From the Desk of Gus Mueller
From the Desk of Gus Mueller

Anybody out there old enough to remember the late 1970s? Sony introduced this device called the “Walkman,” people were dancing to the Bee Gees’ top hit “Stayin’ Alive,” and there was my favorite happening...on October 14th, 1978, Jimmy Carter signed the bill legalizing small-batch beer brewing, the event that triggered the opening of microbreweries across the U.S.
In the world of fitting hearing aids, this was the time frame when we finally realized that repeated speech testing as a form of verification was not valid or reliable, and we were quickly moving on to using prescriptive fitting methods, with the Berger method the prescription du jour. This approach, of course, required the use of soundfield function gain to determine if prescriptive targets were being met—an unreliable measure, but all we had.
In 1979, word started to spread that Dave Preves of Starkey Labs had developed a method to use a hearing aid microphone in the ear canal, connected to the Frye (Fonix) test system, to assess the real-ear gain of hearing aids. Within a few years, a probe-tube version of this procedure became available from several manufacturers, and we were off and running—functional gain measures were in our rear-view mirror. That was 40 years ago!
To some extent, many aspects of today’s probe-mic verification procedures are the same as they were back then, but also, due to changes in hearing aid processing, prescriptive fitting approaches, and advances in the equipment itself, there have been several changes. Today, what has become routine, is to use a speech-shaped input signal and verify to soft, average and loud validated prescriptive targets using the real-ear aided response, followed by an MPO verification with swept tones. But is “routine” always good enough? Is there another level of verification to consider? I think so, and so does this month’s 20Q guest author.
Susan Scollie, PhD, is a Professor in the School of Communication Sciences and Disorders and the Director of the National Centre for Audiology at Western University. Dr. Scollie is internationally known for her work related to the pediatric patient, as is the work of many others from her research group. In addition to all her research efforts, she also is actively involved in the audiology training program at Western and recently was honored for her teaching excellence.
Of course, one cannot mention Western University or Susan Scollie without thinking of the DSL hearing aid prescriptive method. As most of you know, this approach was developed by Richard Seewald in the early 1980s, and has been revised in subsequent years as technology changed and additional research findings became available. Since the V5.0 revision in 2005, the face of the DSL has been Dr. Scollie. Last year, Dr. Scollie and her team were honored by receiving the Governor General’s Innovation Award for developing this fitting approach. In case you’re curious, the Governor General is Canada’s head of state, and the representative of the Queen/King, so seems to me this is a pretty big deal!
So, sit back, think good thoughts about the Governor General and Jimmy Carter, and let Susan take you to the “next level” of hearing aid verification in her excellent article.
Gus Mueller, PhD
Contributing Editor
Browse the complete collection of 20Q with Gus Mueller CEU articles at www.audiologyonline.com/20Q
20Q: Next-Level Hearing Aid Verification
Learning Outcomes
After reading this article, professionals will be able to:
- Describe how to link speech-based hearing aid verification to normative data and initial evaluation of aided outcomes of clarity and loudness.
- Describe at least two advantages of using headphones for real-time listening.
- Identify specific test strategies for specific hearing technologies, including frequency lowering, bone conduction hearing aids, and streaming.

1. What exactly do you mean by next-level verification? When I think about verifying hearing aids, I think about fitting to a validated prescription to make sure that I’ve provided beneficial speech audibility. Is there more to it?
I think there is a lot more to it! Sometimes, it seems like “verification” gets thought of as just running a wiggly line through some targets because we’re supposed to do that. But really, a good hearing aid analysis can provide a whole lot more. We can certainly start with ensuring smoothness, bandwidth, and good speech audibility, and fitting to targets throughout a period of acclimatization is a great way to do that. In fact, we’ve had strong evidence (Almufarrij et al., 2021, 2022; McCreery et al., 2017) and protocols (APSO, 2021; Bagatto et al., 2016; Sanchez et al., 2020) to support the idea that this is the foundation of a good hearing aid fitting. Studies indicate that clinician fitting and fine tuning improves fit to targets (Folkeard et al., 2020, 2018). Hearing aid users value good speech quality and clarity as important factors in their outcomes and preferences, and sometimes these factors are also related to specific hearing aid features such as phone compatibility and/or streaming (Picou, 2022; Saleh et al., 2021). There are a lot of features to fit on today’s hearing aids. Fortunately, hearing aid analyzers do a lot more than just measure speech in quiet, so especially when I’m teaching, I’ve been thinking about how we can maximize our use of verification equipment to meet the needs of the patients we serve and to improve our understanding of how hearing aid technologies work.
2. Well, that all sounds great, but hearing aid verification isn’t really a new topic. Why are we talking about it today?
I’ve noticed increased interest in hearing aid verification recently, for example, in the content at professional meetings. Particularly, if I compare the emphasis on verification now, to the historical low point in the early 2000’s, things have changed a lot. Twenty years ago, many clinicians had concerns about validity in verifying “digital” hearing aids, turning instead to fine tuning within the fitting modules without a verification crosscheck. The reliance on fitting modules opened the door to a concerning amount of variability in fittings provided from different companies for the same audiogram. Professional associations recommended that we verify to bring this back into the control of the fitter. But concerns with using verification persisted.
3. What were the concerns at that time?
Well, some early digital hearing aids had the first noise reduction systems ever on the market. Some could not be disabled, and even if they could be disabled for testing, it was not common practice to do so. Today that would be ok, because our modern speech-based verification can successfully test the gain and output of hearing aids for speech in quiet whether the noise reduction is on or off – it just doesn’t matter anymore. But back then, most of the non-speech noises and tones that we were using for verification were treated as noise by the hearing aids and were subsequently attenuated. Sometimes, this was such a problem that it was not possible to tune the aids to targets with these test signals.
In the figure below (Figure 1), I’m showing a hearing aid that I tested in the early 2000’s with a clinical steady-state speech-shaped noise signal (in green) and with calibrated speech (in black). You can clearly see that the speech-shaped noise does not provide a good estimate of speech output. What you can’t see is that the gain of the hearing aid changed over the first few seconds of the testing. This is mainly due to the noise reduction system in this hearing aid, which was turned on for this test. That’s fine if you are actually testing noise reduction – something we can talk about later – but recall that at this time we mostly use hearing aid analyzers to run ANSI tests and to fit to targets for speech in quiet. When we saw these results, fitters were concerned about test validity. Papers describing these concerns (Kuk, 2003) and providing evidence of the magnitude of the problem (Scollie & Seewald, 2002) were available at that time. Other unhelpful factors included widespread use of insertion gain verification, which does not show the mapping of audibility onto the listener’s dynamic range (Moore, 2006). Today, we verify with calibrated speech in SPL (sometimes called speech mapping) and avoid insertion gain, so these issues are no longer a concern with modern high-quality verification equipment.
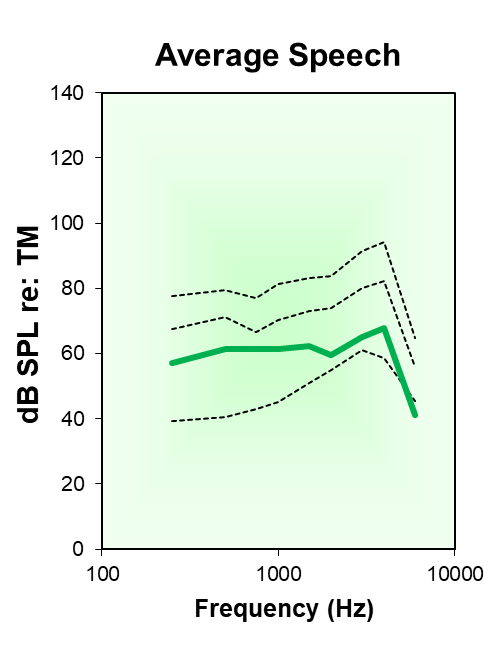
Figure 1. Example of aided speech output (- - -) for a hearing aid with active noise reduction. The top, middle, and bottom black lines represent the spectra for speech peaks, long-term average, and valleys. The middle dashed line can be compared to the solid green line, which is the hearing aid’s response to steady-state, speech-shaped noise.
4. It seems like we’ve made a lot of progress. What kind of changes have you noticed?
The biggest change has been the implementation of hearing aid analyzers that test hearing aids with calibrated speech, along with standardized analyses of the aided speech signal (Holube et al., 2010). This enables use of the now-widely-implemented Speech Intelligibility Index (ANSI, R2020; Scollie, 2018). Our industry has now developed modern verification systems with calibrated speech and consistent displays that map speech audibility, and provided advanced tests of signal processing. These advances have made some much-appreciated improvements over where we were a few decades ago. These days, we have normative data for fits to targets and aided SII that can help us to characterize how well-fitted our hearing aids are (Dao et al., 2021; Moodie et al., 2017). This is a measure of clinical service quality that clinicians and students find helpful as a learning tool, a counseling tool, or both. Some have begun to look at SII metrics as predictors of hearing aid outcome, linking the quality of the fitting to the long-term benefits of hearing aid use (McCreery et al., 2013). An example of how this is used in a typical hearing aid fitting is shown in Figure 2. Shown here are two moderate-gain fittings, fine tuned to the DSL v5-adult targets.
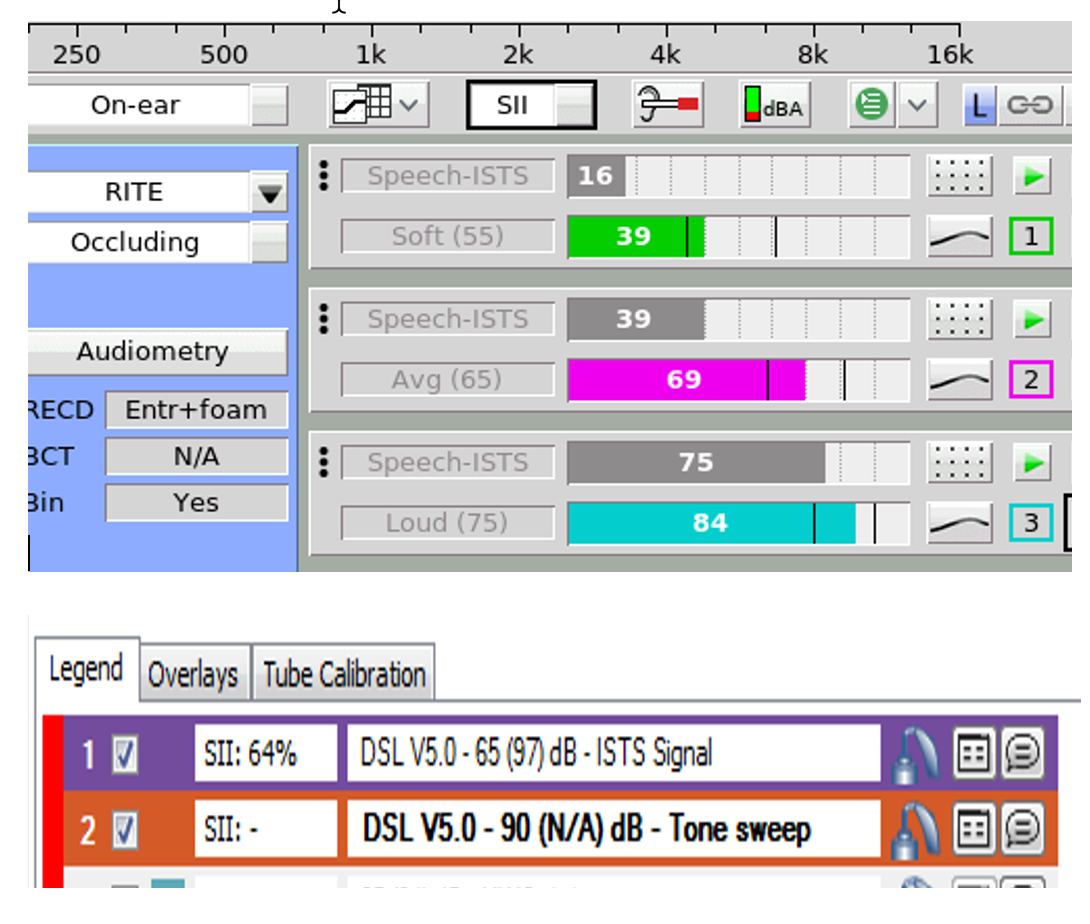
Figure 2. Example of aided Speech Intelligibility Index (SII) values, expressed as a percentage, for two different hearing aid fittings conducted on two different verification systems. In the top pane, grey bars indicate unaided SII and colored bars indicate aided SII in Tests 1 and 2, and vertical black bars indicate the normative range for the aided value (Audioscan Verifit 2). In the bottom pane, an aided SII of 64% is shown on Test 1, along with the unaided test level (65 dB) and the aided overall level of speech (97 dB) (Otometric Aurical PMM).
5. Those are some great technical advances, but with everything going on with OTC hearing aids right now, do you think that maybe that is the real reason why people seem to be interested in verification again?
It’s probably a big factor. At professional meetings these days, it can seem like most hearing aid sessions are about OTCs. I see an increased emphasis on best practices for clinician-based services, including routine in-ear hearing aid verification. Some argue that we need to strive for optimized outcomes to differentiate clinician-based services from the direct-to-consumer service model. Interestingly, even in sessions about direct-to-consumer hearing products, I’ve noticed professionals using their verification equipment to assess new devices such as OTCs, hearables, and other direct-to-consumer hearing products. My hearing aid analyzer is the first thing I reach for as well, when a new device comes along. Hearing aid analysis is a great tool to help us understand the potential and the limitations of new products in this time of change. Effective use of our in-clinic equipment may help us to provide better advice to our patients. There’s just no replacement for a good-quality analysis of hearing aid output and signal processing.
6. I couldn’t agree more! So, in your opinion, what makes a good-quality verification?
Modern hearing aid analyzers now use well-standardized speech signals and speech analysis strategies. This means that even if a hearing aid fitting is verified on two different brands of analyzers, clinicians should expect to see a very similar and clinically equivalent result, at least for speech in quiet verification. Essentially, there is a tried-and-true speech analysis originally developed for use at Bell Telephone Labs for the Articulation Index, and it laid the foundation for how to measure speech reliably (Dunn & White, 1940). Later, Robyn Cox and Denis Byrne described how it could be used to describe the spectral shape and dynamic range of speech passages for use in Audiology contexts (Cox, Mateisch, & Moore, 1988; Cox & Moore, 1988; Byrne et al., 1994), but it wasn’t available yet for use in hearing aid analysis until the first Audioscan Verifit system was launched in the early 2000’s. Percentile-based speech analysis was later picked up for use in European hearing aid test standards, together with the development of the International Speech Test Signal (ISTS: (Holube, Fredelake, Vlaming, & Kollmeier 2010). The ISTS and its inclusion in new test standards led to wider implementation of equivalent speech analysis by most hearing aid verification systems. Because the ISTS is unintelligible in any language, monolingual passages have also been developed that are matched in level and shape to the ISTS (Garolla et al., 2013). Monolingual passages are important: we can play a passage to a patient that they can understand, which creates a very interesting bridge between verification and validation of the fitting.
7. Validation? I thought we were talking about verification.
We are, but validation is all about making sure that aided benefit and outcomes are acceptable. So why do we verify? Good verification results should lead to good outcomes, right? One study demonstrated that providing better-quality fittings (through real-ear measurement) not only gave more benefit, but influenced how patients felt about the services they received (Amlani et al., 2017). What’s the link between verification and outcomes? Certainly, fitting to targets aims to provide a beneficial amount of aided audibility. But there’s something more going on here. Let’s think about why verification might be meaningful to the patient themselves. They see you fine tuning their aids with a computer, and as you make changes they hear the differences. Remember, you are using a calibrated, reliable, repeated speech passage. Because that stimulus is consistent, they can hear how the sound produced by the hearing aids changes as you fine tune. Because the stimulus is real speech, you can ask them if that speech is clear, comfortable, and balanced between ears. Speech-based verification makes our services observable to the hearing aid wearer. They can understand that hearing aids are highly adjustable, which I think encourages partnership and communication. Co-designed rehabilitation strategies are a hot topic, and maybe it’s time we started thinking about patient-centred hearing aid verification as part of that. We know that groups like the Ida Institute have been advocating for patient-centred care for many years. If you read their guide on Partnering for Great Hearing Care, one of the recommendations is to acknowledge that “your client is an expert about him/herself and treat your client like a teammate” (Ida Institute, 2022). Let’s think about what that means during the technology-heavy processes of hearing aid verification and fine tuning. At the heart of those procedures, we want to ensure that the hearing aid is tuned to provide clear, comfortable sound, intelligible speech, and good loudness balance between the two ears for bilateral fittings. In many cases, the best information available on these outcomes is the patient’s own opinion. Experts recommend that we need to break down the power dynamic (Ida Institute, 2022; Ryall et al., 2021) between clinician and patient in order to create a partnership. Maybe that’s about letting the hearing aid user be the expert about their own perception of aided sound.
8. Well, I’m all in favor of patient-centred practice, but how do we use verification equipment to partner with hearing aid users?
First, recognize that the graphical displays are really designed more for us than for the patient. Hearing aid users find them confusing and appreciate clear explanations of what we are doing with all of our wiggly lines and buttons: the information provided might be overwhelming and stressful (Ryall et al., 2021). Second, remember to put the patient in charge of whether the hearing aid is providing them with good access to sound. Third, most verification equipment now comes with high-quality headphones that let you listen to the hearing aid output from the probe-tube microphones. Consider the impact of telling the patient, “Let’s listen to your hearing aids together, and you tell me how they sound to you.” while you put the headphones on? The purpose of those headphones doesn’t need a lot of technical explanation. Letting them tell you about their experience of loudness, clarity, and balance while you listen and fine tune together creates partnership (See Figure 3). This simple act of co-listening puts the patient in charge.

Figure 3. Hearing healthcare professional co-listening to telecoil-transduced speech, together with the hearing aid wearer. Both are able to hear the aided sound at the same time.
9. So, are you saying that the patient should get to decide their own fitting? What about targets?
Hey, I’ve got no problem with targets. What I’m thinking about is patient-centred, outcomes-oriented verification in which we ask the patient about their own perception of aided sound, and use that together with prescriptive targets and our professional knowledge. Adjusting for preference doesn’t always mean a poor fit to targets – we can often achieve both together, and modern evidence-based protocols include the use of both a prescription and fine tuning to patient preference.”(APSO, 2021; Polonenko et al., 2010; Sanchez et al., 2020). Besides, there are other benefits to listening to hearing aids over headphones; we also want to make listening accessible and comfortable not only for the hearing aid wearer, but for the clinicians as well, who themselves have diversity of hearing.
10. I like accessibility and comfort! Tell me more about that.
Well, I think most of us have tried to do listening checks of hearing aids through listening tubes. I don’t know about you, but I often encounter more feedback on the listening tube than is produced in the patient’s ear. I find that, and the loudness of the hearing aid through the tube to be uncomfortable. I also know that I’m listening to the hearing aid through long tubing with resonances from the tubing, and even with a damper in the tube it really is not a good representation of what the aid produces in the patient’s ear. The levels for high power fittings can be uncomfortably loud for clinicians who do not have hearing loss, and tube-based listening headsets are not an accessible solution for clinicians and trainees who use hearing technologies themselves, like hearing aids or cochlear implants. These are all big problems, but there is an alternative. Headset jacks on many hearing aid analyzers route the output from the test microphone(s) to headphones that the clinician can wear, with a volume control adjustment. These are provided to help you listen to the hearing aids at a comfortable volume if you have normal hearing sensitivity. However, those headphones and/or the headphone jack can also help to provide accessibility for clinicians or trainees who use hearing aids or cochlear implants. It just takes a little bit of creativity. I’ve been routinely pulling them into my classroom for several years now. For my students who use hearing aids or cochlear implants, we try either putting the headphone on, over their own devices’ microphones – this is a low-tech solution that I learned from one of my students who liked to listen to music this way. For a higher-tech solution, we patch the headphone jack output to their personal remote microphone system. This wirelessly sends the aided signal directly to their own hearing devices. We take turns listening to the fitting, to determine whether we are both hearing output, sound quality, distortion, feedback, hearing aid signals, and the various sounds of speech during listening checks. This builds confidence as they learn that their listening check results are the same as mine. Either the headphone solution or the remote mic patching solution can provide access to listening check. This is an important accessibility factor in my classroom, as I assume it would be in the workplace.
11. Ok, I get it. You skip the stethoclip and use headphones instead. What are you listening for?
Great question. At a basic level, you can listen for good sound quality, low noise floor, and lack of distortion or intermittency. While you are fine tuning you can ask about loudness and clarity and balance between ears, while you are also listening. You can even listen for occlusion effect problems while measuring the patient’s own “eee” productions. You can get a lot of information from your own ears, pick up unexpected problems, and learn what hearing aids should sound like. Most prescription hearing aids these days have clean signal processing, reasonable bandwidth, and smooth frequency responses – essentially, good hearing aids should sound good. Especially in our current era of regulated versus non-regulated hearing products, knowing what good versus bad signal processing sounds like has never been more relevant.
12. I’ve heard that frequency lowering can affect sound quality. What do you do differently for those fittings?
If you are fitting more advanced technologies, you can use listening checks together with verification, to both measure and hear how a frequency lowering processor is affecting the speech signal. In studies, we see poorer sound quality with strong settings, but this effect is reduced if the aids use moderate settings and/or adaptive processing (Glista et al., 2019). Our three step procedure is: 1. fit the device to targets with frequency lowering disabled, in order to get the most out of the aid’s gain and therefore minimize how much lowering is needed; 2. If necessary, enable the frequency lowering and tune it for strength using a synthetic “s”; and 3. play running speech through the combined fitting and listen for clarity, paying special attention to settings that maintain vowel quality and that let you hear the difference between “s: and “sh”. The example below (Figure 4) shows three different strengths of frequency lowering, with “A” being too strong, “B” being just right, and “C” being too weak. If possible, co-listen with your patient and assess their perceptions and preferences. This strategy is described in detailed fitting protocols and has been tested for good outcomes and sound quality (Glista et al., 2017, 2019). The synthetic /s/ stimulus (Scollie, Glista, et al., 2016) is widely available for use in clinics.

Figure 4. Sample hearing aid fitting displayed on an Aurical PMM hearing aid analyzer. The lower grey shaded region is the area at and below the listener's thresholds. The three colored spectra are the synthetic /s/ stimulus, at hearing aid settings with frequency lowering at three different strengths. The “B” setting was the chosen setting: it is the weakest setting that places /s/ within the hearing aid user’s auditory area.
13. How about listening over headphones to determine the effects of noise reduction?
Great point. With a verification system and headphones, you can measure the hearing aid’s response to a noise signal and at the same time see and hear how slowly or quickly a noise reduction system takes to activate. Noise reduction systems vary a lot in their activation time and strength (Scollie et al., 2016). Verifying the degree of noise reduction provides good insight into the hearing aids’ adaptive behavior. This can help you determine if you have tested the noise reduction at full strength or whether it was still adapting. Knowledge of noise reduction activation speed can help you to counsel the patient on what to expect. On the other hand, how strong is the noise reduction system once it is activated?
As example of how you might examine this is shown in Figure 5. As shown, the noise reduction system reduced pink noise by 7 dB and multitalker babble by 4 dB. If a wearer was having loudness challenges in noisy places, running this test would let me see how strong the noise reduction is currently, and help me decide if I need to find a stronger setting, as part of providing an effective noise management strategy in the fitting. This type of testing is also popular when new hearing aids are released, as a way of getting to know what signal processing options they provide.
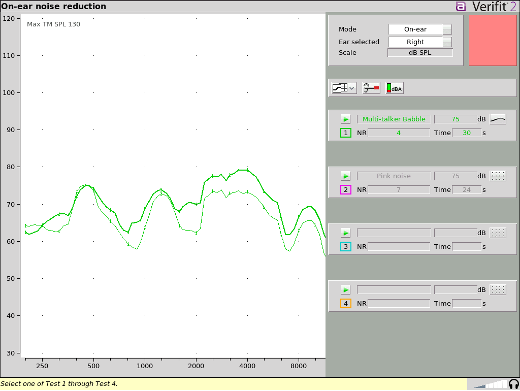
Figure 5. Sample noise reduction testing, completed with the Audioscan Verifit2 system. Test 1 indicates that the hearing aid can successfully reduce high-level multitalker babble by 4 dB (green spectrum) while Test 2 measured a 7 dB reduction for pink noise (spectrum not shown). The timer in each test allows the tester to time how long the hearing aid takes to reach maximum effect.
14. You haven’t mentioned feedback reduction systems. Do you have a method to check them out?
Verification headphones are also great for detecting feedback problems. If you listen while you fit, you can become aware of feedback during fitting more easily. This is especially true if the feedback is low-level or intermittent, which can easily be missed while fine tuning. The aided peaks arising from undetected feedback may look like the hearing aid is over target, when the real problem that needs solving is the feedback itself. An example of this is shown in Figure 6. The large peak just above 2000 Hz is actually feedback. If you listen with the headphones, you can hear the feedback happening, so you know that this is not just a gain peak that needs fine tuning. This can save time by helping you target your hearing aid adjustments to the correct type of re-programming.
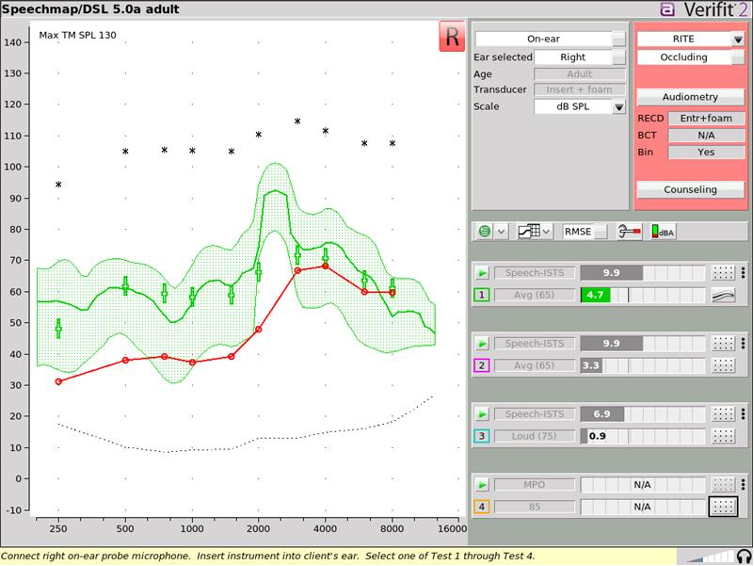
Figure 6. Real ear aided response for a speech signal presented at 65 dB SPL. Wearing headphones, the fitter was able to hear that the hearing aid was producing intermittent feedback during the fine-tuning session. The large peak above 2000 Hz is the acoustic feedback.
15. I’m starting to become of fan of co-listening! Any other benefits?
There are a few. First, unless we routinely listen to hearing aids while we are programming, we can become blissfully unaware of how often they go mute while a program is loading. Co-listening can help you know when to pause while talking to the patient rather than continuing as though the aids are still on. Second, listening while pairing to a phone or remote microphone is incredibly helpful: you can hear the pairing signals produced by both devices and do a better job of getting them paired quickly, as well as coaching the patient on how the devices work together. What you observe while listening can then be compared to objective measures—an example of alert signal measurement is shown in Figure 7. This can help improve ease of use, which is important for today’s app-controlled features (Saleh et al., 2021).
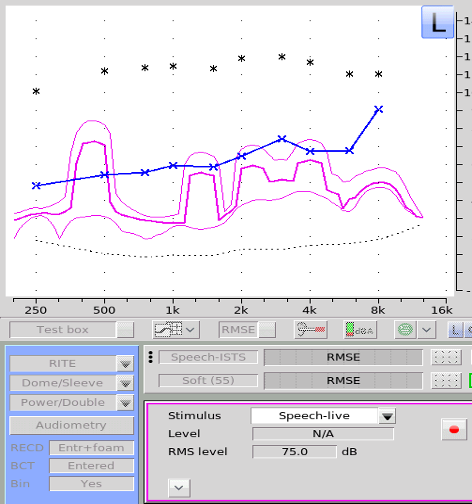
Figure 7. Verified levels of a hearing aid's user alert signal that a program change has occurred. The lowest-frequency component of the chime is just below 500 Hz and is well above the listener’s threshold. The higher-frequency portions of the chime are lower in sensation level. If the listener had difficulty hearing the chime, it could be adjusted to a louder level to improve awareness of this alert.
16. Sounds like this headphone-listening procedure can avoid some pitfalls with verification and fine tuning of apps and streaming. Any recommendations?
In addition to listening over headphones while pairing, and verifying, it’s a good idea to brush up on how different music is from speech. Remember that those targets we like to use are really only for speech – music needs more bass and less treble (Vaisberg et al., 2021). These days, so many of our fittings tend to be open fit, so for listening to speech and other environmental sounds, we provide the low frequencies as unaided, vent-transmitted sound. But consider that none of the vent-transmitted bass will be available in the streamed program, so you have to add back in that low-frequency gain or the streamed voice and especially streamed music will sound thin and/or tinny. Here’s an example (see Figure 8): the open-fit device looks to have a good low-frequency response, but the real ear occluded response confirms that this is mostly from unaided, vent-transmitted sound. We tested the default music streaming program by pairing to the user’s phone and playing music while measuring the output with the hearing aid analyzer. The wearer felt that the music was tinny, which agreed with how the stream sounded over headphones. To fix this, we adjusted the low-frequency gain to improve the bass response.
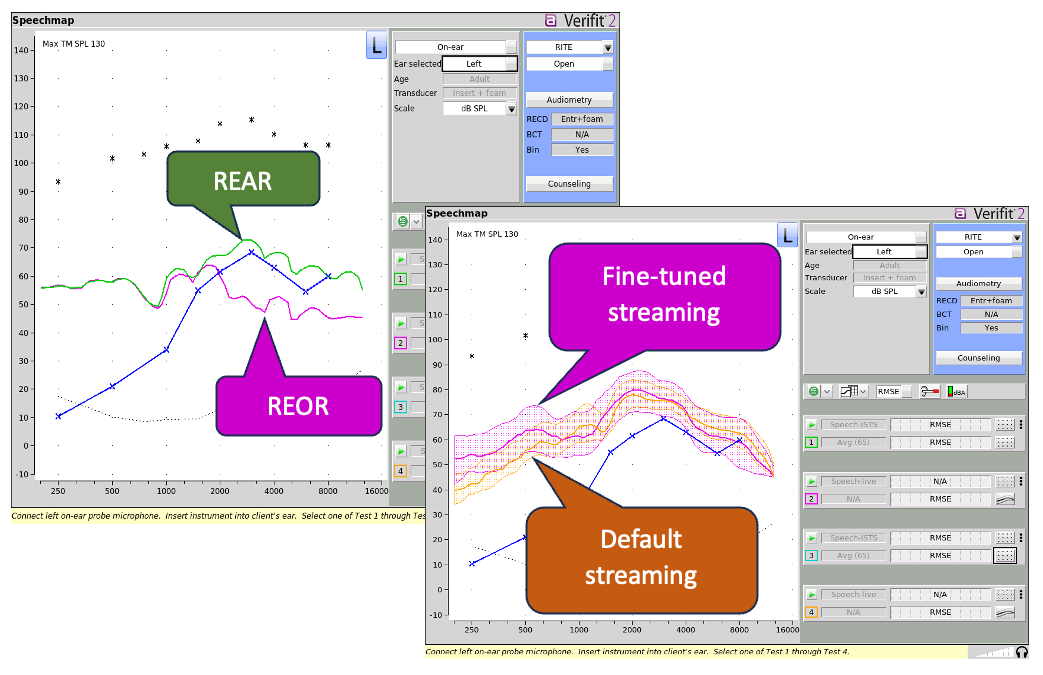
Figure 8. Top left pane: On-ear verification of an open-fit hearing aid's response to speech when on (REAR) and when muted (REOR). This illustrates that the aid is open to almost 2000 Hz. Bottom right pane: The same open aid was tested for streamed music to check audibility, bass response, and perceived sound quality. It provided the orange response at default settings for streamed music. A bass-boosted response was provided in fine-tuning, as shown by the magenta curve.
17. How about more specialized fittings, like fittings for bone conduction hearing aids?
Listening checks with bone conduction hearing aids can be really tough. I’ve had various strategies suggested to me over the years, including using a bite bar and touching the abutment to my tragus or mastoid. These strategies do work to some degree, but involve a lot of either infection control (for the bite bar) or feedback (for on tragus or mastoid). I find that I can obtain a better, more comfortable listening check with the headphones and can quickly pair and check streaming for bone conduction hearing aids that offer connectivity, in addition to fitting to targets as shown in the example below (see Figure 10). I can also keep both hands free to handle and program the device if I am not holding it to my head while checking it. Of course, this requires a coupler-like device called a skull simulator, but these are now commercially available.
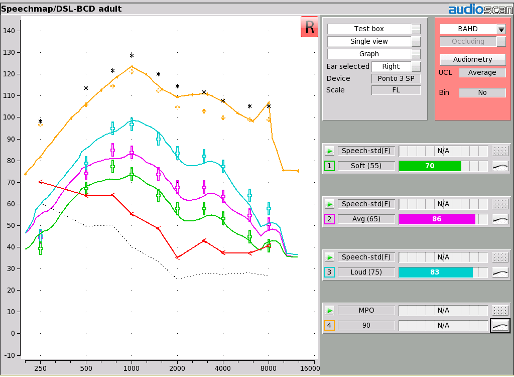
Figure 9. A verified fitting of a bone-anchored hearing aid, completed with the use of a skull simulator connected to a hearing aid analyzer. This is similar to fitting an air-conduction hearing aid on a coupler, because it is completed within the test box.
18. Another fitting arrangement that gives me verification problems is that of a CROS/BiCROS. Any guidance?
Measuring whether CROS or BiCROS fittings overcome head shadow is one of the main points when verifying these fittings—especially for the CROS. Over the headphones, you can really hear a clear loudness boost when you add in that CROS mic, and this helps to know that the transmission is successfully activated. You can also measure the combined output, with sounds played to the CROS mic and transmitted to the recipient ear. If you compare CROS off to CROS on, you get a clear measurement of head shadow versus CROS transmission. Most protocols recommend placing the speaker at a 45 degree azimuth on the CROS side for this step (Killion & Revitt, 1987), for best reliability. However, measuring CROS transmission from 90 degrees may maximize head shadow to help see the CROS activation. Either way, modern verification systems provide specialized CROS test modes that are designed for use in CROS and BiCROS real ear measurements, and provide good information about transmission from the CROS microphone to the recipient ear.
19. I’m almost out of questions, so I have to ask—how does all this relate to hearing aid fittings for infants and children?
Thinking back to the older ASHA and AAA protocols, we have had a nice workflow of Assess, Select, Prescribe, Verify, and Validate as the main steps to follow for about 20 years now. This overall sequence has largely been maintained in more recent protocols, including our newest update of the Ontario Infant Hearing Program’s Protocol for the Provision of Amplification (Bagatto et al., 2023). Within this, there are just a few critical variations for hearing aid fittings for infants and young children. At assessment, we can predict the infant’s behavioral audiogram from auditory evoked potentials, and corrections are sometimes necessary. We can expect early hearing aid fittings to be based on partial audiograms, with two to three thresholds per ear. We can expect ear canal acoustics to affect the assessment data, and also to change over time, and we can measure that and correct for each individual child, over time. At selection and prescription, children are typically provided with more gain. When verifying, younger children are more likely to have their hearing aids fitted on a coupler rather than on ear, and corrections for this can be measured and used. Verification and fitting of remote microphone systems are also more common in children, and requires the use of specific procedures. But other than these pediatric tweaks, the basics of hearing aid verification are really similar across ages, using the same equipment and principles. Regardless of patient age, we don’t verify to follow best practices. We verify to optimize outcomes. For pediatric fittings, we are more likely to be verifying in the coupler, but for many hearing aid analyzers, listening to the aids from within the coupler is also a possibility with verification headphones. As with the examples that I’ve already mentioned, this can speed up listening checks for the aids alone and the aids paired with remote microphone systems, because you can hear the pairing signals and the live microphone signals from both the aid and the remote microphone. Headphone demonstrations to parents can be effective for informational counseling and device use coaching. One suggestion is to use live voice listening to let parents hear their own voice as processed through their child’s hearing aids. For older children who receive on-ear verification, verifying on-ear, especially for open-fit hearing aid users (Kim & Ricketts, 2013) and co-listening may be effective once the child is developmentally ready. If they are not able to sit for real-ear verification, new corrections to simulate venting in the test box are a nice option to have ready (Pumford et al., 2021). We can use a variety of strategies depending on the specific patient’s needs and abilities.
20. Thanks for taking me to the “next-level” of verification. Anything I forgot to ask?
I think you covered most everything. I would like to add, however, that some of the tips we’ve talked about today can’t be done with pre-calibrated, pre-recorded test signals. Using a verification system that lets you turn off the test signal and measure the hearing aid’s response to real-world signals gives flexibility for special circumstances, streaming, and troubleshooting the unexpected. If you are shooting for the moon in your fittings, your best friend may be a fully-featured hearing aid analyzer that provides not only a lot of tests, but a lot of flexibility. If you have already invested in this type of system, I hope that these examples give you some ideas about getting the most out of your equipment in a patient-centered way.
References
Almufarrij, I., Dillon, H., & Munro, K. J. (2021). Does Probe-Tube Verification of Real-Ear Hearing Aid Amplification Characteristics Improve Outcomes in Adults? A Systematic Review and Meta-Analysis. Trends in Hearing, 25, 233121652199956. https://doi.org/10.1177/2331216521999563
Almufarrij, I., Dillon, H., & Munro, K. J. (2022). Do we need audiogram-based prescriptions? A systematic review. International Journal of Audiology, 1–12. https://doi.org/10.1080/14992027.2022.2064925
American National Standards Institute. (1997, R2020). Methods for calculation of the Speech Intelligibility Index, ANSI S3.5-1997. New York: Acoustical Society of America.
Amlani, A. M., Pumford, J., & Gessling, E. (2017). Real-Ear Measurement and Its Impact on Aided Audibility and Patient Loyalty. Hearing Review, September. https://hearingreview.com/hearing-products/testing-equipment/real-ear-measurement-impact-aided-audibility-patient-loyalty
APSO. (2021). S2.1 Hearing Aid Fitting for Adult & Geriatric Patients. Audiology Practice Standards Committee. https://www.audiologystandards.org/standards/display.php?id=102
Bagatto, M., Moodie, S., Brown, C., Malandrino, A., Richert, F., Clench, D., & Scollie, S. (2016). Prescribing and Verifying Hearing Aids Applying the American Academy of Audiology Pediatric Amplification Guideline: Protocols and Outcomes from the Ontario Infant Hearing Program. Journal of the American Academy of Audiology, 27(03), 188–203. https://doi.org/10.3766/jaaa.15051
Byrne, D., Dillon, H., Tran, K., Arlinger, S., Wilbraham, K., Cox, R., Hagerman, B., Heto, R., Kei, J., Lui, C., Kiessling, J., Kotby, M.N., Nasser, N.H.A., El Kholy, W.A.H., Nakanishi, Y., Oyer, H., Powell, R., Stephens, D., Meredith, R., Sirimanna, T., Tavartkiladze, G., Frolenkov, G.I., Westermann, S., & Ludvigsen, C. (1994). An international comparison of long-term average speech spectra. Journal of the Acoustical Society of America, 96, 2108-2120.
Cox, R.M., Mateisch, J.S., & Moore, J.N. (1988). Distribution of short-term rms levels in conversational speech. Journal of the Acoustical Society of America, 84, 1100-1104.
Cox, R.M., & Moore, J.N. (1988). Composite speech spectrum for hearing aid gain prescriptions. Journal of Speech and Hearing Research, 31, 102-107.
Dao, A., Folkeard, P., Baker, S., Pumford, J., & Scollie, S. (2021). Fit-to-Targets and Aided Speech Intelligibility Index Values for Hearing Aids Fitted to the DSL v5-Adult Prescription. Journal of the American Academy of Audiology, 32(02), 090–098. https://doi.org/10.1055/s-0040-1718707
Dunn, H.K. & White, S.D. (1940). Statistical measurements on conversational speech. Journal of the Acoustical Society of America, 11, 278-288.
Folkeard, P., Bagatto, M., & Scollie, S. (2020). Evaluation of Hearing Aid Manufacturers’ Software-Derived Fittings to DSL v5.0 Pediatric Targets. Journal of the American Academy of Audiology, 31(05), 354–362. https://doi.org/10.3766/jaaa.19057
Folkeard, P., Pumford, J., Abbasalipour, P., Willis, N., & Scollie, S. (2018). A Comparison of Automated Real-Ear and Traditional Hearing Aid Fitting Methods—Audioscan. The Hearing Review. https://hearingreview.com/hearing-loss/patient-care/hearing-fittings/comparison-automated-real-ear-traditional-hearing-aid-fitting-methods
Garolla, L. P., Scollie, S. D., & Martinelli Iório, M. C. (2013). Development of the speech test signal in Brazilian Portuguese for real-ear measurement. International Journal of Audiology, 52(8), 572–576. https://doi.org/10.3109/14992027.2013.791031
Glista, D., Hawkins, M., Bohnert, A., Rehmann, J., Wolfe, J., & Scollie, S. (2017). The Effect of Adaptive Nonlinear Frequency Compression on Phoneme Perception. American Journal of Audiology, 26(4), 531–542. https://doi.org/10.1044/2017_AJA-17-0023
Glista, D., Hawkins, M., Vaisberg, J. M., Pourmand, N., Parsa, V., & Scollie, S. (2019). Sound Quality Effects of an Adaptive Nonlinear Frequency Compression Processor with Normal-Hearing and Hearing-Impaired Listeners. Journal of the American Academy of Audiology, 30(7), 552–563. https://doi.org/10.3766/jaaa.16179
Holube, I., Fredelake, S., Vlaming, M., & Kollmeier, B. (2010). Development and analysis of an International Speech Test Signal (ISTS). International Journal of Audiology, 49(12), 891–903. https://doi.org/10.3109/14992027.2010.506889
Killion M, Revit L. Insertion gain repeatability versus loudspeaker location: You want me to put my loudspeaker WHERE? Ear Hear. 1987;8(5)[Suppl]:68S-73S.
Kim, H., & Ricketts, T. A. (2013). Test-Retest Reliability of Probe-Microphone Verification in Children Fitted with Open and Closed Hearing Aid Tips. Journal of the American Academy of Audiology, 24(07), 635–642. https://doi.org/10.3766/jaaa.24.7.11
Kuk, F. (2003, August 2). Changing with the Times: Choice of Stimuli for Hearing Aid Verification. The Hearing Review. https://hearingreview.com/practice-building/practice-management/changing-with-the-times-choice-of-stimuli-for-hearing-aid-verification
McCreery, R. W., Brennan, M., Walker, E. A., & Spratford, M. (2017). Perceptual Implications of Level- and Frequency-Specific Deviations from Hearing Aid Prescription in Children. Journal of the American Academy of Audiology, 28(09), 861–875. https://doi.org/10.3766/jaaa.17014
McCreery RW, Bentler RA, Roush PA. 2013; Characteristics of hearing aid fittings in infants and young children. Ear Hear 34 (06) 701-710
Ministry of Children, Community and Social Services, Ontario Infant Hearing Program (2023). Protocol for Provision of Amplification, version 2023.01. Editors: M. Bagatto & S. Scollie. Contributors: Moodie, S., Seewald, R., Hyde, M. El-Naji, R., Brown, C., Beh, K., Glista, D., Hawkins, M., Easwar, V., Tharpe, A.M., Crukley, J., Levy, C., Zimmo, S., Moodie, K.S., Richert, F., & Parsa, V. Accessed from: https://ir.lib.uwo.ca/nca/12/.
Moodie, S. T. F., The Network of Pediatric Audiologists of Canada, Scollie, S. D., Bagatto, M. P., & Keene, K. (2017). Fit-to-Targets for the Desired Sensation Level Version 5.0a Hearing Aid Prescription Method for Children. American Journal of Audiology, 26(3), 251–258. https://doi.org/10.1044/2017_AJA-16-0054
Moore, B. C. J. (2006). Speech mapping is a valuable tool for fitting and counseling patients. The Hearing Journal, 59(8), 26. https://doi.org/10.1097/01.HJ.0000286371.07550.5b
Picou, E. M. (2022). Hearing Aid Benefit and Satisfaction Results from the MarkeTrak 2022 Survey: Importance of Features and Hearing Care Professionals. Seminars in Hearing, 43(04), 301–316. https://doi.org/10.1055/s-0042-1758375
Polonenko, M.J., Scollie, S.D., Moodie, S., Seewald, R.C., Laurnagaray, D., Shantz, J., & Richards, A. (2010). Fit to targets, preferred listening levels, and self-reported outcomes for the DSL v5.0a hearing aid prescription for adults. International Journal of Audiology, 49(8), 550–560. https://doi.org/10.3109/14992021003713122
Pumford, J., Scollie, S., Folkeard, P., Pietrobon, J., & Abbasalipour, P. (2021). Vent Corrections for Simulated Real-Ear Measurements of Hearing Aid Fittings in the Test Box, AudiologyOnline. https://www.audiologyonline.com/articles/audioscan-vent-corrections-27884
Saleh, H. K., Folkeard, P., Van Eeckhoutte, M., & Scollie, S. (2021). Premium versus entry-level hearing aids: Using group concept mapping to investigate the drivers of preference. *International Journal of Audiology, 1–15. https://doi.org/10.1080/14992027.2021.2009923
Sanchez, V. A., Arnold, M. L., Reed, N. S., Oree, P. H., Matthews, C. R., Clock Eddins, A., Lin, F. R., & Chisolm, T. H. (2020). The Hearing Intervention for the Aging and Cognitive Health Evaluation in Elders Randomized Control Trial: Manualization and Feasibility Study. Ear & Hearing, 41(5), 1333–1348. https://doi.org/10.1097/AUD.0000000000000858
Scollie, S.D. (2018). 20Q: Using the aided speech intelligibility index in hearing aid fittings. AudiologyOnline, Article 23707. Retrieved from www.audiologyonline.com
Scollie, S. D., & Seewald, R. C. (2002). Evaluation of Electroacoustic Test Signals I: Comparison with Amplified Speech. Ear and Hearing, 23(5), 477–487. https://doi.org/10.1097/00003446-200210000-00009
Scollie, S., Glista, D., Seto, J., Dunn, A., Schuett, B., Hawkins, M., Pourmand, N., & Parsa, V. (2016). Fitting Frequency-Lowering Signal Processing Applying the American Academy of Audiology Pediatric Amplification Guideline: Updates and Protocols. Journal of the American Academy of Audiology, 27(03), 219–236. https://doi.org/10.3766/jaaa.15059
Scollie, S., Levy, C., Pourmand, N., Abbasalipour, P., Bagatto, M., Richert, F., Moodie, S., Crukley, J., & Parsa, V. (2016). Fitting Noise Management Signal Processing Applying the American Academy of Audiology Pediatric Amplification Guideline: Verification Protocols. Journal of the American Academy of Audiology, 27(03), 237–251. https://doi.org/10.3766/jaaa.15060
Vaisberg, J.M., Beaulac, S, Glista, D., Macpherson, E.A., Scollie, S.D. (2021). Perceived sound quality dimensions influencing frequency-gain shaping preferences for hearing aid-amplified speech and music, Trends in Hearing, 25, 1-17. https://dx.doi.org/10.1177/2331216521989900
Citation
Scollie, S. (2023). 20Q: next-level hearing aid verification AudiologyOnline, Article 28775. Available at www.audiologyonline.com