Editor's note: This article/text course is an edited transcript of a live webinar. Please download supplemental course materials here.
Today’s lecture, Application of ABR and Objective Assessment of Infant Hearing, is an important one. There are three more lectures in this electrophysiology series presented on AudiologyOnline this month. In lecture two, I will talk about electrocochleography (ECochG) in general, but focus on the application of auditory neuropathy spectrum disorder (ANSD). Lectures three and four will be given by Sam Atcherson, Ph.D. from the University of Arkansas in Little Rock. Sam is the editor of a recent auditory electrophysiology book and is very knowledgeable on the topic. His specific themes will be cortical evoked responses and the neurodiagnostic applications of auditory evoked responses.
I will start by giving you a quick rationale for why early diagnosis of hearing loss in infants is important. I know that you are all audiologists, and I do not think any of you would argue with the point that early diagnosis of infant hearing loss is important, but there are colleagues of ours in pediatrics as well as other professionals and parents who may not appreciate the importance of hearing on communication. It is very important to have that information readily available for educating and counseling these groups.
Next we will talk about some of the various stimuli that can be used to elicit the ABR in infants and young children. All of the different types of stimuli can be used together or at different times to get the best results. We will spend quite a bit of time talking about the test protocol for ABR recording in children and walk through a test protocol which is evidence-based and clinically proven. We will also discuss measurement analysis of tone burst and bone-conduction ABRs and how the results are analyzed. I am going to make the point that bone-conduction ABRs are just as important as bone-conduction pure-tone audiometry. What would you think of the audiologist who said, “I never do bone conduction; I just do air conduction.” You know that they would not be diagnosing hearing loss accurately in many cases. The same is true for ABR measurements. We are trying to get all the information from ABR we ever would from behavioral testing, too.
Lastly, I will spend a few minutes talking about how to record ABRs without sedation, as well as options for sedation.
Universal Newborn Hearing Screening and Early Identification of Hearing Loss
Things changed dramatically for early identification of hearing loss in infants in March of 1993. It is an event that I still recall as if it happened last month. There was an incredible consensus conference in Bethesda, Maryland on the National Institutes of Health (NIH) campus. There were at least 500 people in the audience; in fact, so many people showed up, they had to have overflow rooms with closed-circuit TV. Imagine a big amphitheater-auditorium with a stage and a podium off to one side. The moderator was an otolaryngologist from Chicago. On stage was a panel of 16 experts, including James Jerger, plus statisticians, a parent of a child with hearing impairment, a pediatrician, and an ethics expert. People presented 20-minute evidence-based papers on a variety of topics at this conference. I gave the ABR lecture and had never been so nervous in my life. At the end of all this, a position statement was prepared. Every recognized newspaper and TV station was there to cover this news. To the surprise of everyone, this consensus group recommended universal newborn hearing screening. At that point, everybody began to think this could happen. That was 20 years ago.
The group identified some research questions about the benefits of early intervention. This meeting and subsequent document generated some heated controversy. Two of the primary recommendations to be defined were, “How early is early?” and, “Is early intervention of benefit?” There was anecdotal evidence that it was of benefit, but it had not yet been defined if it was beneficial for all children.
The general conclusion was that all babies should be screened at birth. The recommendation was for universal newborn hearing screening, but there were some questions that needed to be answered. Christine Yoshinaga-Itano began to answer these questions with a lot of energy. Her studies demonstrated, without any doubt, that “early” means six months. That was a big surprise, even to her. Many of us thought that early intervention meant one year or perhaps sometime in the first four years after a child is born.
Christine Yoshinaga-Itano showed that the brain is being shaped by auditory stimulation, and that the foundation for hearing, language, and speech was being laid in the first six months before a child utters their first real word. That revolutionized our time strategy for early identification of hearing loss. It put techniques like the ABR back on the radar, because there was no other way to obtain this information. There was nobody in the world, including Christine Yoshingaga-Itano and Marion Downs, her mentor, who could adequately assess hearing in children under the age of six months using behavioral techniques. We needed electrophysiologic techniques.
Dr. Yoshingaga-Itano’s first five years of research in this area started right after the conference. She showed early intervention must be six months or earlier, and that early intervention by six months does help all children with hearing loss, even those with mild to moderate loss (Yoshinaga-Itano, Sedey, Coulter, & Mehl, 1998). Further, hearing loss has a negative impact on language. These classic papers are full of valuable information and argue for early intervention. They have been replicated many times over.
Dr. Yoshingaga-Itano’s data, as well as other simultaneous studies, showed that auditory brainstem response (ABR) and otoacoustic emissions (OAEs) were feasible for hearing screening in children and could be done in a cost-effective and accurate way. That led to the next breakthrough, which was the recommendation by the American Academy of Pediatrics for universal newborn hearing screening. The American Academy of Pediatrics is a very academic group who relies strongly on evidence. They had been a little skeptical as to whether or not hearing screening of all babies was a good idea, but in 1999 they concluded that it was. By the year 2000, most states started to implement universal newborn hearing screening using these recommendations.
Recording ABR in Infants and Children
I want to talk about how we elicit the diagnostic ABR in infants after a failed newborn hearing screening. You may be seeing an older child who passed the newborn hearing screening but now parents have concerns a year or two later. Remember, 15% of all children who pass a newborn hearing screening at birth will ultimately have hearing loss. Let me rephrase that more accurately. If you take 100 children with hearing loss and you look back at the perinatal events, 15 out of the 100 children with hearing loss will have passed the newborn hearing screening and have delayed-onset hearing loss. Some of the children we are assessing are not necessarily two to three months old. Some of you are not in countries where universal newborn hearing screening is a reality, so this information applies to children of any age. Early identification means as early as you can. A year-and-half to two years might be the first time that hearing loss is identified.
Stimuli
In 2007, the Joint Committee on Infant Hearing (JCIH) issued the most recent position statement on early identification of hearing loss. If you evaluate hearing in children, you need to be familiar with this document. It covers the entire gamut from how to screen for hearing loss in different patient populations, including well-baby versus intensive care nurseries, to how to diagnose and manage hearing loss. It also talks about the role of the pediatrician, who is the medical home for most infants. They should be referring patients to audiologists on a regular basis. It is not our responsibility to track every baby after birth to see if they have a hearing loss. That is the responsibility of the primary care physician. I urge you to read or review this document and refer to it often.
Among the different procedures connected with the diagnosis of hearing loss in infants from birth to six months, the ABR is the most important technique. Other supplemental techniques include OAEs, tympanometry with a 1000 Hz probe tone, auditory steady-state response (ASSR) and acoustic reflex measures. It is safe to say that without the ABR, we would have no way of diagnosing hearing loss consistently in newborns and infants under the age of six months.
What stimuli should we use? We need to use frequency-specific stimuli like tone bursts. There is a new variation of that called the chirp, which I will address in a moment. I am a strong proponent of beginning the ABR with a click stimulus. You can do this in under two minutes. With that valuable information, you can sort out what type of auditory dysfunction that child has. You can also instantly determine the presence or absence of a cochlear microphonic. A robust cochlear microphonic in the absence of an ABR raises a red flag for ANSD.
While reviewing some guidelines for diagnosis, I was reminded that the British audiologists jump straight to the tone burst. I want to give you a quick rationale for why I think you should start with the click before going to the tone burst.
One important concept is the unavoidable, inevitable trade-off between the duration of the stimulus and the frequency specificity when stimulating the ABR. In other words, the longer the duration of the stimulus, the more frequency specific it is, such as a pure tone. The tone burst, which is one or two cycles, or sometimes as many as six cycles, still has tonal characteristics. The tone burst activates a general frequency region, but it is not a single frequency. A click has a short duration of 0.1 milliseconds or 100 microseconds. It is going to produce a very wide frequency spectrum. In fact, the spectrum of a click coming out of the earphone is representing the frequency response of that ear phone, from very low frequencies up to very high frequencies.
Click
Why are we interested in the click if it does not provide frequency specificity? With a click, we can miss low-frequency hearing loss because the click centers around high frequencies. The stimuli will activate the base of the cochlea, so the click ABR will appear be normal. Even a high-frequency precipitous loss will likely result in a normal ABR because there is plenty of energy in the click below 4000 Hz that will produce a normal ABR. A high-frequency loss hearing loss that begins around 2000 Hz and slopes precipitously might result in the presence of an ABR. However, the latency would be delayed, because the ABR would not be generated up in the 2000 to 3000 Hz region; it would be generated more in the 1000 to 1500 Hz region. This is because the traveling wave would have farther to go before the response would be generated.
Some people say the click is a waste of time. It is a waste of time if you spend 15 to 20 minutes recording it, but if you discipline yourself and spend 2 minutes, it is well worth that time. The click ABR is large and well-formed. Click responses are very synchronous. If you can record a clear wave I, III, and V, and if the latencies are normal, then you know there is good hearing somewhere. Even if the ABR is normal at 85 dB, it still tells you there cannot be more than a moderate high-frequency loss at most.
If you record both rarefaction and condensation clicks, then you can examine the cochlear microphonic. The cochlear microphonic recorded from rarefaction and condensation click stimuli should normally appear out of phase. However, large amplitudes in these tracing may raise some concerns, especially if not distinguishable ABR waves follow. If you can record a normal ABR with appropriate morphology, then you can rule out auditory neuropathy and neural hearing loss. You can also rule out a profound sensory loss as well as conductive loss. I can get an ABR at a high intensity in a quiet child in a matter of 30 seconds to a minute. That is a good use of our time for the information we obtain.
If the ABR looks normal with well-formed waves I, III and V and normal interwave latencies, but the response as a whole is delayed in latency, it is almost always purely conductive. At 35 seconds in to the ABR, I can already determine know there is a conductive loss. If wave I is large and well-formed, that often indicates that cochlea is normal in that conductive loss. If wave I is diminished and morphology is poor, that tells you there is likely a sensory hearing loss in the high frequencies. If there is a delay between I and III or I and V, that may be a neural loss, but you have to take the infant’s age into consideration. It may be delayed maturation, which is normal until 18 months. Shifts in interwave latencies may also be caused by anesthesia or low body temperature. Delayed interwave latencies need to be interpreted in the context of other factors.
The click also helps determine whether or not bone conduction is necessary and if auditory neuropathy is suspected. It can also help you decide how to approach the rest of the ABR assessment. If click ABR is normal down at 20 dB, then you know that hearing is adequate somewhere in the high frequencies. If the child is sleeping naturally and could wake up any second, I recommend going directly to 500 Hz tone bursts. Then, you might finish with OAEs, and if they are all normal, you have ruled out any significant hearing loss, even though you do not have all the tone burst frequencies.
I have just summarized why the click is important. The ultimate goal, of course, is to evaluate hearing at different frequencies throughout the speech spectrum. I like to have a clear ABR down to threshold for 500 Hz and 4000 Hz, and then at 1000 or 2000 Hz, depending on the apparent configuration of the loss. I want to define auditory threshold using ABR very confidently so that my colleagues who are pediatric hearing aid experts can confidently amplify the entire speech spectrum using a technique like DSL or NAL. Our goal is to do everything we can to enhance normal communication and speech and language development in the child. The diagnostic ABR allows for the first hearing aid fitting and gives the child good auditory stimulation in the first six months.
Tone Burst Stimuli
Tone bursts are the most popular option for obtaining frequency-specific responses. We could use pure-tone stimuli that are modulated in amplitude if were recording the ASSR, which is an option. These are not mutually exclusive. Very often I will use tone bursts for some frequencies where there is a clear ABR, and I will use ASSR at other frequencies where there is no ABR due to the severity of loss.
The chirp is a swept stimulus, from low to high frequency. The low frequencies are presented approximately 5 milliseconds earlier than the high frequencies. In this case, lower frequencies can reach the apex of the cochlea at about the same time that the high frequencies reach the base of the cochlea. In theory, both the chirp and click stimuli allow for simultaneous activation of the entire basilar membrane. The problem with the click stimulus is that the most basal (high-frequency) region gets activated first, and the neurons connected to those hair cells fire first. Picture the traveling wave moving along the basilar membrane to the apex, but the ABR has come and gone. By the time the low frequencies reach the apex 5 milliseconds later, the ABR is over. With the chirp stimulus, we can activate the entire cochlea.
ABR Test Protocol
Back in the late 1970s, we had the clinical equipment and ABRs became rather commonplace in large medical centers. Back then, we were taking equipment that was designed to be used with adults, using protocols designed for neurodiagnostic ABRs when looking for acoustic tumors, and we are applying those protocols to children. By trial and error and a lot of systematic clinical study, we began to refine that test protocol.
Thankfully, in the year 2013, we have a protocol that is evidence-based. Every one of the recommended parameters is selected based on research evidence. I guarantee that if you have a quiet baby and use this protocol, you will get the best ABR a child can produce. There are variations in the protocol across professionals and, but the general protocol is widely accepted.
Transducers
In the United States, and most places except England, inserts are the transducer of choice. The British are very skeptical about using inserts, because they are concerned that we cannot calibrate the sound in a tiny ear canal. The bigger the earphone, the less impact small versus big ear canals have on the actual intensity. But in fact, the results from thousands of babies has shown that even babies with perfectly normal hearing do not have thresholds of -20 or -25 dB, which is what you would expect if we were getting much higher effective stimulus intensities with inserts. The advantage of inserts far outweigh any slight disadvantage of not knowing exactly what the intensity is for a specific infant.
Type of Stimulus
The two major types of stimuli are clicks and tone bursts, but we now also have chirp stimuli. You can use each of them at some time during the ABR assessment. We have more and more tools in our toolbox to do a better job in evaluating children.
Frequencies
You want frequencies of 500 to 4000 Hz. There is a rationale for going out to 8000 Hz, and with ASSR, we can test down to 250 Hz. That is not possible with the ABR, and we will talk more about how we use different frequencies in different sequences at different times.
Duration
The click has a duration of 0.1 milliseconds (100 microseconds), which is very brief. For tone bursts in the United States, most people use two cycles of rise, two cycles of fall, and zero plateau. So for 1000 Hz, the two cycles would be 2 milliseconds. For 500 Hz, the two cycles would be 4 milliseconds. In England, they recommend two cycles of rise time, one plateau, and two cycles of fall. It probably does not make much difference either way.
Ramping
The consensus is that Blackman ramping is the ideal setting. Ramping is the way each stimulus goes from the absence of a stimulus to the maximum intensity. Blackman was an electrical engineer who developed a mathematical equation that provided a rapid onset in the stimulus without generating unwanted spectral splatter.
For most systems, we want the artifact reject feature on so that a child’s extraneous movements are rejected. The more artifact there is, the slower the testing will go because those stimuli are being rejected. As a general rule, if the muscle and movement artifact is rejecting more than 10% of the stimuli, you need to try to quiet the child; if the artifact is continually high and a recording cannot be made, you might think about the possibility of sedation. Some systems have weighted averaging, which means that instead of stopping the recording to reject artifact, it keeps collecting data and weighs more heavily the samples that contain a response versus samples with noise.
Analysis
Epoch
When you are using low-frequency tone bursts such as 500 or 1000 Hz, you need an analysis time of 20 milliseconds. When I am using a click stimulus or a high-frequency tone burst like 4000 Hz, I will use 15 milliseconds. When you are recording ABR, you want a timeframe that allows you to see the ABR in the middle of that timeframe. You do not want the ABR to be squished at the beginning, and you certainly do not want most of the ABR at the end of the timeframe, because if there is any delay in the response, you may not even see it.
If you recorded a click ABR at a high-intensity and the latency is around 6 milliseconds, a timeframe of around 12 to 15 milliseconds is perfect. If you are recording a low-frequency tone burst, like 500 Hz, the wave V response is about 5 milliseconds longer. It takes 5 milliseconds for the traveling wave to get from the base to the apex. Even at high intensities, the typical latency for a wave V at 500 Hz is around 10 milliseconds, so a 20-millisecond timeframe would be adequate.
Sweeps
“Sweeps” is an old term referring to each time a stimulus is presented. With each presentation, the system sweeps through the analysis time looking for a response. The number of sweeps is the number of stimuli. The British group recommends replicated waveforms with 3000 sweeps each. This is where I differ from my British colleagues. To me, that is more time consuming than necessary if you already have a very good signal-to-noise ratio. If you have a quiet, sleeping baby with normal hearing sensitivity, I guarantee that you are going to see an ABR after 500 sweeps when using a click stimulus.
My approach is to stop presenting stimuli, not at a specific number, but when the signal-to-noise ratio is adequate. If the response is two or three times bigger than any background noise after 500 sweeps, you gain nothing by presenting another 2,500 stimuli. On the other hand, if you have a child with a hearing loss or you are down to threshold, you may need to average 3,000 or more sweeps in order to enhance the response to become large enough for you to see above the background noise. I recommend cautiously stopping the stimulation when the signal-to-noise ratio is clear, and then replicating if you are using that information for threshold.
Electrode Location
Everyone has their own preference when it comes to electrodes. Disposable electrodes provide the benefit of infection prevention because they are sterile when they come out of the pack. There are a variety of electrodes, and some work better than others.
As far as electrode placement, high forehead is adequate in most cases. High forehead is indicated by the label Fz; F is for frontal lobe, z for midline. There are those who insist on the vertex, Cz, but I do not like scrubbing the fontanel of an infant, which is basically scrubbing the child's dura on the brain. Research clearly shows no consistent benefit in using the vertex over high forehead for infants. If possible, I would put the electrode on the earlobe, notated by A, for auris or ear. If you are putting the electrode on a mastoid, the symbol would be M.
There are some considerable advantages of the earlobe over mastoid, particularly a larger wave I. There is also less hair growth there, and you can keep the electrode away from the bone oscillator if you have to do bone conduction. The ground electrode can be placed anywhere, but a lower forehead location is very convenient, because you are already scrubbing that area, and there are no hairs, so tape or your sticky disposable electrode tends to stay on very well.
Filter Settings
The bottom line is to keep the low frequencies in whenever possible. If you can use a 30 Hz high-pass setting, then you include all the child's ABR energy. If you have to go up to 75 Hz or 100 Hz, do it, but be aware that you are more likely to filter out some of a younger infant’s ABR. The low-pass end of the filter can be 2000 or 3000 Hz, depending on how peaky you your ABRs. I like sharp peaks, but maybe you do not.
Do not use the notch filter. That removes energy in the region of 60 Hz, but also above and below. The notch filter takes a big chunk of the ABR energy out of the infant’s response before you even try to record it.
Measurement and Analysis
Measurement and analysis can be confusing for some people. I am going to make it simple. We have to do secondary calibration of stimuli for ABR stimuli because they are so brief that most of us cannot use our inexpensive sound level meters to calibrate it. Unlike pure-tone and speech audiometry, we are not typically performing ABR measurements in a sound-treated room where the ambient noise meets certain standards. We are doing them in a regular clinic room. We may be going to the intensive care nursery. We may be going to the operating room. We could be going to a patient's room. We might be off-site. We need to collect our own normative data on a small number of normal hearing adults. Modern-day ABR systems are remarkably stable. Once you have done this for your system, you do not have to do it on a regular basis. Look at it as more of a systematic biological check before you first start using your system.
First, find three to five adults with hearing thresholds of 10 dB or better out to 8000 Hz and normal OAEs. Make sure you remember their names so you can get them back if you ever need to do this again. Find their behavioral thresholds for air- and bone-conduction click, 500, 1000, 2000 and 4000 Hz. Perform this in your clinic in the room where you going to do the ABR. You need to know the lowest behavioral thresholds for those tone bursts. We cannot expect to record an ABR below where the normal-hearing person just perceives the stimuli.
The average value on the screen of your equipment for their behavior threshold becomes 0 dB nHL. For example, the average normal-hearing person can just hear the 500 Hz tone burst behaviorally at 20 dB, so 20 dB on the screen becomes 0 dB nHL, 40 dB on the screen is 20 dB nHL and onward from there. Do not perform this correlation in a sound booth and then go out and test the patient somewhere else.
There is another value that you need to think about. The ABR threshold does not typically occur at the behavioral threshold. The stimulus needs to be a bit above the behavioral threshold in order to activate the neurons and detect the response at a distance with the electrode on the scalp. When you are recording an ABR, you track the ABR wave V down to the lowest possible level, and then it disappears. For example, let’s say the response was not there at 15 dB, but began to emerge at 20 dB. That is not the behavioral threshold. The behavioral threshold will be a little bit better. There is some discussion and debate about exactly how much you need to subtract from the ABR threshold to estimate hearing level. It is sometimes called edB HL (estimated dB HL); the British use a somewhat different expression, but it is all about the same. If you use a 10 dB correction factor for all the stimuli including click, you will not be far off. You might find that some people do not use any correction for a click, because the click is so big, but they use 10 dB for all the tone bursts. There is plenty of information in the literature on this. I would advise you to talk to some colleagues and come up with your own plan. Many people subtract 15 dB from the ABR threshold intensity to estimate dB HL at 500 Hz, and 10 dB for the rest of the tone bursts. You can then plot the auditory thresholds on a form that looks like an audiogram. Plot the ABR thresholds and then show the estimated dB HL.
Figure 1 gives a quick breakdown of correction factors according to different researchers (Bagatto, Moodie, Scollie, Seewald, Moodie, et al., 2005; Hall, 2007). This is how much you would subtract from the ABR threshold to estimate hearing level.
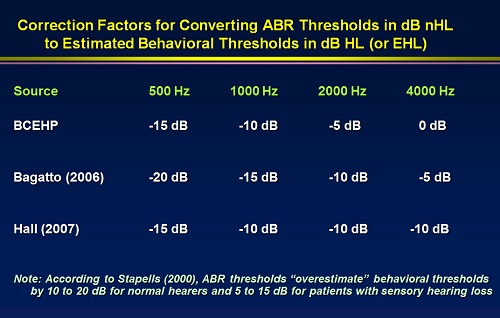
Figure 1. Correction factors applied to ABR thresholds by tone burst frequency to estimate hearing level. BCEHP= British Columbia Early Hearing Program.
This is the last step. You have found the lowest intensity level that produces a wave V, and now you want to estimate the audiogram threshold. These are the values that you use. David Stapells, as well as many others in replicated studies (Stapells & Oates, 1997), has clearly shown that behavioral threshold in dB is highly correlated with ABR threshold in dB. This works. This is the most important evidence in support of using ABR to estimate hearing thresholds for hearing aid fitting, and the correlation is stable.
Chirps
There is very prominent evidence that chirps have value. I am not suggesting we eliminate the tone burst. I think clicks and tone bursts are the workhorses for ABR, but there is definitely a role for the chirp, and the evidence is mounting very quickly. If you have not heard the chirp, it does sound like chirping birds.
Again, when you stimulate the cochlea with a click, you are activating the entire cochlea from the base to the apex. The problem is that the ABR is generated primarily by the neurons in the basal region. When you are using a tone burst, you are activating a relatively wide range of the cochlea, and yet only the very first part of the tone burst is producing the response. Much of the energy in the stimulus is wasted. With the chirp, we are giving the low-frequency energy a head start as it moves toward the apex of the cochlea. That tends to shift the wave V, which usually is delayed for the lower frequencies. It gives the wave V an opportunity to be produced five milliseconds earlier than it normally would. Wave V for 500 Hz is being produced around the same time as wave V for other frequencies, because the same process is being used for other frequencies. Wave V for 2000 Hz starts 1 to 2 milliseconds earlier, 500 Hz starts 5 milliseconds earlier, and 4000 Hz starts about 1 millisecond earlier. The click is instantaneous. We end up stacking the wave V responses, resulting in a larger wave V. The whole cochlea is contributing to the chirp click ABR.
It is important to note that the chirp was designed for use at low intensities. At high intensities, there are mechanical factors when stimulating the cochlea that make the chirp even worse than the traditional stimulus. Figure 3 shows tracings of click and chirp stimulus. Note the waveform produced by a high-intensity click at the top. There is good morphology with well-formed waves I, III, and V. Interwave latencies are normal.
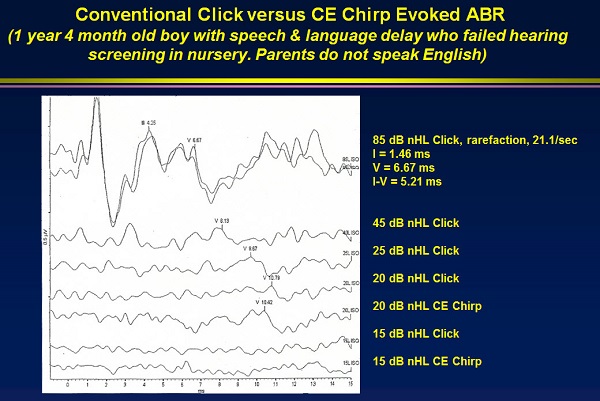
Figure 2. Comparison of a chirp click stimulus compared to a traditional click.
Next, I dropped down to a 45 dBnHL click (Figure 2). I recorded a nice wave V, and the latency shifted out as you would expect from 85 to 45 dB. I do not replicate. Once I am quite confident there is a response, I do not replicate as I decrease intensity. I decreased again to 25 dB for a traditional click and see a nice wave V; it is tracking down beautifully. I get down to 20 dB, and the response is still there, but it is getting smaller. All the little bumps you see at 20 dB are background noise. This is probably at about a 2:1 signal-to-noise ratio, where the response is barely there above the noise. You could always replicate to prove it.
Then I tested with the chirp to help me prove that this was a response. You can see the 20 dBnHL chirp under the 20 dB click (Figure 3), and it is beautiful. There is no question that 20 dB is the response. I did decrease to 15 dB for both the click and the chirp, and the responses disappeared. In this case, the chirp made me very confident that this child's threshold for the click is 20 dBnHL.
Figure 3 illustrates the same concept, but with a 4000 Hz tone burst. Everything starts out the same, but it gets very small very quickly. I went to 25 dB with the traditional tone bursts and there is no response and nothing that replicates. This is all background noise. I went to 30 dB with the chirp, and it is beautiful. Then I went down to 25 dB for the chirp, and it was perfectly repeatable. Based on what we have already learned, if there is an ABR at 25 dB at 4000 Hz, it is likely that the hearing threshold is probably around 15 dB, which is normal. I would not normally go any lower because I am interested in getting information for other frequencies. In this case (Figure 3), I was able record 5 dB lower in threshold, from 30 dB to 25 dB, by using the chirp. That is another advantage of the chirp, and it is due to the fact more of the cochlea is activated and the amplitudes are larger so that you can see them.
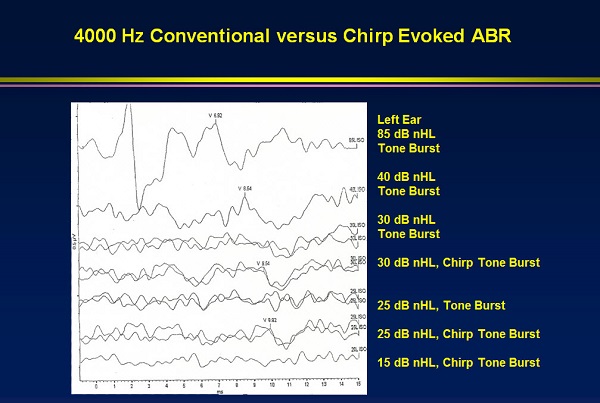
Figure 3. Comparison of 4000 Hz tone burst to 4000 Hz chirps.
I am stopping the averaging whenever I see a clear response. Figure 3 shows a good example of this when using chirps. I am using a stimulus rate of 37.7/sec, so it is not taking very long. In each tracing, every one of you could easily identify wave V. It is right where it should be. I would probably replicate the lowest intensity (15 dB), but the total time of less than 3000 sweeps was a little over a minute for all of this. You could obviously vary this. You could replicate the lower intensities or descend further to find the no response. In short, this is a way to get all the information you need for all the frequencies in both ears in a reasonable amount of time. The chirp does have value.
When we are done with that, we plot the ABR thresholds. Then we estimate the behavioral thresholds. These estimations are what you would use to decide whether or not you needed amplification.
An international study published last year (Gøtsche-Rasmussen, Poulsen & Elberling, 2012) showed that the amplitudes are the same for chirp octave bands and for regular tone bursts. Givens and Stuart at East Carolina University showed that the spectrum for the traditional tone burst and the spectrum for the chirps is the same. The information we are getting from chirp stimuli is equivalent to the information for tone bursts, except the amplitude is larger for chirps. Stangl, Rentmeester and Hood (2013) presented data that the amplitude for chirps is larger than both clicks and tone bursts, all the way down to the lowest intensity. I am a believer in chirps.
I would like to point out that the waveforms of tone bursts are more rounded than clicks. You will lose wave I as you move to the low frequencies, and the latencies will shift out; that is associated with travel time. Recognizing those changes will help you utilize the ABR in estimating threshold. Always compare the waveform latencies at different intensities and look at the whole ABR in that context. That is the way you can confidently identify thresholds at low levels, which is very important.
Bone conduction ABR
If you have the opportunity to do a bone conduction ABR on an infant under the age of four to six months versus waiting until they are older, test them when they are younger; the temporal bone is not yet fused to the other bones so you never have to worry about crossover or masking. The goal with bone conduction ABR is to record a wave I from the electrode on the side of stimulus. If you can do that, then you know that wave I is coming from the ipsilateral auditory nerve, and you have an ear-specific response. For example, if you stimulate the right ear and all you see are waves III and V, but no wave I, then you do not know for sure if the right ear producing the response. If you use a two-channel protocol and you get a wave I on the stimulus side and no wave I from the other channel, then you can be 100% certain that you do not need masking and that you have an ear-specific result.
The protocols are very well-established. You can get the best possible frequency response from a bone oscillator using a correct handheld strategy. When looking at the latencies for air conduction versus bone conduction, if the wave V latency is the same for air and bone, you must be stimulating the cochlea at the same level. The question is, “How much greater intensity did you need to present by air conduction to get the same wave V latency you got by bone conduction?” You overcame the air bone gap if you did that. That is a very clear, well-defined concept. You can estimate the air-bone gap with ABR.
Unsedated ABR Techniques
Sleep deprivation is a great technique for unsedated ABRs. Ask the parents to keep the child up late the night before, schedule the patient at 8:00 in the morning, and have someone come with the driver to keep the child stimulated in the car. As soon as they arrive, prep the baby’s skin, and they will probably fall asleep.
There are other strategies you can use, including melatonin, which is a safe alternative to sedation (Schmidt et al., 2007). It has been done with ABR. It is used for ECochG. You can find a vast selection of literature on the medical uses of melatonin. Chloral hydrate is not used any longer in the United States, not because it is not safe, but because the child does not wake up right away. They just keep sleeping and it is not very effective. It is not a good use of time, so anesthesiologists have stopped using it.
In the operating room (OR), we typically use Propofol or other general anesthesia. The OR is a very good place to record an ABR. The downside is there can be some health concerns. You do not want to immediately defer to the OR. Always try sleep deprivation if you can first. Anesthesia should be considered only when other alternatives have been tried and have not worked. A study in Pediatrics last year indicated that children who undergo anesthesia before the age of three are at a higher risk for developmental delays later in life (Ing, DiMaggio, Whitehouse, Hegarty, Brady, et al., 2012).
You also have the option of using a device like the Vivosonic Integrity, which has a special type of weighted averaging, a special type of electrode and Bluetooth technology that can minimize electrical artifacts. Patients do not have to be asleep. You can obtain good results from children who are reasonably quiet.
We will not talk about the ASSR, but certainly it should be part of your test battery, particularly for children with severe to profound hearing loss who do not have an ABR. It will help you sort out those children who are cochlear implant candidates immediately versus those who are likely to benefit from hearing aids.
Questions and Answers
Does a normal ABR indicate normal hearing or normal auditory function at the level of the brainstem?
First of all, let me differentiate between “normal hearing” and “normal hearing sensitivity.” I use the term “normal hearing” when I am referring to the whole hearing process, including auditory processing and how we use hearing for communication. With pure-tone audiometry, we are only measuring hearing sensitivity. But that can be confused with the perceptual detection of a sound. We could say “auditory thresholds,” which is what I usually say when I am being precise.
We are estimating auditory thresholds with the ABR. The ABR is not a test of hearing by any means and for many reasons. Technically, we are not measuring normal hearing sensitivity. That term would be reserved for behavioral testing. I am not a picky person when it comes to semantics, but we do need use the terms carefully.
At what level should click be performed, and are you worried about waking a sleeping child?
If the child is sleeping naturally and I believe they have normal hearing based on otoacoustic emissions (OAEs) or some other findings, I will start at 70 to 75 dBnHL and go down. My motto is never wake a sleeping child, but if the child is still sleeping, I will go back and test 80 or 85 dBnHL if wave I was not clear at 70 dBnHL.
The British group recommends not going to the very highest intensities unless there are no OAEs; this is very good advice. If OAEs are absent and there are no recordable ABR tracings or cochlear microphonic up to 80 or 85 dB, I do not think there is any danger in going to the highest levels. You have ruled out auditory neuropathy, and then you can go to the very highest level. Sometimes you only start to see a clear response when you get the highest intensities, particularly if there is a sensory loss. When determining threshold, I would go down to 20 dB whenever possible, because that will rule out any hearing loss greater than 10 dB HL.
How does a chirp differ from a regular TB at 4000 Hz?
The concept of a chirp is similar to a click. The click activates the entire cochlea, but the ABR response to a traditional click is only produced by high frequencies. The tone burst is rather frequency-specific, but the spectrum of the chirp, click and the tone burst is the same. Let’s say the tone burst has a two-cycle rise and fall time. It is the onset of the stimulus that generates the ABR. There is still a lot of energy in that tone burst that is not used. With the chirp, all of that energy is being used. It is similar to what we described for the click, but on a more limited scale on the cochlea.
Stapells recommends calibrating the ABR using peak-to-peak equivalent SPL values instead of establishing clinical norms. What are your thoughts on this?
David Stapells is a friend and colleague, and I highly respect his writings and recommendations. Most of us do not even have sound level meters anymore, so you would have to bring in a technician to do the measurements, which is not a bad idea. Peak-to-peak equivalent SPL is a way of knowing the exact intensity of your stimuli in dB SPL. Unless you consistently perform your ABRs in a sound booth, however, you are going to be using stimuli that are not high enough in intensity in certain settings. In other words, peak-to-peak SPL is a good way to verify the intensity level in a very quiet environment, but in a typical clinical environment, it is very misleading.
Peak-to-peak equivalent SPLs will certainly tell you that your equipment is stable, that your intensity level is not changing and that your earphones are still good, but I think you still need the behavioral follow-up in the different test settings where you will use the ABR.
Is there a difference in using alternating stimulus for click and then separating out condensation and rarefaction runs?
If your equipment allows you to use an alternating stimulus and then separate out the rarefaction and condensation waves, I recommend doing that. It is very time efficient, and you can compare rarefaction and condensation ABRs for the very same conditions. In other words, they were collected at the same time, as opposed to doing 2000 sweeps with rarefaction and then 2000 sweeps with condensation. If you cannot do it that way, then you have to do it the old-fashioned way. I always start with rarefaction. If you want to be safe, always use rarefaction and condensation at a high level. Make sure there is an ABR there and then proceed.
If you have differing thresholds between ABR and VRA and you need to fit a hearing aid, do you rely more on the physiological response or the behavioral response?
If I were giving a four-hour lecture on this topic, I would have some slides showing that there are several factors that influence behavioral findings that do not influence the ABR. That is one reason why we are doing the ABR; factors such as maturation, cognition, attention, motivation, and sometimes even language, in terms of instructing the child, are removed. Even though we tend to think of it as a gold standard, there are times when the behavioral test is in error and the ABR is telling us the truth.
If you are recording ABR and you get a threshold that is showing less hearing loss than the behavioral results, I would trust the ABR. If it is the other way around, I would probably trust the behavioral. That is where the crosscheck principle comes in. I would expect that child to have normal OAEs. I would expect acoustic reflexes to suggest normal hearing. We like to see agreement across our tests. This is true for ASSR and behavioral tests as well. Sometimes the electrophysiological results give us better estimates of hearing than behavioral results. Obviously, that varies depending on the child.
Thank you for participating today, and we hope you can join us for the other webinars in this month's electrophysiology series.
References
Bagatto, M., Moodie, S., Scollie, S., Seewald, R., Moodie, K., Pumford, J., & Liu, R. (2005). Clinical protocols for hearing instrument fitting in the Desired Sensation Level Method. Trends in Amplification, 9(4), 199-226.
Gøtsche-Rasmussen, K., Poulsen, T., & Elberling, C. (2012). Reference hearing threshold levels for chirp signals delivered by an ER-3A insert earphone. International Journal of Audiology, 51(11), 794-799. doi: 10.3109/14992027.2012.705901
Ing, C., DiMaggio, C., Whitehouse, A., Hegarty, M. K., Brady, J., et al. (2012). Long-term differences in language and cognitive function after childhood exposure to anesthesia. Pediatrics, 130, e476-485. doi: 10.1542/peds.2011-3822
Hall, J. W. (2007). New handbook of auditory evoked responses. Upper Saddle River, NJ: Pearson.
Stapells, D. R., & Oates, P. (1997). Estimation of the pure-tone audiogram by the auditory brainstem response: a review. Audiology & Neuro-otology, 2(5), 257-280.
Schmidt, C. M., Knief, A., Deuster, D., Matulat, P., & am Zehnhoff-Dinnesen, A. G. (2007). Melatonin is a useful alternative to sedation in children undergoing brainstem audiometry with an age dependent success rate: A field report of 250 investigations. Neuropediatrics, 38, 2-4.
Stangl, S., Rentmeester, L., & Hood, L. J. (2013). Auditory brainstem responses to clicks, chirps, tonebursts, and octave-band chirps. Poster presented at the 2013 Meeting of the American Auditory Society. Scottsdale, Arizona.
Yoshinaga-Itano, C., Sedey, A. L., Coulter, D. K., & Mehl, A. L. (1998). Language of early- and later-identified children with hearing loss. Pediatrics, 102(5), 1161-1171.
Cite this content as:
Hall, J.W. (2013, September). Application of ABR in objective assessment of infant hearing. AudiologyOnline, Article 12079. Retrieved from: https://www.audiologyonline.com


