From the Desk of Gus Mueller
From the Desk of Gus Mueller

Back in 1998, I was editing a monthly column for a trade journal, and was having trouble coming up with new audiology topics. I asked my friend Jay Hall if he could come up with something that was a little different. A month later, we published Jay’s article entitled: “Hyperacusis . . . it’s real and it can hurt.” At that time, not many audiologists were doing research or publishing in the area of hyperacusis, or even talking about it. That’s all changed, which you’ll read about in this month’s excellent 20Q.
As most of you know, hyperacusis is a condition where an individual has a reduced tolerance and increased sensitivity to everyday sounds in their normal environment. This loudness discomfort can be associated with, or cause other emotional pathologies related to sound such as misophonia, a dislike of certain types of sounds (e.g., chewing), or phonophobia, a fear of sounds. While there may be varied origins of the disorder, studies have suggested that excessive auditory gain in the central auditory pathways plays an important role in the development of hyperacusis. It’s often associated with hearing loss, but people with normal hearing (at least for routine audiometry) also experience the disorder.
For our 20Q piece this month, I called on the same friend, and we’re fortunate to have an author who indeed has been studying hyperacusis for decades. James W. Hall III, PhD, holds academic appointments as Professor (part-time) at Salus University and the University of Hawaii, a position as Extraordinary Professor and the University of Pretoria South Africa, along with other adjunct and visiting professor positions in the USA and abroad. He has held many leadership roles in the American Academy of Audiology, and currently serves as Chair of the Board of Directors of the Accreditation Commission for Audiology Education.
Dr. Hall is internationally known for his hundreds of publications, and most of you own at least one of the 10 textbooks that he has published. He is perhaps best known for his engaging and informative workshops, which he has conducted around the world.
I'm guessing many of Jay's "big thoughts" occur in the summer while sailing his Cape Dory on the Muscongus Bay, not too far from his home in Waldoboro Maine (only a few miles from where his great-great-grandfather lived). In the winter months he turns those thoughts into words, writing articles like this in St Augustine Florida, no doubt to stay close to Juan Ponce de Leon's fabled Fountain of Youth!
Gus Mueller, PhD
Contributing Editor
Browse the complete collection of 20Q with Gus Mueller CEU articles at www.audiologyonline.com/20Q
20Q: Audiological Care for Patients with Hyperacusis and Sound Tolerance Disorders
Learning Outcomes
After this course, readers will be able to:
- List, define and describe sound tolerance disorders, including hyperacusis, misophonia and phonophobia.
- Describe a clinical process for assessment and management of patients with sound tolerance disorders in an audiology practice.
- Explain the role of counseling in managing patients with sound tolerance issues.
 James Hall
James Hall1. The title of this article is a little confusing. Isn't "hyperacusis" the same thing as "sound tolerance disorders"?
Hyperacusis is definitely an auditory disorder characterized by abnormally reduced tolerance to loud sounds, but there are also other types of sound intolerance involving fear or extreme dislike of selected sounds. Let's focus first on hyperacusis as audiologists are most often involved in its assessment and management. If you want, we can also review other disorders of decreased or reduced sound tolerance.
2. OK. What is hyperacusis? Is it increased sensitivity to faint sounds?
No, hyperacusis is not hypersensitive or extra-good hearing. Hyperacusis is a reduced tolerance to supra-threshold sounds. Typically, these are moderate to high-intensity sounds that are easily tolerated by most people, but are bothersome, annoying, uncomfortable, or even painful to a person with hyperacusis. In other words, environmental sounds encountered each and every day are perceived as much too loud. David Baguley and Gerhard Andersson (2007) succinctly and clearly define hyperacusis as an “Experience of inordinate loudness of sound that most people tolerate well, associated with a component of distress ... this experience has a physiologic basis ... but it also has a psychological component.“
3. In my graduate program, I didn't learn much about hyperacusis or any other disorders of reduced sound tolerance. Is there much published research on the topic?
Yes, and the number of studies on hyperacusis steadily increases. For example, a search of the literature with PubMed using the keyword "hyperacusis" showed that barely 100 articles were published back in the 1990s, whereas more than 200 articles were published between 2000 and 2009. And, we're on track to reach least 450 peer-reviewed journal articles in the decade from 2000 through 2019. This growing literature includes prevalence studies, investigations on the mechanisms or pathophysiology of hyperacusis, and a number of papers on management options (Fackrell et al., 2017). There are some excellent review articles on hyperacusis (e.g., Baguley, 2003; Baguley & Hoare, 2018), and even several books devoted to the topic (Baguley & Andersson, 2007; Fagelson & Baguley, 2018). And, David Baguley, a world-renown expert on hyperacusis, provided an excellent update on hyperacusis in your 2017 AudiologyOnline 20Q article.
4. Let's say I see that a patient with hyperacusis is on my clinic schedule. Do you have any practical suggestions, or perhaps a step-by-step protocol for my assessment of this patient?
Yes. But you need to take a few preliminary steps before you even begin providing these services. First, you need to educate your referral sources, including pediatricians, about disorders of decreased sound tolerance. Let them know that you are able to help children and adults whose chief complaint is increased sensitivity to loud sounds. This includes patients who are annoyed or who experience distress, or even pain, whenever they hear everyday environmental sounds. Encourage these referral sources to use ICD-10-CM code H93.233 (hyperacusis, bilateral) for reimbursement purposes. Don't forget to also discuss this exciting plan with your front desk staff and patient scheduling team. You'll probably want to create a hyperacusis category in your scheduling template for any patient with chief complaints about problems with loud sounds, as well as review your case history form to determine if updates are in order. One more preliminary step: create a page on your clinic website with an upbeat summary of what you can do to help prospective patients with disorders of decreased sound tolerance.
5. Good suggestions. So, a patient is now on my schedule for hyperacusis. What's next?
Two steps are really important before you get to the formal assessment of a patient with a chief complaint of intolerance to loud sounds. First, beginning with your initial encounter with the patient, even if it's via email or telephone before the actual clinic visit, give the patient or parent of a child hope. Sincerely express concern and demonstrate compassion about their intolerance to loud sounds. At the same time, confidently inform the patient that much is known about the problem and that you will do your best to help them. Also, review the patient's history with special attention to any neurological diseases or other disorders that may have sound intolerance as a feature. Ask the patient if there are any specific sounds or listening settings that are especially bothersome. Sources of bothersome sounds often include vacuum cleaners, hair dryers, children crying, and sirens. And, do your best to assess the impact of the patient's sound intolerance on daily activities and quality of life. And, finally, before you begin the actual auditory assessment you should assure the patient that you will not use high volume levels for the test sounds. Still, always encourage patients to alert you immediately if they experience annoyance or discomfort when hearing any of the test sounds.
6. I'd like to hear more about the history for patients with decreased sound tolerance, and some of the diseases that I should ask about.
Ok, let's consider your question as part of an overall protocol for a comprehensive assessment that's appropriate for any patient with concerns about loud sounds. Important steps are shown in Figure 1.
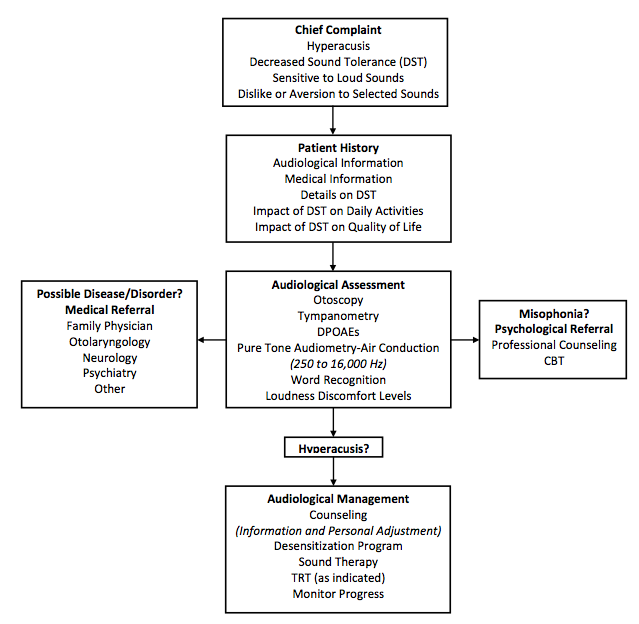
Figure 1. Protocol for the assessment of a patient with concerns about loud sounds.
Following otoscopy, I begin with tympanometry to rule out middle ear dysfunction. It's a good idea to alert the patient that they will hear a buzzing sound before you insert the aural immittance probe. Some patients will find the probe tone uncomfortably loud. Do not try to measure acoustic reflexes. The high stimulus intensity levels may cause discomfort, distress, or even pain. Next, I record distortion product otoacoustic emissions (DPOAEs) across a frequency range of 500 to at least 8000 Hz (about 5 frequencies per octave) with f1 and f2 stimulus intensity levels of 65 and 55 dB SPL. Again, remind the patient that you will discontinue the test if the sounds seem too loud, but also point out that test findings will be very helpful in learning more about their sound tolerance problem. In my opinion, DPOAE findings are very important because they almost always will verify to you and to the patient that cochlear function is entirely normal.
7. What about pure-tone audiometry? I assume we need to record an audiogram as part of the assessment.
Of course, you need to record an audiogram but there are a few minor differences in how you perform pure-tone audiometry with this patient population. Begin at low-intensity levels of about 20 or 30 dB HL and descend from there. Most patients will have normal hearing sensitivity so higher stimulus levels aren't needed. And, perform pure-tone audiometry for frequencies above 8000 Hz, up to at least 16,000 Hz if possible. Finally, if the patient has no history of middle ear disease, and tympanometry and OAE results are normal, there's no need to perform bone conduction pure-tone audiometry. While you have the patient in the sound room, take an additional few minutes to measure loudness discomfort levels for pure-tone and speech signals. Be sure to use an ascending intensity approach (starting about 25 dB HL), progressing very gradually to the level the patient reports as uncomfortable. Keep in mind that level may be only 50 to 60 dB HL. Diagnostic assessment permits quick and confident differentiation of hyperacusis versus loudness growth patterns common with cochlear hearing loss. The findings for otoacoustic emissions measurement and pure-tone audiometry are almost always normal in patients with decreased sound tolerance disorders.
8. I’ll use your recommendations. I recently heard the unusual word “misophonia.” Is misophonia the same thing as hyperacusis?
As I already indicated, the term hyperacusis implies a reaction or intolerance to the physical characteristics of most sounds. The term “misophonia” has a different meaning. Misophonia is a distinct irritation or dislike of specific soft sounds (Jastreboff & Jastreboff, 2013; Spankovich & Hall, 2014). The word literally means “hatred of sound.” Patients with misophonia often complain about very distinct sounds, often those produced by a family member during activities like chewing, swallowing, and lip-smacking. The phrase Selective Sound Sensitivity Syndrome or 4S is used by some to describe the same phenomenon, but misophonia now seems to be preferred among audiologists and other health professionals, like psychologists.
9. While we’re talking about terminology, what about phonophobia?
As you can probably figure out, the word phonophobia means fear of sound, although most patients express anxiety rather than fear about hearing specific sounds. The patient's discomfort in hearing certain sounds involves anticipation, learning, and conditioning. This type of sound intolerance is experienced by persons during a migraine attack. A diagnosis of phonophobia has psychological implications for assessment and management so the term is falling out of favor among audiologists who evaluate and treat patients for hyperacusis. To reiterate, the term “decreased sound tolerance” is now used in referring to patients with various disorders involving intolerance to sound including hyperacusis, misophonia, and/or phonophobia (Jastreboff & Jastreboff, 2013).
10. I would think that some of these patients would need to be referred to a medical specialist or some other health professional.
You are right. Information about the patient’s decreased sound tolerance must be considered in the context of overall health status. Decreased sound tolerance, and especially hyperacusis, may be a symptom of a variety of central nervous system disorders like depression, migraine, post-traumatic stress disorder, Tay Sach’s disease, Ramsay-Hunt Syndrome, and multiple sclerosis to name just a few. Hyperacusis is also reported by 40 to 50% of patients with bothersome tinnitus. If the patient history raises any concerns about the possibility of a disease or a medical disorder, your management should include referral to an appropriate health care professional. For example, a patient with a history suggesting possible central nervous system disorder like migraine or depression would be referred to a neurologist or a psychiatrist. A child with sensory disturbances in addition to hyperacusis, including intolerance to light and tactile stimulation, would be referred to an occupational therapist for evaluation of possible sensory integration disorder. Patients taking medications that are associated with hyperacusis need to consult with their family physician or the physician prescribing the drugs. And, some patients with hyperacusis benefit from consultation with a psychologist who has expertise in cognitive behavioral therapy (Andersson, 2013).
11. You mentioned that sound tolerance disorders can occur in children as well as adults. Is decreased sound tolerance associated with any specific pediatric diseases?
Absolutely. Decreased sound tolerance including hyperacusis is often a distinct characteristic in children with Williams syndrome, autism spectrum disorder (ASD), and even auditory processing disorders (Rosing, Schmidt, Wedderkopp, & Baguley, 2016). I should also point out here that hyperacusis is sometimes cited as an adverse effect of certain prescription drugs that affect the central nervous system including Effexor, Prozac, Zoloft, and others.
12. Let's say I have a patient who has decreased sound tolerance yet none of those serious diseases or disorders. What can be done for him or her?
I'll begin my answer to that reasonable question with a declarative statement: All patients with decreased sound tolerance can be helped. One of the first steps in management is to thoroughly explain the problem to the patient or the parents if the patient is a young child. It’s reassuring for patients and parents to realize that decreased sound tolerance is not uncommon and that there are experts available who can make an accurate diagnosis and coordinate effective treatment for the problem. Audiologic test results almost always confirm that the patient’s hearing sensitivity is entirely normal. Most patients with hyperacusis are worried about loud sounds damaging their hearing. A patient's worry and extreme concern are quite reasonable when you realize that loud sounds produce severe discomfort and even the sensation of pain. It’s very reassuring for a patient to know that comprehensive hearing test results are normal, and even very sensitive measures like DPOAEs show no evidence of inner ear dysfunction. Counseling is very important. In fact, for most patients with decreased sound tolerance, counseling is intervention.
13. Counseling is intervention. I like that phrase. Are you suggesting that counseling is particularly important for patients with decreased sound tolerance?
Yes, counseling is essential for any patient with decreased sound tolerance. And, it’s directed to the specific problems the patient is experiencing. Counseling inevitably includes a recommendation for sound enrichment. In response to their discomfort with loud sounds, patients with hyperacusis tend to reduce their exposure to environmental sound stimulation. Some patients even regularly use earplugs or earmuffs to “protect” their ears from loud sounds. Unfortunately, these well-intentioned strategies further decrease tolerance to sound. Patients are strongly encouraged to surround themselves with soft and relaxing sound, and to progressively increase their exposure to typical everyday sounds. Evidence suggests that sound therapy is effective in some patients with hyperacusis (Pienkowski, 2018; Fackrell et al., 2017)
Counseling must include a simple review of what is known about the underlying mechanisms of hyperacusis. Patients need to understand that their reaction to loud sounds is due to activation of parts of their brain that control emotional and fear responses to sound. For successful management of hyperacusis, patient knowledge is powerful. Obviously, the explanation of the mechanisms of hyperacusis is given at a level that the patient can understand.
14. Is professional counseling from other disciplines ever needed for this challenging patient population?
Definitely. For most hyperacusis patients I begin the management process with intensive counseling and recommendations for sound enrichment. Patients are regularly followed either with clinic visits or at least email communication to monitor progress. A small proportion of patients with debilitating hyperacusis show inadequate progress. I then recommend consultation with a psychologist, and preferably one with expertise in cognitive behavioral therapy (Juris, Andersson, Larsen & Ekselius, 2014). Audiologists are more likely to refer patients with misophonia for professional counseling or multi-disciplinary (e.g., psychological and psychiatric) evaluation and therapy (Spankovich & Hall, 2014).
15. What other treatment options are available for patients with decreased sound tolerance?
A program to desensitize the patient to specific sounds is usually effective, in addition to general sound enrichment (Jastreboff & Jastreboff, 2014; Frackell et al, 2017). Here’s how it works. You first question the patient or the parent of a child about the sounds that are most bothersome. Let’s say the list includes sounds from a vacuum cleaner, a barking dog, a child crying, thunder, a slamming door, and an ambulance siren. The patient or parent records the sounds on some device or, if that’s not possible, downloads sound clips from the internet. Then the patient listens to the sounds for a period of about 15 minutes at least 4 or 5 days per week.
16. That's interesting. Can you provide a few more details about how this training works?
Sure, I’ll even give you an example. First of all, it’s important for the patient to control the volume of the bothersome sounds during the desensitization sessions and to gradually increase the loudness from week to week. If the patient is a child, it’s also important for the parent to talk rationally with the child about the sounds. For example, “Emily, I know an ambulance sound is scary. I don’t like to hear the sound of an ambulance siren because it means someone is sick. But the person in the ambulance is going to a hospital where they’ll get better. And, you’re not sick or injured in an accident. The ambulance sound will be over soon and it won’t hurt your ears.” It’s quite remarkable how soon a patient with hyperacusis will begin to tolerant sounds that were once so bothersome.
17. Are there other evidence-based treatment options that are proven to help patients with decreased sound tolerance?
Tinnitus retraining therapy (TRT) is one well-defined approach for patients who require more extended management than what we’ve already talked about (Jastreboff, 2007; Jastreboff & Jastreboff, 2013; Jastreboff & Jastreboff, 2014). There are actually dozens of papers describing findings for TRT in children and adult with hyperacusis. Fackrell and colleagues (2017) published an excellent review article describing a meta-analysis of clinical intervention outcomes for hyperacusis in adults.
18. I thought tinnitus retraining therapy was only appropriate for tinnitus. It’s appropriate also for hyperacusis and other patients with decreased sound tolerance?
Absolutely, the underlying principles and rationale for the use of Tinnitus Retraining Therapy apply also for hyperacusis. Indeed, audiologists often apply features of TRT, such as directive counseling and sound enrichment, in the routine management of most patients with hyperacusis (Spankovich & Hall, 2014). I summarized the directive counseling component of TRT when I answered your question about how counseling is intervention. Directive counseling explains to the patient the role of increased gain within the central nervous system and the emotional (limbic system) and fear (autonomic system) responses to sound in hyperacusis. Directive counseling also educates the patient about how sound therapy can take advantage of brain plasticity to promote habituation or readjustment to sound. I should clarify here that evidence in support of TRT as a management option for hyperacusis does not extend to patients with misophonia. Professional counseling is a more appropriate option for that specific form of decreased sound tolerance
19. All this sounds very positive but there must be some patients with severe decreased sound tolerance who just can’t be helped.
Not really. All patients with decreased sound tolerance can be helped. That’s my first message to a patient with hyperacusis. An appropriate treatment strategy based on an accurate assessment and diagnosis will improve quality of life for all patients with decreased sound tolerance. It’s true that some patients will progress more rapidly and an occasional patient will not return to normal sound tolerance, but all can be helped.
20. Any new treatments for decreased sound tolerance on the horizon that we haven’t covered yet?
I’ve been around this business long enough to know that new and improved treatment options are inevitable as long as research efforts continue. As I mentioned earlier in our discussion, basic and clinical research on hyperacusis has increased dramatically in recent years. I refer you again to recent review articles for an update on the evidence-based clinical interventions (e.g., Fackrell et al., 2017). I have no doubt that patients will benefit soon from our increased understanding of these fascinating disorders.
References
Andersson, G. (2013). The treatment of hyperacusis with cognitive behavioral therapy. ENT & Audiology News, 21, 86-87.
Baguley, D.M. (2003). Hyperacusis. Journal of the Royal Society of Medicine, 96, 582-585.
Baguley, D.M., & Andersson, G.A. (2007). Hyperacusis: mechanisms, diagnosis, and therapies. San Diego: Plural Publishing.
Baguley, D.M., & Hoare, D.J. (2018). Hyperacusis: major research questions. HNO, 66, 358-363.
Fackrell, K., Potgeiter, I., Shekhawat, G.S., Baguley, D.M., Sereda, M., & Hoare, D.J. (2017). Clinical interventions for hyperacusis in adults: A scoping review to assess the current position and determine priorities for research. BioMed Research International, Article ID 2723715. Retrieved from: https://doi.org/10.1155/2017/2723715
Fagelson, M., & Baguley, D.M., (Eds.), (2018). Hyperacusis and disorders of sound tolerance: Clinical and research perspectives. San Diego: Plural Publishing.
Jastreboff, P. (2007). Tinnitus retraining therapy. Progress in Brain Research, 166, 415-423.
Jastreboff, P., & Jastreboff, M. (2013). Using TRT to treat hyperacusis, misophonia and phonophobia. ENT & Audiology News, 21, 88-90.
Jastreboff, P. & Jastreboff, M. (2014). Treatments for decreased sound tolerance (Hyperacusis and misophonia). Seminars in Hearing, 35(2), 105-120.
Jüris, L., Andersson, G., Larsen, H.C., & Ekselius, L. (2014). Cognitive behaviour therapy for hyperacusis: a randomized controlled trial. Behav Res Ther, 54, 30-37. doi:10.1016/j.brat.2014.01.001
Pienkowski, M. (2018). Rationale and efficacy of sound therapies for tinnitus and hyperacusis. Neuroscience. pii: S0306-4522(18)30608-0. doi: 10.1016/j.neuroscience.2018.09.012
Rosing, S.N., Schmidt, J.H., Wedderkopp, N., & Baguley, D.M. (2016). Prevalence of tinnitus and hyperacusis in children and adolescents: A systematic review. BMJ Open, 6:e010596. doi:10.1136/bmjopen-2015-010596
Spankovich, C., & Hall, J.W. III. (2014). The misunderstood misophonia. Audiology Today, 26(4), 14 - 23.
Citation
Hall, J.W.III. (2019). 20Q: Audiological care for patients with hyperacusis and sound tolerance disorders. AudiologyOnline, Article 24772. Retrieved from www.audiologyonline.com