This text course is an edited transcript of a MED-EL live webinar on AudiologyOnline. Download supplemental course materials.
Learning Objectives
By the end of this course, you will be able to understand the intrinsic and extrinsic factors that impact listening and spoken language outcomes, describe three categories of listening and spoken language outcomes, and discuss appropriate communication pathways for communication development.
Structure versus Function
In order for the communication system to work, you first have to have the anatomical structures in place. Then you have to have the function, which is more of the skill required to make those structures work. I look at it as the audiologists and/or the surgeons are tasked with the structure. They provide amplification or the surgical correction including cochlear implants to bypass poor or absent structures that may not be working.
Then it is the task of the teachers of the deaf, speech-language pathologists, early interventionists and audiologists to deal with function, which is how we go about developing the listening and spoken language skills. This also includes working with the parent or caregiver so they are part of this process.
Structure
Structure would include cochlear implants, such as MED-EL’s new Synchrony CI system, which has the RONDO or SONNET audio processor with the fine tuner, and structure can also be hearing aids.
Function
Function, in this case, means auditory development. Norm Erber coined the phrases of auditory development back in the early 80’s as detection, discrimination, identification, and comprehension. This is what we work on for a child or an adult who is deaf and does not have access to sound. We want to provide them with the structure, so we fit hearing aid or they receiver a cochlear implant. Then we have to develop the function, which will be how well they can detect, discriminate, identify, and comprehend sound to which they have access.
Outcomes/Expectations
For a child or an adult who receives a cochlear implant, we are looking at their ability to develop listening or auditory skills. In the last few years, many different terminologies have been passed around such as auditory skills, listening skills, aural skills, verbal skills, et cetera. What I am talking about is all the same. We are looking at an individual’s ability to develop their auditory or listening skills as well as their verbal or spoken language skills. When we provide structure in the form of amplification, we are specifically looking at their new access to sounds, how well are they able to listen and understand, and how well are they able to utilize the cochlear implant to develop speech production, articulation intelligibility skills and verbal language skills.
Not everyone who receives a cochlear implant has the same kind of outcomes, but we do want to hold our expectations high so they can achieve their best potential. I will talk about a Children’s Implant Profile (ChIP) that we can use as a counseling tool to identify and discuss factors that may impact outcomes so we can set realistic expectations. As a side note, it is necessary to teach individuals who are profoundly deaf how to listen. We all know that as wonderful as cochlear implants are, we cannot put them in, walk away, and expect the child or adult to develop listening skills. They need to have auditory practice.
Communication Options
How do we go about developing detection, discrimination, identification, and communication? For children, it starts with the communication option that they are going to use. This is part of counseling for parents. We need to let them know all of the options so they can make informed decisions. Their choice should not be solely based around what the school program offers; parents should have the full array of options.
NCbegin.org, the Beginnings for Parents of Children who are Deaf or Hard of Hearing Inc., has put together what I consider to be the most comprehensive chart, which compares all the options in a non-biased way. They give a definition, talk about the primary goals of each of the approaches, discuss what is expected for receptive and expressive language development, what is expected for hearing, as well the expectation of involvement by the family or primary care giver.
I am going to go through the main options from their chart, in no particular order.
American Sign Language
American Sign Language (ASL) is categorized as a visual approach. They talk about it as a bilingual approach, which includes development of ASL and English. ASL is a natural, manual, visual language that has its own grammar and linguistic principles. English is addressed through the use of teaching strategies for English as a second language.
The primary goal is that the individual would acquire age-appropriate internal language as a basis for learning a second language and opportunities for academic achievement. It is to provide a basis for learning written and, when possible, spoken English as a second language. The primary language learned would be ASL. To add to that, when it comes to the hearing, they state that it encourages individual decisions about amplification. Some individuals choose to have amplification, and some will not.
Auditory-Verbal
On the other end of the communication spectrum is auditory-verbal, which you have may heard of as listening and spoken language, which is an older term. This is purely an auditory approach. It emphasizes spoken language development through listening, one-on-one therapy, and use of the residual hearing with optimal amplification. The child does not rely on visual cues.
The primary goal for the auditory-verbal approach is to develop spoken language through listening by following the stages and sequence of typical development. Another goal is to develop the skills necessary for successful mainstreaming in school and integration into the hearing community. Their attitude when it comes towards hearing is that early, consistent, and appropriate of hearing technology is critical to this approach. For ASL, it was about individual decisions. If you are going to follow the auditory-verbal communication approach, then you would be counseled heavily that appropriate use of technology and consistency is critical.
Cued Speech
Cued speech is another option, which they consider to be a combined approach. It is an auditory-visual communication approach that combines a system of hand cues with natural mouth movements of speech, specifying each sound. The hand shape, which gives you the consonant groups, at a location, which gives you the vowel groups, cues a syllable.
The goals for this are to provide clear communication in spoken language of the home, develop the phonemic language base, achieve full literacy in conversation, reading, and writing, and support speech reading, speech and auditory skill development. When it comes to hearing, they state early, consistent, and appropriate use of hearing technology is important to this approach. Remember that for auditory-verbal, they said that use of hearing technology was critical. In cued speech, it has dropped down to important to the approach.
Auditory-Oral
The auditory-oral approach is deemed as a combined approach. They define it as teaching a child to use remaining hearing through amplification and using speech reading, natural gestures or visual cues to aid in the understanding. However, the visual cues are not sign language cues. It is more of gestures, reading, and speech reading.
The primary goal is to develop spoken language through listening and visual cues (not sign language), to develop spoken language and communication skills necessary for school success and integration into the hearing community, and early, consistent and appropriate use of hearing technology is important.
Simultaneous Communication
The last main option is simultaneous communication. I believe this was previously called total communication. It is an educational philosophy that uses spoken language and sign language simultaneously. We are talking about Signing Exact English (SEE). ASL and spoken English are not compatible due to word order and grammatical differences between the two languages. Simultaneous communication uses an English-based sign language which can include speech, speech reading, finger spelling, natural gestures and use of residual hearing.
The primary goal is to provide a bridge to the development of spoken language in the very young child. It is to provide communication between the child and his or her family, teachers, and peers using sign language. It is to support integration into both the hearing and deaf communities, and when it comes to hearing, consistent appropriate use of hearing technology is strongly encouraged. Not all children can benefit from each of the different approaches, based on the different factors that impact their outcomes.
Cochlear Implant Recipients
For ease of this presentation, I have categorized patient population into two groups: children and older recipients. When I talk about children, I am talking about those who are usually no older than 5 to 7 years of age. These are children who have most likely not developed auditory skills or verbal language prior to getting a cochlear implant. There may be some minimal skills with hearing aids, but they are severely to profoundly deaf, and could not get the access to sound through their hearing aids and required a cochlear implant. Now we are working on developing their language through habilitation.
Older recipients are those who have likely developed at least functional verbal language. They have already developed listening skills and language, but have lost the skill to progressive loss, sudden hearing loss or meningitis, et cetera. They have had the skill, and now we have given them structure with a cochlear implant to get back to the function. We are rehabilitating, not teaching them language for the first time.
Children: Intrinsic Factors
There are many different factors that influence different outcomes. The intrinsic factors are those with which the child comes to us; you cannot change those.
Duration of Deafness
One will be age or duration of deafness. If the child is two years old and they have been profoundly deaf since birth, then that is two years duration of deafness. If we have a child who is seven years old and they had a progressive loss, they would have an age of seven, but the duration of deafness would be slightly less because they had access to the ability to develop listening and spoken language if they had been appropriately amplified before their hearing dropped into the severe or profound range.
We all know that less duration of deafness is better. I can point to the work of Anu Sharma (2005) that showed children three-and-a-half and under can have a P1 latency that looks the same as children with typical hearing. Fifty percent of children with deafness who are three-and-a-half to around five-and-a half will have a P1 that looks the same as children with typical hearing, and the other 50% will not. None of the children who were six-and-a-half to seven years of age and older had the P1 that looked the same as children with typical hearing.
If you were seven or eight years of age and you had never had access to sound, then they would say that your brain was starting to reorganize, and the auditory pathway was not stimulated. Structure falls into the function. We know that younger sound stimulation, and in this case implantation, is better.
Pre/Post-Lingual Deafened
This is the same thing. Even if you have a hearing loss but have appropriate amplification whereby that pathway is stimulated and you are able to develop some auditory skills or verbal skills, it is a better indicator for outcomes than if you did not have access to sound and had not developed any lingual skills.
Medical Findings and Etiology
Medical findings come into this. Are there other issues going on? What is the health of the child? The surgeon will look at that. Is hearing loss the only issue, or are there other complicating matters going on? Is the hearing loss due to the hair cells or is there an issue with the nerve?
Neural Survival
We would love to have a full-functioning, robust auditory nerve. It is a bit hard to test how well the nerve is functioning. This is where we have to look at behavioral function when we have children with auditory neuropathy and are considering providing them with cochlear implants. Maybe they are getting a signal going through, but how clear is that signal? Are they just getting enough to have detection of sound or are they getting enough to have complete discrimination of sound? Maybe the discrimination is only length difference, but they cannot get enough acoustic information to hear that “oo” and “ee” are different sounds.
Maybe the child has awareness of “oo” and “ee”, and if you do a length difference “ee” versus “oo oo oo”, the nerve is passing that signal along. But when you do “ee” versus “oo”, it is not giving enough information, and those sounds appear to be the same. It is important with children, whether their diagnosis is auditory neuropathy, Mondini malformations, common cavities, and other structural issues, to not only look at function, the detection, but also how accurate their discrimination is.
Neural survival is important, although our current tests to define it are still weaker than we would like. We look at CAT scans or MRIs and know that the presence of a narrow auditory internal canal very well puts that child at risk for having an absent nerve.
Cognition
We want to know the child’s cognitive abilities. It will certainly come into play for developing some of the skills.
Additional Disabilities
Does this child have hearing loss with a concomitant disorder such as autism? What about blindness or other motor disabilities? Those will certainly impact language outcomes. We need to look at the whole child.
Children: Extrinsic Factors
Extrinsic factors are ones over which we have a little more influence.
Functional Use of Hearing Aids
One is functional use of the hearing aids. When we get this child, have they been identified? Have they been wearing hearing aids, and if so, has someone been working with the child to develop listening skills? It is not just enough to put the hearing aids on a child and send them home. You have to have some services to focus on developing listening skills. It does not happen automatically for hearing-impaired children. You have to work at it.
Communicative Intent
Communicative intent of the child or of the adult will come into play. This makes a difference if there is diagnosis of autism, but also I have seen children, who because they do not have access to sound, shy away from language. They do not understand what is going on, and when someone starts talking to them, they will look away, so people may think that they fall onto the spectrum. These children have received implants and access to sound, and a year later, there is a completely different personality in the child. We do not want to say that because they do not have great communicative intent that they have autism. We do need to look at what their communicative intent is.
Availability of Habilitation Services
As I stressed already, habilitation services are key. Are there services available for each patient?
Educational Program
Is the educational program willing to be somewhat flexible or work with the family if they only want to work on listening skills? Is there even a program like that for children with hearing loss? This is small incidence population, and in some very rural areas, this might be the only child who has a hearing loss. They end up placing them in a special education program with a special education teacher who may not know anything about deafness. The peers in the child’s classroom are children who likely have cognitive or intellectual disabilities, autism, and other things going on. That is not appropriate for this child who just has hearing loss or deafness as their only challenge.
Behavior
We need to look at the child’s behavior, attention and focus. What is their workability scale? How hard do I have to work at getting the child to focus and be in joint attention or a thinking place with me? They may be playing with a toy and I can be talking about it. I can be inputting the language of what they are doing and what they are playing with versus a child who flits from one to the next to the next. If they are constantly moving with a short attention span, they are not getting any language in there.
Parental Involvement
Parental involvement is paramount. How much follow-up and hard work is a parent going to be doing with the child? Do they understand their role in this journey of cochlear implantation? What is their compliance level? How is their follow-up? What are other stressors in the family? We are expecting the parents to do a lot and to be the primary teachers of the child. They may even have to learn a second language such as ASL. Do they understand the time and energy commitment that this is going to take? The same goes for developing listening and spoken language.
If this is a single mom with children, is that a lot to deal with? If this is a family who has other children with special needs, this can be a large stressor in the family. It becomes difficult to spend the amount of time needed on the child with hearing loss. We need to take a look at all of that and help with as much as we can.
What is their support system? Are they new to the area with no other relatives around to help? Do they have extended family members or friends that are helping in this whole process?
Older Adults: Intrinsic Factors
For older adults, we look at some of the same things. We look at the duration of deafness. If they lost their hearing at eight years of age and they are now 46 and have decided they want an implant, we have to do some counseling about their expectations about auditory benefit and skills. If a 62-year-old with a progressive hearing loss has another drop that now prevents them from getting enough access to understand speech, there will be a different outcome.
The medical findings are equally important. We are concerned with their overall health at this age and the etiology of their hearing loss. We talked about cognition and additional disabilities in children; this is the same in this case.
Older Adults: Extrinsic Factors
Functional Hearing, Compliance
Extrinsic factors include the functional use of hearing aids or residual hearing. An example may be if you were identified with a hearing loss and had hearing aids when you were young. When you became a teenager, you stopped wearing hearing aids and have not worn them in the last 30 years. If you are an audiologist working with adults, that is not an uncommon story. That is part of the compliance with amplification. Have they been wearing hearing aids and stimulating those auditory pathways or have those auditory pathways been sitting for an extended number of years?
Availability of Services
For children, the availability of habilitation services can be an issue depending upon where they live, but the law states the education department or the state health department must provide educational programs for children zero to three that meet certain criteria. They get early intervention and they go to specialized preschools and services in the school. When you get to be an adult, it is a different story.
Maybe the insurance companies will cover the cochlear implant surgery or the devices, but when it comes to the therapy or follow-up services, there are far fewer insurances that cover it for adults. Even if it is covered or if adults are willing to private pay for it, there are far fewer places to find rehabilitation services for adults. They are readily available for children. When it comes to adults, some of the implant centers will provide follow-up therapy, but I know there is a problem all over the U.S. finding professionals who will work with adults on developing auditory skills once they have received a cochlear implant. They are not as abundant as pediatric centers, however.
Commitment to Practice
I think this is a huge piece when counseling adults. Some adults have an expectation that they will get the implant and then in the next few weeks, they will be hearing like they did before. They must be counseled that learning to listen with an implant takes practice and time.
Family Dynamics
That goes right into the family dynamics and the social situation. Do the communication partners in the family understand that the patient will not suddenly hear normally? They cannot talk to the patient and expect them to understand everything. Are they willing to put in time, practice, patience, and energy to help this individual develop some listening skills? Is there even someone available who can be the communication partner? We have to look into that.
Children’s Implant Profile - Modified
You may be familiar with a ChIP, or Children’s Implant Profile, which was developed years ago. There are now many modified versions. In the last 20 years, everything has changed about cochlear implantation from the incision of the surgery, the time of the surgery, the programming, even how we approach doing therapy with children and adults. It has been a growing field where we started off in infancy in the early 90’s and we are learning, adapting and changing.
The same thing goes with implant profiles. Centers that I know use it have adapted it to meet their center’s needs. It is a great counseling tool to have something written down to show families or individuals the strengths they have and challenges that might impact their outcomes. You can talk about what those outcomes may be.
The profile is usually divided into five sections. You score these as no concern, some concern, or great concern. It is not a numbered questionnaire where you quantify some kind of score. It is an overall profile of the strengths and the challenges.
We have been working on a modified, basic ChIP. I will provide you some examples and give you practice with it so you can have an idea of the different factors and what it is like to try to rate them. It is not as black and white as you think.
For adults, we want to be able to look at the medical history, the physical health, the radiological reports, the duration of deafness, the audiological profile, the functional use of amplification, speech and language performance, their verbal skills and listening skills, speech production, and if they have minimal listening or spoken language skills. What are their visual language skills?
Do they use speech reading or have they developed an extensive sign language communication, or do they use rudimentary gestures with no language base? We are interested in their reading skills. What is their family structure and support, everyone’s expectations and commitment to rehabilitation? What is the availability and the skill of the person who would be providing the services?
Pediatrics: Age, Medical
There is also a profile for the children. We look at chronological age (younger is better), duration of deafness (shorter time is better), medical/radiological (Mondini aplasia or common cavity) to see if we can get a full electrode array insertion for cochlear implantation.
Audiological
You will need the audiological assessment and information about the ability to test the child, because that will blend into the ability to program the implant. If you have a child who is very active with a short attention span, they are not easy to test and they are not going to be easy to program. You may not get much time with the child so it helps to be able to plan from the beginning how you will best use their “good” time.
Residual Hearing
What are they using for amplification and residual hearing if they are wearing hearing aids? Do they use it consistently? I get concerned when I see a child that should have access to sounds, yet they are not doing anything versus the child who is using every decibel, tuned into hearing and wanting to use it.
Speech and Language
As far as speech and language are concerned, we are looking at their nonverbal skills and their verbal skills. Particularly when you have very young children that are candidates for cochlear implants, ask what you think they will do with a cochlear implant. You want to look at their listening in spoken language, but they have been profoundly deaf since birth, and they have very minimal skills. You could possibly administer the PLS (Preschool Language Scale), which gives you an age-equivalent score of receptive language and expressive language. But also look at the nonverbal language such as following gestures, pointing, and some of the communicative intent. There are skill levels associated with these.
You might find out that their nonverbal language falls solidly in the 12 to 15 month range and they are using gestures such as “up” and “give it to me.” If the child is doing this, then you have a better sense that they are not as far behind in their language; they have some symbolic language or pre-symbolic language, they just do not have access to sound.
Play Skills
We also look at their play skills, because play and language are very compatible and develop similarly. If a child is showing play skills appropriate for their age, this will give more insight into their development.
Behavior
We look at their attention and behavior for language. How hard do I have to work at being able to be in the thinking place where I can talk about language? Are they watching me and trying to do the gesture while hearing me say the language at the same time? Or is this a child who takes the block, throws it, and runs to the other side of the room and is off to something else?
Other Factors
Multiple handicaps will impact outcomes. Family structure and support will play a significant role in outcomes. It is very important that parents are involved. A child will not meet their potential if the family cannot follow through and be part of the process. The educational environment is important. The skill level of the service provider is also important. There is a different skill set into developing the auditory skills.
With the older population, I talked about the availability of support services and the expectations of the family. Do they understand hearing loss and what technology can and cannot do? We have looked at cognitive and learning style; how teachable is the child?
Expectations
Through experience, we have seen three different categories of outcomes. The first one we call comparable, the second is functional, and the third is assist. Keep in mind that there is a range within each category, and a child is not necessarily held hard-and-fast to one category. With the quality or quantity of habilitation, a child can change.
Auditory skills can fall in one category and verbal skills can fall in another. If you have cerebral palsy with motor involvement, oral-motor issues and dysarthria, clearly that will impact your speech production skills. You may have comparable for auditory, but you might have assist for speech production.
Case #1
Case number one is a child who is 12 months of age, diagnosed at birth with profound, bilateral sensorineural hearing loss, received hearing aids at six months, and the MRI showed no structural abnormalities. The child has no other issues.
The family has extended family nearby. The father works eight hours a day, and mom is a stay-at-home mom. Audiological testing was done at 12 months using behavioral observation, which would be appropriate, and they got reliable results. The child is able to follow some simple gestures and uses gesturing and pointing to communicate.
The child received services from a speech-language pathologist in the area once a week, but the individual has no experience with hearing loss, is willing to learn, and the school district is in the process of hiring a teacher of the deaf. The family has done much research on their own and have extensively questioned the doctors and audiologists regarding hearing loss and their options.
When we look at a child like this from the standpoint of a profile, the only two things that might be of concern are the educational environment and availability of support services. When we see a child like this, we think of comparable communication. We would expect this child to develop listening and spoken language or oral skills comparable to peers with typical hearing. Deafness is the only challenge, and the skill development can take place in a natural environment, top down. Academic learning should be in the mainstream with minimal to moderate support.
If we were looking at an adult in comparable communication, we would expect them to develop their listening skills to the levels acquired prior to their hearing loss; they would be more age-appropriate, be able to use their implant to converse easier in situations including some background noise.
For the child, the communication pathway could focus on the development of spoken language through listening. The auditory-verbal or auditory-oral approaches would be appropriate, in that they are able to access communication without the need for manual or visual means. They would not need sign language or cued speech. That is not to say the family would choose that as their option, and that is fine. However, I am saying that if they were considered to comparable communication, we would expect that they could access communication through listening alone, and they would not need manual support. If the family wants them to learn to be bilingual, they can certainly choose that option.
Case #2
The second case is a child who is two years and 10 months old. The child was diagnosed at birth with severe to profound sensorineural hearing loss and received hearing aids at 18 months. We would automatically wonder what happened to the child for those 18 months before hearing aids. The MRI showed no structural abnormalities, and there are no other health factors.
They recently moved a significant distance away from other family members. They do not know many people in the area. The testing utilized behavioral observation with some inconsistent results. The child had a lot of false responses. He was easily distracted and required a test assistant. The child is using pointing and gesturing with some pushing and pulling. He receives services once weekly for 45 minutes from a teacher of the deaf. The teacher reports the child has a somewhat short attention span. Mom sits in the session, but minimally participates.
The public school has two different preschool classes; one is oral and one is simultaneous communication. The family has some understanding of hearing loss and cochlear implants, and feel that the cochlear implant will provide the child with normal hearing. The child has been exposed to some signs, but requires much repetition to learn and did not readily use the signs. He instead continues to point to indicate his wants.
We look at the profile and start to see we have some areas that are of no concern and some areas that are of mild or moderate concern. It is not the same type of profile as the first child. We see a few more challenges and might consider this more of functional communication. We would expect this child to develop listening and spoken language skills, but maybe not to the level of typical hearing peers; that it is not done with ease. It might require more intensive support, and there might be other language issues.
We would expect him to enter what we call a modified mainstream. They are in the mainstream, but they have a lot of support services, usually with a teacher of the deaf, speech-language pathologist, even a reading specialist. Sometimes they may be in the regular school program, but have a special class while also getting a resource specialist or maybe even English as a second language. The barrier is more language learning rather than access to sound. It is more appropriate using a simultaneous top-down and bottom-up approach.
For an older recipient who is considered functional communication, we would expect they would have improved ability to converse in some situations. They may improve some vocabulary and language. It would help improve speech reading, speech production or vocal tone, but would not be with the ease that an adult with a comparable communication would experience.
For a child in the category of functional communication, an appropriate pathway would focus on development of spoken language through listening, but may include multimodality approaches, with some of the visual cues such as speech reading or gestures. It could include auditory-verbal, auditory-oral, cued speech or simultaneous communication.
I will give the caveat that if you are going to go with cued speech or simultaneous communication, there needs to be equal emphasis on the manual and the listening communication. If the family is not going to be committed to being fluent in manual language, then we have to be very careful about this approach. We do not want to have the child be jack-of-all-trades and master-of-none. Pick something in which you are going to be very fluent and expose that child to a fluent language.
Case #3
The last case study is a child who is five years and nine months, was initially tested at three and a half years and diagnosed with profound bilateral sensorineural hearing loss. The child was not seen again until five years and nine months. They recently moved to this country, do not have hearing aids, and the MRI showed no structural abnormalities. The family has many extended family members living close by.
The testing at five years and nine months used play audiometry, but the child required extensive training to learn the task. The child is using a lot of gesturing and pointing to communicate with some made up signs, but does not attempt to read lips. The child generally follows pointing or routines, but has no interest in other types of communication attempts.
The child does not yet attend any educational program or receive any services, as there are no services available in their area. They have improved understanding of hearing loss and cochlear implants, but still need much counseling from an audiologist. The child is socially engaging and attempts to communicate with family and strangers using gestures and pointing. The child is very visual, watches to see what is expected and will follow easy visual routines.
At this age with minimal language, we would call this an assist communication. This child would be expected to develop some listening and spoken language skills to assist communication, but primary communication needs to be through visual means. These children may be outside that suitable range of implantation or have multiple disabilities so we want to keep that whole-child perspective with realistic expectations in mind. He or she would require more of a multimodality approach with a self-contained classroom rather the mainstream environment, and reaching the point of personal best will be slow and laborious. The educational program needs to take into consideration the primary disability of the child and if the child has other challenges such as autism, intellectual disability or developmental delay.
Older recipients who would be in this kind of category would have some increased ability to speech read, may show environmental sound awareness and some speech awareness, but they would have more difficulty comprehending speech or language.
Appropriate communication pathways would emphasize the multimodality learning approach. Senses other than hearing are going to be the primary learning modality. Those are required to access communication. This can include American Sign Language, cued speech, and simultaneous communication. You can use techniques, but not the approach of auditory-verbal or auditory-oral because it would not give the individual the potential to develop as much communication as they may possibly have.
It may also include augmentative alternative communication or for an individual with autism using PECS (picture exchange communication system) or other appropriate approaches specific to the individual’s needs. It is appropriate to develop the listening and verbal skills to a basic level. We do not want to just say they are not a candidate for an implant; they can use that to assist.
Activity
I am going to give you a chance at doing a ChIP on a child. The child is four years, one month, and was brought to the audiologist with concerns that the child can no longer hear. The parent reported that up until about age three-and-a-half, he would follow simple, routine directions and use some single and two-word utterances or approximations, but the speech was not clear, and then it started to decrease.
At four years, one month, about six months later, they brought the child in for audiological testing and it revealed a profound bilateral sensorineural hearing loss. The MRI showed no structural abnormalities. The family has many extended family members living around who are involved. They used play audiometry, and the child’s results were deemed to be reliable and valid. The child used some previously learned single and two-word utterances, but has not added to that expressive language in the last six months. He follows gesturing and pointing, and appears to understand some lip reading of simple utterances like come here, stop, and no.
The child does not attend any educational program or receive any services. There is a preschool program in the area that works with children who have hearing loss. The family has a simple understanding of hearing loss and cochlear implants, but still need much counseling from the audiologist. The child plays appropriately with toys, but his attention is fleeting and needs much redirection to stay focused on a task that is more parent driven. How would you categorize this child? Figure 1 shows this child’s modified ChIP.
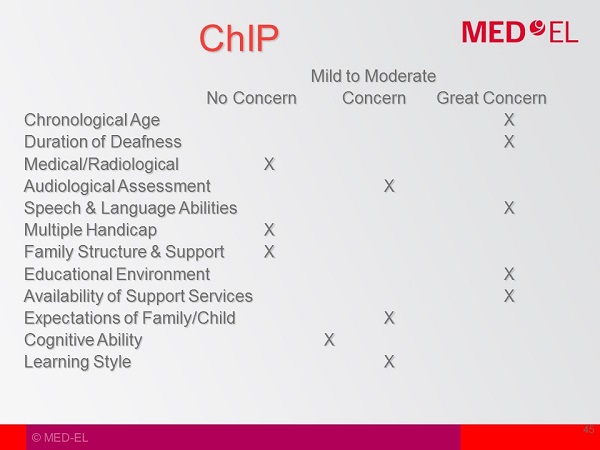
Figure 1. Modified ChIP for case activity.
Chronological Age
Chronological age is rated as mild to moderate. Even though he is four years, one month, clearly he had some kind of access to sound, because he developed some listening in spoken language up to three years, six months. It was not age-appropriate, and we do not know if he had a moderate loss or if there are other issues going on.
Does he have a language disorder and is that why language is behind? He clearly developed some listening and spoken language, so therefore, I marked this as mild to moderate. If you were four years one month with no language, then I would mark it as great concern.
Duration of Deafness
Duration of deafness is mild to moderate. The child had some language development up to about three-and-a-half, and then six months after that did not add to the language base and identified with profound sensorineural hearing loss.
Medical/Radiological
Medical/radiological is not a concern. The MRI showed no concerns.
Audiological Assessment
This not a concern. I think they were able to do appropriate play audiometry, and the results were valid and reliable.
Speech and Language
I marked this as mild to moderate. Again, the child had developed some language up to three-and-a-half years of age. It was not quite appropriate, but he still had developed some language.
Multiple Handicaps
No concern, as there are no other handicaps.
Family Structure and Support
Not a concern. Extended family are near and involved.
Educational Environment
This is of great concern because he is not receiving any services, but there is one available in the area.
Expectations
I marked this as mild to moderate as parents need more understanding.
Cognitive Ability
Cognitive ability did not seem to be a concern.
Learning Style
I marked mild to moderate. He needs a bit more direction. That could also be a child who cannot hear and does not want to be parent directed because he does not understand what is going on.
These are areas that we look at as concern. It does not mean that they all come to fruition. I would have placed him as a functional child with the possibility to be a comparable child. If parents do not follow through or get him into a program, he could drop down to an assist. This gives you an idea of looking at the different factors and how to project outcomes.
Resources
The LittlEARS Auditory Questionnaire looks at the first 24 months of auditory development so you can see if a child is developing skills appropriately. The LittlEARS diary also looks at the first 24 months and asks great questions about auditory development.
Auditory Skills Checklist is 27 questions and can be used with very young children up to adults, because it follows the auditory hierarchy of detection, discrimination, identification, and comprehension. You can know where the individual is and where they may be having breakdowns in their communication.
The Common Objects Test looks at auditory memory. Can they follow one key-word or two key-word directions?
The EARS (Evaluating Auditory Responses to Speech) is a great resource for schools, and it does the same thing. It is a battery of tests and goes from detection to discrimination to identification to comprehension. It is great for teachers or audiologists in the schools to use.
The TeenEARS is used for teenagers and is comprised of seven tests and one questionnaire. It also looks along the auditory hierarchy.
Conclusion
We want to look at the whole individual, not just the ears. There are both intrinsic and extrinsic factors when we are looking at performance outcomes. Some of these factors have more of an impact than others, and you start to get three different outcomes: comparable, functional and assist.
Comparable will develop listening in spoken language skills typical to their hearing peers. Functional will develop listening in spoken language, but it is not done with as much ease and may not be quite to the level of their hearing peers.
Individuals that need more multimodality and have other issues going on or are outside of the ideal range of implantation are considered assist to communication. There is a range within each of these categories, and you can certainly change categories depending upon the circumstances. We want to set our expectations accordingly, and we want to consider the different communication options that will meet the individual’s needs and potential.
References
Erber, N.P. (1982). Auditory training. Washington DC: AG Bell Association for the Deaf.
Sharma, A., Martin, K., Roland, P., Bauer, P., Sweeney, M. H., Gilley, P., & Dorman, M. (2005). P1 latency as a biomarker for central auditory development in children with hearing impairment. Journal of the American Academy of Audiology, 16(8), 564-573.
Cite this Content as:
Therres, M. (2015, October). Auditory development series: factors that impact listening outcomes. AudiologyOnline, Article 15466. Retrieved from https://www.audiologyonline.com.

