 From the Desk of Gus Mueller
From the Desk of Gus Mueller

I’m guessing that most of you reading this use an audiometer on a daily basis, or at least have at some time in your life. And really, what is more interesting than the history of the clinical audiometer? A few years back, Wayne Staab wrote a nice review on this topic that you can find here. My current interest was to check out the frequency range that was available on some of these early instruments.
Some of you might have heard of the Western Electric 2-A, which was the first popular commercially available audiometer (in the U.S.) in the 1920s and 1930s. The 2-A had eight test frequencies: octave intervals between 64 Hz and 8192 Hz. As the name “2-A” suggests, this equipment replaced the Western Electric 1-A, an audiometer that was patented in 1914, and according to Wayne’s article, 25 1-A instruments were sold in 1925—cost per unit was $1500. As a reference, in 1925 a new Ford Model T car sold for ~$400. Nearly as interesting as the sales price, was that the test frequencies for this audiometer ranged from 32 through 16,384 Hz!
So indeed, one audiometer started off with test capabilities of extended high frequencies, but mostly because of design and calibration reasons, ever since production of the Western 2-A, we have become accustomed to using audiometers (and audiograms) with 8000 Hz as the highest test frequency. Could it be that this is because we don’t learn much that is useful by determining thresholds above this frequency? Not so, and fortunately, in recent years both researchers and clinicians have explored what we can learn from testing what are commonly called “extended high frequencies” (EHFs). We have one of those leading EHF researchers with us this month at 20Q.
Srikanta Mishra, PhD, is a professor in the Department of Communication Sciences and Disorders at the University of Texas Rio Grande Valley. As many of you know, he has numerous publications in the area of extended high frequency audiometry, as well as research in the areas of pediatric audiology, the efferent auditory system, and auditory physiology. His work on hearing in children is supported by NIH/NIDCD, and in recent years he has been honored as the recipient of JAAA Editors’ award. Dr. Mishra also is a member of numerous professional committees, and serves as a reviewer for several journals and grant applications.
While the production of the Western 1-A audiometer was over 100 years ago, we are fortunate that like the audiometer, Sri also has an interest in test frequencies above 8000 Hz. As you read his excellent review, I think you’ll be a little surprised in the useful information that can be obtained from testing these (commonly) hidden frequencies.
Gus Mueller, PhD
Contributing Editor
Browse the complete collection of 20Q with Gus Mueller CEU articles at www.audiologyonline.com/20Q
20Q: Extended High Frequency Hearing Loss - Translating Science into Clinical Practice
Learning Outcomes
After reading this article, professionals will be able to:
- Explain which frequencies and equipment are needed for audiometric testing for extended high frequencies.
- Discuss the prevalence of EFH hearing loss in adults and children.
- Discuss the relationship between hidden hearing loss and extended high frequency loss.

1. You say “extended.” What exactly do you consider the extended high frequencies?
We all know that humans can hear up to 20 kHz, yet hearing assessment in the clinic usually is restricted to 8 kHz. Frequencies above 8 kHz, therefore often are termed as extended high frequencies (EHFs) or ultra- or very-high frequencies. Typically, the audiometric test frequencies for this region are 10, 11.2, 12.5, 14, 16, and 20 kHz. The specific frequencies available, however, may depend on the make and model of the audiometer.
2. Doing audiometric testing for the EHFs is something new?
You might think so, but can you believe that the first-ever commercially available audiometer (Western Electric 1A) in the early 1920s came with test frequencies up to 16 kHz (Vogel et al., 2007)? And it was priced at $1500! Fast forward to a century later—last time I checked, one would need $1500 to just add the module for EHFs to a standard audiometer. Notably, had the later models, e.g., Western Electric 2A, not eliminated the EHFs, perhaps we will not be talking about this topic today!
Natural speech contains salient information in the EHF range (9 to 16 kHz) that is essential for accurate polar angle localization (Best et al., 2005) and also important for perceiving the sound quality of music as well as speech (Moore & Tan, 2003). Although the literature on the role of EHF audibility in speech-in-noise recognition has been mixed, recent studies that carefully considered EHF content in the speech materials consistently show that access to EHFs particularly improves speech-in-speech recognition, i.e., speech in the presence of competing talkers for adults (e.g., Trine & Monson, 2020). Not only adults but children also perceptually benefit from access to EHFs (Flaherty et al., 2021).
3. What special equipment do I need to conduct EHF testing?
Several companies, e.g., Etymotic, Radioear, and Sennheiser, manufacture headphones that can be used to deliver sound at standard frequencies as well as EHFs. Both American (ANSI S3.6-2010) and international standards (ISO 389-5:2006; ISO 389-1:2017) exist to calibrate the audiometers for EHFs. In my experience, most third-party service providers have the technical capability to calibrate the audiometers with EHFs. Of course, we are talking about air-conduction testing only.
4. I’ve heard that our EHF hearing ability develops differently than the other frequencies. True?
Most certainly. It appears that hearing in the EHFs is early to mature and early to decline! For example, hearing thresholds for 1 kHz improve until about ten years of age, whereas the threshold improvement for 10 kHz is achieved by around five years of age (Trehub et al., 1988). The reasons for this frequency-dependent change in hearing sensitivity could be a mix of sensory as well as cognitive factors. In a large study (n=444 ears), we found that hearing sensitivity in the EHFs can start to decline from 21 years of age in healthy normal-hearing adults (≤ 20 dB HL in the standard frequencies, 0.25 through 8 kHz) (Mishra et al., 2022a). Lee and colleagues have reported similar results (Lee et al., 2012). In 4-to-19-year-olds (n=1084 ears), we found early signs of decline in EHF hearing sensitivity at around nine years–that's quite fascinating but also concerning. These findings suggest EHF hearing loss may be a sensitive predictor of early presbycusis.
5. Interesting. I haven’t conducted this testing myself. Are hearing thresholds in the EHFs reliable?
In short, the reliability of thresholds in the EHFs is no different than that elsewhere on the audiogram. Several studies report various statistical indices of test-retest reliability of hearing thresholds in the EHFs. In young adults (18-38 years), we found that the test-retest variability in thresholds is generally within ±10 dB for both within and across test sessions (10 days apart) for 98% to 100% of individual ears (Mishra et al., 2022a). The variability was slightly higher for 16 kHz relative to 10 and 12.5 kHz, and in general, the variability was larger across test sessions than the same test session. Similar results for EHF threshold testing have been reported for elderly listeners (60-79 years) (Matthews et al., 1997). In children with normal audiograms (4-18 years), more than 90% of individual ears had test-retest threshold differences within ±10 dB for individual EHFs (Mishra et al., 2022b). These results are highly comparable to the threshold variability in the standard frequencies and are consistent with clinically accepted norms.
6. What are the best EHF frequencies to test? Do I need to do testing at all that are available on the audiometer?
To strike a balance between efficiency and clinical usefulness, I would suggest 10, 12.5 and 16 kHz. Clinically, EHF audiometry is well received as an early detection tool for potential ototoxic hearing loss, with an increased interest in its use for hearing conservation programs. Both ototoxic monitoring and hearing conservation programs aim to detect changes in the cochlea as early and as subtle as possible. The usefulness of EHF audiometry in individual case diagnostics has been found for several unique patients such as Fabry disease, genetic hearing loss, fluctuating hearing loss, autoimmune disease, etc. (Rodríguez Valiente et al., 2016). It could also serve as a monitoring tool for examining the cochlear status in children with chronic otitis media. And obviously, EHF audiometry is needed to diagnose EHF hearing loss.
7. From what you have said, it sounds like I can expect to find that many of my patients will have an EHF loss?
Yes, that is true. Hearing loss in the EHFs can occur despite normal audiograms. And of course, EHF hearing loss can co-occur with hearing impairment in the standard frequencies. But, let me clarify that when we use the term “EHF hearing loss” we are typically referring to elevated thresholds (>20 dB HL) in the EHF range in the presence of a normal audiogram. EHF hearing impairment is widespread among the general population, be it adults or children, and 16 kHz is most affected. To more specifically answer your question, one report suggests that 64% had EHF impairment among 18-65-year-olds, and 56% of adults under 30 years had EHF loss (Motlagh Zadeh et al., 2019). We found that 19% of young adults (19-38 years) had EHF loss. One study reported that nearly 32% of children with listening disorders and 20% typically-developing children (6-14 years) had EHF loss (Hunter et al., 2021), and another study reported the prevalence to be 24% among 4 to 5-year-olds (Nakeva von Mentzer, 2020). We found a 7% prevalence of EHF hearing loss among the school-aged population sampled (4-18 years) who did not have a history of tympanostomy tubes (Mishra et al., 2022b). Likewise, a Columbian study showed a 10% prevalence of EHF loss for 13-to-19-year-olds (Peñaranda et al., 2020). Regardless of the exact prevalence, the reported estimates of pediatric EHF loss are alarming.
8. That’s a high prevalence. I suspect there are probably several different related causes?
There are, probably some that we have yet to identify. In adults, EHF hearing loss can result from noise, ototoxicity, infections, etc., but perhaps the largest contributor would be early aging and a host of complex factors, including lifestyle and possibly genetic. Other risk factors include ototoxicity from substance abuse, head trauma and traffic noise exposure in motor-bike riders. Similarly, EHF hearing impairment in children can occur due to several causes, such as pressure equalization tube surgery for treating otitis media (Hunter et al., 1996), ototoxicity from cystic fibrosis treatment (Al-Malky et al., 2015), or from heavy metal exposure (Shargorodsky et al., 2011). In addition, prematurely born and/or NICU babies are at a greater risk for EHF hearing loss. And, as with any other hearing loss, EHF loss can also occur due to idiopathic reasons.
9. Does someone with EHF loss have normal cochlear function for the standard frequencies?
One would expect hearing loss in the EHFs to have no effect on the cochlear functioning elsewhere in the audiogram. However, surprisingly, hearing loss in the EHFs is associated with subtle, subclinical cochlear deficits in the standard frequencies where the hearing thresholds are normal. In our adult study, we found that the magnitude of distortion product otoacoustic emissions (DPOAEs) recorded in the 2-5 kHz region was significantly lower for EHF-impaired than EHF-normal adults (Mishra et al., 2022a; see Figure 1). And, some adults with EHF hearing loss had no measurable DPOAEs. Observe in Figure 1 that the DPOAE magnitude is consistently lower for the EHF-impaired group (in red) for all f2 frequencies. Very similar results were found for children (Mishra et al., 2022b). Importantly, the highest DPOAE f2 frequency (5 kHz) was one octave lower than the lowest EHF tested (10 kHz), meaning that there were likely no far-basal sources that contributed to DPOAEs.
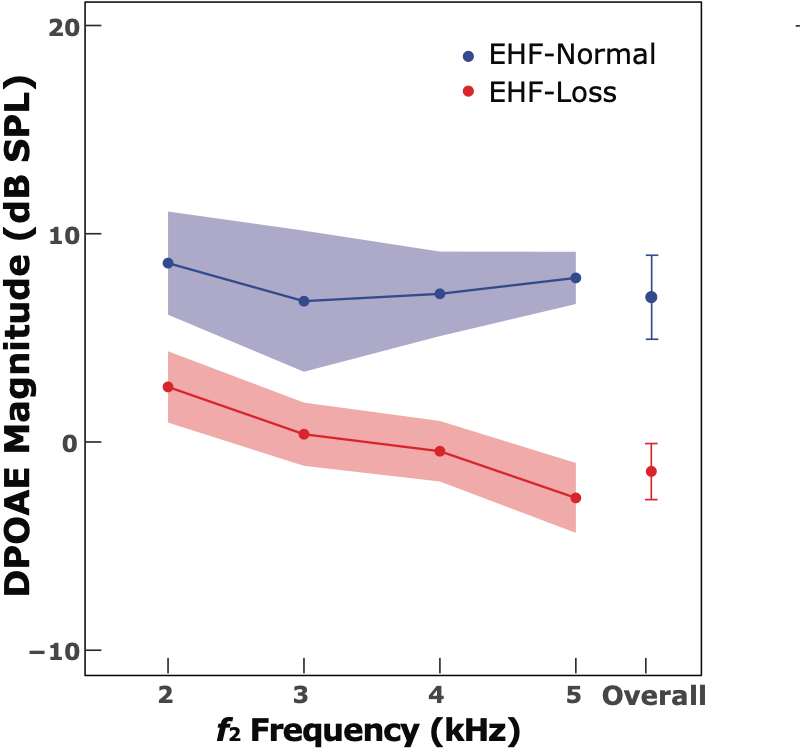
Figure 1. Adults with EHF hearing loss have lower DPOAEs. The mean DPOAE magnitudes are shown as filled circles; lines across f2 frequencies connect the mean values; shaded areas and error bars show 95% confidence intervals for the corresponding means. Data were adapted from Mishra et al., 2022a.
10. A “normal audiogram” isn’t always normal hearing?
Right. EHF hearing loss could be the missing link between a normal audiogram and absent or abnormal OAEs, and occasionally, listening-in-noise complaints. Interestingly, psychoacoustic measurements also provide corroborating evidence. In one study, listeners with a normal audiogram but elevated EHF thresholds and speech-in-noise deficits had relatively poorer frequency selectivity at 2 kHz (Badri et al., 2011). Thus, the factors that alter EHF hearing sensitivity could produce subclinical cochlear dysfunction even though the hearing thresholds in the standard frequencies are clinically normal. Data from animal models suggest that up to 40% outer hair cell loss may not produce deficits in pure-tone hearing sensitivity (Cody, 1992).
There is a significant association between hearing sensitivity in the standard frequencies and EHFs among normal-hearing individuals. In addition, our studies demonstrated that the mean pure-tone average for standard frequencies for the EHF-impaired group was 2.5 dB higher for adults (and 4 dB for children) than their respective normal-hearing counterparts. Others have reported similar findings as well (Motlagh Zadeh et al., 2019). Based on this, an individual who currently has EHF impairment will likely develop hearing loss over time in the standard frequencies. As I mentioned earlier, it appears that EHF hearing loss can be considered as an early indicator of clinical hearing loss.
11. Do these EHF losses really affect speech understanding?
We know that many individuals with normal audiograms complain of difficulty understanding speech in noisy backgrounds. In fact, one estimate suggests that 25.3 million Americans have hearing difficulty but no hearing impairment (Edwards, 2020). EHF hearing impairment may be one of the culprits in these clinically normal-hearing listeners.
Just like most other hearing loss, EHF hearing loss affects speech perception in complex listening environments. Using digit triplets in multi-talker babble, we found that listeners with EHF hearing loss have relatively poorer speech recognition thresholds (higher SRT-50 values) than adults without EHF loss (Mishra et al., 2022a). That is, they need a more advantageous signal-to-noise ratio (SNR). The magnitude of the SNR effect was of the order of 2.4 dB. This SNR effect is not small; it corresponds to ~15% or more change in the speech-in-noise recognition score. Interestingly, we found a similar effect for children as well (Mishra et al., 2022b). But, more importantly, when we carefully examined the results with children using statistical modeling, we found that EHF hearing loss slows down the development of speech-in-noise perception, as shown in Figure 2. The rate of improvement in SRT with age is slower for children with poorer EHF hearing relative to children with normal hearing.
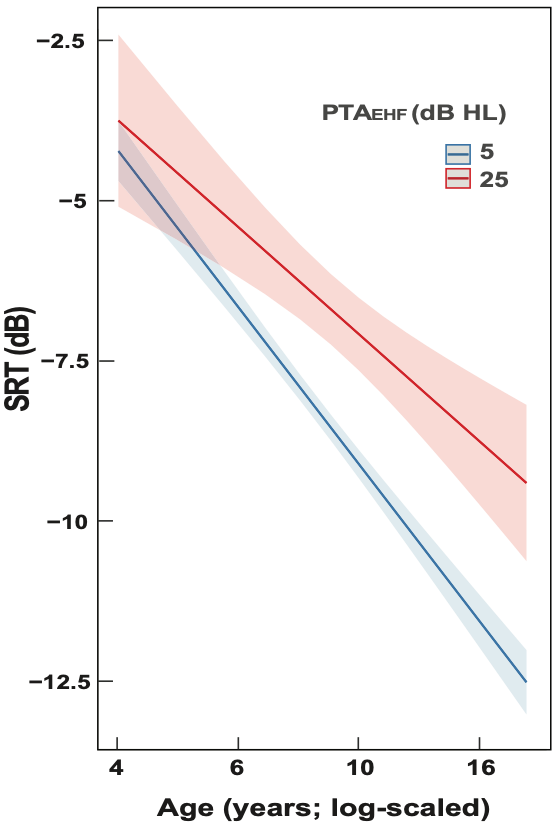
Figure 2. Children with EHF hearing loss have altered (slower) hearing-in-noise development relative to EHF-normal children. The speech recognition threshold (SRT) is the lowest SNR at which a 50% correct score can be obtained using the digit triplet test with multi-talker babble (lower SRTs represent better speech-in-noise recognition). The speech stimuli had energy in the EHFs, and the SRT was measured using Sennheiser HDA 300 headphones. The blue and red lines represent functions for 5- and 25-dB HL of pure-tone average for EHFs (PTAEHF), respectively. The line function for children with poorer EHF hearing (red) is shallower than that for better EHF hearing (blue), i.e., the SRT improves relatively slowly with age for children with poorer EHF hearing than for better hearing. The corresponding shaded areas show the 95% confidence intervals of the mean lines; based on the statistical model outcome from a cross-sectional dataset (Mishra et al., 2022b).
12. Why would EHF loss affect auditory perception and/or development in children?
It is well known that hearing loss, regardless of degree, type, or duration during the early years of life, is associated with altered central auditory mechanisms and perception. For example, be it otitis media (deficits in sound conduction), a slight degree of hearing loss (16-25 dB HL), or transient/ temporary impairment, all are associated with poorer auditory resolution and speech-in-noise perception. I hypothesize that children with EHF hearing loss are deprived of stimulation from the full auditory spectrum, and this degraded auditory experience during childhood is associated with poorer perception and/or prolonged auditory development.
13. Could this cause problems for children’s listening in the classroom?
That is reasonable to assume. It is well known that many classrooms for young children can be very noisy, and children must learn in suboptimal acoustic environments. Children with EHF hearing loss will miss out on the potential advantage provided by the EHF audibility. This lack of EHF advantage may exacerbate the effects of other factors such as inattentiveness for children. Occasionally, since the clinical audiogram is normal, EHF hearing loss could potentially mimic learning disorders leading to misdiagnosis.
There also appears to be a link between EHF loss and developmental communication disorders in children. Although a relationship between elevated (but normal; ≤ 20 dB HL) EHF hearing thresholds and listening disorders (aka auditory processing disorders) remain to be established, a link between EHF hearing and spatial hearing (Listening in Spatialized Noise—Sentences talker advantage scores) for children has been found (Petley et al., 2021). Some recent evidence suggests that children with EHF hearing loss may have speech sound disorders (Nakeva von Mentzer, 2021). Given the high prevalence of hearing impairment and subclinical auditory deficits in children with autism, I would predict that some children with autism may have EHF hearing loss if I'm allowed to make a reasonable guess.
14. We’ve been hearing a lot about “hidden hearing loss” in recent years. Is this also related?
Possibly, yes. Hearing loss in the EHFs has been postulated to be an indicator of cochlear synaptopathy in the lower frequencies (Bharadwaj et al., 2019), although experimental evidence from humans currently is not compelling. Liberman et al. reported that noise-exposed listeners had higher EHF thresholds, altered electrocochleography, and poorer word-in-noise recognition, as one would expect in listeners with hidden hearing loss (Liberman et al., 2016). However, not all studies on cochlear synaptopathy or hidden hearing loss show unequivocal results. Likewise, the relationship between tinnitus and EHF hearing loss is somewhat tenuous.
15. Many individuals with no hearing loss have poor speech-in-noise performance. You mentioned earlier that the same often is true for EHF losses?
Right. I have a little more to add on that topic, as we have some emerging evidence to support the functional consequences of EHF hearing loss in adults. For example, one study (Motlagh Zadeh et al., 2019) showed a relationship between EHF hearing loss and self-reported hearing-in-noise difficulty among listeners with normal audiograms. Likewise, others have reported individual cases with EHF loss and complaints of difficulty understanding speech in noisy environments (Rodríguez Valiente et al., 2016). We found some adults with EHF loss, with and without significant noise-exposure history, self-reported listening in noise difficulty (Mishra et al., 2022a). In an ongoing study, we have made some preliminary but important observations: (a) individuals with EHF loss self-report more difficulty in everyday, real-life complex listening and communication situations that often involve spatial hearing, (b) listening is relatively more effortful for EHF-impaired listeners.
16. Is there anything we can do regarding prevention of EHF loss?
Extended high frequency hearing loss most likely occurs from basal cochlear damage; unfortunately, it isn’t reversible, but in some cases, it is preventable. Since EHF hearing loss is an early predictor of hearing impairment in the standard frequencies, preventative measures can be deployed early on. One of the obvious prevention techniques is to protect against noise exposure. I wish aging could be prevented too!
In children, anything that minimizes the effects of otitis media should provide some protection. Importantly, we should at least monitor hearing frequently in listeners with EHF hearing loss for future hearing loss in the standard frequencies. Although commercially available hearing devices provide what is labeled “extended bandwidth,” it is not extended to the frequencies that relate to EHF loss. Those devices are for listeners who have hearing impairment in the standard audiometric frequencies.
17. Before we finish, I have a practical question for you. If I start conducting this testing, how do I bill for it?
Empirical evidence (both research and clinical), equipment, and standards support the routine use of EHF audiometry, but yes, who will pay for the extra time and effort for the audiologic testing? Currently, no code exists explicitly for EHFs. For extended pure-tone audiometry, one may consider using a modifier -22 (92552-22). An important practical aspect to keep in mind, however, is that payers may not like the modifier used too frequently. Maybe there will be a separate CPT code for EHF testing in the future?
18. Getting out of the clinic for a moment, how does EHF loss enter into current hearing science research?
The frequency at which the neural code for perceiving a pure tone transitions from a temporal to a place mechanism is an important question and a polemic issue in auditory neurosciences (Verschooten et al., 2019). To answer this question, Moore and Ernst (2012) measured frequency difference limens as a function of several frequencies and found that the transition occurs at about 8 kHz. This approach would not have been feasible without measuring difference limens for EHFs. We adopted a similar approach to find the transition frequency (~ 6 kHz) for children (Mishra et al., 2021). Another fundamental question in hearing sciences is whether the middle ear or cochlear tonotopicity imposes the high frequency limits of hearing. Yasin and Plack (2005), using psychophysical tuning curves at a range of frequencies, including EHFs, reported that up to 17 kHz, the high-frequency limitation in humans is imposed in part by the middle-ear attenuation characteristics and not by the cochlear tonotopicity.
19. What else might we learn about EHF hearing loss?
In adults, EHF hearing loss not only acts as an early warning sign for clinical hearing loss, but could potentially indicate a high risk for age-related cognitive deficits. For instance, a significant negative correlation between interaural asymmetry in EHF hearing and measures of global executive function have been reported for young adult listeners (Brännström et al., 2018).
When children have EHF hearing loss, it could potentially impede spoken language development and auditory cognition, affecting their ability to excel in school. EHF hearing loss also could contribute to the inter-individual variability observed in auditory and speech-language developments among typically-developing, normal-hearing children. These are all fairly reasonable predictions, but of course, need direct experimental evidence.
20. Do you see a day when EHF testing is a routine clinical procedure?
Although some audiologists may already be performing EHF hearing tests in special cases, such as ototoxicity monitoring, currently, there is no general clinical intent to identify, monitor, or manage EHF hearing loss. I hope that our conversation helps to create awareness among clinicians and researchers alike, at least for pediatric hearing assessments.
Unlike many advances in auditory sciences, research findings on EHFs are easily transferable to the clinic, as the equipment (audiometer) and the expertise to measure thresholds already exist. Audiologists worldwide need no additional training to test hearing in the EHFs!
References
Al-Malky, G., Dawson, S. J., Sirimanna, T., Bagkeris, E., & Suri, R. (2015). High-frequency audiometry reveals high prevalence of aminoglycoside ototoxicity in children with cystic fibrosis. Journal of Cystic Fibrosis, 14(2), 248–254. 10.1016/j.jcf.2014.07.009
Badri, R., Siegel, J. H., & Wright, B. A. (2011). Auditory filter shapes and high-frequency hearing in adults who have impaired speech in noise performance despite clinically normal audiograms. The Journal of the Acoustical Society of America, 129, 852-863. 10.1121/1.3523476
Best, V., Carlile, S., Jin, C., & van Schaik, A. (2005). The role of high frequencies in speech localization. The Journal of the Acoustical Society of America, 118(1), 353–363. doi:10.1121/1.1926107
Bharadwaj, H. M., Mai, A. R., Simpson, J. M., Choi, I., Heinz, M. G., & Shinn-Cunningham, B. G. (2019). Non-invasive assays of cochlear synaptopathy – candidates and considerations. Neuroscience, 407, 53–66. doi:10.1016/j.neuroscience.2019.02.031
Brännström, K. J., Karlsson, E., Waechter, S., & Kastberg, T. (2018). Extended high-frequency pure tone hearing thresholds and core executive functions. International Journal of Audiology, 57(9), 639–645. doi:10.1080/14992027.2018.1475755
Edwards, B. (2020). Emerging technologies, market segments, and MarkeTrak 10 insights in hearing health technology. Seminars in Hearing, 41(1), 37–54. doi:10.1055/s-0040-1701244
Flaherty, M., Libert, K., & Monson, B. B. (2021). Extended high-frequency hearing and head orientation cues benefit children during speech-in-speech recognition. Hearing Research, 406, 108230. doi:10.1016/j.heares.2021.108230
Hunter, L. L., Blankenship, C. M., Lin, L., Sloat, N. T., Perdew, A., Stewart, H., & Moore, D. R. (2021). Peripheral auditory involvement in childhood listening difficulty. Ear and Hearing, 42(1), 29–41. doi:10.1097/AUD.0000000000000899
Hunter, L. L., Margolis, R. H., Rykken, J. R., Le, C. T., Daly, K. A., & Giebink, G. S. (1996). High-frequency hearing loss associated with otitis media. Ear and Hearing, 17(1), 1–11. 10.1097/00003446-199602000-00001
Lee, J., Dhar, S., Abel, R., Banakis, R., Grolley, E., Lee, J., … Siegel, J. (2012). Behavioral hearing thresholds between 0.125 and 20 kHz using depth-compensated ear simulator calibration. Ear and Hearing, 33(3), 315–329. 10.1097/AUD.0b013e31823d7917
Liberman, M. C., Epstein, M. J., Cleveland, S. S., Wang, H., & Maison, S. F. (2016). Toward a differential diagnosis of hidden hearing loss in humans. PLoS ONE, 11, e0162726. 10.1371/journal.pone.0162726
Matthews, L. J., Lee, F. S., Mills, J. H., & Dubno, J. R. (1997). Extended high-frequency thresholds in older adults. Journal of Speech, Language, and Hearing Research, 40(1), 208–214. 10.1044/jslhr.4001.208
Mishra, S. K., Renken, L., Hernandez, M., & Rodrigo, H. (2021). Auditory development of frequency discrimination at extended high frequencies. Ear & Hearing, 42, 700–708. 10.1097/aud.0000000000000972
Mishra, S. K., Saxena, U., & Rodrigo, H. (2022a). Extended high-frequency hearing impairment despite a normal audiogram: Relation to early aging, speech-in-noise perception, cochlear function, and routine earphone use. Ear & Hearing, 43, 822-835. 10.1097/AUD.0000000000001140
Mishra, S. K., Saxena, U., & Rodrigo, H. (2022b). Hearing impairment in the extended high frequencies in children despite clinically normal hearing. Ear & Hearing, Advance online publication. 10.1097/AUD.0000000000001225
Moore, B. C. J., & Ernst, S. M. A. (2012). Frequency difference limens at high frequencies: Evidence for a transition from a temporal to a place code.The Journal of the Acoustical Society of America, 132(3), 1542–1547. 10.1121/1.4739444
Moore, B. C. J., & Tan, C.-T. (2003). Perceived naturalness of spectrally distorted speech and music. The Journal of the Acoustical Society of America, 114(1), 408–419. 10.1121/1.1577552
Motlagh Zadeh, L., Silbert, N. H., Sternasty, K., Swanepoel, D. W., Hunter, L. L., & Moore, D. R. (2019). Extended high-frequency hearing enhances speech perception in noise. Proceedings of the National Academy of Sciences of the United States of America, 116(47), 23753–23759. 10.1073/pnas.1903315116
Nakeva von Mentzer, C. (2020). Phonemic discrimination and reproduction in 4-5-year-old children: Relations to hearing. International Journal of Pediatric Otorhinolaryngology, 133(February), 0–11. 10.1016/j.ijporl.2020.109981
Nakeva von Mentzer, C. (2021). Audiometric profiles in children with speech sound disorder: Subclinical hearing loss as a potential factor. Clinical Linguistics and Phonetics, 35(9), 847–873. https://doi.org/10.1080/02699206.2020.1833369
Peñaranda, D., Pérez-Herrera, L. C., Hernández, D., Moreno-López, S., Perea, I., Jacome, M., … Peñaranda, A. (2020). Prevalence of extended high-frequency hearing loss among adolescents from two rural areas in Colombia. International Journal of Audiology, 60(5), 365-373. doi:10.1080/14992027.2020.1828631
Petley, L., Hunter, L. L., Zadeh, L. M., Stewart, H. J., Sloat, N. T., Perdew, A., … Moore, D. R. (2021). Listening difficulties in children with normal audiograms: Relation to hearing and cognition. Ear and Hearing, 42(6), 1640–1655. 10.1097/AUD.0000000000001076
Rodríguez Valiente, A., Roldán Fidalgo, A., Villarreal, I. M., & García Berrocal, J. R. (2016). Extended high-frequency audiometry (9000–20000Hz). Usefulness in audiological diagnosis. Acta Otorrinolaringologica (English Edition), 67(1), 40–44. 10.1016/j.otoeng.2015.02.001
Shargorodsky, J., Curhan, S. G., Henderson, E., Eavey, R., & Curhan, G. C. (2011). Heavy metals exposure and hearing loss in US adolescents. Archives of Otolaryngology - Head and Neck Surgery, 137(12), 1183–1189. 10.1001/archoto.2011.202
Trehub, S. E., Schneider, B. A., Morrongiello, B. A., & Thorpe, L. A. (1988). Auditory sensitivity in school-age children. Journal of Experimental Child Psychology, 46(2), 273–285. 10.1016/0022-0965(88)90060-4
Trine, A., & Monson, B. B. (2020). Extended high frequencies provide both spectral and temporal information to improve speech-in-speech recognition. Trends in Hearing, 24, 1–8. 10.1177/2331216520980299
Verschooten, E., Shamma, S., Oxenham, A. J., Moore, B. C. J., Joris, P. X., Heinz, M. G., & Plack, C. J. (2019). The upper frequency limit for the use of phase locking to code temporal fine structure in humans: A compilation of viewpoints. Hearing Research, 377, 109–121. 10.1016/j.heares.2019.03.011
Vogel, D. A., Mccarthy, P. A., Bratt, G. W., & Brewer, C. (2007). The clinical audiogram: Its history and current use. Communicative Disorders Review, 1(2), 81–94.
Yasin, I., & Plack, C. J. (2005). Psychophysical tuning curves at very high frequencies. The Journal of the Acoustical Society of America, 118(4), 2498–2506. doi.org/10.1121/1.2035594
Citation
Mishra, S.K. (2022). 20Q: Extended high frequency hearing loss - translating science into clinical practice. AudiologyOnline, Article 28181. Available at www.audiologyonline.com


