 From the Desk of Gus Mueller
From the Desk of Gus Mueller
Things change. A few of you remember fitting hearing aids in the 1960s and early 1970s, when for ethical reasons, audiologists were not allowed to sell hearing aids. The patient paid for a hearing aid evaluation, at which time the audiologist would conduct speech recognition testing with three (or maybe four) different BTEs from a stock of 20 or more that were on consignment. The “best” instrument would be selected based on the highest word recognition score—sometimes by a margin of only 2 or 4%--and the audiologist would then provide the patient with a list of dispensers in the neighborhood where the recommended product could be purchased. The patient was asked to schedule a follow-up visit so that the audiologist could give his or her “approval” to the overall fitting. Some patients returned, most didn’t.

Gus Mueller
A hybrid dispensing model emerged in the mid-1970s. The patient was referred to a “middleman,” who sold the hearing aids to the patient for only slightly more than wholesale, but didn’t do the fitting. This allowed for all fitting and follow-up to be conducted by the primary audiologist, who simply charged for services. Then, in the late 1970s, it became ethically okay for audiologists to sell hearing aids directly. Many initially tried a fee-for-service approach, but it was soon realized the consumers were accustomed to a bundled model, which actually was much simpler. That pricing scheme for hearing aid sales was soon adopted by most; this bundled model currently is used by 85% or so of audiologists.
But things change. Today we have internet sales of all types of hearing aids, and we have PSAPs, many of which are very much like a “hearing aid.” We have big box stores selling hearing aids, and we have manufacturers rapidly buying up practices. Can audiologists continue to use the dispensing model that has served them well for nearly 40 years?
While these current happenings are hot topics at cocktail party discussions, not too many audiologists want to share their views in print. Fortunately, one of audiology’s most reasoned thinkers was willing to do just that for this month’s 20Q. Robyn Cox, PhD, is Professor Emeritus at the University of Memphis, and Director of the Hearing Aid Research Lab (HARL; www.HARLmemphis.org). Her notable research spans four decades, and she has received numerous awards from journals for her work. She also has been named the prestigious Carhart Lecturer by the American Auditory Society, and has been awarded the American Academy of Audiology’s Career Award for Research in Audiology.
As most of you know, over her career Robyn has developed a lot of different tests, procedures and assessment tools, many of which have clever acronyms. Here at AudiologyOnline, we’d personally like to thank her for the AFAFF, APHAB, CONTOUR, CST, DOSO, ECHO, IOI-HA, MSU, PHAB, PHAP, RSIN, SADL, SIR, WICIT, VIOLA, and all the others we can’t remember. A tremendous contribution to our profession.
And things do change. As you might have gathered from the “Emeritus” in her title, Dr. Cox recently retired from the University, but tells us she will continue her research projects for a few more years. In fact, she gave us a glimpse of some of the findings from her most recent project in this 20Q article. So, sit back and enjoy reading the thoughts from one of the best, as Robyn gives us some ideas of how we might deal with all the changes around us related to hearing fitting and dispensing.
Gus Mueller, PhD
Contributing Editor
April 2014
To browse the complete collection of 20Q with Gus Mueller CEU articles, please visit www.audiologyonline.com/20Q
20Q: Hearing Aid Provision and the Challenge of Change

Robyn Cox
1. In the few years I’ve been practicing, I’ve noticed that a lot of what my professors taught about hearing aid fitting isn’t actually done in the “real world”. I’m okay using the fitting practices I’ve learned in my current job, and think I can make a decent living doing them. Why change?
Whether or not they fit hearing aids using accepted best-practice, I bet we could agree that many audiologists focus on selling as many high-cost premium hearing aids as possible in order to make a living. This focus needs to change because there are forces at work that oppose the status quo. To meet the coming challenges, audiologists of the future will have to change the way they do things if our profession is going to prosper rather than fade away.
2. Sure, I’ve heard other people saying that sort of scary stuff, but I think it’s just the same old gloom and doom. Exactly what kind of forces do you mean?
Pressures are rising because both consumers and research funders are asking for proof to justify the high costs of hearing aids.
Our baby boomer patients are more tech-savvy than their parents were. They have computers and smart phones and they access the Internet for information. They look at reviews, hearing aid websites, etc. Access to information – right or wrong – about hearing aids is greater than it used to be. These patients are value-conscious and increasingly aware of the different options they have in hearing devices, which we can talk about later. They believe that traditional hearing aids are expensive and they wonder if they’re worth it. Also, I assume you know about the Consumer Reports article in 2009 that reported on the journeys of several patients as they shopped for hearing aids. CR reported that the patients encountered “high prices … mediocre fittings … and lack of information.” Whether you agree with the report or not, it gave hearing aid practitioners, both audiologists and hearing instrument specialists, a black eye.
At the same time, there is growing public health concern about the low penetration level of hearing aids in the burgeoning population of older people. Policy makers and research funders have noticed that only 20-25% of older adults with hearing loss seek hearing aids, even though hearing aids could be helpful to them. In 2009, NIDCD sponsored a high-profile workshop to explore affordability and accessibility of hearing aids for adults with mild to moderate hearing loss. Since then, NIDCD has sought to fund research that could help to improve utilization of effective hearing health care for this group. All in all, agreement is increasing that our current status quo does not seem to be working very well for a lot of people. The time seems right for disruptive innovations to appear.
3. Disruptive innovation? What in the world is that?
Disruptive innovations are new ideas or products, or new ways of applying old ones, that shake up an existing market. Often disruptive innovations will come along when the market has become sluggish and there is a pent-up demand for products that is not being satisfied by the status quo. Sound familiar?
Disruptive innovations sometimes end up completely replacing earlier ways of doing things.
For example, when mass-produced, inexpensive automobiles were introduced in the early 20th century, they put a lot of horses out of business, not to mention the carriage makers and drivers. Another example is in the camera industry. Before about 2000, cameras were based on analog technologies and chemically developed films. Then low cost digital cameras came along with their advantages of being able to store hundreds of high quality pictures in a small memory card. Now the digital camera has almost totally replaced traditional film cameras. These were disruptive innovations.
4. Hmmm…Can you give me some examples in our field?
Sure, consider smartphones. The cellphone is not only a gadget for calling and texting, but also a platform that has great potential for applications in our field. For example, several major hearing aid manufacturers now offer mobile apps that can turn a smartphone into a hearing aid remote control. Thus, there is no need for the patient to buy a remote and extra accessories. In addition, smartphone apps can turn an iOS or Android device into a hearing aid. For example, BioAid is a free app that can turn an iPhone into a hearing aid by processing sounds picked up by the iPhone microphone and delivering the amplified sounds over headphones in real time. BioAid provides 6 presets according to the way amplification is prescribed. These are just examples. You will find more if you search for “hearing aid” in the app store. And you can bet that there are more sophisticated applications in the developmental pipeline.
In addition to technology innovations, the current hearing aid dispensing system is facing a challenge from big-box retailers, like Costco. The major advantages of getting hearing aids from Costco hearing aid clinics are low price and efficiency. Costco sells hearing aids from the “Big Six” manufacturers, which guarantees the quality of the products. According to a report in the New York Times in 2013, Costco charges its hearing aid customers half or less of the average retail price in the U.S. Regarding services, Costco hearing aid clinics have a diagnostic/fitting protocol including audiometry, speech recognition testing, self-report measurements, and real-ear measurement. Many customers have reported receiving satisfactory service and products via Costco’s hearing aid dispensing program. Over the past four years, Costco’s hearing aid sales have grown by an average of 26% a year. Although debates about this dispensing model in our field are vigorous, we cannot deny that this retail model has been accepted by at least some consumers and received positive reviews. It’s worth mentioning that quite a few audiologists have chosen to work in Costco hearing aid clinics.
Another important example of disruptive innovation in our field is the recent prominence of personal sound amplification products (PSAPs). These provide amplification to help people hear sounds that are soft or at a distance. Thus, listeners with hearing impairment, especially those with mild hearing loss, potentially could benefit from PSAPs. Some PSAPs are offered by manufacturers that have not previously been involved with hearing aids (e.g. Able Planet). The advantage of using PSAPs is that they are not subject to state or federal regulations and easily can be obtained at stores or online.
All these new developments add up to mounting pressure on the way we traditionally do business.
5. I’ve heard that some people are worried that PSAPs will cut into their sales. Can you explain more about what these products are like?
Certainly, it’s quite simple. Personal Sound Amplifier Products (PSAPs) are gadgets that amplify sounds but they are not advertised as intended for helping people with hearing loss. They are advertised for such applications as helping hunters to hear soft sounds, helping with “hard to hear” sounds, and “making voices easier to understand”, etc. Because they are not theoretically intended to compensate for hearing loss, PSAPs are not regulated by the FDA. They can be sold over the counter or online just like iPods or non-prescription reading glasses. Actually low-tech PSAPs have been around a long time. You’ve seen them advertised in the newspaper or on TV, typically for very low prices.
What has changed more recently is the potential for creating high-tech, high quality PSAPs that might, for some people, rival the usefulness of traditional hearing aids and can be sold at relatively low cost without professional input. At this time, there are several PSAPs available that appear to be of relatively high technological level and are sold for much less than a traditional hearing aid in a professional setting. For example, a PSAP that at one time was selling at Best Buy for $399.99, had 16 bands and channels, digital noise reduction, volume control, telephone coil, and a “speech enhancement circuitry.” Sounds a lot like a hearing aid, doesn’t it?
6. In spite of what you’re saying, I’m not really worried because those products are inferior to the premium products that I recommend to my patients – aren’t they?
Actually, there is remarkably little published evidence to show that premium hearing aids give better real-world outcomes than basic hearing aids or PSAPs. Some NIH-funded projects are underway to search for this kind of evidence and we can expect to see results in the next couple of years. With my colleagues, Jani Johnson and Jingjing Xu, I have been doing this kind of research in our lab for the last several years. So far, our data suggest that if there are real-world outcome differences between basic and premium hearing aids, they are not likely to be large. For example, this was shown in a recent student project in our lab (Breitbart et al., 2014). This lab-based study compared examples of premium hearing aids, basic hearing aids, and high quality PSAPs. We measured 6 devices, two in each category. Each device was fit on KEMAR to match the NAL-NL2 targets for an average mild to moderate hearing loss as well as possible. Three types of everyday sounds were used as test stimuli: speech, noise, and music. Each of the three sounds was recorded through each hearing device on KEMAR. Twenty adult listeners with mild to moderate sensorineural hearing loss listened monaurally using an ER-2 insert earphone. A double round-robin paired-comparison tournament was performed using the 6 recordings of each sound. During each tournament, the 6 different hearing device conditions were paired against each other twice. Results are summarized in Figure 1. Analysis showed that there were no significant differences in preference for premium, basic, and PSAP conditions when the stimulus was music or everyday noises. Also, premium hearing aids were not significantly preferred over basic hearing aids with any stimulus. However, when the stimulus was speech, both the premium and the basic hearing aids were significantly more preferred than the PSAPs.
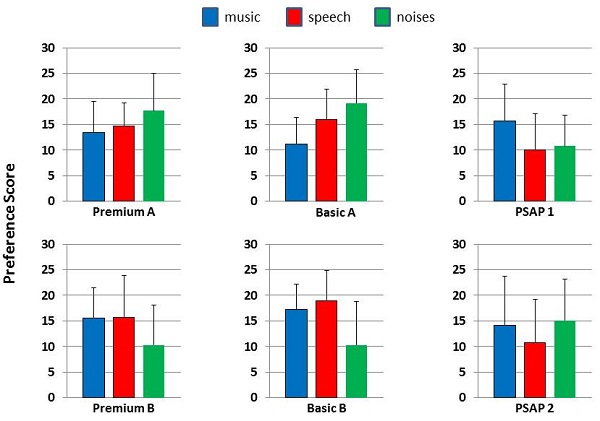
Figure 1. Preference scores for each stimulus. Data are given for two premium hearing aids, two basic hearing aids and two PSAPs.
Because this research was done in a sound-treated room with closed molds and without individualized fittings, there are limitations on its real-world generalizability. Even so, it is important to note that there were not substantial differences in preferences among the three types of devices. An interesting trend that emerged is that some devices seem to perform better for speech whereas others performed better for noises or music. In other words, it appeared that different devices were specialized to process different types of stimuli more effectively. This underlines the importance of individualized professionally-driven device selection. It is critical to understand the patient’s goals for amplified sound and to choose the appropriate device to best suit his/her needs. However, the best device might not necessarily be a premium hearing aid.
7. Whoa. I need a minute to process this. I have really believed that premium hearing aids are better than basic hearing aids. If I can’t justify selling premium hearing aids at a high cost, how am I going to make a living?
This is one of those needed fundamental changes that I am talking about. The high cost that you are referring to typically includes not only the device, but also your professional services and expertise. By bundling your services together with the product, you are sending the message that your services are not worth paying for. As a result, the value of your services tends to become invisible to the consumer, and perhaps to yourself as well. This has to change.
When you think about it, your educational preparation has given you a lot to bring to the hearing health care table. For example, you can explain the impact of hearing impairment to patients, understand your patients’ individual needs and provide individualized recommendations about different treatment options. You can optimize hearing aid fittings based on your knowledge, and can provide education about hearing loss and technologies. You can counsel patients and their communication partners, and impact patients’ quality of life in complex and meaningful ways.
For example, last week Jani Johnson was telling me about a patient who had purchased hearing aids through a retail hearing aid clinic. But he felt like the dispenser just wanted to sell hearing aids for profit, and did not want to take time with him. The patient was not satisfied with the hearing aids, and continued to seek follow-up counseling, but he felt that the dispenser just wanted to rush him out of the clinic. Eventually, the patient gave up wearing the hearing aids. His family felt that he purposefully had chosen to withdraw from them and they were resentful. After Jani’s professional counseling about his hearing loss and communication strategies, he and his family gained a deeper understanding and a greater optimism that his communication problems could be managed. He said that this experience literally saved his marriage.
Similarly, another member of our team, Jingjing Xu, told me about an individual who had previously sought hearing aids at two different hearing aid clinics, but had never been counselled about her hearing loss. She was told only that she needed to purchase hearing aids, which she was understandably unwilling to do without further information. After Jingjing explained the likely effects of her hearing loss and the treatments available, she felt less helpless and more comfortable moving forward with a treatment plan.
The point here is that audiologists are prepared by their education with a unique skill set to help hearing-impaired people manage their communication problems and improve their quality of life. We are potentially very valuable members of the hearing health care team and these services deserve to be reimbursed in and of themselves. In the future, audiologists need to build their practices around this unique skill set. This is what we can do that no one else can do.
I’m not an expert at breaking out all the numbers, but others have shown that this approach works. For example, John Coverstone (2012) wrote an article on the topic here at 20Q two years ago.
8. You must be living in a dream world. I have to think that my income is going to take a nasty dive using that approach. Moreover, how will I get paid by insurers or Medicare?
You’re not the first person in my career to accuse me of being a dreamer. But the first step toward positive change is a dream. Therefore, the first thing we have to do as audiologists is decide for ourselves what kind of professionals we want to be in the 21st century. Then, we need to devise a plan to make that happen.
As a general rule, our current professional identity (both how others see us and how we see ourselves) is that of diagnostic technicians and/or hearing aid sellers. This is despite our extensive graduate education, broad scope of practice guidelines, and the career aspirations of most new audiologists who are entering the field. I’m sure you know that audiology began as a rehabilitative profession. But over time, we turned away from and abandoned our rehab roots. This limited identity we have created for ourselves is now reflected in the limited services for which audiologists can be reimbursed by third party payers using current procedural terminology (CPT) codes. Do you know why that is?
9. OK, I’ll bite. Why is that?
Because that’s what we wanted! Yes – we did this to ourselves. Jani was telling me about a recent presentation by Judy Abrahamson (2014) in which Judy explained that in the late 1970’s and early 1980’s, the audiology leadership took the position that our profession was becoming a diagnostic profession that was no longer engaged in auditory rehabilitation. Laura Wilber, Professor Emeritus of Audiology at Northwestern University and 1982 President of ASHA, recalls attending meetings at the ASHA office during these years in which this belief was expressed. The number of items regarding rehabilitation on the ASHA audiology certification exam was questioned because “we don’t do that anymore.” Audiologists at meetings with Medicare and Medicaid representatives concerning professional access to CPT codes declined access to the rehabilitation codes stating they would not be needed by audiologists since audiology was exclusively a diagnostic profession. Fast-forward 25 years, and here we are. The current comment “We can’t be reimbursed for rehabilitation” is the result of the decisions at these meetings.
So you are correct that many of the practical changes I am suggesting currently are not covered by outside payers like Medicare. Nevertheless, these services when conscientiously provided by professionally trained audiologists have substantial value for our patients. By unbundling professional services from the costs of devices, we make their value visible both to patients and to third parties (and to ourselves). Next steps? 1) Document: Systematically document the effectiveness of these services. 2) Advocate: Use this documentation as evidence in favor of changes in policies that will allow audiologists to gain access to these codes. Essentially, we need to change history.
10. I don’t know how to begin thinking about changing my whole view about what I do in such a radical way.
In principle, it’s pretty simple: Audiologists need to restore their image to one of professionals who exist to help people manage hearing problems in their daily lives. This begins with assessing real-life difficulties, and continues with discussing the full spectrum of available treatment approaches, and helping the patient and family decide how to proceed. Although we have become focused on seeing ourselves as hearing aid sellers, there are several other effective treatments that can help people with hearing problems.
11. I can’t think of any really effective treatments other than hearing aids.
In addition to traditional hearing aids, we can offer group rehabilitation, individual training, home study, implants, ALDs, and let’s not forget, our patients always have the option not to do anything at this time except explore the extent of their hearing problems. In fact, there are so many options, it is difficult explain them to patients without overwhelming them. Some people have recommended the use of a decision aid for this purpose. We have tried this and have found it to be very helpful.
12. Sounds interesting. What is a decision aid?
I got this idea from reading the research of Leplante-Lévesque, Hickson, and Worrall (2010). Then, after I Googled “Decision aid”, I realized they have been used quite a bit in other fields. The decision aid is a visual tool that helps to organize and systematize a set of options. Audiologists can use it to facilitate a conversation with the patient to help them decide on a treatment plan. It should be used in a "shared decision making" context, where you let the patient know his/her options, you ask the patient what they think, and you provide guidance based on the information you have already gathered about the patient. Figure 2 shows the first page of a decision aid used in a hearing clinic. This decision aid is modeled on the one published by Leplante-Lévesque and her colleagues. On this page we briefly describe five different treatments, as well as a possibility of doing nothing at this time.
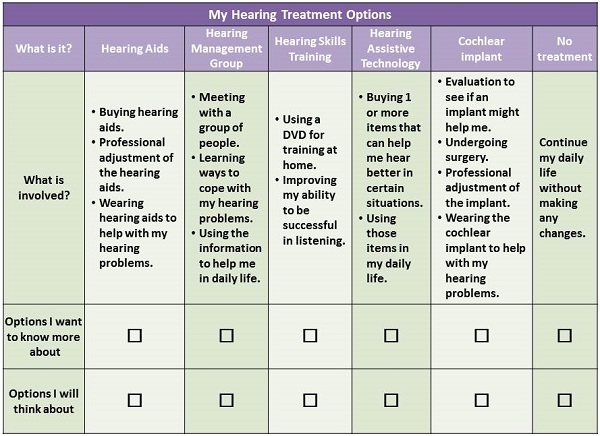
Figure 2. First page of a decision aid used in a hearing aid clinic.
13. I think I get it. Will you give some specifics about exactly how you would use this decision aid?
Sure. We introduce the decision aid with patients in an interview after having taken their history, done the audiogram, completed various disability/attitudes questionnaires with them, and discussed goals with the COSI (Dillon & James, 1997). All of this makes it easier to personalize how we use the decision aid with each patient.
Next, we make sure the patient understands that we are a hearing problem treatment center, not just a hearing aid clinic. We explain that there are several options for how they might proceed. The patient might benefit from one treatment, or from a combination of treatments. The treatment might or might not include traditional hearing aids. We then briefly go over all of the options that are available for them at this center. At this point we provide opinions about which treatments might be helpful based on what we know about the patient's needs.
Next, the patient decides which of those options they want to discuss in more detail, and which ones they might want to think about and possibly discuss later. Patients are encouraged to choose as many options as they are interested in.
After that, we go over the details about what is involved for each treatment that the patient selected. We outline what the patient would be expected to do, and the pros and cons of each choice. For any options that the patient wants to think over at home we provide them with informational material to take with them. This helps focus their thinking. They also take a copy of the decision aid home and we encourage them to show it to people around them and discuss the options. If they don’t decide right away, we call them about 1 week later to check what they have decided to do. A complete copy of this particular decision aid can be found at www.harlmemphis.org, along with a demonstration of how it can be used.
14. I see you have five different treatment options there. I understand about hearing aids and cochlear implants, and of course I know what assistive listening devices are. What do you mean by the other two?
I am glad you asked. The treatment option “Hearing management group” refers to a group aural rehabilitation (AR) program which typically involves several group meetings over a period of weeks. Group AR is flexible but often addresses issues related to device use, reductions of auditory handicap, and quality of life improvement. Recently, a web-based tool has been produced to facilitate program development. It is called The Group Rehabilitation Online Utility Pack (GROUP; Montano et al., 2013). GROUP provides hearing professionals with evidence-based resources to facilitate the creation and implementation of group AR services. In a group AR program, participants can listen to other people who are in the same boat and share feelings and experiences. Participants gain a deeper understanding of their communication problems and they can learn different coping strategies from each other. Another advantage is that group AR programs are time and cost effective because counseling and training are simultaneously provided to several people, often including family members. Hawkins (2005) conducted a systematic review of group AR programs. He concluded that there was evidence to support benefits from participation in terms of reduction in self-perceived hearing handicap, better use of communication strategies, and use of hearing aids. A more recent review (Chisolm & Arnold, 2012) bolstered Hawkins’s conclusions, and performed a meta-analysis on 7 of the reviewed studies. The effect size, calculated as a Cohen’s d, was -.352, indicating a small but significant effect on hearing handicap after participating in a group AR program.
Another option on our decision aid is “Hearing skills training”. This refers to individual auditory training using one or more of the recently developed programs for this purpose. This type of training is usually provided to an individual patient via a computerized program or a DVD-based program. It can be done at home or in your office. Programs are often categorized as analytic, synthetic, or a combination of the two. Analytic training facilitates bottom-up processing, using speech consonants and vowels, as the training materials to improve discrimination and recognition of speech components. Synthetic training facilitates top-down processing and typically includes materials with linguistic context, such as sentences and paragraphs, to exercise listening skills and the ability comprehend meaning from incomplete or distorted stimuli. Sweetow and Palmer (2005) conducted a systematic review of hearing skills training and concluded that there was evidence to support its effectiveness in improving speech understanding. A more recent systematic review (Chisolm & Arnold, 2012) agreed, showing that a meta-analysis on 6 studies revealed a significant effect size of .35.
So you see, there is evidence that patients typically benefit from hearing management groups and hearing skills training. Either type of treatment (or both) will likely result in positive outcomes. However, there are no standardized guidelines regarding which program(s) to recommend. Professional counseling is necessary and critical to identify the most appropriate approach for an individual patient in order to yield maximum benefit. Also, remember that these treatments can be independent of, or combined with, using amplification.
I know you said you know about assistive listening devices (ALDs), but do you really use them? ALDs can be a viable option for many listeners who have hearing difficulties only in specific settings such as evening TV-watching with the family. Such patients might not feel ready to embrace a commitment to traditional hearing aids. If a listener’s major communication difficulty is situationally limited, an appropriately chosen ALD may go a long way to resolving the problem. Let’s remember to say “we’ve got an ALD for that!” When recommending ALDs, professional counselling and thorough instruction are important and should be provided to maximize perceived benefit.
15. Ok, I see how the decision aid works, but it won’t work for me because I cannot offer cochlear implants.
Hold the phone! It’s important to realize that we change the treatments on the decision aid any time we feel there is something more effective or we want to add or delete any treatment. Your decision aid should include any treatments that you are willing to offer.
As a matter of fact, you could include an option for a person to obtain their own hearing devices (e.g., a PSAP or online hearing aid), and have a consultation with you about the pros and cons, and how to optimize the device for the patient.
16. Are you kidding me? How could I possibly offer to fit PSAPs into my clinic?
I’m not kidding. You actually have all of the skills necessary to do this. I would suggest that you start with real-ear verification measures to determine the best PSAP settings to give amplification close to the NAL-NL2 prescription. Through this process, you will be able to counsel the patient about the likely benefits of the device and where they may still have difficulties. In addition, you would of course provide your professional counseling about managing their communication difficulties. In fact, in the unbundling model I mentioned earlier, your services for fitting the products could be very similar for a PSAP and a premium hearing aid, depending on what measurements and counseling you do.
17. I’m hesitant to include the option for no treatment, because how will I get paid?
That’s the beauty of re-thinking your role in treating hearing problems. You are providing professional hearing loss treatment – not just selling hearing aids. Therefore, if your patient is not ready to move forward with any treatment for their hearing loss, you don’t suffer financially just because you didn’t “make a sale”. Instead, you are paid for the time spent in the consultation and for your expertise. Also, in this scenario you would expect that the patient now understands all of their options, does not feel judged or pressured, and has made an action plan with you for a follow-up of some sort (e.g., annual hearing check). This session has the potential to help you to establish return business and get the word out to others about the variety of services that you offer.
18. After spending so much time and money on my education, surely the fact that I have an Au.D. will attract patients to me even if I don’t use your newfangled decision aid.
I hate burst your bubble again, but audiologic services are pretty much invisible in modern health care at this time. As a matter of fact, Jani has done some research interviewing adults here in Memphis about their perceptions of hearing health care (Johnson, 2011). The vast majority had no idea where to seek services for hearing problems/hearing aids or what might be involved in that process. They didn’t know the term “audiologist” or the difference between audiologists and other non-audiology hearing healthcare workers. Several individuals held the opinion that the goal of all hearing aid dispensers (audiologists and non-audiology dispensers) is to sell products, not to help people. The current model of hearing aid dispensing reinforces these perceptions by emphasizing marketing claims of hearing assistive technologies and playing down the skills of the audiologist.
19. You have challenged me (and your other readers) to make some pretty substantial changes that are not entirely comfortable. What if we decide not to make these changes you’re talking about? What’s the worst that could happen?
Well, you’re asking me to predict the future, but OK. I think that if audiology and audiologists do not change and adapt, we are likely to be overtaken by circumstances. At this point, we do not have a unique identity, quite a few existing patients are not very satisfied with our services, and we are not attracting many new patients. Hearing-impaired boomers are looking for a better mousetrap, and there are more than a few smart individuals who are trying to figure out how to provide it in a way that does not include audiology.
20. What if we do implement these changes? What is likely to happen?
In a word, growth. This is an exciting time in our profession. Changing our collective identity and the way we conduct business will lead to growth and improvement in several areas. I expect that we would see some of the following results.
Improved patient outcomes: Building our practices around our unique skill-set will allow us to implement a model of optimized individual care and shared decision making about treatment. This will improve the quality of our services, build trust, and boost patient satisfaction.
Increased job satisfaction: Audiologists will be able to apply their expertise and feel confident that they are making their best efforts to help people manage their hearing problems in their daily lives. They will not feel the desire to abandon their professional education and best clinical practices in favor of less-than-satisfactory clinical practices once they are in the “real-world”.
Improved professional image and increased visibility: Highlighting the value of our skills and expertise will improve our professional image among potential consumers and other parties. This should lead to increased professional and word-of-mouth referrals. In addition, improved self-image and increased recognition of our own value would eliminate our tendency to apologize for our service charges by hiding them within the cost of a hearing aid, freeing us from an unhealthy dependence on hearing aid sales for profit.
Competitive advantage in a changing marketplace: Marketing our unique skill-set rather than focusing on claims about hearing assistive technologies will give us a competitive advantage over technology-focused models for hearing help. Further, it gives us the flexibility to accommodate industry changes and embrace innovations like PSAPs and smart phone technologies rather than struggle against them. This allows for growth and improvement of our profession as a whole and allows us freedom to adapt to meet the challenges of the future.
More patients: If we provide a longer menu of treatment options and more attention to the individual needs of each patient, this will grow our profession. We can help many of the 75-80% of people with hearing problems who are on the sidelines right now. Changing our professional image will attract more of them to our practices.
References
Abrahamson, J. (2014, February 27). Group programs in rehabilitative audiology. Paper presented at the 44th Annual Mid-South Conference on Communicative Disorders, Memphis, TN.
Breitbart, D., Xu, J., Johnson, J., and Cox, R. (2014, April) Is there a preference between hearing aids and personal sound amplification products (PSAPs)? Retrieved from https://www.harlmemphis.org/
Chisolm, T., & Arnold, M. (2012). Evidence about the effectiveness of aural rehabilitation programs for adults. In L. Wong & L. Hickson (Eds.), Evidenced-based practice in audiology: Evaluating intervention for children and adults with hearing impairment (pp. 237–266). San Diego, CA: Plural.
Coverstone, J. (2012, March). 20Q: Fee for service in an audiology practice. AudiologyOnline, Article 776. Retrieved from https://www.audiologyonline.com/
Dillon, H., A. James, et al. (1997). "The Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids." Journal of the American Academy of Audiology 8: 27-43.
Hawkins, D.B. (2005). Effectiveness of counseling-based adult group aural rehabilitation programs: a systematic review of the evidence. Journal of the American Academy of Audiology, 16, 485-493.
Johnson, J. (2011). Influence of culture on appraisal of hearing impairment. Unpublished doctoral dissertation, University of Memphis, Memphis, TN.
Laplante-Lévesque, A., L. Hickson, et al. (2010). A Qualitative Study of Shared Decision Making in Rehabilitative Audiology. Journal of the Academy of Rehabilitative Audiology 48: 27-43.
Montano,J., Preminger, J., Hickson, L.,and Gregory, M.(2013). A New Web-Based Tool for Group Audiologic Rehabilitation. Am J Audiol. 22. 332-334.
Sweetow, R., & Palmer, C. V. (2005). Efficacy of individual auditory training in adults: A systematic review of the evidence. J Am Acad Audiol., 16, 494–504.
Cite this content as:
Cox, R. (2014, April). 20Q: Hearing aid provision and the challenge of change. AudiologyOnline, Article 12596. Retrieved from: https://www.audiologyonline.com


