Editor’s Note: This text course is an edited transcript of a live webinar. Download supplemental course materials.
Dr. Lisa Christensen: Today I will talk about the Cochlear Baha Softband, how to determine candidacy, and how to perform the evaluation and fitting.
Candidacy
Conductive Hearing Loss
We commonly think of patients with permanent conductive hearing loss when we discuss Baha candidacy. These hearing losses may be due to disorders such as Treacher Collins syndrome, microtia and atresia without a syndrome, or Down syndrome, which also contributes to fluctuating hearing loss. These cases can be unilateral or bilateral, but both can be fit with the Softband.
Mixed Hearing Loss
My personal candidacy criteria for mixed hearing loss is a bilateral loss with a bone conductive pure-tone average (PTA) of 35 dB or less for children. They are growing, acquiring speech and language, and we need to access all the soft sounds. I always use a power device with those children, erring on the side of caution so that all of those soft sounds are available for speech. Mixed hearing loss can be unilateral or bilateral, and as with conductive hearing loss, it can fluctuate as well.
Single Sided Deafness (SSD)
SSD is typically a severe to profound sensorineural loss. However, SSD can also present as a profound mixed loss or a severe to profound conductive loss. When we refer to SSD in the traditional sense, we are looking at profound sensorineural hearing losses. I consider SSD hearing candidacy to be 15 dB or better in the normal functioning ear.
This threshold level is not as critical when we look at implanting the Baha, but families still need to know what would happen if the loss progresses in a Softband situation. A Baha processor is easily removed, and if it is implanted, there is no danger to the cochlea. I think it is important to talk to families so that you know the medical history. Perhaps there is an enlarged vestibular aqueduct or something causing the unilateral hearing loss that could be progressive in nature. It is always important to mention that on the front end.
Guidelines: Softbands vs. Implants
There are no age restrictions to using a Baha on a Softband. As soon as we know there is a hearing loss, we can start the fitting process. Bilateral conductive or mixed losses are quick and easy like a traditional hearing aid fitting. I have a bit of a bias on SSD and unilateral losses. I like for those to be fit once the child is sitting up with head control so that we can get the processor behind the affected ear. There are unilateral or bilateral Softband styles available.
Implants are a bit different because of the Food and Drug Administration (FDA) guidelines for a surgical procedure. The FDA guideline requires a child to be five years of age or older to receive the Baha implant. Think of the Softband as the bridge between hearing and surgery.
Frequently Asked Questions
When we look at Softbands, there are two frequently asked questions. First, when can or should a child be fit? Second, how can a Softband fitting be verified and validated? If you are unsure what to do, always follow the guidelines set forth by our professional organizations, such as the American Academy of Audiology (AAA). We will discuss their most recent guidelines that were published in June 2013.
Fitting air conduction behind-the-ear (BTE) aids when anatomically possible is the first choice for many people. If not anatomically possible, they can choose bone conduction hearing aids. As far as reimbursement, demonstrating the inability of BTEs as a viable solution will help you secure Softband funding. I choose to lay both devices out and let the families decide what may be best for them. I have worked with families where the great-grandparents were raising the child, and they had dexterity issues. They did better with the Softband on the child than they did with the BTEs. There may be other family preferences. When the child is a candidate for a Sotband or a BTE, we need to consider letting the caregivers look and make their own decision.
The next big question is when do we fit these children? If it is a bilateral conductive or mixed hearing loss, we fit as soon as possible. We follow the 1-3-6 early hearing detection and intervention (EHDI) guidelines (screen by one month, confirm by three months, and begin treatment or fitting by 6 months), fitting these children with the same urgency as we would a traditional hearing aid. Because there are no age restrictions on the Softband, we can fit it long before we implant. Some of these children will be implanted when they are five years old, but some will receive other surgical intervention, such as atresia repair or stapedectomy, prior to a Baha. Again, sometimes the Softband is the bridge to arrive at the final result.
In the case of bilateral fittings when a sound processor is placed behind each ear, I like to wait until the child has head control. You may find the same with unilateral losses. Many of you know that car seats, carriers, and other infant devices that make it hard to keep something placed behind the ear. When babies are a little older, it is easier to fit those Softbands and to keep them on, particularly once they are sitting well and spending more time upright during the day. Obviously, that does not fall in line the EHDI guidelines of fitting by six months, as some infants only start learning to sit around six months of age. However, it has been my experience that parents have a smoother experience from the beginning when we wait until there is head control.
Two Ears are Better than One
We all know that two ears are better than one. Figure 1 is an aided audiogram for a 4-year-old female with Treacher Collins syndrome. She wears the Divino. We used conditioned play audiometry (CPA) to test her. The black B on the audiogram is for unilateral Baha or bone anchored implant and the red B is for bilateral Baha. It is easy at first glance to see that two are better than one. This patient gets better functional gain at about every frequency but 1000 Hz.
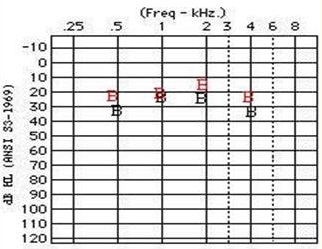
Figure 1. Audiogram from a 4-year old female with Treacher Collins syndrome who uses Divino processors. Black B = unilateral Softband fitting; Red B = bilateral Softband fitting.
Another case is shown in Figure 2. This is a 6-year-old male with Treacher Collins syndrome who wears BP100 processors. You can see that his binaural thresholds in red are better than the unilateral fitting in black. He is a little older and more reliable on the whole.
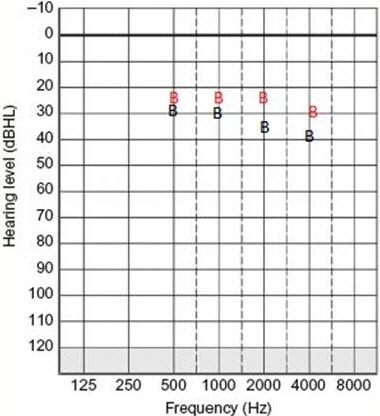
Figure 2. Audiogram from a 6-year old male with Treacher Collins syndrome who uses BP100 processors. Black B = unilateral Softband fitting; Red B = bilateral Softband fitting.
Fitting
Let’s look at how to fit the Baha Softband. We have discussed head control for a more successful Baha fitting, but let’s also think about the placement of that Baha. You may not want to do a bilateral fitting on an infant. It is very difficult to place something behind both mastoids, especially when the infant spends a lot of time on their back, moving their head side to side looking around, which causes the processors to pop off the Softband. So where do we put that processor?
On infants, placement does not always have to be on the mastoid, although we consider it to be the best placement. Many studies, including those that look at auditory brainstem response (ABR) waveforms with mastoid placement versus forehead placement, show that in the beginning, forehead placement is sometimes better than the mastoid. I have had parents who put it on the temple area; some place it in the middle of the forehead. We are looking for anywhere that will stay consistently on the head and give the child access to sound. When these children begin walking and are upright throughout the day, you will want to put the processor in the best placement that you can, likely the mastoid.
Teaching families and other professionals how to place the Softband and keep it on can be a daunting task. When we fit it ourselves, we say to “put it tight, but not too tight”. Helping parents find that perfect fit is sometimes difficult. I like to do functional gain to test how the child will do with a particular fit, and then I show the parents what it feels like on the head. Have them put it on and take it off, and feel of it each time. This is for cases when you have a cooperative baby.
If you want to be highly technical about the exact pressure to use in the fitting, you could use a spring scale. You could also do a search and choose a study that documents how much pressure is needed to be applied. When you show that level, you can teach the parents and the family how to get it back to that level. I think the easiest way do it is to use the functional gain and have the family demonstrate the strap and processor placement consistently. You do not have to tighten or loosen the band every time you put it on and off. The Softband does not have an elastic and Velcro closure; you slide it on and off. You can show them the perfect fit, and as the child grows, the parents will know when to let it out a little bit.
I would like to show you a video of a four-month-old baby at her fitting. You can tell that her mom is holding her up. I had the camera sitting still, but Marley is not sitting still. This is just to show you how easily she will move around and how hard it can be to keep the processor on her mastoid.

I am trying things out, finding out what is too tight and what is too loose. Once I feel like I have a decent fit, I show the mother that the band is not too tight and it will not hurt her, yet it is not so loose that it will slide off every time she moves. Then I will pull it off and get ready to fit the processor on it. I do a lot of that fitting in the beginning without the processor on it because it is easier for me, and if it accidentally turns on, we will not have feedback.
At times, she might want to wear it on her forehead. We will snap on the processor and get everything ready for her. If you move it back behind the affected ear, she is big enough to wear it there while up and sitting. If she is rolling around on the floor or having tummy time, they would most likely have it on the forehead to keep that on.
Verification
Softbands that are fit bilaterally for conductive or mixed hearing losses are like most pediatric hearing aid fittings, except for one big thing: there is no real-ear measurement. Think about these things. Is there a real-ear measurement for a cochlear implant? Did we routinely use real-ear measurements when we fit children in the past? Did we still fit children with amplification? Yes, we did. Do we still fit children with cochlear implants? As pediatric audiologists, we get stuck thinking, “I have to do this,” whether that is real-ear measurements, fitting with certain prescriptive target, et cetera. We are often fearful of doing something that makes us rely on ourselves and our behavioral skills more than we are used to. When in doubt, follow the rules.
State Licensure Laws
What does your state licensure say about pediatric fittings? I am going to show you the Arkansas licensure laws for fitting hearing aids and Baha, but you need to do this for your state. So far, the Softband is more like what we used to have as traditional bone conduction hearing aids. In Arkansas, the current licensure law says there are two ways to fit and verify hearing aids in general. The preferred method is by soundfield testing or by“instruments that objectively measure,” which refers to probe-microphone measurements. They say that probe-mic measurements are preferred, but real-ear-to-coupler differences (RECD) can be used if the patient is unwilling. In the case of using a Softband, or an implanted Baha for that matter, we would use functional gain because there are no real-ear measurements that can be done.
Professional Protocols
The AAA Pediatric Amplification Protocol from 2003 tells us that electroacoustic measurement is the first choice and the second is aided threshold for sounds, but they are not recommended for the following four reasons:
- Prolonged cooperation time from the child is required. This is true. You have to have a bag of tricks when you do extended functional gain testing.
- Frequency resolution is poor.
- Test-retest reliability is frequently poor; (Seewald, Moodie, Sinclair, & Cornelisse, 1996)
- Misleading information may be obtained in cases of severe to profound hearing loss, minimal or mild loss, or when non-linear signal processing, digital noise reduction, or automatic feedback reduction circuitry is used.
All of those will affect how functional gain is presented in the booth. That is also to be included when we look at Baha. We do have to be cognizant of newer digital technology and the changing features when we do functional gain testing.
They go on to look at aided thresholds in sound field. In AAA’s new revision (2013), bone conduction was added, and it says that the aided audiogram is the only way to verify a bone conduction aid. We know that that is the closest thing in the document that relates to Softband fittings.
Figure 3 shows what our Softband verification will look like. I use a B so that I know the response was a Softband or an implanted Baha, rather than a BTE.
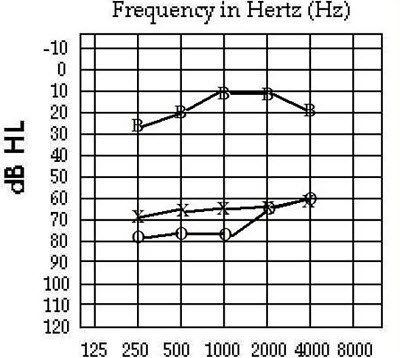
Figure 3. Softband verification, indicated by the B.
Audiological Guidelines
Let’s look through some audiological guidelines. We cannot use RECD, and as such, we have to rely on behavioral testing. The testing skills you need to acquire are as follows:
- Behavioral Observation Audiometry (BOA)
- Visual Reinforcement Audiometry (VRA)
- Conditioned Play Audiometry (CPA)
- Frequency-specific stimuli
- Speech Audiometry
- Physiologic Assessments:
- Acoustic immittance, including tympanometry and acoustic reflex testing
- Otoacoustic Emission (OAE) testing
- Electrophysiologic Audiometry:
- Auditory Brainstem Response (ABR)
- Auditory Steady State Response (ASSR)
When we work with children and infants, especially those with Bahas, we have to be able to elicit behavioral responses. We have to know our patient’s developmental level and what test will produce the specific results that we need. We have to think about reliably testing infants under six months of age. Those are things that many of us do not think about anymore when we use ABR to estimate thresholds, but we have to start to look at some of those things here.
Behavioral Observation
Infants under six months of age (chronological or developmental) who have been fit with a Baha need to be verified using behavioral observation audiometry (BOA). Those aided and unaided thresholds or the functional gain for speech are going to give you the information you need to verify the fitting. It keeps in line with the EHDI 1-3-6 guidelines. We cannot have intervention in place by six months if we do not have a good unaided test or diagnosis of hearing loss in conjunction with an ABR, most likely. We need to secure a proper fitting, which means that we know for certainty how the Softband works on the infant.
If you want to learn more about BOA, look up the article, Testing Babies: You Can Do It! Behavioral Observation Audiometry by Jane Madell (2011). In states where we struggle with loss to follow- up, you may not get babies in before six months. However, these are the infants that are fairly well known because you can visually see the hearing loss in the form of atresia or microtia. They are going to show up earlier than your traditional sensorineural hearing loss, which is more of an “invisible” loss.
When considering VRA and CPA, we have to look at developmental age. Sometimes we can get a 5-month-old up to 24 months with VRA. Getting behavioral testing, especially if you are not doing sedated ABRs, is a lot to demand for a five, six, or seven-month-old. That is one of the reasons AAA says it requires so much time and cooperation. You will have to find some things to entertain these children longer than usual.
These appointments can be long, and many times you do not get everything you need in that one appointment. Moreover, these sessions can be stressful for the parents if the child stops cooperating. Those who work with children on a regular basis know there is a small window of time in which to engage these babies and get reliable information. Think about that in your unaided and aided appointments.
You might look at are different speeds of light around VRA boxes. Several places at Arkansas Children’s Hospital, where I previously worked, had custom-made VRA boxes. They tend to hold a child’s attention a little longer. Use running lights around the outside, two to three animals inside, lights, movement, and any extra things you can come up with. Video VRA may prolong some time with children, also. Working in pairs by having another audiologist as an assistant in the booth will help keep the kids entertained and focused during these longer sessions.
CPA follows the same concept. Even though children are a bit older for this kind of test method, we still need to have many, many different toys in order to keep children engaged and to get all the information needed to do a Softband fitting. AAA has resources on pediatric assessment that you can find here.
Validation
Once the verification is complete, the next step is validation. This website Success for Kids with Hearing Loss provides a wealth of free information that is available for download or print. If you are concerned about cost, you can find free tools. Keep in mind that anything you currently use for validating traditional BTE fittings with children will work well for Softband validation for bilateral conductive and mixed losses. Here are some examples:
- ELF - Early Listening Function
- CHILD - Children’s Home Inventory of Listening Difficulties
- Preschool SIFTER – Preschool Screening Instrument For Targeting Educational Risk
- SIFTER – Screening Instrument For Targeting Educational Risk of Elementary School Children
- Secondary SIFTER - Secondary Screening Instrument For Targeting Educational Risk
- LIFE-R – Revised Listening Inventory For Education
- LIFE – Learning Inventory For Education
- LIFE Student Appraisal
- LIFE Student Appraisal Pictures
- LIFE Teacher Appraisal
- CHAPS- Children’s Auditory Performance Scale
- SAC-A-Self Assessment of Communication – Adolescent
- SOAC-A– Significant Other Assessment of Communication – Adolescent
- FLE – Functional Listening Evaluation
- Children’s Peer Relationship Scale
- Minnesota Social Skills Checklist for Students who are Deaf - Hard of Hearing
- PARC– Placement Readiness Checklists for Children who are Deaf or Hard of Hearing (Colorado)
Unilateral Hearing Loss
If you have a child with a unilateral conductive or mixed hearing loss, you can put masking in the normal ear and test for functional gain on a Softband for verification. However, you cannot do that with a child with SSD because there is only one working cochlea.
For example, consider a child with a profound sensorineural hearing loss in the right ear. If you put masking noise in the left ear with the sound processor on the right mastoid, functional gain will not be very good because you have stimulated the good cochlea with noise.
For a unilateral conductive or mixed loss, you can do this to verify one side because there is still cochlear function on the impaired side. If it was an atretic right ear and a normal left ear, you could put some masking noise in the left ear, put the Softband on the right side, and test functional gain.
SSD
With this population, one of the concerns is localization. Another concern is understanding speech in noise, which can dominate a child’s home and school life. The third concern is the head-shadow effect.
When it comes to infants and children, will the functional gain tell us anything about any one of those three areas? No. Should we still worry about these three factors when there is an emerging trend for cochlear implants for SSD? There was a good article in Audiology Today (Torres & Zeitler, 2013) about a child who was implanted with a cochlear implant for SSD. I think we still need to worry about that, because there are many children who have an absent cochlear nerve, who will still need to consider a Baha for one ear. There are still malformed cochleae where a cochlear implant will not be the most realistic choice for auditory improvement.
Methods
Even with Softbands, we still need to conduct validation. What gives us useful information that can be tested on infants and children? Speech-in-noise testing is one, which can be done fairly easily with most children. We need to make sure that we can verify this prior to our fitting. With regard to infants, I know I have said to use those EHDI 1-3-6 guidelines, but I am going to tell you that if you have a two or three-month-old with a unilateral sensorineural hearing loss, there are very few ways that will work well with that age.
For younger children and some toddlers, we can get body parts with and without noise. You can have them point to their face or body, to their mom, a doll, Mr. Potato Head, or anything else you decide. Doing this task well depends on the language and developmental level of the child.
You could conduct outcome measurements that are easier for the parents, like the ELF or CHILD. Those are appropriate for the parent, speech langiage pathologist or early childhood worker in their home.
When you think back about the licensure law, it does not say that outcome measurements are going to help you. It does not say that is how you are going to continue to practice and keep your license. What do we need to do then? My suggestion is that you wait until you can conduct verification. I know that is a terrible thing to make some of these children wait that long, but you would not put a CROS (contralateral routing of signal) on that child, either. There is no other thing that you would do earlier that would give you any more information or be any more helpful. As I said, wait it out until they are old enough to do some of these things with and without noise so that you have a way to verify.
Unilateral Conductive Hearing Loss
What if the child has only unilateral conductive loss? These cases are not high priority, especially when you talk to some of our surgeons. I had a family who told me several times that the doctor said he was going to fix their son’s hearing loss - when he turned eight years old. That is a fine line that we have to walk as audiologists, because you do not want to undermine the ear, nose, throat (ENT) physician. Most of the time, however, that “fixing”, is often the atresia/microtia repair on the outside; it is the facial plastics procedure that they are going fix and not necessarily the hearing. You need to be very specific with the families and the physicians to determine what is meant by “fixing.”
Be vigilant in educating these families that unilateral conductive hearing loss has been proven to have complications, some long-term, but not as much as unilateral sensorineural losses. A study from Kesser, Krook and Gray (2013) looked at forty atresia patients. Unlike unilateral sensorineural loss cases, none of these children repeated a grade, but 65% of them needed additional resources. Almost 13% used a hearing aid, 32% used an FM system, 48% had an individualized education plan (IEP), and 45% were in speech therapy. There was obviously an indication that some of those children had issues with speech and language and listening and learning, or they would not have been in those services.
They concluded that unilateral, conductive atresia patients do have an educational impact. Those children have delayed performance, even though it is not as profound as a group with unilateral sensorineural hearing loss. They still show educational delays, speech and language delays, and are need of devices to help them. It does matter that it is a unilateral loss, and even in those cases of unilateral atresia, we do need to fit those children.
Data
Now that we have verification and validation, let’s see how this all works together. In 2005, the first Softband study (Hol, Cremers, Coppens-Schellenkens, & Snik) had only two subjects, a three-year-old and a 29-month-old. Hol et al. compared Baha to a standard Oticon bone conduction aid. They found that the Softband was a valid intervention for those children with congenital bilateral aural atresia who were too young for the percutaneous Baha system.
We know that it worked well on two children, but we needed more data. I was involved in a retrospective study (Nicholson, Christensen, Dornhoffer, Martin, & Smith-Olinde, 2011) that looked at patient charts from 2002 to 2006. We pulled charts from about 20 infants and children with a mean age of about 5 years (range = 8 months to 16 years). I want to preface this by saying that sometimes 16-year-olds wear Softbands. One of the particular children in this study was a swimmer that we worried about being in the water so much with a percutaneous abutment. We held off on implanting for a long time. There was also another child who had undergone multiple cleft repair surgeries and did not want another surgery; they were happy wearing a Softband. We see those cases more frequently with females than males because it is a little easier to wear a headband for a girl than a boy.
The inclusion criteria for our study was that they have a bilateral, symmetrical conductive loss, and we fit them unilaterally. We came out with functional gain of about 40 dB across the board and 35 dB in the highs. That puts them in a range to hear more of the speech spectrum, especially for the atretic children with 50-60 dB conductive hearing losses.
We can compare this Softband or implanted performance with that of traditional bone conduction. Some argue that traditional bone conduction aids are cheaper than the Softband. However, we need to look back and see if there is justification for the extra cost.
In a retrospective study, we pulled charts of 10 subjects, ages 6 months to 18 years (Christensen, Smith-Olinde, Kimberlain, & Dornhoffer, 2012). Patients had congenital, bilateral conductive losses. They were fit with a traditional bone conduction device, then a Softband device, and then they were eventually implanted. This was the reason there were only 10 subjects. Most of the children were brought in when we first started to do Baha, and they tried on the Softband and had some exposure to that outside of their bone conduction aid.
Everything was compared back to the bone conduction transducer, which yielded the unmasked bone conduction thresholds from the unaided testing. The functional gain with the Baha implanted was very close to the unmasked bone conduction thresholds. We then compared those results to the Baha on a Softband and a traditional bone conduction hearing aid.
We knew that the functional gain with a Baha would be more, but we did not know what how much more until we looked at the data. We found was that the unmasked bone conduction transducer from the audiometer gave the most gain of any device. The implanted Baha was second best, and it statistically was the same as the bone conduction transducer. The Softband came in third and provided more functional gain than the traditional bone conduction aids.
So why does the Baha outperform the traditional bone conduction aid? I think that some of it is the physical fit. In the past, we had to cut the old metal headbands with a saw to make those fit some of the infants’ small heads. Then they outgrew them and we would have to order a second one. It would slip and move; the Softband is a better, more consistent fit. It is harder to make a custom fit with the metal headband, especially for smaller patients. The Softband can be custom fit it for each child, and I imagine that it also feels better to wear a Softband long-term than a metal device.
Funding
I also wanted to discuss funding for Softband. Funding issues can many times be cleared up by following the steps we have gone through today. If you can show the loss improves with a loaner Baha fitting, you can make great strides with reimbursement. For example, you have a bilateral atresia patient with private insurance through dad’s employer. The plan does not cover Baha, but if you can show the hearing loss with and without the device, then you can objectively document how much better they are hearing with the device. You can write it out for a company and show that the device improves hearing and quality of life.
You can also include published data that is applicable to your case, such as what I have presented today. Functional gain is very easy for someone to look at on an audiogram, especially if you use the audiogram that delineates the levels of hearing loss down the side or includes a speech banana so the reader can understand what the patient is hearing. Speech-in-noise testing will help you when you provide a measurement, like 100% in quiet and only 50% in noise. Almost everyone understands percentages.
Softband Scenarios
Scenario #1
Let’s discuss some specific scenarios for different patients. Scenario 1 is a child with Treacher Collins Syndrome who failed a newborn hearing screening. An ABR was done at three weeks of age. We found moderate conductive hearing loss in both ears. In the past, I had a physician come to me and ask why we did not put a Softband on a child right away. The argument was that the child had atresia, so we knew the loss is conductive. In truth, we do not always know that. That is why the ABR is so important.
We must distinguish conductive from sensorineural components in all children. In the case of Treacher Collins, we would assume with high certainty that the loss would be conductive, but I have had referrals for infants to be fit with a Softband for conductive loss when a confirmation ABR revealed no response. We had one patient with non-syndromic microtia, but after further diagnostic evaluation, we determined she had no VIII nerve on either side. We could have put the Softband on and let her go home from the hospital. Who knows how long it would have taken for us to figure out that she was getting nothing out of that device. Always be thorough with your diagnostic information before you proceed with any kind of fitting.
Back to the scenario, even though we know this patient has Treacher Collins, we do the ABR at three weeks with both air conduction and bone conduction, which revealed moderate conductive hearing loss bilaterally. We did not do unaided confirmation BOA in this case, but did fit a Softband at two months of age. We did need to use BOA to verify the fitting, however. I am comfortable using the ABR as a diagnostic tool, and it does save time in the beginning, as long as the results are consistent. At this point, we only had to use BOA to verify the fitting.
For validation, we can use outcome measures like the ELF or the IT-MAIS. That way we can bring in the caregivers and therapists who regularly work with the child, especially auditory-verbal therapists. The validation is not something that we do the first day because parents need some time to contemplate their thoughts, but it might be something that we hand out at the beginning of the fitting so parents can start thinking about what to watch for.
Scenario #2
The next scenario is an eight-month-old with cleft palate. This age may be more in the comfort zone for most people, because we do not have to use BOA or look for sucking responses. We diagnosed bilateral, conductive hearing loss. With the cleft palate, we can hypothesize that there is fluctuating hearing loss as well. One thing that I like about using a Softband, especially for children with Down syndrome or cleft palate, is that the Baha helps keep hearing consistent by working with a normal bone conduction line. If we had fit this child with BTEs, we would have been in a constant struggle of whether the aids were too loud or too soft as the middle ear fluid changed; the bone conduction line stays the same in the presence of fluid.
We can do VRA or an ABR to make the diagnosis for an eight-month-old. VRA is still applicable, and we need functional gain and validation again. At eight months, we can use some of those early developing skills to verify. For validation, we can look at the ELF or IT-MAIS.
Scenario #3
Here is a more difficult case. This child is six years old with Down syndrome. We can likely still do CPA for age and developmental level. She has a mild, permanent conductive loss due to a middle ear stapes problem, but with Down syndrome, there is ongoing persistent chronic otitis media. In the past, we would have been aggressive in management and fit her with an FM system for school. We are hoping that she is seated close to the teacher, because she is not completely mainstreamed. When she is mainstreamed, we can hope that the soundfield system will overcome the background noise and larger class size.
If we put BTEs on the mild loss, then we would be juggling too loud and too soft, as in the cases of otitis media. These children fluctuate between good hearing and poor hearing as the fluid fluctuates. Again, when you use the Softband, those concerns can be mitigated because you know it is working directly with bone conduction and is not reliant on air conduction thresholds.
To verify, we would use CPA. We have decided that the conductive hearing loss is more severe than what is being managed with tubes, and we are going to try a Baha on a Softband. If the child is high functioning or a normal six-year-old with cleft palate or other straightforward conductive hearing loss, the teacher could complete a LIFE for the educational setting. We could have the child fill out the student version in some cases. We could also do a CHILD. In this case, we are probably only going to get the LIFE from the teacher and the CHILD from the parent. This is assuming that this is a patient for whom we are just starting intervention. Unfortunately, that does happen frequently.
Conclusions
In conclusion, we should fit Softbands early. It might not mean a bilateral fitting initially; that depends on the developmental status of the child and the age of identification. Even children with bilateral conductive losses may have a unilateral fit in the beginning. You can move to the bilateral Softband later when the child has improved head control. It might also mean using an alternative processor placement, such as the forehead. It is not ideal, but it will get us through to the next level until we can place it where it needs to be for the long term.
Aided testing is a must for verification. You are going to use the same outcome measures as you would for any other hearing aid validation. You are going to use things that work well for children. When you are using a validation measurement for a child with a SSD, look for ones that focus on listening skills, such as the CHILD.
Let’s use bilateral Softbands and see if we can get a little more research on them. It is great that I can compare and show where children are hearing better with two processors over one, but I would love to see many more cases that we could pull together for more data.
Questions and Answers
What types of stimuli do you typically use for soundfield testing?
I use a both narrowband noise and warbled tones. It depends on the child and what allows them to attend longer. I make notes on the audiogram which one I have used.
We have found that you can end up with interactions with the more advanced signal processing and automatic functions. Sometimes noise is a better stimuli if you are trying to get the lowest threshold.
References
American Academy of Audiology. (2013). American Academy of Audiology clinical practice guidelines: Pediatric amplification. Retrieved from https://audiology-web.s3.amazonaws.com/migrated/PediatricAmplificationGuidelines.pdf_539975b3e7e9f1.74471798.pdf
Christensen, L., Smith-Olinde, L., Kimberlain, J., Richter, G., & Dornhoffer, J. (2010). Comparison of traditional bone-conduction hearing aids with the Baha system. Journal of the American Academy of Audiology, 21(4), 267-273. doi: 10.3766/jaaa.21.4.5.
Hol, M. K., Cremers, C. W., Coppens-Schellenkens, W., Snik, A. F. (2005). The BAHA softband: A new treatment for young children with bilateral congenital aural atresia. International Journal of Pediatric Otorhinolaryngology, 69(7), 973-980.
Kesser, B. W., Krook, K., & Gray, L. C. (2013). Impact of unilateral conductive hearing loss due to aural atresia on academic performance in children. Laryngoscope, 123(9), 2270-2275. doi: 10.1002/lary.24055.
Madell, J. R. (2011). Testing babies: You can do it! Behavioral observation audiometry (BOA). SIG 9 Perspectives on Hearing and Hearing Disorders in Childhood, 21, 59-65. doi:10.1044/hhdc21.2.59
Nicholson, N., Christensen, L., Dornhoffer, J., Martin, P., & Smith-Olinde, L. (2011). Verification of speech spectrum audibility for pediatric Baha Softband users with craionfacial anomalies. Cleft Palate-Craniofacial Journal, 48(1), 56-65. doi: 10.1597/08-178.
Seewald, R. C., Moodie, K. S., Sinclair, S. T., & Cornelisse, L. E. (1996). Traditional and theoretical approaches to selecting amplification for infants and young children. In F. Bess, J. Gravel, & A. M. Tharpe, (Eds.), Amplification for Children with Auditory Deficits (pp. 161-191). Nashville, TN: Bill Wilkerson Center Press.
Torres, J., & Zeitler, D. M. (2013). Cochlear implantation for single-sided deafness in a child. Audiology Today, 25(5), 28.
Cite this content as:
Christensen, L. (2014, December). The Baha Softband: candidacy, evaluation and fitting. AudiologyOnline, Article 13117. Retrieved from: https://www.audiologyonline.com