Promoting Social Engagement and Exploring the Benefits of Signia IX Multistream Architecture
AudiologyOnline: You’re an industry veteran who has written many articles and conducted dozens of webinars for us at AudiologyOnline over the past 20 years, what are some of the recent trends in Audiology that are capturing your attention?
Brian Taylor, AuD: The first thing that comes to mind is artificial intelligence (AI) and how AI continues to evolve in hearing healthcare, and more specifically, hearing aids. Don Nielsen and Joshua Alexander, respectively, summarized these topics in their 20Q articles last year so well that I don’t need to talk about them – just click on these links and read for yourself.
Beyond AI, one topic that has interested me recently is healthy aging and the role audiologists play in helping older people maintain or restore an active lifestyle. Kathy Pichora-Fuller writes a column for Canadian Audiologist, What’s New About Getting Older, that is a must-read. I was particularly struck by one of her 2024 columns, Loneliness is Not an Age-Related Problem that Audiologists Can Solve Alone. In this column, she discusses the difference between social isolation and loneliness and how hearing loss might affect these conditions. Additionally, her article provides a concise overview of how social isolation and hearing loss might contribute to cognitive decline in older adults.
Shortly after I read this column, I was with my family in south Florida to visit my recently widowed mother-in-law. She lives in a large retirement complex with hundreds of seniors. It was astounding to see the number of older adults with this “triple-threat” problem: They live alone, have trouble hearing and do not wear hearing aids. So many times, I encountered someone at the mailbox, pool or fitness center and had to practically shout at them during our conversations because he or she couldn’t hear. The most interesting part is that all these individuals are healthy enough to lead a completely independent existence, but they live alone. This experience got me thinking, how can properly fitted hearing aids promote better social engagement?
AudiologyOnline: What do you mean by social engagement?
Brian Taylor, AuD: Social engagement refers to the degree of involvement or participation an individual has in social activities, interactions, or relationships within their community or society. In short, it is one essential type of human connectedness. Social isolation and loneliness are two independent, yet related components of social engagement.
There is research suggesting social engagement is essential for promoting well-being, community cohesion, and the overall functioning of society. It can also enhance an individual's sense of belonging and purpose. Of course, it’s important to acknowledge there is tremendous individual variation in just how much social engagement a person might want or need. But it is also safe to say that for aging adults, hearing loss often gets in the way of social engagement. For example, a recent study indicated that many persons with hearing loss describe a lack of effective coping strategies and tended to rely on avoidance of social interactions, which deepened their isolation and loneliness (Bennett, et al 2022). Your readers also might find it interesting that a couple of recent extensive literature reviews (Shukla, et al 2020, and Bott and Saunders, 2021) determined there is a link between both social isolation and loneliness and untreated hearing loss.
AudiologyOnline: What role might audiologists play in promoting social engagement?
Brian Taylor, AuD: The simple answer is to fit hearing aids and ensure they are worn properly. Beyond that, Pichora-Fuller, in her article linked above, mentions social prescribing, which involves referring those at risk for social isolation and loneliness to agencies and services that promote social involvement. In my opinion, social prescribing could be as basic as encouraging patients to join a bowling league or coffee klatch. You could even say that group aural rehabilitation courses are a form of social prescribing, but these types of in-person classes for patients have generally fallen out of favor in the US.
AudiologyOnline: Tell us more about how hearing aids might promote social engagement.
Brian Taylor, AuD: Although Bott and Saunders’ (2022) scoping review uncovered a handful of studies that suggested hearing aids and/or cochlear implants reduce social isolation/loneliness, this an area that needs more research.. There are several potential benefits of hearing aids that might promote better social engagement. Better communication both one-on-one and in groups, reduced cognitive load, increased confidence in social situations and restored enjoyment of music are some that come to mind.
AudiologyOnline: You mentioned this is an area that would be benefit from more research. There must be a few studies that have examined how hearing aids might help promote better social engagement.
Brian Taylor, AuD: To date, the small number of studies have shown mixed results. One study (Dawes et al 2015) examined several health-related outcomes including social engagement on a large sample size of about 650 adults. They used a proxy measure of social engagement: the average number of hours per week spent in solitary activities using a computer, watching TV, or reading. They found no significant differences between hearing aid users and non-users in social engagement. Essentially, hearing aid use did not change the amount of time involved in these more solitary activities.
Another study conducted in the UK with a very different design had a different outcome. They divided 106 adults with hearing loss into two groups (Holman et al 2021). The intervention group was fitted with their first pair of hearing aids and the control group were not fitted. Both groups had to complete a battery of self-report outcome measures four times: before the fitting, and at 2-weeks, 3-months, and 6-months post-fitting. These self-reports captured several variables related to fatigue, listening effort, social participation restrictions, as well as work, social and physical activity levels. The researchers found that social activity level increased and social participation restriction decreased significantly after hearing aids were fitted to the intervention group. The control group did not experience these benefits to social engagement.
AudiologyOnline: Let’s turn our attention to hearing aid technology. What features help with listening situations that involve social interactions?
Brian Taylor, AuD: Let’s assume that most social interactions involved two variables: 1.) background noise and reverberation, and 2.) multiple talkers or sounds of interest. All manufacturers rely on some combination of wide-dynamic range compression to restore audibility and microphone technology + processed-based noise cancellation to manage the signal to noise ratio (SNR) in these listening environments. Today all manufacturers offer increasingly sophisticated signal processing strategies that combine directional microphones, digital noise reduction and compression to enhance patient benefit in noisy, multi-talker situations --- places where a lot of social interaction typically occurs. One of the more interesting aspects of hearing aid dispensing these days is trying to understand how each manufacturer implements these features in their devices. All have a unique approach to how directionality, noise reduction and compression work together.
AudiologyOnline: I recall reading in a 20Q article from February 2024 by Richard Windle that said for older adults directionality it is always beneficial to improve the SNR of the listening situation. Why not just fit all patients with a basic, adaptive directional microphone system? After all, isn’t directionality pretty much the same across all manufacturers?
Brian Taylor, AuD: Yes, all manufacturers provide directionality in their hearing aids, but how they work is often quite different. With one or two exceptions, I don’t think you can find a “basic,” adaptive two-microphone directional system in a prescription hearing aid today. Like all the other features, directional microphones are getting extremely sophisticated, and every manufacturer has a different implementation of either a two-mic or four-mic array. Let me first describe a “basic,” or perhaps better stated, a traditional approach to directionality.
Let’s take a walk down memory lane. I think it will help us appreciate the current level of sophistication in directional microphone systems. More than 30 years ago, hearing aids employed decent-quality directional microphones that boosted sounds, usually speech coming from the front of the wearer, while reducing sensitivity for sounds typically originating from the back and sides of the wearer. Several studies, reviewed by Bentler (2005), demonstrated that these two-microphone arrays, also known today as unilateral beamformers, did a good job of improving the wearer’s SNR when speech is arriving from the front.
Anyone fitting these older unilateral beamformers, however, is keenly familiar with their limitations. Optimizing SNR improvements was predicated on getting the talker(s) of interest in the so-called “sweet spot” where sounds were boosted the most. This directional region of sensitivity was typically wide enough that it often included unwanted noise from the side (off-axis locations), yet it was too narrow to boost the speech of more than one talker.
Some of these limitations associated with two-mic array, unilateral beamformers were addressed with the introduction of 4-mic array, bilateral beamformers. Although studies show modest SNR improvement in bilateral beamformers compared to unilateral beamformers (Kumar, et al 2023, for a review), they still have some of the same limitations associated with unilateral beamformers, as described above.
AudiologyOnline: That’s a nice review of directionality. Tell us about Signia’s current iteration of this technology.
Brian Taylor, AuD: Signia’s latest approach to directionality, found in the IX product line, relies primarily on a feature trademarked, RealTime Conversation Enhancement (RTCE). This feature is based on multistream architecture (MSA), which was designed and engineered to leverage the benefits of bilateral beamforming while addressing its shortcomings in multi-talker situations.
AudiologyOnline: Tell us how RealTime Conversation Enhancement based on multistream architecture works?
Brian Taylor, AuD: Multistream architecture builds upon existing split-processing technology, which was introduced in IX's predecessor, Signia’s Augmented Xperience (AX) platform. In its original implementation on the AX platform, split-processing employed adaptive unilateral beamformers to separate signals arriving from the front and rear of the wearer. (Note that in noisy situations in which the intensity level above ~70-72dB SPL, bilateral beamforming was activated).
With the introduction of IX, with RTCE and multistream architecture (MSA), this split-processing strategy now operates with more specificity for sounds coming from the front of the wearer. Specifically, the algorithm in IX, RealTime Conversation Enhancement, first analyzes the input signals to detect speech sources, estimates talker locations and models turn-taking dynamics of multi-talker conversations. Several front-facing bilateral and unilateral beamformers are then deployed, as necessary, to provide a boost in gain for multiple talkers in the frontal hemisphere of the wearer. Consequently, the multibeam processing in RTCE can detect and track multiple talkers in a group conversation, allowing the wearer to focus on each talker.
AudiologyOnline: What evidence do you have that RTCE in Signia IX is effective?
Brian Taylor, AuD: We have conducted multiple studies, using a variety of research methods, which demonstrate its effectiveness.
The first set of studies proving the efficaciousness of IX’s multistream architecture are what I call benchtop studies. Benchtop studies are often used in Industry to authenticate new features. That is, demonstrate that new features work as intended. Our engineers conducted two benchtop studies using the Hagerman phase-inversion technique. This is a common procedure used in hearing aid research to accurately measure the signal-to-noise ratio (SNR) at the output of a hearing aid by presenting the same sound with an inverted phase, allowing researchers to isolate and analyze the speech signal separately from background noise. The Hagerman technique is commonly used in benchtop studies to evaluate the efficacy of a hearing aid's noise reduction algorithms on the KEMAR.
In the first benchtop study, using the Hagerman approach, in a simulated, noisy group conversation of +4 dB SNR, IX yielded an absolute SNR improvement of 8 dB compared to unaided listening. Additionally, in this simulated noisy situation, IX did 4 dB better than the closest competition.
Subsequently, in the autumn of 2024, following competitors’ recent product launches, we wanted to compare the performance of IX to these new devices. Results showed that IX still outperformed the closest competition in this simulated environment by more than 3dB. I would encourage readers to check out the details of these studies by clinking on the above links.
AudiologyOnline: So, in a carefully controlled lab experiment that didn’t involve humans, you showed some significantly better performance compared to other processing strategies. What about studies that used actual hearing aid wearers?
Brian Taylor, AuD: Signia researchers have conducted a variety of laboratory studies, too. In one, using sentence-length speech material made to simulate a multi-talker situation in a reverberant classroom, there was a 1.1dB benefit, which was estimated to be ~20% improvement in intelligibility, with RTCE and MSA activated in the hearing aids.
In other lab-based studies, Signia researchers have demonstrated RTCE and MSA have positive effects on how the brain processes speech in background noise, including enhancing contrasts between speech sounds in the wearer’s soundscapes using the mismatch negativity (MMN) and reducing neural signatures of listening effort as quantified by alpha power in the electroencephalogram (EEG).
Most recently, in a direct comparison to a recently launched device that uses a deep neural network for noise reduction, Signia IX yielded an average SNR improvement of between 1.3 and 2.8 dB over the DNN-based feature in the competitor’s device. This equates to 14% improvement in word and 17% improvement in sentence understanding at a SRT criterion of 50%. A majority (60%) of participants also rated listening significantly less effortful with Signia IX than the competitor’s device. Additionally, the researchers found that Signia IX yielded 85% relative improvement in noise tolerance compared to the competitor’s hearing aid. This equates to an increase in the duration of time listeners were willing to stay in noise by seven minutes with IX compared to the DNN technology. Again, I encourage readers to click on the links above to read the details for themselves.
AudiologyOnline: Thanks for sharing those studies. I can see that Signia’s research team has been quite busy. Although lab studies are helpful, they don’t always relate to listening in the real world. Do you have any real-world studies using IX?
Brian Taylor, AuD: Yes. Researchers at Western University conducted a wearer preference study in a busy mall. Hearing aid wearers were asked to judge several listening criteria including clarity, background noise, listening effort and focus as they participated in conversations with MSA-on versus MSA-off. Ratings for preference between programs indicated a significant preference for the MSA-on condition. This study was published in Sept 2024 at the American Journal of Audiology and it can be accessed here. Results of this real-world study demonstrate that Signia’s multistream architecture leads to superior performance in social situations.
AudiologyOnline: Thanks for sharing. Before we end, any final thoughts?
Brian Taylor, AuD: Although these technological advances give us a lot to be excited about, I believe that audiologists need to continually balance their enthusiasm for technological innovations with the need to deliver humanistic care. As smart as these algorithms inside modern hearing aids are, they’re still not a replacement for promoting human connections – a facet of everyday life that require the person-centered skills of a clinician. Technology is merely a tool for improving the quality of life and human flourishing of individuals with hearing loss. In that spirit, I leave your readers with a challenge. Figure 1 illustrates what author Ted Gioia calls the 8 Pathways to Human Connection. Given the prevalence of social isolation, loneliness and hearing loss is our aging communities, make it your mission to find the important pathways for each patient in your clinic that will help them get reconnected. Chances are good that the combination of well-fitted hearing aids and humanistic counseling will restore these pathways.
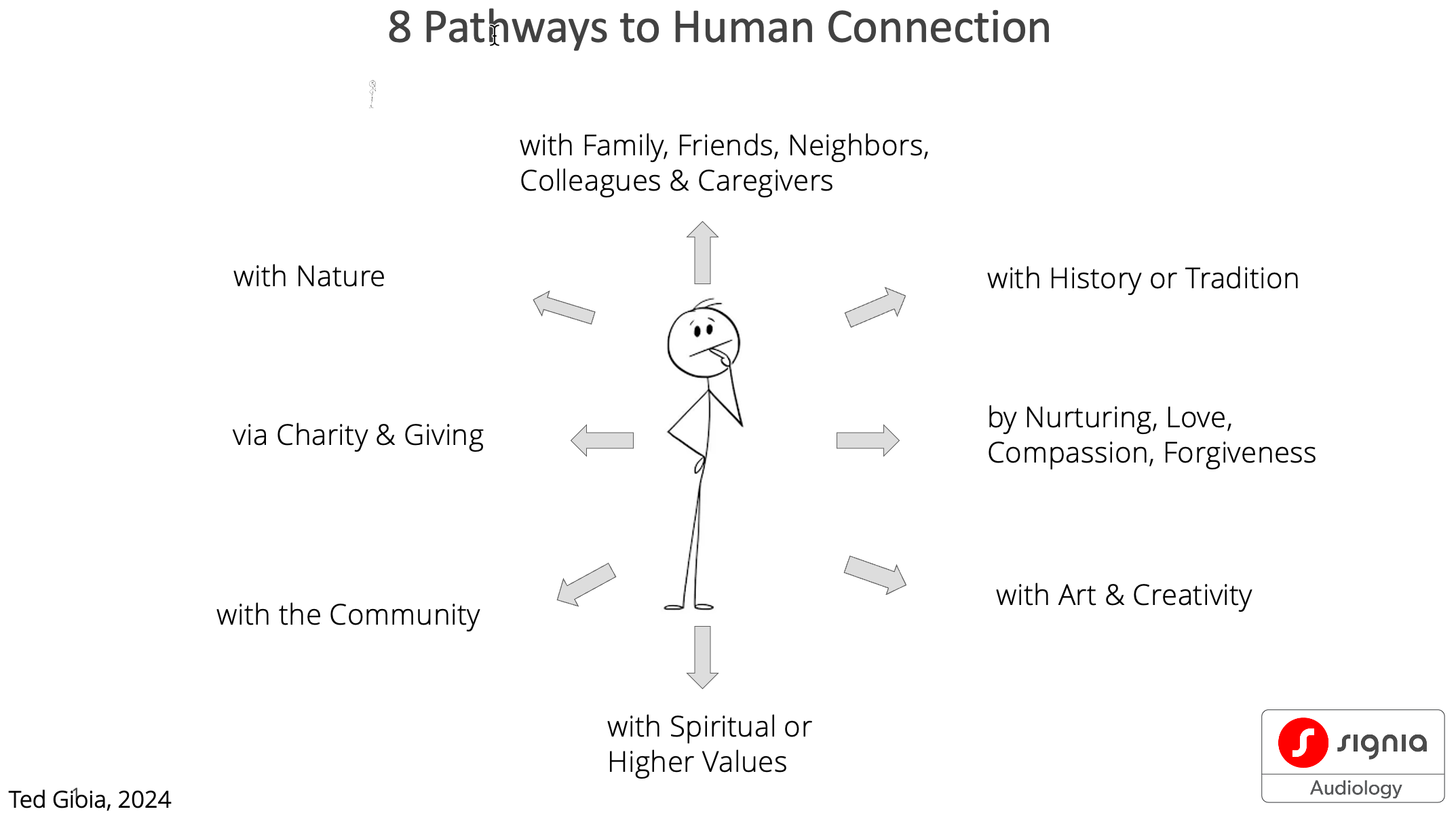
Figure 1. The 8 pathways of human connection that can be restored for the individual with hearing loss through audiologic intervention.
References
Bennett, R. J., Eikelboom, R. H., Sucher, C. M., Ferguson, M., & Saunders, G. H. (2022). Barriers and facilitators to delivery of group audiological rehabilitation programs: a survey based on the COM-B model. International journal of audiology, 61(2), 130–139.
Bentler R. A. (2005). Effectiveness of directional microphones and noise reduction schemes in hearing aids: a systematic review of the evidence. Journal of the American Academy of Audiology, 16(7), 473–484.
Bott, A., & Saunders, G. (2021). A scoping review of studies investigating hearing loss, social isolation and/or loneliness in adults. International journal of audiology, 60(sup2), 30–46.
Dawes, P., Cruickshanks, K. J., Fischer, M. E., Klein, B. E., Klein, R., & Nondahl, D. M. (2015). Hearing-aid use and long-term health outcomes: Hearing handicap, mental health, social engagement, cognitive function, physical health, and mortality. International journal of audiology, 54(11), 838–844.
Holman, J. A., Drummond, A., & Naylor, G. (2021). Hearing Aids Reduce Daily-Life Fatigue and Increase Social Activity: A Longitudinal Study. Trends in hearing, 25, 23312165211052786.
Kumar, S., Guruvayurappan, A., Pitchaimuthu, A. N., & Nayak, S. (2023). Efficacy and Effectiveness of Wireless Binaural Beamforming Technology of Hearing Aids in Improving Speech Perception in Noise: A Systematic Review. Ear and hearing, 44(6), 1289–1300.
Shukla, A., Harper, M., Pedersen, E., Goman, A., Suen, J. J., Price, C., Applebaum, J., Hoyer, M., Lin, F. R., & Reed, N. S. (2020). Hearing Loss, Loneliness, and Social Isolation: A Systematic Review. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery, 162(5), 622–633.
All Signia hearing aid studies linked above can be found here in the online Signia Professional Library.
Brian Taylor, AuD, is the senior director of audiology for WSA. He can be contacted at brian.taylor@wsa.com.


