 From the Desk of Gus Mueller
From the Desk of Gus Mueller
In the early 1970s, most clinical audiologists were pretty excited about a new testing procedure that had been developed—it was called the auditory brainstem response, or ABR (or BSER back then). Clinically friendly equipment—such as the Nicolet CA1000—soon became available, and this testing was then fairly routine in many clinics. If an adult patient had some unexplained asymmetry for audiometric thresholds, or suspicious looking acoustic reflex findings, they were scheduled for a diagnostic ABR. Workshops and seminars on interpreting these ABR findings were plentiful, and there even was a band of audiologist purveyors who called themselves the “Merry Bumpologists.”

Gus Mueller
Some things change. Many of the Bumpologists have retired, and we have more or less also retired the routine use of the diagnostic ABR; it’s more efficient to simply order an MRI. But one thing that hasn’t changed is the value of the ABR for estimating hearing sensitivity for infants and children. This too was around in the 1970s, but the techniques and equipment have improved considerably, and this clinical testing now can be conducted with excellent reliability and validity—when correct procedures are followed.
We of course want to use Best Practice for all of our audiologic work, but if there is ever a time when it is critical, it’s when conducting ABRs for threshold estimation with infants. Not providing an adult patient appropriate hearing aid gain at 4000 Hz certainly is not good, but reporting that an infant has normal hearing when he actually has a severe hearing loss falls into a totally different category of error. In this installment of 20Q, we searched out an individual who is an expert on all the latest protocols and standards that can guide us to do things the right way, and he’s agreed to share his thoughts and insights with us here.
Jace Wolfe, Ph.D., is the Director of Audiology at the Hearts for Hearing Foundation. He is an adjunct Assistant Professor in the Audiology Department at the University of Oklahoma Health Sciences Center and also has an appointment at Salus University. He is a member of the Better Hearing Institute’s Pediatric Advisory Board as well as the Audiology Advisory Boards for Cochlear Americas, Advanced Bionics, and Phonak.
Dr. Wolfe is a noted author. Many of you are familiar with his popular book, Programming Cochlear Implants, now in its 2nd edition. Directly related to this month’s topic is his periodic column in the Hearing Journal titled--"The Tot Ten.” We’re always game for one-upmanship here at AudiologyOnline, so Jace will be providing us with “The Tot Twenty.”
As you go through this article, you’ll be reminded that many of our colleagues have put in considerable effort to provide protocols and procedures necessary for conducting ABR testing with infants and children correctly. And thanks to Dr. Wolfe for laying it all out in an informative, organized and easily digestible manner.
Gus Mueller, PhD
Contributing Editor
October 2014
To browse the complete collection of 20Q with Gus Mueller CEU articles, please visit www.audiologyonline.com/20Q
20Q: ABR Assessment in Infants - Protocols and Standards

Jace Wolfe
1. I’ve been asked to get involved with newborn auditory brainstem response (ABR) testing. It’s not something I’ve been doing lately. Help!
No problem! Over the past few years, a number of experts have created excellent clinical guidelines that provide detailed instructions on how to complete a comprehensive ABR assessment in infants and young children. These documents have filled a very basic void in our profession; the provision of a frequency-specific ABR assessment protocol that is evidenced-based, provides an accurate estimate of a child’s auditory function, and most importantly, limits the potential of mistakes. In fact, I would go so far as to say that audiologists who are conducting ABR assessment using tactics that deviate substantially from what may be found in these documents are placing themselves and their patients at risk.
2. Okay, you’ve got my attention. I would guess that a lot has changed since I last did ABR tests with children decades ago?
First, as you probably know, universal newborn hearing screening is now a reality across the United States and in many other places around the world. It is now well-accepted that a diagnostic, frequency-specific ABR with tone burst stimuli should be completed for infants who do not pass their hearing screening, and I do believe that most pediatric audiologists are completing this testing. However, what has changed is a greater understanding of the issues and pitfalls that can lead to diagnostic errors. The unfortunate truth is that almost everyone has been performing these tests sub-optimally and, unfortunately, many unknowingly still do.
3. So, your last statement makes it sound like things aren’t going as well as they could?
True. I would contend that if you reviewed the results of ABR assessments conducted at 10 different randomly-selected audiology clinics around the country, you would most likely find 10 different “protocols” that were used to complete these assessments, and in some cases, the differences would likely be quite startling. Additionally, these differences may be found in several different areas. For instance, you would likely find substantial variability in the stimulus parameters that were used to elicit the responses, the acquisition parameters that were used to record the responses, and the strategies the clinicians used to interpret the responses. This variability stems from the fact that there are currently no professional guidelines available in the United States that explicitly spell out how a clinician should administer an ABR assessment to evaluate auditory function and estimate auditory function in infants. More specifically, I believe that it is fair to say that there is no consensus and there are no guidelines that indicate exactly, not only the stimulus and acquisition parameters the clinician should use, but also the order in which testing should be completed (e.g., test order for tone burst frequency, air/bone conduction, ear, etc.). The same goes for a lack of protocol for the analysis of waveforms and the interpretation of results.
4. So, there’s obviously a lot of variability. Does that really matter?
This variability is important, because it increases the likelihood that mistakes will be made. Although some of the variability in the ABR protocols is probably not that big of a deal, the lack of a standardized “game plan” to accurately complete the testing certainly enhances the likelihood that mistakes may occur, especially when administered by inexperienced clinicians. Common sense suggests that when ten clinicians do things ten different ways, they all are probably not doing things the right way! Conducting ABR assessment and analyzing squiggly lines (i.e., ABR waveforms) obtained from newborns, particularly those with hearing loss, may be one of the most challenging tasks in clinical audiology. The challenging nature of this task is enhanced by the fact that mistakes with infant ABR assessment can lead to lifelong deleterious effects.
5. You’re suggesting that if the correct protocol isn’t followed, a child could end up with the wrong diagnosis?
Absolutely. If a child with hearing loss is mistakenly identified as having normal hearing, then the intervention that the child needs is delayed, and auditory brain development and speech, language, and auditory abilities may be delayed and compromised for life. On the other hand, if a clinician were to diagnose hearing loss in an infant who actually has normal hearing, then that infant may receive a treatment (e.g., hearing aids) that is not needed. Likewise, if hearing loss is over-estimated in a child who does have hearing loss, then his hearing aid output may be set too high, which may lead to discomfort or even worse, an additional noise-induced shift in hearing loss. Furthermore, audiologists may held liable for these types of mistakes, and in fact, there are instances in which large settlements have been paid to families of children who have hearing loss but were erroneously declared to have normal hearing after an errant ABR assessment. All clinicians should be equipped with an evidenced-based protocol that facilitates a time-efficient, accurate ABR assessment while limiting the potential for mistakes.
6. Does an evidence-based protocol or guideline even exist?
There are several good guidelines that all clinicians completing ABR assessment in infants and young children should review. Here are a few that I like:
- The English Newborn Hearing Screening Programme (NHSP) Guidance for ABR Testing in Babies.
- British Columbia Early Hearing Program’s Diagnostic Audiology Protocol.
- Ontario Infant Hearing Program Audiologic Assessment Protocol. Available at https://www.mountsinai.on.ca/care/infant-hearing-program/documents/IHPAudiologicAssessmentProtocol3.1FinalJan2008.pdf
Another good read that is not exactly a clinical guideline but rather a summary of good ABR clinical practices is a fairly recent publication by David Stapells, who was instrumental in the development of the British Columbia ABR guideline:
David R. Stapells (2010) Frequency-specific ABR and ASSR threshold assessment in young infants. In eds. R.C. Seewald & J.M. Bamford, A Sound Foundation Through early Amplification 2010: Proceedings of the Fifth International Conference. pp 67-106. Phonak Publishing, Stafa, Switzerland. Available at https://www.Phonakpro.com
7. What’s so special about these guidelines?
They all have different virtues, but the documents I’ve mentioned here all have a common thread. You might have noticed that none of them are from the U.S. These guidelines have been developed in countries or provinces in which universal healthcare is provided by the government. Now, I am certainly not here to argue the merits and limitations of government-sponsored healthcare. I will say, however, that many countries with government-sponsored healthcare have developed detailed protocols for all facets of audiology. These types of standards should be present in all healthcare systems.
8. Why does the healthcare delivery model matter for ABR guidelines?
In the ideal world, healthcare delivery should be evidenced-based, time-efficient, thorough but not superfluous or excessive, and accurate. It also would possess safeguards or controls that are designed to limit mistakes. Such a system would effectively deliver the services a patient needs while limiting both the potential for mistakes and the liability of the provider. Indeed, many of the guidelines mentioned above are designed to achieve these objectives. Most importantly, they are evidenced-based, and they are created to facilitate accurate ABR testing and minimize the possibility of egregious mistakes.
9. I indeed will check out those guidelines, but can you review a few of the high points for me now?
Certainly. Let’s start with waveform analysis. The English NHSP ABR guideline notes that the primary method of determining whether a response is present or absent is via visual interpretation. Objective measures may also be used for response analysis, but subjective visual interpretation of ABR waveforms should serve as a fundamental component of analysis. Based on the clinician’s subjective analysis, he/she may label ABR waveforms as one of the three outcomes: Clear Response, Response Absent, or Inconclusive. This contrasts with the view that there are two outcomes (response present or not). The third category, Inconclusive, is vital and represents real-life uncertainty for those waveforms where there is insufficient confidence to label the waveform as convincingly showing the presence or absence of a response. When a scientist (or audiologist) doesn’t know he or she must say so! These Inconclusive waveforms must not be allowed to contribute to the definition of threshold. Additionally, the guideline stresses that waveforms should be replicated when they contribute to the finding of a Clear Response at threshold or a Response Absent just below threshold.
10. I’m definitely following you so far, but I could use a little more of a description of what they mean by Clear Response, Response Absent, and Inconclusive.
To be classified a Clear Response, waveforms must meet a handful of criteria. First, two or more waveforms collected at the same intensity must be highly correlated with one another, particularly when the waveforms are used to define threshold. This criterion was been touted by Dr. Jay Hall for years. As he has consistently noted, “If the response does not repeat, then your test is not complete!” By “highly correlated” I mean that the two waveforms should have a high degree of overlap with one another when visually reviewed by the audiologist.
11. Got it. What other criteria must be met for a Clear Response?
For one, the amplitude of the response (i.e., wave V or possibly wave III if it is larger than wave V) should be at least 40 nanovolts and possess an amplitude that is three times higher than the noise. In other words, the size of wave V should be at least three times greater than the residual noise in the waveform. Also, the waveforms should possess the expected characteristics of an ABR elicited by the given stimulus. In other words, the latency of the peak(s) in the waveform should fall within an expected time range, the morphology or shape of the waveform should be similar to what one would expect, and the amplitude of the response should be within the range of amplitudes typical for an ABR response. Here, I like to adhere to the old principle, if it looks like a duck, waddles like a duck, and quacks like duck, then it’s probably a duck. For our case, it has to look like an ABR waveform to be counted as a Clear Response. Of course, this means that the clinician needs to know how an ABR waveform should look! These criteria are designed to ensure a high (over 95%) level of confidence that a genuine response is present. You might think that’s overly strict but just what percentage of the time do you want to be wrong? I’ve provided an example of a Clear Response and an indication of the amplitude of the response in Figure 1.
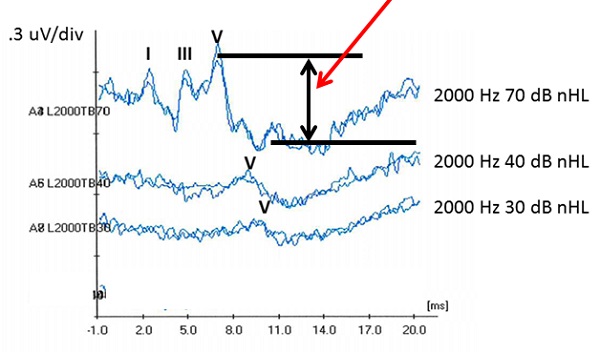
Figure 1. These waveforms illustrate an example in which a Clear Response was obtained at 30 dB nHL.
12. Okay, I’m okay on what constitutes a Clear Response. How about a Response Absent? If it’s not there, it’s not there, right?
Well, we are a little more sophisticated than that when making our decision. ABR waveforms must also meet several criteria to be labeled as a Response Absent. The replicated waveforms should be appropriately flat with no evidence of a response. Also, the residual noise level should be sufficiently low to be confident that a small response is not being obscured by noise (the English guidance specifies less than 25 nanovolts, measured in a certain way). An example of a Response Absent is shown in Figure 2.
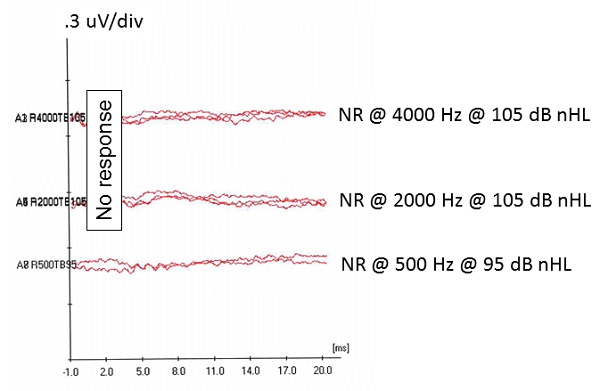
Figure 2. These waveforms illustrate an example in which a Response Absent was obtained.
13. Maybe I should know this, but how do I determine the residual noise level?
Let me start by saying that many contemporary ABR systems provide a calculated estimate of the residual noise level, though there appears to be some variation in the numbers they provide. These values may certainly be used as a guide to determine the noise level of a waveform if your system offers this, but since not all systems do, the English ABR guideline suggests a way that the clinician can subjectively estimate the residual noise level from examining the waveforms.
14. Sounds good to me. How do I do it?
It’s actually not hard. The residual noise level may be estimated by determining the average difference between two optimally superimposed waveforms. In other words, this estimation is done by determining the gap between two waveforms, averaged across the entire recording window. “Optimal” superposition of waveforms is such that their average gap (across the entire time base) is minimized. Most ABR systems provide a “superimpose” function that does this for us.
Admittedly, it may be difficult to “eyeball” the magnitude of the average gap between two waveforms. With that in mind, Guy Lightfoot, Ph.D. and John Stevens, Ph.D., co-authors of the English ABR guideline, suggest an alternative approach. Lightfoot notes that the average noise level may often be estimated by determining the location at which there is maximum separation between the two waveforms. He states that the average noise level often corresponds to about 1/3 of the magnitude of the maximum separation between the two waveforms.
See Figure 3 for an example of the subjective estimation of residual noise level. The English 25nV noise criterion is technically demanding unless test conditions are very good (in practice this usually means the baby is soundly asleep) but, like the Clear Response criterion, it is designed to provide a high degree of confidence that no response is present.
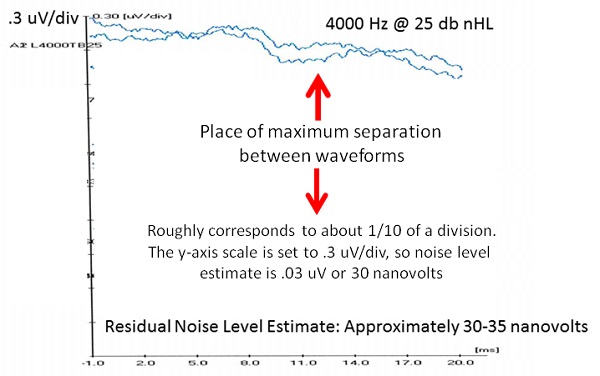
Figure 3. These waveforms provide an illustration for how the residual noise level may be estimated.
15. I think I know what Inconclusive means, but what does the guideline have to say?
On some occasions, waveforms may not satisfy the criteria for either a Clear Response or a Response Absent. In these cases, it is most appropriate to classify the response as Inconclusive. This may happen for a variety of reasons. Most commonly, a clinician will label waveforms as Inconclusive because a Clear Response is not recorded, but the residual noise level is too high to ensure that a low-amplitude response is not present. In these cases, the clinician should take steps to try to quiet the state of the child, reduce competing noise sources, or conduct further signal averaging.
16. Okay, that’s simple enough. What else constitutes a waveform that should be classified as Inconclusive?
Clinicians may also label a response as Inconclusive when the residual noise level is sufficiently low but the criteria for Clear Response are not met (e.g., if the response amplitude is not three times larger than the noise, the latency, amplitude, and/or morphology are suspect, and/or the response amplitude does not increase with increases in stimulus intensity). Figure 4 provides an example in which it is most appropriate to label the responses as Inconclusive. The response amplitude is not three times larger than the noise, and the response amplitude also does not appear to increase with a 5 dB increase in stimulus intensity. What’s the likelihood that this is a genuine response? You could say 40%? Maybe some would say 70%? We may as well toss a coin – not very scientific! The only safe decision is to disregard these waveforms when defining the hearing threshold. In this case, the clinician would be best served by increasing the stimulus intensity by 5 to 10 dB to see of a Clear Response may be obtained.
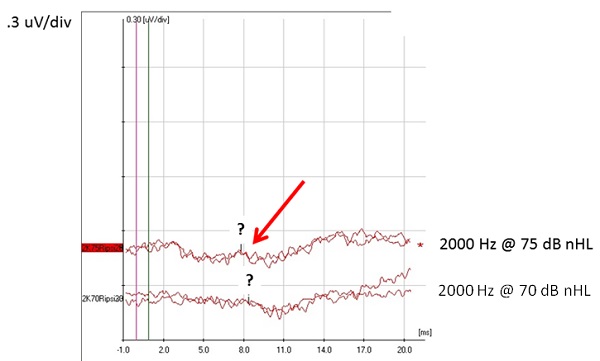
Figure 4. These waveforms illustrate an example in which it is most appropriate for the audiologist to level the results as Inconclusive.
17. That’s fair enough, but now I have quite a few criteria to keep in mind when attempting to classify waveforms. I hope I am able to keep all of this straight.
In short, the clinician should ask the following question, “Do I have a high degree of confidence that the response is either present or absent?” If the clinician cannot answer affirmatively, then the waveform interpretation should be Inconclusive. I should note that labeling waveforms as Inconclusive is often quite difficult for audiologists. We are accustomed to providing answers to the families we serve, so it’s not in our nature to say we aren’t sure. However, for waveforms that do not clearly meet the criteria for a Clear Response or Response Absent, then everyone is better off when we don’t take a dangerous leap and make a cloudy interpretation that is not well supported by appropriate criteria.
18. You still have me a little concerned about making a mistake. Does the guideline mention any other steps that I can follow to improve accuracy?
I am glad you asked, because as a matter of fact, the guideline does include a very important recommendation that will greatly reduce your chances of making a mistake in your ABR analysis. The guideline advocates for the use of what is referred to as the “gold standard threshold” assessment.
The English ABR guideline states that: “ABR threshold is defined as the lowest level at which a Clear Response is present, with a Response Absent recording at a level 5 or 10 dB below the threshold, obtained under good recording conditions.”
For the gold standard procedure, NHSP recommends recording replicated waveforms at a presentation level that is 10 dB above the level at which the ABR threshold was obtained. There are three main things to look for:
- These ABR waveforms (collected at a presentation level 10 dB above threshold) should have a wave V that is greater in amplitude and shorter in latency than the wave V obtained at threshold.
- The waveforms collected at the higher intensity should have a more defined morphology (wave V should be more prominent and wave III and possibly wave I may also be more salient).
- The correlation between the two waveforms should be greater.
Additionally, the gold standard approach calls for the clinician to also obtain at least two replicated waveforms at a level that is 10 dB lower than the presentation level at which the ABR threshold was obtained. This step further ensures that the clinician has correctly identified the true threshold level. It is a sort of safety net – if there is any disagreement over the status of the waveforms at threshold it is unlikely that any “error” will exceed 10 dB.
19. I want to be the Michael Phelps of pediatric audiology! What else do I need to know to go for the gold?
A couple of additional things are worth mentioning in regards to the gold standard approach. First, the guideline recommends that the gold standard approach should be completed for at least one frequency for an air conduction tone burst stimulus in each ear, and when needed, one frequency for a bone conduction tone burst stimulus in each ear. Stated differently, the clinician is not required to satisfy the gold standard criteria for all tone burst frequencies that are evaluated. The document actually suggests completing the gold standard approach for testing with the 4000 Hz tone burst. Although one may make a good case for using the gold standard approach at 4000 Hz, I personally prefer to implement the gold standard approach for a 2000 Hz tone burst, as it resides near the middle of the speech frequency range. The gold standard may be applied at all test frequencies if time allows. However, in the case of a baby for whom amplification is necessary, several frequencies are likely needed. The option to obtain “non-gold” standard threshold at additional frequencies is a pragmatic compromise between scientific precision and breadth of clinical information in such a case. Finally, if a Clear Response is obtained at a level consistent with normal to near normal hearing sensitivity (e.g., 30 dB nHL at 2000 Hz), then it is unnecessary to obtain replicated waveforms below that level. However, it is still important to collect two repeatable waveforms 10 dB above that level to ensure that amplitude and waveform correlation have increased and latency has decreased. An example of the gold standard response is provided in Figure 5. These waveforms were collected in response to a 2000 Hz tone burst from an infant with normal auditory function. As shown, a Clear Response is obtained at the stopping level of 30 dB nHL, so there is no need to obtain waveforms at lower levels. However, the Clear Response was verified by also obtaining replicated waveforms to a 2000 Hz tone burst presented at 40 dB nHL. As expected, the response amplitude increased, the latency decreased, and the morphology improved at the higher level. That’s the gold standard approach in a nutshell.
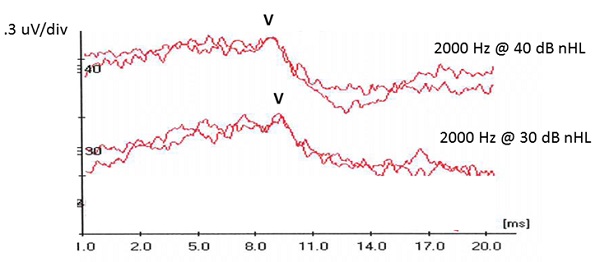
Figure 5. These waveforms illustrate an example in which the audiologist adhered to the NHSP gold standard to ensure that a response was present at 30 dB nHL.
20. That’s exactly what I needed to know. BUT, I have ton of additional questions about the specific testing. Can we do this again next month?
I’m just getting started. Count me in!
Cite this content as:
Wolfe, J. (2014, October). 20Q: ABR assessment in infants - protocols and standards. AudiologyOnline, Article 12999. Retrieved from: https://www.audiologyonline.com


