 From the Desk of Gus Mueller
From the Desk of Gus Mueller

Have you heard the news? Over-the-counter (OTC) hearing aids are coming soon! Seems like we’ve been hearing that for 5 years or more. We have. As we now are in the second ½ of 2022, I think we can say that yes, they probably really are coming soon.
The arrival of OTC hearing aids has some audiologists, rightfully so, concerned that this new product and distribution system will affect their livelihood. Potentially, this could impact not just private practice audiologists, but also those in clinics and hospitals, and even university training programs. What to do? One approach is to do nothing. After all, direct-to-consumer hearing aids are ubiquitous, and have been around a long time. It seems we have survived them just fine.
For the sake of our discussion here, however, let’s assume it’s best to do something. One suggestion has been to expand and unbundle all hearing aid related services. Be that person that all these OTC buyers go to when their aid is dead, their receiver is plugged, or they can’t figure out how to put it in their ear. Not fun, but maybe would work. Another suggestion is to make the counter your counter. The OTC hearing aid user then already will know your practice when it’s time to transition to more traditional hearing aids (if that ever happens).
A somewhat different approach to supplement revenue, which also has been discussed frequently, would be to start providing other audiologic services not directly related to the sale of hearing aids. Rehabilitative audiology? A center for APD evaluations? Increased pediatric referrals? Industrial audiology? Or, you could simply “follow the endolymph,” and differentiate your practice by conducting neurodiagnostic vestibular-balance testing. This latter notion is intriguing, but does require a bit more serious thought, as it likely would involve acquiring some rather expensive equipment, and maybe a little extra training. But would it be worth it? Seems like a worthy topic for our monthly 20Q.
I think it was Benjamin Franklin who said: “If you want something done, ask a busy person to do it.” This proverb prompted our 20Q Question Man to track down one of the busiest and most noted international experts on vestibular-balance evaluations, Richard Gans, PhD. Dr. Gans is the Founder and CEO of The American Institute of Balance (AIB). He is known world-wide for his workshops, scientific articles, textbook chapters, and books. In addition to his many publications, he has developed numerous diagnostic and treatment protocols for imbalance, oscillopsia and BPPV. Several of you reading this likely have attended one of his training workshops, as over the years, his group has trained more than 13,000 professionals.
Dr Gans is a past president of the American Academy of Audiology, and has received the Lifetime Achievement Award from this organization. His numerous honors and awards also include an Honorary Doctorate from A.T. Still Health Science University.
Yes, OTC hearing aids are coming, and yes, we might have to change a few things that we do. Adding vestibular-balance testing is an option, and if that’s the route you choose, this excellent review by Richard certainly will get you started in the right direction.
Gus Mueller, PhD
Contributing Editor
Browse the complete collection of 20Q with Gus Mueller CEU articles at www.audiologyonline.com/20Q
20Q: Adding Vestibular-Balance Neurodiagnostics to Your Audiology Practice
Learning Outcomes
After reading this article, professionals will be able to:
- Explain the benefits of adding vestibular-balance neurodiagnostics to an audiology practice.
- List the tests in a comprehensive neurodiagnostic vestibular-balance battery.
- Discuss the audiologist's role in the treatment and management of various vestibular and balance disorders/conditions.

1. It seems like suddenly everyone is talking about adding vestibular and balance diagnostics in their audiology practice. What’s going on?
Well, several things. First, reimbursement is at very high levels and there are new CPT codes for the VEMP tests, which have pushed the overall reimbursement rate per patient to over $600. This excludes the classic audiology tests, which add another $100. Secondly, there is a huge, underserved population who needs access to evidence-based neurodiagnostics to help with the management of dizziness, vertigo, and elevated fall risk. Thirdly, the professional audiologist wants to practice to their highest level of licensure and scope of practice and differentiate themselves from competitors who are still limited to a largely hearing aid dispensing business model. When you consider the competition from manufacturer-owned clinics, online, big-box, and whatever the OTC products may siphon off, why would you want to limit your practice to similar products which are available through an emerging market with a wide variety of distribution points?
2. Why do you think that audiologists, with a few exceptions, have not previously seriously considered adding vestibular neurodiagnostics? It has been part of our scope of practice for decades.
That’s a great question. Not only has the American Academy of Audiology (AAA) and the American Speech-Language-Hearing Association (ASHA) included vestibular evaluation within our scope, but virtually all states with licensure do as well. More importantly, so do the Centers for Medicare & Medicaid Services (CMS), Medicare, Medicaid, nearly all private insurers, and Medicare Advantage Plans. Twenty-eight states with vestibular-specific Local Coverage Determination (LCD), which I co-authored in 2006, limit Medicare payment for the family of vestibular codes to audiologists, otolaryngologists (ENT), and neurologists. This excludes all other healthcare professionals.
3. That seems like a good group to be connected with!
You’re right. In essence, the government, to ensure a higher standard of care and to reduce fraud by unqualified providers, has placed audiologists in an enviable position. Therefore, it’s even more surprising that only a relatively small number of audiologists have embraced this. I believe there are three primary reasons that this avoidance has occurred, and all due to misinformation or disinformation: 1.) The idea that reimbursement is poor, 2.) The cost of entry due to equipment, and 3.) The lack of training and availability of excellent clinical sites during AuD education.
4. Let’s say I’d like to get started with neurodiagnostic testing. What tests would you say should be included in the neurodiagnostic vestibular-balance battery?
The family of neurodiagnostic tests includes a wide variety of tests that will provide the most comprehensive picture of peripheral and central vestibular function as well as the status of the condition, i.e., acute, chronic but uncompensated, or partially or fully compensated. Likewise, they help provide a full understanding of the status of the dysfunction, the level of functional impairment (what are the patient’s physical limitations), as well as best triage and clinical pathways for the patient.
Here is the full list:
- Auditory Brainstem Response (ABR)
- Electrocochleography (ECochG)
- Videonystagmography (VNG) with/without calorics
- Rotary Chair
- Ocular vestibular myogenic potential (oVEMP)
- Cervical vestibular myogenic potential (cVEMP)
- Postural Stability (Computerized Dynamic Posturography, Gans Sensory Organization Test, etc.)
- Neurocognitive screening
- Video Head Impulse Test (vHIT)
- Dynamic Visual Acuity (DVA) Test
Naturally, every patient does not require all these tests. These are available to be selected by the clinician or referring physician based on the nature of each patient's complaints and symptoms. However, patients cannot always verbalize the nature of their symptoms in a manner that will allow the clinician’s “best guess” of appropriate testing with 100% certainty. The patient may already have spent weeks or months and hundreds of dollars in insurance co-pays trying to get a definitive answer to solve their debilitating condition. So, why not provide the patient with the most comprehensive evaluation possible, so as not to prolong the patient's chronic and often debilitating condition?
5. Makes sense, but I have to admit, I’m not familiar with all those tests. Could you walk me through what they are, and how and why they are valuable?
Each of the tests looks at a different part of the peripheral and central vestibular system (Gans & Rutherford, 2020). An overview of each test, its pros-cons, and its usefulness in therapy interventions are shown in Table 1. Perhaps most importantly, each test can provide the functional status of a specific component of the mechanism, which is far more complex and intricate than the cochlea, for example. A good metaphor is a photograph of a house. You can see there is a roof, a door, and windows, so structurally it may look like a fine house. However, you cannot tell from the photograph if the lights work, if there is running water, and whether the plumbing is working. Therefore, even patients who have normal MRI and imaging benefit from comprehensive neurodiagnostic testing. Imaging may tell us if the system is intact from a structural and anatomic perspective, but how does it function?
This focus on the functional impairment caused by the congenital or acquired condition or disorder is a key to engaging the best medical treatment, management, or (re)habilitation strategies specific to the patient’s unique symptoms. The efficacy (how effective it is) and efficiency (how timely it works) of vestibular rehabilitation therapy (VRT), balance retraining therapy (BRT), and fall prevention strategies are directly related to an accurate assessment. That assessment should take into account which segments of the system are partially or fully impaired, what remains intact, and what is resolved (compensated) or remains unresolved (non-compensated). Since most patients with chronic symptoms (except for Meniere’s or vestibular schwannoma), will likely be referred for non-medical management, the most accurate assessment of the functional impairment will save costs to the insurers. It will also save patients in co-payments, and the inconvenience of needless travel and appointments.
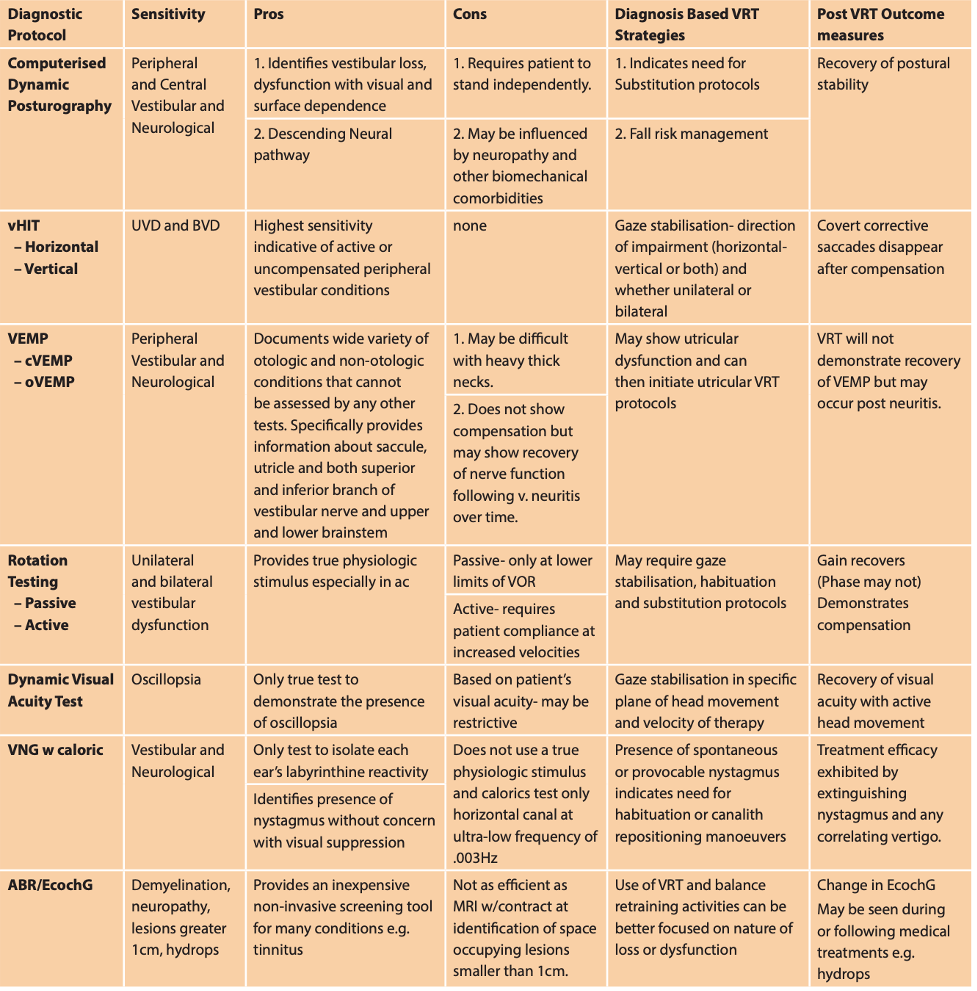
Table 1. Overview of neurodiagnostic tests.
6. That looks like a lot of tests and equipment. What is really needed regarding equipment, space, and time to run all these tests?
The good news is that all the equipment can easily fit into a space as small as 100 square feet, about the size of a large closet. The equipment that should be considered the minimal basics to be a neurodiagnostic vestibular-balance facility is:
- Rotary Chair
- VNG with caloric irrigator
- Evoked Potential system (ABR, ECochG, cervical and ocular VEMPs)
- Gans SOT (AIB Balance Performance Foam)
These tests can all be run with the patient in the rotary chair that reclines for Auditory Brainstem Response (ABR), positional tests, and calorics. The rotary chair rotates at slow speeds controlled by software at 360 degrees and is a true physiologic stimulus, unlike the caloric test which is completely based on thermal convection of the inner ear fluids, not movement. The Rotary Chair thus is a far better test and provides information about recovery and compensation. Excluding the full classic audiology battery, all the tests listed in Table 1 can be run comfortably within 90 minutes.
7. That sounds reasonable. From a business perspective, how does the return on investment (ROI) work out?
Financial information you can use to calculate ROI is shown in Table 2. The reimbursement amounts shown are the national average. California and New York are somewhat higher.
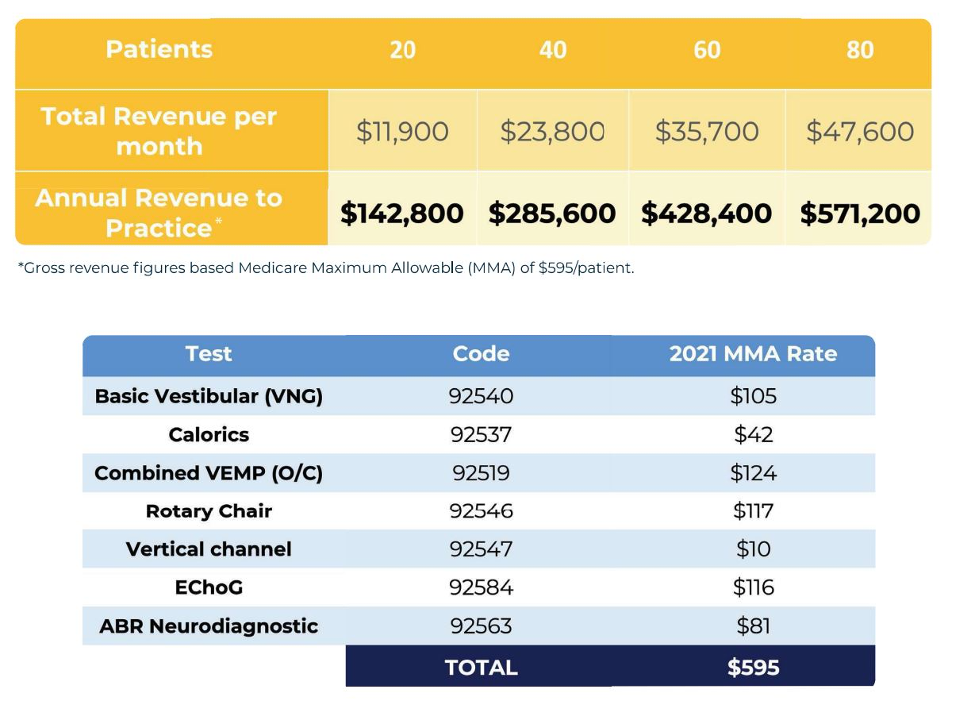
Table 2. Upper table: Financial projection by test and number of patients monthly; Lower table: Test, code and 2021 MMA rate.
The cost of equipment alone is approximately $94,000 to conduct all the tests listed in Table 1. If this were amortized over 60 months, the monthly payment is about $1,800 per month. So, three (3) patients per month pays for the equipment.
8. I have heard that many patients who undergo neurodiagnostic vestibular-balance testing also have hearing loss. Is that true?
Yes, in fact, it is estimated that upwards of 30% of patients who undergo neurodiagnostics are found to have a bilateral sensorineural hearing loss (SNHL), severe enough to be considered candidates for hearing aids. Naturally, when this is discussed as part of the patient’s plan of care, many are interested in pursuing amplification. This is especially the case when presented with the data from the Johns Hopkins Center suggesting a much higher incidence of falls, as much as 3-4 times, in all age groups who have untreated hearing loss (Deal et al., 2019). Our clinic data suggests that on average, 30% of those who undergo testing and are found to have treatable SNHL move forward with the purchase of hearing aids.
9. I have a few physicians that already refer to me, but should I be concerned that additional referrals for this extended testing aren’t going to happen?
I don’t think so. Dizziness is the #1 complaint heard by physicians from patients over the age of 65, and the #3 complaint told to physicians for all age groups, preceded only by headache and backache. According to the National Institutes of Health (NIH), more than 90 million Americans seek care for dizziness every year. A recent article in the Journal of Otolaryngology-Head and Neck Surgery (Adams & Marmor, 2022) looked at data from 805,454 patients seeking care for dizziness at hospital emergency departments and clinics and found that there was no consistency in care or treatment offered. The authors concluded, “This unwarranted variation evidences uneven care quality, cost inefficiency, and potential over-or-underuse of services”. Therefore, well-trained and competent audiologists will garner a reputation and long-term following as a valuable resource to the medical community in helping their patients with a wide array of equilibrium conditions causing dizziness, vertigo, and falls.
10. That’s a lot of people! What are the most common causes of dizziness or vertigo?
When you consider the many causes, it’s easier to categorize these into otologic vs. non-otologic and acquired vs. congenital. Likewise, many common medical conditions such as diabetes, hypertension, migraine, cardiovascular disease, and neurodegenerative conditions all are frequent comorbidities. Table 3 identifies many of the common causes.
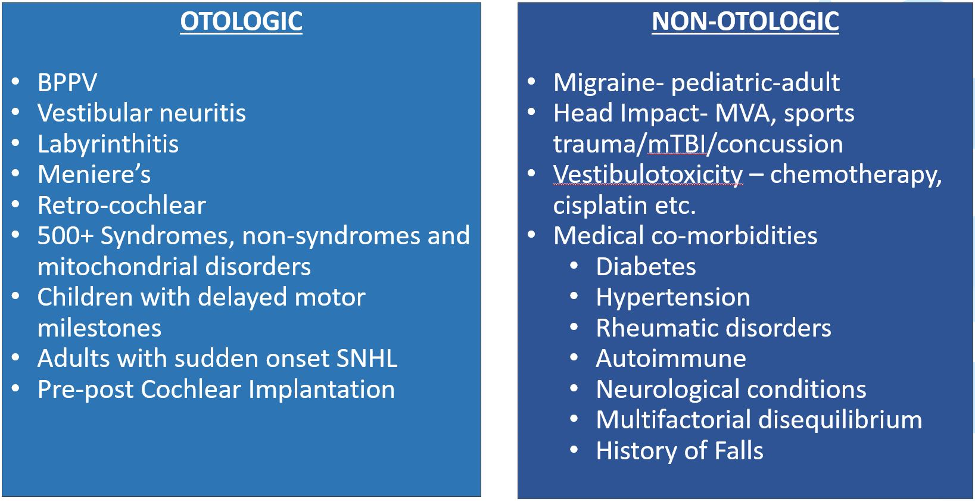
Table 3. Common otologic and non-otologic conditions causing dizziness and vertigo.
11. What treatments are available?
Otologic conditions such as Superior Canal Dehiscence Syndrome (SCDS), Meniere’s Disease (MD), vestibular schwannoma, and vestibular neuritis will require surgical or medical management. These conditions, however, are greatly in the minority of cases that will be seen in the general population and in a fully operating “diagnostic vestibular-balance” clinic, unless it is otology-based. The most common otologic condition by far is benign paroxysmal positional vertigo (BPPV). As our patients often say, “It’s only benign if you’re not the one who has it!” Fortunately, over the past 30+ years, with the evolution of canalith repositioning maneuvers (CRM), almost 100% of patients with BPPV can be successfully treated, regardless of the nature of the canal involvement. For others with chronic symptoms related to an acquired unilateral peripheral vestibular hypofunction or complete loss, vestibular rehabilitation therapy (VRT) has become the gold standard for recovery and return to everyday activities.
12. It sounds like the treatment for BPPV really works well. Is that why the treatment has become so popular?
Absolutely. At our clinics, since 1994 we have treated over 15,000 patients with great success. On average, the typical patient only requires 1.25 treatment visits. We are proud to say that our six research articles on BPPV are referenced as the gold standard of care by most major associations and societies. There are now many canalith repositioning maneuvers, e.g., Epley, Gans, Herdman, and Semont, for treatment of the posterior semicircular canal and others specifically for the horizontal and superior canals. To produce excellent outcomes, it’s critically important for the clinician to be certain of the ear(s) and canals involved. It is not uncommon to have bilateral BPPV and multiple canals post-head trauma.
13. You also mention success with vestibular rehabilitation therapy? Is it like tinnitus retraining therapy (TRT)?
Not really. VRT was first introduced in the late 1940s. Since then, it has evolved into a clinical science with a clear evidence-based foundation and hundreds of well-documented research articles, textbook chapters, and very good science from investigators worldwide. It is universally recognized as the gold standard of non-medical treatment for patients with chronic and often debilitating symptoms. These symptoms may include motion-provoked dizziness, a sense of after-motion, or a reliance on the senses of vision or touch to keep one’s balance.
Categories of treatment may include adaptation, habituation, and substitution. These are then combined according to the functional impairment of the patient and through a systematic approach to re-create the symptoms through repetitive movements. The goal is to strengthen the remaining or residual function of the damaged system but in the brain, not the ear. This is termed central compensation and is most likely occurring at the level of the brainstem and cerebellum. Unlike TRT, it is not teaching the patient to manage the symptoms or learn to live with it with lesser annoyance. Rather, the treatment ameliorates or extinguishes the symptoms; it is not just providing a tolerance strategy. It is very different, as we are changing the brain's actual response to motion and the environment.
14. It seems that for some patients, we will be working collaboratively with physical therapists and occupational therapists. How does that work?
Great question, let me first provide some background. According to the American Physical Therapy Association (APTA), as of 2019, there were approximately 319,000 physical therapists (PT) licensed in the USA and about 126,000 occupational therapists (OT). Most are employed by large corporations, with hundreds of locations, while a minority are in private practices, hospitals, and nursing facilities. Most PT and OT academic programs do introduce vestibular topics but to a very limited degree. Most PT and OT professionals wishing to gain competency and certification do so through post-graduate training. The two best known trainings are the Emory University Program and our own, American Institute of Balance (AIB) workshops (see www.Dizzy.com/workshops). These are intense curricula requiring at least 28 hours of academic-didactic and hands-on manual training with an examination.
15. Is a physician referral also involved when working with PTs and OTs?
Although many states allow direct access to PT and OT, Medicare and most 3rd party payers mandate a physician’s referral. The therapists must create a Plan of Care/Treatment, which must state their goals and objectives for the patient, which are to be met within a reasonable timeline. The referring physician receives this information as well as the outcome at the time of the patient’s discharge from therapy. PT and OT services are billed in 15-minute units. The reimbursement rate per 15-minute unit may range from $16-24 depending on payer, locale, negotiated rates, etc. Likewise, Medicare and many MCO payers will have limitations on the number of visits available to the patient.
16. So, trying to figure out what’s going on with a patient without them first undergoing testing wastes time and is not helpful?
Exactly. The key for the therapist is to be efficient, and efficacious and to have available as much information as possible regarding the patient’s functional impairment. That requires an understanding and collaboration with the audiologist providing the neurodiagnostic testing. For example, there is no specific VRT therapy to treat a 60% right unilateral weakness on caloric tests or an absent c-VEMP in the right ear. Does the patient present with oscillopsia (blurred vision with head movement)? If so, in what directions *e.g., horizontal, vertical), and at what frequencies of head movement? This is where the audiologist’s role and guidance to the therapist are so priceless. Without this information, the therapist will be left to guess what’s going on and simply try to help with therapeutic VRT protocols the best they can.
17. We know that falls in the elderly are a big problem. What can audiologists do to play a role in the prevention of this costly and common problem?
Audiologists can have a very positive impact in this area. The National Institutes of Health (NIH) considers falls in the elderly to be a national health care crisis. Balance-related falls are the leading cause of accidental death in persons over age 65 years. More importantly, falls are also responsible for nonfatal morbidities of fractures, mild traumatic brain injury, and wound care for persons with diabetes. There also might be a downward spiral or cascade effect from falls which then does not enable an older adult to stay in his or her own home and “age in place”. Data from 2014 indicated that 30% of older adults (65 and older) in the U.S. reported falling at least once, and the estimated 29.0 million falls that year resulted in 7.0 million injuries and approximately 27,000 deaths (Bergen et al., 2016). Fall injuries often also require costly medical intervention. The total estimated medical cost was approximately $50.0 billion in 2015, including fees for hospital and nursing home care, doctors, and other professional services. Obviously, this is a big concern for the older adult who fears loss of independence, as well as for their families, and for third-party payers.
18. And more balance testing by audiologists would be helpful?
Naturally, we cannot truly prevent individuals from falling, but the inclusion of the audiologist providing neurodiagnostic balance testing can better identify at-risk individuals and develop appropriate interventions. For example, the older adult patient who becomes unsteady following a bout of vertigo due to a shingles outbreak may be an ideal candidate for VRT and recovery when testing reveals only a unilateral non-compensated peripheral vestibulopathy. Conversely, a patient who has undergone chemotherapy and shows a severe total bilateral loss due to vestibulotoxicity will have a less promising recovery. That person will require an assistive device and management of activities of everyday living, as a bilateral loss cannot compensate.
We have just published a research paper entitled, “Association of cognitive impairment and fall risk in older adults: An analytical cross-sectional study,” which found that older adults with even mild cognitive impairment (MCI) may be at elevated fall risk by 14X times (Chua et al., 2022). We believe this will be an important contribution to the literature on how we think about the best tools for fall risk assessment and the introduction of cognitive screening in the realm of the neurodiagnostic audiologist.
19. Before we finish, I understand that you and your colleagues at the American Institute of Balance (AIB) have a highly regarded educational and clinical program and that there is now a network of clinical programs to help audiologists. Could you tell me more about this?
Yes, for 30 years the AIB has provided classes, workshops, and certification programs to over 13,000 professionals worldwide. This includes audiologists, physicians, and physical and occupational therapists. We also operate our own clinics in several states and see about 1,000 patients per month. Over the past 36 months, we have launched AIB Centers of Specialty Care. There are currently 68 audiologist-owners operating 100 clinics in 32 states. This is through an exclusive licensing agreement with a protected territory with full support including staff training, marketing, ongoing online clinical support, patient education, physician referral, and patient acquisition. Perhaps the most important feature is our remote proprietary test over-read plans, which takes away the necessity of the audiologist-owner to need a vestibular guru within their own four walls. They have access to 33 AIB professionals to provide them with everything they need to ensure their success. You can visit AIB Centers of Specialty Care at our website, www.dizzy.com for more information.
20. This has been great! Any last thoughts for audiologists who are interested in pursuing neurodiagnostic vestibular-balance testing?
Absolutely! Read, read, read, and then read more! Put away your old textbooks from grad school. They become outdated very quickly. Commit to being a lifelong learner and reading journal articles from across many specialties including physical medicine, neurology, otolaryngology, psychiatry, internal medicine, geriatrics, etc. No single specialty owns this topic and you’ll need to understand and integrate a diverse background of topics to become a master. One of my favorite quotes is from the motivational speaker Earl Nightingale, “If you spend an extra hour each day of study in your chosen field you will be a national expert in that field in five years or less.”
References
Adams, M. E., & Marmor, S. (2022). Dizziness diagnostic pathways: Factors impacting setting, provider, and diagnosis at presentation. Otolaryngology-Head Neck Surgery, 166(1), 158-166.
Bergen, G., Stevens, M. R., Burns, E.R. (2016). Falls and fall injuries among adults aged ≥65 years - 2014 U.S. CDC Morb Mortal Wkly Rep, 65, 993–998.
Chua, K., Fauble, B. M., & Gans, R. E. (2022). Association of cognitive impairment and fall risk in older adults: An analytical cross-sectional study. Journal of Otolaryngology-ENT Research, 4(1), 8-12.
Deal, J. A., Reed, N. S., Kravetz, A. D., Weinreich, H., Yeh, C., Lin, F. R., & Altan, A. (2019). Incident hearing loss, and comorbidity a longitudinal administrative claims study. JAMA Otolaryngol-Head Neck Surgery, 145(1), 36-43.
Gans, R. E., & Rutherford, K. (2020) Multidisciplinary approach to the management of the adult dizzy patient. ENT & Audiology News, 29(2), 2-4.
Citation
Gans, R. E. (2022). 20Q: Adding vestibular-balance neurodiagnostics to your audiology practice. AudiologyOnline, Article 28232. Available at www.audiologyonline.com

