 From the Desk of Gus Mueller
From the Desk of Gus Mueller

As some of you know, I live on an island in south-central North Dakota, surrounded by the waters of the Missouri River—not just any island, but the largest island in the state. For the most part, island life is pretty serene and laid back, but a couple hundred years ago, a significant historical event happened just a few miles up the river. In November, 1804, the most famous duo in American history, Meriwether Lewis and William Clark, chose this location for their winter camp, where they stayed for several months. It was during this winter that they drew a new map of our country.
So, what does this all have to do with audiology? Well, it’s important to note that since the famous Lewis and Clark duo, all other noted duos have totally ignored North Dakota. Orville and Wilbur never made it west of Iowa. Thelma and Louise’s road trip was abruptly cut short in Utah, and for unknown reasons, we were even shunned by Hall and Oates! But all that changed a month ago, when Vandy audiologists Todd Ricketts and Ben Hornsby arrived at my home for an extended weekend visit.
Our Vanderbilt connection goes back 25-30 years, so to no one’s surprise, there were many late night (and very late night) discussions, usually centered on something related to hearing aids and hearing aid fitting. While you might think we dug into such things as machine learning, deep neural networks and soundscapes, we usually landed on issues that were much more basic. The one topic that seemed to spark lively comments from all three of us, was the use (or non-use) of speech-in-noise testing related to routine clinical practice and the fitting of hearing aids. We didn’t agree on everything, but what we did agree on was that there is no good reason why speech-in-noise testing is not used more.
Our thoughts of course are not unique, and over the years several articles have been written on the importance of this testing. Is there really any reason to add one more article to that list? We thought so, and that is the topic of our 20Q for this month—which, somehow ended up being a 40Q, as the questions just didn’t seem to stop.
You all already know my weekend visitors. Todd A. Ricketts, Ph.D. is Professor and Vice Chair of Graduate Studies and the Thomas L. and Jane Wilkerson Yount Endowed Chair in Hearing & Speech Sciences, Vanderbilt University Medical Center, in Nashville, TN. Ben Hornsby, PhD, is an Associate Professor, also from the Vanderbilt University Medical Center. Both Dr. Hornsby and Dr. Ricketts are internationally known lecturers and researchers, and have published extensively. Ben and Todd also have been key contributors in maintaining the 20-year #1 ranking of the Vanderbilt audiology training program.
Unlike the famous duo of Lewis and Clark, the Ricketts-Hornsby visit did not result in us drawing a new map of the U.S., but what we did try to do is draw your attention to the many reasons why the use of speech-in-noise testing needs to be expanded in routine clinical practice and the fitting of hearing aids.
Gus Mueller, PhD
Contributing Editor
Browse the complete collection of 20Q with Gus Mueller CEU articles at www.audiologyonline.com/20Q
20Q: Speech-in-Noise Testing - Too Useful to be Ignored!
Learning Outcomes
After reading this article, professionals will be able to:
- Describe recommended presentation levels for earphone QuickSIN testing.
- Recall the administration and scoring of the QuickSIN.
- Interpret QuickSIN findings when used for differential diagnosis.
- Interpret evaluation of QuickSIN scores.
1. Before we get into all of this, let’s get one thing out in the open. Is this entire conversation going to be about you three guys telling me that I’m a bad person for not routinely doing speech-in-noise testing?
Mueller: Not at all. You probably have some very good reasons for not doing the testing. You’re the one asking the questions, so we can go any direction you like. As you might guess, we would like to talk about some reasons why we think that speech-in-noise (SIN) testing should be clinically embraced more than it currently is, and yes, hopefully move you a notch or two in that direction. What is missing in many discussions on this topic, is Monday Morning practical “how-to” information, so we’d be happy to also go that direction if you like.
2. Sounds good to me. I don’t remember much about SIN testing from my AuD program days. Is this whole concept something new?
Mueller: Noted Northwestern University audiologists Ray Carhart and Tom Tillman were recommending it in 1970 (Carhart and Tillman, 1970). In 1980, we were treated to this often-cited quote from the AAA founder Jim Jerger: “We are, at the moment, becalmed in a windless sea of monosyllables. We can sail further only on the fresh winds of imagination.” At the time, he was probably referring to the benefits of the Synthetic Sentence Identification (SSI) test, which used a continuous talker background signal. That was over 40 years ago.
In the last couple of decades, there have been several people and publications encouraging the routine use of SIN testing. One notable person doing work in this area has been audiologist Richard Wilson, who developed the Words-In-Noise (WIN) test. I recall back when I was the Editor of the Page Ten column in The Hearing Journal, he wrote a great article on all the reasons why the clinical use of SIN testing is important (Wilson, 2004). He and VA colleague Rachael McArdle came back four years later with a follow-up article on clinical SIN testing, which they were brave enough to title “Change is in the air.” It might have been in the air, and maybe it’s still in the air, but seems to be moving at a snail’s pace.
3. I agree, but I don’t feel that I’m alone. I would guess that there are surveys that tell us just how many audiologists really are doing SIN testing?

Hornsby: Well, there have been several surveys conducted over the years. For example, From the 1970’s to the late 1990’s Fred Martin did periodic surveys regarding audiology clinical practice, but those data are getting pretty old, and routine SIN testing was relatively rare during that time period. Unfortunately, since the turn of the century survey data focused on clinical practices related to speech testing are pretty limited and the results from those surveys are variable.
The variability isn’t a surprise because how the survey questions are phrased, and who is actually responding to the survey, can vary widely. This could clearly impact any findings. Regardless, I recall that our own Gus Mueller did a survey back in 2010 and asked people how often they do SIN testing? He found that ~10 percent of audiologists do the QuickSIN “most of the time”, and another ~20% said that they do the testing “some of the time” (Mueller, 2010). A response of ~30% of audiologists saying they “routinely” do a SIN test is fairly respectable, but Gus, I believe that you mentioned in the article that these findings probably were inflated?
Mueller: Right you are. This was a paper-and-pencil survey taken by audience members (n=107) who had just listened to me give a talk on the benefits of conducting the QuickSIN! I suspect that influenced their ratings.

Ricketts: I recall there was a survey conducted that included a question on SIN testing about six years ago (Clark et al, 2017). They reported that 29% of audiologists do this testing for >50% of their patients, which isn’t too bad.
Mueller: As you maybe noticed Todd, one problem with that survey was the low response rate, which was 88 of 1220, even after two reminder emails. That’s 7%! Here is my take on this survey, and many other surveys that focus on what is common clinical practice. Most audiologists who are encouraged to reply to these surveys (or are in one of my courses on SIN testing!) are pretty well aware of Best Practice, and what “should be” done clinically from what they see in articles and audiology social media sites. If you sort-of know what the right answer is, but you’re not doing it, it very well could be that you simply don’t complete the survey, or you don’t exactly tell the truth. My guess is that the audiologists who are routinely doing SIN testing (e.g., with >50% of patients) is less than 29%. To support this, I see from that same survey that 63% of the 7% of respondents reported that they are conducting probe-mic verification for >50% of their patients. This is a much higher number than what has been reported in other surveys (e.g. Zitelli et al, 2020, Mueller, 2014), and if you have your ear to the ground, what we know to be true.
4. What about audiologic standards and guidelines? Is SIN testing recommended in these? If not, maybe that’s why it’s not often done.
Mueller: To some extent, this depends on whether we’re talking about doing the testing as part of the routine audiologic exam, or as part of a hearing aid evaluation.
Hornsby: Right. If we start with the basic audiologic evaluation, the guidelines and practices advocated by the AAA and the ASHA don’t really talk much about SIN testing, per se. In fact, the only guideline specific to speech testing as part of a standard audiologic assessment that I am aware of is one for measuring the SRT (ASHA, 1988). Neither the AAA nor the ASHA have published guidelines for measuring suprathreshold speech recognition. So yes, I agree with you, this lack of guidance may play some role in why SIN testing isn’t used more routinely. Although to be fair, despite having a (albeit old) published guideline, my understanding from clinicians is that the ASHA recommended SRT method isn’t used much either.
Rather than talking about specific test materials or test protocols, the AAA and ASHA guidance tends to focus on the broad outcomes expected from the audiologic assessment (e.g., the process should “assess auditory function” or determine “the type and magnitude of hearing loss and the need for treatment including candidacy for amplification”). Both organizations recommend assessing suprathreshold speech understanding as part of the that process, but they don’t provide much guidance in terms of specific test materials or protocols to actually use in that process. What specifics are provided focus almost exclusively on using monosyllabic word recognition in quiet (WRQ). In terms of recommendations for SIN testing, most published documents from the AAA and the ASHA that I’ve seen either don’t mention it at all, or broadly recommend it because it may “…provide information about an individual’s hearing in conditions representative of real-world situations” (ASHA, n.d.). In other words, suggesting it may be better (compared to WRQ) for assessing real-world communication ability.
5. That’s interesting. Do the hearing aid fitting guidelines have much to say regarding SIN testing?
Hornsby: I believe that there may be more practical guidance in these documents when it comes to using SIN testing to assess candidacy and validate fittings. Todd, I’m pretty sure that you’ve been involved in writing some of these guidelines for hearing aid fittings.
Ricketts: I have, but most of these documents really don’t discuss SIN testing very explicitly. I, and I assume other authors when writing these guidelines, always made the assumption that SIN assessment was an obvious part of what we labeled “hearing assessment.” However, I think many readers may have mistakenly believed that this term referred only to threshold testing. Of course, many authors, including those that have developed SIN measures, have pointed out that threshold measures alone are actually a pretty limited way to characterize hearing ability, since individuals with the same hearing thresholds demonstrate such a large range of SIN scores (e.g, Moore et al 2014; Wilson et al, 2007). Since the publication of these guidelines though, greater utility of these measures related to hearing aid decisions has been demonstrated, so I would hope future hearing aid fitting guidelines discuss this more explicitly.
Mueller: Speaking of guidelines that might be a bit dated, there recently has been an independent group, the Audiology Practice Standard Organization (APSO), who have written some “standards” for audiology, which in principle, are different from guidelines and best practice documents. These were published just a couple years ago. John Coverstone from the APSO, describes it as follows (Mueller et al, 2021): https://www.audiologyonline.com/articles/20q-new-hearing-aid-fitting-27938 “APSO is in no way working to create standards...We are simply bringing experts together and using the existing research and accepted clinical practices to document the standards that already exist.”
The APSO standard for the audiologic diagnostic evaluation was just recently released. Regarding SIN testing, it states the following: “Audiologists may perform speech recognition in noise to assess functional capacity.” “May perform” sounds a lot like “may not perform” to me. The APSO hearing aid fitting standard, however, has a much stronger statement: “Pre-fitting testing includes assessment of speech recognition in noise, unless clinically inappropriate.” (for review of APSO hearing aid fitting standard, see Mueller et al, 2021)
6. The standards and guidelines only “sort of” say I should be doing SIN testing, and surveys, limited as they are, show that most of us are not. Convince me why I should start.
Hornsby: Well, I’ll let Todd and Gus talk to you about how SIN testing might be useful in the selection and fitting of hearing aids, but I’d like to start from the perspective of the basic audiologic assessment. To make this an apples-to-apples comparison we should probably first be clear about why it is very common for almost all audiologists to conduct suprathreshold word recognition in quiet (WRQ). I'd put its POTENTIAL utility into two broad categories: 1) Assessing functional speech communication, perhaps identifying someone who should have a formal evaluation for a cochlear implant, and 2) assisting with differential diagnosis (e.g., cochlear damage vs vestibular schwanoma, brainstem or cortical pathology, cochlear synaptopathy, etc).
WRQ can, when obtained under optimal test conditions provide some useful information (see Mueller and Hornsby, 2021 for review https://www.audiologyonline.com/articles/20q-word-recognition-testing-let-26478). But unfortunately, and despite its routine use, the information it can provide is quite limited. In terms of the goals of speech testing as part of the audiologic assessment, WRQ is not highly correlated with real-world communication function, nor is it a highly sensitive or specific measure of retrocochlear pathology, so its utility for differential diagnosis is also limited, although recently, Zapala et al, 2013 suggested that computational models combining WRQ with other audiometric measures may enhance its utility—but we won’t get into that here.
Given the limited information WRQ provides about functional communication and/or towards differential diagnoses, it is reasonable to ask whether SIN testing can provide as much, or more, information. If we start with the goal of assessing functional speech communication ability, a strong case can be made that the “gold standard” of whether someone has a problem or not is self-reported ability (Vermiglio et el., 2018). Clinical measures of WRQ are not good predictors of self-rated hearing difficulties, particularly in noise, in part, because the tests are often conducted at high presentation levels in an attempt to find maximum performance (see Mueller and Hornsby (https://www.audiologyonline.com/articles/20q-word-recognition-testing-let-26478), for review). In contrast, although not perfect by any stretch, analyses suggest that some SIN tests are sensitive to self-reported SIN deficits (Vermiglio et al., 2018).
Finally, we’ve known for some time that SIN measures can be used to identify those most likely to do poorly on a WRQ task but not vice-versa. Here are some data that you might find interesting. They come from a study by Richard Wilson (Wilson, 2011), comparing WRQ vs. SIN test results in over 3000 individuals. Here are some key points of his findings:
- Approximately 70% of the patients had speech recognition performance in quiet (NU-6) that was good or excellent, but only ~7% of these very same patients had SIN scores classified as normal.
- Of the total, only 222 (6%) had normal performance for the speech-in-noise test; 218 (98.5%) of these same patients also had normal performance for the NU#6.
- Of the over 3000 patients who had abnormal performance on the speech-in-noise, 1383 (46.1%) had scores on the NU-6 of 92% or better.
The bottom line from Wilson’s research, and what has been shown in other studies: SIN test results are very good at predicting speech-in-quiet findings, but speech-in-quiet scores are very poor at predicting SIN performance.
Mueller: These findings seem to lead to a very simple solution—if you’re in a busy clinic and only have time to do one of those two tests—traditional monosyllables-in-quiet vs. a SIN test, the logical test to conduct would be the SIN.
Hornsby: That certainly has been suggested over the years. Recently, Matt Fitzgerald and colleagues of Stanford have been collecting data related to this very topic, and some of his findings were recently published (Fitzgerald et al, 2023). His suggestion is that SIN (he used the QuickSIN) measures should be the default test of speech perception in routine audiometric testing, and that word recognition in quiet only be performed when it is likely to be suboptimal.
7. You really think that clinicians are going to stop routinely doing conventional monosyllable word recognition testing?
Mueller: No.
8. Me neither. Tell me how these SIN findings are going to change my treatment plan, hearing aid fittings or patient counseling?
Ricketts: Gus and I have talked about this in a couple of our books, so here is an adapted version of our thoughts, which we maybe can use for talking points later (Mueller et al, 2014; Ricketts et al, 2019):
- For patients with hearing thresholds in the mild or better range, speech-in-noise testing might help quantify hearing problems, and help guide hearing aid fitting decisions. For example, consider a patient who comes in with a complaint of not hearing well, who essentially has normal pure-tone sensitivity. If they also exhibit significant difficulties with SIN recognition, they may be a more successful hearing aid candidate (particularly when also using microphone array technologies), than a patient with excellent SIN test performance.
- The testing can identify ear-asymmetries that might not have been evident in the pure-tone audiometric results, and which can affect hearing aid fitting decisions, and post-fitting counseling.
- The results of the SIN testing can inform decisions regarding hearing aid technology and assistive listening devices, e.g., help identify those who might need additional help from an assistive listening device or those that might need more aggressive implementations of processing aimed at improving the SNR.
- Some types of pre-fitting speech-in-noise results can help identify when there is a frequency region for which amplification provides a detriment instead of a benefit (e.g., “is chasing the highs worth it?”).
- The results of the testing are useful for counseling in multiple ways including, but not limited to, provision of realistic expectations, introduction of listening strategies, adoption of assistive technologies, and demonstration of potential hearing aid and/or hearing aid processing benefits and limitations.
- The testing can be used to measure change over time—both negative, which sometimes is not directly correlated to change in hearing loss, or positive, which on occasion will occur due to acclimatization to hearing aid amplification, changes in technology, or in some cases, rehabilitative services.
Mueller: And I’d like to add, that while this isn’t directly related to your treatment plan, consider that most patients report that understanding speech in background noise is the reason they are considering the use of hearing aids, and this could very likely be the reason that they came to you for help in the first place. In keeping with the current emphasis on patient-centered care, to not do testing to examine the patient’s primary complaint, to me seems illogical and not fair to the patient. If you told an optometrist that you were having problems seeing things clearly that were a distance away, wouldn’t you expect him or her to test that complaint? And by the way, they do. We know that patient-centered care improves trust and increases satisfaction.
9. A lot of things to think about, and I have a lot of questions. But first, how do I even decide what SIN test to use?
Mueller: Where to start? Good question. One thing to consider is if you want to do a test that has a fixed SNR, which is scored in percent correct, or a test that has a variable SNR (either in fixed steps or adaptive presentation based on patient responses) for either the speech or the background noise. The variable SIN test usually is scored for the “50% correct point” which is then reported as either the SNR-50 or the SRT-50—two terms that mean the same.
10. SRT-50? You’re referring to our old standbys of baseball, cowboy, ice cream, etc.?
Mueller: No. But I understand the potential confusion, as when you do the classic SRT-in-quiet measure, you indeed are looking for the level needed to correctly repeat 50% of the test items. The speech recognition threshold (SRT)-50 term, however, has been used for decades in the SIN testing world. It is the SNR where the patient is scoring 50% correct for the speech task, which could be syllables, words or sentences depending on the test. As I mentioned, this also has been referred to as the “SNR-50” (a term you might like better), and with one SIN test, the HINT, the Reception Threshold for Sentences (RTS). The SRT-50 will vary from test to test depending on the speech material, background noise, presentation level, how the test is scored, and probably a few other things. Maybe we can talk about this variance later, as it’s important for patient counseling.
11. What is the best, variable or a fixed SNR?
Ricketts: Again, this is something we’ve summarized before (Mueller et al, 2014, Ricketts et al, 2019), and here are some highlights. There are clinical advantages to both the variable and fixed SNR methods of measuring speech recognition in background noise.
First, some advantages of the variable models:
- Eliminate floor and ceiling effects (i.e., scoring at or near 0% or 100%), a common problem when a fixed SNR is used. The problem with this happening is that we don’t actually know what this result means. For example, if a patient scores 100% at a +12 dB SNR, we don’t know how they would score, for example, at +8 dB SNR. Is their SIN ability so good that they would still score 100%, or would they be down to 40%? That lack of information really limits our understanding of the limits of the patient’s SIN performance.
- The 50% correct point for most patients can be obtained more reliably and efficiently than using a lengthy word list with fixed SNR.
- Because of the strong reliability and efficiency, we can determine significant differences between patients, test sessions, between the right and left ears, or different hearing aids and/or hearing aid settings more quickly, and when smaller differences are present, compared to fixed SNR methods.
- The 50% correct SNR finding can be helpful for patient counseling (patients can be made aware of listening situations where the SNR typically is more adverse than their SRT-50). We find this can be useful for expectations counselling, with the caveat that SRT-50 tests do not always correlate that well to speech-in-noise performance in the real world.
12. That all sounds good. Are there limitations of the SRT-50 approach compared with using a fixed SNR?
Ricketts: There are, here are the primary ones:
- The results may not be as easy to explain to the patient—telling a patient his or her SRT-50 is +10 dB is not very meaningful.
- May be difficult for patients to relate their performance during the test administration to the real world, particularly when using an adaptive procedure. Specifically, since the SNR is continually adjusted to focus in on 50% performance, two individuals with very different SRT-50s would both report that they scored about one-half of the words correct.
- The results may not be as easy to explain to third parties and referral sources. Even seasoned audiologists are not always certain if a SRT-50 score of +4 dB is good or bad, and to make it more confusing, that in turn will depend on the specific test being given (the SRT-50 score that is good for one speech test might just be “okay,” or even “bad” for another).
The choice of variable versus fixed SNR testing, your test levels, and how it all is set up, really specifically comes down to what your goals are for doing SIN testing.
13. Alright, I’ll try to file all that away, and what else should I be considering?
Mueller: A lot. For routine clinical use, here are some criteria that I’d be looking for when adopting a SIN test:
- Good sensitivity and specificity
- Good test-retest reliability
- Good inter-list equivalency
- Established norms for both normal hearing and hard of hearing
- Published critical differences
- Easy to administer and score
- Time efficient
- Readily commercially available
- Auditorily ecological
14. “Auditorily ecological?”
Hornsby: That was going to be my question—not sure where this term came from?
Mueller: Okay, I admit, I might have made up that specific word combination, but I think it fits. Stuart Gatehouse probably was one of the first to write about “auditory ecology” over 20 years ago (Gatehouse et al, 1999). Technically, ecological means “the relation of living organism [like hard of hearing people] to one another and to their physical surroundings;” auditorily, we would then think about what communication settings are important and typical. Regarding SIN testing, this would mean that we might want to use a task that uses meaningful words or sentences, rather than digits or nonsense syllables. And, if using a fixed SNR test, use an SNR that is typical of real-world listening situations. This seems like a no-brainer to me, but it isn’t always the case.
Hornsby: Right, I’ll add my two cents on that topic. Selecting the parameters for a speech test, like the speech materials, the background noise (if any), their levels and SNRs, etc, should be driven first and foremost by what information you want to obtain from the test. Are you interested in differential diagnosis? Assessment of “real world” function? Validation of hearing aid benefit? Something else? Regardless of the type of information you want, for the test to be useful it must have the other characteristics that Gus described a few moments ago (e.g., good reliability and sensitivity). To obtain those characteristics a test developer may sacrifice some degree of “auditory ecology”. That said, all other things (like reliability and sensitivity) being equal, we should strive to use test materials with auditory ecological validity.
Ricketts: Great points, and I think this brings up another factor to consider when thinking about our goals of doing SIN testing. Specifically, one of the reasons it is difficult to approximate “real world” performance on a speech-in-noise test is that the speech presentation level, the SNR, and the individual patient’s hearing loss all can interact to affect audibility even before we introduce other “real world” factors like reverberation, distance, visual cues, etc. For example, if we focus on one real-world environment, let’s say conversational speech levels (e.g., 60 dB SPL), someone with a moderate-to-severe flat hearing loss might do very poorly in quiet and adding a lower-level background noise (e.g., creating a +5 to +10 dB SNR) might have little to no impact. This is because their poor performance in quiet may be driven by the low audibility of speech and the low-level background noise may be largely inaudible.
15. That all makes sense, but a tad complicated. I’m curious though, do we know what SNRs are typical for our patients out in the real world?
Mueller: We mostly do, and I think that Ben has some comments on this. But first, something that relates, and that I’ve found is useful for patient counseling, goes back to the data of the Pearsons et al, 1977 report. One of the many things they looked at was the SPL of the talker’s voice when background noise was present. We’ve all been in conversations where the background noise varied in intensity, and we usually change the intensity of our voice accordingly, in an attempt to maintain a positive SNR for our communication partner. To some extent, this happens without us even thinking about it, a phenomenon known as the Lombard effect. Unfortunately, however, there is not a linear relationship. That is, the increase in the talker’s voice fails to equal the increase in the background noise (roughly only 3-6 dB for every 10 dB increase in the noise). As reported by Persons et al (1977), when the background noise is 55-60 dB SPL, the average SNR is about +5 dB, a level which would be adequate for understanding for most with normal hearing, and maybe even those with a mild-moderate hearing loss. But once the noise reaches 75 dB SPL, the talker’s voice will start falling below the noise level—their data show an average SNR of -1 dB, making communication difficult, even for a person with normal hearing.
Now, on to what Ben has for you on typical SNRs.
Hornsby: You’re right, there have been several studies in the past 5-10 years that have looked at this question using very different methodological approaches (e.g., Smeds et al., 2015; Wu et al., 2018; Weisser & Buchholz, 2019; Benítez-Barrera, et al., 2020). While these results vary in some ways, their primary findings generally replicate the results of Pearsons et al. (1977). People with, and without, hearing loss listen, and try to communicate, in diverse settings where SNRs can range from +30 dB (essentially quiet) to -10 dB (imagine a very noisy restaurant, train or airplane). Despite the wide range of SNRs that we are exposed to, the majority of settings we listen in have relatively positive SNRs. For example, Smeds et al (2015) used acoustic recordings collected by adult hearing aid users during their typical daily routines to estimate the speech and background noise levels, and SNRs, of their acoustic environments. Consistent with the Pearsons data, Smeds et al found that the SNRs people listened in were typically quite positive and were rarely negative. Wu et al (2018) also analyzed recordings of adults with hearing loss made in their everyday environments. Like Smeds et al, they found that negative SNRs were rare (only ~7.5% of SNRs were negative). In fact, ~70% of the environments had SNRs >+5 dB and ~50% were >+9 dB.
16. You almost make it sound like background noise isn’t much of a problem. My patients tend to disagree with you.
Hornsby: We shouldn’t let these data I just reported mislead us into thinking that background noise isn’t a problem just because we aren’t in it all that often. Poorer SNRs indeed are common in some settings, think social settings when we are around lots of people. For example, Smeds et al found that when the setting consisted of multiple talkers (like a restaurant or social gathering) the average SNR was only ~+5 dB. Clearly, most people don’t spend the majority of their day listening in settings where there are multiple simultaneous talkers. However, when we are in those settings, the SNR is often challenging, making understanding difficult.
Mueller: Relative to that last comment, Ben, I think we know that most people with hearing loss tend to avoid noisy places simply because they know that they won’t do well, which of course then influences the “typical” SNR ratings found in research studies. It is not uncommon, however, for those very same patients to have a very noisy situation as #1 on their COSI, simply because that particular situation is very important to them. We also have the patients who still want to frequently hang out in noisy bars and restaurants, or are more or less required to because of work-related events. And we know, many of these places are very noisy—it might be tough to find a +5 dB SNR unless your friends talk really loudly. For example, I recall a study that assessed noise levels in 30 restaurants in Orlando, FL, during a busy time of the day, usually the evening dinner hour (Rusnock and Bush, 2014). More than ½ of the restaurants had average noise levels over 75 dBA, and 5 (16%) had significant portions of their noise level above 80 dBA, with maximum SPLs over 85 dBA. Only 7 (23%) had significant portions of their SPL range below 70 dBA. All 7 of the latter group were counter-service only—not my kind of destination for a nice social dinner with friends.
I guess my point here, is that it’s pretty important to know how these patients are doing in background noise, even if they typically live in a quiet world.
17. All good to know. Let’s go back to that long list you gave me of all the things that make up a good SIN test. That’s a lot to think about. Maybe you all could give me a couple of your “Five-Star choices?” How about starting with the fixed SNR tests?
Ricketts: Hmm. Five Star? That might be tough in this category. I can tell you, however, what is a “Zero-Star.” That would be taking your monosyllabic NU-6 list, randomly adding some background noise, and delivering it live voice. Yes, that has been done.
I’ve used several different fixed SNR tests in research projects, but picking one or two good ones for routine clinical use is a little more difficult. The problem is that many of these tests just take too long, and/or they suffer from the floor and ceiling problems we just talked about. However, there are a couple of fixed SNR tests that can be useful clinically for a few specific populations.
One well researched example is the AzBio (Spahr, et al, 2012). While originally developed for evaluating patients with cochlear implants, the AzBio is increasingly used with other patients, particularly those that have considerable difficulty recognizing speech-in-noise, but for whom there is interest in test materials that are more difficult than speech in quiet (e.g., patients with moderately-severe or greater hearing loss using hearing aids or hearing aids in combination with cochlear implants, referred to as bimodal or hybrid depending on the configuration). In addition to strong psychometric properties, the AzBio has a large number of equivalent lists, includes male and female talkers, uses sentences with more current content and language in comparison to tests developed decades ago, and even has versions appropriate for kids (Pediatric AzBio and BabyBio; Holder et al, 2016)!
A much more niche example of a fixed-SNR test is the Connected Speech Test (CST; Cox et al, 1987). It consists of 24 equivalent pairs of passages with 9 or 10 sentences about a familiar topic, spoken by a female talker. The CST was designed to be used primarily for a criterion measure for research studies of hearing aid benefit, and indeed has been used extensively for this purpose. The clinician scores the patient’s response based on 25 key words in each passage spoken in a multi-talker babble background noise. In addition to very strong psychometric properties in general, normative data for audio-only and audiovisual presentation modalities have been published (Sherbecoe and Studebaker, 2003). Despite a fairly long test time, this makes this test a potentially valuable tool clinically, for example, when we want to know how much a hearing aid might improve speech recognition for an individual with profound hearing loss when there are both audio and visual cues. There is no “standard” SNR for presenting this test, but for clinical purposes I’d recommend somewhere in the +7 to +12 dB SNR range depending on just how much the patient struggles in noise and whether you are using the audio-only or audiovisual version.
18. What are your picks for a variable SNR test?
Ricketts: For routine clinical use, it seems reasonable to go with what I understand already is the most popular in clinics today—the QuickSIN or its similar cousin, the BKB-SIN (Killion et al, 2001). Both essentially meet most all of the important clinical criteria that Gus listed earlier. In addition, in their standard form both are designed to measure the influence of noise on speech recognition, while limiting the influence of audibility. However, they are also flexible enough to include other configurations that can be used for assessing other goals.
QuickSIN and BKB-SIN: The QuickSIN has 12 primary lists intended for clinical use, however, since its development, research has shown that only seven of these 12 lists have been found to be equivalent for both normal hearing and hard of hearing patients. There also are three pairs of lists on the original CD intended for research use.
Each list has six sentences, with five key words that are scored (i.e., 30 key words/list). The background noise is a four-talker babble, and is adaptively increased in six 5 dB steps, going from an SNR of +25 dB to 0 dB. One thing that makes this test “clinician friendly” is that in the standard version, the six different SNRs are packaged together (speech and noise) and presented in turn without clinician adjustment—more convenient than some SNR tests, where the clinician has to manipulate the intensity of the speech, and/or the background noise signal. In addition to the standard materials, what you’ll find on the original CD, are versions which separate the speech and noise and allow for clinician control of SNR, allowing for a wide range of testing goals (e.g., evaluating the effectiveness of microphone array technologies if you have the correct loudspeaker arrangement).
The BKB-SIN has this same range of flexibility but has the advantage of slightly smaller critical differences through the use of list pairs instead of single lists, while also being a much easier test because of the use of a male talker and more simple language. These changes also allow for the use of the BKB-SIN test with children and normative data are available for those as young as five years old (Etymotic Research, 2005).
While the BKB-SIN has the advantage of pediatric utility, the QuickSIN also has a unique feature not found in other widely-available clinical speech-in-noise tests. Specifically, there are versions which provide and manipulate high-frequency gain. The High Frequency Emphasis (HFE) lists provide a relative increase in level above 1 kHz which peaks at a 30 dB gain increase at 3 kHz and above. This version is coupled with a HFE with low pass (HFE-LP) version that takes the HFE version and steeply rolls off the level above 2 kHz. Used together, and compared, these two versions can provide a very rough indication of whether individuals with steeply sloping hearing losses in the high frequencies may actually perform more poorly if high frequency audibility is provided. Since high demands for high frequency gain can affect issues related to receiver size and feedback, identification of the somewhat rare individual for which high frequency audibility has a negative effect, can provide important clinical information when we are “chasing the highs”.
WIN: Another good test is the Words-In-Noise (WIN; Wilson and Burks, 2005). The WIN is similar in general construction to the standard QuickSIN and BKB-SIN in that the speech and noise is presented at high level and the SNR (multi-talker babble noise) is decreased in a stepwise fashion (e.g., in 4 dB steps from +24 dB to 0 dB). In the case of the WIN, the speech and noise signals are mixed together into a single track, so separating the speech and noise for presentation from separate loudspeakers is not possible. In addition, the noise level is fixed at a high presentation level and the level of the speech is varied (e.g., from 80 to 104 dB SPL). Consequently, the intended use of the WIN related to hearing aids, is primarily as a pre-fitting measure. The most obvious difference between the WIN and the QuickSIN is that words (NU#6) are used as the test stimuli instead of sentences. Using the WIN, five words are presented at each of the 7 SNRs.
HINT: It only seems reasonable, that if we are talking about hearing-in-noise tests, we should mention the HINT . . . which, by the way, stands for . . .Hearing In Noise Test (Nilsson et al, 1994; Vermiglio, 2008). The HINT uses an adaptive SNR procedure, but in the standard version, the noise level is fixed at 65 dBA and the speech levels are adaptively varied based on the patient response. The adult version of the HINT is available in 22 languages and there is a pediatric version (HINT-C) available in five languages. Most recently in the US, the use of the HINT has been focused on assessment of job critical hearing skills (e.g., law enforcement), and it is not commonly available, or used in typical clinical settings. That said, because it is available in so many different languages, it might be a more common SIN test in other countries.
Matrix Test: And finally, another test that we should mention is the Matrix Test, which has evolved from the German Oldenberg Sentence Test, commonly referred to as OLSA (Wagener et al, 1999). One way the Matrix test differs from the previous tests we have talked about is that there is a very high level of flexibility in how it can be constructed, scored and administered, that we don’t have with other SIN tests. Gus, I know you’ve done work using this test in some research projects, right?
Mueller: I have, and you’re right, there are a lot of options in the test software. One big advantage of this test is that it is available in 16 different languages for clinical use. Specifically for the U.S., we typically would use the American English Matrix Test (AEMT). Even though the AEMT has been out for several years, I don’t really see that it is being used much clinically (in the U.S.). One reason for this simply might be availability, as I don’t think that it is commonly loaded on most audiometers, but maybe could be.
One thing about the AEMT, however, that maybe shouldn’t bother me, but it does, is that performance for normal hearing individuals is a negative SNR—the mean for the AEMT is an SNR of -8.6 dB (other languages have similar means), and if we use two standard deviations for defining “normal,” the range then is SNRs of -6.8 dB to -10.4 dB. It seems strange to think of a patient with an SRT-50 of -6 dB as being “abnormal.” If we look at normative data from the WIN and the QuickSIN, we’re seeing SRT-50 cut-off scores of around +5-6 dB or better to define normal performance, which makes more sense to me regarding real-world listening, and is more useful for patient counseling.
Hornsby: Hmm, the differences in the absolute SNR that leads to 50% correct for normal hearing listeners doesn’t bother me the same way. I’d go back to which test provides me with the best information. But I do see your point, Gus, and if multiple tests can give me similar information, then definitely, having a test where the outcomes are more relatable to everyday conditions might be useful for counseling purposes. In fact, a few years back Rich Wilson and colleagues (Wilson et al, 2007) compared four different commonly used SNR-50 speech tests, by giving all four tests to the same group of individuals with hearing loss. The mean SNR-50 results were quite different:
- BKB-SIN SRT-50 = 5.0 dB
- HINT SRT-50 = 8.9 dB
- QuickSIN SRT-50 = 12.3 dB
- WIN SRT-50 = 14.0 dB
Mueller: Thanks for adding this. These data clearly point what we’ve been alluding to. The clinic-to-real world applications often are a little messy. Imagine a patient who is the “engineer type” (you all know what I mean) and he tells you that he wants to do well in his favorite restaurant, where the SNR is + 8 dB (yes, he brought in the measurements). Your counseling easily could be influenced by what clinical SIN test you choose to use.
19. Thanks for all the options. For now, I think I’m going to go with the QuickSIN, as that is what a couple of my audiology friends use, and I’m pretty sure it already is loaded on my audiometer. What do I need to know?
Mueller: As Todd mentioned, the QuickSIN seems to be the choice of most clinicians today, partially because it’s available with most audiometers, and in some cases, is the only SIN test that is pre-loaded on the equipment. Here are a few key things to consider:
- Importantly, the test is scored in SNR-Loss, not SRT-50 (SNR-50) like most all other adaptive SIN tests. Early QuickSIN research showed that individuals with normal hearing had an average SRT-50 ~+2 dB, and for this reason, SNR-Loss is computed by subtracting the patient’s number of words correct (out of 30) from 25.5, rather than 27.5, to derive the SNR-Loss score. A sample score sheet is in Figure 1. If the math looks too overwhelming, never fear, your audiometer will score it for you. You just need to click on what words the patient misses for each sentence.
- We recommend always doing at least two lists (60 key words), and then taking an average of the scores. As Todd already mentioned, it is important that you only use the lists that are equivalent in terms of difficulty. It could be that all 12 of the lists have been stored on your audiometer. The research of McArdle and Wilson (2006) found that only 7 of the 12 original lists provided homogenous results for both listeners with and without hearing loss: 1, 2, 6, 8, 10, 11, and 12.
- Once you have an average score for each ear, you can determine a general categorization of the patient’s SIN ability from the table found in the QuickSIN manual (See Table 1), or other data you might have from published studies.
- For the earphone testing, you will want ear-specific information—two lists/ear. For the aided testing, it’s preferred to again test each ear independently, but you could get by with bilateral measures.
- You also need to be aware of the critical differences—when is a difference really a difference?
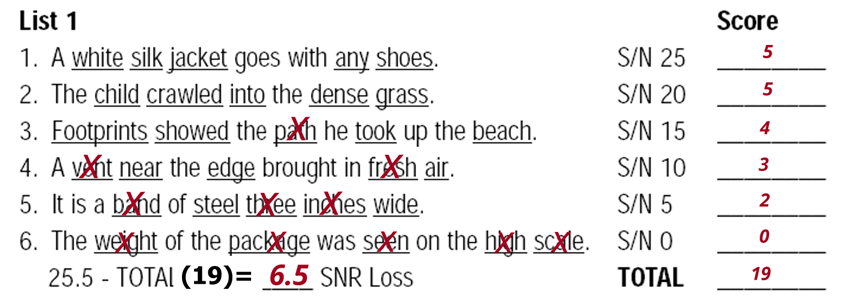
Figure 1. Sample scoring for a single list of the QuickSIN. The total number of correct key words for the six sentences (19 in this example) is subtracted from 25.5 to obtain the SNR-Loss.
| SNR-Loss 0-3 dB | Normal/Near Normal |
| SNR-Loss 3-7 dB | Mild SIN Disability |
| SNR-Loss 7-15 dB | Moderate SIN Disability |
| SNR-Loss >15 dB | Severe SIN Disability |
Table 1. Guidelines for interpreting QuickSIN test results.
20. I’m not really following the critical difference thing. How exactly would I use that?
Mueller: The same way that you use the Thornton and Raffin critical difference chart when you do monosyllabic word recognition testing (see Mueller and Hornsby, 2021 for review https://www.audiologyonline.com/articles/20q-word-recognition-testing-let-26478). Table 2 has the critical difference values for both a 95% and an 80% confidence level—the 95% values are most commonly used—note that as expected, the more lists you use, the smaller the critical difference will be.
Let’s say you just finished doing earphone testing using two lists/ear, and the patient had an average SNR-Loss of 8 dB in the right ear, and 10 dB in the left ear. Is the left ear worse than the right? No, because the difference is smaller than the critical difference of 2.7 (see 95% value on chart for 2 lists). What if you did unaided and aided testing soundfield using two lists/condition and the patient scored 8 SNR-Loss unaided, and 4 dB SNR loss aided. Was their aided performance better? Yes, because 4 dB (the difference) is larger than the critical difference of 2.7 dB.
| Number of Lists | 1 | 2 | 3 | 4 |
| 95% C.D. | 3.9 | 2.7 | 2.2 | 1.9 |
| 80% C.D. | 3.2 | 2.2 | 1.8 | 1.6 |
Table 2. Critical differences for comparison between two QuickSIN test conditions at a 95% and 80% confidence level relative to number of lists for each condition.
21. You haven’t talked much about presentation level? I saw a recent poll on this topic at an audiology Facebook page, and the results were that most clinicians use the patient’s MCL for the QuickSIN. Do you agree?
Mueller: Not in the slightest. Here are three reasons why the patient’s MCL is a poor choice:
- For earphone testing, we want to ensure optimum audibility. Most of our patients have downward sloping hearing losses, many with normal or near-normal hearing in the lows. Their MCL often is well-below the level we need to optimize audibility for the high frequencies.
- For aided testing, we need to use a level that has at least some real-world validity (e.g., the known average SPL values of soft speech and/or average speech). It seems unlikely that the patient’s communication partners will somehow know to speak at his or her MCL.
- MCLs are a range, not a specific level. Hence, when follow-up testing is conducted, whether it’s earphone or aided soundfield, it’s important to use the same presentation level as previously had been used—the MCL often varies from session to session.
22. Okay, don’t ask me why I pay attention to internet polls. So what level do I use?
Mueller: This really depends on why you are doing test, what Ben and Todd described as testing goals. There are at least three levels which may be appropriate, which we briefly discussed earlier.
- Reason #1: To determine the patient’s SIN performance while limiting the role of audibility. Think of this as somewhat like a SIN-Max, as in PB-Max. This test is conducted under earphones at a high presentation level. The QuickSIN manual states that when the PTA is 45 dB or less, conduct the testing at 70 dB HL (83 dB SPL), and when the PTA is >45 dB, conduct testing at the patient’s Loud, But Okay level (just below their LDL). Importantly, this is the “standard” version of the QuickSIN and this methodology was used for collection of the normative data and in many studies comparing different SIN tests. These are the presentation levels you would want to use if your goal is to compare your patient’s score to normative data. This same set-up can be used to look at differences between the ears.
- Reason #2: To determine if “chasing the highs” is detrimental for a patient with a steeply loping audiogram. Again, this test is conducted under earphones at a high presentation level. However, the results of the HFE and HFE-LP list are compared.
Ricketts: Hey Gus, before you get to your next reason, let me jump in here for a moment. You’re taking about presentation levels, and sometimes visualizing things helps, so I just went to my lab and conducted some real ear aided response (REAR) measures for the QuickSIN lists presented at 53, 63 and 83 dB SPL, which would correspond to 40, 50 and 70 dB HL. This is for a patient with a typical high-frequency loss going from 20 dB HL in the low frequencies, to 70 dB HL in the highs. Shown on the screen (See Figure 3) is the LTASS for the different levels—the peaks (not shown) will be ~12-15 dB higher. What is clearly shown, is that if the reason for the SIN testing is to estimate the patient’s “best ability,” we need a relatively high presentation level to ensure that speech in the high frequencies is audible. This goes back to your point Gus, regarding the limitation of using the patient’s MCL, which often does not optimize audibility. Notice that for 50 dB HL, even if we consider the peaks of speech, there would be little or no audibility above 1500 Hz.
I also did a second real-ear measure for a patient with the same hearing loss, which relates to the second reason for conducting QuickSIN testing—the presentation of the HFE lists. Shown are the earcanal outputs for the standard QuickSIN lists and the HFE lists using a presentation level of 83 dB SPL for both (See Figure 3).
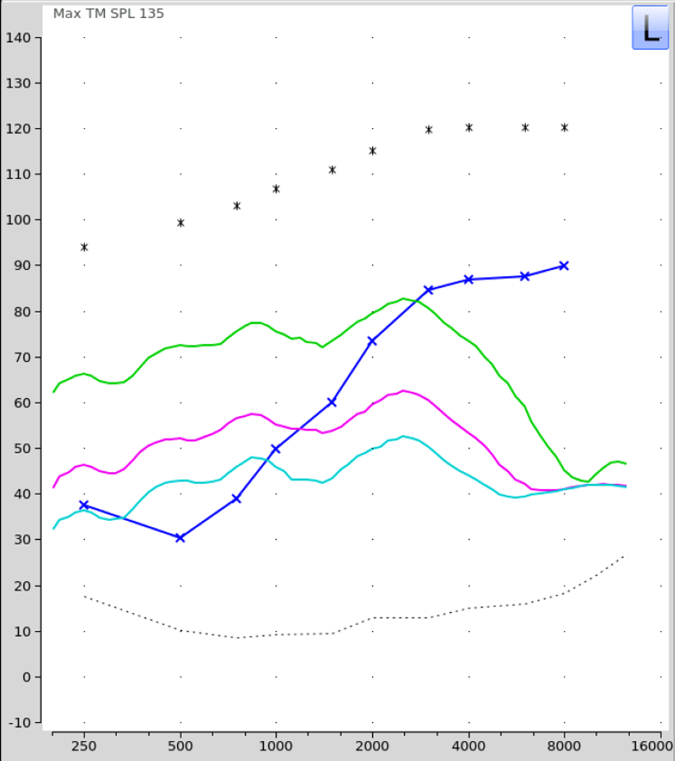
Figure 2. Average REAR levels for the Quick-SIN standard lists presented at 53, 63, and 83 dB SPL (40, 50 and 70 dB HL). Relative audibility for the average levels (speech peaks will be ~15 dB higher) is shown for a patient with thresholds sloping from 20 dB HL in the lowest frequencies to 70 dB HL in the high frequencies (blue tracing).
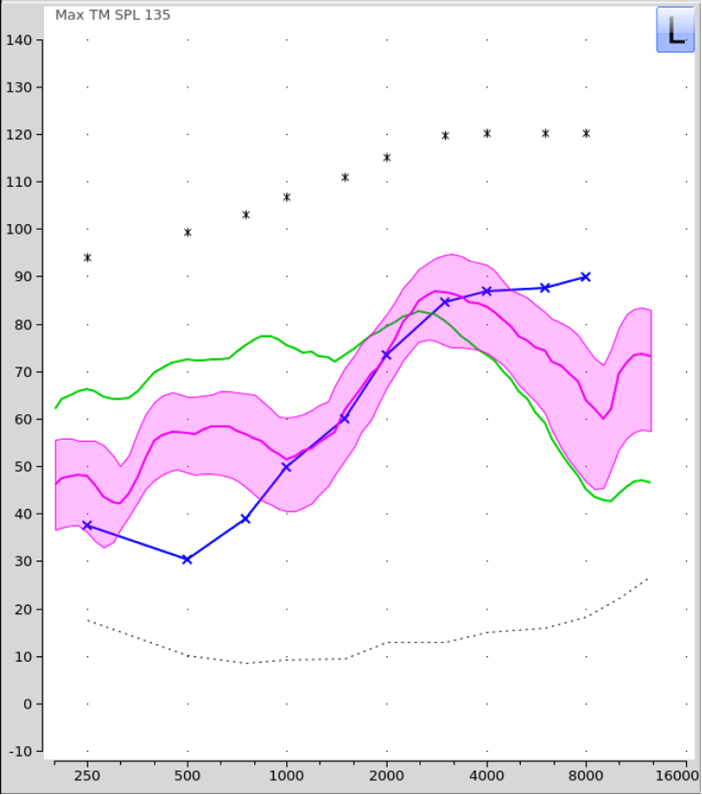
Figure 3. Average REAR levels for the QuickSIN standard lists (green LTASS) versus the HFE lists presented at 83 dB SPL (70 dB HL; see pink shaded region). Audibility for the HFE list is shown for a patient with thresholds sloping from 20 dB HL in the lowest frequencies to 70 dB HL in the high frequencies (blue tracing).
Mueller: Thanks Todd. Jumping in is fine when you have data that useful! Audibility is an amazing thing. I did, however, have one more reason for doing QuickSIN testing:
- Reason #3: To demonstrate to the patient that “hearing aids work.” This is conducted both unaided and aided at a level slightly below average speech—causal speech is considered to be 53-55 dB SPL (~40 dB HL). The test is delivered from a single loudspeaker in front of the patient so we‘re mainly showing hearing aid benefits related to improved audibility.
You know, now that I’m thinking about soundfield speech testing, there is something that I’d like to ask my two colleagues:
We’re often talking about “average speech levels.” It seems that in many research studies, 65 dB SPL is used. Clinically, most think of 50 dB HL as “average.” If I wanted to do soundfield testing at “average levels,” the correct SPL would be ?
Ricketts: There have been several studies that have looked at “average” levels for conversational speech. Most try to focus on the level produced at one meter with an “average” vocal effort. One place that investigators tried to put this all together is the Speech Intelligibility Index (SII) standard (ANSI S3.5 1997). After reviewing many studies this standard settled on 62 dB SPL as the level for average vocal effort (and 82 dB SPL for “shouted” speech).
Hornsby: I agree with Todd that if you look across studies (like the ANSI group did) a reasonable level seems to be about 62-63 dB SPL. 65 dB SPL is pretty close to that, but I’ve not found a clear path of citations explaining where that number comes from. In reality, determining “average” conversational speech levels is not as simple as you might think. Lots of factors can impact the level of our speech. For example, the background noise we are talking in, the distance between the talker and listener, even whether we know we are being recorded! Let’s use the male and female speech levels from the Pearsons data you mentioned. Those were the measured levels for male and female talkers who were in an anechoic chamber and had been instructed to say: "Joe took fathers shoe bench out; She was waiting by my lawn" over and over until told to stop. They were instructed to repeat the sentences in a "normal" voice, or a "raised" voice, or "As loudly as possible" or in a "shouted" voice. To me this doesn’t sound a lot like an “average conversation”.
One sneaky thing the researchers did was actually record the participants as they were chatting with the researchers in the anechoic chamber while waiting for the “study” to start (i.e., prior to them actually saying anything about “Joe”). In the paper, the Pearsons’ group calls these levels "casual" and the means were actually 5-6 dB lower (i.e., 50 and 52 dB for females and males, respectively) than the “normal” speech levels. To me it would seem this "casual" speech level would be more "normal" than what Pearsons actually calls "normal". In other words, if we take people into an anechoic chamber and tell them to “talk normally” they may actually raise their voices!
Mueller: Whew! I was sort of looking for an answer from you two guys that was only one or two sentences. I should have known better!
Hornsby: You should have, and so you shouldn’t be surprised that I’m not finished! The last point I think is important for clinicians to be aware of is your comment of how we often think a dial value of 50 dB HL corresponds to a speech level of around 62-65 dB SPL. However, we know that speech is a complex signal, its level varies over time, across speakers, and between speech materials. So while this may happen in some instances, it may not always be the case. However, and importantly, the 13 dB HL to SPL difference is how the QuickSIN was originally calibrated at the time when the 70 dB HL presentation level was recommended.
23. How about we get back to my questions! I understand the “SIN-Max” thing, but during earphone pre-fitting testing, don’t we also want to know how the person is doing for conversational speech?
Mueller: I’m not sure how it would change your treatment plan. But sure, if you have the time, you could do earphone testing at ~45-50 dB HL. Your results of course, will most always be significantly poorer than those obtained at the high presentation level, simply due to the reduced audibility of the important high frequencies (what Todd just showed in Figure 2). I don’t really find the results of this testing too useful—I guess it might give some sort of validation of the patient’s complaints, and would give you (and the patient) an indication of what improvement is possible with an appropriate hearing aid fitting (i.e., the difference between the SIN scores for the two levels).
24. Earlier you mentioned SIN testing for people with normal hearing that have the complaint of understanding in background noise. I’ve had some of those patients. Do we know what is causing this problem?
Mueller: There are probably several causes, all leading to the same general complaint. One of these is believed to be cochlear synaptopathy; Sharon Kujawa did a nice review of this in a 20Q back in 2017 (https://www.audiologyonline.com/articles/20q-cochlear-synaptopathy-interrupting-communication-20946). This refers to cochlear synapses that can be lost from noise exposure and aging, or their function can be altered or disabled due to genetic mutation. These fibers are important in coding responses to transient signals in the presence of background noise, and therefore, the synaptopathy could contribute to speech-in-noise difficulties, even before thresholds are elevated (Kujawa, 2017). Some have referred to this as “hidden hearing loss,” although in some cases, it might only be hidden because most audiologists do not do SIN testing.
Hornsby: I agree, there are probably several things that could lead to someone with “normal” hearing having complaints of difficulty understanding speech, especially in noise. Gaby Saunders was interested in these kinds of patients back in the late 1980s (Saunders & Haggard, 1989) and used the term “Obscure Auditory Dysfunction (OAD)” to describe them (“King-Kopetzky syndrome” has also been used to describe individuals with such complaints; Zhao & Stephens, 1990). Research from that time confirmed that some people with these types of subjective complaints (not all) also do poorly on SIN tests. Regardless, researchers have suggested that their complaints, and relatively poor performance when present, could be due to a variety of factors, such as mild cochlear (or middle ear) dysfunction, psychological disorders, auditory processing deficits, or combinations of factors (Zhao & Stephens, 2007).
25. Your last comment prompts me to ask—is the QuickSIN a test of APD?
Mueller: That wasn’t the design of test, and I don’t really see it being used for that purpose. That’s not to say, that someone with APD might score poorly on the QuickSIN. Unlike some other SIN tests using speech noise or multi-taker babble, the 4-talker babble of the QuickSIN has considerable informational masking. It’s not uncommon at the difficult SNRs for a patient to become confused and start repeating back words from the babble, not the primary talker. And in fact, a recent study from the University of Pittsburgh (Cancel et al, 2023) reported on 47 patients with normal or near-normal hearing who underwent assessment for APD because of complaints of hearing loss and/or problems understanding speech in background noise. The authors report that the QuickSIN had a sensitivity (hit rate) of 77%, and a specificity rating of 78% (i.e., false alarm rate of 22%) for this group of patients. But again, I’d stick with tests that have been specifically designed for APD assessment.
26. Is there also an audiologic differential diagnostic utility for using the QuickSIN?
Mueller: If you’re referring to identification of retro-cochlear pathology, such as space-occupying lesions, QuickSIN findings probably don’t have the sensitivity or specificity to be used for that purpose. But, with that said, what you might find interesting, is a recent publication from the researchers we mentioned earlier from Stanford University. They reported some intriguing data related to your question, for 73 individuals with confirmed vestibular schwannomas (Qian et al, 2023). Receiver operating characteristic curve analysis showed that the asymmetry observed for the QuickSIN was more sensitive and specific for detecting vestibular schwannomas than the pure-tone average asymmetry or the word-recognition-in-quiet asymmetry. So, while not great, QuickSIN findings could be better than what audiometrically is typically used in some clinics.
27. I know the QuickSIN is quick, but I just don’t know that I’ll have time to do it on all my adult patients with hearing loss. Do you have some triage suggestions?
Mueller: Here is one thought, based on no evidence, but I’ll toss it out anyway. I hate to suggest short cuts—but, you could do one list bilaterally under earphones (at the high presentation level). This will only use one minute of your time. Think of it as a SIN screening. According to the QuickSIN manual, the score obtained from a single list is accurate to about 2.2 dB. So you would know that if the measured SNR-Loss was only 1-2 dB or better, at least one ear was probably at or near normal (e.g., SNR-Loss of ~3-4 dB or less). Typically, the bilateral score will be at least as good as the best ear. Of course, the full-blown QuickSIN is only going to take 4-5 minutes for two ears, so does this really help that much?
Ricketts: I agree with simply doing the full procedure. As we’ve discussed, more than one research group has suggested SIN testing is a better tool for routine clinical use than the WRS in quiet. Given all the potential utility, minimally testing unaided SIN at a high level seems to routinely provide too much useful information to ignore.
28. Okay, let’s move on to the fitting of hearing aids, which is when I’ll probably be using this test the most. I see how pre-fitting testing might improve my treatment plan, but earlier you suggested that I also could do SIN testing following the fitting itself?
Mueller: Yes, we mentioned a couple ways you could use these measures. One was that you could do soundfield SIN testing as a demonstration procedure. That is, conduct aided testing at a speech level near average—this means you’ll need to know the SPL in your test room for a given HL value. This testing is something that you’ll do after you already have the hearing aids programmed to a validated prescriptive fitting, verified with probe-mic measures—importantly, this aided SIN testing is really just a demonstration, as it is not highly correlated with benefit in the real world, and it is definitely NOT a substitute for real-ear verification. However, if aided performance falls below your previously measured unaided results obtained under headphones at a high presentation level, you might question why. Are you sure you have the aids programmed correctly?
29. I assume that if I use something like the manufacturer’s first fit, and don’t fit to prescriptive targets, the aided QuickSIN scores might be unacceptably low?
Mueller: You assumed correctly—more so than you might think. Ron Leavitt and Carol Flexer (2012) did a study looking at this very thing. Using the QuickSIN presented at 57 dB SPL, they tested a group of experienced hearing aid users, fitted bilaterally with the premier hearing aids of the Big Six, programmed both to the manufacturer’s first fit, and to the NAL algorithm. Averaged across all participants for the six instruments, SNR-Loss improved by ~6 dB when the hearing aids were programmed correctly. Most notably, for two of the products, the average improvement was ~10 dB! While unfortunately, this study had few participants, it is consistent with the findings of other studies showing significantly better outcomes for NAL-based fittings than for manufacturer first fits (e.g., Valente et al, 2018).
30. Well, hopefully not many are using proprietary fittings. So then, I have to ask, should I expect that my aided results, conducted at an average speech level, would be as good or better than my pre-fitting earphone unaided findings?
Mueller: Well, remember when we first sat down for this little chat, and in my introduction, I was telling you about our late-night discussions of a month ago regarding SIN testing? I think I said that the three of us agreed on most everything? Well, you just hit an area where our opinions might somewhat differ.
My thoughts go like this. When we do the earphone testing at a high presentation level, the SIN score for the patient should be “about as good as it gets.” When we are sending the patient out the door with a pair of new hearing aids, it seems reasonable that the fitting goal would be to provide aided SIN performance that will be “about as good as it gets.” How do we know if we’ve met that goal? To me, we could think of the aided QuickSIN score (using average-level speech) as a form of validation of the gain and output programming—are the aided SIN findings equal to or better than the earphone scores? Now, of course, even if we obtain good aided results, this doesn’t mean that the patient will be delighted with his real-world SIN performance. Expectations, listening situations, and many other factors will be in play. But, we at least know, that from a device standpoint, we gave it our best shot for him to be delighted.
Ricketts: I’m not 100% in disagreement, but I think we have to be a little careful for two reasons. First, if we actually measured an “SNR-Max”, this probably wouldn’t be our target. We know from many studies focused on the development of prescriptive gain targets that in general as we increase audibility for speech signals average performance improves, but only up to a point. At higher levels the loudness of speech becomes unpleasant (or uncomfortable) and people won’t wear this prescription, even if it improves their speech understanding (and in some cases it does not!). Instead, NAL-NL2 (for example), balances useable audibility with comfort and prescribes gain that results in less than maximum audibility. Secondly, we are not actually measuring “SNR-Max” for most people when we do SIN testing, in part because the speech signal isn’t shaped to the hearing loss. While we are limiting the influence of audibility by using a high presentation level, its influence is not eliminated. For example, high frequency audibility will be increasingly limited for people as hearing loss increases beyond 65-70 dB HL.
Despite these arguments, I think having a comparable unaided QuickSIN for high levels to aided QuickSIN for conversational levels is pretty good rule-of-thumb. We just may need to be careful when the results don’t line up, but we probably can explain the differences due to audibility factors (e.g., an individual with a mild high-frequency hearing loss might have better audibility for the unaided condition than the aided condition).
31. You mentioned earlier that it’s important that I know the soundfield SPL relative to my HL dial settings. How do you recommend I measure that?
Ricketts: If your SIN test is built into your audiometer, that information should be available, but it is not always clear. In addition, since you probably have your audiometer professionally calibrated, you might not have a sound level meter (SLM) available. That said, you can pick up a cheap SLM online for $20-$50 that will typically be accurate to within a dB or two. Of course, there are also many SLM apps for smartphones available as well. While many can be calibrated against a SLM if you can borrow one for a few minutes, a few are accurate within a couple of dB, if they are using known smartphone hardware. For example, the National Institute for Occupational Safety and Health (NIOSH) has a free app designed to work with Apple devices that works as a Type II SLM (accurate to +/- 2 dB), see - https://www.cdc.gov/niosh/topics/noise/app.html. When using the QuickSIN, first, zero the VU meter using the calibration tone track. Then, set your dial to 70 dB HL, play one channel of the calibration noise track out of your speaker and note the HL dial to dBA level reported by the app. For example, if the dial reads 70 HL and the app reads 83 dBA with the smartphone in the position of the patient, you know that the dial-to-SPL difference is about +13 dB. This correction value will apply to all dial settings. If you want to do the “casual-level” soundfield testing that we talked about earlier, and you wanted to use a presentation level of 55 dB SPL, then you would set your audiometer to 42 dB HL (55 dB minus 13 dB).
32. Good. So I’ll make sure I use the right correction values. What next?
Ricketts: As we just discussed, the SPL presentation level that you choose to use in the sound field might be anywhere from 50 to 70 dB SPL or so, depending on your goal. Bilateral testing will give you a good demonstration, but if the outcome is unexpected, you could test each ear individually.
33. You’ve now mentioned a couple times that I could simply do aided bilateral testing. Is it safe to assume that the bilateral score will be as good or better than the best ear?
Mueller: In most cases, yes. With the QuickSIN, when audibility is not an issue, it is not common to see an individual ear score significantly better than the bilateral score (e.g., McArdle et al, 2012)—recall the “critical differences” we discussed earlier; a 2.7 dB or smaller dB difference (if you’re using two lists) is not really a difference. The unilateral-better-than-bilateral finding, sometimes called “binaural interference,” is most commonly observed for individuals with APD, using speech tests sensitive to this disorder.
34. I’m still a little concerned that my patients won’t really understand “SNR-Loss.” Is there a way to simply convert the SNR-Loss score to percent correct for patient counseling?
Mueller: There is, but I think it would only make it more confusing to the patient. Consider this example: After you averaged the SNR-Loss for the two different lists, your patient had an average SNR-Loss of 2 dB for both ears, which is considered “normal” (see Table 1). This means that he correctly identified 47 of the 60 key words (two lists; 30 key words/list). This is a percent correct score of 78%. Most patients would not think of 78% correct as being “normal.” I think you are better off to simply use the classification categories (see Table 1).
35. You also mentioned earlier the use of SIN testing for a demonstration of hearing aid benefit?
Mueller: Yes, and you’re going to like this, as I’m going to suggest a scoring method that indeed uses percent correct. For this testing, we want to use “casual” speech (~55 dB SPL)—a little below average, and conduct unaided and aided measures. It’s probably okay to just do the testing bilaterally, unless there is significant ear asymmetry. What I think works well is to then plot out percent correct for each of the six SNRs measured (with two lists, you have ten key words for each SNR, so the math is simple). What you will commonly see is that for the very easy SNR of +25 dB, there will be little difference in aided vs. unaided, as the patient probably did pretty well unaided. And also, at the most difficult SNR (0 dB) it’s common that the patient will score 0% for both conditions—it’s of course important to inform the patient that normal hearing individuals also have problems at this SNR. Where you commonly see the most advantage for aided is for the +5, +10 and +15 dB SNRs—SNRs that commonly are encountered in real-world activities (see example of unaided vs. aided testing in Figure 4).
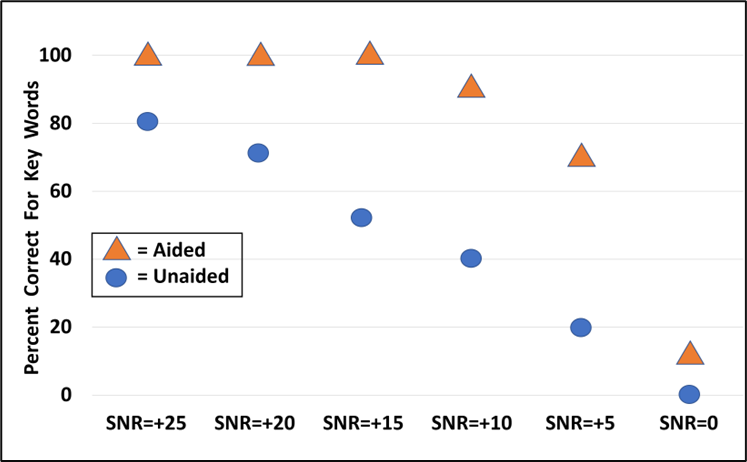
Figure 4. Example of using the QuickSIN for bilateral aided vs. unaided testing. Two lists were presented at each SNR for each condition. The values shown represent the percent correct for the 10 key words for each SNR, for the two different test conditions.
36. This is all great, and I’m excited to start doing SIN testing, but I have to ask: Do all these clinical measures really relate to real-world benefit and satisfaction?
Mueller: Great question. If you want to cherry pick, you could find published articles that answer your question in very different ways. For the moment, I’m going to hang my hat on a recent systematic review, where six types of behavioral pre-fitting measures were evaluated (Davidson et al, 2021). There were 1342 articles identified, and after specific inclusion criteria were applied, 21 studies were included in the final analysis. The pre-fitting tests that showed significant correlations with hearing aid satisfaction were the speech-in-noise tests. Interestingly, but maybe not surprisingly, two tests that historically have been used to predict benefit with hearing aids, degree of hearing loss and speech recognition in quiet, were not correlated with hearing aid satisfaction.
Ricketts: I agree this is another example of how unaided SIN testing can give us clinically important information. However, we should also consider that there is no clear relationship between real-world outcomes and aided SIN measures. For this reason, I think the greatest utility for aided SIN testing relates to demonstration, rather than true validation.
Hornsby: Ditto to what both Todd and Gus already said. And to reiterate some prior points, even if performance on a SIN task doesn’t directly reflect real-world performance, when done correctly, it can give us clinically important information that may not be available from traditional word-recognition-in-quiet testing.
37. So here’s the big question, how do I get paid for doing all this extra testing?
Mueller: Some might say it isn’t “extra,” but we’ve already had that discussion. Here are some suggestions:
- Related to the hearing aid fitting (Bundled Approach): This is an easy one. SIN testing is an important component of fitting hearing aids, and it seems reasonable that it simply would be part of the “service bundle.”
- Related to the hearing aid fitting (Itemized/Unbundled Approach): Again, SIN testing is a component of fitting hearing aids, and accordingly, would be on the same list as the other itemized services, billing for the time involved for the testing and discussing findings with the patient.
- Not related to the hearing aid fitting: For starters, the three of us are not billing experts, so I recommend you check with your favorite audiology or practice management organization, all of which have experts in this area. Just to help you out a little, I did pose your question to one of those experts, audiologist Deb Abel, and she informed me that when there is no dedicated CPT code, 92700 (Unlisted otorhinolaryngological service or procedure), is the best option and could be considered part of a functional communication needs assessment that could include other tests (e.g., cognitive and/or dexterity screenings) for a more holistic/global view of the patient and setting realistic expectations.
38. Back at the beginning you mentioned you’d be happy to toss out some practical advice. How about some summary step-by-step guidelines concerning how I should do this testing Monday Morning?
Mueller: Monday Morning? We’re liking your thinking! As we’ve mentioned, this really will depend on your reason for doing the test. Here are some guidelines for the two most common reasons:
Reason for doing test: Estimate optimum QuickSIN performance
- Seat patient, give instructions and fit with insert earphones.
- Use the standard QuickSIN recording. Only use the seven lists that are equivalent: 1, 2, 6, 8, 10, 11, and 12.
- Select a presentation level of 70 dB HL, or if PTA >45 dB, use patient rating of “Loud, But Okay” (just below the LDL).
- Select appropriate masking (speech noise) for the non-test ear.
- Test each ear independently. Present two QuickSIN lists to each ear. Take average of these two scores to derive SNR-Loss for each ear.
- Use the critical difference chart to determine if the right and left ear scores are significantly different, and/or if the scores obtained are different from previous testing.
- Use the SNR-Loss results to counsel the patient regarding performance (e.g., normal, mild difficulty, moderate, etc), and SIN expectations with hearing aids (e.g., does he just need audibility, advanced technology, or, assistive listening devices?).
Reason for doing test: Demonstration of aided benefit
- Establish HL to SPL difference for calibrated location in soundfield where patient will be sitting; loudspeaker at 0 degree azimuth.
- Seat patient in soundfield calibrated position, and give instructions. Fit the patient with hearing aids programmed to use settings (e.g., real-ear verified NAL-NL2)
- Use the standard QuickSIN recording. Only use the seven lists that are equivalent: 1, 2, 6, 8, 10, 11, and 12.
- Select a presentation level that will result in 53-55 dB SPL at the calibrated soundfield location (this will be around 40 dB HL, but will vary with equipment/setting).
- Testing first conducted bilaterally unaided. Two QuickSIN lists. Take average of these two scores for the SNR-Loss. Note: If the patient’s loss is so severe that they are not understanding any of the words at the +25 dB SNR in the unaided condition, increase presentation level accordingly—raise to average-level speech (~63 dB SPL).
- Patient is then fitted bilaterally to appropriate use setting (e.g., NAL-NL2 real ear verified) and aided bilateral testing is conducted. Two QuickSIN lists. Take average of these two scores for the SNR-Loss.
- Use the critical difference chart to determine if the aided scores are better than the unaided scores.
- Use the SNR-Loss results to counsel the patient regarding aided hearing aid benefit. Convert the percent of words correct for each of the six SNR ratios to compare aided to aided (for two lists, there are ten key words for each SNR). It is helpful to graph them on a chart for the patient (See Figure 4).
39. Thanks. Exactly what I needed. Do you happen to have any sample case studies handy?
Mueller: Most certainly. Here are a few that we’ve put together over the years (see Mueller, 2016 https://www.audiologyonline.com/articles/signia-expert-series-speech-in-18336 for additional QuickSIN cases):
Patient A: A young woman says she is having problems at work, struggling to understand colleagues, causing some problems. Her pure-tone thresholds are no worse than 15 dB at any frequency, and she scored 100% on the NU#6 monosyllabic words-in-quiet list. Immittance/reflexes also normal.
- Without SIN results: You might start wondering if there are other things going on at work and she is just using this “can’t hear” thing as an excuse.
- With SIN results: Her SNR-Loss is ~6 dB bilaterally. You fully understand why she is having a problem, and tailor your counseling and treatment plan accordingly.
Patient B: A middle-aged man with a typical downward-sloping noise-induced hearing loss states that he only will wear hearing aids that are “invisible”—has seen internet ads for the iCIC models.
- Without SIN results: You might want to steer him toward RICs, explaining why good directional technology (not available with iCIC) is important, and will provide significant benefit in background noise.
- With SIN results: His SNR-Loss is no worse than 2 dB in either ear, within the range of normal. You now feel okay going with his wishes, as if you give him appropriate audibility, he should do okay in background noise without directional processing.
Patient C: An older man in his 90s, with a relatively symmetrical moderate-to-serve loss, states that he only wants to purchase one hearing aid. What ear do you fit?
- Without SIN results: You’ll talk about things like ear for telephone, situational listening (in car?), and other ear-specific factors.
- With SIN results: His SNR findings show 8 dB SNR-Loss for the right ear, 13 dB SNR-Loss for the left. If other factors are a toss-up, or only mildly important, you’re going to fit the right ear, to give him the best shot at SIN understanding.
Patient D: Very active woman in her 70s, with moderate long-standing hearing loss secondary to Meniere’s. When completing the pre-fitting COSI, the #1 rated item on her list was understanding her friends during their weekly dinner at the Blarney Stone restaurant.
- Without SIN results: You’ll smile and tell her that you like the food there too. You’ll make sure she gets the best directional technology on the market, and hopefully she’ll do just fine.
- With SIN results: Her SNR-Loss is ~14 dB SNR in both ears—much worse than you would have predicted from her audiogram and speech-recognition-in-quiet testing. You’ve been to the Blarney Stone and know it’s a very noisy Irish Pub, with typical SNRs of +5 dB or worse. You now start talking about realistic expectations, maybe not having this item as COSI #1, alternative listening devices for this situation, or maybe finding her a quieter restaurant.
Patient E: A demanding fellow in his 70s, who purchased his first set of hearing aids from you three weeks ago. He’s back with his hearing aids (and the contract), saying that you told him that they will help him in background noise, but they don’t. It’s looking a lot like a return for credit.
- Without SIN results: After doing data logging, you point out to him that he really hasn’t given the hearing aids much of a chance; he has to become accustomed to using them, etc, etc.
- With SIN results: You pull out the chart from the day of the fitting, showing him the unaided vs. aided testing, where indeed he did much better using hearing aids at SNR of +5 and +10 dB. You ask him if he wants to do that test again. He does. You take him to the booth and test him unaided and aided, using a casual level of speech (e.g., 53-55 dB SPL). Following the aided testing, you point out that the results are the same as before; there indeed was background noise, and he did significantly better when aided. He agreed. He’s going to give the aids another shot.
40. Thanks for all the information. Any closing words?
Mueller: I think the bottom line is to ask yourself this: If I implement SIN testing into my routine practice, will I end up with a better treatment plan for many of my patients? Will I learn more about the quality of my hearing aid fittings? Will my counseling be more patient-centered and effective? Will the testing help establish patient trust and loyalty? In all cases, I think the answer is “yes.”
References
American Speech-Language-Hearing Association. (1988). Determining threshold level for speech [Guidelines]. Available from www.asha.org/policy.
American Speech-Language-Hearing Association (n.d.). Hearing Loss in Adults (Practice Portal). Retrieved from /Practice-Portal/Clinical-Topics/Hearing-Loss/.
Barbee, C. M., James, J. A., Park, J. H., Smith, E. M., Johnson, C. E., Clifton, S., & Danhauer, J. L. (2018). Effectiveness of auditory measures for detecting hidden hearing loss and/or cochlear synaptopathy: A systematic review. Seminars in Hearing, 39(2), 172-209. Thieme Medical Publishers.
Benítez-Barrera, C. R., Grantham, D. W., & Hornsby, B. W. (2020). The challenge of listening at home: Speech and noise levels in homes of young children with hearing loss. Ear and Hearing, 41(6), 1575-1585.
Cancel, V. E., McHaney, J. R., Milne, V., et al. (2023). A data-driven approach to identify a rapid screener for auditory processing disorder testing referrals in adults. Scientific Reports, 13, 13636. https://doi.org/10.1038/s41598-023-40645-0
Carhart, R., & Tillman, T. W. (1970). Interaction of competing speech signals with hearing loss. Archives of Otolaryngology, 91, 273–279.
Clark, J., Huff, C., & Earl, B. (2017). Clinical practice scorecard—Are we meeting clinical practice standards. Audiology Today, 29(6).
Cox, R. M., Alexander, G., & Gilmore, C. (1987). Development of the Connected Speech Test (CST). Ear and Hearing, 8(5 Suppl), 119S-126S. doi: 10.1097/00003446-198710001-00010.
Davidson, A., Marrone, N., Wong, B., & Musiek, F. (2021). Predicting Hearing Aid Satisfaction in Adults: A Systematic Review of Speech-in-noise Tests and Other Behavioral Measures. Ear and Hearing, 42(6), 1485-1498.
Etymotic Research. (2005). BKB-SIN[TM] speech in noise test version 1.03 (compact disc). Elk Grove Village, IL: Etymotic Research.
Fitzgerald, M. B., Gianakas, S. P., Qian, Z. J., Losorelli, S., & Swanson, A. C. (2023). Preliminary Guidelines for Replacing Word-Recognition in Quiet With Speech in Noise Assessment in the Routine Audiologic Test Battery. Ear and Hearing, 20, 00-00.
Gatehouse, S., Elberling, C., & Naylor, G. (1999). Aspects of auditory ecology and psychoacoustic function as determinants of benefits from and candidature for non-linear processing in hearing aids. Danavox Symposium.
Holder, J. T., Sheffield, S. W., & Gifford, R. H. (2016). Speech understanding in children with normal hearing: Sound field normative data for BabyBio, BKB-SIN, and QuickSIN. Otology & Neurotology, 37(2), e50-e55.
Killion, M. C., Niquette, P. A., Revit, L. J., & Skinner, M. W. (2001). Quick SIN and BKB-SIN, two new speech-in-noise tests permitting SNR-50 estimates in 1 to 2 min. The Journal of the Acoustical Society of America, 109(5_Supplement), 2502-2502.
Kujawa, S. (2017, August). 20Q: Cochlear synaptopathy - interrupting communication from ear to brain. AudiologyOnline, Article 20946. Retrieved from www.audiologyonline.com
Leavitt, R., & Flexer, C. (2012). The importance of audibility in successful amplification of hearing loss. Hearing Review, 19(13), 20-23.
McArdle, R. A., & Wilson, R. H. (2006). Homogeneity of the 18 QuickSIN™ lists. Journal of the American Academy of Audiology, 17(3), 157-167.
McArdle, R., Killion, M., Mennite, M., & Chisolm, T. (2012). Are two ears not better than one? Journal of the American Academy of Audiology, 23(3), 171-181.
Moore, D., Edmondson-Jones, R., Dawes, P., Fortnum, H., McCormack, A., Pierzycki, R., & Munro, K. (2014). Relation between speech-in-noise threshold, hearing loss, and cognition from 40–69 years of age. PloS One, 9(9), e107720.
Mueller, H. G. (2010). Three pre-tests: What they do and why experts say you should use them more. Hearing Journal, 63(4), 23-28.
Mueller, H. G. (2014). 20Q: Real-ear probe-microphone measures - 30 years of progress? AudiologyOnline, Article 12410. Retrieved from: https://www.audiologyonline.com
Mueller, H. G. (2016). Speech-in-noise testing for selection and fitting of hearing aids: Worth the effort? AudiologyOnline, Article 18336. Retrieved from https://www.audiologyonline.com.
Mueller, H. G., Ricketts, T., & Bentler, R. (2014). Modern Hearing Aids: Pre-fitting testing and selection considerations. San Diego: Plural Publishing.
Mueller, H. G., & Hornsby, B. W. Y. (2020). 20Q: Word recognition testing - let's just agree to do it right! AudiologyOnline, Article 26478. Retrieved from www.audiologyonline.com.
Mueller, H. G., Coverstone, J., Galster, J., Jorgensen, L., & Picou, E. (2021). 20Q: The new hearing aid fitting standard - A roundtable discussion. AudiologyOnline, Article 27938. Available at www.audiologyonline.com.
Nilsson, M., Soli, S. D., & Sullivan, J. A. (1994). Development of the hearing in noise test for the measurement of speech reception thresholds in quiet and in noise. The Journal of the Acoustical Society of America, 95(2), 1085-1099.
Pearsons, K., Bennett, R., & Fidell, S. (1977). Speech levels in various noise environments (Report No. EPA-600/1-77-025). Washington DC: US Environment Protection Agency.
Qian, Z. J., Vaisbuch, Y., Gianakas, S. P., & Tran, E. D. (2023). Evaluation of Asymmetries in Speech-in-Noise Abilities in Audiologic Screening for Vestibular Schwannoma. Ear & Hearing, 20, 00-00.
Ricketts, T., Bentler, R., & Mueller, H. G. (2019). Essentials of Modern Hearing Aids. San Diego: Plural Publishing.
Rusnock, C., & Bush, P. (2014). An Evaluation of Restaurant Noise Levels and Contributing Factors. Journal of Occupational and Environmental Hygiene, 9(6), D108-113.
Saunders, G. H., & Haggard, M. P. (1989). The clinical assessment of obscure auditory dysfunction—1. Auditory and psychological factors. Ear and Hearing, 10(3), 200-208.
Sherbecoe, R. L., & Studebaker, G. A. (2003). Audibility-index predictions of normal-hearing and hearing-impaired listeners' performance on the connected speech test. Ear and Hearing, 24(1), 71-88.
Spahr, A. J., Dorman, M. F., Litvak, L. M., Van Wie, S., Gifford, R. H., Loizou, P. C., ... & Cook, S. (2012). Development and validation of the AzBio sentence lists. Ear and Hearing, 33(1), 112.
Smeds, K., Wolters, F., & Rung, M. (2015). Estimation of signal-to-noise ratios in realistic sound scenarios. Journal of the American Academy of Audiology, 26, 183-196.
Valente, M., Oeding, K., Brockmeyer, A., Smith, S., & Kallogjeri, D. (2018). Differences in word and phoneme recognition in quiet, sentence recognition in noise, and subjective outcomes between manufacturer first-fit and hearing aids programmed to NAL-NL2 using real-ear measures. Journal of the American Academy of Audiology, 29(8), 706-721.
Vermiglio, A. J. (2008). The American English hearing in noise test. International Journal of Audiology, 47(6), 386-387.
Vermiglio, A., Soli, S., & Fang, X. (2018). An argument for self-report as a reference standard in audiology. Journal of the American Academy of Audiology, 29(3), 206-222.
Wagener, K. C., Brand, T., & Kollmeier, B. (1999). Entwicklung und Evaluation eines Satztests für die deutsche Sprache II: Optimierung des Oldenburger Satztests [Development and evaluation of a sentence test for the German language II: Optimization of the Oldenburg sentence test]. Zeitschrift Audiologie/Audiological Acoustics, 38(2), 44–56.
Weisser, A., & Buchholz, J. M. (2019). Conversational speech levels and signal-to-noise ratios in realistic acoustic conditions. The Journal of the Acoustical Society of America, 145(1), 349-360.
Wilson, R. (2004). Adding speech-in-noise testing to your clinical protocol: Why and how. The Hearing Journal, 57(2), 10-19.
Wilson, R. (2011). Clinical experience with the words-in-noise test on 3430 veterans: Comparisons with pure-tone thresholds and word recognition in quiet. Journal of the American Academy of Audiology, 27(7), 405-423.
Wilson, R. H., & McArdle, R. (2008). Change is in the air – in more ways than one. Hearing Journal, 61(10), 10-15.
Wilson, R. H., & Burks, C. A. (2005). The use of 35 words to evaluate hearing loss in terms of signal-to-babble ratio: A clinic protocol. Journal of Rehabilitation Research and Development, 42, 839–852.
Wilson, R., McArdle, R., & Smith, S. (2007). An evaluation of the BKB-SIN, HINT, QuickSIN, and WIN materials on listeners with normal hearing and listeners with hearing loss. Journal of Speech, Language and Hearing Research, 50(4), 844-856.
Wu, Y. H., Stangl, E., Chipara, O., Shabih, S., Welhaven, A., & Oleson, J. (2018). Characteristics of Real-World Signal to Noise Ratios and Speech Listening Situations of Older Adults With Mild to Moderate Hearing Loss. Ear and Hearing, 39(2), 293-304.
Zapala, D. A., Stamper, G. C., Bogle, J. M., Jagger, S. L., & Lundy, L. B. (2023). Clinical Utility of the Standardized Word Recognition Score. Ear and Hearing, 10-1097.
Zhao, F., & Stephens, D. (2007). A critical review of King-Kopetzky syndrome: Hearing difficulties, but normal hearing? Audiological Medicine, 5(2), 119-124.
Zhao, F., & Stephens, D. (1996). Hearing complaints of patients with King-Kopetzky syndrome (obscure auditory dysfunction). British Journal of Audiology, 30(6), 397-402.
Zitelli, L., Jedlicka, D., Scagline, T., Reitz, A., Cody Leslie, and C. Palmer. "The results are in: 2020 member survey of the use of real-ear probe microphone measurements." Audiology Today (2020).
Citation
Mueller, H. G., Ricketts, T. & Hornsby, B. Y. G. (2023). 20Q: speech-in-noise testing - too useful to be ignored! AudiologyOnline, Article 28760. Available at www.audiologyonline.com




