From the Desk of Gus Mueller
 Consumers shopping to purchase hearing aids often are looking for the best brand, like they might do if they were purchasing a television or a dishwasher. We of course know that by far, what is most important is not the brand of the instruments, but how the devices are programmed for each individual patient. The best hearing aid on the market can be rendered worse than a PSAP if programmed wrong. That’s a lot of pressure for us to “get it right.” And how do we do that?
Consumers shopping to purchase hearing aids often are looking for the best brand, like they might do if they were purchasing a television or a dishwasher. We of course know that by far, what is most important is not the brand of the instruments, but how the devices are programmed for each individual patient. The best hearing aid on the market can be rendered worse than a PSAP if programmed wrong. That’s a lot of pressure for us to “get it right.” And how do we do that?

Gus Mueller
We need a good starting point, and it’s not something we want to tackle on our own. Earl Johnson, in his 20Q article of 2012, pointed out that even when you have a general idea of the gain that a person might need, with today’s multichannel instruments, you still have 1430 possible frequency responses remaining from which to choose. And that is just for one input level. Fortunately, we can rely on validated prescriptive fitting methods, such as the NAL-NL2 and DSLv5. The researchers behind these methods have done all the heavy lifting for us.
Some might say another option would be to use a manufacturer’s proprietary formula to fit the instruments. Research suggests that this approach is a bit risky - actually, make that very risky. One of my favorite studies from the past few years was conducted by Ron Leavitt and Carol Flexer (2012). They tested the premier instruments of the six leading manufacturers, using the QuickSIN, with the hearing aids programmed first to the manufacturer’s proprietary fit, and then to a NAL-NL1 fitting. When the NAL-NL1 fitting was applied, the mean QuickSIN SNR score improved by nearly 7 dB across instruments, and around 10 dB for the products of two manufacturers. Those are huge improvements—large enough to change a patient’s quality of life.
We know we need a good starting point to fit hearing instruments, we know that there are validated prescriptive methods that provide this for us, and we know these validated methods clearly trump proprietary fittings. So how are we applying all this in clinical practice? We’ll explore that topic in this month’s 20Q.
Gus Mueller, PhD
Contributing Editor
May, 2015
To browse the complete collection of 20Q with Gus Mueller CEU articles, please visit www.audiologyonline.com/20Q
20Q: Today's Use of Validated Prescriptive Methods for Fitting Hearing Aids - What Would Denis Say?
- Participants will be able to explain the advantages of using validated prescriptive methods for fitting hearing aids.
- Participants will be able to describe the drawbacks of not using a validated prescriptive method for fitting hearing aids, or using non-validated methods such as “clinical hunch” or manufacturers’ best fit.
- Participants will be able to explain the current status of the use of validated prescriptive methods among hearing care professionals.
1. Denis?
Yes, Denis Byrne was a noted Australian audiologist. He died in April of 2000, so his main body of work probably was before your time. He didn’t invent hearing aid prescription, but through his work we are able to use these methods based on a sound rationale and self-critical research. If I had to name a “father of prescriptive hearing aid fittings,” he certainly would be my man.
2. When I hear prescriptive fittings and Australia together, I think of the NAL (National Acoustics Laboratories) fitting method. Was that his baby?
It certainly was, and to some extent it still is, as much of his basic philosophy regarding that method is still in play. Here is a little history to help catch you up. Back in 1976, an article from Australia was published in the journal Scandinavian Audiology describing a new prescriptive fitting method for hearing aids. The article was written by Dr. Byrne and his colleague Dr. Will Tonnison. While the paper was highly regarded, the method itself had little clinical impact in the U.S. At the time, many audiologists still believed it was necessary to use speech audiometry to select the best hearing aid, and the few who did favor prescriptive fittings quickly latched onto the Berger method, which was also introduced about this time.
When the revised version of the Australian method, the NAL-R, came out 10 years later (Byrne & Dillon, 1986), the U.S. climate was quite different. Clinically friendly probe-mic equipment was now available, and most audiologists had started using some form of a prescription fitting approach. The cleverly designed multi-colored slide rules made the NAL-R math a little easier, and so audiologists began adopting this method. Custom hearing aids were popular at the time, and these slide rules were handy devices for calculating the desired 2-cc coupler values that were needed when these hearing aids were ordered.
Figure 1. Hearing aid fitting slide rules available from the NAL, commonly used in the 1980s. These slide rules were used to calculate the 2-cc coupler output that would correspond to NAL fitting targets when ordering custom instruments. Separate slide rules were available for BTE, ITE and body level instruments.
The NAL-R method soon was included on probe-mic equipment, with fitting targets for insertion gain already calculated. It quickly became the most popular fitting method for adults in the U.S., and probably around the world. By this time, Harvey Dillon had become part of the research team at NAL that was behind these algorithms.
By the early 1990s, non-linear hearing aid fittings were becoming the norm, so what we saw next was the first non-linear version of the NAL, the NAL-NL1. Around five years ago, a revision of this method was introduced, the NAL-NL2, and that is the version in use today.
3. Thanks for the review. So what would Denis say?
For starters, he’d probably say there is no reasonable alternative to using a prescriptive method to fit hearing aids. The moment that something as simple as selecting the maximum gain, or what instrument to fit to a given patient, a prescriptive method must be used in some rudimentary form. What he did say, back in 1982 was this (p. 176):
“The only choices are whether we admit to using a theoretical procedure, or even realize that we are doing so, and whether we are prepared to say what procedure we are using . . . The only problem with confessing to using a theoretical procedure is that it inevitably exposes our inadequacies.”
I think he’d also say that he’s a little disappointed that his research findings from all those years of hard work are now mostly ignored, as most people fitting hearing aids seem to prefer the manufacturer’s fitting algorithm.
4. I agree that using the manufacturer’s algorithm has become popular, but isn’t that a prescriptive method too?
In a sense it is, but the key term here is a validated prescriptive method. And by validated, I think we would all agree that we are looking for optimum levels of benefit and satisfaction, which nearly always relate to good audibility and speech understanding. Of course you could define validation as the best “first acceptance,” the most “natural” sounding, or the least amount of feedback - but what if it is at the expense of overall benefit in terms of actual hearing? If good validation information is available for the manufacturer’s proprietary fittings, comparing them to the NAL or DSL algorithms, I haven’t seen those data published for the current versions.
5. What about simply using clinical experience to fit hearing aids? I hear many audiologists say they tweak the fitting from the very beginning to obtain a better result.
I’d be the first to admit that our validated methods such as the NAL-NL2 are for the average patient, and indeed, some tweaking will be required for some patients. But, you have to start somewhere. If you really know a clinician that has a better starting place than the NAL-NL2, or DSLv5, or any other validated method, encourage him or her to publish that algorithm as soon as possible.
In November of 2001, Harvey Dillon gave the Denis Byrne Memorial Lecture at the annual meeting of the American Speech and Hearing Association. A transcript of this talk was subsequently published at AudiologyOnline (Dillon, 2001). The entire transcript is a great read, but specifically relating to your question, here is what Harvey had to say about Denis:
From time to time, Denis encountered critics of his work who claimed they selected and adjusted hearing aids using their considerable ''clinical experience''. Furthermore, they claimed, such methods were more effective than anything based on a formula could ever be, as they took many more aspects of the patient into account than did any prescriptive approach. While Denis readily agreed that there was more to a patient than an audiogram, he was scathing of ''experience'' as a scientific approach to audiology. His attitude can be summarized in the following three paraphrases:
- If you can't write down the rules you use, you probably don't understand what you do.
- If it's not written down, no one else can do it, and no one can test whether it's better or worse than some alternative approach.
- If you can't evaluate your procedure you can't improve it.
6. Okay, we’ll table “clinical experience” for the moment. Going back to the manufacturer’s proprietary fittings—there must be some research comparing these fittings to methods such as the NAL?
There is. I reviewed some of this research last year in an AudiologyOnline article (Mueller, 2014a), so I won’t go over all of it again here. Briefly, we know that in lab studies individuals will do much better for speech understanding in noise using the NAL fitting (Leavitt & Flexer, 2012). And, we know that the NAL fitting is preferred by the majority of the users in the real world compared to proprietary fittings, and this preference also is reflected in significantly greater benefit on self-assessment scales of benefit such as the APHAB (Abbreviated Profile of Hearing Aid Benefit; Abrams, Chisolm, McManus, & McArdle, 2012).
7. Those data were collected a few years ago. Software and hearing aids have changed. Maybe things are better with current proprietary formulae?
I don’t think so. Let me review a project we completed at the University of Northern Colorado, published recently by Sanders and colleagues (2015) in the Hearing Review. These data were collected in October of 2014, so this is pretty much the same software and hearing aids that you are using today. We examined the real-ear output (16 ears) for premier hearing aids for the proprietary fitting for five leading manufacturers. We tested at three input levels, 55, 65 and 75 dB SPL, using the real speech signal of the Audioscan Verifit. The results are shown in Figure 2.
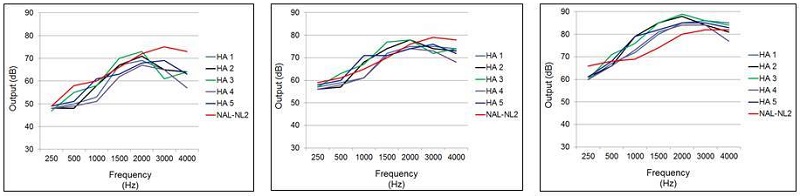
Figure 2. Mean earcanal SPL output for the proprietary fitting (experienced user, bilateral fitting) of five leading manufacturers for a mild-to-moderate downward sloping hearing loss. Data shown left to right for inputs of 55, 65, and 75 dB SPL. The NAL-NL2 targets are displayed as reference. (Adapted from Sanders et al., 2015).
This was for a downward sloping hearing loss, going from 25 dB in the lows, to 70 dB in the highs. The NAL-NL2 targets also are plotted. Granted, the proprietary methods aren’t geared to meet NAL-NL2 targets (you could simply use the NAL algorithm if they were), but this provides a reference. Notice that we do see a 5-8 dB difference among manufacturers, but perhaps more remarkable is that the pattern of the output for all the proprietary fittings is considerably different than that of the NAL-NL2. Maximum output is applied in the 1500-2000 Hz range rather than in the higher frequencies where the hearing loss is the greatest. This hypothetical patient only had a 60-70 dB loss at 3000-4000 Hz, so audibility before feedback isn’t an issue, and I therefore don’t quite understand this “boost-in-the-mids” logic.
8. Did you conduct speech recognition for these different fittings?
No, but we did record the SII (Speech Intelligibility Index) that was present for all the measurements for each participant, which was calculated automatically by the probe-mic equipment. These values for the three input levels compared to the NAL-NL2 fitting are shown in Figure 3.
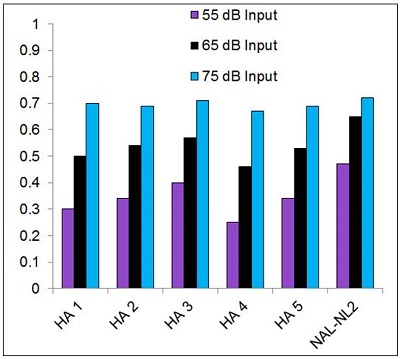
Figure 3. Mean SII values (as calculated by Audioscan Verifit) for the proprietary fitting (experienced user, bilateral fitting) of five leading manufacturers for a mild-to-moderate downward sloping hearing loss. Data shown are for inputs of 55, 65, and 75 dB SPL. The SIIs for a precise fitting to NAL-NL2 targets are shown as a reference. (Adapted from Sanders et al., 2015).
As shown in the Figure, for the 55 dB input, there is a sizeable difference between the SII of most of the proprietary fittings compared to the NAL-NL2. As the input goes up, the differences become smaller. The most conservative fitting for the 55 dB input was HA-4, with an SII of only 0.25, compared to 0.47 for the NAL-NL2. For some listening situations, going from 0.25 to 0.47 can improve speech recognition substantially.
9. At least the SII is similar to the NAL-NL2 for the higher inputs?
That’s what the chart says, but I’m not so sure that would be true for real world listening, assuming the patient has control of the volume of the hearing aids. Let’s go back to Figure 2 and look at the output for the 75 dB input for HA-3. This is the hearing aid that had an SII about the same as the NAL for this input level. Note that the output in the mid frequencies (1000 to 2000 Hz) is about 10 dB greater than the NAL prescription. Could the NAL be that far off on their calculations of preferred loudness for this frequency range? I’m thinking that for many patients this will be too loud, and as soon as this person turns down the gain, those SII values will drop (along with the ones for average and soft too). Yes, I recognize that they also could turn down gain for the NAL-NL2 fitting, but if gain is optimized across frequencies, there is less chance that this will happen.
10. So I’m now wondering why some dispensers use the proprietary fittings? But, if most adults are fitted to the NAL gain and output targets maybe it doesn’t matter much?
It matters. My best guess is that no more than 10% of patients are fitted to the NAL prescriptive targets. That’s exactly why I’m going with the “What would Denis say” theme.
11. What? How can it be that low? Where are you getting those numbers?
I’ll gladly work through my thinking for you.
First, to state the obvious, if you’re not using probe-mic measures to obtain the correct output in the earcanal, you’re not fitting to the targets. Matching things up on the manufacturer’s fitting screen just doesn’t cut it—we can talk about that later if you like. So the first thing we need to look at is what percent of people fitting hearing aids are routinely using probe-mic verification. That’s probably no more than 25-30% (see Mueller, 2014a; Mueller & Picou, 2010).
Secondly, we also can look at what percent of professionals, when fitting hearing aids to adults, are selecting “NAL” (or “DSL”) in the fitting software to begin with. Manufacturers report that as many as 75% or so of their customers use the company’s “default proprietary fitting.” And this is not just anecdotal reports or idle speculation. That figure is based on monitored software activity collected from dispensing professionals. Now I guess it’s possible that someone could first select the manufacturer’s proprietary algorithm and then verity to NAL targets using probe-mic measures, but this seems unlikely.
Also, Erin Picou and I conducted a survey a few years back regarding the use of probe-microphone measures (Mueller & Picou, 2010). We asked respondents who already had categorized themselves as people who used probe-mic routinely, to identify the primary reason they conducted this testing. They were given four possible choices, including what we thought was the most logical: “to match gain and/or output to prescriptive fitting targets (e.g., NAL or DSL) displayed by the probe-mic equipment.” Only 27% selected this reason.
So to summarize, only 25% or so of dispensers initially set out to fit to the NAL by selecting it in the manufacturer’s software. Only 30% or so of these do probe-mic testing, and many of the audiologists doing probe-mic testing are not doing it for the purpose of verifying prescriptive targets. I think that leaves us with something around 10% (or less) who actually are fitting to the NAL.
12. You’re suggesting that when you click on “NAL fitting” in the software you’re not getting a NAL fitting in the real ear? Why is that?
I don’t know exactly why, but this isn’t really breaking news. David Hawkins and Jodi Cook told us about this back in 2003. And just three years ago Aazh, Moore and Prasher (2012) reported that of 51 fittings, after programming to the manufacturer’s NAL in the fitting software, only 29% matched NAL-NL1 targets within +/- 10 dB. Now this was only for one manufacturer, but unfortunately, it appears to be the norm.
13. How do you know this is the norm across manufacturers?
Comparing the manufacturer’s NAL-NL2 fitting to real-ear NAL-NL2 targets for different inputs also was part of the Sanders et al. (2015) research from the University of Northern Colorado that I mentioned earlier. The test protocol for real ear measures using 16 ears was essentially the same as used for the testing for the proprietary fittings; downward sloping audiogram, bilateral fitting, experienced user. The results of this testing is shown in Figure 4.
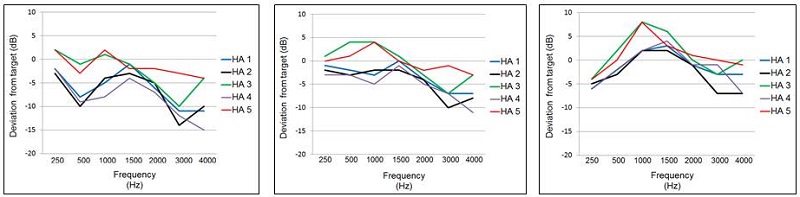
Figure 4. Mean deviation (dB) from NAL-NL2 real-ear prescriptive targets for the manufacturer’s NAL-NL2 fitting (experienced user, bilateral fitting). The zero line represents a precise NAL-NL2 fitting. Data shown for the five leading manufacturers for a mild-to-moderate downward sloping hearing loss. Data displayed left-to-right for inputs of 55, 65, and 75 dB SPL. (Adapted from Sanders et al., 2015)
For these data, we displayed the findings as deviation from target, with the zero line being a perfect real-ear fit to the NAL-NL2. As shown, except for HA-5, the output varies considerably from NAL-NL2 targets. The pattern of deviation from NAL-NL2 seems to be fairly consistent among manufacturers:
- Reduced gain for soft inputs
- Roll-off of high frequencies above 2000 Hz
- Boost in gain for mid-frequencies, to the extent that output exceeds NAL-NL2 targets for the 75 dB inputs
- A more linear fitting than prescribed by NAL-NL2
Interestingly, while the real-ear findings of 4 of the 5 manufacturers’ NAL-NL2 algorithms differ significantly from the desired NAL-NL2 targets, they are quite similar to the respective manufacturer’s proprietary fittings, and they tend to fit NAL-NL1 a little better than NAL-NL2.
14. How did the fittings look on the manufacturer's fitting screen?
For 1000 Hz and above, the output shown on the fitting screen never deviated by more than 1 dB from the NAL-NL2 targets shown on the fitting screen.
15. Could it be that there were just a few people with strange ears that threw off the mean values?
The large mismatch to target in the highs was a pretty common finding for all subjects, except when HA-5 was fitted. As reported by Sanders et al. (2015), individual data for the 80 fittings (16 ears x 5 products) at the 55 dB SPL input revealed that, in 59 of the 80 cases (74%), the measured output varied from the NAL-NL2 target by 10 dB or more for at least one frequency (250-4000 Hz). If HA-5 (the product that resulted in a reasonably close fitting to NAL-NL2) is removed from the calculations, of the remaining 64 fittings, 86% varied by 10 dB or more from the desired NAL-NL2 fitting targets. For these later 64 fittings, compliance with the NAL-NL2 was somewhat better for the 65 dB SPL input, but there still were 35 (55%) of the fittings where the ear-canal SPL deviated by 10 dB or more from the desired output. This was nearly always in the high frequencies.
16. You mentioned that the manufacturer’s NAL-NL2 fitting tended to be more linear?
Yes, which is why if you look at the higher frequencies, the deviation from target becomes smaller as the input increases. Maybe not surprisingly, the proprietary fittings are even more linear. We can observe this if we go back to Figure 2. Note that for the 55 dB SPL input, the NAL-NL2 targets are around 73-75 dB SPL for the 2000-4000 Hz range. For the 75 dB SPL inputs, you’ll see that the NAL targets are around 82-85 dB SPL for the same frequency range, roughly a 10 dB change in output for a 20 dB change in input—what you might expect for someone with a dynamic range of 40-45 dB. Now if you look at one of our test instruments, say HA-3, you see that the mean real-ear output went from around 65 dB SPL for the 55 dB SPL input to around 85 dB SPL for the 75 dB SPL input. This is a 20 dB change in output for a 20 dB change in input!
17. Regarding people fitted to the NAL—maybe more are fitted to the NAL than you think, as they are using trainable hearing aids and have trained to the NAL?
I think that is very unlikely, but a good question and interesting to talk about. If we think about trainable hearing aids, there are really two different approaches (see Mueller, 2014b for review). In one case the user trains the hearing aids by adjusting gain and/or frequency response for different inputs and listening environments. Another type of training is controlled by the audiologist. This is utilized when hearing aids are purposely programmed below a desired level, and then automatic gain increases are introduced over time (e.g., 1 dB/week over six weeks). The notion is that the increase is so gradual that the user will adjust to it. For the first type of training, the user of course needs a method to easily change gain (VC, remote), and needs to do this repeatedly for training to occur. For the second type, you wouldn’t want the patient to have control of the gain, as he or she would simply counter the programmed increase by turning gain down.
Regarding the user-controlled training, we know that if the hearing aids are initially programmed to NAL targets, trained gain, on average, will be close to NAL targets (Palmer 2012; Keidser & Alamudi, 2013). This is even true for experienced users who have used hearing aids not programmed to NAL targets for several years prior to the new fitting (Mueller & Hornsby, 2014). But, we also know that if you start the person below the NAL prescriptive targets (e.g., 6 dB or so), they will not train up to the NAL (Mueller, Weber, & Hornsby, 2008). Recall that all the proprietary fits and manufacturer NAL fits were below the true NAL for 2000 Hz and above for soft and average inputs.
The type of training controlled by the fitter has the potential to end up being a NAL fitting, but only if the initial fit has the same output spectrum as the NAL prescriptive targets, and just needs an overall gain boost. For this to work, however, the output would first have to be verified with probe-mic, which, as we’ve already discussed, is seldom used for verification of prescriptive targets. So I don’t see that either type of training is going to increase the number of people out there walking around with a NAL fitting.
18. I do use the NAL-NL2 fitting most of the time, but it concerns me that sometimes the NAL target is actually below the patient’s threshold? I’ve heard some workshop lecturers say that we should just ignore targets and turn up gain. Do you agree?
No. Didn’t we already cover the issue of clinical hunch versus decades of research? What you are referring to is something that you often will see in downward sloping losses when the loss in the 3000-6000 Hz range is 70-75 HL dB or greater. And this is not just something you see with NAL; you will see the same with the DSL when fitting adults. Figure 5 is a sample patient for whom I’ve entered a downward sloping hearing loss that drops to 80 dB in the highs. Patient characteristics were adult male, experienced user, bilateral fitting.
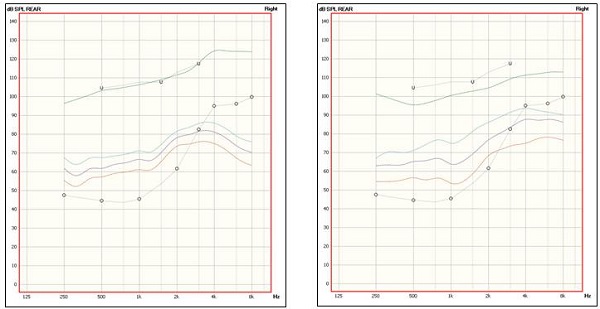
Figure 5. Sample patient with downward sloping hearing loss, reaching 80 dB HL in the high frequencies, programmed for adult male, experienced user, bilateral fitting. Prescriptive targets for soft, average and loud are shown for both the NAL-NL2 (left panel) and DSLv5 (right panel).
What you see on the left panel is the NAL-NL2 targets for soft, average and loud, and the right panel shows the same for the DSL. These LTASS (long term average speech spectrum) output targets are a little greater for the DSL in the high frequencies, but note that for both methods, targets are below the 4000 Hz thresholds. I’m okay with this, and here is why:
- First, the LTASS is just that, the average. You have to consider that the peaks of speech will be 10-12 dB above this, and may be audible. It is helpful to display the amplitude range (e.g., 30th to 99th percentile) of the amplified speech signal to obtain a better estimate of audibility. This is an option on most all probe-mic equipment.
- For losses such as shown in Figure 5, it’s important to consider effective audibility. Will an increase in audibility in these high frequencies really lead to improved speech recognition? There is a point where the payoff for audibility is very minimal (See Ching, Dillon, Katsch, & Byrne, 2001).
- Each patient has a preferred loudness level. Adding loudness at these high frequencies easily could prompt the patient to turn down gain. This would result in less gain for the mid-frequencies, where the contribution of audibility has a greater impact on intelligibility.
- And finally, it just seems rather unlikely that both the NAL and DSL team of researchers would be wrong.
As Harvey Dillon has explained nicely on several occasions (e.g., Dillon, 2006), with each patient we have a gain/loudness budget. If you have already reached your budget, spending another dB at one frequency might mean losing a dB at a different frequency. Choose your frequencies very carefully—spend your loudness where you get the biggest contribution to intelligibility.
19. So if validated prescriptive fittings lead to better outcomes, and it’s easy to verify the output in the real ear with probe-mic measures, why doesn’t everyone do it?
That is the million dollar question. I don't know the answer.
20. Do you see things getting better in the future?
As Neils Bohr, Mark Twain or maybe Yogi Berra said: It’s difficult to make predictions, especially about the future! Given that validated prescriptive methods have been around for about 50 years, and the ability to verify these methods using clinical probe-mic measures has been around for over 30 years, it seems that if this practice was going to catch on, it would have happened by now. But there are a couple of current happenings that could move things in the right direction.
For the past ten years or so, an option has been available that allows probe-mic equipment to link with the manufacturer fitting software and automatically fit the hearing aid to target. You just sit back and watch. There hasn’t been too much research with this approach, but it appears to be fairly valid and reliable. Unfortunately, the approach was limited to only a couple manufacturers and one or two probe-mic systems. This is changing, as more probe-mic systems now have this capability, and the link can be made with more hearing aid manufacturers. It certainly makes it easier to fit to target, and maybe, as a result, it will help to get a few more people on board.
A second factor that could cause change in the fitting culture relates to the fitting practices of Big Box stores. Many (if not most) of these stores use prescriptive fittings, verified with probe-mic measures. Could this encourage private dispensing practices to do the same?
So, back to what would Denis say? About 20 years ago in a 1996 JAAA article, he expressed concern that in the future, a scenario could exist that rather than using validated prescriptive methods, hearing aids would be fitted using manufacturer-specific proprietary formulae for calculating amplification requirements. He stated (p 378):
The scenario described raises concerns, both scientific and philosophical. Scientifically, the concern is that amplification may become prescribed by a wide variety of proprietary formulae of which few, if any, are validated by published research. A possible philosophical problem is that control of the fitting process is taken away from the fitter, who is responsible for the care of the client.
References
Aazh, H., Moore, B.C., & Prasher, D. (2012). The accuracy of matching target insertion gains with open-fit hearing aids. American Journal of Audiology, 21(2),175-80.
Abrams, H.B., Chisolm, T.H., McManus, M., & McArdle, R. (2012). Initial-fit approach versus verified prescription: comparing self-perceived hearing aid benefit. Journal of the American Academy of Audiology, 23(10),768-78.
**Byrne, D. (1982) Theoretical approaches for hearing aid selection. In Studebaker GA, Bess FH. The Vanderbilt hearing-aid report. Upper Darby, PA: Monographs In Contemporary Audiology, 175-179.
Byrne, D. (1996) Hearing aid selection for the 1990s: where to? Journal of the American Academy of Audiology, 7, 377–395.
Byrne, D., & Tonnison, W. (1976). Selecting the gain of hearing aids for persons with sensorineural impairments. Scandanavian Audiology, 5, 51–59.
Byrne, D., & Dillon, H. (1986) The National Acoustic Laboratories’ (NAL) new procedure for selecting the gain and frequency response of a hearing aid. Ear & Hearing, 7, 257–265.
Ching, T.Y., Dillon, H., Katsch, R., Byrne, D. (2001). Maximizing effective audibility in hearing aid fitting. Ear & Hearing, 22(3), 212-24.
Dillon, H. (2006). What’s new from NAL in hearing aid prescription. Hearing Journal, 59(10),10-16.
Dillon, H. (2001, December). The research of Denis Byrne at NAL: Implications for clinicians today. AudiologyOnline. Retrieved from: https://www.audiologyonline.com/
Hawkins, D., & Cook, J. (2003). Hearing aid software predictive gain values: How accurate are they? Hearing Journal, 56(7), 26-34.
Johnson, E. (2012, April) 20Q: Same or different - Comparing the latest NAL and DSL prescriptive targets. AudiologyOnline, Article 769. Retrieved from: https://www.audiologyonline.com/
Keidser, G., & Alamudi, K. (2013). Real-life efficacy and reliability of training a hearing aid. Ear & Hearing, 34(5), 619-629.
Leavitt R., & Flexer, C. (2012). The importance of audibility in successful amplification of hearing loss. Hearing Review, 19(13), 20-23.
Mueller, H.G. (2014a). 20Q: Real-ear probe-microphone measures - 30 years of progress? AudiologyOnline, Article 12410. Retrieved from: https://www.audiologyonline.com
Mueller, H.G. (2014b). Trainable hearing aids - Friend or foe for the clinician? AudiologyOnline, Article 12774. Retrieved from: https://www.audiologyonline.com
Mueller, H.G., & Hornsby, B.W.Y. (2014, July). Trainable hearing aids: the influence of previous use-gain. AudiologyOnline, Article 12764. Retrieved from: https://www.audiologyonline
Mueller, H. G., Hornsby, B., & Weber, J. (2008). Preferred hearing aid gain using trainable hearing aids. Journal of the American Academy of Audiology, 19(10), 758-773.
Mueller, H.G. & Picou, E.M. (2010) Survey examines popularity of real-ear probe-microphone measures. Hearing Journal, 63(5), 27-32.
Palmer, C. (2012, August). Implementing a gain learning feature. AudiologyOnline, Article 11244. Retrieved from: https://www.audiologyonline.com/
Sanders, J., Stoody, T., Weber, J.E., & Mueller, H.G. (2015). Manufacturers’ NAL-NL2 fittings fail real-ear verification. Hearing Review, 21(3), 24-32.
Cite this Content as:
Mueller, H.G. (2015, May). 20Q: Today's use of validated prescriptive methods for fitting hearing aids - what would Denis say? AudiologyOnline, Article 14101. Retrieved from https://www.audiologyonline.com


