Learning Outcomes
After this course, participants will be able to:
- Determine BAHS candidacy using the audiogram
- Explain the benefits of treating conductive/mixed and unilateral profound hearing losses using a bone conduction device
- Define contraindications for BAHS surgery
- Ascertain whether a patient is a candidate for a bilateral or unilateral fitting using the audiogram
- State the impact of low MFO on sound quality and explain why increasing the MFO of BAHS devices benefits all users
- Indicate the effect different methods of sound transmission can have on output and outcome
Introduction
The agenda for today's presentation includes the following topics:
- BAHS Principles
- BAHS Candidates
- Advantages of BAHS device
- Contraindications for surgery
- Bilateral Conductive and Mixed Hearing Losses
- Ponto 3 Super Power
- The Importance of Increased MFO
- Methods of Sound Transmission
- Skin Drive and Direct Drive
Although there are different terms used in the industry (e.g., BCD, bone conduction devices), for the purposes of this course, the acronym BAHS (bone anchored hearing system) will be used to distinguish Oticon Medical's bone anchored device from a competitor's product.
BAHS Principles
The Ponto is Oticon Medical's bone anchored hearing system. We named our system "Ponto", which is Latin for "bridge". We feel that our BAHS devices are a bridge for the hearing impaired to sound.
I would like to start with a brief video, highlighting the main components of the Ponto BAHS system.
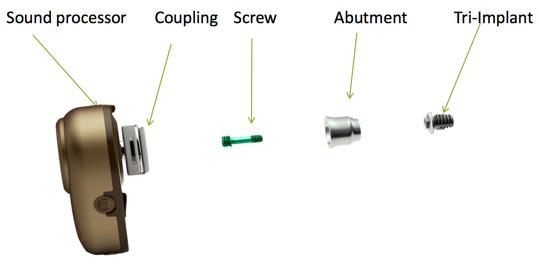
In Figure 1, we see the main components of the Ponto BAHS. These components include the sound processor, the coupling that attaches to the abutment via a screw, which is then connected to the tri-implant and implanted into the bone. The overall process can be described as follows: the external sound processor takes the acoustic sound signal from the environment and transforms that into vibrations. The sound processor is attached to the abutment, which is connected to a very small titanium implant, which is secured in the bone of the skull. That direct contact transfers the vibrations through the skull bone to both cochlea. There is some slight attenuation by the bone, so it is quieter in the side opposite to the fitting. In general, bone does not attenuate sound very well, so the cochlea are not very well acoustically isolated. The abutment comes in different sizes, depending on the patient's skin thickness. The implant comes in different sizes too, depending on the bone thickness.
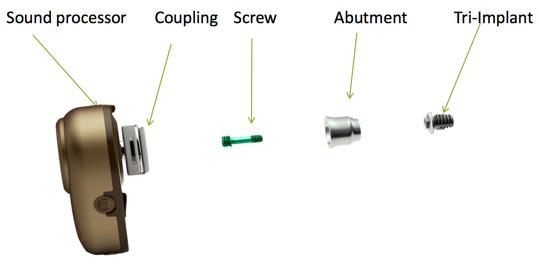
Figure 1. Components of BAHS devices and implant.
This is all possible through a natural process called osseointegration, whereby the bone itself begins to grow onto the titanium implant, creating a strong physical connection between them. This occurs because the bone cells naturally want to integrate with the titanium implant. As a result, the direct route for sound transmission is established. Osseointegration is a property of titanium, and it was first discovered by Professor Per-Ingvar Branemark in the 1950s, through his work with dental implants. Ultimately, this process was successfully adapted for use in bone conduction.
BAHS Candidates: Conductive and Mixed Hearing Loss
Who are the candidates for these devices? There are two main BAHS candidacy indication categories and one secondary indication category. Audiologically speaking, patients can be fitted with a Ponto system if they have conductive and mixed hearing losses, or if they have a unilateral profound hearing loss, also known as single-sided deafness (SSD). The secondary indication category includes patients who have other physical characteristics or other medical conditions that make wearing a conventional hearing aid impossible.
What information do we need to see on the audiogram to help us determine if an individual is a candidate for a bone anchored system? The first question we need to ask is if the device would be able to compensate for the inner ear hearing loss. This is obviously a key indicator for a BAHS fitting. To find this out, we examine the patient's bone conduction threshold. For a patient to be able to use a Ponto system, their BC thresholds can go up around 65 dB HL, on average. It's easy to calculate this average: you add up the thresholds, the four individual frequencies, and divide by how many there are. If it's less than 65 dB HL, then we can go with Ponto.
The second question in determining candidacy is a bit more complex: Is the use of a bone anchored device a better solution than traditional hearing aid? Research has shown that if the patient's air-bone gap is on average, greater than 30 decibels, their speech recognition scores will likely be better than conventional hearing aids (Mylanus, van der Pouw, Snik & Cremers, 1988; de Wolf, Hendrix, Cremers & Snik, 2011). However, it is important to remember that the answer to this second questions is not a requirement; it is simply a supportive indicator of benefit. It is not a hard and fast rule. If the patient had an air-bone gap that was not quite 30 dB HL, it would still be worth trialing a BAHS, as they may still obtain a benefit.
Calculating Candidacy
The two items that need to be calculated to determine BAHS candidacy of someone with conductive and mixed hearing loss are the average BC threshold and the average air-to-bone gap. First, to determine the average BC threshold, calculate the average BC response at .5, 1, 2 and 3 kHz. The average BC that we can fit to is up to 65 dB HL. Add up all of these BC responses and divide by the quantity to obtain the average. The second criteria we need to look at is the average air-to-bone gap (ABG). First, calculate the average between the AC and BC responses at .5, 1, 2 and 4 kHz. The average ABG should be around 30 dB HL. Remember that this is just a rule of thumb.
Advantages of a BAHS Device
The air-bone gap is closely tied to the advantage of the BAHS device and how it confers an advantage to BAHS candidates over hearing aids. A hearing aid needs to provide more gain as compared to a bone anchored device for the same hearing loss, as it needs to take into account and overcome the air-bone gap. As it delivers sound through air conduction, via the ear canal, the middle ear, the bigger the conductive component (shown by a wider air-bone gap), the more sound is lost before it even reaches the cochlea. Which means even more gain is necessary just to reach the patient's threshold.
An analogy that I like to use to explain this is to think about putting earplugs into your ears to simulate a conductive hearing loss. In order for you to hear me, I would have to shout, because I'm using the very pathway that is blocked. If I were shouting, my voice would be distorted. The hearing aid is in a similar position. However, a bone anchored hearing aid bypasses the ear canal completely. It doesn't vibrate the eardrum or the middle ear: it directly stimulates the cochlea via bone conduction, using a completely different route. As such, it does not have to overcome the conductive element of the patient's hearing loss (in this case, an earplug). This means it uses less gain in compensating for the hearing loss, compared to a hearing aid, and is thus able to deliver a better sound quality.
Traditional Hearing Aid vs. Bone Anchored Hearing Aid
Let's take a look at this bone anchored advantage. As I said, a high amount of gain can cause distortion in the signal delivered to the patient, as the hearing aid is pushed close to its limit more often. We know from life, if you push anything close to its limit all the time, it might not work at its best. Also, this higher gain needed by a hearing aid can cause problems with feedback, just as a louder sound delivered through the loudspeaker can leak out of the ear canal and be picked up by the microphone of the hearing aid. I'm sure many of you are familiar with the high pitch feedback noise which occurs when you place a microphone near a speaker. This is the same concept. As such, a tight earmold is used to prevent sound from escaping the ear. This tight earmold, for a lot of people, is quite uncomfortable. As the BAHS device does not have to compensate for the air-bone gap, it uses less gain, which leads to better sound quality and fewer issues with feedback. As an added bonus, the sound is transmitted by vibration through the bone, so the ear canal is completely clear. This could be especially useful for patients who have chronic ear infections, as it keeps the air going through the ear canal.
Example Candidates
Patients who have any of the following conditions may make good candidates for a bone anchored device:
- Otitis media with effusion (OME)
- Chronic otitis media
- Aural atresia/Microtia
- Otosclerosis
- Traumatic injury to middle ear structures
- Ossicular disease
- Cholesteatoma
For the purposes of today's session, we will be focusing on the first three conditions.
Otitis media with effusion. For the majority of this webinar, we will be talking about an abutment level device; however, it is possible to use a bone anchored device temporarily via a soft band (an elastic band around the head). The soft band can be very useful with the condition known as otitis media with effusion (OME). In most cases, OME is a transient disease, affecting mainly children. Most children recover spontaneously or with surgical treatment (grommet insertion). However, in some patients, OME can be a fluctuating, semi-chronic condition (e.g., in those with Down Syndrome or cleft palate). If OME is treated with a traditional BTE hearing aid, the hearing aid would need to be constantly refitted as the hearing fluctuates. If this condition were to be treated with a bone conduction device, it would clearly and directly stimulate the cochlea, with no refittings necessary.
Chronic otitis media. Chronic otitis media is a long-standing, persistently draining condition that may involve perforation of the eardrum. In patients with chronic otitis media, BTEs with occluding earmolds are contraindicated, as they may have an adverse effect on ear discharge (because air isn't getting to the ear, it can exacerbate the infection). Left untreated, chronic ear discharge may lead to cochlear damage (Papp, Rezes, Jókay & Sziklai, 2003). While BTEs are not a safe choice, percutaneous BAHS can be used with favorable outcomes (Snik et al., 2005). Literature has shown that replacing BTEs with BCDs had a significant positive effect on ear discharge (Macnamara et al., 1996; Mylanus et al., 1998; McDermott et al., 2002). The observed reduction of infections resulted in fewer outpatient visits -- an important consideration for patients, in terms of convenience, and for hospitals, in terms of cost-benefit of treatment (Hol et al., 2004).
Aural atresia/Microtia. A systematic review of over 107 papers related to aural atresia was published the Journal Otology and Neurotology (Nadaraja, Gurgel, Kim & Chang, 2013). Patients with aural atresia/microtia are ideal candidates for a BAHS device. Some of these patients can undergo surgery for repair. To define a successful outcome after atresia repair, a rather broad criterion is used. If the remaining air-bone gap is 30 dB or less, the outcome is considered sufficient. A meta-analysis of six different studies showed that only 57% of patients fulfilled this criterion one year post-op (Nadaraja et al., 2013). Thus, many patients may still need amplification post-surgery (Evans & Kazahaya, 2007). Another analysis by Nadaraja and colleagues found that atresia patients who are fitted with BAHS require fewer follow up visits and have fewer complications after surgery. Again, this proves to be a more cost-effective measure, due to a reduction in booked appointments. Additionally, it's much better for the patient outcome.
Case Study
Patient BV had bilateral chronic otitis media since childhood. This individual is 50 years old, and she is a Ponto user with a long history of ear infections and several failed attempts at fixing her hearing loss through surgical interventions. Though she received benefit from wearing traditional hearing aids, she could not consistently use them because they blocked off her ear canals and perpetuated her ear infections.
In 2004, this patient had a BAHS fitted in the left ear, and then she was bilaterally fitted in 2005. Since then, her ear infections were reduced and she has considerably fewer visits to the clinic. Patient BV benefited from BAHS because it leaves the ear canal clear of any external interference. As more gain is needed with a hearing aid, a tight-fitting earmold is required, which can exacerbate the issue. BAHS relieves the patient from needing these earmolds and allows the discharge to clear.
BAHS Candidates: Single-Sided Deafness
Another indication category for the use of BAHS devices is SSD or single-sided deafness. Some people may know it as a profound unilateral sensorineural hearing loss. These patients have one completely nonfunctioning cochlea and one functioning cochlea. When looking at their audiogram, you'll see two very different threshold measurements: one showing normal or near-normal hearing, the other showing a profound sensorineural hearing loss.
A patient qualifies as a BAHS SSD candidate if their better ear has a normal or near-normal hearing (with an average air conduction threshold of < 20 dB HL), and the worse ear has a profound hearing loss. They can also be a candidate for BAHS treatment if they cannot have a CROS aid, (e.g., have an allergic reaction to an earmold), or if they are a candidate for a CROS aid, but choose not to use an air conduction CROS system. For patients with SSD, the sound processor is placed on the deaf side and picks up sound that is then transferred to the functioning cochlea on the opposite side via bone conduction, working as a CROS device.
Candidates for a BAHS include individuals with SSD caused by:
- Acoustic neuroma
- Sudden deafness
- Congenital causes
- Cholesteatoma
- Ototoxic drugs
- Meniere's disease
CROS vs. BAHS
How does a BAHS system compare to CROS? As you may know, a CROS system is where the deaf/worse ear wears a receiver, which wirelessly transmits the signal to a processor in the better hearing ear. This not only involves partially occluding in the worse ear but also partially occluding the better ear, as the processor needs to be anchored onto the ear and deliver sound to the ear canal. This, along with having to take care of two devices, increased pressure on battery life, and having to maintain a constant wireless connection, can lead to poor acceptance of a CROS aid. In contrast, a BAHS device leaves both ear canals open. You only need one device, which does not have to maintain a constant wireless connection, and it has a normal battery drain (Niparko, Cox & Lustig, 2003).
A recent analysis of 14 studies over 296 patients (looking at both subjective and objective data) favored treating SSD with a BAHS device (Kim et al., 2017). Kim and colleagues also found that in all experiments, in a variety of different scenarios, patients using a BAHS device either had the same or better scores for speech understanding in noise, as compared to a CROS aid.
Other Medical Indications
There is a small group of patients with other medical indications who can be good candidates for BAHS. Just by looking at their audiograms, we might not think of them right away as a potential Ponto user. They are likely to have a purely sensorineural hearing loss. This category includes individuals who have physical constraints for fitting. These patients may have skin allergies or external otitis that is aggravated by the use of an earmold (for example, a plastic allergy). Also included in this category are patients who have ear canal stenosis (narrowing) that makes using a traditional earmold unsuitable. For some, a BAHS device can be a viable alternative. However, these patients still must have bone conduction thresholds below 65 dB HL to ensure that Ponto will be adequate for their hearing loss.
Another important consideration with this patient group is to set their expectations appropriately. If we are only looking at the audiogram, the best purely audiological solution is hearing aids. They are likely to have heard better with a hearing aid at some point in their life. It's important to acknowledge this, but also to counsel the reasons why a BAHS device is an appropriate solution. Looking at it holistically, it's better for the patient to be using some type of correction rather than nothing at all.
Case Study
This patient is a 60-year-old female with moderate sensorineural hearing loss. She'd been to the clinic multiple times over the course of five years. In many ways, she could be considered the standard presbycusis patient. However, she had an allergic reaction to earmolds, causing dermatitis and occasional ear infections. Numerous earmolds had been made for this patient using different types of coatings. Regardless of the material or the coating used, the patient's skin would flake and dry. Dentin also did not work, even when using an open dome. It irritated the canal where it touched, and the hearing aid was much more prone to whistling, which she also didn't like. She was constantly coming in to see an ENT for aural towelettes or swabs if she had an infection. It seemed as though every avenue was exhausted.
The ENT was so exasperated by the situation that a gold-plated, metal earmold was made and exported over to the country, as it had been shown to help some allergic cases. This did help a bit, but as you can imagine, it was too heavy and bulky in the patient's ear, which caused pain. In conclusion, this patient is a strong candidate for a BAHS device, even though they may not look like it from their audiogram. It's not because of a conductive element to the hearing loss, but because of dermatitis and infections caused by contact with the earmold and closing of the ear canal. A BAHS device would provide amplification and keep the ear canal clear.
Who is Not a Candidate?
It is important to acknowledge the reasons why a patient may not be an appropriate candidate for BAHS surgery. There are patients out there who, for reasons beyond their control, have poor hygiene and are unable to properly care for and clean their abutment site. In some individuals, their bone quality will not support the implant if it's too thin or too brittle (e.g., due to radiation treatment). Other patients may have a skin condition at the implant site that would reduce their ability to heal following surgery. In some countries (including the United States, Canada, and Singapore), the surgery is not performed on children under the age of five. The general consensus behind waiting until the child is older is to allow time for the skull bone to become thick enough or strong enough to tolerate the implant, which typically occurs after age five. If you want to do some more in-depth reading about BAHS candidacy, or if you would like a quick recap, Oticon Medical has candidacy guides for your perusal.
Bilateral Conductive and Mixed Hearing Losses
Next, we will review how to decide when to go for a bilateral fitting, as well as how to decide which side to fit when we can't fit bilaterally.
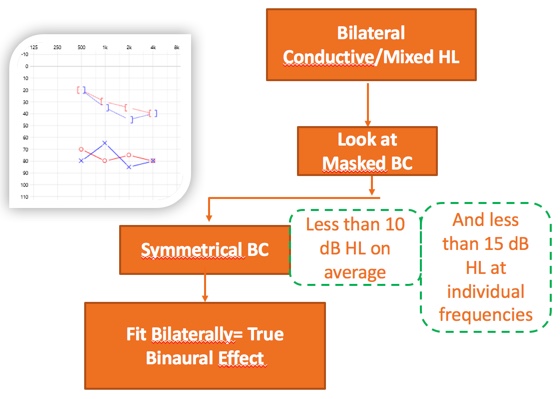
First, let's take a look at bilateral conductive and mixed losses (Figure 2). Because we are dealing with the bone conduction domain, all we have to do is look at the masked BC results. In this particular case, we can disregard the AC. If the BC is symmetrical, fit bilaterally, you'll obtain a true binaural effect. Our definition of symmetrical here is less than 10 dB difference on average, between the two masked bone conduction results, and less than 15 dB at individual frequencies. If that's the case, you can fit bone anchor devices bilaterally, and achieve a true binaural effect.
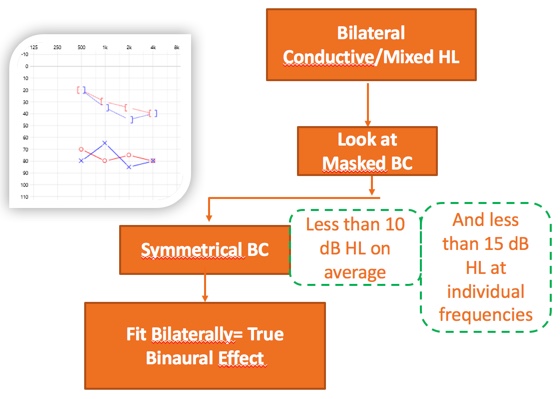
Figure 2. Bilateral fitting: making a decision.
Bilateral Fitting
When using the air conduction route with a hearing aid, two ears can be stimulated independently very easily, because they are acoustically quite well isolated from each other. One of the reasons why a bone anchored device can be used for an SSD patient is that with bone conduction stimulation, the two cochleae are not acoustically well isolated from each other. The skull transmits the bone conducted vibrations with very little dampening. Therefore, with one BAHS device, not only is the ear on the side of the fitting stimulated, but also the contralateral ear. Attenuation and vibrations from one cochlea to the other have a wide variation between people, and even between frequencies (anywhere from plus or minus 20). In other words, bone conduction stimulation of the cochleae is poorly acoustically isolated. However, and crucially, they are isolated just enough to be able to fit BAHS bilaterally and obtain a binaural benefit. As long as the bone conduction results are fairly symmetrical, we can obtain binaural benefit from a bilateral fitting.
Benefits of Bilateral Fitting
As I've said, the skull provides just enough attenuation to acoustically isolate the BAHS output. This has been shown to lead to an improvement in speech recognition in noise, improved localization of sounds, and being able to utilize binaural squelch. If you are not familiar with a binaural squelch, I'm going to briefly explain it. If a subject is listening to speech coming from their front, and noise coming from the left, speech in the two ears will be in phase. However, the noise, which is coming from the left, will be perceived differently by the two ears, not only because of the head shadow but also because of the intra-aural time differences, caused by the different traveling times of the noise to the left and right ear. This difference in intra-aural time for speech and for noise is used by the brain to perceptually separate the speech and noise and is referred to as binaural squelch. All these bilateral fitting benefits have been proven by research, and they also translate over to BAHS.
Unilateral Fitting
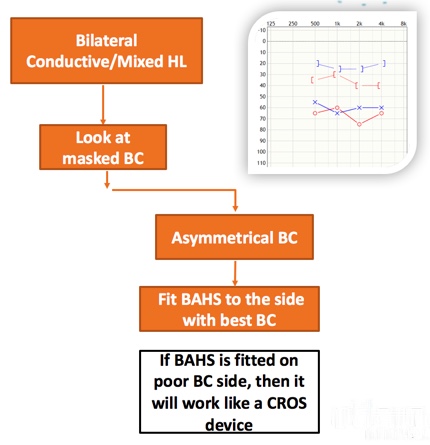
When it is appropriate to do a unilateral fitting, and which side do we fit? We're going address that question, this time with a different audiogram (Figure 3). When we look at the masked BC of this bilateral mixed conductive hearing loss, it's asymmetrical: the left masked BC is better than the right masked BC. In this case, which side do we fit? We fit the side with the best bone conduction threshold. If the BAHS is fitted on the side with the poorest BC threshold, it will act somewhat as a CROS device. When there's an asymmetrical BC, always fit the side with the best BC.
Figure 3. Unilateral fitting: making a decision.
Let me explain that again in a different way. As I mentioned before, the two cochleae are isolated just enough to be able to get a binaural benefit, but they are poorly acoustically isolated. In other words, if one cochlea is more sensitive to sound than the other (i.e., the bone conduction thresholds are better by more than 10 dB), regardless of which side the processor is fitted, only stimulate the ear with the best conduction, as the sound is transferred through the skull with little attenuation and picked up by the most sensitive ear. In summary, in order to make a decision as to whether to fit bilaterally or unilaterally, we need to look at the masked BC. If it is symmetrical, you can fit two BAHS and achieve a bilateral effect. If it's asymmetrical, simply fit the side with the best BC.
Ponto 3 SuperPower
The Ponto 3 family of sound processors consists of the Ponto 3, the Ponto 3 Power, and the most powerful all-in-one, abutment level sound processor, the Ponto 3 SuperPower (Figure 4). No matter what processor we use, at the core of the Ponto 3 family of products is BrainHearing. Our devices are designed to give the best sound quality in order to empower the brain. This is the recipe for how that sound quality is delivered: increased maximum output, greater bandwidth, and using the power of the IniumSense technology to deliver clarity without distortion.

Figure 4. Ponto 3 family.
Challenge in BAHS: Maximum Output is Low
All users can benefit from an increased maximum output. However, the challenge with bone anchored hearing systems is that the maximum output of the sound processors is relatively low. Humans have a loudness discomfort level of about 90 dB HL via bone conduction route. In his blog, "SnikImplants", Professor Ad Snik summarizes the maximum output of a number of BAHS products. Products like the Ponto 3 with a fitting range of up to 45 dB HL have a maximum output of around 67 to 69 dB HL, which is about 20 dB lower than a patient's loudness discomfort level. SuperPower devices, such as the Ponto 3 SuperPower, have a maximum force output (MFO) of about 80 to 85 dB HL. Despite being the most powerful abutment level product on the market, the maximum force of the Ponto 3 SuperPower still comes short of that loudness discomfort level. This means that even SuperPower products can't cause loudness discomfort, in the vast majority of patients.
Why is maximum output a challenge in BAHS? Why does someone who is as respected as Dr. Ad Snik have a whole area of his website is dedicated to this topic? It's because transmitting sound via vibrations through the skull bone is not as efficient as transmitting sound via the ear canal. As such, the MFO with BAHS devices is much lower than the maximum power output (MPO) of hearing aids. That means that the MFO of a BAHS device is lower than the uncomfortable loudness levels. Therefore, all patients can benefit from increased MFO.
Committed to Providing a Higher MFO
The Ponto 3 SuperPower combines a discrete, small design and a battery that lasts. It's an abutment level processor: there are no strings and no need for any bulky ear- or body-worn devices. It's the world's first single-unit SuperPower device.
With each iteration of our Ponto products, Oticon Medical is committed to providing higher MFO to try and increase that key component of our BrainHearing strategy. Why do we focus on this? What is the benefit? In our daily life, we experience a number of different listening environments. Within all of these environments, the sound level varies. Some of these environments have the great degree of sound variance (e.g., conversation in noise, at a music concert). A SuperPower processor allows us to capture more of that dynamic range of sound, making it easier to listen in those environments where sound varies the most. After all, we want to capture as much of the natural world as possible, to allow our users to experience clear, quality depth of sound.
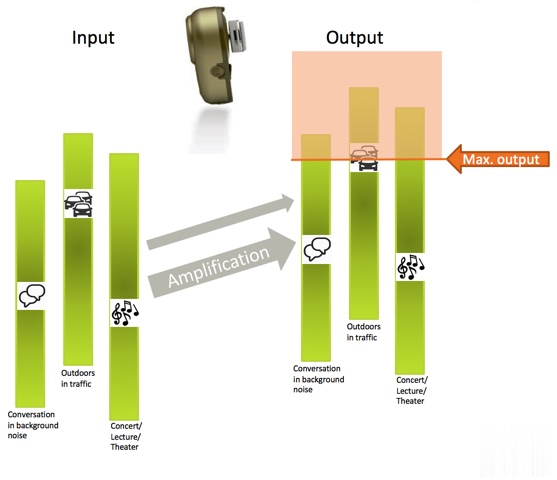
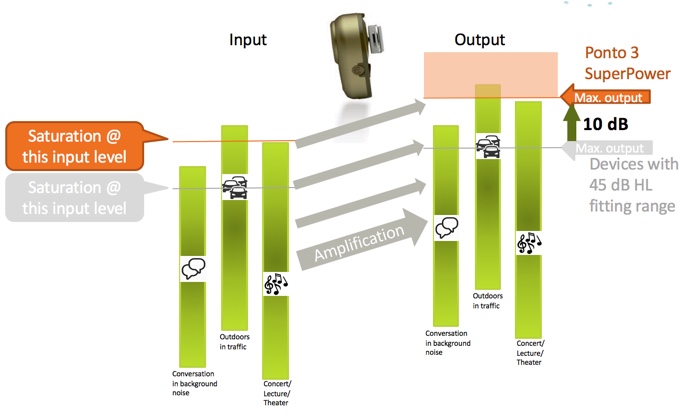
How Does It Work?
On the left of Figure 5, you can see some of the sources of sound input that a user might experience: conversation in background noise, outdoors in traffic, at a concert or lecture hall, or in a theater. On the right, indicated by the orange arrow, you can see the maximum output of the device. Any hearing device has a max output level. The output of the device cannot exceed that level. No matter how much the input is increased, the output will stay exactly the same and physically cannot become louder.
Figure 5. Explaining maximum force output.
As sound is amplified, you can see as the input increases, so does the output, but only up to a certain level, known as the maximum output. The input level at which this occurs is called the saturation point. Inputs louder than that saturation point lead to distortion in the device. Therefore, sounds above that saturation level are not naturally reproduced and will be distorted and unclear. Variance in dynamics of input levels beyond the saturation level is not reproduced; it is only the dynamics in the sound environments and speech below the saturation point that can be naturally reproduced.
When you use a device like the Ponto 3 SuperPower, which has a higher maximum output, you see an MFO increase of up to 10 dB (Figure 6). The saturation level increases as well. What does that mean? Anything below that saturation point is naturally reproduced. With the Ponto 3 SuperPower, the user is able to gain a much larger proportion of the dynamics in the environment that are reproduced without being limited.
Figure 6. Maximum output with Ponto 3 SuperPower.
Ponto 3 SuperPower is an optimal solution for all patient groups, not just those with the largest losses. A higher MFO means better utilization of the patient's dynamic range. The user will benefit from hearing a more natural sound, especially in louder listening environments. For patients with mixed hearing loss, the higher MFO gives them a larger dynamic range, and more headroom in the device, so more sounds are reproduced naturally, without being limited. It's also coupled with the excellent feedback management and IniumSense processing chip. For soft band and headband users, this higher MFO helps to address skin attenuation. Additionally, using the Ponto 3 SuperPower, SSD patients will be better able to loudness match sounds from the device to the normal hearing ear.
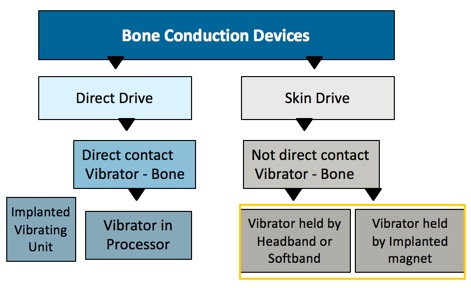
Methods of Sound Transmission
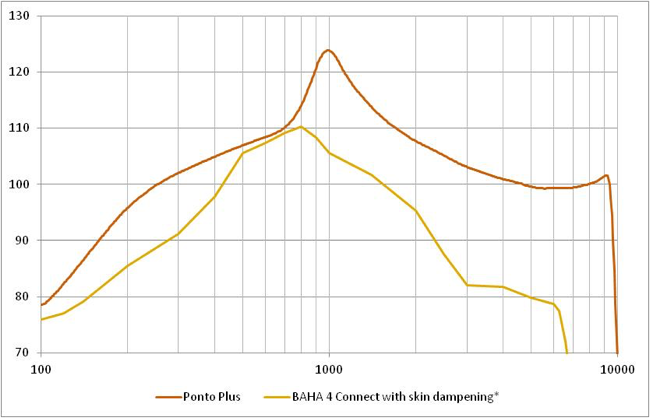
Using the graph in Figure 7, we will review the different methods of sound transmission for bone conduction devices: skin drive and direct drive (Briggs et al., 2015). Direct drive devices send vibrations via a direct route to the bone. Skin drive devices send vibrations through the skin before they reach the bone. This is a simple and easy way to categorize any BAHS device.
Figure 7. Direct drive vs. skin drive.
This is a soft band device (Figure 8). Soft bands can be useful for patients who aren't within the indications for surgery, or for children under five. The soft band is a skin drive solution: sound goes into the sound processor, vibrates the vibrating unit, which vibrates the skin before it gets to the bone. The analogy I like to use is that its kind of like throwing a blanket over a speaker. You've got that covering over it, so you're having to increase the sound to get through it.
Figure 8. Softband device.
Some solutions on the market hold the processor in place with magnetic attraction rather than an elastic band. In this case, surgery still has to take place to insert the metal disk. The disk is inert; it doesn't move and it doesn't provide any vibrations. It's just there to provide a magnetic attraction. When the surgery is finished, after the appropriate healing time, the processor can then be magnetically connected. Both a soft band and vibrator held in place by an implanted magnet are skin drive solutions, which provide similar outcomes, output, and performance.
An example of a direct drive solution would be what we've been discussing throughout this presentation: a processor connected to an abutment, which is osseointegrated directly into the bone, providing direct contact with the bone, with no attenuation, so you get the biggest maximum output. There are also some processors which have an implanted vibrating unit. There is a processor on the outside, which is attached to the skin via magnet again, but this time, all it's doing is sending across information through the skin to this implanted vibrating unit, which is implanted directly into the bone. There's a direct contact between that vibrating unit and the bone, so again, it's considered a direct drive. In summary, anything that has direct contact between the vibrating unit and the bone is direct drive, providing the biggest maximum force output. Anything that is attached to the skin and the vibration has to go through the skin is considered skin drive, and has an attenuated output.
Physical Facts with Skin Drive Solutions
As shown in the graph in Figure 9, there is a 10 to 20 dB attenuation in the mid to high frequencies with skin drive solutions (magnetic solutions or soft band). These devices have lower perceived output in the mid to high frequencies. The yellow line shows the force output of one such skin drive solution. The orange line shows the performance of our last generation of Ponto plus, a direct drive solution.
Figure 9. Attenuation in skin drive solutions vs. direct drive.
Conclusion
In summary, skin drive solutions do definitely have their place, but we're a company that believes in direct drive solutions for the longer term. A study was conducted with sixteen patients who had the exact same bone anchored processor (Lunner, Rudner, Rosenbom, Ågren & Ng, 2016). Each patient was fitted with first with a soft band, and then a direct drive solution, and they were subjected to a swirl test. The subjects could correctly repeat 95% of the speech words correctly, however, we weren't testing their hearing: we wanted to test their recall. With a direct drive solution, patients were able to remember 13% better, as compared to when they wore a skin drive solution. In short, they had improved BrainHearing with a direct drive device. The basic tenet behind BrainHearing is if you provide the best sound quality to the brain, it doesn't have to spend so much time trying to understand, trying to fill in the gaps, and you can put more effort into other things.
References
Briggs, R., Van Hasselt, A., Luntz, M., Goycoolea, M., Wigren, S., Weber, P., ... & Cowan, R. (2015). Clinical performance of a new magnetic bone conduction hearing implant system: results from a prospective, multicenter, clinical investigation. Otology & Neurotology, 36(5), 834-841.
de Wolf, M. J., Hendrix, S., Cremers, C. W., & Snik, A. F. (2011). Better performance with bone‐anchored hearing aid than acoustic devices in patients with severe air‐bone gap. The Laryngoscope, 121(3), 613-616.
Evans, A. K., & Kazahaya, K. (2007). Canal atresia:“surgery or implantable hearing devices? The expert's question is revisited”. International Journal of Pediatric Otorhinolaryngology, 71(3), 367-374.
Hol, M. K., Spath, M. A., Krabbe, P. F., van der Pouw, C. T., Snik, A. F., Cremers, C. W., & Mylanus, E. A. (2004). The bone-anchored hearing aid: quality-of-life assessment. Archives of Otolaryngology–Head & Neck Surgery, 130(4), 394-399.
Kim, G., Ju, H. M., Lee, S. H., Kim, H. S., Kwon, J. A., & Seo, Y. J. (2017). Efficacy of Bone-Anchored Hearing Aids in Single-Sided Deafness: A Systematic Review. Otology & Neurotology, 38(4), 473-483.
Lunner, T., Rudner, M., Rosenbom, T., Ågren, J., & Ng, E. H. N. (2016). Using speech recall in hearing aid fitting and outcome evaluation under ecological test conditions. Ear and hearing, 37, 145S-154S.
Macnamara, M., Phillips, D., & Proops, D. W. (1996). The bone anchored hearing aid (BAHA) in chronic suppurative otitis media (CSOM). The Journal of Laryngology & Otology, 110(21), 38-40.
McDermott, A. L., Dutt, S. N., Reid, A. P., & Proops, D. W. (2002). An intra-individual comparison of the previous conventional hearing aid with the bone-anchored hearing aid: The Nijmegen group questionnaire. The Journal of Laryngology & Otology, 116(S28), 15-19.
Mylanus, E. A., van der Pouw, K. C., Snik, A. F., & Cremers, C. W. (1998). Intraindividual comparison of the bone-anchored hearing aid and air-conduction hearing aids. Archives of Otolaryngology–Head & Neck Surgery, 124(3), 271-276.
Nadaraja, G. S., Gurgel, R. K., Kim, J., & Chang, K. W. (2013). Hearing outcomes of atresia surgery versus osseointegrated bone conduction device in patients with congenital aural atresia: a systematic review. Otology & Neurotology, 34(8), 1394-1399.
Niparko, J. K., Cox, K. M., & Lustig, L. R. (2003). Comparison of the bone anchored hearing aid implantable hearing device with contralateral routing of offside signal amplification in the rehabilitation of unilateral deafness. Otology & neurotology, 24(1), 73-78.
Papp, Z., Rezes, S., Jókay, I., & Sziklai, I. (2003). Sensorineural hearing loss in chronic otitis media. Otology & neurotology, 24(2), 141-144.
Snik, F. M., Mylanus, E. A., Proops, D. W., Wolfaardt, J. F., Hodgetts, W. E., Somers, T., ... & Tjellström, A. (2005). Consensus statements on the BAHA system: where do we stand at present?. Annals of Otology, Rhinology & Laryngology, 114(12_suppl), 2-12.
Verstraeten, N., Zarowski, A. J., Somers, T., Riff, D., & Offeciers, E. F. (2009). Comparison of the audiologic results obtained with the bone-anchored hearing aid attached to the headband, the testband, and to the" snap" abutment. Otology & Neurotology, 30(1), 70-75.
Citation
Samra, B. (2018, April). Bone anchored hearing systems - principles and candidacy. AudiologyOnline, Article 22366. Retrieved from www.audiologyonline.com