Editor’s note: This text-based course is a transcript of the webinar, 2019 Coding and Reimbursement Update, presented by Kim Cavitt, AuD.
Learning Outcomes
After this course learners will be able to:
- List the new HCPCS codes for 2019.
- Evaluate the changes to United Healthcare hearing aid coverage.
- Describe the audiologists' role in the Merit-Based Incentive Payment System.
Updates & Changes
CPT & ICD 10 Changes
CPT, which is current procedural terminology, are codes that represent the diagnostic and rehabilitative procedures that we provide. ICD 10, which is the International Classification of Diseases, the 10th revision. Neither one has had any audiology-centric CPT changes for 2018-2019. ICD 10 codes go into effect on October 1st of a given year. On October 1st of 2018, there were no audiology-centric or audiology-pertinent ICD 10 changes. CPT changes go into effect on January 1st of every year, and there were no audiology-centric CPT changes that went into effect for January 1.
HCPCS Changes
The Healthcare Common Procedure Coding System (HCPCS) represent products, hearing aids, cochlear implants, auditory osseointegrated devices, auditory brain stem implants, and the services that support those devices. There were changes for HCPCS in 2019. The changes mainly centered around CROS and BiCROS, and these new codes and changes did go into effect on January 1, 2019. A CROS system is where a patient wears a “hearing aid,” functioning as a receiver, on the normal hearing ear and a “hearing aid,” functioning as a transmitter, on the “unaidable” ear. A BICROS system is where a patient wears a hearing aid/receiver on the better hearing ear and a “hearing aid,” functioning as a transmitter, on the “unaidable” ear. The hearing aid and “hearing aid” receivers and “hearing aid” transmitters can be in-the-ear (ITE), in-the-canal (ITC), and/or behind-the-ear (BTE) types/styles and the patient can be fit with different types/styles in each ear. The new codes will now reflect these options. CROS and BICROS can come in many configurations in the ear, in the canal behind the ear, and they can be combinations of those configurations.
New Codes: CROS/BICROS
The new codes will reflect these configurations. It is important to know that before you start to utilize a new code set, please consult your payer fee schedules, agreements, and their websites. Some payers, especially State Medicaid, workers comp, managed Medicaid programs may not recognize a new code set. For example, when digital codes came out they never recognized them and they still pay in the hearing aid code set without technology. This could be the same at the state, especially State Medicaid/workers comp level. So again, the existence of a code is not a guarantee of third-party coverage or payment, nor is it a guarantee of an increase allowable rate. That is something you need to work on in terms of a renegotiation process with a payer. Just because the new codes came out, does not mean they will be recognized and you will see an increase in coverage. So let's first talk about the new codes, and I have made a table to explain how these codes work.
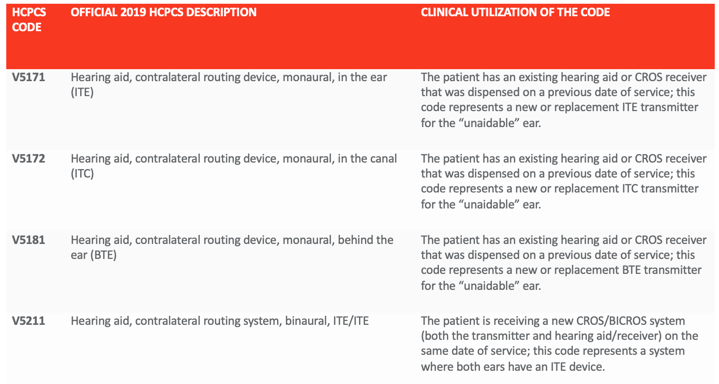
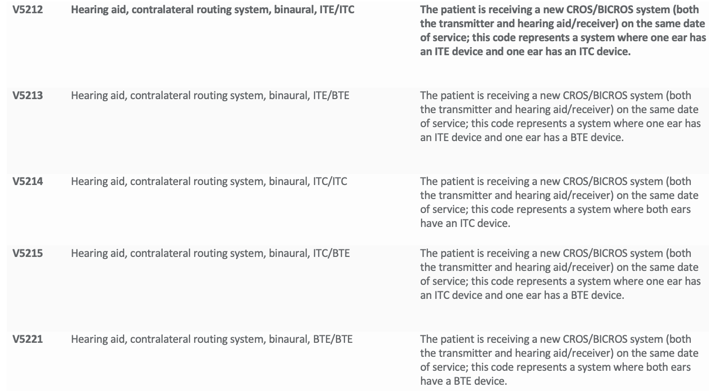
Table 1. New codes for CROS/BICROS in 2019.
First V5171, which is the hearing aid contralateral routing device, monaural, in the ear. These first codes are mainly for patients who already have an existing device on one ear, and you are adding a transmitter to the other side. So again, for V5171, the patient has an existing hearing aid or CROS receiver that was dispensed on a previous date of service. V5172 represents a new or replacement ITE transmitter for the unaidable ear. V5281 means it's the BTE transmitter. When you use the term system, that means it's both pieces. It does not mean that you are going to add a hearing aid code and both pieces would be represented by this singular code. So V5211 is a hearing aid contralateral routing system, binaural, both pieces, and both pieces and ITEs. Then you have your contralateral routing system, binaural, ITE/ITC, one ear has an ITE and one ear has an ITC. The code that is most commonly used which is V5221, which is a BTE/BTE configuration. Again, these codes that I just listed are representing both pieces, you would not add another code on for another device.
Revised Codes: CROS/BICROS
A dispensing fee is something that is very ill-defined. State Medicaid and managed Medicaid programs consider the dispensing fee to be the fitting fee, even though there is a separate code for fitting orientation. In my opinion, a dispensing fee is your practice's fee for everything around the evaluation (e.g., ordering, setting up, programming and fitting). Again, the exception to that would be State Medicaid programs that consider that dispensing fee to be your fitting orientation fee. Other than that, a dispensing fee is separate from fitting orientation because again, that code exists. So, V5200 is your dispensing fee for CROS. V5230 is a contralateral routing system, binaural, glasses. Then there is your dispensing fee for the BiCROS, which is V5240. The dispensing fee is not represented by another code, and many State Medicaid plans and other payers as well as consider the dispensing fee to represent the fitting orientation. This is another example of before you bill things out, your total needs to be the same. You need to have a usual and customary rate for your CROS and BICROS systems. That rate is the same whether it's private pay or insurance. Your totals always need to be the same when the claim goes out the door. How it is coded can depend on the payer. So if some payers don't recognize the fitting orientation code, you will take those monies that would be coded as fitting orientation and put them back into the cost of the code for the device. Let's say they represent fitting orientation and dispensing fee, those then would be coded separately. Some payers will recognize both and some won't recognize a dispensing fee. They will only recognize fitting orientation, but your total that is billed out needs to be the same as a total that will be paid for a private pay patient.
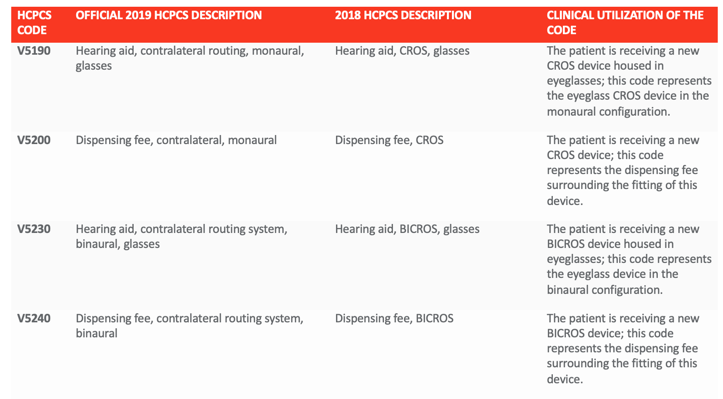
Table 2. Revised codes for CROS/BICROS in 2019.
Deleted Codes: CROS/BICROS
There were some codes that were deleted in 2019. While HIPAA says they are supposed to use standard transaction and code sets, some payers (e.g., Medi-Cal) can get what we would call HIPAA waivers that they can still use a code set that they so choose. Most private payers are not going to recognize these codes that have now been deleted, but again, you may need to work with payers here in the beginning, especially in a transition period to see what codes they recognize. Some payers (e.g., State Medicaid, managed Medicaid) may have difficulties transitioning to this new code set. Practices may need to file appeals. If you get denied, I would always bill new codes. This is when it's really valuable to always have an updated code manual or access to an electronic version of the code manual. In your appeal, you can send the new codes to the payer as part of your appeal process to say these codes were deleted, and these codes are its replacement.
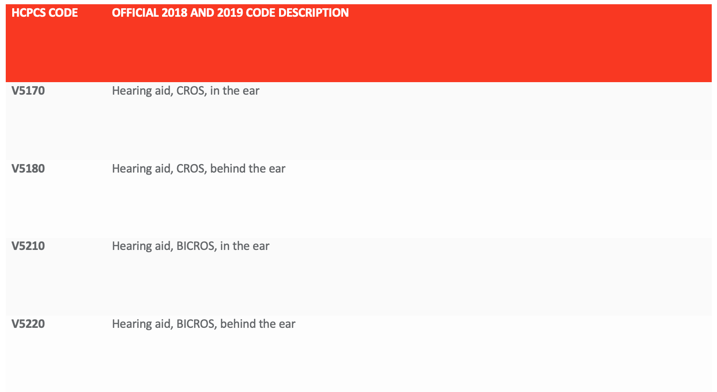
Table 3. Deleted codes for CROS/BICROS in 2019.
Billing Examples
Here are some examples in an itemized or unbundled manner:
CROS billing. The patient is receiving a new BTE CROS system, with a behind the ear device in each ear.
- V5221 - CROS devices (represents both units)
- V5220 - Dispensing fee
- V5011 - Fitting and orientation
- V5020 - Real-ear measurement
- V5264/5 - Earmold or insert, each
- V5266 - Battery (each)
BICROS billing. The patient has a profound hearing loss in their left ear and a moderate hearing loss in their right ear. The patient wears a behind-the-ear hearing aid in the right ear that was purchased in 2018. They would like to add a behind-the-ear transmitter to their left ear in 2019. So now, this isn't a whole system, this is just a new replacement transmitter.
- V5181 – CROS transmitter
- V5240 – Dispensing fee
- V5011 - Fitting and orientation
- V5020 - Real-ear measurement
- V5264/5 - Earmold or insert, each
- V5266 - Battery (each)
Third-Party Medical Policies 2019
Now I want to discuss medical policy changes. Many payers have exceptional websites and communicate in newsletters regarding the guidance of changes to their medical policies. I want to make sure that everyone knows how to look at these and how to find them. You need to look every year. I always recommend in December looking at all your new fee schedules. Take a peek at the Medicare fee schedule and you see if there are any changes to hearing aid policies for insurers and then set your policies for the following year accordingly. Again, these medical policies can often times be available in patient manuals on the payer websites. So let's first talk about some medical policies.
UnitedHealthcare's Medicare Part C (Medicare Advantage Plan)
This first one is UnitedHealthcare's Medicare Part C or Medicare Advantage Plan. In this plan, they are going to use a third-party administrator (TPA). A third-party administrator is a middleman that has negotiated coverage, benefits, or discounts with an insurer or employer group. In this example, UnitedHealthcare purchased its own third-party administrator, which is EPIC. So there is a whole contingent across the country of Medicare Part C plans or Advantage Plans that now have access to amplification. These benefits are either through HiHealth, which is United's hearing aid product that they have manufactured for them or through EPIC. The patient is limited to two aids every two years, one for each hearing-impaired ear. From HiHealth, the patient has a $300 to $370 copay for each aid. Through EPIC, that patient has a $400 to $2025 co-payment depending on technology. The patient will not be able to access these benefits for this Advantage Plan unless you are part of EPIC. You would not be able to access the HiHealth.
UHC Commercial
UnitedHealthcare also created a new medical policy for its commercial plans. This is a national policy. This is directly from their communications, "Standard plans include coverage for wearable hearing aids that are purchased as a result of a written recommendation by a physician." So in other words, UnitedHealthcare wants a medical clearance. That medical clearance needs to come after the hearing test is done. "Benefits are provided for the hearing aid and for charges for associated fitting and testing. The wearable hearing aid benefit does not include batteries, accessories or dispensing fees." This means the patient is then responsible for those costs (e.g., batteries, accessories, dispensing fees). Patients should pay those costs separately as separate line items on the date of fit. You should not bill it, these should be things that the patient pays for separately. This next part is really important because this is now opening the door for UnitedHealthcare to allow for an upgrade. "If more than one type of hearing aid can meet the member's functional needs, benefits are available only for the hearing aid that meets the minimum specifications for the member's needs, again, what's medically necessary. If a member purchases a hearing aid that exceeds these minimum specifications, UnitedHealthcare will only pay for the amount that it would have paid for a hearing aid that meets the minimum specifications, and the member would be responsible for paying any difference in cost." You need to have an upgrade waiver that reflects this language that UnitedHealthcare only pays for aids that meets someone's minimum specifications. If the patient chose something more technologically advanced (e.g., streams, rechargeable) then the patient is responsible for differences in costs. I would have that patient pay those differences in costs at the date of fit. You don't want to be in the role of this collector, you want to be in the role of the refunders. You want to collect all patient responsibilities (e.g., co-payments, co-insurance, deductibles, out-of-pocket, non-covered expenses) on the date of fit. Your financial policies should reflect that.
Aetna
Now let's talk about some medical policies as it comes to Aetna. This is their national medical policy and is important because this is about what they will cover. "Air conduction hearing aids are considered "medically necessary when the following criteria are met":
- Hearing thresholds 40 decibels (dB) HL or greater at 500, 1000, 2000, 3000, or 4000 hertz (Hz); or
- Hearing thresholds 26 dB HL or greater at three of these frequencies; or
- Speech recognition less than 94 percent."
Aetna will not cover amplification for hidden hearing loss that has the normal audiogram. Again, this is their coverage policy. Another thing that is important to know that, "Aetna considers implantable hearing aids and semi-implantable hearing aids experimental and investigational for all other indications because its effectiveness for indications other than the ones listed above has not been established." For example, they are not going to pay for an Earlens as they deem that experimental. You can often times again find these online through their portals. You need to make sure that you are reading the communications when they send you a monthly newsletter.
BCBS
Blue Cross/Blue Shield is run independently in every state. There are some states that because some plans manage other plans that have more consistency. For the most part, every Blue Cross/Blue Shield plan is different. They often times have password-protected portals that you are going to need to go into to look at their policies and look at their guidance. Please reach out to your local BCBS through their websites to find out if there are any hearing aid or audiology policies related to you. Again, this is where you will find things that they deem experimental.
FEHP. It's also important to talk about FEHP. I find in my consulting work that many people believe that FEHP is one size fits all. For example, that everybody has the $2,500 benefit. Well, that's actually not how it works. Federal employees can select from a myriad of different options that varies state to state. This link will take you to a map of the United States. You will click on your state and then it will show you all of the different benefits that can exist. What's really great about this link is it will give you the plan document for all of the different plans. You will see what the hearing aid or audiology coverage is. It's typically very easily identified.
Copy and paste into your browser: https://www.opm.gov/healthcare-insurance/healthcare/plan-information/plans/
BCBS FEHP plan:
- "Hearing aids for children up to age 22, limited to $2,500 per calendar year.
- Hearing aids for adults age 22 and over, limited to $2,500 every three calendar years. Benefits for hearing aid dispensing fees, fittings, batteries, and repair services are included in the benefit limits described above.”
- The patient is responsible for all costs which exceed $2500.
It's an inclusive benefit, that means you can't bill separately for fittings, dispensing fees, batteries, or repair services. The patient is responsible for all costs that exceed the $2,500. The patient can upgrade, but you need to have them sign an upgrade waiver. The upgrade waiver needs to reflect that they could have been fit with something within their benefit, but they have chosen to upgrade. Every Blue Cross/Blue Shield, and now United fitting should have an upgrade waiver in place and signed at the date of the hearing aid evaluation. So you want to make sure that they are acknowledging that they want to proceed with the upgrade, but the form needs to really clearly indicate that they could have gotten something within their benefit.
Telehealth
The Medicare definition of telehealth is “the use of electronic information and telecommunications technologies to support and promote long-distance clinical health care, patient and professional health-related education, public health and health administration. Technologies include video conferencing, the internet, store-and-forward imaging, streaming media, and terrestrial and wireless communications." Store and forward is asynchronous telehealth.
Telehealth & HIPAA
Audiologists have to ensure before they begin providing telehealth, that their transmission systems all meet the HIPAA security requirements. These requirements “ensure the confidentiality, integrity, and availability of all e-PHI they create, receive, maintain or transmit." Does your state allow an audiologist to provide telehealth services to people in their state? So when you make that first leap, you either need to use an office management system, like counseling has telehealth built in. You could use that, or you need to hire an IT consultant. This is really a one-time thing until, unless new rules came out, you need to just hire someone to help you set up a telehealth platform. You can only control your end of the equation, that's your responsibility. You can't control the patient end of the equation. Because we have to protect electronic protected health information that we transmit. You can't use FaceTime, SMS, instant messaging, Skype, unencrypted email.
Then the next step is how you are going to monetize it. For example, if a patient wanted to participate in telehealth, one of the requirements I would have is to keep their credit card on file in a secure system. Here are a couple of great links:
- https://www.telehealthresourcecenter.org/sites/main/files/file-attachments/hipaa_for_trcs_2014_0.pdf
- https://www.hipaajournal.com/hipaa-guidelines-on-telemedicine/
Telehealth Coding - Modifiers
Telehealth services can only be provided by audiologists when allowed by your state law and when your HIPAA security requirements are met. Medicare and most private payers do not cover services provided via telehealth. Telehealth is just a mechanism, not a separate code. You can have different kinds of service and can add modifiers. You would change the place of service code for telehealth to 02 and then there'd be modifiers. In order for you to be able to track what procedures you provided via telehealth, you would need modifiers.
- GQ: Telehealth provided via interactive audio and video telecommunications systems.
- GT: Telehealth provided via an asynchronous telecommunications system.
Healthcare Reform: Merit-Based Incentive Payment System (MIPS)
- https://qpp.cms.gov/
- https://qpp.cms.gov/mips/quality-measures
- https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/CPIA-Performance-Category-slide-deck.pdf
- https://www.cms.gov/Medicare/Quality-Payment-Program/Resource-Library/2019-QPP-proposed-rule-fact-sheet.pdf
Why is MIPS Important?
Every year, Medicare comes out with the proposed rule. This includes the things they are thinking about implementing. Then around the first Monday in November, they come out with the final rule, which includes the things they are going to implement starting on January 1. Audiology was the only doctoral profession that was excluded in the proposed rule, but as a profession, we do not want to be excluded from being part of a quality system. The measures illustrate our value to the patient and health system. We want the government collecting data on how well we contribute to a patient's quality of life and healthcare outcomes. The activities around MIPS differentiate us from over-the-counter and hearing aid dispensers in the marketplace. These activities illustrate the evidence-based, patient-centered practice of audiology.
The final rule added audiology, along with speech-language pathology, occupational therapy, physical therapy and clinical social work, as eligible professionals in the MIPS.
MIPS Participation Options
Refer to this link for participation options: https://qpp.cms.gov/mips/individual-or-group-participation
Important note - What kind of setting do you practice in? If you practice in a hospital, multidisciplinary clinic, otolaryngology or physician practice you may have different reporting requirements, reporting methods and guidelines. If you work in one of these practice settings, please immediately reach out to your practice administrator to determine your MIPS requirements. Your practice could be enrolled as an alternate payment model, which has different MIPS reporting requirements than it would be if you were in an audiology-only practice.
Participate as an individual. If you are going to be reporting and you do not work in the settings listed above (hospital, multidisciplinary clinic, otolaryngology or physician practice) we recommend that you focus on reporting as if you are an individual. An individual is defined as a single clinician identified by their National Provider Identifier (NPI) tied to a single tax identification number (TIN). If you report only as an individual in 2019, you will report measures and activities for the practice(s) under TIN(s) under which you are MIPS-eligible and you will be assessed across all four performance categories (except for audiology - we will only be assessed across two performance categories) at the individual level. Your payment adjustment will be based on your Final Score derived from the four MIPS categories. Audiologists are only going to be assessed across two performance categories: we will be assessed for our quality, which would be 85% of our score, and improvement activities, which would be 15%.
Report as a Group. You could also report as a group which I do not recommend. We do not know enough in 2019 about what group reporting looks like. A group is defined as a single TIN with 2 or more clinicians (at least one clinician within the group must be MIPS eligible) as identified by their NPI, who have reassigned their Medicare billing rights to a single NPI. If you report only as a group, you must meet the definition of a group at all times during the performance period and aggregate the group's performance data across the four MIPS performance categories for a single TIN. Each MIPS-eligible clinician in the group will receive the same payment adjustment based on the group's performance across all four MIPS performance categories.
Low volume threshold. Even though audiology as a profession is eligible, if you do not bill more than $90,000 to Medicare, if you do not see at least 200 beneficiaries, or if you do not provide at least 200 professional services, you are not required to report MIPS. You actually have an exclusion called the low volume threshold. There are right now are maybe eight audiologists in the country that exceed the $90,000 threshold. Those audiologists, if they are out there, they do need to report. They should reach out to their national associations that they are a member of to get guidance and support. Sometimes when it comes to size of your organization, you also may have different requirements. Right now, most audiologists in this country are eligible but excluded from MIPS due to this low volume threshold when they are individually reporting.
MIPS Scoring & Steps
Four Performance categories make up the MIPS scores, but there are only two that pertain to audiologists and our work: Quality and Improvement Activities.
- Quality (85%)
- This performance category replaces PQRS. This category covers the quality of the care you deliver, based on performance measures created by CMS, as well as medical professional and stakeholder groups.
- Providers have to be able to report up to six measures of performance.
- Can be reported via claims, registries, or electronic health records (EHR).
- Improvement Activities (15%)
- 2 high-weighted activities or
- 1 high-weighted activity and 2 medium-weighted activities or
- At least 4 medium-weighted activities.
- Must occur for 90 days or more.
- Documented by attestation.
MIPS Step #1: Determine Eligibility
- Go to MIPS Participation Status link.
- Insert your National Provider Identifier in the box provided.
- Only the Performance Year (PY) 2018 Participation Status is CURRENTLY available. The Centers for Medicare and Medicaid Services (CMS) plan to have the site updated by early December 2018 and make a PY2019 Participation Status Tool Available.
- The PY2018 Participation Status summary, for your NPI, will give you a snapshot of your Medicare claims data for determination periods between September 1, 2016 – August 31, 2017, or September 1, 2017 – August 31, 2018.
- While this snapshot will provide you with information on your status for 2018 Participation ONLY, it does give you some interim information on your enrollment date, the number of Medicare patients you have seen in the review period, and the amount of Medicare allowed charges you have billed during the review period.
- If, when you check your MIPS eligibility status on the PY2019 tool (which is not yet available), it indicates that you are eligible to report because of participation in an Alternative Payment Model (APM), please immediately reach out to the practice manager of your facility to determine your specific reporting requirements and mechanisms (as the claims-based reporting option might not be available to you).
- Typically, APMs only exist in large hospitals, medical centers, and multi-disciplinary clinics.
- The PY2018 Participation Status summary, for your NPI, will give you a snapshot of your Medicare claims data for determination periods between September 1, 2016 – August 31, 2017, or September 1, 2017 – August 31, 2018.
MIPS STEP #2: Determine if You Are Exempt
Audiologists are MIPS EXEMPT for participating in the MIPS program if, individually, they:
- Have $90,000 or less in Medicare Part B allowed charges for covered professional services; OR
- Provide care to 200 or fewer Medicare beneficiaries; OR
- Provide 200 or fewer covered professional services under the Medicare Physician Fee Schedule (PFS).
These exemptions are collectively called the low volume threshold. 99% of individual audiologists in the United States, whose practice is not enrolled in an Alternative Payment Model (APM), will be exempt from MIPS reporting in 2019.
MIPS Step #3: Determine if You Want to Report
Now step three, you have to determine if you want to report. Exempt audiologists (audiologists who do not meet the low volume threshold) may decide to voluntarily participate in the MIPS program. This can be accomplished by two means:
Voluntary participation:
- Audiologists will not formally sign up/enroll in this type of reporting.
- Audiologists can participate via the same mechanism they reported Physician Quality Reporting Systems (PQRS) Measures.
- Reporting G-Codes via Medicare Part B claims.
- Audiologists will also “attest” to the Improvement Activities (IA).
Opt-In participation:
- Audiologists will officially and formally “opt-in” (the form or process is not yet available).
- Audiologists can participate via the same mechanism they reported Physician Quality Reporting Systems (PQRS) Measures.
- Reporting G-Codes via Medicare Part B claims.
- Audiologists will also “attest” to the Improvement Activities (IA).
- Audiologists would be eligible for payment incentives and payment reductions, based upon their overall MIPS score and performance.
MIPS Voluntary Participation STEP #1: EIDM Enrollment
Let's say you decided to voluntarily participate. The first step if you want to enroll in the system is EIDM enrollment. This account will allow you to track your Quality Payment Program (QPP) performance and score. You can register (or log in to an existing account) at https://portal.cms.gov/wps/portal/unauthportal/home/. Select “PQRS” from the pulldown screen. Don't inadvertently opt into any program as part of the EIDM registration process.
MIPS Voluntary Participation STEP #2: Report MIPS Quality Measures
- Documentation and verification of current medications in the medical record.
- Screening for clinical depression and follow-up plan.
- Falls Risk Assessment
- Falls Risk Plan of Care
- Screening for Tobacco Use/Cessation
- Referral for otologic evaluation for patients with acute or chronic dizziness.
- https://audiologyquality.org/measures/
- https://audiologyquality.org/reporting-pqrs-measures/
- https://qpp.cms.gov/mips/quality-measures
MIPS Voluntary Participation STEP #3: Complete and Attest to Improvement Activities
Reporting options can change with those group reporting or if you are an APM or an ACL. Improvement activities are activities designed to improve clinical practice. Each audiologist must complete at least four of these activities that I'm going to list, and each activity must be performed for 90 days or more during 2019. You will attest to your performance in the EIDM system. You can learn more about the improvement activities at the links I've provided. You can build your own improvement activity list. MIPS Improvement Activity Examples:
- Implementation of formal quality improvement methods, practice changes, or other practice improvement processes.
- Implementation of improvements that contribute to more timely communication of test results.
- Implementation of practices/processes for developing regular individual care plans.
- Implementation of Use of Specialist Reports Back to Referring Clinician or Group to Close Referral Loop.
- Improved Practices that Disseminate Appropriate Self-Management Materials.
- Improved Practices that Engage Patients Pre-Visit.
- Integration of patient coaching practices between visits.
- Leadership engagement in regular guidance and demonstrated commitment to implementing practice improvement changes.
- Participation in a 60-day or greater effort to support domestic or international humanitarian needs.
- Participation in Joint Commission Evaluation Initiative.
- Participation in Population Health Research.
- Participation in private payer clinical improvement activities.
- Participation in User Testing of the Quality Payment Program Website (https://qpp.cms.gov/)
- Practice Improvements that Engage Community Resources to Support Patient Health Goals.
- Promote Use of Patient-Reported Outcome Tools.
- Provide Clinical-Community Linkages.
- Provide Education Opportunities for New Clinicians.
- Provide peer-led support for self-management.
- Regular training in care coordination.
- Regularly assess the patient experience of care through surveys, advisory councils and other mechanisms.
- Tobacco use.
- Unhealthy alcohol use.
- Use evidence-based decision aids to support shared decision-making.
- Use of telehealth services that expand practice access.
- Collection and follow-up on patient experience and satisfaction data on beneficiary engagement.
- Collection and use of patient experience and satisfaction data on access.
- Completion of an Accredited Safety or Quality Improvement Program.
- Completion of the AMA STEPS Forward program.
- Depression screening.
- Engage Patients and Families to Guide Improvement in the System of Care.
- Engagement of New Medicaid Patients and Follow-up.
- Evidenced-based techniques to promote self-management into usual care.
- Implementation of condition-specific chronic disease self-management support programs.
- Implementation of documentation improvements for practice/process improvements.
- Implementation of episodic care management practice improvements.
- Implementation of fall screening and assessment programs.
Reporting Positive Action
Measure Codes
Referral for Acute or Chronic Dizziness
You need to report it at least once per calendar year for 50% of eligible patients. You want a positive reporting, that means that the patient was referred for an otologic evaluation because of dizziness or BPPV, or they are not eligible because they are either already under the care of a physician for this acute or chronic dizziness. The third if you didn't refer them, that would be a negative reporting, and it's just like you didn't report it all. Again, this is the only measure that we have that you need to have a combination of a diagnosis code and a procedure code.
- 92540, 92541, 92542, 92543, 92544, 92545, 92546, 92547, 92548, 92550, 92557, 92567, 92568, 92570, 92575
- Patients that have any of these CPT codes (as well as the ICD-9 CM codes below) fit into the measure’s denominator (the eligible patients for a measure).
- R42 or H81.11, H81.12 or H81.13
Referral Codes:
- G8856: Referral to a physician for otologic evaluation.
- G8857: Patient is not eligible for the referral for otologic evaluation (e.g., patients who are already under the care of a physician for acute or chronic dizziness).
- G8858: Referral to a physician for an otologic evaluation not performed, reason not specified.
- Eligible to report this measure if you perform 92540, 92541, 92542, 92543, 92544, 92545, 92546, 92547, 92548, 92550, 92557, 92567, 92568, 92570, 92575
- And you have a diagnosis of R42 or H81.11, H81.12 or H81.13
Documentation of Current Medications
This is for every patient at every visit for 50% of eligible patients. Anytime we perform any audiologic testing and it's irrespective of diagnosis code. Now, you need to get the frequency, dosage, drug name, and the route. Is it an injection, pill, a spray? Whatever that is, that needs to be in your documentation.
Every healthcare provider is asking these questions. If it comes over to you, you just need to verify it. Go through the medications they have, review the last time they saw you or someone else and make sure that those are correct. You need to do this to the best of your ability. This is the evidence-based practice of audiology. It is so important that you know a patient's medications. Whether or not it's a diagnostic visit or a hearing aid appointment. If a patient's on ototoxic medications, it's going to impact what kind of hearing aid you choose because their hearing may be progressive. It's something that every patient should be instructed to bring in at scheduling. Sometimes you may need to call the primary care physician or the pharmacy to get a comprehensive list, and many patients carry them with them.
Screening for Clinical Depression
This measure is not optional. It was optional at one point, but it's not optional. You need to do it once per calendar year for 50% of eligible patients. Report on the measure when:
- Allowed by your state licensure law (when deemed within the scope of practice of an audiologist within your state; determined through written contact with your state licensing board).
- It is the responsibility of the provider to do this.
- You are appropriately trained and competent to perform a depression screening using a standardized tool AND create a patient plan of care based upon the results of the screening.
- A follow-up plan of care is created, implemented, and documented in the medical record.
- Must, at a minimum, make a referral to a practitioner who is qualified to diagnose and treat depression
Here are the measure codes for clinical depression:
- G8431: Positive screen for clinical depression using an age appropriate standardized tool and a follow-up plan documented.
- G8510: Negative screen for clinical depression using an age appropriate standardized tool and a follow-up plan documented.
- G8433: Screening for clinical depression using an age appropriate standardized tool not documented, patient not eligible/appropriate.
- Patient refuses to participate
- G8432: No documentation of clinical depression screening using an age appropriate standardized tool.
- G8511: Positive screen for clinical depression using an age appropriate standardized tool documented, follow-up plan not documented, reason not specified.
Here are the appropriate depression screening tools:
- Patient Health Questionnaire (PHQ-9)
- Beck Depression Inventory (BDI or BDI-II)
- Center for Epidemiologic Studies Depression Scale (CES-D)
- Depression Scale (DEPS)
- Duke Anxiety-Depression Scale (DADS)
- Geriatric Depression Scale (GDS)
- Cornell Scale Screening
- PRIME MD-PHQ2
Falls Risk Assessment
Report at least once per calendar year for 50% of eligible patients. A risk assessment must include balance, gait and one or more of the following: postural blood pressure, vision and home fall hazards. Documentation on whether or not medications are a contributing factor to falls within the last 12 months is also required.
- Medical record must include documentation of observed transfer from a chair and walking or use of a standardized scale or documentation of referral for assessment of balance and gait.
- Medical record could include documentation that patient is functioning well or not functioning well with vision or documentation of referral for assessment of vision.
- Medical record could include documentation of counseling on home falls hazards or documentation of inquiry on home falls hazards or documentation of referral for evaluation of home falls hazards.
- Medical record could include documentation of whether or not the patient’s current medications could be contributing to falls.
Falls risk assessment tools:
- https://www.mnfallsprevention.org/professional/assessmenttools.html
- Get Up and Go: https://www.aan.com/Guidelines/home/GetGuidelineContent/273and https://www.rheumatology.org/I-Am-A/Rheumatologist/Research/Clinician-Researchers/Timed-Up-Go-TUG
- Tinetti: https://consultgerirn.org/uploads/File/Tinetti_Assessment_Balance.pdfand https://www.bhps.org.uk/falls/documents/TinettiBalanceAssessment.pdf
- Berg: https://www.aahf.info/pdf/Berg_Balance_Scale.pdfand https://www.unmc.edu/media/intmed/geriatrics/nebgec/pdf/frailelderlyjuly09/toolkits/timmbergbalancescale.pdf
Case history questions. Many of the questions to meet these criteria can be answered on a very well-constructed intake form. Have you ever experienced dizziness, unsteadiness or vertigo? Please describe how often. Have you fallen within the past 12 months? If so, were you injured? Describe your injury. Do you experience visual difficulties or disturbances? Do you take a vitamin D supplement? In your plan of care, if a patient does not take a vitamin D supplement, you are going to need to recommend medication management and their falls risk. Falls risk is that they've fallen two or more times in the past year or one time with an injury. With their falls risk, they need to have a plan of care created for them.
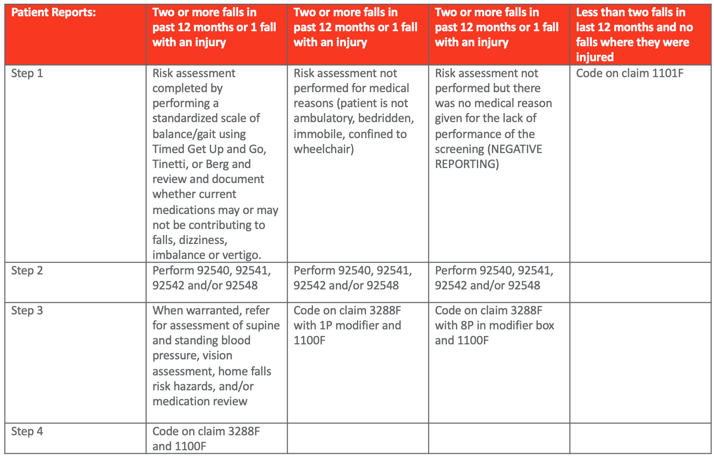
Table 4. Falls risk assessment measure codes.
Falls risk plan of care. If the patient is deemed a falls risk, then you need to make sure that you create the plan of care. The plan of care must include that you are recommending balance and gait training or vestibular rehab. Also, that you are recommending medication management with vitamin D supplementation if the patient isn't already taking them, and this is really at a minimum. Remember, the patient's a falls risk if they've fallen two or more times in the past year or they've been injured by a fall at least once in the past year.
Screening for Tobacco Use
Again, it needs to be performed at least once per calendar year for 50% of eligible patients. This is if you perform a basic vestibular evaluation, audiogram, or an assessment of tinnitus. You'd advise a patient to quit tobacco use and refer the patient to a physician for counseling or pharmacological options. You can have this in your case history to find out if the patient needs the tobacco cessation test assessment: have you ever used a tobacco product in the past 24 months? How often and what type of products have you used?
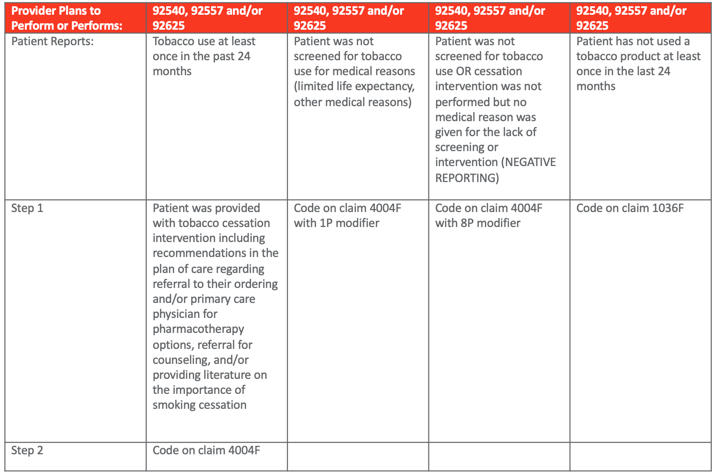
Table 5. Screening of tobacco use codes.
Planning Ahead
Now, planning ahead for MIPS in 2020 and beyond, there are some measures to consider. A lot of these measure were ones that they wanted us to be involved in audiology when PQRS was in its retirement phase, so we could very much see these measures reemerging. One is Elder Maltreatment Screen and follow-up plan. I would tell you that Elder Maltreatment screens are actually part of licensure in Illinois. Elder abuse is mandatory reporting and you have to screen and document it if you suspect elder abuse. It's not uncommon to see in licensure. Body mass index, blood pressure, blood pressure has such a tie to vestibular and pulsatile tinnitus, and pain, which is one of the warning signs of ear disease. So these are things you might want to prepare in advance that you might want to start to explore. I would really like to thank everyone for being part of today's course.
Citation
Cavitt, K. (2019). 2019 Coding and reimbursement update, Article 24685. Retrieved from https://www.audiologyonline.com