Editor’s Note: This text course is an edited transcript of a live seminar. Download supplemental course materials.
Many hearing aid fitting techniques that have been developed over the years have been built on the assumption that hearing loss is similar between the two ears. However, when you approach a case of asymmetrical hearing loss, the fitting path is a bit less clear. There is a good amount of dated literature on fitting asymmetrical hearing losses, but not so much that I can recall recently. In preparation for this course, I reviewed a book chapter by the late Bob Sandlin and Rose Giovanni in one of Michael Valente’s (1994) books, to which I will refer in the course of this presentation. In his most recent Hearing Aids book, Harvey Dillon (2012), spends three or four pages addressing asymmetrical hearing loss. Hopefully I can present some viable strategies that are based on published literature as well as lessons that I have learned over the years in dealing with these complex hearing losses. I will use case examples from patients with whom I have been involved either directly or indirectly.
I am going to talk briefly about binaural hearing. I will provide some background information, but then will move into a discussion on recommendations, strategies and examination of some cases.
Binaural Hearing
As you know, sound comes in on two sides of the head and travels distinct parallel pathways to the brain. The crossover and mixing of information happens at a relatively low level in the auditory system. The brain uses differential information between the ears, such as amplitude, frequency and timing cues of sound sources at the ears to make distinctions between sounds. Although sound comes from two sides, the individual with normal hearing will experience a single unified sound.
We also expect this to happen when we fit hearing aids binaurally to a patient with bilateral hearing loss. One of the almost unstated assumptions is that we are trying to create a single unified sound for the patient, and it is only when something odd happens that the patient might report that they hear two different sounds from one side of the head versus the other. Normally, it should be a relatively seamless experience for the patients so that they have a unified percept.
This becomes more complicated in cases of asymmetrical hearing loss because there is not balanced hearing from both sides. As you go through the process of fitting hearing aids, you are trying to achieve some sort of unified percept, which is sometimes easier to achieve in some patients compared to others. While unified sound is not the only thing you are trying to accomplish when fitting asymmetrical hearing losses, it is it is one of the most important.
Asymmetrical Hearing Loss
Any audiologist knows the classic etiologies that can cause asymmetrical hearing loss. Sometimes an asymmetry is based on asymmetrical exposure to noise. The classic case is the dentist. When I was in graduate school, we would see older dentists who used drills that were positioned on one side of the head, and they developed a hearing loss. You do not see that quite as much now, but you do see asymmetries in hunters and military personnel today.
Remember that hearing loss is a change in physiology. We often think about hearing loss as an audiogram. That is a good shortcut to use for many hearing losses because it captures some of the most important information that we use to fit hearing aids. But when you see a case of asymmetrical hearing losses, it is important to remind ourselves that this is a change in physiology. Some of it shows up on the audiogram, and some of it does not. If it is a disease process or other insult into the auditory system that would naturally affect one side more than the other, then you end up with different physiologies on either side of the head. However, you are trying to put sound through those different physiologies such that it ends up creating a single, unified percept. Sometimes you can achieve that; sometimes you cannot.
Figure 1 shows an audiogram from a patient that I saw at the University of Iowa Medical School. The patient had clear asymmetries in hearing loss. One ear was normal, and one ear had a moderate loss, but very poor word recognition. This is a classic unilateral case of Meniere’s disease. Figure 2 is an audiogram from another patient with Meniere’s disease, but in this case it affected both ears. This patient did end up being a bilateral hearing aid user. As I go throughout the course, you will hear me use the term bilateral instead of binaural because of the nature of the hearing aid fittings. It is probably not a true binaural fitting because you are treating the two ears separately, even though the goal is to come up with a binaural image at the end. Sometimes it does not hurt to remind ourselves that there is a bilateral approach to asymmetrical hearing loss, even if only one ear is compromised.
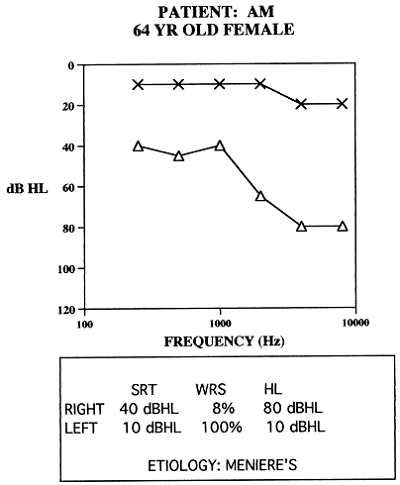
Figure 1. Asymmetrical hearing loss due to Meniere’s disease in a 64-year old patient.
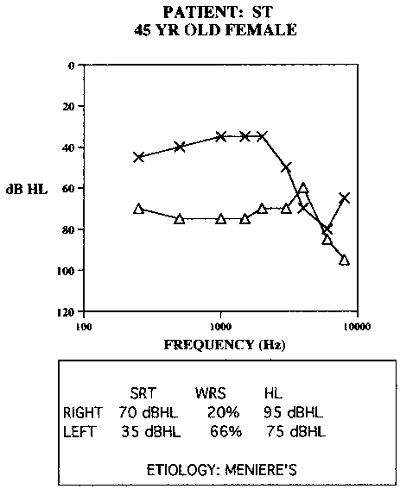
Figure 2. Asymmetrical hearing loss due to bilateral Meniere’s disease in a 45-year old patient.
Figure 3 shows another asymmetrical audiogram. Interestingly, this was an unknown progressive loss. His hearing happened to stabilize at this point. Notice that both the thresholds and the word recognition are a bit better in the left ear than the right ear. In fact, perceptually, his left ear was significantly better than the right ear.
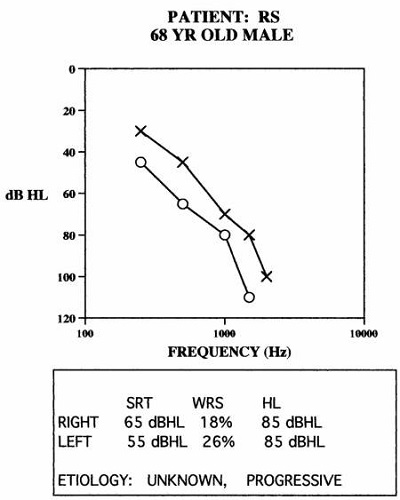
Figure 3. Asymmetrical, progressive hearing loss in a 68-year old patient.
Another patient that I saw in his early 30s was a police officer in a small city in Iowa who woke up one morning and could not hear from his left ear. He had no measurable hearing at the first appointment. Over the course of a few weeks, the hearing thresholds came back to severe to profound in the left ear, but no measurable word recognition. He did end up being a hearing aid user, which I will talk more about later.
Those are some examples of asymmetries in hearing. One of the points that Sandlin (1994) made was that you can have differences in asymmetries and the size of the dynamic range, not just in thresholds and word recognition. Knowing the size of the dynamic range for each ear from threshold to uncomfortable loudness level (UCL) will be significant when you are fitting hearing aids.
Assumptions of Typical Fittings
When you approach hearing aid fittings on “typical” patients, there are some underlying assumptions that may not be applicable when you are fitting atypical, asymmetrical losses.
Prescriptive Targets are Appropriate for All Hearing Losses
One of the goals we keep in mind when using a prescriptive target like NAL-NL2 or DSL is that we must achieve full audibility with nonlinear hearing aids. We must be able to take a broad range of speech inputs and fit those reasonably well within the patient’s remaining dynamic range. That is a very legitimate approach to take, and it works very well for the majority of hearing aid users, but it does not necessarily work for every patient with an atypical hearing loss.
Measureable Hearing is Usable Hearing
Another assumption is that measurable hearing is usable hearing. In other words, if you can obtain a threshold at a given frequency, there will be a useable dynamic range, whether or not you measure or predict what the uncomfortable loudness level (UCL) is going to be. We assume that we can work between threshold and UCL and put an aided signal into that region. That is a reasonably safe assumption for typical hearing losses, but not a safe assumption for asymmetrical hearing loss. Just because you have a threshold does not mean that the hearing in that region is usable. Discussions on cochlear dead regions shed light on that, but I think it is more complex than merely asserting that it is usable hearing or it is a dead zone. Due to the physiological changes in the ear, that question of usability can be somewhere in between. A dynamic range that does not necessarily mean that amplified speech in that range is going to be useful to the patient. Sometimes we get into trouble fitting aids when we think one-dimensionally this way.
Bilateral Hearing Loss Equals Binaural Fitting
Another assumption that we make is that we should do binaural fittings when hearing loss is present in both ears. In North America, the vast majority of fittings are binaural. Some of the sub-assumptions are that we should fit both hearing aids at the same time, that both ears are going to work in the same way if the loss is symmetrical, and that both ears are equal partners in the percept. When treating asymmetrical losses, one of the truths is to never assume both ears are equal partners. They both may contribute, but sometimes you end up with one ear doing more of the heavy lifting than the other ear.
For a typical fitting, we assume unequivocally that both ears are going to work about the same, and that you would give the full prescription to both ears. Sometimes you will not give the full prescription to both ears in an asymmetrical hearing loss. You have to take into account distortion and physiological changes that may not be immediately apparent on the audiogram.
We also assume that a similar loudness will be created between the two ears with a binaural fitting. When we fit two hearing aids at the same time, we assume that we have created a midline auditory image that will provide similar loudness responses on either side of the head. Again, that is probably a safe assumption in many cases, but sometimes you may be trying to create a different amount of loudness on one side of the head versus the other in an asymmetrical hearing loss. These are good examples of where the asymmetries make things a little bit more complicated.
Categories of Asymmetrical Hearing Loss
Both Ears are Aidable, but One Ear is Better
There are three basic categories of asymmetrical hearing loss. The first is where both ears are reasonably aidable, but one ear is better (i.e., Figure 2). Both ears can likely be aided if you look at them individually, but there is still a functional difference between the two ears. I will address fitting techniques in a moment, but you have to decide when you are going to amplify each ear and by how much. The case presented in Figure 2 is one where both of the ears were aidable, in my opinion. This patient was fit bilaterally with hearing aids.
One Dead Ear, One Aidable Ear
The next category is where one ear is dead and unusable and the other is aidable. You might think these patients would be cochlear implant candidates, and while this is sometimes true, not everyone ends up with a cochlear implant because of personal choices or risks of surgery. Clinically, you still have to deal with this as an amplification-only case and you cannot necessarily count on using other technologies. In cases like this, the aidable ear will be doing all the work. The way of approaching that ear could be a little bit different. Sometimes the one aidable ear still does not work very well. This may be due to a progressive loss, sudden hearing loss or other etiology where the one ear does not function as well as we would expect. These patients can be tricky to work with because hearing is so compromised; but on the other hand, these patients will take whatever you can give them because they are down to one ear. Sometimes these patients can be quite fulfilling to work with because anything you can do for them helps them. I will give you an example of a patient in this category later.
Figure 4 shows an example of one dead ear on the left side and one somewhat-aidable ear on the right side. She had a history of Meniere’s disease that devastated her left-ear hearing. Her case was more complicated because her right-ear hearing thresholds were very unstable, even though she had had this condition for a long time. She had a very small dynamic range. She could not get an implant due to surgical risks associated with heart issues she had. Her only choice was to get a hearing aid on the right ear. She was completely dependent on that hearing aid due to the instability of her hearing. She was one of the most challenging patients I had ever seen because of her condition. She was the type of person who deserved to have reprogramming done on a regular basis because of the fluctuations in her hearing. She was committed to staying connected to an auditory world, but she needed a tremendous amount of help to maintain that connection on an ongoing basis.
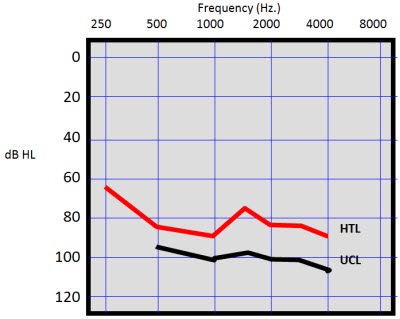
Figure 4. Patient with dead ear on the left side and severe hearing loss in the right ear due to Meniere’s disease.
One Normal Ear, One Aidable Ear
One of the most complex types of cases is where one ear is normal and the other ear is aidable. These cases can be multifaceted because the patient continues to receive normal auditory perception from one side of the auditory system. If you put a hearing aid on the compromised side, it has to mix with the normal acoustic hearing coming from the other side of the head. Some audiologists find that fitting challenging. You would think that the worse the hearing loss, the more difficult the fitting will be. However, in some cases, it could be that the reason to wear a hearing aid on the one ear is not related to speech communication, but perhaps to other issues.
Figure 5 is the audiogram from a police officer who had sudden hearing loss in one ear. He ended up using a powerful hearing aid on the left ear. The only time that he would wear the hearing aid was when he was on duty as a patrol supervisor. When he was working, he wanted to wear a hearing aid in the left ear to feel a sense of completeness to his hearing. It made him feel more secure. I talked to him about the head-shadow effect and how he was probably hearing sounds from the right side long before a reasonable amount of gain on the left side would even cause some sort of perception on the left side. But he still insisted that the hearing aid on the left side made him feel more secure. He felt that he was sensitive when sounds came from that side, and he had a sense of completeness with the auditory world that he missed when he did not have the hearing aid on the left side. He was absolutely convinced that there was a value to wearing the hearing aid in selective situations.
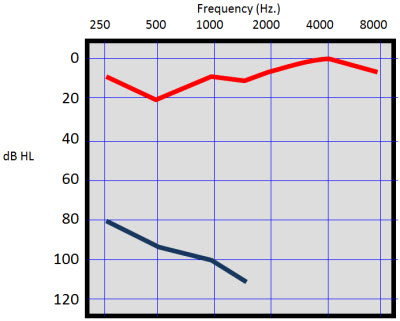
Figure 5. Patient with severe, sudden sensorineural hearing loss in the left ear.
Fitting Suggestions
Let me walk you through some fitting suggestions that I have developed for myself over the years. These are based on materials I have read, from cases, and from input that I have received from other audiologists. None of these are hard-and-fast rules, but rather suggestions that you might find to be useful when dealing with asymmetrical hearing loss.
Do Not Say No Until you Know
The first one is, “Do not say no until you know.” Several decades ago, there used to be rules about how much asymmetry could exist before fitting bilateral hearing aids did not make clinical sense. Over the last couple of decades, most people have come to the conclusion that there are no good rules to determine whether or not a hearing aid will work well for the patient. I have a very specific and clear philosophy on that. The only way that you know that an ear cannot use a hearing aid is if you fit a hearing aid to that ear, give the patient time to adapt, make appropriate adjustments, and the patient tells you it provides no benefit. Beyond that, I do not think that there is any justifiable rule that helps you predict that ahead of time.
We like to predict whether or not a patient is going to get benefit from a hearing aid. We spend a lot of time hypothesizing whether or not a hearing aid is going to work, when hearing aids are a totally reversible procedure. I do not understand why more audiologists are not more willing to try something. We cannot say with certainty that a hearing aid is going to help or not. My default position is to try it and see what happens.
Sandlin and Bongiovanni (1994) discussed an asymmetrical case where some professionals agreed to fit the right ear but not the left. They went on to say that the patient presented to these audiologists could be fit bilaterally and, in fact, was successfully fit bilaterally. Another good example is from Feldman and Oviatt (1993). They presented an audiogram that was vastly asymmetrical in the low frequencies. The left ear sloped from normal to moderately-severe, and the right ear was a flat, severe hearing loss. The right ear seemed to be useless under headphones because there was no measurable word recognition. This patient had worn a hearing aid only on the left ear for number of years, but was never given the opportunity to wear a hearing aid on the right ear. The clinicians fit a hearing aid to the right ear, gave the patient time to acclimate and did some follow-up adjustments. They tested word recognition in quiet and noise with a hearing aid on the left ear only and then with hearing aids in both ears. Going from a hearing aid only in the left ear to hearing aid in both ears raised the word recognition score in quiet from 76% to 92%, and from 56% to 88% in noise using a +10 signal-to-noise ratio. Remember that this was with an ear that appeared unaidable. This is one of the best cases that I can think of that validates the statement, “Do not say no until you know.”
It only takes a few cases like this to demonstrate that we really do not know how the asymmetrically-affected auditory system will combine input from two different sides under the influence of hearing aids. How the brain puts together that information may be different for everyone.
Aim for a Fused, Binaural Image
The second fitting suggestion aims for a fused binaural image. If the person is hearing two different things from two sides of the head, it is going to be very distracting to the patient, to the point where few patients would end up using hearing aids bilaterally. When you go about fitting asymmetrical losses, you have to create a balance between the two ears. Exactly how much gain and in what frequency region you have to provide it becomes an individually-adaptive approach to find what works well for the patient. The goal is to get a fused binaural image. If you cannot create that fused binaural image, there is a higher likelihood that the patient will reject wearing hearing aids on both sides at the same time. What it takes to meet that goal may be difficult to predict based on looking at the patient's audiogram.
Targets are Only a Starting Place
The next piece of advice is that targets are only a starting place. Do not be surprised if you end up providing less gain to the poorer ear. If you have an asymmetry with two aidable ears, it is likely that the better of the two ears is going to be doing most of the auditory work and signal processing that the brain uses for speech understanding. The other ear may contribute, but it does not add as much as you might expect. Oftentimes, you can over-amplify the poorer ear because you are trying to reach targets. What you are doing is adding more distortion into the person’s auditory system than it can handle. If you veer away from target, it is more likely that you will use significantly less gain on the poorer ear than you might expect. Many times, the poorer ear has more threshold-based loss than the better ear. The tendency is to drive the gain up on the poorer side, but you will create more problems and unbalanced loudness.
This brings up another point. Most hearing aids have volume controls. If you are working with asymmetrical hearing loss, volume controls are a must, especially on the poorer side because you do not know how it will react to amplification. The patient needs to have the opportunity to make volume adjustments to match the better side.
Figure 6 shows a case where thresholds were poorer in the left ear than the right, but the word recognition scores were poor in both ears. The patient was fit with powerful linear hearing aids in both ears. He reported that the left ear sounded fine, but the right ear was a hindrance and created distortion when he turned it up. When I tested aided word recognition, putting the hearing aid on the right side decreased his word recognition score compared to wearing the left hearing aid alone. He was interested in continuing to look for a solution on the right side. When I looked at the amplification characteristics of the right hearing aid, there was a large peak around 1000 Hz, because I wanted to make sure that I gave him a good deal of gain up to 1000 Hz because that is where he had the most useable hearing. I ended up giving him more gain than his auditory system could handle. This was an auditory system that was sensitive to being overdriven too easily. I ended up re-fitting him with a multichannel nonlinear hearing aid on the right ear, dialed in the compression and kept the insertion gain down.
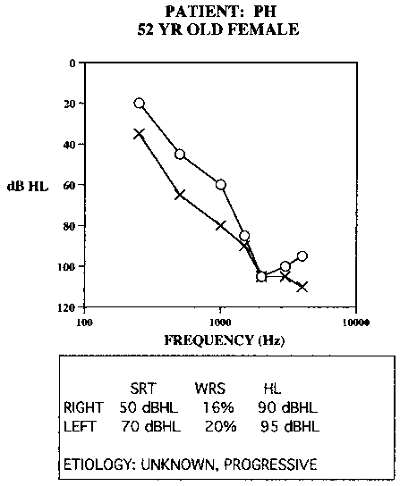
Figure 6. Asymmetrical hearing loss with poor word recognition. Hearing aid fitting on the poorer ear did not improve word recognition, but increased distortion.
When I tested him using the hearing aid just in the right ear and then using both hearing aids together, his best score was 42% bilaterally. He did end up being an effective bilateral hearing aid user, but it required me to reevaluate the way I was approaching the hearing loss in the right ear. I had to take a more subtle approach using a multichannel, nonlinear hearing aid. I did not use as much gain as you might expect based on the thresholds, but he ended up being a successful hearing aid user because the left ear was working well; the right ear added something to the total picture.
Consider Serial Fittings
The next suggestion that many audiologists do not consider is to perform serial fittings, meaning fitting one hearing aid first and then adding the second hearing aid later. In almost all cases, the recommendation is to fit the better ear first, making sure that you do a very good job with fitting that ear all by itself, and then add the second ear to the fitting up to a point where it adds something to the fitting of the better ear. You have to be careful to not add something to the better ear that detracts from the first fitting that you did. One of the best ways to do it is to do the two fittings at different points in time. Sometimes it helps to separate the two ears so the patient can distinctly determine which ear is benefitting from the amplification, and if there is distortion, they will be able to identify that individually. The fitting scenario is more successful if the patient is not confused or disappointed by too much input at one time. Likewise, you are better able to address their needs and concerns when you know what each ear is hearing independently. If you take the time to perfect the fitting on the better ear and then add the second fitting later, it might clear things up for both you and the patient.
Figure 7 shows an audiogram from a case where I used this approach. The patient had bilateral hearing loss from Meniere’s disease. The right ear was clearly hearing better than the left ear. When she was ready to start with hearing aids, I fit only the right ear. It took about two months to make sure that that fitting worked out well, and then I added a hearing aid on the left side. You do not have to wait two months, but there happened to be fluctuation in the left ear in this case, so I waited a little bit.
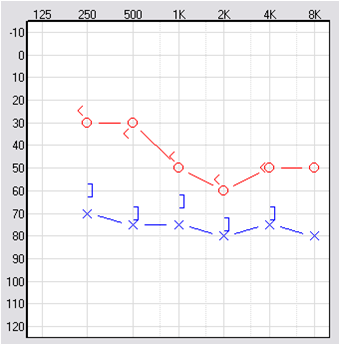
Figure 7. Asymmetrical hearing loss due to Meniere’s disease; the right ear was fit prior to the left ear.
She was fit with a power hearing aid on the left ear. I was not planning on using high gain on the left ear; I was going to treat it with gain parameters similar to the right ear, even though the thresholds were worse and more unstable. I did not want to overdrive that ear. That is a very classic case where using a serial fitting philosophy worked out well for the patient. She ended up being a bilateral hearing aid user.
Consider Advanced Technology Features
The next fitting suggestion is to consider the advanced features. Some hearing aids use binaural communication to talk to each other across the head. We have technology that is designed to try to preserve interaural intensity differences to aid in localization. You may find that you want to disengage some of the binaural processing features for asymmetrical hearing aid users. You are not talking about a truly binaural system when the ears are hearing differently. One ear is probably doing more work than the other, and some of the advanced features might not work the way you would expect. You should consider the features based on the way that binaural system works, and decide whether or not you want to apply those to asymmetrical fittings. Again, it depends on how different the ears are and what your goals are for the fitting.
Proper Role of Monaural, CROS & Bi- CROS Fittings
It is important to talk about CROS (contralateral routing of the signal), Bi-CROS or monaural fittings for some of these patients. Not all asymmetrical hearing losses that are aidable can be fit bilaterally. There are some situations where you try a fitting on the poor ear and you find that it does not help or even makes things worse. I have only shown successful cases, but they do not all work out that way. One of the things to remember about a CROS or Bi-CROS fitting is that one ear is unusable. Many people would consider a Bi-CROS fitting for asymmetrical cases. I think that it is fine to consider a Bi-CROS fitting, but only after you have proven to yourself and to the patient that fitting the poor ear is not going to help.
Recall the case of the police officer (Figure 5). If we put a CROS hearing aid on him, theoretically, we could take sound coming from his bad side and move it over to his good ear. That would be fine, but I wanted to see whether or not I could create the sense of security he was looking for by stimulating the bad side of the auditory system. It was not so much that he needed the sound from that side, but he wanted to feel the sound coming in that side of his auditory system. That was part of the security he was looking for. In many cases, somebody with a profile like that would probably end up using a CROS hearing aid, but his case was unusual. When one ear is normal and the other is severe to profound, you will be successful fewer times than not when fitting the poorer ear. But this is why you prove it. Do not say “no” until you know for sure that it is not going to work out. CROS and Bi-CROS hearing aids have their place with this population, but only after you have ruled out that you cannot do direct amplification on the poor ear and attain something useful for the patient.
When someone comes in with two aidable ears, I do not think we often have the dilemma of only being able to fit one of them. Perhaps the patient is absolutely convinced, however, that they are going to use one versus two. If you are forced to fit only one ear, it makes more sense to fit the ear for which you expect amplification to be most helpful and provide the best sound quality. Hopefully you are not put in the position where you can only fit one ear, but if so, you should aim to regain some of the binaural effects for the patient. With any luck, you can make a strong case to your patients that you think they should be fit with amplification in both ears.
Outcome Measures
Outcome measures are a way to verify your fittings. You want to provide verification in a variety of different ways. Real-ear measures are appropriate, but remember that sometimes your gain value may be very different, especially in the poor ear. Matching targets might not tell you what you need to do. You could do word recognition in the sound field, aided and unaided, or aided in one ear, or aided in both ears. All those things make sense. Dillon (2012) talks about a simple localization test you can do. One of the points to remember is that success may be defined by the patient in ways that seem odd to us. Know ahead of time that a traditional outcome measure might not capture why the patient wants to wear the hearing aid.
I try to ask three simple questions to patients. It is not an official questionnaire, but the questions address things that I am interested in knowing in these asymmetrical cases. One of things you want to know is how often they are wearing their hearing aids, either monaurally or binaurally. This will give you an indication of how they use the hearing aid.
The second question checks to see if they are getting a unified sound perception or if they are still hearing two different sounds. That is something that you need to know so it can be addressed properly through follow-up visits.
The third question aims to discover why they want to use the hearing aid, especially for the poorer ear. If you are fitting a monaural hearing aid on a patient with severe hearing loss and normal hearing in the opposite ear, you want to try to ascertain what they feel the benefit is. It may be speech understanding in quiet or noise, identification of sounds in the environment, localization, or the idea of balancing the hearing from both ears. Many of these patients end up with tinnitus. One reason they like to wear the hearing aid is because it reduces tinnitus. That is another factor to consider. The motivation and benefit needs to be defined from the patient’s standpoint.
Case Examples
I want to walk through a few case examples to show you some of this in practice. My wife is an audiologist in private practice, and has shared the following cases with me. She has allowed me to speak to the patients, use the questionnaire and further examine each case.
Case #1: TF, 52-year-old Female
The first patient is a 52-year-old female with congenital hearing loss that seemed to be stable (Figure 8). Although she had the hearing loss all her life, she only came in to be fit with hearing aids a few years ago. She reported that her right ear was dead or totally unusable. When you look at the audiometric thresholds, there are threshold asymmetries of only 5 to 10 dB HL, and a word recognition score in quiet that is only 20% worse in the right ear from the left ear. But the patient, over a number of years, had decided that her right ear was not usable. Fortunately, she was fit with bilateral hearing aids, and she is now an active, full-time user of hearing aids. She is a very social person, and she would not go an hour without wearing both of her hearing aids. She communicates very effectively. She is also an avid user of connectivity technology, which can be highly beneficial for patients with severely compromised hearing.
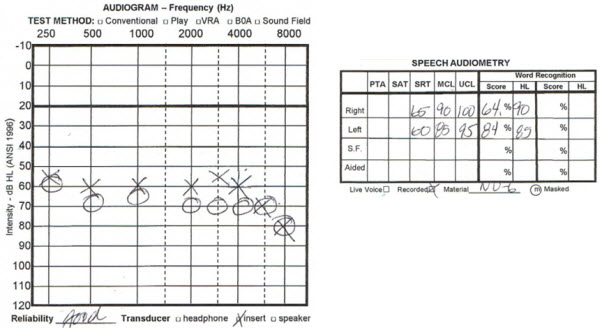
Figure 8. Audiogram from a 52-year-old female with congenital hearing loss who perceived her right ear to be much worse than the left.
Case #2: WA, 86-year-old Male
The second case is of an 86-year-old male with relatively symmetrical hearing loss and word recognition scores (Figure 9). However, he confidently felt that his left ear was significantly better than his right ear. Many audiologists would say that the thresholds were fairly balanced between ears, but his perception was that he had a good ear and a very bad ear. When it was suggested that he get hearing aids in both ears, his opinion was that it would be futile to fit his right ear because it did not work for him. We went ahead and tried hearing aids on both ears, and now he is a very successful user of bilateral hearing aids. Both of these cases illustrate the point that it does not take a great deal of asymmetry to cause an imbalance in perception.
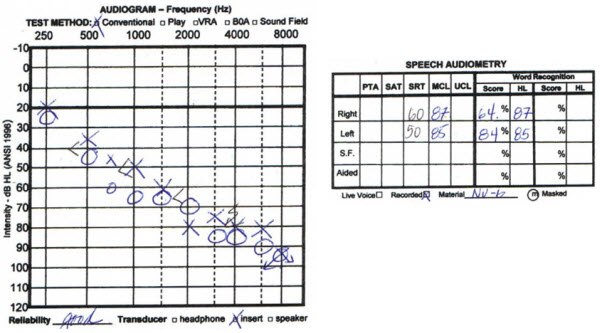
Figure 9. Audiogram from an 86-year-old male with symmetrical hearing loss but perceived functional imbalance between ears.
Case #3: TR, 75-year-old Male
Next we have a case that is the opposite of what we have just discussed. This 75-year-old gentleman thought he only had one bad ear (Figure 10). He thought his right ear was fairly good and his left ear was bad. He tried to get by with being fit only on his left ear. After trying that for a couple years and realizing he was still not hearing well, he agreed to be fit with a hearing aid on the right ear also. When he put the two hearing aids together, he then felt that he was doing well. It was a combination of not only fitting the poorer ear, but also aiding the better ear. He never considered that he needed a hearing aid on the right ear because it was his “good” ear. It took him a while to understand that, but once he did, he was very happy with the outcome. He reports that he uses his hearing aids most waking hours. He has a unified percept of sound, and he would not consider not wearing both of his hearing aids. He just needed the opportunity to try something on both ears to convince him that he could hear better with both ears receiving amplification.
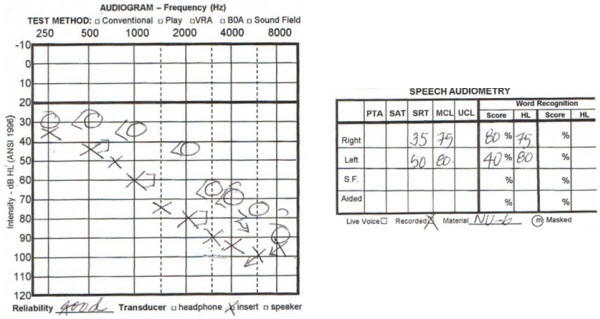
Figure 10. Audiogram from a 75-year old male with asymmetrical hearing loss who felt his right ear was not compromised prior to hearing aid fitting.
Case #4: QL, 68-year-old Male
The next case is a 68-year-old male (Figure 11). Again, hearing thresholds do not differ greatly between the ears, but the word recognition scores are vastly different. This patient did not have any measurable word recognition score in the right ear, but he is a full-time user of hearing aids in both ears. He reports that he uses a hearing aid on the right ear because it gives him a sense of security and confidence. He does not feel complete if he is only aiding his left ear. We can assume that he is communicating based on his skills from the left peripheral auditory system, but the addition of amplified sound to the right ear gives him a complete sense of the sounds around him. His reasons for using hearing aids are a little different than the other cases.
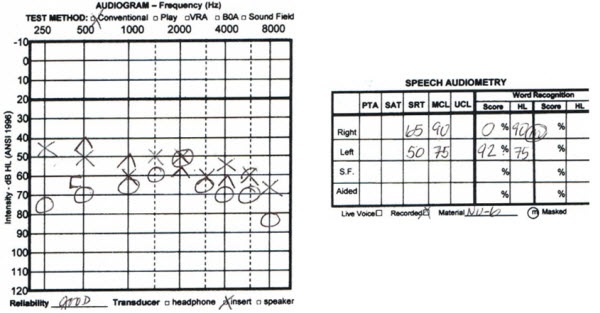
Figure 11. Audiogram from a 68-year-old male with asymmetrical hearing loss and word recognition scores. He is a bilateral hearing aid user.
Case #5: BR, 83-year-old Female
BR was first fit in both ears 13 years ago when she was 71 (Figure 12). Notice that there is a bit of asymmetry in the word recognition scores, with the left ear scoring better than the right ear. When she was retested in 2006, there were still some asymmetries in the word recognition score and the thresholds worsened a bit. She was a successful hearing aid user with hearing aids in both sides throughout that time. However, very recently her word recognition started to bottom out in both ears (Figure 13). You see the thresholds are still reasonably close to each other, but her word recognition is poor. She has recently stopped using the hearing aid on the right ear because it is not giving her benefit anymore. She is using a more powerful hearing aid on her left side only. These hearing losses can be fairly complex, and they can change over time.
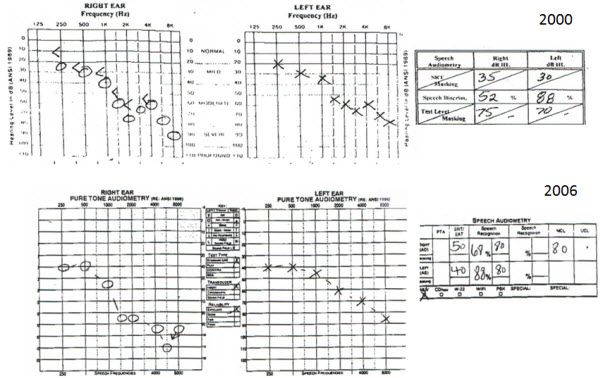
Figure 12. Data from BR, a then-71-year-old female patient who was fit bilaterally.
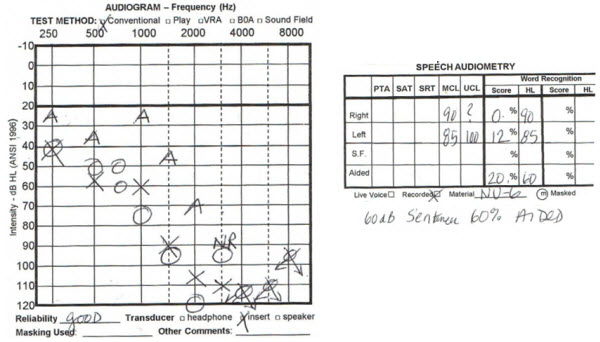
Figure 13. BR at 83 years of age, with progression in hearing loss and decrease in word recognition scores, bilaterally.
Case #6: VT, 75-year-old Female
The last example is from a 75-year-old female (Figure 14). She wanted to try using a hearing aid on one side. She had a hearing aid on the left side first. She found that it was not giving her what she wanted due to her word recognition. Then she tried a hearing aid on the right side only. She would not commit to wearing two hearing aids at once. She tried different styles and went back and forth between hearing aids for a few years. When she came back last year, she finally agreed to be fit with two hearing aids, despite drops in her word recognition scores. Although she had tried using two hearing aids a few years ago, her needs were not as great, and she was still talking herself into getting by with just using one hearing aid. Four years later, she experienced more changes in her hearing (Figure 15) and got to a point where she needed to use both the hearing aids at the same time. Now she is a successful user of bilateral hearing aids. Her demands increased and the changes in her hearing required that she do something different.
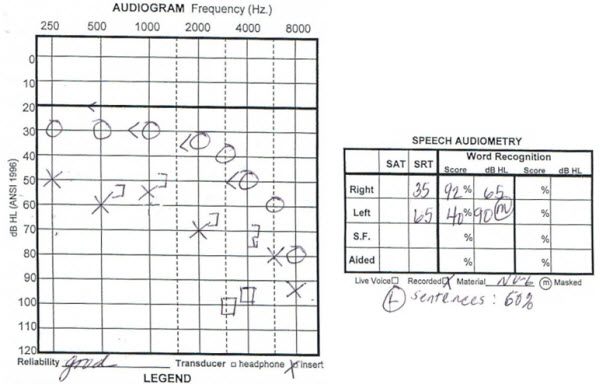
Figure 14. Audiogram from a 75-year-old female with asymmetrical hearing loss and word recognition scores. At this time, the patient only used one hearing aid.
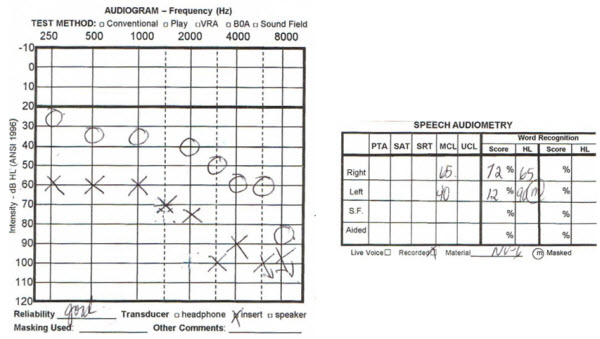
Figure 15. Audiogram from the same patient, recorded four years later, showing a decrease in word recognition scores. The patient chose at this time to wear two hearing aids.
By seeing these case examples, I hope you were able to get an idea of how to approach asymmetrical losses. They can be challenging, but they are also very engaging and give you an opportunity to test your mettle as an audiologist.
Questions and Answers
You show very few bone conduction tests on the audiograms in your case studies. Are you sure they are all sensorineural?
In all cases, if you do not see bone conduction testing on the audiograms that I presented, rest assured that they were sensorineural. Sometimes based on the format, I did not necessarily put all that on. All the cases I referenced today were specific for sensorineural hearing loss.
Should we give patients with asymmetrical hearing loss more time to adjust to the hearing aids?
Yes, absolutely. It could take a good deal of time to adjust to these fittings, especially if you are doing staggered fittings. The overall time that it may take for the patient to adjust to a fitting might be longer than you expect.
Do you feel that auditory deprivation may be another factor to consider when fitting the poorer ear?
Absolutely. Even if an ear is a poor fit for hearing aids, it does not mean that it will not be a candidate for auditory deprivation, which is another justification for fitting both ears. Even if the ear has a lot of distortion, it does not mean it cannot be usable. If you stop trying to put sound in the ear, the patient will indeed experience some auditory deprivation. In some of these cases, maybe auditory deprivation was what was going on in the first place, leading to the poor word recognition scores. In either case, trying to do something to bring it back up is likely a good idea.
References
Dillon, H. (2012). Hearing aids (2nd ed.). New York, NY: Thieme.
Feldman, A., & Oviatt, D. (1993). BiCros or binaural: A case study. Seminars in Hearing, 14(3), 229-233.
Sandlin, R. E., & Bongiovanni, R. (1994). In M. Valente (Ed.), Strategies for selecting and verifying hearing aid fittings (pp. 221-252). New York, NY: Thieme.
Cite this content as:
Schum, D.J. (2013, October). Asymmetrical sensorineural hearing loss: Fitting strategies. AudiologyOnline, Article 12222. Retrieved from: https://www.audiologyonline.com


