings recommended by the device manufacturer and consider adjusting the gain if needed. If the remote microphone is too soft or not loud enough, the gain setting may be one that's overlooked as a possibility.
Activation of RM. The RM can be automatically activated when the transmitter is switched on, like with the Roger system. Or, it can be manual, such as with the Mini Mic 2+, where the recipient is controlling their streaming and whether or not they're listening with the Mini Mic 2+. The type of remote mic chosen will determine how the RM gets activated. The child's age and developmental level may influence your choice in this regard.
Monitoring. Finally, professionals should consider how the device use will be monitored. We'll discuss some of the different ways to confirm whether remote microphone fittings are providing benefit (e.g., visual verification using the lights on the processor or the app or objective testing that can be used to communicate benefit to the student or IEP team). This is a consideration that requires advanced planning. If close monitoring is going to be required, the professionals in contact with the student on a daily basis have to be involved early on in the decision-making process.
Confirmation of Remote Microphone (RM) Fittings
In almost all cases of remote microphone fittings, there are many different ways to confirm that a student is hearing with a device. It depends on the equipment you have available and the child that you're working with.
Check processor lights. First, the easiest and most obvious choice is to take a look at the processor lights. You can use the new wireless guide, the website, or the instruction manual for the processor to see what the lights should be doing. Remember that there is a special setting for the lights to be active all the time that is enabled in some children's processors, but for older children, it may not be enabled, and their lights may just be set for an alert. You'd have to talk to the child's clinic to find out which is the case, or you can just tell by the fact that the light is not on all the time. In general, blue lights indicate that there is some kind of wireless connection or streaming with the N7 or Kanso.
Check Smart App or remote. Another way to check the fitting is to use the Smart App for the Nucleus 7 or the remote assistant for the Nucleus 6 or Kanso. Those devices will show you not only that a remote mic is connected, but whether it's receiving sound or not, which can be incredibly helpful. You can also use the Smart App and remote assistants to set the mixing ratio for the processor. The Nucleus smart app is especially helpful; it could be loaded to the teacher or school professional's iOS device and then paired with the student's processor very easily. There's a caregiver mode that can be chosen to indicate that the user of the app is not the student themselves or the parent, which is helpful to ensure there are no privacy concerns. You can check out instructions on how to pair the Smart App on our website or YouTube channel and the information is also in the wireless guide. The good news about using the Smart App is you don't have to purchase a remote assistant to be able to connect to a Nucleus 7.
Listen with monitor earphones. To give you a better sense of what the child is hearing through the remote microphone, consider the use of monitor earphones. This option has the advantage of being able to relay exactly what the child is hearing. For example, if the child is reporting static or poor sound quality, a quick check of the sound through the monitor earphones will help you determine the source of the issue.
Perform a behavioral listening check. Finally, there is a low tech way that many professionals use to check a fitting: the behavioral listening check. An easy one is the Ling 6 Sound Check where the student can just repeat back or identify what they're hearing through the remote mic. I did want to mention that if you choose to test this way, make sure that you are providing the sound where the child cannot hear through their environmental mic, but only can hear you through the remote mic. I often used to do this testing from behind a closed door to make sure that the child was only hearing through the remote mic, but you really need a partner to do this because they have to record the child's responses. If your partner can hear you through the closed door, the child can probably hear you as well.
Monitor Earphone Adaptor
Figure 6 shows a close-up of the monitor earphone adaptor for the Nucleus 7. It's very easy to use. It can be connected to listen to the processor by itself, or you can connect it in conjunction with the Roger 20 if you're using that to listen to the output from the remote mic system. Whenever I've been asked to help with troubleshooting, (e.g., with a child who is reporting some kind of sound or intermittent signal), I always recommend listening to the sound processor and remote mic connected to the sound processor before doing anything else. I have found that what can be reported as static could be something as simple as a transmitter mic that's rubbing against the teacher's shirt on a lanyard. Sometimes, "intermittency" is just the adaptive signal for the Roger 20 at work in a very quiet room where it lowers the gain for the transmitter. In addition to looking at what the lights are doing, or using the Smart App or the remote, I'd strongly recommend keeping the monitor earphones on hand for any troubleshooting.

Figure 6. Close-up of the monitor earphone adaptor.
Behavioral Evaluation of RM-HAT Fittings
Now that we've selected the remote technology and fit it to the student, we need to ensure we are evaluating that fitting and that we are giving the student the support that they need. There are lots of different ways to evaluate a remote mic fitting. While you can verify fittings electroacoustically, and there is now a protocol set up to evaluate CI fittings, the most common way to evaluate fittings remains behavioral testing (Schafer et al., 2013; Nair et al., 2017).
The pyramid in Figure 7 gives you an overview of the different kinds of tests that might be used, from the easiest to administer ("Can you hear me now?") all the way up to full testing in a sound booth to comprehensively determine the benefit of the remote mic. Remember that you can also use questionnaires for the student or for the teacher to measure benefit. Once again, I'd recommend the AAA guidelines for a lot of great detail about how to complete the booth testing with the remote mic system. Their protocol contains detailed information about the setup and the test procedures you can use. The Functional Listening Evaluation (FLE) from Cheryl DeConde Johnson is another great tool that I used to use quite a lot. It's a great option when booth testing is not available to you, or if you want a more of a real-world objective test of how a student is performing with the remote mic system. In my experience, the FLE is a great tool, not only to help you objectively measure what benefit the system is providing but also to demonstrate that benefit, perhaps to a student who's reluctant to wear their remote mic or a teacher who doesn't understand the benefit. Information on how to do this test can be found on Cheryl DeConde Johnson's website (www.successforkidswithhearingloss.com) or by entering “functional listening evaluation” into a search engine, such as Google.
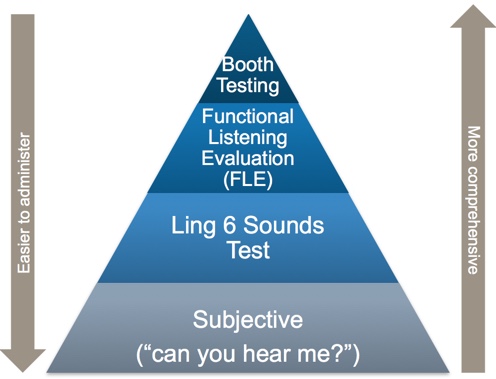
Figure 7. Behavioral evaluation of RM-HAT fittings.
Regardless of the methods that you use, some type of objective testing is valuable to confirm the benefit the student is receiving. If there are any questions at all that a remote mic setup is not working well, objective testing will give you the data and information you need to make an informed decision about its continued use. In my experience in the schools, I found this objective information to be absolutely invaluable to either confirm benefit or help me with troubleshooting. Children with cochlear implants are no different than children with hearing aids in this regard, and the same evaluation tools can be used with both.
Tools and Resources
Cochlear is now offering two different Classroom+ Kits for our school partners. The purpose of these kits is to package items specifically for schools so they not only come with the equipment you need but also the guides and info to help you use that equipment more effectively.
The first kit is the Classroom+Monitoring Kit. The cost for this kit is $185.00 and it includes the monitor earphones for the Nucleus 5, 6, and 7 along with a lunch box for storage and a luggage tag to help you keep track of everything. This kit is great for those of you who want the equipment to help monitor your remote mic fittings.
The second kit is the Classroom+Connectivity Kit. It includes the Mini Mic 2+, the lunchbox for storage and luggage tag, along with some brochures for use. The cost is $335 (essentially, the cost of a Mini Mic 2+). This kit is great for those of you who want to try the Mini Mic 2+ with students, or just have an extra one on hand for troubleshooting. Each of the items in these kits can also be purchased separately. You don't have to purchase them as part of a kit. The brochures are available at no charge. You can contact our Procare customer service team for information about how to order (procare@cochlear.com or 1-877-883-3101).
There is also a multitude of resources available online. Our main website (www.Cochlear.com/US) contains user manuals, instruction videos, and information about each of the processors and accessories available. If you click on "For Recipients", you'll find the support pages for each of the individual processors. We also have a section on our website that's designed for self-service by families called "Cochlear Family" (www.cochlear.com/us/cochlear-family). It's kind of a "one-stop shop". Recipients can log in, they can see warranty details, ask for a replacement equipment, get specific information about their device, and they can order parts and accessories from the Cochlear store. I'd recommend that you encourage the recipients and families you work with to take advantage of this resource.
Another online tool is Communication Corner (www.cochlear.com/us/communication-corner). This is a site that contains all of our rehabilitation resources. You can customize a program for the child you're working with based on their age and experience level. You can also get ideas for therapy, either at school or at home. I encourage you to check this resource out if you work with aural rehabilitation of children with hearing loss, not just those with cochlear implants.
Our YouTube channel (www.youtube.com/cochlearamericas) includes recipients' stories, videos about everything from choosing an implant to upgrading as well as all our instructional videos. By following us on social media (Facebook, Twitter, and Instagram), you can stay updated on what's new with Cochlear.
Finally, I'd like to introduce the Concierge and Volunteer Team. Our Cochlear volunteers are people who have walked in the shoes of the families that you work with. They are there to support them on every step of the journey. They can answer questions about surgery, about candidacy, about considering an implant, and help them with the selection of accessories before surgery. You can feel free to connect your families to the Concierge by phone (1-877-897-4474) or email (concierge@cochlear.com).
Video: Growing up with Cochlear
I'm going to wrap today's course with the following video that features recipients talking about their experience.
- My name is Kristen and I'm 18 years old.
- I'm Megan and I'm 16 years old.
- I'm Lexie and I'm 13 years old.
- I'm Dillon and I'm 15 years old.
- I'm Karen, I'm 14 years old.
- I got my first Cochlear implant when I was one year old, and my second Cochlear implant when I was four years old.
- We're brother and sister. I was three and three and a half and Dillon was two and two and a half.
- I got my first one when I was 18 months and I got my second one when I was seven.
- When I was one-year old I got my first one, and my second one, I was five years old.
- Being friends with all these people that are deaf have been amazing because it helps me feel like I'm less alone in the world.
- You're not alone.
- Mine's pretty cool, right?
- These are the sisters I never had. We grew up Cochlear!
- [Interviewer] How many times have you guys upgraded your processors?
- Oh, gosh.
- Okay, alright.
- Okay, Kristin, you can go first, I gotta do the math.
- Oh no, I got this, okay.
- [Megan] We all upgraded to the Kanso and it's amazing.
- It's just nice in that you can't even see mine right now, can you? And so I like it that way.
- Every teenager is self-conscious about something. So in, let alone being a deaf teenager, that's also another thing to be self-conscious about. So it helps with that. Music is definitely one of my favorite sounds.
- Some kinds of music, not all of them.
- One Direction, Five Seconds of Summer.
- Ed Sheeran.
- Yeah, I could go on, yeah. Fall Out Boy.
- Justin Bieber.
- Yeah.
- No, I'm sorry, I'm not on the Bieber train. The phone clip is by far my favorite wireless accessory. It's within enough distance to my phone in my back pocket and my phone clip in my backpack that I can walk around school all day listening to music and listening to music in class.
- And not be in trouble for those times.
- Yeah, yeah.
- And not get in trouble for headphones.
- I will be the first one to admit I do listen to music in class and my teachers don't know but it's okay, I'm passing all my classes.
- Yeah.
- My favorite is the Mini Mic.
- Mini Mic is better for more teacher-classroom situations.
- The teacher would have it on them or, like, a necklace on them or clip it on them, like on a shirt.
- Like, the Mini Mic is a whole lot more subtle than a lot of traditional FM systems I've used in the past.
- If you're in the cafeteria and it's really loud and you just want to, like, talk with something about like a test coming up, it would be a one-on-one conversation because all of this sidetracks. This is all out and it's just me and my friend.
- I like the TV streamer.
- I really like it because I can turn my TV on mute and it still streams to my processor so that everybody else in my house doesn't hear that TV.
- Well, like, I recommend to get Cochlear implants because, like, it's probably the best thing that's ever happened to me because I wouldn't be standing here right now and I wouldn't have these amazing people right beside me right now, so.
- Yeah, having the Cochlear implant has completely changed my life and I don't know where I would be without it. It's been one of the biggest blessings that I've ever had and I'm so thankful every day to have it.
- The Cochlear implant changes your life, like Kristin said, and it also opens up new doors and new windows of opportunity that you would have never had before if you, if you had just, you know, stuck with hearing aids or hadn't gotten a cochlear implant, you'd be missing out on a lot.
References
References are cited on the slides in the course handout.
Citation
Donaldson, A. (2018). Classroom+learning series: Nucleus technology in the classroom. AudiologyOnline, Article 23938. Retrieved from www.audiologyonline.com


