 From the Desk of Gus Mueller
From the Desk of Gus Mueller

World-famous pilot Charles Lindbergh and the remote programming of hearing aids? A connection perhaps? Well . . . sort of! Twenty years ago, in one of the first and most noted examples of telemedicine, dubbed the Lindbergh Operation, surgeons in New York City’s Mount Sinai Medical Center removed the gallbladder of a 68-year-old woman located in Strasbourg, France, using a remote-controlled robotic system. You would think, that if you could take out a gall bladder from a distance of 4,000 miles, you certainly should be able to remotely program a hearing aid for someone who just lives across town, right? Well, that didn’t happen until several years later.
I remember an article authored by audiologists Jason Galster and Harvey Abrams, titled “Are you ready for remote hearing aid programming,” with the sub-heading, “If not you should be getting ready for this next step in patient care.” That article is from 2012! Yes, nine years ago. As you all know, that “next step” was a big one . . . or there were several little ones in between.
Things finally did start to ramp up with remote programming a few years ago, although at the onset, many audiologists were no more than lukewarm regarding the implementation. When the effects of the pandemic struck last March, however, things changed, and even those who said “I’ll never get involved with that” were considering this patient-care strategy as an option.
Today, remote programming is available from all major manufacturers, but like anything, adding a new procedure related to fitting hearing aids requires some initial training. And as you would expect, each manufacturer has approached this feature somewhat differently. If only there were someone who could summarize the similarities and differences among all the different manufacturers? Wait—we have found just that person!
Lori Zitelli, AuD, is a Senior Audiologist at the University of Pittsburgh Medical Center. She also serves as an instructor for the University of Pittsburgh’s AuD program. Her special audiologic interests include treatments for tinnitus, clinical research, clinical education, and interventional audiology. Her publications are related to inpatient audiology services and the role of audiology in interdisciplinary teams within the medical setting.
Dr. Zitelli currently serves on the Academy of Audiology’s Conference Program Committee, is Chair of the AAA Member Connect Subcommittee, and is a Trustee of the Academy Foundation. She recently was selected as one of the Academy’s Jerger Future Leaders of Audiology.
While there is little mention of Charles Lindbergh in Lori’s excellent 20Q, there is a lot of talk about the different aspects of remote hearing aid fitting and adjustment, how this varies from manufacturer to manufacturer, and why you might want to consider adding this service to your current patient-care toolbox.
Gus Mueller, PhD
Contributing Editor
Browse the complete collection of 20Q with Gus Mueller CEU articles at www.audiologyonline.com/20Q
20Q: Remote Hearing Aid Programming - Getting Started
Learning Outcomes
After reading this article, professionals will be able to:
- Explain clinical uses or reasons for professionals to offer remote hearing aid programming.
- List resources and considerations for getting set up to do remote hearing aid programming with major hearing aid manufacturers.
- Summarize the results of key studies looking at how remote hearing aid programming affects patient satisfaction.
 Lori Zitelli, AuD
Lori Zitelli, AuD Author’s Note: The specific information presented here was accurate as of January, 2021. The accuracy of the information was confirmed with each manufacturer. This type of technology is evolving quickly, so some information may have changed, but this should give you an idea of what you need to consider when deciding what level of remote services to offer. Each manufacturer approaches remote programming differently, so tables and specific information has been included for each question when appropriate to indicate differences among manufacturers.
1. What exactly do you mean by "remote programming?"
We are all familiar with face-to-face hearing aid care. During this type of appointment, the patient shows up, we attempt to connect the hearing aids to the software, we say curse words when we can’t get them to connect (kidding, kind of!), we make programming adjustments and verify audibility and prescriptive targets, we disconnect the hearing aids, and then the patient leaves our office. When fine tuning adjustments are needed, they return to our offices and we complete the process again. This method is straightforward, familiar to all, and works well when the patient can physically access us in our office spaces.
The ability to program hearing devices remotely (e.g., when the patient is at home and the clinician is in their office or in their own home) improves patient access to follow-up care when they are unable to be seen for a face-to-face visit in the office or prefer to stay at home.
2. When did remote hearing aid programming services become available?
Remote programming capabilities have been available for a few years now in a variety of forms (anyone remember Starkey T2 and Widex ToneLink?), but many clinicians became particularly interested in providing these services in 2020 during the COVID-19 pandemic. During this time, when many individuals were unable to access in-person healthcare, patients still wanted to receive services – and since many offices were not seeing patients in person, the services needed to be provided via telehealth. This shift occurred across the healthcare spectrum (Wosik et al., 2020) and was keenly felt in the audiology community (Saunders & Roughley, 2020). Many people - individuals wearing hearing aids and those with untreated hearing loss alike - suddenly experienced greater difficulty communicating secondary to 1) an increase in the amount of communications occurring via video and phone platforms, 2) the increased distance required to interact safely with another individual, 3) the reduced acoustic and visual information available because of masking requirements, or other issues.
3. I get it, but I’m not sure I totally understand how this would fit into my practice.
How about I give you a couple of examples. I could provide several, but I’ll pick two that I think illustrate how this type of care can improve access. In my clinic, we work with all of the major hearing aid manufacturers.
This particular patient happens to have a Phonak hearing aid. She is a delightful 75-year old woman who underwent a translabyrinthine resection of an acoustic neuroma in her left ear when she was in her late 20s, resulting in a profound sensorineural hearing loss in her left ear. She began to develop hearing loss in her right ear in her 60s and became my hearing aid patient (see her most recent audiogram in Figure 1). It is also relevant to tell you that she has experienced chronic pulmonary issues with several bouts of pneumonia over the past few years.
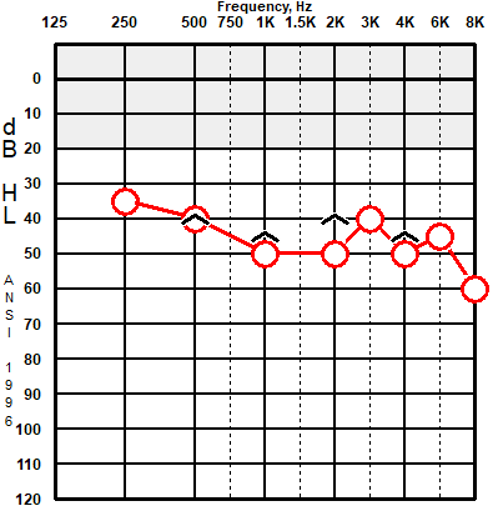
Figure 1. Audiogram for right ear for sample patient. She has no hearing in her left ear.
Her previous hearing aid was accidentally run over by a vehicle (I know!) and needed to be replaced. Given her history of pulmonary issues, she indicated that she preferred telemedicine options whenever possible so that she could avoid coming into contact with other individuals in our office during the COVID-19 pandemic. Following her updated audiogram and hearing aid fitting (both completed in-office), she had several questions and a programming request, so we set up a time for a remote programming session. Phonak’s remote programming strategy is synchronous, meaning we connected in real time via a video chat (more on this later). She connected through her phone; I connected through my Phonak software. She described that she wanted the gain to be slightly softer, so a small global gain reduction was completed in real time. She immediately noticed the difference and stated how much more comfortable she was (and how glad she was that she wouldn’t have to reduce the volume each time she put the hearing aid on). She was very pleased that she could accomplish this without coming to the office - so much so that I suspect I will only see her in-person when absolutely necessary in the future.
A second example involves a patient with symmetrical, mild to moderate high frequency sensorineural hearing loss and bothersome tinnitus. He lives about 45 minutes outside of the city and has to travel through a tunnel to get to my clinic (not a deal breaker, but Pittsburgh tunnels are notorious for causing awful traffic problems). His initial Tinnitus Handicap Inventory (THI) score was 84/100 (this indicates a catastrophic self-perceived handicap). This was his first pair of hearing aids (they were GNResound devices). On the day of his hearing aid fitting (in the office), I didn’t activate the tinnitus sound generator (TSG). He was a first-time hearing aid user and requested a few weeks to adjust to the devices without the TSG. Additionally, many patients with bothersome tinnitus find that amplification alone sufficiently reduces their tinnitus perception (although, with such a significant self-perceived handicap, I did plan to activate the TSG eventually). After wearing the devices for a few weeks, he did report that his tinnitus was less noticeable but he was interested in activating the TSG to see if he was able to further reduce his tinnitus awareness/annoyance. We scheduled a time to connect remotely so that he could avoid traveling into the city and I activated it. During our remote programming session, I explained how to set the TSG appropriately. Since that time, we have made some other small remote adjustments (decreasing the default volume of the TSG, re-shaping the sound slightly to more closely resemble pink noise than white noise). He has been very pleased. I’m seeing him soon, so I’ll be interested to see what his new THI score will be!
4. Those are nice stories. I’d consider doing something like that. How exactly does remote programming work?
The majority of current remote programming services are possible because of cloud-based connections. Patients will log into their manufacturer-specific app and connect to the cloud. The hearing professional will establish a secure cloud connection with the hearing aid user via Bluetooth and make adjustments to the devices.
One thing to remember about these cloud-based services is that you may need to remember to log into the cloud each time the devices are programmed, even if the programming takes place in-person in your clinic. I had one patient who wanted a remote programming adjustment, and then needed to be seen in the office for a dome issue. While she was in the office, she requested another small programming adjustment. Because she was with me in the clinic, I programmed the devices without logging into the cloud. By doing this, I unknowingly disconnected her hearing aids from the cloud. The next time she wanted a remote adjustment, we had to spend time reconnecting her devices first.
There are a few exceptions to cloud-based programming:
A. Signia provides a cloud-based service for newer, wireless devices but also provides a non-bluetooth option for older Primax and Binax devices. The adjustments that can be made in the Signa Telecare app for the older devices can be thought of as equalizer settings (low-, mid-, and high-frequency gain offsets). The app communicates with hearing aids by sending commands that are encoded in high-frequency tones. WidexLink is similar and works with some current hearing aid lines (Moment, Evoke, Beyond).
B. Widex uses a neck-worn device, which they call RemoteLink, that connects to the hearing aids instead of relying on a cloud-based service. By using RemoteLink, Widex has eliminated any limitations that some of the cloud-based services encounter (something we maybe can talk about later). Thus, any adjustments that can be made in-office can be made remotely with Widex devices as long as the patient has access to the RemoteLink. This can be accomplished through some loaner or rental program, or more efficiently, by simply including the RemoteLink as part of the purchase price, as you would with a charger. Regardless of how you choose to approach this, make sure you pair the RemoteLink that the patient will be using to their programming file before you give it to them (it will not work if this step has been skipped).
5. Is remote programming only available in the “premier” products?
No! Each manufacturer provides remote programming capabilities at all technology levels. Let me clarify - not all devices have this capability, but there are at least some models in each technology level that offer this option for each manufacturer. For example, there are specific Unitron devices at the 3, 5, 7, and 9 technology levels that can be programmed remotely, but not all Unitron hearing aids can be programmed this way (only the Discover Next line has this capability).
Table 1 includes a list of platforms, technology levels, and models that can be programmed remotely.
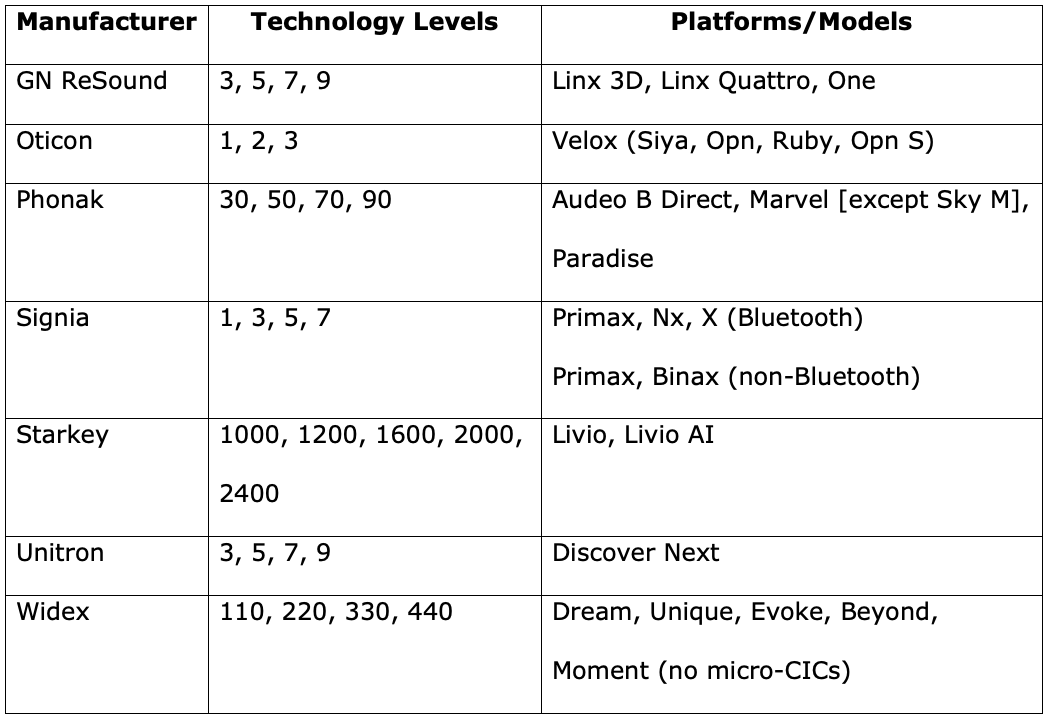
Table 1. Remote programming platforms/models and technology levels for major hearing aid manufacturers.
6. How will I know when my patients want an adjustment?
To start, patients can always contact you via a phone call, e-mail, or secure electronic messaging system – or however they would normally contact you - to let you know that they need an adjustment. In these cases, you would set up an appointment time to connect remotely with your patient (just like you would for an in-person adjustment).
Additionally, GNResound, Signia, & Starkey users can indicate that they want a programming adjustment through their manufacturer-specific app. You can configure your GNResound Online Services, Signia Telecare, and Hearing Care Anywhere accounts so that you will receive an email to notify you that an adjustment has been requested.
7. My schedule is pretty busy. How do you manage this when receiving constant requests for adjustments?
I was afraid of this too! Initially, I envisioned a cascade of emails from all of my patients telling me about the problems they are having with their devices. This isn’t what happened, though. My advice would be to schedule a planned time to check for notifications from patients each day (or assign someone in your office to check this). Alternatively, you could make sure your assistant or front desk staff have access to these messages by setting up a forwarding rule in your email for these notifications or giving them access to the programming software. Then, once you know which patients need an adjustment, you can have your front desk staff call them to schedule a specific appointment time. During this time, you can connect with them in real-time to provide remote care or send the programming change to their phone for them to access at their convenience.
8. You mean there is an option to do this asynchronously, like e-mail? It might be nice to have the flexibility to respond when I have time.
It depends on the manufacturer. Oticon, Phonak, and Widex provide synchronous remote care (i.e., in real time via a two-way audio and video connection). To connect with your patients remotely using these manufacturers, you’ll need a webcam and microphone/speaker connected to your computer. In the software, there will be a window where you can see your patient’s face while you are making adjustments. For these visits, it will probably be easiest to schedule a specific time to meet during your workday. You can find a way to indicate on your schedule that it will be a remote visit, and it can be scheduled like any other follow-up programming adjustment appointment.
Unitron provides remote care asynchronously. After you communicate with the patient to find out what adjustments are needed, you’ll make the programming changes and save it to the cloud. Then, the patient will access the settings at their convenience through the app on their phone. You may find that you have time to address these issues between patients, over your lunch break, or at other times throughout the day – or, if you prefer, you can schedule a time to make the adjustments and send them to the patient. Whatever works best for you is how you should approach this!
GNResound, Signia, and Starkey provide options for both synchronous and asynchronous remote programming.
9. How can I be sure that this will work? I do not want to set up an appointment with my patient and then not be able to connect to them.
Reasonable question. I recommend reaching out to your manufacturer representative and asking them to do a practice session with you. It helped me immensely to do this before connecting with my first patient. When I was able to do it successfully during the practice session, I knew that I had set up my remote programming account correctly and that I would be able to access the patient without any issues on my end. It also really helped me to know what to expect and what limitations I might encounter when connected with a patient. It may be beneficial to send your patient a brief message ahead of time with some tips (e.g., make sure they have access to a strong internet connection, make sure their phone is sufficiently charged) or provide a handout that you can include with their paperwork on the day of the delivery with tips for remote programming. I have been doing several remote programming sessions every week for the past few months, and would say that there have been very few instances where I was unable to connect to the patient and complete the session. In one recent case, the patient was not receiving the notification that I was trying to connect to him, and it turns out that he had not enabled the app to access his microphone and camera. Once he completed this step, we were able to connect without any problems.
10. Do I need any special set-up to start doing remote programming?
Yes, there are some up-front things to take care of. Let’s start with programming accounts. Each manufacturer requires the provider to establish an account to access remote programming services. Frequently, these accounts are linked to their online portals (e.g., GNResound Online Services, MyUnitron, PhonakPro). Setting up these accounts is simple – actually, you may already have one if you order hearing aids online! I have provided some information in Table 2 that specifies what kind of account is needed for each manufacturer and how you can obtain these accounts, if you need one.
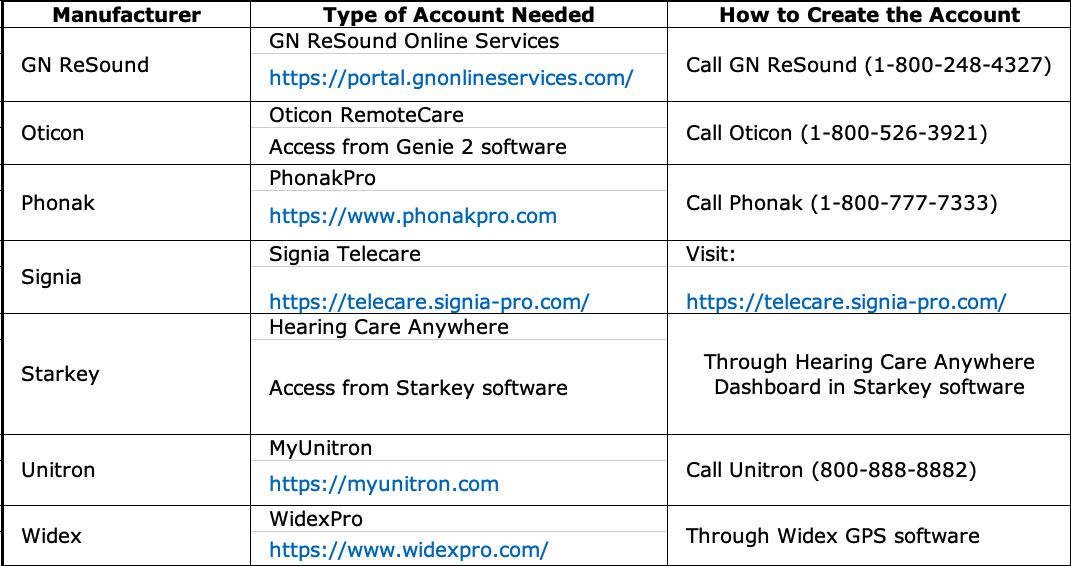
Table 2. Information about setting up remote programming accounts with the major hearing aid manufacturers (type the web addresses into your browser). Download PDF here.
11. What else should I be thinking about when it comes to remote hearing aid programming?
Depending on where you work, there could be access issues. In late 2020, many hospital systems and universities tightened their cybersecurity due to the risk of ransomware attacks targeting sensitive information. As a result, some providers may have issues related to firewalls and specific cybersecurity settings that restrict their access to cloud-based services or patients outside of their network. Each manufacturer has a team of IT specialists who can provide information to your IT group that may allow you to provide remote services despite these restrictions.
Additionally, if you plan to provide remote care to patients who do not live in your state, please consult your state licensure laws first. Many regulations related to telehealth were relaxed during the COVID-19 pandemic, but it’s always important to make sure we are providing care within the boundaries set by our licenses.
12. Are there programming limitations associated with remote care?
There are some limitations that will apply to all manufacturers. For one, you of course won’t be able to complete real-ear probe microphone measurements for remote sessions when the patient is in their own home and this is the gold standard for verifying audibility and prescriptive targets. In most cases, however, this will be conducted in-person during the initial fitting, so you do have a baseline for reference. Aside from that, each manufacturer has their own strategy for providing remote care, so the specific limitations you encounter will vary depending on which manufacturer you are working with. For example, you may not be able to remotely create or delete a program, make programming adjustments to the tinnitus sound generator, complete the feedback calibration, complete in-situ audiometry, or update firmware. I’ll provide a summary chart at the end of our discussion.
13. It seems like there may be a lot of preparation needed. What needs to be done ahead of time and how do you have time for this?
Fortunately for all of us, each manufacturer provides a guide that outlines exactly how you can provide these services, frequently with step-by-step directions, screenshots, and other useful tips. Many hearing aid manufacturers provide a guide that specifies exactly what the patient needs to do prior to any remote programming appointments (yes, these are in the chart I mentioned too). You could include this handout with the other paperwork that you provide to your patient on the day they receive their hearing aid. It’s also nice to have an electronic version available that you can send to them when they inevitably lose the copy you originally gave them!
The patient typically needs to create an account (sometimes this is contained within the manufacturer’s app; it also could be separate from the app). Sometimes they need to sign a manufacturer consent form indicating that they consent to this type of care in order to activate this capability (this may also be done through the manufacturer’s app). They will need to make sure the manufacturer’s app is downloaded to their phone and the hearing aids are connected to their phone via Bluetooth. These are all things that we can help our patients do at prior appointments, if we know they are going to be interested in remote programming at some point in the future. During the remote session, the patient needs to have access to a stable internet connection. As we discussed earlier, for Widex remote programming adjustments, they’ll also need access to the RemoteLink device.
If the patient uses devices powered by disposable batteries, most manufacturers recommend that the batteries are new while accessing remote programming services. If the batteries are rechargeable, there must be a charge level that is sufficient. One manufacturer specifies that the charge needs to be greater than 30% to support remote programming services. Most manufacturers don’t specify a minimum percentage charge level, but more is always better in these instances. The battery consumption occurring during these types of communications with the devices will be greater than normal. You may want to remind your patient to make sure their devices are charged adequately. Additionally, they’ll need an adequate charge level for their cell phone.
In terms of having time for this, once you invest a little bit of time getting all of the accounts set up and familiarizing yourself with how this process works, it’s very simple and fast. I actually completed 2 remote programming appointments this morning in under 20 minutes each (including the documentation)!
14. My patients tend to have a mix of iPhones and Android phones. Does that matter?
All of the manufacturer apps can be downloaded on both Android and Apple devices. There may be some requirements related to the specific version of the operating system that are required or the specific phone model. Each manufacturer provides a list of compatible models. See the chart at the end for links.
15. What if I never activated the remote programming feature when I saw the patient in person?
This was an issue for us in the spring and summer of 2020, when many patients were unable or unwilling to attend face-to-face visits in our clinics. Several people wanted remote programming adjustments, but many of the manufacturers required that this capability be “activated” while connected to the software – which, of course, we had not done because we had not needed to!
Each manufacturer now approaches this differently. For patients using Starkey and Signia devices, this option must still be activated while the hearing aids are connected to the software. So, this would not be possible unless the patient comes into the office to activate this feature (or, thinking outside the box, if they are unable to physically come to the office, they could drop off or mail the devices to you, let you activate remote programming by connecting the devices to the software, and pick them up or wait for you to mail the devices back to them). You and your patients will have to determine how much effort you want to expend to achieve this end.
Unitron devices can be remotely programmed after the fact, as long as the devices had at some point been connected to the TrueFit Software (version 4.3).
Although Widex hearing aids don’t need to be connected to software to activate this feature, the RemoteLink device does need to be paired to the patient’s file in the Widex GPS software before remote programming is possible.
Oticon, Phonak, and GNResound devices can participate with remote programming without having this feature activated in the software, although all do require some form of a “first fit” at some point prior to remote programming. This could be done without the patient present.
16. I’m worried that patients will feel less satisfied if they don’t receive face-to-face service.
You can rest assured that there are several recent studies indicating that many patients feel that remote and face-to-face care are similar. Note that there are different ways to provide remote hearing aid programming (e.g., in some instances, patients used proprietary distance support equipment [this means they had specific software installed on their computer and a programming device that allowed them to connect with their audiologist] rather than the cloud-based remote programming that is common today).
The VA in particular has been employing telecare for several years. Gladden, Beck, & Chandler (2015) reported that, in this population, outcomes for the remote programming delivery model were similar to face-to-face encounters in all outcome measurement areas, including satisfaction. Research also has revealed that for experienced hearing aid users, speech perception ability and self-reported hearing aid benefit were not significantly different when using the device settings that were programmed in-person and remotely (Venail et al., 2019). Other studies have shown that 80% of the remote appointments were perceived to be as effective as in-person appointments (Angley, Schnittker, & Tharpe, 2017) or that they are comparable (Tao et al., 2020).
Froehlich, Branda, & Apel (2018) described a field study in which hearing aid users rated their satisfaction related to their performance in specific situations before and after a home trial period that included remote programming options. On a scale from 1 (extremely dissatisfied) to 7 (extremely satisfied), participants displayed a nearly two-point improvement in satisfaction for certain problematic situations before and after the home trial. Notably, 70% of situations received a highly satisfied rating following remote programming intervention.
Additionally, remote cochlear implant programming was approved by the FDA in 2017. A few recent studies indicated that hearing outcomes obtained following remote programming of cochlear implant devices were comparable to those from in-person sessions. Importantly, the CI users reported similar subjective benefit and satisfaction (Slager et al., 2019; Luryi et al., 2020).
These findings do not only apply to hearing aid or cochlear implant recipients – Jorgensen et al. (2019) reported that significant improvements were experienced by caregivers of patients with hearing loss and mild dementia following remote programming use in the form of reducing caregiver stress and burden.
17. I am not confident that all my patients will be able to communicate with me via video chat. Can we communicate by some other means?
Currently, no manufacturers employ live communication captions for these live, synchronous interactions, but a few of the manufacturers (GN ReSound, Oticon, Signia, Starkey) do provide a chat box that can be utilized to enhance communication if the patient has difficulty hearing you or if there are any microphone/speaker issues on either end.
18. How do you decide which patients are good candidates for remote programming and which ones are not? Or do you just assume that everyone is?
Anyone who does not own a smartphone or use hearing aids that are connected to their smartphone via some type of Bluetooth connection will not be able to participate, so in these cases, the decision is made for you. Additionally, patients without access to a stable internet connection will also not be able to connect remotely. Some patients who struggle with technology may have difficulty completing all of the necessary steps, but you can provide them with very specific instructions if you are concerned that they will not be able to figure out what to do on their own. In some instances, it truly is as simple as them consenting to telecare (which they can do in your office if they need your help) and then answering an incoming phone call. If you run into problems connecting, there are some troubleshooting steps that you can suggest to them (e.g., delete and re-install the app, reboot their phone, make sure they have allowed access to their camera and microphone through the app). If worse comes to worse and you aren’t able to connect with them remotely, you can bring them into your office and try to complete a remote session there (with both of you present in-person). This way, you’ll be able to see exactly what they are doing and address any issues that you are able to identify.
19. Since I’m almost out of questions, here comes the big one: How will I get paid for my time?
This is something you will have to think about. Some audiologists may choose to institute a private-pay charge for tele-services. Others may choose to simply apply the same fee structure that would have applied if the patient was seen face-to-face in their office—in many cases this service has been bundled into the cost of the hearing aids. Either way, if you are planning to collect money from patients directly for remote programming services, you will need to establish a way for them to pay you. This could happen when the appointment is scheduled or after the appointment has taken place. Your front desk staff may collect credit card information over the phone, charge the patient, and mail or e-mail the receipt. You also may choose to generate a bill that the patient will receive after the fact.
You’ll want to keep up with rules around billing and reimbursement for tele-audiology services. This continues to change, so this link will help you connect to the most recent information: AAA Telehealth Guide. Additionally, American Academy of Audiology Members can contact the Coding & Reimbursement committee with questions about providing audiology services via telehealth (reimbursement@audiology.org).
20. I am not sure that I am up for this. If I just ignore it, will it go away?
I don’t think so. Patients have had a taste of tele-audiology and many will expect to continue to access some services like small programming changes remotely. There are all sorts of reasons that might make it difficult for a patient to come into the clinic in person during the years of their hearing aid journey. Hopefully, what we’ve talked about here will give you an idea of the information you’ll need in making your plan for providing remote programming care.
As promised, I've included a summary of information and some helpful links for remote programming with the major hearing aid manufacturers - access the Summary Guide here. If the links in the Summary Guide do not work or become outdated, you can also access the PDF versions of all the individual manufacturer guides from this Google Drive link.
References
Angley, G.P., Schnittker, J.A., & Tharpe, A.M. (2017). Remote hearing aid support: The next frontier. Journal of the American Academy of Audiology, 28(10), 893-900.
Froehlich, M., Branda, E., Apel, D. (2018). Signia TeleCare facilitates improvements in hearing aid fitting outcomes. AudiologyOnline, Article 24096. Retrieved from www.audiologyonline.com
Gladden, C., Beck, L., & Chandler, D. (2015). Tele-audiology: Expanding access to hearing care and enhancing patient connectivity. Journal of the American Academy of Audiology, 26(9), 792-799.
Jorgensen, L., Van Gerpen, T., Powers, T.A., & Apel, D. (2019) Benefit of using telecare for dementia patients with hearing loss and their caregivers. Hearing Review, 26(6), 22-25.
Luryi, A.L., Tower, J.I., Preston, J., Burkland, A., Trueheart, C.E., & Hildrew, D.M. (2020). Cochlear implant mapping through telemedicine - a feasibility study. Otology & Neurotology, 41(3), e330-e333.
Muñoz, K., Nagaraj, N.K., & Nichols, N. (2020). Applied tele-audiology research in clinical practice during the past decade: a scoping review. International Journal of Audiology, 1-9. DOI: 10.1080/14992027.2020.1817994
Saunders, G.H., & Roughley, A. (2020). Audiology in the time of COVID-19: practices and opinions of audiologists in the UK. International Journal of Audiology, 1-8. DOI: 10.1080/14992027.2020.1814432
Slager, H.K., Jensen, J., Kozlowski, K., Teagle, H., Park, L.R., Biever, A., & Mears, M. (2019). Remote programming of cochlear implants. Otology & Neurotology, 40(3), e260.
Tao, K.F., Moreira, T.D.C., Jayakody, D.M., Swanepoel, D.W., Brennan-Jones, C.G., Coetzee, L., & Eikelboom, R.H. (2020). Teleaudiology hearing aid fitting follow-up consultations for adults: single blinded crossover randomised control trial and cohort studies. International Journal of Audiology, 1-12.
Venail, F., Picot, M.C., Marin, G., Falinower, S., Samson, J., Cizeron, G., ... & Puel, J. L. (2019). Speech perception, real-ear measurements and self-perceived hearing impairment after remote and face-to-face programming of hearing aids: A randomized single-blind agreement study. Journal of Telemedicine and Telecare, 1357633X19883543.
Wosik, J., Fudim, M., Cameron, B., Gellad, Z. F., Cho, A., Phinney, D., ... & Tcheng, J. (2020). Telehealth transformation: COVID-19 and the rise of virtual care. Journal of the American Medical Informatics Association, 27(6), 957-962.
Citation
Zitelli, L. (2021). 20Q: Remote hearing aid programming - getting started. AudiologyOnline, Article 27750. Available at www.audiologyonline.com
