Learning Objectives
After this course, participants will be able to:
- Describe the difference between acoustic trauma and more general noise-induced hearing loss.
- List the most common recreational sound exposures that can result in acoustic trauma.
- Identify prevention and treatment options to protect against damage from acoustic trauma.
Introduction
To begin this course, I would like to share a real-world case for which I was an expert witness. In 2007, a 50-year-old woman attended a rock concert with her husband at a relatively small venue (approximately 1,000 seats). Their original seats were obstructed due to construction and they were subsequently relocated. The pair were given seats that were in a prime location but were in close proximity to one of the main loudspeakers. Shortly after the show began, the woman asked her husband to purchase earplugs from the concession area, but they were sold out. After attending the concert for an hour and a half, the couple left. On the way home, the woman's ears were ringing significantly.
The next day, the woman woke up and her tinnitus had not improved. Her husband's ears were also ringing after the concert but recovered the following day. The woman went to their local ENT office. She reported no additional sound exposure other than having attended a few concerts in the past. The couple tried a few times to reach out to the tour management and concert venue. The response they received was not satisfactory, and they filed a lawsuit against the band and concert venue, citing unremitting tinnitus and hyperacusis. They ended up settling out of court, which entailed signing nondisclosure agreements. In general, the nature of these types of agreements is to state that no one is at fault and neither party has to admit error. The challenge with this outcome is that people don't become concerned about losing hearing when they attend rock concerts. Even those of us who work with the sound exposed population discount the idea of one concert causing an acoustic trauma. Part of the conversation today is to set the tone that the vast majority of people who go to shows do not sustain an acoustic injury; however, it can happen and here's an example of where it did.
The patient in this case presented with a stereotypical noise notch seen in Figure 1. It is important to note that it is a significant notch. She has normal hearing down through the low frequencies and then a steep drop to a 50-55 dB notch, classically recovering in the high frequencies. Her word recognition scores were very good. At the ENT visit, she did not complain of hearing loss; instead, her primary concern was tinnitus.
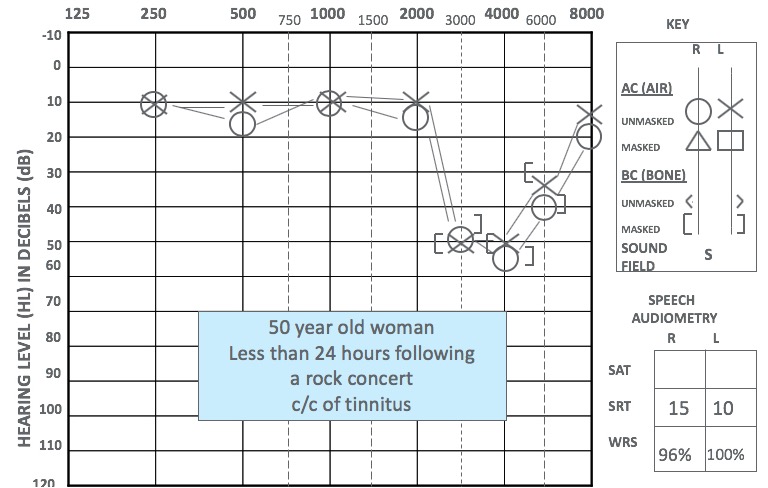
Figure 1. Audiogram less than 24 hours after exposure.
Two weeks later, a follow-up audiogram was performed (Figure 2). At that time, her bilateral hearing thresholds were normal. When performing a noise-induced audiogram, testing 3000 and 6000 Hz is critical. If she had been my patient, I would have tested the inter-octaves. Comparing the two audiograms, she presented with a 35-50 dB temporary threshold shift (TTS).
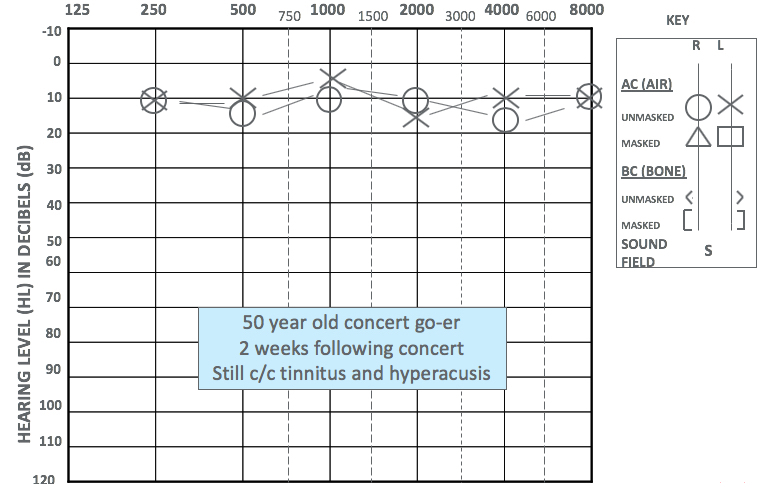
Figure 2. Audiogram two weeks' post exposure.
A patient who has an acoustic trauma is not just someone who experiences a hearing loss. Acoustic trauma also includes tinnitus, hyperacusis (i.e., hypersensitivity to loud sound) and diplacusis. The difference between noise-induced hearing loss and noise-induced hearing injuries include difficulty understanding speech in noise, which is not quantifiable on the audiogram. This can lead to other aspects, such as cochlear synaptopathy.
Preliminary Opinion
This woman experienced a documented sound exposure. We don't know exactly what that sound exposure was, however, we do have documentation that her TTS magnitude was 35-50 dB. She had unresolved tinnitus, and it became clear that she had hyperacusis after that. As an expert witness in this case, my opinion was that her symptoms were consistent with acoustic trauma.
I visited that venue and made previous recordings on two separate occasions of a different band. Those recordings indicated levels of 100-105 dBA and 107-110 dBA. This is in line with published reports at other venues which were measured at 103.4 dBA (Clark, 1992).
William Melnick wrote a summary paper in 1991 to indicate that across species, there is an exponential growth of how much temporary threshold shift you will get from certain sound exposures. For example, to get a TTS of 35-50 dB, you would need a sound exposure of 98.6-107.4 dBA. Let's think about what this woman's total exposure must have been, including not only the level but also the level over time. An allowable sound exposure is 85 dBA with a 3 dB time-intensity trading ratio. She was at the concert for 90 minutes. One to two hours of exposure at 98.6 dBA would result in a 289-579% noise dose. In comparison, one to two hours of exposure at 107.4 dBA would result in a 2211-4422% noise dose. Studies of sound exposure in animals have demonstrated that somewhere between 2500% and 4000%, you will get an acoustic trauma, or a permanent auditory injury, from a single exposure (Melnick, 1991). It is scientifically reasonable that this woman was in the range of sustaining a permanent hearing injury as a result of the sound exposure she experienced at the concert. This information helped the case.
Injury from Noise Exposure
Let us think about the terms injury vs. damage. As an analogy, if you get into a car accident, your car may be damaged, but you might be injured. Thinking of it in terms of hearing damage makes it sound like I damaged my car; it is very impersonal. On the other hand, if we refer to it as an injury, it's personal. When counseling our patients, using the term "injury" helps them understand the personal implications of noise exposure.
Acoustic Trauma
Acoustic trauma occurs when a continuous transient sound transfers enough energy to a cochlea to result in necrosis of the outer hair cells (OHC), inner hair cells (IHC), and cause glutamate excitotoxicity of first-order afferent neurons of the spiral ganglion (cochlear synaptopathy). This can occur when an impact or impulse sound, like an explosion, occurs abruptly. The force of that transient sound exceeds the elastic limit of the tissues. The organ of Corti can be sheared off the basilar membrane when the sound coming through the ear canal, middle ear and cochlea exceeds 132 dB peak SPL. If the sound is more intense than 184 dB, the eardrum is ruptured. We see this 184 dB and above with military sound exposures, such as with the explosion of an IED (improvised explosive device). When you have a shock wave, you don't just rupture the eardrum; you also have ossicular discontinuities. You can even end up with traumatic brain injury. As a result, you could have an auditory processing disability. Lung injuries can develop as well as some injuries to the viscera. Acoustic trauma is not caused by merely a transient sound; it is a massive overdose of sound. You can sustain an acoustic trauma from a single concert.
Chronic Exposure
Let's differentiate between the massive overdose that results in an acoustic trauma and an injury due to chronic noise exposure. This type of injury does not occur from exposure to sounds that are too loud for too long at a single event. Injury from chronic exposure occurs from sounds that are too loud, for too long and too often. The outer hair cells (OHC) are the primary site of lesion. If a person is exposed to noise from 78 dB up to about 132 dB, that's the range where your hearing will recover. You'll have a temporary threshold shift, but you should recover from your tinnitus. However, if you've been exposed to that level of noise often enough, you cross the threshold from recovery over to residual tinnitus, hearing loss and hyperacusis. You now have sustained a permanent threshold shift and a permanent tinnitus. Metabolic overload of the outer hair cells.
At higher levels of noise exposure, a waste product (comprised of oxygen byproducts) is produced that builds up in the cochlea. If there is too much waste that it can't be managed by our natural antioxidant defenses, a cascade of molecular events occurs inside the cell. The DNA unravels and the cell wall starts to bleb and blister, and close off different areas. It breaks into bits with the cell wall intact. These bits are ejected off of the basilar membrane and swept up by the white blood cells. There are supporting cells that maintain the structural integrity of the organ of Corti, but if you've lost that outer hair cell, it's no longer contributing to the active process that is hearing. If there is strong excitotoxicity, the inner hair cell is releasing so much neurotransmitter that it's causing an extreme response of the spiral ganglion cells, and you can end up with neuro pruning. You'll have a normal audiogram, but you may or may not have tinnitus secondary to this. The patient will have difficulty hearing and understanding in noise. This is the perceptual consequence of cochlear synaptopathy.
Signs of Chronic Exposure and Acoustic Trauma
Noise-induced temporary threshold shift (NITTS) and noise-induced permanent threshold shift (NIPTS) 3-6k Hz. The noise notch is due to the acoustics of the ear canal which is a Helmholtz resonator. This resonator provides a boost of gain to sound coming in around 2700 Hz in the average adult male. As a result, that added boost to sound in this frequency range hits the cochlea and causes damage between 3-6K Hz. Any amount of threshold shift that does not recover back to baseline is considered a residual loss (noise-induced permanent threshold shift).
Tinnitus. Another sign of chronic exposure and acoustic trauma is tinnitus, which often presents as tone-like hissing, generally in the range of the peak of noise-notch. For patients who can pitch match their tinnitus, it tends to be at the peak of their noise notch, or just slightly lower in frequency than the peak of the noise notch.
Hyperacusis. Individuals with hyperacusis have hypersensitivity to loud sound. As a result, not only might their floor or pure tone thresholds be poorer, but the maximum sound they can tolerate, or loudness discomfort levels, might also be lower. If it's biological hyperacusis, not a psychological, you can measure abnormally low loudness discomfort levels with acoustic reflex thresholds. Acoustic reflex thresholds can be beneficial in diagnosing but may cause discomfort to the patient.
Diplacusis (abnormal pitch perception). Diplacusis causes a patient's pitch perception to be off. Things will sound sharp or flat, and patients can have a difference between the two ears. This can be especially frustrating for a musician.
Suprathreshold speech intelligibility in noise decline. These patients require a better signal-to-noise-ratio to hear and understand speech in noise. This decline can be measured by tests such as the HINT or QuickSIN.
Necrosis vs. apoptosis. Whether it's traumatic, an acoustic trauma vs. chronic exposure depends on the actual pathophysiology. The inflammatory response is part of our body's defense mechanism. Inflammation is part of our body's immune system. Apoptosis is the death of cells that occurs as a normal and controlled part of an organism's growth or development. With apoptosis, you have limited inflammation. Necrosis is the death of most or all of the cells in an organ or tissue due to disease, injury, or failure of the blood supply. With necrosis, you get lots of inflammation.
Acoustic Trauma from Various Recreational Noises
The following recreational noises have the potential to cause acoustic trauma:
- Firearms Exposure (Unprotected)
- Includes fireworks
- Live Music Events
- Recorded Music
- Musical Occupations (Musician, DJ, Audio Engineer, etc.)
- Motor Sports (NASCAR, Indy 500, Truck Rally, etc.)
Firearms
The number one cause of recreational acoustic trauma is unprotected firearm exposure. In addition to guns, rifles, and pistols, this also includes fireworks. This information comes from two different AudiologyOnline courses. One of these courses was presented by Michael Stewart, PhD (July 2008); the other was presented by Capt. William Murphy, PhD (June 2018).
Generally, the larger the caliber of bullet, the louder the sound. In Figure 3, you can see that as you go from smaller to medium to a large caliber rifle, you get higher sound levels. Also, the shorter the barrel, the louder it is. If you have a muzzle break on it, which keeps the kickback from being strong, this results in a louder sound. If you shoot in an enclosed area, you get a lot more sound bouncing back at you. It is important to note that the risk for acoustic trauma increases 10-fold with every 10-fold increase in rounds fired.
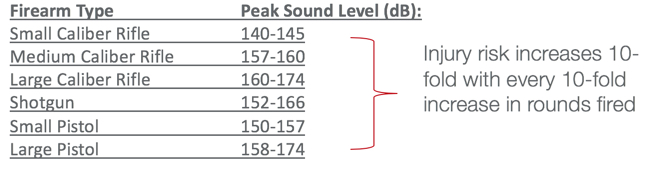
Figure 3. Firearms and peak sound levels.
Acoustic trauma caused by fireworks will be high frequency. Patients exposed to loud fireworks will generally present with tinnitus. Please warn your patients during the holiday celebrations to utilize fireworks with care. One incident of being exposed to fireworks can cause acoustic trauma (Gupta and Vishakwarma, 1989; Ward & Glorig, 1961).
Live Music Events
To reiterate, it is possible to acquire acoustic trauma from attending one rock concert. If a concert attendee has a high susceptibility for noise-induced hearing loss, and they happen to be sitting close to the speakers at an extremely loud concert, their exposure can exceed 2500%, even reaching over 4000%. Some of these venues are required to keep track of their sound levels over time in order to protect themselves against being fined by the local government for exceeding community noise levels. As such, they will have a good running record of what the levels were at the front of house speaker. In those cases, you can look at the patient's ticket stub and determine where they were seated in relation to the loudspeakers. Assuming no reflections, the Inverse Square Law teaches us that for every doubling of the distance from the sound source, the sound intensity will diminish by 6 dB. Conversely, there will be a 6-dB increase in intensity when you halve the distance from the sound source. It stands to reason that people who are closer to the speakers would be subjected to high sound exposures. Some high-profile musicians/bands who have had lawsuits brought against them include Tom Petty (civil suit in Chicago) and Whitesnake (civil suit in Boston).
Recorded Music
Can recorded music cause acoustic trauma? With newer technology (e.g., iPods, iPhones or SmartPhones), in general, the answer is no. However, it is possible to get acoustic trauma using older technology.
Older technology (CD Players). The sound output levels of portable listening devices from CD players can cause an acoustic trauma (Figure 4). The sound levels range from 80-105 dB free-field for most CD players, with one of the players being markedly lower (Fligor & Cox, 2004). The maximum instantaneous peak sound level that a CD Player with earbud earphones could hit, according to the Fligor and Cox (2004) is 136 dB SPL.
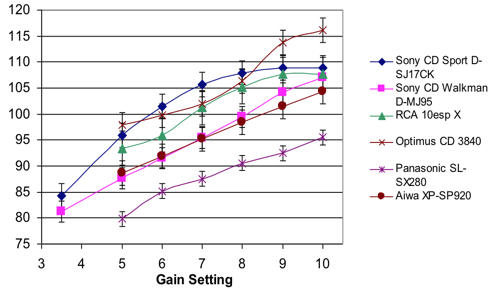
Figure 4. The output of older technology (e.g., CD Players).
Newer technology (smartphones, HD players). The data regarding more modern technology shows a very tight clustering, with max output levels at only about 102 to 103 dBA for the free-field equivalent (Figure 5). Looking at percussion peaks using aftermarket earphones, the iPod earbud measured the highest. Max output levels were about 127 dB peak SPL. There were high peaks, however, it would take thousands of those to cause an acoustic trauma. The newer technology can't produce peaks high enough to cause an acoustic trauma unless you use specific aftermarket earphones that have a high sensitivity. For every additional balanced armature driver that's added into an in-ear monitor, you're doubling the sensitivity. For every volt that's applied to the earphone, you're adding 6 dB maximum sound output. The maximum voltage output of a smartphone, at least in the United States, is 0.5 volts. The Apple EarPod's max output is 105 dB/volt at 1000 Hz. This is not capable of causing damage unless you're listening for more than 15 minutes. In Ultimate Ears, a quadruple driver, non-custom headphone, it is 139 dB/volt. You can get sustained levels up at the highest volume control. Full custom in-ear monitors (e.g., Ultimate Ear 16, JH16, 64 Audio A18) while they can be used safely, have the potential to cause damage. It's all about knowing that it is a powerful system that can significantly exceed what your ears can tolerate. The maximum instantaneous peak sound level that a Creative Zen MP3 Player with iPod earbud earphones could hit 126.9 dB SPL. Users need to set them to a comfortable level in quiet and resist the urge to turn it all the way to the maximum (Portnuff, Fligor & Arehart, 2011).
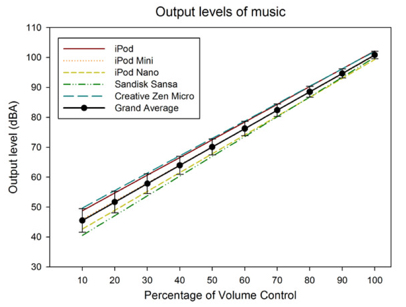
Figure 5. The output of newer technology (e.g., Smartphones, HD Players).
I would encourage any of you who are fitting custom in-ear monitors to use your hearing aid verification equipment and do probe microphone measures. Teach patients the maximum level to which they should set their volume dial before they start to put themselves at risk. Compare their chosen listening level to how long they can listen to using the 85 dBA exchange rate criteria. This will help give them a little bit of guidance. According to the published guidelines, we shouldn't listen for more than 15 minutes. This is how we, as a profession, can bring value to these customers who want full custom in-ear monitors. They're willing to pay $800 to $2000 for a pair of custom headphones, and we can educate them about preventing damage to their hearing. Heed caution when fitting this powerful device to a patient. If they use it unsafely, and if you did not counsel them effectively how to use it safely, you could be at legal risk.
Occupational Noise
It is possible for musicians, DJs, and audio engineers to acquire occupational-related acoustic trauma from their line of work. In 2005, a group of researchers looked at sound levels and exposures at dance clubs in Argentina. Typical sound levels in the dance clubs were 104.3 dBA - 112.4 dBA, with doses routinely exceeding 1600% -- six times the allowable dose (Serra et al., 2005). At this rate, you're quickly going to hit a massive overdose. For musicians and audio engineers, it depends whether they use floor wedges (105-110 dBA) vs. custom in-ear monitors (80-122 dBA). Keep in mind that there is a risk of amplifier malfunction. If the pack they plug their custom in-ear monitor does not have peak limiting, white noise has the ability to blare through the in-ear monitor at full voltage.
Motor Sports
There are a lot of people who love NASCAR races, which last about four hours. If you attend a NASCAR event with reasonably good seats (150 feet away from the track), the average sound exposures are about 101 dBA with a 2016% dose. If you have excellent seats (20 feet away from the race track), the average sound exposure is 106 dBA with a 6400% dose. This translates to 64 times your allowable sound exposure. If you are not using hearing protection, you are likely going to have an acoustic trauma (Rose et al., 2008).
With other recreational vehicles (e.g., ATVs, jet skis, motorcycles), it is tricky to measure the sound levels, as you have a lot of wind noise. Bear in mind that if a person rides one of these vehicles for six hours, they can get a 2500% dose. Clearly, wearing hearing protection during these activities is a reasonable and appropriate thing to do.
Protective Measures
Hearing Protection
Passive. Passive hearing protection (which does not include filters) comes in non-custom and custom forms. Foam earplugs are very effective. If you're using non-custom earplugs, insertion depth is crucial. Putting the plug in all the way ensures that you are blocking out as much as the plug is intended to. If you have a full custom option, not only will things sound better but you will have consistent protection. The personal attenuation rating (PAR) vs. the labeled noise reduction rating (NRR) of non-custom vs. custom hearing protection methods is very different (Neitzel et al., 2004). If it's a custom earplug, the PAR should be at the same level as the noise reduction rating, if not a little bit higher.
Active. In some situations, however, you don't want a consistent amount of sound isolation. Such is the case with hunters: they want situational awareness to be able to listen for game. They also want to be able to hear other hunters in their vicinity, for safety reasons. That's where active hearing protection comes into play. With one-size-fits-most sleeves that are not fit perfectly to the user's ears, in addition to potentially being uncomfortable, low-frequency sound can get through when you fire off a round. You might get a lot of sound coming past the non-custom piece. On the other hand, a full custom earplug is fitted to each user's unique ear shape. All the sound goes indirectly through the microphone and back out, allowing the user to hear soft noises just as loudly, or perhaps amplified slightly. In contrast, when a loud sound occurs, the analog circuit acts faster than the sound wave does, and it provides that amount of attenuation that you need to protect your hearing.
There are a few different custom products on the market. I'm a fan of the products by EDA Medical Research, (now Lucid Audio). Two of their devices for hunters are the Gun Sport Pro and the Blast Pro. For musicians, they have the Music Pro. These devices use a size 10 battery. You can switch from a slightly higher attenuating mode to a slightly lower attenuating mode with a toggle switch.
Chemicals/Medications
There is the potential to have restoration in the early stages. Currently, what's being used for people who have suffered an acoustic trauma are intratympanic steroid injections. Physicians can inject Prednisone into the middle ear space. If the mechanism of damage is necrosis, the steroid, as it crosses over the round window into the perilymph you can get a reduction in how much inflammation occurs, which in turn limits how much damage occurs. This option is invasive. You have to see a specialist who's capable of performing an intratympanic injection quickly, within the first 24 to 48 hours. The faster you get in and have the injection done, the more hearing can be preserved. This reduces how much damage occurs in the first 48 hours due to the necrotic process.
A couple of medical compounds have been used experimentally: N-Acetyl Cysteine (NAC) and D-methionine (D-Met). These are options where there is real potential to allow for rescue against noise-induced hearing loss. Also, a dietary supplement of specific concentrations of vitamins A, C, E, and magnesium could be used prophylactically to lessen a person's susceptibility to noise-induced hearing loss and acoustic trauma.
Summary and Conclusion
In summary, it is possible to sustain an acoustic trauma from recreational exposure, although the vast majority of people do not. Bear in mind that unprotected firearms exposure is the number one cause of recreational noise-induced hearing loss and can cause immediate acoustic trauma. High-level continuous sound can result in severe noise overdose, leading to necrotic death of cells in the cochlea, as the inflammatory process causes widespread damage. You don't need a blast or a transient sound to have an overdose that results in the necrotic effect. Finally, listening to recorded music cannot cause acoustic trauma, except with certain aftermarket earphones/custom in-ear monitors.
References
Fligor, B. J., & Cox, L. C. (2004). Output levels of commercially available portable compact disc players and the potential risk to hearing. Ear and hearing, 25(6), 513-527.
Kujawa, S. & Liberman, M. (2009). Adding insult to injury: cochlear nerve degeneration after “temporary” noise-induced hearing loss. Journal of Neuroscience, 29(45), 14077-14085.
Gupta, D., & Vishwakarma, S. K. (1989). Toy weapons and firecrackers: a source of hearing loss. The Laryngoscope, 99(3), 330-334.
Melnick, W. (1991). Human temporary threshold shift (TTS) and damage risk. The Journal of the Acoustical Society of America, 90(1), 147-154.
Murphy, W. (2018). Assessment of firearm noise exposures and hearing loss prevention. AudiologyOnline, 31240. Retrieved from https://www.audiologyonline.com
Neitzel, R., Seixas, N., Olson, J., Daniell, W., & Goldman, B. (2004). Nonoccupational noise: exposures associated with routine activities. The Journal of the Acoustical Society of America, 115(1), 237-245.
Portnuff, C. D., Fligor, B. J., & Arehart, K. H. (2011). Teenage use of portable listening devices: A hazard to hearing?. Journal of the American Academy of Audiology, 22(10), 663-677.
Rose, A. S., Ebert Jr, C. S., Prazma, J., & Pillsbury III, H. C. (2008). Noise exposure levels in stock car auto racing. ENT: Ear, Nose & Throat Journal, 87(12).
Serra M., Biassoni E., Richter U, Minoldo G. & Franco G. (2005). Recreational noise exposure and its effects on the hearing of adolescents. Part I: An interdisciplinary long-term study. Int J Audiol, 44(2), 782–792.
Stewart, M. (2008). Recreational firearm noise exposure. AudiologyOnline, 11552. Retrieved from https://www.audiologyonline.com
Ward, W. D., & Glorig, A. (1961). A case of firecracker‐induced hearing loss. The Laryngoscope, 71(12), 1590-1596.
Citation
Fligor, B. (2018, July). Acoustic trauma from recreational noise exposures. AudiologyOnline, Article 23542. Retrieved from https://www.audiologyonline.com


