 From the Desk of Gus Mueller
From the Desk of Gus Mueller

Bone-conduction hearing aids have been around for quite a while. Audiology history tells us that we can thank our friends Fallopius and Eustachius back in the 1500s for enlightening us regarding the concept of hearing via bone conduction. Only a century or two later, it was reported that bone-conduction “hearing aids” were being used in the teaching of the deaf (a rod held between the teeth of the speaker and the teeth of the hearing-impaired listener). You’ve maybe even heard that Beethoven, when playing the piano in his later years, supposedly held a wooden drumstick between his teeth, with the other end on the piano’s soundboard.
With the introduction of body aids, we soon had bone receivers on a headband, the first wearable product of this type was introduced in the 1930s. This was followed in the 1950s with eyeglass bone-conduction hearing aids—more cosmetically pleasing and somewhat effective, but a maintenance nightmare. And then, a few decades later, an implantable bone-conduction product became available. If nothing else, we now had a fun acronym, BAHA for this new bone-anchored hearing aid category.
But things change. BAHA is now Baha, and refers to a product, not a category of hearing aids. Moreover, we now have several different ways to provide amplification via bone conduction other than bone anchored, so terms such as bone-conduction device (BCD) or bone-conduction hearing device (BCHD) make more sense. But, why don’t I let our 20Q guest author tell you all about it.
Marlene Bagatto, AuD, PhD, is an Assistant Professor in the School of Communication Sciences and Disorders and a Principal Investigator at the National Centre for Audiology at Western University in London, Ontario. Research in her Pediatric Audiology Strategies and Systems Laboratory focuses on policy and practice integration for infant and child hearing.
Dr. Bagatto served for many years on the Board of Directors of the Canadian Academy of Audiology, also as the president, and recently received the President’s Award from this organization. For the past five years, she has been the Chair of the Canadian Infant Hearing Task Force.
Many of you know Marlene from her work with the award-winning DSL prescriptive fitting method, including establishing standard practice protocols, correction factors for ABR-based hearing assessments, age-based pediatric RECD prediction values, methods for measuring the RECD, normative values for the SII, and pediatric outcome measurement protocols.
Once you read this excellent 20Q article, it clearly will be obvious that we can add “expert in the selection and fitting of bone-conduction hearing devices” to the impressive list above.
Gus Mueller, PhD
Contributing Editor
Browse the complete collection of 20Q with Gus Mueller CEU articles at www.audiologyonline.com/20Q
20Q: Bone Conduction Hearing Devices - Updates and Future Directions
Learning Outcomes
After reading this article, professionals will be able to:
- Explain BCHDs and the different ways they can be worn by the patient.
- Describe the candidacy criteria for BCHDs.
- List the steps involved with verifying BCHDs using a skull simulator.

1. My first question is related to terminology. You say “Bone Conduction Hearing Devices.” Same thing as what I call a BAHA?
Not necessarily. As you probably know, the term BAHA (all capital letters), is an acronym that commonly has been used the past few decades to refer to a Bone Anchored Hearing Aid. The Cochlear company, however, added some confusion a few years back when they named their BAHA product “Baha”—a patient could then have a Baha BAHA! More importantly, there are different ways to provide bone-conducted amplification than bone-anchored, which is why I prefer the term bone conduction hearing devices (BCHDs). This term, and others like it (e.g., BCD), is used in recent literature because it more accurately reflects the device category as a whole. BAHA is not an ideal term to describe the device category because not all BCHDs are worn on a surgically-placed abutment anchored to the skull, and there are more models available that offer a variety of surgical and non-surgical options. Table 1 provides a summary of key terms related to BCHD topics.
Term | Definition |
BAHA | Acronym for bone anchored hearing aid. |
Baha | Product name of a bone anchored hearing aid. |
BCD | Acronym for bone conduction device, a general term used for this device category. |
BCHD | Acronym for bone conduction hearing device, a general term used for this device category. |
Force level | Reference quantity, in micro Newtons (µN), of BCHDs. Noted as dB FL. |
In-situ | Threshold measurement procedure using built-in sound generated from the BCHD. Obtaining these “fitting” thresholds is part of the clinical workflow for fitting BCHDs. |
MFO | Maximum force output, in dB µN, for BCHDs. Provides the upper limit of the dynamic range for BCHD fittings. |
Percutaneous | Through the skin. Some BCHDs are coupled to a surgically-implanted abutment that protrudes through the skin on the mastoid bone to the cochlea. |
RETSPL | Reference equivalent threshold sound pressure level. Used when calibrating audiometric transducers to estimate audiometric zero. |
RETFLdbc | Reference equivalent threshold force level for direct bone conduction. Used when estimating audiometric zero for BCHDs. |
RHCD | Real head to coupler difference. Difference between the BCHD’s response when it is worn on the patient’s abutment versus when it is on the skull simulator. Values are applied to convert the thresholds, using the patient’s device as the transducer, to dB FL. |
Skull Simulator | Similar to coupler microphone within a hearing aid test system. BCHD is attached and vibrates in response to sound. Allows measurement, in dB FL for verification. |
Transcutaneous | Across the skin. Some BCHDs are worn on top of the skin and send vibrations across the skin on the mastoid bone to the cochlea. |
Table 1. Glossary of Terms
2. How else can BCHDs be worn, if not using a surgically-placed abutment anchored to the skull?
What you are referring to is the BCHD approach many of us are familiar with, which uses a titanium screw surgically placed into the mastoid process of the skull that protrudes through the skin of the wearer. To access sound, the BCHD processor is snapped onto the abutment and sound is collected by the microphone and transmitted through vibrations directly to the skull to stimulate the cochlea. This type of device is often described as a direct drive, percutaneous BCHD.
Another approach is an external processor placed on top of the skin that is connected magnetically to a surgically-implanted transducer under the skin, much like the way cochlear implants are worn. Sound is actively transmitted across the skin, or transcutaneously, and vibrates across the bone with this arrangement. An alternative surgical transcutaneous option passively transmits sound from the external transducer to an implanted magnet under the skin. Both surgical transcutaneous options reduce user complications, like skin infections, of having an object protruding through the skin.
Finally, for patients who are not candidates for surgical BCHDs, a non-surgical option is available. The processor is worn on the skin of the mastoid area, held in place using a soft headband or adhesive. These non-surgical, transcutaneous BCHDs are often provided to infants and young children because surgical placement usually is not considered appropriate until they are around five years of age (Wade, 2002). That said, pediatric surgical eligibility varies from country to country and with device type.
3. Are there other differences between these applications of BCHDs?
As you might expect, there are reduced skin infections and other negative surgical outcomes by using transcutaneous rather than percutaneous. Research, however, does indicate that percutaneous BCHDs provide greater benefit in hearing and improved signal quality for the listener compared to transcutaneous devices worn on a soft headband (Ganstrom et al, 2001; Pittman 2019). In particular, improved hearing in the mid- to high-frequencies of 8 to 20 dB has been noted (Reinfeldt et al., 2015). One reason for the differences in outcome is the skin transmission loss that occurs with transcutaneous devices.
Comparing the non-surgical transcutaneous BCHDs, evidence suggests that aided audiograms are similar when conducted using a device coupled to a soft headband versus an adhesive adapter (Favoreel, Heuninck, & Mansback, 2020). Further, the ability to lightly adjust the tightness of the soft headband provides comfort and supports retention, especially when used with infants. These are all important considerations when selecting a BCHD for your patient.
4. Are there some general guidelines regarding which patients are candidates for BCHDs?
Great question! Generally, patients who have conductive or mixed hearing loss and/or cannot otherwise wear an air conduction hearing aid are candidates for BCHDs. Many patients who wear BCHDs have chronic middle ear dysfunction, some with permanent consequences even after corrective surgery. Others have atresia, microtia, and/or stenosis and, depending on the seriousness of the anomaly, cannot accommodate any style of air conduction hearing aid on the pinna or in the ear canal. For these individuals, access to sound can be delivered to the cochlea through the vibrations of the BCHD.
Another group of patients who are considered for BCHDs are those who have a unilateral, profound sensorineural hearing loss (also known as single-sided deafness). A BCHD worn on the affected side gathers sound from that side and stimulates the normal cochlea on the unaffected side. For this type of hearing loss, the BCHD acts much like a contralateral routing of signal (CROS) system. Similar to a standard CROS fitting, however, there may be instances when there is unwanted noise on the BCHD side of the head, which then unfortunately is routed to the normal-hearing ear. This is a challenging listening and communication scenario for infants and young children who are not expert listeners.
Providing BCHDs, as describe above, will depend on the degree of hearing loss, and what device is available from the surgical centre. This varies across jurisdiction and becoming familiar with what is offered in your area will help as you describe the options to your patients.
5. Audiologically speaking, what degrees of hearing loss support candidacy for BCHDs?
Similar to air conduction hearing aids, BCHDs have medium and high power devices. Guidelines for percutaneous BCHDs indicate listeners with conductive hearing loss that have pure tone average (PTA = .5, 1, 2, 3kHz) bone conduction thresholds ranging from ≥45 dB HL to ≤60 dB HL PTA are suitable candidates (Colquitt et al. 2011). Listeners with mixed hearing loss who have an average air-bone-gap of about >30 dB HL are also candidates for percutaneous BCHDs. Alternatively, transcutaneous BCHDs will be suitable if average bone conduction thresholds are no greater than 45 dB HL. Keep in mind these are guidelines and will vary depending on the device and evolve with advances in technology.
6. How will I know when I should talk to my patients about BCHDs?
Babies who are born with congenital aural atresia will be identified even in the absence of universal newborn hearing screening given the physical anomaly they are born with. The discussion about early access to sound can occur with parents as soon as the atresia is identified as part of an early intervention plan.
Aside from early identified congenital anomalies, consulting the guidelines above is a good start. In addition, your clinical recommendations for BCHDs will depend on the etiology of your patient’s hearing loss and whether or not they are or will receive benefit from another type of device (e.g., air conduction hearing aid). It is also important to connect with the surgical team because they will provide insight on the plan for surgical treatment (i.e., corrective and/or BCHD) and what the outcomes are likely to be. The patients themselves may also initiate this conversation based on what they have learned from others on the care team or through their own investigations.
7. You mentioned that children are not candidates for surgical BCHD until they are older. How are these children provided with early access to sound to support spoken language development?
I’m so glad you asked! Within the well-established early hearing loss detection and intervention (EHDI) programs, infants who are born with atresia, microtia, and/or stenosis are offered the necessary services within these programs. Any surgical intervention provided by the otologist often does not occur until the child has physically grown for a few years. This is because the child’s skull must be thick enough to accommodate the current surgical devices. Therefore, rather than delay access to sound for these children, BCHDs on soft headbands or adhesives are provided within the first few months of life. The technology exists to provide infants with conductive and/or mixed hearing loss and their application supports the EHDI benchmarks of early identification and intervention guided by the Joint Committee on Infant Hearing (2007; 2019). For infants whose anatomy cannot accommodate a behind-the-ear air conduction hearing aid and/or have a condition that causes a conductive or mixed hearing loss for more than six months, non-surgical transcutaneous BCHDs are viable options that are available to support spoken language development in young children.
8. Bone conduction hearing aids have a broader application than I realized. I suspect you have done some thinking about how to fit and verify these instruments?
You are correct! However, I began thinking about it because audiologists Bill Hodgetts and Susan Scollie identified this an important area. As I recall, in 2008 Bill became the Program Director for the Institute of Reconstructive Sciences in Medicine (IRSM) in Edmonton, Alberta. He saw a need for better methods of verification for BCHDs and involved the world-expert on the Desired Sensation Level (DSL) prescriptive targets: Dr. Scollie. Their collaboration led to the development of the DSL targets for adults who wear percutaneous BCHD (Hodgetts & Scollie, 2017). These targets are available in the fitting software of some manufacturers of BCHDs as well as the Audioscan® Verifit hearing aid test equipment. Recent work from Toll & Dingemanse (2022) in the Netherlands adapted the NAL-NL2 for 18 patients who wear percutaneous BCHDs. These modified targets, however, are not widely available at this time.
9. How do the prescribed DSL bone conduction targets differ from air conduction targets?
The main difference with the DSL BC targets is a reduction in prescribed gain in the low frequencies to support the listener’s preference of their own voice while wearing the percutaneous BCHD. The details within Hodgetts and Scollie (2017) will give you a deeper understanding of the algorithm calculations and how they were mapped differently from the air conduction targets to provide good outcomes in adult listeners who wear percutaneous BCHDs. Targets for transcutaneous fittings have not yet been developed.
10. I haven’t heard you mention the RECD or probe-microphone measures at all. That’s not like you!
Correct again! I haven’t mentioned the RECD because we don’t use it to fit or verify BCHDs. Since the devices are worn around the mastoid area of the head and provide force level (FL) vibrations rather than sound pressure level (SPL), the ear canal acoustics do not need to be considered in the fitting or verification process. That said, we are able to verify BCHDs in a special coupler called a skull simulator, or while placed on the patient’s head, which is synonymous to real-ear verification of air conduction hearing aids.
If coupler verification of BCHDs is desired, a skull simulator is available within the Audioscan® Verifit, which also offers the DSL BC targets. In a nutshell, the skull simulator has an abutment, much like the one the patient had surgically-implanted, that the BCHD device is snapped onto (See Figure 1)

Figure 1. Skull simulator with bone conduction hearing device (BCHD) attached. Also pictured is a BCHD attached to a soft headband.
The skull simulator is connected to the hearing aid test system and sound is delivered to the attached device. The dB FL output, in microvolts, is measured for various speech inputs as well as the maximum force output (MFO). The BCHD fitting software is used to adjust the output of the device in the same way air conduction hearing aids are. The graph in the hearing aid test system displays the audiometric and electroacoustic information much like an SPLogram. The main difference is the y-axis reference is dB FL, not dB SPL, and the target calculations from DSL reflect this. It is great to see knowledge mobilization at work with the development and implementation of BCHD prescriptive targets within hearing aid analyzers.
11. Is there anything needed from the hearing aid manufacturer to support the application?
It certainly has been a collaborative effort and the involvement of companies that develop BCHDs is critical. One reason is that the BCHD processors vary in their MFO. This is because these devices aim to reduce internal noise which may be heard by a listener who has conductive or mixed hearing loss. Creating low-noise BCHD processors results in a reduction in the MFO and this impacts the effective dynamic range of the device. These differences are significant enough that they are necessary to include in the calculation of the prescriptive targets. Therefore, the MFO details of each model of BCHD is needed within the hearing aid analyzer to generate prescriptive targets and maximize the MFO capabilities of each device.
12. You mentioned earlier that skin transmission loss is a factor for transcutaneous BCHD fittings. Does this affect fitting targets?
Yes, it does. This is the area where I became involved in investigating fitting BCHDs. Since infants and young children are provided with non-surgical transcutaneous BCHDs on soft headbands or adhesives before they can have surgery, ensuring proper access to sound is vital. After all, it is critical for speech access to occur during these early months and years of life to prevent delays. Also, some adult patients may not be candidates for BCHD surgery, and may wear a non-surgical transcutaneous BCHD. Recall that the current BCHD targets are for percutaneous BCHD fittings, not transcutaneous. Characterization of the skin transmission loss and what variables may impact it (e.g., age, skull development, device) is ongoing work that is necessary for the development of prescriptive targets for transcutaneous BCHD.
13. When we fit air conduction hearing aids, we use the thresholds measured during audiometry. Why not use the patient’s audiometric bone conduction thresholds as a starting place for the fitting?
A great question and one that relates to the DSL BC targets themselves (Hodgetts & Scollie, 2017). Recall that the vibrations from the BCHD that stimulate the cochlea are measured in dB FL. The DSL prescription for air conduction fittings uses dB HL to calculate the targets; RECD values are applied, along with the reference equivalent threshold sound pressure level (RETSPL) to convert the dB HL thresholds to SPL for target calculation and comparison to hearing aid output measurements in the test box. With BCHD fittings, real-head-to-coupler difference (RHCD) transforms are applied to convert the thresholds, using the patient’s device as the transducer, to dB FL (Hodgetts & Scollie, 2017). Known as “in-situ” thresholds, this approach supports using the reference equivalent threshold force level by direct bone conduction (RETFLdbc; Carlsson et al, 1995) for percutaneous fittings (ANSI S3.6, 2010).
As we’ve discussed, audiometric bone conduction thresholds gathered during the assessment are useful for determining candidacy for BCHD. However, they do not support the fitting of this device category, because they are measured on a different decibel scale. Research indicates that thresholds obtained with an audiometric bone conduction transducer (i.e., B-71 or B-81) are not equivalent to thresholds measured directly with the individual’s BCHD processor (i.e., in-situ). In-situ thresholds have been shown to be 13 to 35 dB higher (i.e., worse) from 3 to 6kHz compared to audiometric bone conduction thresholds in adults who wear a transcutaneous BCHD on a soft headband (Gascon et al, 2022). Skin transmission loss, age, and processor characteristics are likely contributors to these differences and need to be accounted for in each patient’s fitting, and in-situ thresholds are a good way to accomplish this. In-situ thresholds gathered with the patient’s BCHD can be considered “fitting” thresholds (Gascon et al, 2022). Both approaches are measuring the same inner ear hearing however, the in-situ thresholds account for other variables inherent within fitting BCHDs.
14. If I remember from the earlier questions, the DSL BC targets are for percutaneous BCHDs. So what is the clinical recommendation when fitting transcutaneous BCHDs since you say that those targets have not yet been developed?
This is an area of ongoing investigation. Fortunately, two recent guidance documents have been developed to support audiologists and other health care providers who work with these devices. One is a consensus statement on all things related to bone conduction devices and active middle ear implants (Maier et al, 2022). It provides a framework for procedures and technical considerations for these devices so appropriate information can be shared with our patients. And, it probably has the most authors listed on a single paper I have ever seen!
The second is a clinical consensus document that focuses on non-surgical transcutaneous BCHDs for children (Bagatto et al, 2021). Both documents advocate for gathering in-situ or direct thresholds using the patient’s BCHD. This accounts for device differences and the known skin transmission loss effects of the worn device compared to audiometric bone conduction thresholds. Until we are able to quantify the skin transmission loss and/or device differences, this measurement is recommended to individualize the fitting to the patient.
15. If I want to do this testing in my clinic, what is the workflow?
The device should be placed on your patient as it is to be worn and connected to the manufacturer’s fitting software. Signals at various frequencies are delivered to the patient and a threshold search is conducted. Thresholds across frequency are entered into the fitting software and the DSL prescriptive formula calculates the targets and auto-programs the device. There is an option to choose DSL Child BC targets in the Verifit, though they have not been validated; only adult targets for percutaneous BCHD fittings have.
Next, the in-situ thresholds from the fitting software are entered into the hearing aid analyzer and the same prescriptive formula is chosen to calculate targets. The BCHD is snapped onto the skull simulator and speech and MFO signals are delivered and the force level output is measured in comparison to the calculated targets. For percutaneous BCHDs, adjustments to targets may be applied to achieve optimal speech access. For transcutaneous BCHDs, it is recommended that the percutaneous targets be used descriptively, rather than making adjustments, because the available targets have not been validated for transcutaneous BCHDs.
16. Other than a skull simulator within a hearing aid analyzer that has DSL BC targets, what else is required?
A quiet room, preferably sound-treated, to conduct the in-situ measures is necessary. If you have access to a booth, you can put the Noahlink in with the patient and patch it through to the driver’s side of the booth where a laptop is situated that has the manufacturer’s fitting software. It is important to note that not all clinically-available BCHDs have the ability to measure in-situ thresholds or snap onto clinical skull simulators. Keep this in mind when selecting devices and as new devices and software are released. This is an ever-evolving part of the process, and we suspect the in-situ threshold measures and use of the skull simulator will remain a routine part of the clinical verification workflow.
17. Earlier you mentioned the differences in MFO of the various BCHD processors, and that they are implemented into the hearing aid analyzer for accurate target calculations. What do I need to do regarding this at the verification stage?
Another difference when fitting BCHDs compared to air conduction hearing aids is that the particular model needs to be selected within the hearing aid analyzer (Figure 2). This step ensures that the specific MFO information is used in the calculation of prescriptive targets within the hearing aid analyzer for verification.
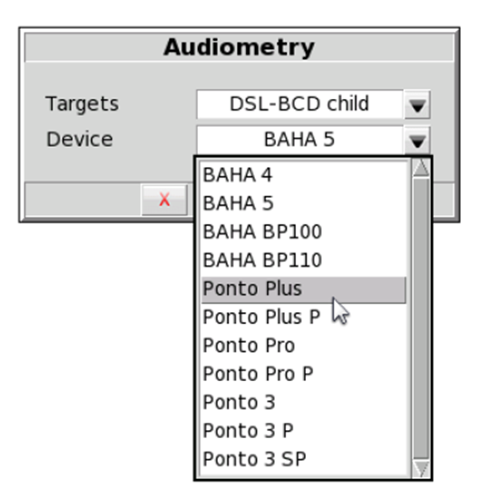
Figure 2. Example of BCHD choices in hearing aid analyzer to support the verification workflow.
18. All this talk about verification and you haven’t mentioned simple, time-honored pure-tone aided sound field testing. Is this used when fitting BCHDs?
Thank you for asking about this! Similar to air conduction hearing aids, aided testing is useful for validating the effectiveness of the fitting, not for verifying device output. Now that we have access to DSL BC targets and a skull simulator to measure the dB FL output of BCHDs in a hearing aid test system, verification that the device is providing audibility across a wide range of inputs and frequencies is possible. This objective verification procedure is ideal for young children or some adults who are not able to provide reliable aided threshold results. It also avoids the limitations inherent in aided threshold testing, such as microphone noise that can mask soft sounds which artificially increases measured aided thresholds. Aided threshold testing does not verify the audibility of speech and MFO in the way skull simulator measurements can. As such, measuring the force level output is the preferred approach for verifying BCHDs (Bagatto et al, 2021; Maier et al, 2022). Although, I recognize that not all clinics are equipped with skull simulators at this point. Therefore, aided testing is a reasonable alternative.
19. Since you mostly have been focusing on the pediatric side of these fittings, what other considerations are important?
Although in-situ thresholds are recommended, this may not always be possible with the infants and young children who are being fitting with non-surgical BCHDs as young as two months of age (Bagatto et al, 2021). Due to their lack of head and neck control in the early months of life, we use frequency-specific auditory brainstem response (ABR) to assess infant hearing. Rather than waiting until they can participate in behavioural threshold assessment reliably, we must use the audiometric bone conduction ABR thresholds for the fitting. This is not ideal, although it is our best compromise until we can define the differences between pediatric audiometric bone conduction thresholds and in-situ BCHD thresholds. The differences mentioned earlier were gathered from adults.
20. It appears there has been a lot of progress made to the fitting and verification procedures of BCHDs. What do you see as the priorities moving forward?
A few things come to mind. First, we need prescriptive targets for transcutaneous fittings, whether they are surgically or non-surgically applied. Part of this will be to further investigate the skin transmission loss and the variables that impact it so that accurate targets can be developed. Second, manufacturers should continue to develop devices that allow for in-situ threshold measurement and coupling to clinical skull simulators. These procedures are likely to remain within the verification workflow for BCHDs, so these features will be necessary for both percutaneous and transcutaneous fittings. Third, the continued collaboration among researchers, manufacturers, clinicians, and end users is critical for the success of this work. Knowledge mobilization is necessary to achieve the ultimate goal which is improved patient outcomes.
References
American National Standard (ANSI/ASA) Specifications for Audiometers, S3.6-2010.
Bagatto, M., Gordey, D., Brewster, L., Brown, C., Comeau, M., et al. (2021). Clinical consensus document for fitting non-surgical transcutaneous bone conduction hearing devices to children, International Journal of Audiology, PAP, DOI: 10.1080/14992027.2021.1939449
Carlsson, P.U., Hakansson, B., Ringdahl, A. (1995). Force threshold for hearing by direct bone conduction, Journal of the Acoustical Society of American, 97(2), 1124-1129.
Favoreel A, Heuninck E, Mansbach A. (2020). Audiological benefit and subjective satisfaction of children with the ADHEAR audio processor and adhesive adaptor, International Journal of Pediatric Otorhinolaryngology, 129, 109729.
Ganstrom, G., Bergstrom, M., Odensjo, M., & Tjellstrom, A. (2001). Osseointegrated implants in children: Experience from our first 100 patients, Otolaryngology-Head and Neck Surgery, 125, 85-92.
Gascon, A., Ostevik, A., Huynh, T., Hodgetts, W. (2022). Which threshold do we trust? A comparison of threshold measurements in adult bone-conduction device users and normal hearing adults, Hearing Research, PAP, DOI: 10.1016/j.heares.2022.108491
Joint Committee on Infant Hearing. (2007). Year 2007 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs, Pediatrics, 120(4), 898-921.
Joint Committee on Infant Hearing. (2019). Year 2019 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs, Journal of Early Hearing Detection and Intervention, 4(2), 1-44.
Hodgetts, W.E. & Scollie, S.D. (2017). DSL prescriptive targets for bone conduction devices: adaptation and comparison to clinical fittings, International Journal of Audiology, 57(7), 521-530.
Maier, H. et al. (2022). Consensus statement on bone conduction devices and active middle ear implants in conductive and mixed hearing loss, Otology & Neurotology, 43(5), 513-529.
Pittman, A.L. (2019). Bone conduction amplification in children: stimulation via a percutaneous abutment versus a transcutaneous softband, Ear and Hearing, 40(6), 1307-1315.
Reinfeldt, S., Hakansson, B., Taghavi, H., & Eeg-Olofsson, M. (2015). New developments in bone-conduction hearing implants: a review, Medical Devices: Evidence and Research, 8, 79-93.
Toll, M. & Dingemanse, G. (2022). NAL-NL2 prescriptive targets for bone conduction devices with an adaptation to device constraints in the low frequencies, Ear & Hearing, PAP, DOI: 10.1097/AUD.0000000000001235
Wade, P.S. (2002). Medical aspects of bone anchored hearing aids and middle ear implants, Trends in Hearing, 6(2), 39-44.
Citation
Bagatto, M. (2022). 20Q: Bone conduction hearing devices: updates and future directions. AudiologyOnline, Article 28318. Available at www.audiologyonline.com


