 From the Desk of Gus Mueller
From the Desk of Gus Mueller

We’re back this month to continue our discussion regarding changes to auditory processing and cognition during normal aging, and in what ways these changes might impact our hearing aid fittings. Our returning 20Q guest author is Richard Windle, PhD, registered Clinical Scientist in Audiology, currently completing training to become a Consultant Clinical Scientist in the English National Health Service (NHS), for which this work supports a Doctorate in Clinical Science. He is based at Kingston Hospital NHS Foundation Trust, London, UK, where he is Audiology Team Leader, heading the vestibular assessment and rehabilitation service.
In Part 1 of this interesting and timely topic, Richard reviewed the changes that likely will occur in the auditory system due to aging and/or reduced cognitive function. He further pointed out that the relative importance of the hearing thresholds, auditory processing, and cognitive function for predicting individual speech perception will depend on the specific situations encountered, and these will vary enormously in real life and among individuals. This takes us to the very important practical question—does our knowledge of these changes alter the way that we program hearing aids?
In my Part 1 introduction, I presented the scenario of Monday morning back-to-back patients, both male, who had very similar audiometric findings, and both were candidates for hearing aids. The notable difference was that the 8:00 patient was 40 years old, the 10:00 patient was 80, with some cognitive decline and age-related auditory processing difficulties. The question then is the obvious...do we program the hearing aids differently for the older fellow? Different prescriptive gain? Changes for compression kneepoints, ratios, and time constants? What about directional processing and DNR?
You’ll find in this month’s Part 2, that Dr. Windle has taken the physiologic information that he presented in Part 1, and brought it into the clinic, to provide us with some great suggestions regarding how we can personalize our hearing aid fittings.
Gus Mueller, PhD
Contributing Editor
Browse the complete collection of 20Q with Gus Mueller CEU articles at www.audiologyonline.com/20Q
20Q: Changes to Auditory Processing and Cognition During Normal Aging – Should it Affect Hearing Aid Programming? Part 2 – Programming Hearing Aids for Older Adults
Learning Outcomes
After reading this article, professionals will be able to:
- Describe how hearing aids affect the speech signal.
- Define the hearing aid parameters that have an effect on signal distortion and how this might impact the aided hearing of older adults.
- Set hearing aids for older adults based on appropriate parameters, including compression speed and compression ratio.

1. Good to talk to you again! I liked the review you provided last month on auditory processing and cognition as we age. And, I believe you promised that this month we could talk about how can we apply this to hearing aid fitting for older adults?
Correct. That was our agreement, and I’m looking forward to it. Recall that one of my main points was that even if our ears remained in perfect physical condition, most of us will still have problems listening in challenging situations as we age because of a “central” decline. Our brains have reduced capacity and speed to cope with the large amount of information thrown at us by a continuous speech signal, especially in the presence of competing sounds. Auditory processing decline also has an effect on our dependence on different speech cues. For example, a decline in the timing (“temporal”) accuracy of the auditory system will make us more dependent on the speech envelope (ENV) as we are increasingly less able to make use of temporal fine structure (TFS). In short, we become increasingly unable to cope with any distortion to speech introduced by hearing aids. This means we need to think carefully about all of the parameters we set in hearing aids, not just gain, in order to ensure that speech perception is not undermined and listening effort is not increased. The way we might do that practically within an audiology clinic is something that I thought we could talk about.
I won’t throw too many references at you in our discussion because it is based on our review paper (Windle et al., 2023), which you can access at https://doi.org/10.3389/fneur.2023.1122420. My thanks go to Harvey Dillon and Antje Heinrich for supporting the original work.
2. We’re on the same page. The more practical information you can provide, the more I’ll like it. Let’s start with what you mean exactly by “distortion”?
This is harder to define than it sounds, but you’ve raised an important point. Audiologists are probably familiar with the distortion measured in a test box, which is “total harmonic distortion”, the change to the output compared to a sine wave input. That’s a very simple definition, but sadly, this is pretty much useless in relation to our discussion about the distortion introduced to a speech signal by a hearing aid. When we think about speech, the concept of “distortion” becomes much more complicated. The whole point of a hearing aid is to change the input signal into something else, so “distortion” is inevitable. However, different types of distortion are introduced to different elements of speech.
Let’s consider the speech envelope (ENV) and temporal fine structure (TFS). If we quickly exaggerate some elements of speech, such as high-pitch fricatives like “f” and “s”, we might exaggerate some of the TFS and that is, presumably, a good thing. However, too much change to these elements of speech will also distort the speech envelope (ENV), and that’s a bad thing, especially for those more dependent on ENV for speech perception, such as those with reduced auditory processing and cognition, and those with greater degrees of hearing loss. There has to be a trade-off between TFS and ENV distortion, and it isn’t obvious how to do this.
Things quickly get even more complicated when we look at what elements of speech the auditory system responds to. The difference in the way two signals are modulated (i.e., the change in their overall amplitude) is an important bit of data that helps us separate competing speakers and other sounds. When these signals are processed together in a hearing aid, it causes “cross modulation” because the combined signal may be interpreted as coming from a single source. More recent research has shown that the auditory system makes use of the interaction between modulation in both the frequency and time domains or “spectrotemporal modulation,” which is also undermined by reduced frequency and TFS sensitivity with age. What happens to this after hearing aid processing really isn’t clear.
As you can see, talking about “distortion” can quickly get very complicated! Getting back to basics, for now, audiologists just need to understand that hearing aids are largely presented to us as a “black box”. In other words, they do all kinds of things to a speech signal that we do not understand in detail, and we do not have clear guidance to define what mix of parameters may be best for any one individual.
3. Can we measure the distortions that you are talking about in a simple way?
Sadly, no, because “distortion” can mean many things. Even if we could define all of the different elements of distortion, we’d need to know which were the most important for different individuals, with differing degrees of processing ability, and which related to speech perception, comfort, preference, and listening effort. There are some very interesting and promising approaches out there, not least the Hearing Aid Speech Perception Index (HASPI) and the Hearing Aid Speech Quality Index (HASQI) (Kates et al., 2018), so there’s hope that this might move us forwards.
4. You’ve told us this is complicated! So, how does it affect the way I should be programming hearing aids?
Despite the complexity in understanding auditory processing and cognition and the effect of hearing aids, there are simpler ways we can think about it and pragmatically modify our approach in clinic. In our review paper, we came up with a set of principles against which we could assess different elements of hearing aid processing (Windle et al., 2023), which I can show you (see Table 1). The point of these principles was to enable us to assess each parameter set during a hearing aid fitting.
| 1 |
|
| 2 |
|
| 3 |
|
| 4 |
|
| 5 |
|
| 6 |
|
Table 1. Basic principles for assessing hearing aid parameters for older adults, from Windle et al. (2023).
5. That’s a lot to think about. What parameters do I need to be thinking about when I’m programming the hearing aids?
I’m sorry to say that the short answer to this is “all of them.” Almost everything we do in programming a hearing aid introduces distortion in some form. The one important exception to this are methods to improve the signal-to-noise (SNR) ratio, including directionality and assistive devices such as wireless microphones. Improving SNR is always a good thing. Everything else may be beneficial or may make it harder to understand speech, especially when considering older adults with some decline in processing. Apart from the gain settings, other parameters we need to consider include: the compression ratio, compression speed, noise reduction, and frequency-shifting. In fact, pretty much any parameter set by the audiologist or left to the default setting of the manufacturer, will have some effect on distortion. This means that we shouldn’t just use the controls we have in the hearing aid fitting software, but we should also be aware of the underlying approach in different hearing aids. Somehow, this all has to be incorporated within an optimum hearing aid fitting for an individual.
6. What do you mean by an “optimum” hearing aid fitting?
It’s important to step back and think what we are trying to achieve with a hearing aid fitting. In the end, we are trying to provide the greatest benefit to each individual patient in whatever way each individual defines “benefit”. It’s important to realize that there may be several conflicting factors that do not always align. For example, maximizing speech intelligibility has to be traded-off against listening comfort and listening effort. Changing a parameter might result in better objective outcomes (e.g., speech intelligibility) but an individual may simply have a different preference despite it not being the optimum “audiological” setting. User preference and objective benefit are not always the same. In my view, it is not sufficient to simply say that an individual “needs to acclimatize”. There are multiple non-auditory factors that come into play, and these can result the patient simply not using the hearing aids sufficiently. We can assess hearing aids in all of their variously wonderful technical complexity, but we are wasting our time, and that of the patient, if we end up with something they simply don’t like and refuse to use, quite apart from wasting valuable healthcare resources.
I know we didn’t set out to talk about non-auditory factors in hearing aid fitting, however, we have to be aware of them and set the technical aspects of the consultation within the broader person-centred care framework, which includes physical, emotional, social, behavioral, and environmental considerations. An “optimum” hearing aid fitting incorporates all of these perspectives. We should also recognize that the cognitive status of individuals will affect clinical interaction. Higher degrees of fluid intelligence enable people to engage more with life, handle problems (e.g., getting used to a hearing aid), and be more proactive in addressing their health needs.
7. All good points, but getting back to hearing aid parameters, are there any that we should focus on first?
Good question! Yes, there are. The most important factors that define the amount of distortion to the speech envelope, ENV, and likely other forms of distortion, are the compression speed and compression ratio. This means that we should not only pay attention to these factors every time we fit a hearing aid, but we should consider the methodology of fitting a hearing aid. For example, conducting real ear measurements is great for setting gain to a prescription target, but if you set the gain to the targets for lower and higher level inputs (e.g., 55 and 75 dB SPL), you might end up with a compression ratio that is inappropriate for a particular individual, especially an older adult with reduced central processing. This will, in turn, be dependent on the compression speed that you’ve selected (or that which is hard-wired in the hearing aid by the manufacturer).
8. It’s been a few years since my classes on compression. Can you give a bit of a review on compression speed and how it affects speech perception?
Let’s start with the basics of compression. This refers to how we “squash” the volume of sounds into the range available to an individual, i.e., between their level of audibility and up to the level where it becomes uncomfortable. There will be more gain employed for quiet sounds and less for louder sounds. The compression speed simply refers to how quickly the gain is changed between these levels in a hearing aid. This is usually described in terms of attack and release times. Attack times refer to how quickly the signal is compressed (i.e., the gain is reduced) when a sound increases in level. Release times describe how quickly the gain increases again when a sound falls to a lower level. In reality, most hearing aids have similar attack times (usually about 1 to 10 milliseconds, ms), which protects users from sudden loud sounds. Hearing aids are largely differentiated as “fast” or “slow” according to the release times which typically vary from 5-200 ms (fast-acting compression, FAC) to 0.5-2 seconds (slow-acting compression, SAC), although the way this is implemented by each manufacturer also varies, which we can discuss later.
Fast-acting compression is sometimes referred to as “syllabic compression.” This is because the gain changes during a spoken word, so some phonemes or syllables are amplified more than others within the word. This type of compression is based on the fact that some elements of speech may be inaccessible to a hearing-impaired listener, typically high-pitched fricatives for those with a high-frequency hearing loss. FAC aims to restore normal loudness perception across the frequency range. Hearing aids with slow-acting compression enhance high-frequency sounds mainly via the application of different amounts of gain in each frequency channel.
Let’s look at what happens to a speech signal when FAC and SAC are employed (see Figure 1). FAC tends to “flatten” the speech envelope because quieter sounds are amplified more than louder sounds, so everything tends towards a more similar level. This causes obvious distortion to the speech envelope, ENV. We should also notice that quiet gaps between sounds are particularly exaggerated, possibly undermining gap detection. Going further, if bilateral aids are applying FAC independently, the relative level of sounds in each ear will be rapidly altered, undermining interaural level differences and localization. It should be clear that aggressive use of FAC can cause significant amounts of distortion to speech cues that may impair speech perception, especially for patients who are more dependent on ENV such as older adults with reduced processing capability or those with greater degrees of hearing impairment. Indeed, FAC might be contradictory to many of the principles of programming hearing aids for older adults that we discussed (see Table 1). By comparison, SAC does not significantly alter the speech envelope. In principle, therefore, SAC should be better for those with reduced degrees of processing and greater degrees of hearing loss, whereas FAC may be better for those with better processing and less hearing loss.
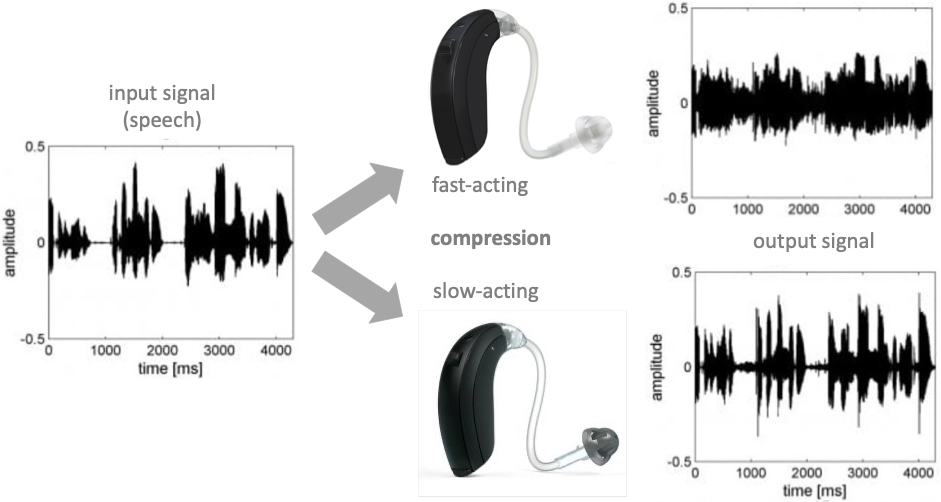
Figure 1. The effect of fast and slow acting compression on a speech signal, based on an exaggerated 8:1 compression ratio; developed, with permission, from Holube et al. (2016).
9. Is there any evidence for these compression fitting guides that you’re suggesting?
Yes. In fact, the discussion over what’s an appropriate compression speed has been continuing since the dawn of digital hearing aids, and it has been a controversial subject. Proponents of FAC pointed out that listeners cannot be aware of the signal if it is presented below the hearing threshold at a particular frequency (Villchur, 2008). But this doesn’t address the issue with distortion, and, at the time, most evidence considered hearing aids with only two channels. Modern hearing aids have many more channels and this increases the degree of distortion when using FAC, which users tend not to like, although it has little effect when SAC is employed (Holube et al., 2016). In principle, FAC helps to make weak phonemes audible in quiet conditions for people with mild-to-moderate hearing loss, but it does not offer benefit in noisy situations and for those with greater degrees of hearing loss.
The seminal set of studies in this field was conducted by Gatehouse et al. (2003, 2006a, 2006b), who compared different compression speed strategies. Overall, the degree of benefit from FAC, relative to SAC, declined as the presentation level of speech increased and as the signal-to-noise ratio fell. FAC also offered greater benefit to those with higher cognitive scores, whereas SAC was better for those with lower cognitive scores. Multiple studies have found similar results, although other studies did not find any strong relationships. As we discussed previously, it is hardly surprising that the results of studies vary because of the wide variation in the tests used for both cognition and speech perception. There is also variation in the type of hearing aid algorithms used and whether study subjects were allowed any time for acclimatization, as well as some variation between experienced and new hearing aid users. We found no good evidence that suggested that either FAC or SAC was always better across all situations. On the whole, we concluded that FAC was likely better for those with relatively good cognition and hearing, and SAC may be better for those with lower degrees of cognition and hearing due to normal aging, although SAC tended to be preferred for comfort on average, and preferences varied between individuals which may not have always been aligned with objective benefit (Windle et al., 2023). Based on the evidence, it is unlikely that we can say for sure what compression speed might be the best for any one individual, but it may be a significant issue for some users so we should, at least, give them the option.
10. What compression speed do today’s hearing aids use?
Our earlier discussion about compression speed was somewhat simplified, comparing ”fast” versus “slow”. In some hearing aids, a range of intermediate speeds can be chosen, and we do not have evidence supporting the use of these. Publications are not always clear about what they mean by “fast” or “slow”. There are also significant differences in the approach to compression by different hearing aid manufacturers. Compression speeds may be applied differently by frequency channel, by direction of change in sound intensity, or adaptive systems that change compression speed by acoustic situation. Furthermore, fast-acting impulse noise protection may be employed as a separate system, although the details of these approaches are usually proprietary.
Let’s think about the main hearing aid manufacturers and apologies, I can’t cover every brand. Current Phonak hearing aids use FAC, and it is only possible to switch out of this by using the manufacturers’ setting for profound hearing loss, which isn’t applicable to most people. GN ReSound, traditionally, also used FAC, but their more recent ranges now enable the clinician to switch between compression speeds in each program. Oticon, WS Audiology (Signia and Widex), and Starkey use adaptive compression. Broadly speaking, these use SAC in situations with any background noise and switch to FAC for quiet speech. The adaptive approach is in-built and usually can’t be overridden except in a few aids, such as Signia. One thing we noticed during our research was that it was not easy to obtain a clear description of compression speed strategies from manufacturers, and it was often a question that had to be referred to international HQ. In general, compression speed isn’t something provided in the product data for any hearing aids. It’s, therefore, unsurprising that audiologists might not be aware of it.
11. What about setting the compression ratio?
The compression ratio describes the range of gain applied across different levels of sound. A linear hearing aid does not change the gain based on the level of the input sound, and the compression ratio is 1.0. The greater the difference between the minimum and maximum gain applied, the greater the compression ratio. A high compression ratio likely improves speech intelligibility in quiet, but can reduce intelligibility in background noise (Goedegebure et al., 2001; Souza, 2002). However, it’s important to remember that the effective compression ratio (i.e., not the one shown on your hearing aid fitting software) will be based on the compression speed. For example, if the level of sound changes abruptly, the gain applied at any one moment will depend on what gain levels have been set (described by the compression ratio) and how long it takes the hearing aid to get there (the compression speed). So, for a continuously changing sound with the same minimum and maximum gain settings, fast-acting compression (FAC) will mean that the gain varies between much higher and lower levels of gain than slow-acting compression (SAC). In other words, for SAC, the gain may not reach its maximum or minimum during speech because the aid hasn’t had time to react before the input level changes again, and a 3:1 compression shown in the fitting software might only be an effective ratio of about 1.5:1. Put in a different way, FAC introduces more distortion to the signal, particularly the speech envelope ENV, and the amount of distortion will largely increase in line with the compression ratio, potentially reducing speech intelligibility. Increasing the number of frequency channels in a hearing aid will also increase the degree of distortion when using FAC. Conversely, a compression ratio of 3.0, shown in your fitting software, will have little effect on ENV cues when using SAC, and the number of hearing aid channels has little effect. Some evidence suggests that hearing aid users tend to prefer lower compression ratios, especially in noisy situations. In summary, a higher compression ratio can be set when using SAC, and we should be particularly careful of increasing the compression ratio when using FAC, especially for those with lower degrees of cognition associated with normal aging.
It should be noted that following a prescription target for 50, 65, and 80 dB HL input levels (e.g., during REMs) may lead you to end up with a compression ratio that may be too high for an individual, especially if the aids are based on FAC. This is why it’s important to think about the process of fitting hearing aids in general, as well as the technical parameters. Verification alone does not make a good hearing aid fitting, and we have to augment this with careful validation and counseling.
12. So, what compression ratio should I use?
The evidence suggests that slow-acting compression should be used for those with lower degrees of cognition due to normal aging and greater degrees of hearing loss. In this case, any compression ratio up to 3.0 (as shown in the fitting software) should be fine.
If fast-acting compression is used for this population, it is difficult to provide clear, evidence-based guidance. There is some evidence that suggests users prefer a compression ratio less than 2.0. Based on our own anecdotal experience and discussions with hearing aid manufacturers, we suggested a value of 1.5 for older adults (Windle et al., 2023).
13. Which patients should we provide with aids using a slow compression speed or reduced compression ratios?
… and that, I’m afraid, is the million-dollar question. Based on current evidence, we simply don’t know at what point we should switch, for example, from fast to slow compression. At the extremes of the range of auditory and cognitive processing, it is likely that fast-acting compression will benefit those with greater capacity, and slow-acting compression will benefit those with lower capacity. It’s also the case that slow-acting compression is likely best for all users in noisy situations, and also for those with greater degrees of hearing loss. However, for the majority of normally aging older adults, in the middle of the “cognitive range” and with mild-to-moderate hearing loss, it isn’t clear which to choose.
Age is a poor indicator of auditory and cognitive processing. As we discussed when we talked last month, cognitive speed and capacity for some processes that support speech understanding decline throughout adult life. However, the range of performance between individuals also increases with age. There’s also another consideration: that between objective benefit and user preference. These are two different things. A user may strongly prefer a particular setting, even if it yields poorer speech intelligibility performance. This may be because of listening comfort, listening effort, or it could be just a subjective preference. In short, the “optimum” setting for any individual may be quite unpredictable. Nevertheless, particularly for older adults who are more likely to have degraded auditory and cognitive processing, we should not assume either setting is best, but we should seek to determine the best option in clinic or provide them with alternatives, making a judgment about the best default program in a hearing aid. In short, offer both options, give it a go, and see how the patient does!
Of course, it should be the aim for research projects to define this situation better, and this is the subject of our ongoing research.
14. What about other hearing aid parameters?
Let’s start with the easy stuff. As we discussed earlier, increasing the signal-to-noise ratio with directionality or additional wireless devices, will always be a benefit and does not distort the processed sound.
Another important feature of hearing aids is noise reduction. The evidence does not suggest this offers any benefit for speech intelligibility, but it does improve sound quality and comfort. There is some evidence that strong noise reduction benefits those with better cognitive processes but may undermine speech intelligibility for those with lower degrees of cognitive function, although some users may still prefer it. Overall, for older adults, we concluded that moderate noise reduction likely improved comfort without affecting speech cues significantly, although preferences may vary between individuals (Windle et al., 2023). Likewise, frequency lowering may benefit those with higher degrees of cognition but can be detrimental to those with lower degrees of cognition.
Again, it’s not possible to be prescriptive about the best hearing aid parameter settings for any one individual, so we concluded that it was important to think about the whole hearing aid fitting process, particularly careful validation of settings. This becomes even more important as more recent research shows that there are interactions between all of the different hearing aid parameters, such that they can’t really be considered in isolation, although it’s currently difficult to determine optimum outcomes across a large matrix of settings.
15. You said that fitting two hearing aids might not always be best. Can you explain?
Fitting two hearing aids to preserve binaural hearing has almost become a doctrine of audiology. However, binaural processing declines throughout adult life. Some older adults may reach the point where binaural processes fail, and we refer to this as “binaural interference”, which becomes more prevalent with age. It shouldn’t be a surprise, therefore, that some studies show that older adults may prefer unilateral aiding and perform better in noisy situations with this fitting. We simply concluded that we shouldn’t presume that bilateral aiding is always best for every individual (Windle et al., 2023).
16. There’s a lot of complexity in all of this. How can we make use of all this information in the clinic?
Older adults can be some of the most complex patients seen in an audiology clinic because of the combined effects of deterioration in peripheral hearing, auditory processing and cognitive domains that support listening and understanding. Certainly, age-related hearing loss should never be treated with “standard care” simply because of its high prevalence. However, the evidence in this area is broadly consistent in many ways and simply suggests that a wider range of considerations should be employed. The good news is that we concluded that many of these considerations can be addressed in a fairly straightforward manner.
Let’s first consider what hearing aid fitting parameters we should look at in clinic, and how we’d do that. We provided a set of statements that we derived from the evidence (Windle et al., 2023), and I have summarized these for you in Table 2. It should be clear that a consideration of hearing aid parameters also has implications for the hearing aid fitting process.
| 1 |
|
| 2 |
|
| 3 |
|
| 4 |
|
| 5 |
|
| 6 |
|
| 7 |
|
| 8 |
|
Table 2. Hearing aid parameter considerations when fitting older adults, based on Windle et al. (2023).
17. What do you mean by considering the hearing aid fitting process?
Fitting hearing aids is a procedure with many parts, contained within a person-centred care model. Our discussion has largely focussed on some of the technical parameters that should be considered, but it should be clear that we need to determine how best, in practice, to assess their effect in clinic. For example, while verification, e.g., real ear measurements (REMs), ensures that a fitting aligns with validated prescriptive targets and provides us with a valuable and objective process of setting gain, it tells us little about other hearing aid parameters, nor the opinion of the patient, their subjective benefit, likely acceptance of hearing aids and adherence to treatment. Focussing too much on the verification process can distract a clinician from other important aspects of the hearing aid fitting process. Furthermore, slavishly following a prescription gain target (e.g. for 55 and 75 dB SPL input levels) can result in an inappropriately high compression ratio without consideration of other parameters. We therefore came up with a further set of statements (Windle et al., 2023) that I’ve summarized in Table 3. In essence, these highlight the importance of balancing the time given to verification with that given to validation and counseling. We defined “validation” as a process in which the clinician aims to provide evidence that the hearing aid settings are suitable for an individual, including all of the parameters discussed above. This may include simple tests of loudness discomfort, and speech intelligibility, more advanced techniques such as speech mapping, paired comparison approaches, or questionnaires and self-reporting tools.
In summary, clinicians should be aware of the factors that can effect speech understanding in older adults, and should undertake basic procedures in clinic to assure themselves that the all of these factors have been appropriately addressed.
| 9 |
|
| 10 |
|
| 11 |
|
Table 3. Hearing aid fitting process considerations when fitting older adults, based on Windle et al. (2023).
18. Would it help to conduct cognitive tests?
It’s unlikely that this would help currently.
First, even if we had a validated set of cognitive tests for the hearing impaired, they may not correlate to the individual preference of a hearing aid user. Second, we do not know all of the cognitive functions that support listening. Third, there are many contentious elements of cognitive tests that may or may not relate to specific elements of listening ability, and the tests can be confounded by hearing or visual impairment because they tend to be depend on listening or vision to perform the test. Finally, it is unclear whether audiologists have sufficient skills to conduct cognitive tests consistently and reliably, quite apart from the capability to extend clinical time and resources to implement them. In short, we would probably be reliant on a proper validation process, as described in Table 3, to be able to individualize settings for each user, so additional testing may not provide any benefit. Having said that, there may be tests that could represent the degree of overall ability, such as gap detection, but this would require a lot of research and validation to prove it added any useful input to the hearing aid fitting process.
19. This has all been great information. Are these all new findings?
Sadly not. The principles we’ve discussed here are not in any way new or novel. In fact, it has been suggested that audiologists pay more attention to the distortional aspects of hearing aid processing since the invention of digital hearing aids. For example, it was highlighted by Plomp (1986), since when there have been some very helpful summaries in Audiology Online by Schum (2013) and Jenstad (2011), who specifically applied these considerations to older adults. The best I can claim for my discussion with you, is that it’s a reminder of those principles with a bit of an update. The mystery is why we don’t talk about this more as audiologists, especially given that older adults are the majority of our patients.
20. Then shouldn’t audiologists know all this already?
Hmm, I feel like I might be running the risk of being run out of town by a crowd of angry audiologists here. But that shouldn’t be the case. Even so, the answer should be “yes”.
Firstly, let’s consider how complex hearing aids have become; and that audiologists would need a deep technical understanding to address all of the signal processing complexities. In some ways, hearing aids represent a “black box” for which we have limited control. Audiologists are patient-facing clinicians whose primary skill, in order to deliver person-centred care, might be regarded as counseling rather than as signal processing engineers. Secondly, information about compression speed and other parameters is rarely, if ever, provided by manufacturers or understood by clinician-facing reps. Thirdly, I’m not sure that the technical considerations discussed above are widely taught in any detail as part of audiology courses. It’s therefore hardly surprising that awareness is not high amongst audiologists. We conducted a survey of clinicians in the UK, and found that most audiologists did not know what the compression speed of their hearing aids was, nor whether they were able to change it. Our discussion here might be thought of as an attempt to increase awareness. However, in the end, I believe a concerted effort is required across hearing aid manufacturers, educators and professional bodies in audiology to increase awareness, improve training and provide the necessary information to audiologists to help them improve the overall quality of services we deliver. Although we have covered some complex issues, the application of knowledge to practice should be relatively straightforward, which is why I have tried to talk about basic recommendations with you.
The bottom line is that we should be aware of the hearing aid parameters that need be looked at, and should be prepared to change them in clinic to see which provide the best outcome for each of our patients. It might be very hard to predict what compression speed setting any individual prefers, which could be based on cognitive status, degree of hearing loss or just sheer unpredictable taste. So, in the end, we just need to try it out.
References
Gatehouse, S., Naylor, G., & Elberling, C. (2003). Benefits from hearing aids in relation to the interaction between the user and the environment. Int J Audiol, 42(Suppl 1), S77-85. doi:10.3109/14992020309074627.
Gatehouse, S., Naylor, G., & Elberling, C. (2006a). Linear and nonlinear hearing aid fittings--1. Patterns of benefit. Int J Audiol, 45(3), 130-152. doi:10.1080/14992020500429518.
Gatehouse, S., Naylor, G., & Elberling, C. (2006b). Linear and nonlinear hearing aid fittings--2. Patterns of candidature. Int J Audiol, 45(3), 153-171. doi:10.1080/14992020500429484.
Goedegebure, A., Hulshof, M., Maas, R. J., Dreschler, W. A., & Verschuure, H. (2001). Effects of single-channel phonemic compression schemes on the understanding of speech by hearing-impaired listeners. Audiology, 40(1), 10-25. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11296937.
Holube, I., Hamacher, V., & Killion, M. C. (2016). Multi-channel compression: concepts and (early but timeless) results: less can be more in the application of compression, time constants, and channels. The Hearing Review, 23(2), 20.
Jenstad, L. (2011). Considerations in Hearing Aid Fitting for Older Adults & Overcoming the Hearing Aid Barrier. Audiology Online, 6 Dec 2011. Retrieved from https://www.audiologyonline.com/articles/considerations-in-hearing-aid-fitting-793.
Kates, J. M., Arehart, K. H., Anderson, M. C., Kumar Muralimanohar, R., & Harvey, L. O., Jr. (2018). Using Objective Metrics to Measure Hearing Aid Performance. Ear Hear, 39(6), 1165-1175. doi:10.1097/aud.0000000000000574.
Plomp, R. (1986). A signal-to-noise ratio model for the speech-reception threshold of the hearing impaired. J Speech Hear Res, 29(2), 146-154. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/3724108.
Schum, D. J. (2013). The Distortional Aspect of Sensorineural Hearing Loss: What Can Be Done. Audiology Online. Retrieved from https://www.audiologyonline.com/articles/distortional-aspect-sensorineural-hearing-loss-11976.
Souza, P. E. (2002). Effects of compression on speech acoustics, intelligibility, and sound quality. Trends Amplif, 6(4), 131-165. doi:10.1177/108471380200600402.
Villchur, E. (2008). Compression in hearing aids: why Fast Multichannel Processing Systems Work Well: Villchur on the controversies surrounding compression in regard to recruitment and speech intelligibility in noise. The Hearing Review, 15(6), 16.
Windle, R., Dillon, H., & Heinrich, A. (2023). A review of auditory processing and cognitive change during normal aging, and the implications for setting hearing aids for older adults. Frontiers in neurology, 14. doi:10.3389/fneur.2023.1122420.
Citation
Windle, R. (2024).20Q: Changes to auditory processing and cognition during normal aging – should it affect hearing aid programming? part 2 – programming hearing aids for older adults. AudiologyOnline, Article 28792. Available at www.audiologyonline.com


