Editor’s Note: This text course is an edited transcript of a live webinar. Download supplemental course materials.
Welcome to Audiology Billing/Coding Reimbursement: 2014 Update. First and foremost, let's talk about the Medicare fee schedule 2014. At the last minute in 2013, the Medicare fee schedule was changed to some degree. That fee schedule was effective from January 1, 2014 through March 31, 2014. Congress is going to need to act in the next two to three weeks to revise these rates or we may see another extension. If you are unaware of the current fee schedule specific to your state or locality, please consult your Medicare Area Contractor’s website. If you are unsure how to locate that, you can search for it, such as Illinois Medicare part B fee schedule, and the search engine will take you directly to the sites.
Physician Quality Reporting System
The Physician Quality Reporting System (PQRS) is a program designed to improve the quality of care for Medicare beneficiaries. Audiologists who bill Medicare Part B have to participate in PQRS in 2014 in order to avoid a reduction. The 2016 reduction will be 2% in all the Medicare reimbursements for that provider, regardless of your clinic location. I want to stress that PQRS follows the provider, not the clinic. Every provider in your clinic needs to be reporting. The PQRS penalty follows the rendering provider.
PQRS does not apply to Part A hospital or skilled nursing. PQRS also does not apply to Medicare Part C, which is Medicare Advantage or the privatized Medicare programs. PQRS does apply to Part B.
You can qualify for PQRS incentives in 2014 and begin reporting at any time, because we are claims reporters. Audiologists report on a CMS-1500 (Centers for Medicare & Medicaid Services) form, which is the form on which our PQRS is reported; the previous form was the HCFA-1500 (Health Care Financing Administration). Until December 31, 2014, a 0.5% bonus will be given for all Medicare-eligible cases when reporting on 50% of eligible measures. If you avoid the penalty in 2014, you will qualify for the incentive because the criteria are the same.
Audiologist Reporting Measures
The three PQRS measures that audiologists can report in 2014 are Measures 261, 130 and 134. Measure 261 is referral for otological evaluation for patients with acute or chronic dizziness. Measure 130 is documentation verification of current medications in the medical record, and Measure 134 is screening for clinical depression and follow-up plan. Measure 188, which is congenital traumatic deformity of the ear, was retired in 2014.
Acute or Chronic Dizziness
Let’s go over code 261, which is the code for referral of acute or chronic dizziness (Figure 1). The diagnosis code for dizziness is 780.4. Dizziness as a diagnosis is a subjective patient complaint. It is what your patient reports before the cause of the dizziness is diagnosed. It is very common, regardless of your clinical setting. Dizziness should be a topic that is addressed on every case history. Regardless of your situation, you should have patients who report dizziness to you, and, as such, you should report dizziness frequently in your audiology practice.
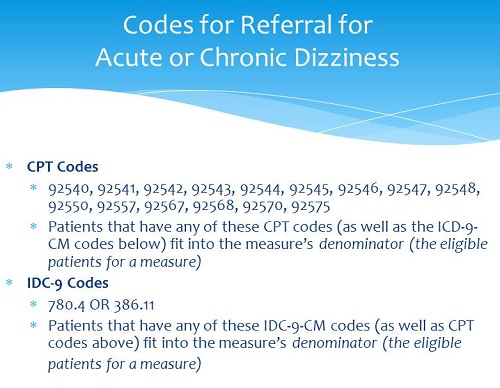
Figure 1. Codes for referral for acute and chronic dizziness.
The data shows that 30% to 40% of patients over the age 60 have some form of dizziness or unsteadiness; the numbers show that this is something for which we will qualify very frequently. Anytime you perform the vestibular family of codes 92540 through 92548, tymps and reflexes (92550), or an audiogram, tymps, and reflexes, or tymps/reflexes and reflex decay, or the Sensorineural Level Acuity test, you qualify to report on this measure if the patient’s corresponding diagnosis is either dizziness (780.4) or 386.11 for benign paroxysmal positional vertigo (BPPV). Regardless of your setting, this is something you should be asking your patients and reporting on at least 50% of the time to avoid the penalty.
G Codes
PQRS is reported via G code. The option for referral for acute or chronic dizziness is G8856. This is used to note that you did refer a patient to a physician for an otologic evaluation because of the report of dizziness. G8857 notates that the patient is not eligible for otologic evaluation because they have been under the care of a physician within the last six months for dizziness. G8858 indicates that you did not refer for otologic evaluation because of the dizziness, but you did not say why. I always advise that we do not know long-term what this data is going to be used for. Eventually this data is going to be available on a website, which we will talk about in a little bit. The reason for PQRS is highest standards of care. If a patient reports dizziness and they are not under the care of a physician, we want to make sure that they are referred accordingly. Some reasons why you might not refer is if the patient is in hospice or if you saw them in an emergent situation. You want to code that judiciously.
Current Medications
The same thing applies for documentation of a patient’s current medications. Patients may not tell you that they have certain conditions, such as diabetes, or about the medications they think are common, like Lasix or insulin; these have a significant effect on hearing. Anytime you use codes that do not have a diagnosis code requirement, you want to make sure that you are reporting that you are documenting current medications (see Figure 2). The next section will cover the codes used to document current medications.
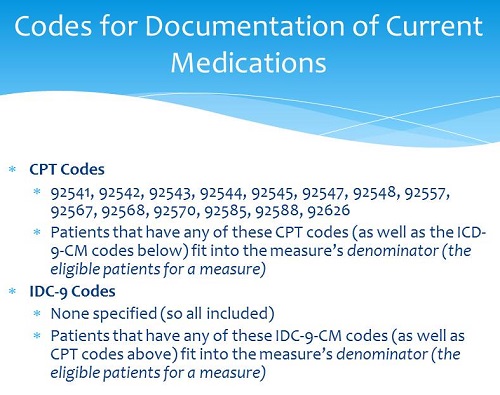
Figure 2. Codes for documentation of current medications.
The first code is G8427. To use this code, you need a current list of medications to check off, and you must document that you confirmed its accuracy. You need prescription, over-the-counter, herbal, vitamin, and dietary supplements. You need the drug name, the dosage in milligrams (mg) or grams (g), and the frequency of the dosage. Do they take it daily, several times a day, or monthly? Is it a pill? Is it a suppository? Is it intravenous (IV)? Is it injected? You need to know how it comes into the body. You need all of this information in order to use that measure for current medications.
If the patient takes no medications, you would use code G8427. You still document current medications; they just do not happen to have any. If that is already in the file, you need to confirm that there are no medications and that your reviewed list was valid for that date of service.
You would use G8430 if they are not eligible. Use this is an emergent situation, if you are with a patient who is cognitively impaired and unaccompanied, or if the patient does not speak English and a translator is unavailable for you to verify that list.
G8428 is for current medications in the instance that you only obtained a partial list from the patient or are missing dosage or frequency.
Documenting current medications is not just about PQRS; it is about good patient care. It is important to ask patients verbally about their medications, and many patients to which the PQRS code applies will carry a list with them. If they have a list with them, make a copy and confirm that the medications are valid. Sign the copy and date it, and place it in your medical record.
Clinical Depression
There are CPT codes that apply for screening of clinical depression (Figure 3). The first is an audiogram, then tympanometry, reflexes, assessment of tinnitus, and evaluation of acoustic reflex status. It has no diagnosis code correlate. Screening of clinical depression is a voluntary code, not a required code. It is not a measure that you have to report 50% of the time. Current medications and referral for acute or chronic dizziness are measures that are required for audiology that we would need to report 50% of eligible cases in order to avoid the penalty. Screening for clinical depression is an optional code.
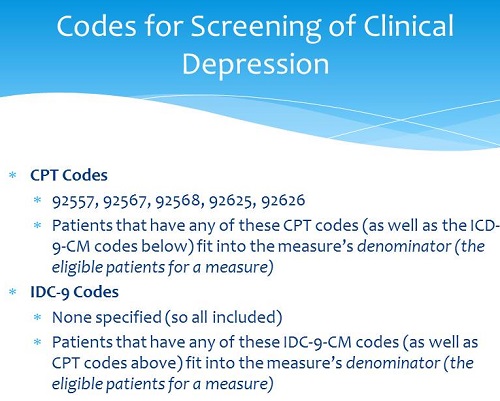
Figure 3. Codes for screening of clinical depression.
Following are the G codes for screening of clinical depression. G8431 means you have a positive screen of clinical depression using age-appropriate standardized tools and the follow-up plan is documented. G8510 means you have a negative screen using age-appropriate tools and a follow-up plan is documented. G8433 means that screening for clinical depression using an age-appropriate tools was not documented, or the patient was not eligible or appropriate for the screen. Again, this would be if the patient was cognitively impaired, you were in an emergent situation or they did not speak English and were unaccompanied.
G8432 means you did not do the screen, and there is no documentation of clinical depression screening using age-appropriate standardized tools. Reporting no documentation is still reporting on PQRS. G8511 is when you have a positive screen for clinical depression documented, but you did not document of a follow-up plan of care and you did not explain why; I would never ever use this one because of the potential ramifications of liability.
There are some important factors related to the clinical depression measure of which you need to be aware. I only recommend that audiologists report on this (Measure 134) when allowed by their state licensure law. Many state licensure laws are general. They are almost nonexistent as to the scope and breadth of what an audiologist can perform in your state. Before you start performing certain procedures, it is important that you first determine if it is allowed within your licensure law. You, as individual providers, do not determine that.
In order to determine if screening for clinical depression is in your scope of practice, you would need to send a written request to your licensure board and have them give you a written notification back. Secondly, you only want to perform Measure 134 when you are appropriately trained and competent, not only to perform the screening itself, but to create the required plan of care as well. You only want to report on Measure134 when you have a follow-up plan of care that is created, implemented, and documented in the medical record. If your patient is depressed and you now have documentation of such, you want to make sure to get them in the proper channels for evaluation and treatment.
Submitting PQRS
A sample 1500 claim form, with PQRS, is available from the Academy of Doctors of Audiology if you are a member. All the national associations have links to sample PQRS forms, as does CMS itself. The ICD-9 or diagnosis codes are placed in box 21. The current procedural terminology (CPT) codes are placed in box 24D; they are not placed in the modifier box. The G codes for PQRS are placed immediately below the corresponding CPT code. To avoid the penalty and qualify for the incentive, you want to report on Measure 261 (dizziness) on at least 50% of the providers’ Medicare eligible claims that contain the diagnosis codes of dizziness (780.4) or BPPV (386.11).
You want to report on Measure 130 (documentation of current medications) on at least 50% of every providers’ Medicare claims when you bill for hearing tests, caloric testing, tympanometry, auditory brainstem response (ABR), comprehensive otoacoustic emissions, and/or cochlear implant or auditory osseointegrated device candidacy testing (92606). Again, the PQRS measure is optional, and you can avoid the penalty and qualify for the incentive without ever reporting this measure a single time.
Omnibus Rule
I want to take this opportunity to talk about the HIPAA (Health Insurance Portability and Accountability Act) Omnibus rules that went into effect September 23, 2013. The Omnibus rules strengthened HIPAA privacy and security and created more definitions of things that we needed to do. It talked in detail about business associates, explaining that a business associate is any entity that creates, receives, maintains or transmits protected health information (PHI) on the behalf of a provider who supplies this information to them or their contractors or subcontractors. It strengthened the fact that if a business associate subcontracts things out, that they are still liable for the subcontractors’ management of PHI. Business associates in audiology are people like hearing aid manufacturers, ear mold manufacturers, office management system providers, potentially your accountant or your attorney if they see patient information in any of your systems, and any computer consultants that you may have. Anyone to whom you are giving access to your systems and patient PHI would be your business associate. As a result, all those business associates need to have business associate agreements in place. We will talk about that again in a little bit.
As another part of the Omnibus rule, patients have the right to request a copy of their electronic medical record be supplied to them in an electronic format. If you are a paperless practice, a patient has the right to request that a copy of the medical records be mailed to them in some form of protected electronic format. Patients who are paying privately for an item or service have the right to restrict any disclosure about this item or service to their health plan.
Let's say you have a patient that does not have hearing aid coverage. They have the right for you to not submit that claim. They may want to pay privately for hearing tests and not bill their insurance. They have the right for you to not submit a claim. I would, however, create a waiver, especially when it comes to a covered service, stating that they understand that they have a benefit that they have chosen not to access.
Marketing has been strengthened, although marketing authorization has always existed in HIPAA. Marketing is any time that you are sending a communication that contains the four cardinal rules of marketing: place, product, price or promotion. If you are sending anything like that to your database, you need the patient’s authorization to do so. That has existed since day one of HIPAA. This is now strengthened as part of Omnibus. Marketing has been redefined as any patient communication where the provider receives financial remuneration from a third-party whose products or services are being marketed. When marketing is being performed using PHI, you must have a specific authorization in place before sending this communication.
It is extremely important that you make a determination of what level of marketing authorization you need in your practice. Remember this only applies to marketing to a database. It does not pertain to newspaper, direct-mail or website marketing. It pertains to marketing your database. If a third-party never pays for any of those communications, or if you never market specific products where you are getting remuneration on the backend in the form of a business development fund or equity ownership in the company, you just need a very simple two-sentence marketing authorization in order to market to your database. However, if a third-party is ever paying in whole or in part to marketing to your database or you are marketing a specific product and the third-party is giving you money in the form of a rebate, fund contributions or equity ownership in the company, you need a longer, more specific marketing authorization in order to continue those actions to your database.
The sale of PHI is prohibited in the Omnibus rule. You must have a defined breach notification process where any situation is presumed to be a breach until the provider, business associate or any other subcontractors perform a risk assessment and determine if there is a low probability that the patient's privacy has been compromised. You must perform a risk assessment and document it.
Let me give you some examples of breaches. Say you mistakenly fax a patient's results to the wrong physician’s office. Because the physician has HIPAA protections in place on their end, this would be a low probability of a breach of privacy. You would still want to document that in the patient's records.
Let's say that you lose a paper chart. You do not know if it is lost or stolen. When you have those types of breaches, those patients need to be notified. Let’s say your system was hacked. That would be a significant breach. That would be an instance where you would need to notify patients because there is a high probability that a patient’s data is compromised. Your practice was broken into or your computer was stolen. Those are high probability breaches that would need to be documented, and those patients would need to be notified.
The Omnibus rule also allows for broader use of PHI for fundraising opportunities and for research purposes. The penalties under Omnibus have now been increased to a maximum of $1.5 million per year. It is a criminal charge. Many fines can range between $100 to $50,000 per violation and degree of culpability, how purposefully you were in your action, and up to 10 years in jail.
What Every Practice Needs Under HIPAA
This is what every practice needs today (Figure 4). You need a 2013 Revised Notice of Privacy Practices that your patients will now re-acknowledge. You need a Revised Business Associate Agreement for 2013 with the Omnibus language; all your business associates need to sign it. If you had Business Associate Agreements signed in 2013, you have until September 23, 2014 to get those updated. If you did not have Business Associate Agreements in place, you have missed the date of implementation, which was September 23, 2013.
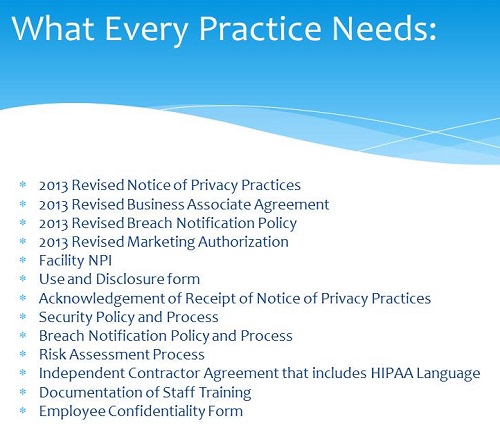
Figure 4. HIPAA documentation and process requirements for 2014.
You need a Breach Notification Policy, and it has to be revised with Omnibus language. You need a Revised Marketing Authorization. Everyone needs a facility National Provider Identifier (NPI) for every facility location.
You need a Use and Disclosure form. A Use and Disclosure form replaces the old medical release; it is just in HIPAA language. It allows for patients to tell you who they want things sent to and who they do not, or who they do not want have access to PHI, which could be a spouse or child. Remember, you cannot divulge PHI to anyone but the patient and/or their power of attorney without that patient's approval, and that includes a spouse. You need an Acknowledgment of Receipt of Notice of Privacy Practices. Every practice since 2005 has needed a Security Policy and Process, and every practice since 2010 has needed a Breach Notification Policy and Process.
You need a Risk Assessment Process. How are you going to handle a breach? How are you going to determine your risks? You need a process of how to document that. You need Independent Contractor Agreements for anybody who is working for you as an independent contractor, and with anyone for whom you are working as an independent contractor; make sure that contains the HIPAA language.
It is of utmost importance to have documentation of staff training. Your staff needs to be trained on privacy, security and breach notification. I strongly recommend Employee Confidentiality forms, which, when signed, makes the employee accountable for keeping PHI confidential. Confidentiality agreements are not difficult to enforce. Make sure you have as many protections in place as possible.
In closing on HIPAA, remember that HIPAA is generally a patient complaint-driven process, although CMS is now going to start auditing people’s HIPAA compliance. As a result of it being primarily a patient complaint-driven process, it is the patient's perception of the communication.
HCFA 1500 Form
Let's talk now about the HCFA 1500 form and how that is going to be changing. The HCFA 1500 changed to the CMS 1500 form on April 1, 2014. The forms you use need to be dated February of 2012. The form has been modified in box 21 to accept the additional digits of ICD-10, and you can begin submitting using this form now. It applies to the paper claim only.
This is a perfect opportunity to stress that I strongly recommend that every practice, regardless of size, consider electronic claims submissions only. Many third-party payers offer the ability to submit electronic claims at little or no cost. Many Medicare Area Contractors offer very low-cost electronic claims submission abilities. The days of paper claims are coming to an end. Anyone who is signing new contracts are being told that they must submit electronically. Instead of buying new forms, I suggest you start exploring electronic claims submissions. Your claim will be denied if you are using the HCFA 1500 form and not the current CMS 1500 form.
Figure 5 is an example of the CMS 1500 form. The changes have been highlighted and numbered. There are wonderful CMS 1500 form resources at the following link: https://www.nucc.org, and the form in Figure 5 can be found at this link: https://www.practicons.com/2013/another-change-in-health-care-cms-1500-claim-forms-are-changing
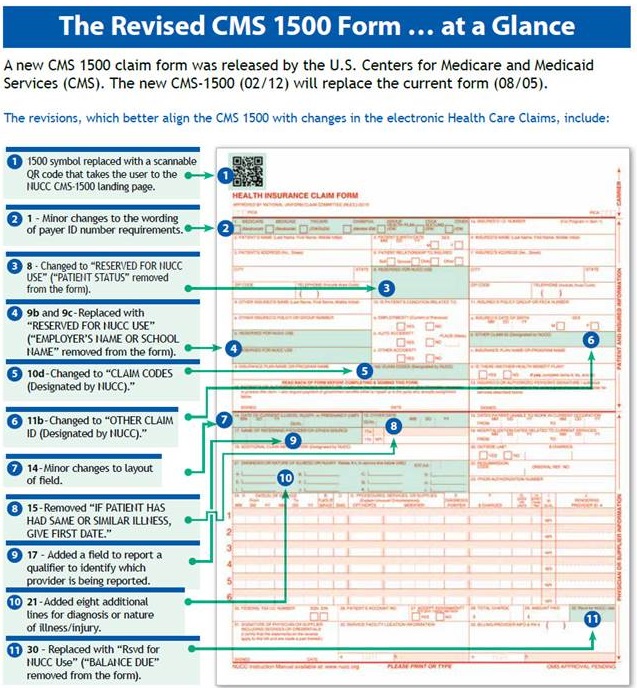
Figure 5. The revised CMS 1500 form, with highlighted changes.
ICD-10
The ICD-10 is a set of code. For those of you who do things electronically, load the new code into your system and educate yourself on what your new options are. If you are still doing paper superbills, have a new paper superbill available, educate yourself on that form, and circle new codes. There will be many resources available. The ADA, American Academy of Audiology (AAA) and American Speech-Language-Hearing Association (ASHA) have ICD-10 resources available. Many are going to offer sample super bills or superbills you can purchase. You need to approach your office management system providers and make sure they are loading the new code into the systems.
The ICD-10 is a vast expansion and change from the ICD-9 codes. The big focus is that you will be able to distinguish right from left from binaural. I am going to be doing an ICD-10 specific webinar for AudiologyOnline as the switch date draws near. ICD-10 goes into effect October 1, 2015. (Editor's note: At the time of the Dr. Cavitt's live webinar, the ICD-10 effective date was October 1, 2014. On April 1, 2014 this date was changed to October 1, 2015. Therefore, this text course was updated, but the course handout from the live webinar may reflect the old date).
What You Need to Do
First, you need to update your paper superbills or office management system options to reflect ICD-10 code changes. You are going to need to purchase a manual or software for those situations when an ordering physician or physician with whom you work has a diagnosis that is not something within the scope of audiology or is atypical. There are some free options available. Mapping is a system where you take ICD-9 code and you translate it into ICD-10 code. I want to caution you on maps, because we are going from fewer codes to more codes, and you may be leaving some of the new options behind. Instead, I advise people to look at the code list, see what options there are, put as much in your system or on your form as possible, and then start selecting them.
You want to consult any of your Medicare local coverage determinations and PQRS measures on how ICD-10 influences those programs. You are going to see all of the Alternative Quality Contract (AQC) do the translation over to ICD-10. All those materials and translations will be available from your Medicare Area Contractors on your local coverage determinations. I cannot stress this enough. Providers code; staff, except certified coders, do not code. Audiologists code; dispensers code. You should be selecting the code. Providers need to be trained on what their options are. There are some great myths and facts documents at the following link: https://www.cms.gov/Medicare/Coding/ICD10/Downloads/ICD-10MythsandFacts.pdf
Terms
Going forward, you will see an ICD-10 measure called unrestricted hearing. Unrestricted means they have no hearing loss. This is for the person who has normal hearing in one ear and a mixed or conductive or sensorineural hearing loss in another ear. The unrestricted codes will be used for when people have a unilateral loss only. You will report the diagnosis code for the ear that has the hearing loss, and then unrestricted hearing will tell you that the other ear is normal.
Salpingitis means inflammation. You are going to see a lot of new measures for the external auditory system. You can have salpingitis of the external auditory canal or salpingitis of the Eustachian tube.
Stenosis means narrowing. And while we have been used to terms about the narrowing of the canal and stenotic, collapsing ear canals, that now will exist as an ICD-10 diagnosis.
Impacted cerumen is not incidental. Impacted cerumen has a very specific definition, and that is cerumen that is blocking clinically significant portions of the ear canal. That means you cannot visualize the eardrum.
ICD-10 Examples
Figure 6 shows a slide of some ICD-10 examples.
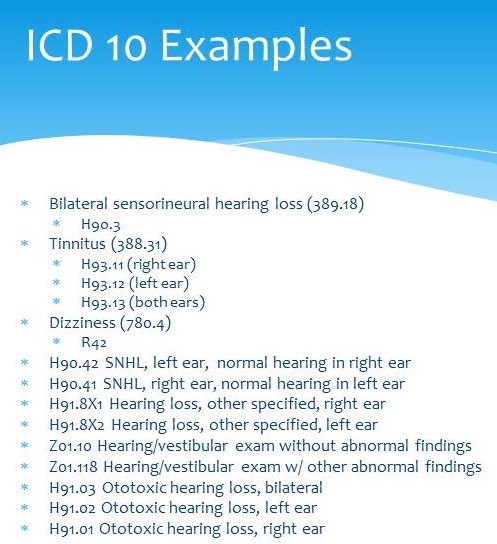
Figure 6. ICD-10 code examples.
Bilateral sensorineural hearing loss, which is currently 389.18 will become H90.3. It is a coincidence that the preceding letter is an H; it does not stand for “hearing.”
In ICD-9, there is a code for subjective tinnitus and a code for objective tinnitus. In ICD-10, it is just tinnitus. The subjective tinnitus code 388.13 will translate to H93.11, which is tinnitus in the right ear, H93.12, tinnitus in the left ear, or H93.13, tinnitus in both ears.
Currently, the code for dizziness is 780.4. That diagnosis will change to R42. ICD-10 codes can go out to seven characters, and those characters can be letters numbers or periods.
Another examples of a new code is H90.42, which is sensorineural loss in the left ear and normal hearing in the right. It would read sensorineural hearing loss left, unrestricted hearing in the right ear. H90.41 is sensorineural hearing loss in the right ear, normal hearing in the left ear.
H91.8X1 is hearing loss, other specified, right ear. Let me give you an example of when you would use this. Let's say that someone has a mixed hearing loss in the right ear and sensorineural hearing loss in the left. You would use both of these codes: hearing loss, other specified, right, and hearing loss, other specified, left. That is how you would differentiate different types of hearing loss in different ears. The two codes you would use would be H91.8X1 or H91.8X2.
Next, let’s say you did an exam, but you have normal hearing with no abnormal findings. That would be Z01.10. Yes, we had V codes in ICD-9, and those led to denials. We do not know if these Z codes will lead to denials because they have not been utilized yet. As contractors, you want to read anything that comes from Medicare or your private insurers about coverage decisions based upon ICD-10. Read any documentation they send you. We do not know for certain how they are going to approach it.
Z01.118 is hearing/vestibular exam with other abnormal findings. You might have abnormal findings outside of the auditory system that have been documented in the medical record. We will also have codes for ototoxic hearing loss and a whole system for reporting what the ototoxic agent was. This diagnosis code would be combined with the code for the ototoxic agent. That would be H91.03 for bilateral, H91.02 for left ear, and H91.01 for right ear.
Contracting in 2014
Towards the end of the calendar year as a new year approaches, you need to take a look at your third-party contracts with a fresh eye. Consider how each payer processes codes for every item or service that you provide within the practice. What does medical necessity mean to each payer? That is what drives their coverage. Do you have a current fee schedule which lists the allowable amount for every payer with whom you do business?
Read your contracts. When you do not know an answer, pose those questions in writing to the payer. Stop trying to deal with them over the phone. Review their answers, and then decide whether you want to accept their terms as written, renegotiate those terms, or terminate your agreement. Other than Medicare, you are a voluntary participant in third-party contracting. You do not have to participate. As a result, you need to take a good look about whether all business contracts are in your best interest.
Modifiers
A review of modifiers is important. The 22 modifier is increased procedural service, which means that you are doing more than the norm. That can be used for things like auditory steady-state response (ASSR), middle to late latency response, ABR, high-frequency audiometry, Eustachian tube function testing added to a tympanogram, fistula testing added to tympanogram, et cetera. Those can be used to reflect the additional time.
A 33 modifier is preventative service. This code is only used for newborn hearing screenings and their follow-up testing as required by law. The 50 modifier is bilateral procedure. This code only applies to the cochlear implant programming codes, because those are written as monaural. You can either bill it as two monaural procedures, or reflect it with a 50 modifier for a bilateral procedure.
The 52 is reduced services. This is used when you did not do all the components of a code on both ears or when you have only tested one ear. A distinct procedural service, 59, is when you have unbundled portions of a bundle. Let's say you decide, in the vestibular family of codes, that you are going to do calorics, positionals, and gaze, but you are not going to do optokinetics or tracking. When you bill the positionals and gaze, you would add the 59 modifier to show it is a distinct procedural service.
The GA modifier means you have a required advanced beneficiary notice (ABN) on file. The GX modifier means you have a voluntary ABN on file. The GY modifier is when the item or service is statutorily excluded or does not meet the definition of a Medicare benefit, and you are requesting a Medicare denial.
Lastly, RT means right ear and LT means left ear.
CPT and HCPCS Codes
There are no new CPT or HCPCS (Healthcare Common Procedure Coding System) codes for 2014, but there are codes that are now becoming more commonly seen in contracts. These are S1001, S0618, and V5298. Contact each private payer to determine how they will address some of these codes before using them.
S1001 is a deluxe item, patient aware. S0618 is audiometry for obtaining a hearing aid. That is a temporary code which is oftentimes record recognized by Blue Cross/Blue Shield. You will be surprised of its reimbursement when it is allowed.
V5298 is hearing aid, not otherwise specified. This is a code that is individually reviewed. This would be a code that you would consider for a Lyric or any other deep insertion or disposable type of hearing aid. This is a code you might want to consider for a combo tinnitus masker/ hearing aid. Again, you want to first know how your insurance is going to handle these codes.
Local Coverage Determinations
Figure 7 shows the Medicare local coverage determinations that currently exist in the United States for vestibular and auditory testing. Novitas, and those covered under Novitas, have a local coverage determination. First Coast in Florida has tympanometry. They also have a vestibular testing only local coverage determination. Vestibular testing, which can have effects over the code 92557, exists for Palmetto and Noridian contract members.
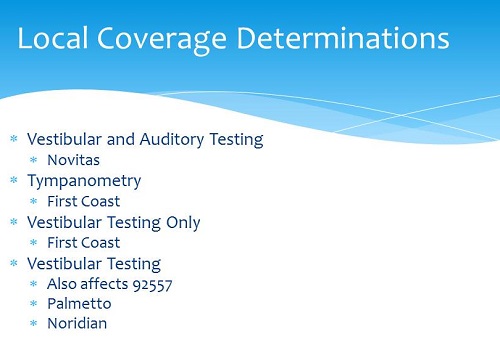
Figure 7. Local coverage determinations for vestibular and auditory testing.
Documentation
Your medical record, which is either the physician order, the audiological report, the chart or electronic record itself, must describe the medical necessity of each item or service you provide; it must say why you did what you did. I am going to tell you that medical necessity is not just about Medicare and Medicaid; it is part of every third-party contract I read. You need to be able to document medical necessity. An audiogram, in and of itself, does not constitute sufficient medical necessity. You need a report. Some of the codes we use require report, and the need for report is built into the code description.
Documentation must include the date of service and the full name and credentials of a provider, not initials. It needs to be in ink or in a computer system, and must be legible to be read. The old rule applies: “If it is not documented, it didn't happen.”
Medicare Reasons for Covered Testing
The Medicare rules as they pertain to audiology can be found at the following link: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c15.pdf Section 80.3, which is audiologic testing, and section 80.6, which is the physician order requirement, is clearly documented. Medicare does not pay for testing when the type and severity of the current hearing, tinnitus, or balance status needed to determine the appropriate medical or surgical treatment is already known before the test or if the test was ordered for the sole purpose of fitting or modifying a hearing aid.
Medicare covers tests to evaluate a suspected change in hearing, tinnitus, or balance or to evaluate the causes of hearing, tinnitus, or balance disorders. They will also provide coverage to determine the effects of medication, surgery, or other treatment, as well as for re-evaluation to follow-up on changes in hearing, tinnitus or balance over time. They cover testing after the failure of a screening test, but they will not cover the screening itself. Diagnostic analysis of a cochlear implant and associated programming is covered, as is the diagnostic testing pre and post implantation for and auditory prosthetic devices, such as a bone-anchored hearing system.
Physician Compare
Let's talk a bit about Physician Compare. Physician Compare is a new website that Medicare is offering to their members that allows them to find, compare and choose physicians and other healthcare providers who are enrolled in Medicare (https://www.medicare.gov/physiciancompare/search.html). This is a provision of the Affordable Care Act. Audiologists are currently listed in Physician Compare. I strongly encourage you to take a look. If you are not listed or your data is incorrect, you need to follow the steps on the Physician Compare site to make modifications. Your PQRS participation, or lack thereof, will be noted on the Physician Compare website.
Every year the office of the Inspector General comes out with a work plan (https://oig.hhs.gov/reports-and-publications/workplan/index.asp#current). It tells you what is in the Medicare audit sights for the coming year. Some items that are important to audiology are related to noncompliance with assignment rules and excessive billing to Medicare beneficiaries. That means billing above and beyond the allowable amount, inappropriately billing patients for items or services that Medicare would have covered with the physician order, medical necessity, and place of service coding errors. These are all items for which they are going to begin auditing. Place of Service 11 is an office; if you are not in your office seeing that particular patient, you need to change the place of service accordingly. Those codes are readily available; if you need them, please contact me. This is an easy audit, and they are going to be looking closely at discrepancies in place of service.
What to Watch for in 2014
Please watch both the national news and your national association’s information releases to keep you in the loop. Look for the Medicare reimbursement changes to the sustainable growth rate and how that is going to affect us.
Watch for ICD-10 training and resources. You are going to see a surge in information and exposure in the summer. Please take a look at all those resources and get trained as much as possible before October. You will also want to be familiar with the hopeful expansion of PQRS, which has an increased number of codes in 2015.
Cite this content as:
Cavitt, K. (2014, June). Billing, coding & reimbursement: 2014 update. AudiologyOnline, Article 12707. Retrieved from: https://www.audiologyonline.com


